Short abstract
Given the widespread adoption and technical possibilities of mobile technology, mobile health apps could be potentially effective tools to intervene in people’s daily routines and stimulate physical activity. Self-determination theory and the motivational technology model both suggest that mobile technology can promote health behaviour change by allowing users to customize their online experience when using mobile health apps. However, we know very little about why and for whom customization is most effective. Using a between-subjects experimental design, we tested the effects of customization in mobile health apps among a convenience sample (N = 203). We assessed the effects of customization on perceived active control over mobile health apps, autonomous motivation to use mobile health apps, and intention to engage in physical activity, and tested the moderating role of need for autonomy. Structural equation modelling showed that customization in mobile health apps does not increase perceived active control, autonomous motivation, or the intention to engage in physical activity. However, an interaction effect between customization and need for autonomy showed that customization in mobile health apps leads to higher intentions to engage in physical activity for those with a greater need for autonomy, but not for those with a lesser need for autonomy. The implications for theory and practice are discussed.
Keywords: Customization, mobile health apps, need for autonomy, active control, autonomous motivation, physical activity
Introduction
Physical inactivity is a leading risk factor for global mortality, and it drastically increases people’s chances of being diagnosed with life-threatening diseases, including heart disease, stroke, diabetes and cancer.1–3 Globally, it has been estimated that one in four adults are insufficiently active.3 Although research has shown that the majority of people intend to engage in physical activity, nearly half of them fail to act upon those intentions.4 A growing amount of research proposes that mobile health apps could be valuable and potentially effective tools to encourage people to engage in behaviours associated with a healthy lifestyle, such as physical activity.5,6 As smartphones and other wearable technology such as smart watches and bracelets have become an integral part of our lives, they may be especially suitable to intervene in people’s daily routines.5–7
Based on assumptions from self-determination theory,8 the motivational technology model9 argues that customization in mobile health apps is expected to provide autonomy support in the sense that it enhances the user’s perceived active control over the mobile app environment and thereby helps users form autonomous motivation to use mobile health apps. Customization refers to the ability to self-tailor the mediated environment – such as mobile health app content and features – to match one’s individual preferences.9,10 The formation of autonomous motivation, that is, when an individual experiences free choice and makes a conscious decision to do something, is important to initiate health behaviour change and maintain change in the long-term.8 However, not all mobile apps are necessarily perceived as autonomy supportive to all individuals. Although self-determination theory suggests that everyone has a basic need for autonomy, individual differences exist in the need for autonomy regarding health-related decisions.11,12 Therefore, whether mobile health apps increase people’s perceived active control and autonomous motivation to use mobile health apps, and subsequently help to support health behaviour change, depends not only on the affordances mobile technology can offer (e.g. customization), but also on individual differences in their need for autonomy.
Most mobile health technologies are not evidence- or theory-based,13–15 and currently only have a small to moderate impact on health behaviour change.16,17 This calls for more systematic knowledge to enhance our understanding of what makes mobile health apps effective and for whom. We therefore adopted a theory-based approach using self-determination theory to examine how customization in mobile health apps and individuals’ need for autonomy can help explain physical activity. More specifically, this article explores the effects of customization in mobile health apps on people’s intention to engage in physical activity, examines perceived active control over and autonomous motivation to use mobile health apps as the underlying mechanisms explaining customization effects, and investigates the role of need for autonomy as a potential moderating factor of effects.
Understanding customization in mobile health apps
In mediated environments, such as in mobile health apps, a customizable interface can be modified based on explicit user input and provides information that is tailored to the user as a unique individual.10 Customization differs from traditional tailoring in the way the personalization process occurs. Where traditional tailoring typically starts with an assessment of individual characteristics, which is then used as input for system-driven algorithms to deliver tailored content in a preplanned format,18 customization offers the individual user a central role in the personalization process by enabling users to take active control over the content, which enhances a sense of autonomy.9,19 While tailoring has gained substantive attention over the past decades, especially in the field of health communication,20–22 research into customization is still in its nascent stages.
The motivational technology model has made a first attempt to explain customization effects. This model draws upon self-determination theory to understand the key psychological processes involved in the use of self-monitoring technologies, such as mobile health apps. By applying key principles of self-determination theory to online technology, such as mobile health apps, the motivational technology model argues that letting users navigate, interact, and customize their own online health experience should produce feelings of competence, relatedness, and autonomy, respectively.9 According to self-determination theory, competence, relatedness, and autonomy are essential for one to be autonomously motivated toward a goal.8 In human–computer interaction research, it has been repeatedly shown that increasing the navigability of technology enhances users’ feelings of competence,23,24 and in computer-mediated communication research, there has been a strong focus on how interactivity between individual users has an impact on feelings of relatedness in online communities.25,26 Yet, the effects of customization have rarely been studied. Therefore, the focus of this study will be on testing the part of the motivational technology model that involves customization.
The motivational technology model links customization to self-determination theory’s concept of autonomy, because having active control over online content and features and the possibility to adapt these to one’s preferences may create a feeling of autonomy. In addition to perceived involvement and perceived identity, the agency model of customization introduces perceived active control as one of the key psychological mechanisms that explain the relationship between customization and outcomes.19 Perceived active control is particularly relevant to customizable mobile health apps, as it allows users to actively control how the technology works.27 Based on the theoretical notions of the motivational technology model and self-determination theory, we discuss how customization may ultimately lead to higher intentions to engage in physical activity.
The mediating role of perceived active control and autonomous motivation
Customizable media environments encourage users to play an active role in their interaction with digital media, creating a strong sense of active control.19,27 For example, studies on customization features in games,28 web portals,10 and avatar creation,29 all show that regardless of what features could be customized, users reported a stronger sense of active control over their online experience than users who were not allowed to customize features. Through a feeling of active control, customization can build autonomy; according to self-determination theory, people are supposed to feel autonomous when they feel or understand the personal relevance of the task they are engaging in.30 The motivational technology model posits that perceived active control over one’s online experience results in greater autonomous motivation to engage in online technologies, which ultimately enhances intentions to perform health behaviours.9 While presented as a theoretical model for designing digital health applications, there is currently a lack of empirical research examining the proposed relationships between customization, perceived active control, autonomous motivation to use digital health technologies, and intentions to engage in a certain health behaviour.
In related fields, such as digital gaming and exergaming (i.e., active video gaming in which physical activity is incorporated into gameplay), the role of specific design characteristics in the effectiveness of technology has already been studied more elaborately.31 Research in these fields has demonstrated that customization features, such as the opportunity to customize one’s own avatar, ultimately enhance autonomous motivation to engage in the game.32,33 Besides, Peng et al.32 argue that the association between customization and autonomous motivation can be explained by the concept of perceived active control. That is, customization is assumed to create conditions that fulfil people’s need for autonomy through generating an increased sense of active control over the technology at hand, which ultimately leads to a greater autonomous motivation. According to the motivational technology model, such autonomous motivation could ultimately result in behaviour change, which is often the main outcome of mobile health app research.34 Thus, we hypothesize:
H1: Customization (vs. non-customization) leads to increased levels of perceived active control over mobile health apps, which in turn leads to enhanced levels of autonomous motivation to use mobile health apps, which ultimately leads to higher intentions to engage in physical activity.
The moderating role of need for autonomy
Although self-determination theory suggests that everyone has a basic need for autonomy, some people prefer to choose their own path when it concerns health-related decisions, while others have a higher need for external control and prefer to be guided by clear-cut expert advice from professionals or peers.11,12 This suggests that although customization is expected to promote behaviour change through creating an autonomy-supportive environment, customization does not have to be effective for all individuals. For customization to be effective, it has to be based on a careful match between the users’ needs and preferences on the one hand and customization features on the other.30 To illustrate, two earlier studies considered the need for autonomy in the context of offline health communication and found that newsletters that were framed in an autonomy-supportive way were more effective for people with a greater need for autonomy than newsletters that were framed in a more directive manner.11,12 In a similar vein, customization features in mobile health apps could be more effective for people with a greater need for autonomy than for people with a lesser need for autonomy, as customization features create an autonomy-supportive environment that especially matches the needs and preferences of people with a greater need for autonomy. We thus hypothesize that:
H2: The effect of customization (vs. non-customization) on the intention to engage in physical activity, as mediated by perceived active control over and autonomous motivation to use mobile health apps, is moderated by the need for autonomy, such that the effects of customization are more pronounced for people with a greater need for autonomy than for people with a lesser need for autonomy.
Methods
Design and power analysis
To test the proposed model, we used a 2 (customization: present vs. absent) × 2 (need for autonomy: lesser vs. greater) between-subjects experimental design with customization being manipulated in the experimental design and need for autonomy the quasi-experimental factor. A power analysis showed that a sample size of 179 was required to detect medium-effect sizes (statistical power = .80, alpha = .05, f = .25). Ethical approval was provided by the ethics committee of the Amsterdam School of Communication Research (reference number: 2017-PC-7994).
Stimulus material
A prototype version of a health app was developed for this study via the app prototyping platform InVision.35 InVision allows users to create interactive user experience demonstrations for web and mobile. Some prototype design features can be made directly on the platform, such as to display content on a black versus a white smartphone, but other features, such as graphic elements, have to be developed and imported from a design program, such as Adobe Illustrator. Once the design elements are in place, one can use InVision to assign different commands to the various elements, that is, when clicking on a certain place on the screen the user will be guided to a new screen within the same prototype. At the time of the study, the service cost $15 USD a month for up to three prototypes. The app prototype developed for this research took 2 weeks to test and finalize. The platform was easy to use without any prior coding or user design knowledge.
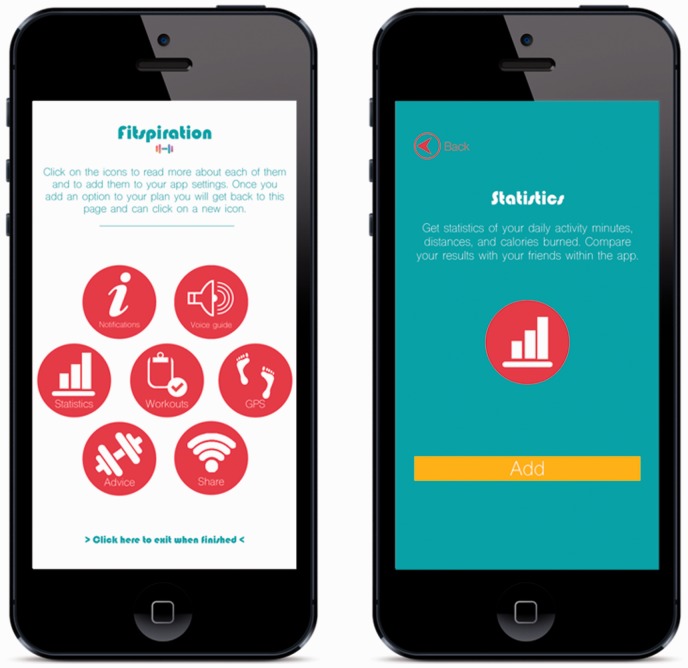
The app entailed a workout app with seven different features, which were based on a recent review on effective health app features,16 and two existing popular workout apps (i.e. Runkeeper and 7 Minute Workout). More specifically, the app included self-monitoring (i.e. statistics), feedback (i.e. voice guide and advice), and social network (i.e. share) features as proposed by Zhao et al.,16 as well as GPS, notifications, and workout features as incorporated by Runkeeper and 7 Minute Workout apps. Tapping or clicking on the different features in the home screen led participants to the separate app-feature screens. Figure 1 visualizes two screens of the prototype app.
Figure 1.
Example screens of the customizable version of the health app, including the home screen (left) and statistics screen featuring the add button (right). The non-customizable version of the health app did not include the add option, nor the instructions on the home screen on how to use the add option.
The home screen consisted of an overview of the seven features. In both conditions, participants were able to click on the features, which directed them to separate screens about each specific feature. In the customization condition, participants were able to add each of these features to their personal dashboard using an ‘add button’, which was visible on each of the separate app-feature screens. After ‘adding’ a feature, participants were directed back to the home screen, where they could continue browsing the features and add additional features to their personal dashboard. In the control condition, participants were only able to browse the features and they did not have the option to add features to their personal dashboard. To keep the customization and control condition as identical as possible, participants in the customization condition were not able to review their personal dashboard based on the features they added.
Participants and procedure
Participants were invited to take part through social media networks, emailing, and snowballing. The recruitment message contained a link to the online questionnaire. The questionnaire included questions on the personal background of participants (e.g. age, gender, education, personal interest in health) and questions regarding their need for autonomy. After those questions, participants were randomly assigned to either the customization or control condition, and were instructed to engage in a demonstration health app that was part of the online survey. The questionnaire and stimulus materials were presented in English. Participants were free to complete the survey on their laptop, smartphone or tablet. In addition, participants in the customization condition were instructed on how to use the add button within the prototype app. After engaging with the health app, participants were asked about their perceptions of the health app (e.g. perceived active control over and autonomous motivation to engage in health apps), and their intentions to engage in physical activity in the near future. A manipulation check assessed whether participants took note of the customization manipulation as intended. Furthermore, the online questionnaire recorded from which operating system participants completed the survey, informing us whether participants did so on a laptop, smartphone or tablet. All participants provided informed consent through the online questionnaire.
Measures
Intention to engage in physical activity
Intention to engage in physical activity was measured by asking the participants to indicate, on two 7-point semantic differential scales, to what degree they intended to engage in physical activity (e.g. walking, moving, biking, swimming, exercising, etc.) for at least 30 min 5 times a week for the next 3 months (1 = ‘very likely’ to 7 = ‘very unlikely’, and 1 = ‘strongly disagree’ to 7 = ‘strongly agree’).36 A mean scale was created by averaging the items, where higher scores indicated stronger intentions to engage in physical activity (M = 5.02, standard deviation (SD) = 1.57, range = 1.00–7.00; α = .78; r = .65).
Perceived active control
Perceived active control over the app was measured by the perceived active control subscale from the Interactivity Scale used by Voorveld, Neijens and Smit,37 replacing ‘website’ with ‘app’ in all items. Items included ‘I feel that I had a great deal of control over my visiting experience in this app’, which were measured on a 7-point scale ranging from 1 = ‘strongly disagree’ to 7 = ‘strongly agree’. The four items were averaged, and higher scores indicated that participants perceived more active control over the app (M = 5.47, SD = 0.90, range = 2.50–7.00; α = .82).
Autonomous motivation
Autonomous motivation to use health apps was measured by adapting four items on intrinsic motivation in physical education.38 Items included ‘Using health-related smartphone apps is fun’, and were rated on a 7-point Likert scale ranging from 1 ‘strongly disagree’ to 7 ‘strongly agree’. Items were averaged into a mean scale where higher scores indicated higher levels of autonomous motivation (M = 4.97, SD = 1.29, range = 1.00–7.00; α = .90).
Need for autonomy
Need for autonomy was assessed with the Health Causality Orientations Scale,39 which was developed based on the General Causality Orientation Scale,40 and adjusted to a health context. The scale consisted of five scenarios (e.g. You have been advised that setting goals is a good way to motivate yourself to change your health behaviours. How likely are you to set your own goals?), and participants were asked to give their opinion on a 7-point Likert scale (1 = ‘very unlikely’ to 7 = ‘very likely’). The five scenarios were averaged into a mean scale, where higher scores indicated higher levels of need for autonomy (M = 5.72, SD = 0.75, range = 3.40–7.00; α = .64). Since the range and mean suggested moderately negative skewness of the need for autonomy scale, a median split was performed to create two comparably sized groups of people with relatively lower (range = 3.40–5.80, n = 112, 55.2%) and higher (range = 6.00–7.00, n = 91, 44.8%) need for autonomy. (An overview of all measurement items can be found in the supplemental material.)
Background characteristics
We measured participants’ age, gender, level of education, nationality, and general interest in their personal health. For education, participants were asked to indicate whether they attained less than a high school graduate degree, a high school graduate degree, a bachelor’s degree in college, a master’s degree, or a doctoral degree. Participants’ interest in personal health was assessed by asking: ‘How interested are you in your personal health?’, to be rated on a 7-point scale (1 = ‘not at all’, 7 = ‘very much’). Higher scores indicated higher levels of interest in personal health.
Manipulation check
To test the manipulation of the independent variable, we asked participants whether or not they perceived the app as giving room for customization on a 7-point scale (1 = ‘not at all’, 7 = ‘very much’): ‘When using the app, did you feel that you had the opportunity to customize the app (make potential changes to the app yourself)?’
Statistical analysis
Means (M), Standard deviations (SD), and Pearson correlations for all variables are reported in Table 1. To test for successful manipulation, an independent sample t-test was conducted. The hypothesized model was tested with a structural equation model (SEM) using AMOS version 22. To maintain sufficient statistical power to test the hypothesized model and decrease the likelihood of falsely accepting the null hypothesis, we did not include any of the background variables (i.e. age, gender, education level, health interest) in the analyses. All variables were standardized using z-scores. Model fit was assessed with chi-square (χ2), the root mean squared error of approximation (RMSEA), the minimum discrepancy divided by its degrees of freedom (CMIN/DF), the standardized root mean square residual (SRMR), the Tucker–Lewis Index (TLI), and the Comparative Fit Index (CFI). To test the indirect effects, we used 5000 bootstrap samples with a 95% bias-corrected confidence interval (CI).41,42 To present the mean scores for the customization and non-customization conditions divided by the level of need for autonomy, three 2-way analyses of variance (ANOVAs) were performed with customization and need for autonomy as independent variables and perceived activity control, autonomous motivation, and intention to engage in physical activity as dependent variables. Simple effects analyses with the Bonferroni correction were performed in case of significant interaction effects.
Table 1.
Descriptive statistics and correlation matrix of study variables (N = 203).
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Age | – | ||||||||
| 2. Gendera | −.20** | – | |||||||
| 3. Educationb | −.07 | .07 | – | ||||||
| 4. Interest in personal health | .03 | .08 | −.07 | – | |||||
| 5. Condition | .04 | −.06 | .03 | −.02 | – | ||||
| 6. Perceived active control | −.09 | .06 | −.11 | .20** | −.05 | – | |||
| 7. Autonomous motivation | −.06 | .22** | −.02 | .22** | .01 | .22** | – | ||
| 8. Intention to engage in PA | .03 | .04 | −.02 | .29*** | −.01 | .03 | .21** | – | |
| 9. Need for autonomyc | .06 | −.07 | −.03 | .23** | −.03 | .03 | −.05 | .23*** | – |
| M | 32.17 | 0.69 | 0.90 | 5.91 | 0.49 | 5.47 | 4.97 | 5.02 | 0.45 |
| SD | 12.37 | 0.46 | 0.30 | 1.17 | 0.50 | 0.90 | 1.29 | 1.57 | 0.50 |
Note: aGender was dummy coded into 1 = male, 0 = female. bEducation level was dummy coded into 1 = higher-, 0 = lower levels of education. cNeed for autonomy was dummy coded into 1 = higher-, 0 = lower levels of need for autonomy,however, using the mean scale of need for autonomy resulted in similar correlation coefficients and the same (in)significant relationships between need for autonomy and the other variables.
PA = physical activity.
**p < .01. ***p < .001.
Results
Participants
In total, 306 people started the survey, of which 203 fully completed it (66.3%). We collected responses from participants residing in 31 different countries. The majority of participants resided in the Netherlands (n = 72, 35.5%) or Norway (n = 55, 27.1%). Participants were on average 32.17 years old (SD = 12.37, range = 19–69), and 69.5% of participants were female (n = 141). The majority of our participants had attained higher levels of education, such as a bachelor’s degree (n = 119, 58.6%), a master’s degree (n = 60, 29.6%), or a doctoral degree (n = 4, 2.0%), and a minority had attained lower levels of education, including high school graduate degree (n = 17, 8.4%) or less than high school graduate degree (n = 3, 1.5%). Generally, participants were interested in their personal health (M = 5.91, SD = 1.17, range = 2.00–7.00). For 48 participants (23.6%), the online survey program was – for unknown reasons – unable to successfully record from which operating system the survey was completed. Of the participants whose operating system was recorded (n = 155, 76.4%), most completed the survey on a computer (n = 119, 76.8%), some on a smartphone (n = 33, 21.3%), and a minority on a tablet (n = 3, 1.9%).
Manipulation check
A manipulation check revealed that participants in the customization condition reported significantly higher levels of perceived customization in the health app (M = 4.83, SD = 1.53) than those in the non-customization condition (M = 3.44, SD = 1.63), t (201) = −6.25, p < .001, d = 0.85, 95% CI [−1.82, −0.95]. The manipulation can thus be considered successful.
Model testing
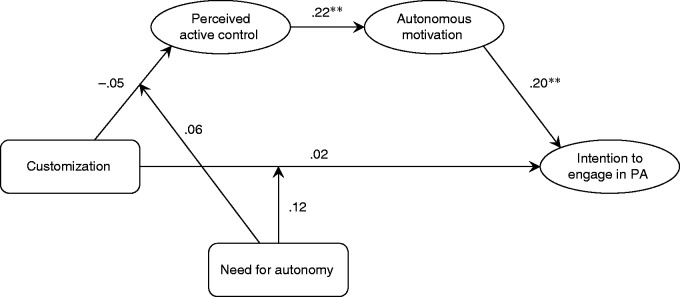
Based on the model fit criteria,43,44 our hypothesized model showed a very good fit to the data: χ2(4) = 1.05, p = .902, CMIN/DF = 0.263, TLI = 1.505, CFI = 1.000, RMSEA = .000, SRMR = .016. Figure 2 shows the standardized path coefficients and statistical significance for individual pathways in the model; the measured/observed and latent variables are denoted with rectangles and circles, respectively.
Figure 2.
Structural equation model depicting perceived active control over the health app and autonomous motivation to use health apps as serial mediators of the effect of customization on the intention to engage in physical activity, with need for autonomy as moderator of the effects. Model fit (N = 203): χ2 (4) = 1.05, p = .902, CMIN/DF = 0.263, TLI = 1.505, CFI = 1.000, RMSEA = .000, SRMR = .016. Estimates presented are standardized path estimates.
**p < .01.
We hypothesized that customization (vs. non-customization) would lead to increased levels of perceived active control over mobile health apps, which in turn would lead to enhanced levels of autonomous motivation to use mobile health apps, which would ultimately lead to higher intentions to engage in physical activity (H1). Compared with the non-customizable app, the customized app did not significantly increase participants’ perceived active control (β = −.05, p = .492). Therefore, despite the positive significant correlations between perceived active control and autonomous motivation (β = .22, p = .001), and between autonomous motivation and the intention to engage in physical activity (β = .21, p = .001), our data did not support the hypothesized indirect serial mediation effect of customization on the intention to engage in physical activity through perceived active control over and autonomous motivation to use mobile health apps (β = −.002, 95% CI [−0.01, 0.004], p = .267). We therefore reject H1.
H2 predicted that the effect of customization (vs. non-customization) on the intention to engage in physical activity, as mediated by perceived active control over and autonomous motivation to use mobile health apps, would be moderated by the need for autonomy. Therefore, it was expected that the effects of customization would be more pronounced for people with a greater need for autonomy than for people with a lesser need for autonomy. Although the data did not reveal the proposed moderated mediation effect (see Figure 2), a two-way ANOVA showed a significant interaction effect between customization and need for autonomy on the intention to engage in physical activity, F(1, 199) = 4.06, p = .045, η2 = .02. Simple effects analysis showed that in the customization condition, participants with a greater need for autonomy reported significantly higher intentions to engage in physical activity (M = 5.66, SD = 1.66) than those with a lesser need for autonomy (M = 4.50, SD = 1.62), F(1, 199) = 14.13, p < .001, η2 = .07. In the non-customizable app condition, on the other hand, no significant differences in the intention to engage in physical activity were revealed between participants with a greater (M = 5.19, SD = 1.42) versus a lesser need for autonomy (M = 4.89, SD = 1.39), F(1, 199) = 0.96, p = .327, η2 = .00. Although not mediated, this moderation effect provides partial support for H2 by demonstrating that the effect of customization on the intention to engage in physical activity is significantly stronger for people with a greater need for autonomy than for people with a lesser need for autonomy. The descriptive statistics for the simple effects analysis are presented in Table 2.
Table 2.
Descriptive statistics for all modelled variables for participants in the customization versus non-customization conditions divided by level of need for autonomy (N = 203).
|
Customization condition |
Non-customization condition |
||||||
|---|---|---|---|---|---|---|---|
| Lesser need for autonomy | Greater need for autonomy | Lesser need for autonomy | Greater need for autonomy | F | p | eta2 | |
| Perceived active control | 5.38 (0.99) | 5.48 (0.82) | 5.51 (0.81) | 5.51 (0.97) | 0.21 | .651 | .001 |
| Autonomous motivation | 4.92 (1.34) | 5.06 (1.28) | 5.13 (1.00) | 4.76 (1.54) | 2.00 | .159 | .010 |
| Intention to engage in PA | 4.50 (1.62) | 5.66 (1.66)*** | 4.89 (1.39) | 5.19 (1.42) | 4.06 | .045 | .020 |
Note: Means (with standard deviations within parentheses) and F-statistics are presented for the 2 (customization: present vs. absent) × 2 (need for autonomy: lesser vs. greater) design. Mean scores within the customization condition significantly differ between those with a greater and lesser need for autonomy. All dependent variables were measured on a 7-point scale with higher scores indicating higher perceived active control over the health app, autonomous motivation to use health apps, and intention to engage in physical activity. Eta-squared indicates the effect size of the interaction between condition and need for autonomy using the following designations: .10 = small, .25 = medium, .40 = large.
PA = physical activity.
***p < .001.
Discussion
By adopting a theory-based approach, this article aimed to enhance our understanding of how and for whom mobile health technology could be an effective tool to increase physical activity. It has been suggested that mobile health apps can provide autonomy support when people are making health-related decisions, and could thus be effective tools for fostering autonomous motivation and health behaviour change.45–47 Based on assumptions derived from self-determination theory and the motivational technology model, we examined whether a customization feature within a mobile health app, via mechanisms of perceived active control over and autonomous motivation to use mobile health apps, could create such an autonomy-supportive environment to increase people’s intention to engage in physical activity. Moreover, we tested whether the effects of customization hold for all types of individuals in terms of their need for autonomy. Our results showed that individual differences in need for autonomy may influence the effectiveness of autonomy-supportive tools and features, such as mobile health apps and customization.
The first important finding of our study was that need for autonomy may help explain the conditions under which customizable health tools could be effective. Although customization did not necessarily lead to higher intentions to engage in physical activity for all individuals, it did for people with a greater need for autonomy. This extends the notion that individual differences are important considerations when it comes to health-related need for autonomy; our study showed that these individual differences may have an impact on the effectiveness of health technologies, such as mobile health apps. Scarce previous research has centred on the moderating effect of need for autonomy in the context of health, mainly focusing on the way in which health information was framed (i.e. autonomy-supportive vs. directive frame).11,12 This study not only adds to the limited knowledge about the prevalence and impact of the health-related need for autonomy, but also extends this knowledge to a mobile health app setting, demonstrating that mobile health app features, such as customization, can differently impact behavioural intentions dependent on individuals’ need for autonomy.
The second finding we would like to highlight is that despite the absent relationship between customization and the proposed underlying mechanisms of behavioural intention (i.e. perceived active control over and autonomous motivation to use mobile health apps), we found significant relationships between the proposed serial mediators and the intention to engage in physical activity. It therefore seems that if a mobile health app is able to trigger these underlying mechanisms (i.e. perceived active control and autonomous motivation), it could affect health outcomes, such as physical activity, through increased intention. However, our manipulation of customization did not lead to increased perceived active control over the study’s mobile health app, and thus not to the desired increase in intention. It is possible that our way of realizing customization did not create a strong sense of perceived active control over the mobile health app. Instead, it is plausible that the effect of customization on intention to engage in physical activity among participants with a greater need for autonomy could be explained by other underlying processes that have been identified in tailoring literature, such as increased attention to the app content or increased perceived personal relevance.20,48 The elaboration likelihood model of persuasion49 explains that the degree of perceived personal relevance of information increases one’s motivation to elaborate on this. Accordingly, it could be that participants with a greater need for autonomy perceived the customizable app as more personally relevant, which increased their motivation to use the app content and features more elaborately.
Furthermore, our findings present important implications for theory and practice. For theory, our results help unpack the mechanisms that are (not) at work in explaining customization effects. From a theoretical perspective,8,9 it is anticipated that creating autonomy-supportive environments through customization could enhance perceived active control over and autonomous motivation to use mobile health apps, and ultimately lead to behaviour change. Our findings, however, show that customization in the form of an add button in mobile health apps does not necessarily trigger mechanisms of perceived active control over mobile health apps. This finding calls for investment in research that identifies and tests the effectiveness of different types of customization features. Moreover, it should be noted that this study only focused on customization as a way of enhancing autonomous motivation and behavioural intentions. The motivational technology model also suggests considering ways to improve the navigability and interactivity of technology to elicit feelings of competence and relatedness, respectively, which also contribute to enhancing autonomous motivation.9 In a similar vein, the agency model of customization also suggests looking at perceived involvement and perceived identity as explanatory mechanisms of customization effects.19,27 Both extending and deepening our theoretical and empirical knowledge could enhance our understanding of how best to create online environments that actually lead to health behaviour change.
Moreover, we demonstrated the importance of considering individual differences when designing mobile health apps, as various app features might not be equally effective for all individuals. This finding strengthens the idea of tailoring content and features of mobile health apps based on people’s need for autonomy.39 One way to cater to people’s varying need for autonomy would be to offer a customization feature in mobile health apps that is content-tailored by default. For example, such apps could start with a basic assessment of personal characteristics (e.g. age, weight, height) and preferences (e.g. frequency of receiving notifications, targeted goals), on the basis of which the app could provide tailored information to the individual user.18 Such tailored information is expected to benefit a variety of (health-related) outcomes because it provides personally relevant feedback.20,21,50 Based on the findings of our study, future mobile health apps may benefit from adding customization features to ensure that – especially for those with a greater need for autonomy – users can exert active control over changing certain information elements. Mobile health apps could easily apply such tailoring strategies, making it an especially interesting tool to offer personalized health information to a wide variety of individuals.
Limitations and future research directions
This study has some limitations that need to be addressed. First, although participants in the customization condition experienced higher levels of perceived customization than participants in the non-customization condition, the perceived level of customization in the customization condition was still relatively low. Customization in this study was realized by including an add button in the mobile health app, which created the perception that participants could actually add workout options to their personal plan. As there was no personal plan to be reviewed in the study’s mobile health app (because it was a prototype), we could speculate that this relatively weak ‘dose’ of customization may not have been sufficient to elicit the intended effects, such as enhanced perceived active control over mobile health apps. Future research could focus on measuring engagement with the various features within customizable versus non-customizable mobile health apps to further our understanding of how people use customization features and mobile health apps in general. Such insights may shed light on when and how customization can be effective in mobile health apps.
Further research could also focus on how to effectively engage those with a lesser need for autonomy. Earlier research has, for example, shown that more directive communication styles could be especially effective for people with a lesser need for autonomy.11,12 In addition, mobile health apps developed especially for these people could also use more explicit personalization strategies and, for instance, provide users with app content that is data-driven instead of providing them with customization features that require more active user involvement.51
Second, our finding that those with a greater need for autonomy display different levels of intention to engage in physical activity than those with a lesser need for autonomy should be interpreted with caution. Despite it being common in related research,52 the use of a median split to analyze the effect of need for autonomy might have led to a loss of information when interpreting the results. Although participants on either side of the median split were quite homogenous due to the relatively small range in need for autonomy overall, we treated people with different scores as if they were the same. Moreover, earlier research has shown the complex patterns of interaction between the health-related need for autonomy and the need for external control.11,12,39 The distinction between those with a greater and lesser need for autonomy could be an oversimplified view of people’s need for autonomy, as it ignores people’s potentially co-existing need for external control, that is, the need for guidance from others such as peers and experts. In fact, the need for autonomy and need for external control could be context-dependent, such that a person wishes to actively choose how to change health behaviours in one situation (e.g. when adopting a new diet), whereas that same person wishes to receive clear-cut expert advice in other situations (e.g. when being diagnosed with a chronic disease). This context-dependency might be worth considering in future research efforts.
Another future research direction could be to longitudinally validate our findings, and thus the motivational technology model. As the data presented are of cross-sectional nature, we cannot claim that there are causal relationships between perceived active control, autonomous motivation to use mobile health apps, and the intention to engage in health-related behaviours. To validate the claim that perceived active control and autonomous motivation to use health-related technology drive the intention to engage in health-related behaviours, longitudinal research is needed to predict the intention to engage in physical activity. Furthermore, future research could focus on extending our findings beyond behavioural intentions to health behaviour outcomes, and to more ecologically valid settings. Most people have positive intentions to engage in physical activity, but many of those people fail to act upon their intentions.4 It is therefore crucial to assess the impact of mobile health interventions on behavioural outcomes in addition to behavioural intentions, to overcome the intention–behaviour gap and extend our knowledge on the effectiveness of mobile health apps in changing actual health behaviours. Another area of research that may need attention is the generalizability of mobile health app research to real-world contexts. Although using a prototype provided the precise experimental control needed to examine the effects of customization, a next step would be to test whether such effects hold for real mobile health apps.
Conclusions
This study investigated the effects of customization in mobile health apps and the role of need for autonomy in explaining its effectiveness. The results showed that when people with a greater need for autonomy had the opportunity to customize a health app, they reported higher intentions to engage in physical activity than when they did not have this opportunity. This effect was not found for those with a lesser need for autonomy. Our study provides relevant implications for health app design and health communication at large by suggesting that differences in need for autonomy may need to be considered to optimize the impact of mobile health communication efforts. As mobile apps are increasing in popularity and functionality, effective mobile health solutions may advance healthier lifestyles.
Supplemental Material
Supplemental material, DHJ888074 Supplementary material for Customization in mobile health apps: explaining effects on physical activity intentions by the need for autonomy by Nadine Bol, Nina Margareta Høie, Minh Hao Nguyen and Eline Suzanne Smit in Digital Health
Acknowledgements
We would like to thank Professor Kenneth Resnicow for sharing with us the items from the Health Causality Orientations Scale. Furthermore, we would like to thank the two anonymous reviewers for their kind reviews and valuable suggestions for improvement of the manuscript.
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Contributorship
NB and NH researched literature and conceived the study. NH was involved in the study design and data collection. NB conducted the analyses. NH and NB wrote the first draft of the manuscript. HN and ES shaped the writing of the theoretical framework. All authors critically reviewed the manuscript and approved the final version of the manuscript.
Ethical approval
The ethics committee of the University of Amsterdam approved this study (reference number: 2017-PC-7994).
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Guarantor
NB
Peer review
This manuscript was reviewed by reviewers, who has chosen to remain anonymous.
Supplemental material
Supplemental material for this article is available online.
References
- 1.World Health Organization. Global status report on noncommunicable diseases 2014, http://apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdf?ua=1 (2014, accessed 5 March 2019).
- 2.World Health Organization. Noncommunicable diseases: key facts, http://www.who.int/mediacentre/factsheets/fs355/en/ (2018, accessed 5 March 2019).
- 3.World Health Organization. Physical activity, http://www.who.int/mediacentre/factsheets/fs385/en/ (2018, accessed 5 March 2019).
- 4.Rhodes RE, De Bruijn GJ. How big is the physical activity intention–behaviour gap? A meta‐analysis using the action control framework. Br J Health Psychol 2013; 18: 296–309. [DOI] [PubMed] [Google Scholar]
- 5.Middelweerd A, Mollee JS, Van der Wal CN, et al. Apps to promote physical activity among adults: a review and content analysis. Int J Behav Nutr Phys Act 2014; 11: 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fanning J, Mullen SP, McAuley E. Increasing physical activity with mobile devices: a meta-analysis. J Med Internet Res 2012; 14: e161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klasnja P, Pratt W. Healthcare in the pocket: mapping the space of mobile-phone health interventions. J Biomed Inform 2012; 45: 184–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000; 55: 68–78. [DOI] [PubMed] [Google Scholar]
- 9.Sundar SS, Bellur S, Jia H. Motivational technologies: a theoretical framework for designing preventive health applications. In: International conference on persuasive technology. Proceedings of the 7th international conference on persuasive technology (eds M Bang and EL Ragnemalm), Linköping, Sweden, 6 June–8 June, 2012, paper no. LNCS 7284, pp.112–122. Berlin, Heidelberg: Springer-Verlag.
- 10.Kalyanaraman S, Sundar SS. The psychological appeal of personalized content in web portals: does customization affect attitudes and behavior? J Commun 2006; 56: 110–132. [Google Scholar]
- 11.Resnicow K, Zhou Y, Hawley S, et al. Communication preference moderates the effect of a tailored intervention to increase colorectal cancer screening among African Americans. Patient Educ Couns 2014; 97: 370–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Resnicow K, Davis RE, Zhang G, et al. Tailoring a fruit and vegetable intervention on novel motivational constructs: results of a randomized study. Ann Behav Med 2008; 35: 159–169. [DOI] [PubMed] [Google Scholar]
- 13.Knight E, Stuckey MI, Prapavessis H, et al. Public health guidelines for physical activity: is there an app for that? A review of android and apple app stores. JMIR Mhealth Uhealth 2015; 3: e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Conroy DE, Yang CH, Maher JP. Behavior change techniques in top-ranked mobile apps for physical activity. Am J Prev Med 2014; 46: 649–652. [DOI] [PubMed] [Google Scholar]
- 15.Riley WT, Rivera DE, Atienza AA, et al. Health behavior models in the age of mobile interventions: are our theories up to the task? Transl Behav Med 2011; 1: 53–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhao J, Freeman B, Li ML. Can mobile phone apps influence people’s health behavior change? An evidence review. J Med Internet Res 2016; 18: e287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gal R, May AM, van Overmeeren EJ, et al. The effect of physical activity interventions comprising wearables and smartphone applications on physical activity: a systematic review and meta-analysis. Sports Med Open 2018; 4: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kreuter MW, Strecher VJ, Glassman B. One size does not fit all: the case for tailoring print materials. Ann Behav Med 1999; 21: 276–283. [DOI] [PubMed] [Google Scholar]
- 19.Sundar SS. Self as source: agency and customization in interactive media In: Konijn E, Utz S, Tanis M, et al. (eds) Mediated interpersonal communication. New York: Routledge, 2008, p. 58–74. [Google Scholar]
- 20.Lustria MLA, Cortese J, Gerend MA, et al. A model of tailoring effects: a randomized controlled trial examining the mechanisms of tailoring in a web-based STD screening intervention. Health Psychol 2016; 35: 1214–1224. [DOI] [PubMed] [Google Scholar]
- 21.Krebs P, Prochaska JO, Rossi JS. A meta-analysis of computer-tailored interventions for health behavior change. Prev Med 2010; 51: 214–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull 2007; 133: 673–693. [DOI] [PubMed] [Google Scholar]
- 23.Gwizdka J, Spence I. Implicit measures of lostness and success in web navigation. Interact Comput 2007; 19: 357–369. [Google Scholar]
- 24.Katsanos C, Tselios N, Avouris N. Evaluating website navigability: validation of a tool-based approach through two eye-tracking user studies. New Rev Hypermedia Multimed 2010; 16: 195–214. [Google Scholar]
- 25.Domahidi E. The associations between online media use and users’ perceived social resources: a meta-analysis. J Comput Mediat Commun 2018; 23: 181–200. [Google Scholar]
- 26.Liu D, Ainsworth SE, Baumeister RF. A meta-analysis of social networking online and social capital. Rev Gen Psychol 2016; 20: 369–391. [Google Scholar]
- 27.Kang H, Sundar SS. When self is the source: effects of media customization on message processing. Media Psychol 2016; 19: 561–588. [Google Scholar]
- 28.Kim K, Schmierbach MG, Chung M, et al. Is it a sense of autonomy, control, or attachment? Exploring the effects of in-game customization on game enjoyment. Comput Hum Behav 2015; 48: 695–705. [Google Scholar]
- 29.Hanus MD, Fox J. Source customization reduces psychological reactance to a persuasive message via user control and identity perceptions. J Interact Advert 2017; 17: 1–12. [Google Scholar]
- 30.Katz I, Assor A. When choice motivates and when it does not. Educ Psychol Rev 2007; 19: 429–442. [Google Scholar]
- 31.Sailer M, Hense JU, Mayr SK, et al. How gamification motivates: an experimental study of the effects of specific game design elements on psychological need satisfaction. Comput Hum Behav 2017; 69: 371–380. [Google Scholar]
- 32.Peng W, Lin J.-, Pfeiffer KA, et al. Need satisfaction supportive game features as motivational determinants: an experimental study of a self-determination theory guided exergame. Media Psychol 2012; 15: 175–196. [Google Scholar]
- 33.Birk MV, Atkins C, Bowey JT, et al. Fostering intrinsic motivation through avatar identification in digital games. In: Proceedings of the 2016 CHI conference on human factors in computing systems, San Jose, USA, 7 May–May 12, 2016, paper no. xxx, pp.2982–2995: New York: ACM.
- 34.Free C, Phillips G, Galli L, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med 2013; 10: e1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.InVisionApp Inc. InVision, https://www.invisionapp.com/ (2019, accessed 3 January 2019).
- 36.Ajzen I. Constructing a TPB questionnaire: conceptual and methodological considerations, http://www.people.umass.edu/aizen/pdf/tpb.measurement.pdf (2002, accessed on 5 March 2019).
- 37.Voorveld HAM, Neijens PC, Smit EG. The relation between actual and perceived interactivity. J Advert 2011; 40: 77–92. [Google Scholar]
- 38.Ntoumanis N. A self‐determination approach to the understanding of motivation in physical education. Br J Educ Psychol 2001; 71: 225–242. [DOI] [PubMed] [Google Scholar]
- 39.Smit ES, Bol N. From self-reliers to expert-dependents: identifying classes based on health-related need for autonomy and need for external control among mobile users. Media Psychol 2019: 1–24. [Google Scholar]
- 40.Deci EL, Ryan RM. The general causality orientations scale: self-determination in personality. J Res Pers 1985; 19: 109–134. [Google Scholar]
- 41.Bollen KA, Stine RA. Bootstrapping goodness-of-fit measures in structural equation models. Sociol Methods Res 1992; 21: 205–229. [Google Scholar]
- 42.MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: distribution of the product and resampling methods. Multivariate Behav Res 2004; 39: 99–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hooper D, Coughlan J, Mullen MR. Structural equation modelling: guidelines for determining model fit. Electronic J Bus Res Methods 2008; 6: 53–60. [Google Scholar]
- 44.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling 1999; 6: 1–55. [Google Scholar]
- 45.Bradway M, Årsand E, Grøttland A. Mobile health: empowering patients and driving change. Trends Endocrinol Metab 2015; 26: 114–117. [DOI] [PubMed] [Google Scholar]
- 46.Schnall R, Bakken S, Rojas M, et al. mHealth technology as a persuasive tool for treatment, care and management of persons living with HIV. AIDS Behav 2015; 19: 81–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fogg BJ. Persuasive technologies. Commun ACM 1999; 45: 27–29. [Google Scholar]
- 48.Ariely D. Controlling the information flow: effects on consumers’ decision making and preferences. J Consum Res 2000; 27: 233–248. [Google Scholar]
- 49.Cacioppo JT, Petty RE, Kao CF, et al. Central and peripheral routes to persuasion: an individual difference perspective. J Pers Soc Psychol 1986; 51: 1032–1043. [Google Scholar]
- 50.Lustria MLA, Noar SM, Cortese J, et al. A meta-analysis of web-delivered tailored health behavior change interventions. J Health Commun 2013; 18: 1039–1069. [DOI] [PubMed] [Google Scholar]
- 51.Kaptein M, Markopoulos P, De Ruyter B, et al. Personalizing persuasive technologies: explicit and implicit personalization using persuasion profiles. Int J Hum Comput Stud 2015; 77: 38–51. [Google Scholar]
- 52.Bright LF, Daugherty T. Does customization impact advertising effectiveness? An exploratory study of consumer perceptions of advertising in customized online environments. J Mark Commun 2012; 18: 19–37. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, DHJ888074 Supplementary material for Customization in mobile health apps: explaining effects on physical activity intentions by the need for autonomy by Nadine Bol, Nina Margareta Høie, Minh Hao Nguyen and Eline Suzanne Smit in Digital Health