Abstract
It is of significant importance to scientifically assess and efficiently address chronic constipation in the elderly population. Therefore, organizing some domestic experts of geriatrics and gastroenterology, we have formulated this consensus to reference for clinical staff.
Keywords: constipation, risk assessment
1. INTRODUCTION
Chronic constipation (CC) is a common geriatric syndrome1, 2, 3, 4 characterized by reduced stool frequency, hard stools, and/or difficult defecation. Currently, it is mainly diagnosed with Rome IV criteria and patient's self‐reported; that is, symptom onset should occur at least 6 months before diagnosis, and symptoms should be present during the last 3 months and more than one‐fourth of defecation must include 2 or more of the following: straining,lumpy or hard stools, sensation of incomplete evacuation, sensation of anorectal obstruction/blockage, manual maneuvers to facilitate defecations, and fewer than 3 spontaneous bowel movements per week.5, 6 CC is common in the elders, and its prevalence rate increases with patient's age. Multiple community‐based large‐scale epidemiologic studies show that the prevalence rate of CC in patients older than 60 years is 15%‐20%,7 in patients more than 84 years old could be 20.0%‐37.3%,1, 2, 4, 7 and in patients who accept long‐term care could be as high as 80%.2, 4, 8, 9 It has a significant impact on quality of life in the elderly as well as their physical and mental health.8, 10 Also, it takes a large amount of healthcare resources5, 11 and remains to be a tough clinical challenge.
2. TYPES OF CHRONIC CONSTIPATION IN THE ELDERS
Chronic constipation in the elders could be the result of multiple factors, including functional or organic diseases of colorectum and anus, and drugs. Thus, it also can fall into primary and secondary constipation, with the former one referring to constipation caused by colorectum and anal functional diseases and the latter one caused by organic diseases or drugs.
Chronic functional constipation: Chronic functional constipation is the most common type in the elderly population. It can be divided into 4 subtypes according to the characteristics of patient's intestinal motility and rectal anal function change1, 12: (1) slow‐transit constipation (STC)—With decreased colonic motility, the elders are vulnerable to slow‐transit constipation.7, 13 Its feature is prolonged colonic transit time, with symptoms of reduced stool frequency, hard stools, and/or difficult defecation predominate14; (2) evacuation disorder—that is, functional constipation, also previously known as outlet‐obstructed constipation. This is mainly manifested in straining, sensation of incomplete evacuation, sensation of anorectal obstruction/blockage, and even needing manual maneuvers to facilitate evacuation. This type of constipation is also common in the elderly population7; (3) mixed constipation—proofs of delayed colon transit and anorectal defecation disorder coexist in patients; (4) normal transit constipation (NTC)—often seen in constipation‐predominant irritable bowel syndrome (IBS), in which abdominal pain and discomfort are associated with constipation and symptoms relief after defecation.15 This type of constipation is rarely seen in the elderly population.
Organic constipation: common diseases that can cause chronic constipation in the elders, see Table 1.
Drug‐induced constipation: Commonly used drugs by the elders that can cause or aggravate constipation are opioid analgesics, tricyclic antidepressant, anticholinergic drugs, antihistamine agents, antiparkinsonian drugs, ganglionic blocking agents, NSAIDs, antacids containing calcium carbonate or aluminum hydroxide, bismuth, iron, calcium antagonist, diuretic, and some antibiotics.12
Table 1.
Common diseases that can cause chronic constipation in the elders
| Category | Diseases |
|---|---|
| Intestinal diseases | Tumor, diverticulosis, hemorrhoids, anal fissure, inflammatory bowel disease, ventral hernia, intestinal volvulus, rectal prolapse, rectocele, ileus caused by external compression from tumor/other, strictures caused by inflammation/trauma/radioactivity or surgery, history of pelvic or anal surgery, etc. |
| Neurological disorders/neuropathy | Cerebrovascular disease |
| Multiple sclerosis | |
| Parkinson's disease | |
| Spinal cord pathology caused by trauma/tumor | |
| Autonomic neuropathy | |
| Cognitive impairment/dementia, etc. | |
| Myopathy | Amyloidosis |
| Scleroderma | |
| Systemic sclerosis, etc. | |
| Electrolyte disturbance | Hypercalcemia |
| Hypokalemia | |
| Hypermagnesemia, etc. | |
| Endocrine/metabolic conditions | Diabetes mellitus |
| Hypothyroidism | |
| Hyperparathyroidism, etc. | |
| Cardiac disease | Congestive heart failure, etc. |
3. COMPLICATIONS AND IMPACT OF CC IN THE ELDERS5, 10, 11, 16, 17, 18, 19, 20, 21
Aggravate cerebrovascular disease: Cerebrovascular diseases are common among the elderly population. When having constipation, patients have difficulty in defecation and as a consequence increase abdominal pressure, blood pressure, and myocardial oxygen consumption, which may be life‐threatening as they predispose to cerebral hemorrhage, angina, and myocardial infarction.
Stercoral obstruction of colon, intestinal wall ulcer, and colonic perforation: When long stagnating in the sigmoid colon or the rectum and water be absorbed, feces grow hard and even become fecal stone, which can obstruct enteric cavity and induce ileus. Besides, long‐term compression of the feces can cause intestinal wall ulcer, occasionally leading to the life‐threatening fecal peritonitis as a result of intestinal perforation.
Induce diverticulosis and diverticulitis: Tension of colonic smooth muscle and the thickness of the muscle in the elderly population tend to decrease. And increased pressure in the colon of CC patients causes thin‐walled out‐pouches to develop diverticulum, in which feces cannot be timely evacuated because of constipation. These factors predispose to diverticulitis.
Induce or aggravate hemorrhoids and rectal prolapse: During defecation, patients need to hold breath of intense effort, which leads to increased pressure at the rectum neck and cutting‐off of the venous drainage, causing congestive hypertrophy and repeated distal shifts of the anal pad. The fibrous septum in the pad gradually relaxes until it ruptures, accompanied by venous plexus stasis, expansion, fusion, and even mixed by small arteriovenous fistula, and eventually developing into hemorrhoids. For hemorrhoids patients, constipation will cause it aggravate. The weak and relaxed pelvic floor tissue in the elders, in combination with CC, can cause long‐term elevation of intra‐abdominal pressure, thus inducing or aggravating rectal prolapse.
Increase risk for colon cancer: Constipation holds up feces in the colonic lumen, which increases the concentrations of carcinogens and prolongs mucosal contact with them, and thus increases the risk for colon cancer.
Inducing or aggravating abdominal hernia: The abdominal muscles atrophy and long‐term elevation of intra‐abdominal pressure in the old constipation patients can easily induce or worsen abdominal hernia and even predispose to incarcerated hernia.
Melanosis coli: CC patients and those who frequently use anthraquinones are vulnerable to melanosis coli.
Inducing ischemic colitis: CC can increase intestinal cavity pressure and decrease intestinal mucosal blood supply, thus increasing the risk for ischemic colitis. CC is a major risk factor for ischemic colitis in the elders.
Psychological disorder: CC disturbs patients, making them in low spirit and hard to concentrate, and even bringing about insomnia, anxiety, and depression, thus affecting daily work and life, and reducing work efficiency and quality of life.
Urinary retention and urinary tract infection: The rectal feces in the CC patients compresses urinary tract, leading to urinary retention and urinary tract infection. Besides, CC in the elders can cause fecal incontinence (pseudodiarrhea) and volvulus of sigmoid colon.
4. COMPREHENSIVE ASSESSMENT OF CC IN THE ELDERLY
4.1. Risk factors assessment
Fluid intake: Although the liquid requirements vary with individual, when the daily total fluid intake is <1.5 L, water in the gut decreases and can cause dry feces and reduction in fecal volume, hence leading to constipation. As the sensation of thirsty decreases in the elders, they do not always feel thirsty even in dehydration. It is helpful to decide whether the fluid intake is sufficient by examining patient's urine volume, skin elasticity, and moisture of the oral mucous membrane.12, 22
Diets: Dietary fibers can not only increase the stool volume, retain moisture, and thus softening stool, but also increase bowel movement. However, as the masticatory function declines in the elders because of tooth loose and loss, they usually fine‐tune their diet, which results in insufficient fiber intake (<25 g/d). There is less stimulation of the intestinal wall, which in turn affects the colonic transit time, bowel movement frequency, and stool volume.12
Activity level: Reduction in activity will increase the risk for constipation.23 Old patients, who are wheelchaired, immobile, or with impaired physical mobility, are lack of exercise for a long time and suffer from declined intestinal peristalsis. When feces remain in the bowel for too long, more water within the feces will be absorbed, thus resulting in hard stools, inducing and aggravating constipation. In addition, reduction in activity can cause abdominal muscle atrophy, decreased muscle strength, and making it hard to hold breath and defecate. Activity‐reducing‐associated constipation is the most common in weak and chronic bedridden elderly in patients.4, 22, 24
Environment: Inappropriate defecation environment, such as lack of privacy, unable to use toilet alone, needing help with defecation, and inconvenient facilities, can induce suppression of the awareness of defecation in the elders and worsen constipation.
Psychological factor: The elders often have to face many challenges, such as being sickly, bereaved, and living alone. Psychological factors, such as anxiety and depression, and adverse life events will bring about a great negative impact on the elderly's life quality.1 Psychological factors can affect the gastrointestinal tract's sensory, movement, and secretion.10, 12, 25 In addition, by inhibiting parasympathetic nerve, they can also impair defecation reflex, which results in constipation.26, 27, 28 Clinically, tools such as Self‐rating Anxiety Scale (SAS) and Self‐rating Depression Scale (SDS) can be applied to assess patient's psychological condition.
Social support: Social support includes objective and subjective support. Objective support refers to direct assistance in material and finance, committed marriage, and children's loving care, while subjective support means patient's satisfaction on emotions, such as being respected, supported, and understood. Meanwhile, social support should include another dimension, that is, how much patients have utilized the social support and other's help. Like other chronic diseases in the elderly population, CC is closely related with social support, which can decrease morbidity of old age constipation.29 CC patient's life quality is positively correlated with social support and utilization of it,30 and whether patients lack social support could be preliminarily judged by Social Support Rating Scale.
4.2. Clinical assessment
Symptoms and fecal character: Symptoms include stool frequency, defecation habits, degree of straining, whether complicated by bloating, pain, and other abdominal discomfort as well as chest tightness, pain, and dizziness. Fecal character can be assessed by Bristol Stool Scale.31
Alarming signs: Alarming signs include hematochezia or positive fecal occult blood test (FOBT), anemia, abdominal pain and mass, changes in appetite, weight, and defecation habit.5, 6, 12 Besides, patient's family history of intestinal diseases should be taken into consideration, such as colorectal polyps, colorectal cancer, and inflammatory bowel disease.14, 15
Constipation‐associated organic diseases: To identify the organic diseases mentioned above which can cause constipation mainly by case history, physical examination, and necessary laboratory test.22, 24
Comorbidity and general condition: Organ function declines in elderly people who usually have multiple chronic diseases. Frailty, a kind of geriatric syndromes, is quite common in the elderly,32, 33 which refers that a group of symptoms can be induced by tiny external stimuli, as the reserve function of multiple systems, organs, or tissues has declined to the threshold. The colonic transit time in healthy old people is <5 days, whereas in the frailties, it can be as long as 8 days.25 The activity of the elderly's diaphragm, abdominal muscle, and colonic smooth muscle declines with age, leading to insufficient evacuation motility. Moreover, aging may change elder people's body structures such as the pelvic floor structure, rectocele, rectal mucosal prolapse, and perineum descending. This is also one of the factors causing high prevalence of CC in the elderly population, especially in the females.1, 14, 25, 34
Medication: (1) Carefully asking the medication of the drugs mentioned above that could cause constipation: Because of comorbidity, the elderly often need polypharmacy; hence, the chance of taking the constipation‐associated drugs increases, which is another important factor for the elderly population's constipation.4, 10, 26 (2) Carefully asking the medication of laxatives, including the category, dosage, frequency, and duration of laxative, as well as suppository, enema, and other cathartic prescription or nonprescription drugs. Long‐term laxative, especially stimulant laxative usage, could impair intestinal myenteric plexus, decrease colonic reactivity to the stimulus of intestinal contents, make colonic movement frail, and even lose the ability of independent defecation. Such colon is called as “cathartic colon.”
Cognitive function: There is high prevalence of cognitive disorder among the senile constipation patients, and the severity of constipation is positively correlated with cognitive disorder.35, 36 Therefore, assessing patient's cognitive function, which can be performed by Mini‐Mental State Examination (MMSE), is helpful to formulate individualized constipation intervention.
Physical examination: Attention should be paid to abdominal tenderness and abdominal mass. Physical examination includes general, abdominal, and anorectal checkup. The digital rectal examination is especially important because it helps to learn not only the fecal impaction, stricture of anus, rectal prolapse, or rectum mass, but also the paradoxical or nonrelaxing puborectalis activity.5, 7, 12
Screening examination: Blood routine, urine routine, and fecal occult blood test (FOBT) should be the indicators of routine checkup and regular follow‐up for the elderly patients.5, 7, 12 For those with severe CC or alarming signs, further examinations, such as colonoscopy, blood biochemical, thyroid function, and other relative imageological examinations,12 are required to determine whether constipation is caused by organic diseases. For those suspected functional constipation, intestinal motility and anorectal function tests are recommended, including colonic transit study, anorectal manometry, and balloon expulsion test,5, 7, 12 as well as anorectal (or pelvic floor muscle) surface electromyography. For the aged patients or the elders with vital organ diseases or mobility problems, their acceptability to the screening examination and its feasibility should be carefully assessed and taken into full account to avoid over checking.1
Severity assessment: According to the severity of symptoms and impact on daily life, constipation can be divided into 3 degrees: mild, moderate, and severe.5, 37 Mild: Symptoms are mild and do not affect patient's life, and patients can rebuild normal defecation through overall treatment and short‐term medication. Severe: Symptoms are severe and lasting and greatly impact patient's work and life. Medications are required, cannot be interrupted, or may be even ineffective.27 Moderate: Fall in between mild and severe. Refractory constipation, which is also known as chronic refractory constipation, falls in severe degree. Medication and various nonsurgical treatments are ineffective for this type, and patients may need surgical treatment. This type is often seen in outlet construction constipation, colonic inertia, and severe IBS.26
5. MANAGEMENT OF CC IN THE ELDERLY
5.1. Adjustment of lifestyle
Sufficient dietary fiber intake38, 39: This is the foundation of the disease control, and sufficient dietary fiber (≥25 g/d) intake should be necessary. However, foods rich in fiber are usually poor in taste, while the masticatory function declines in the advanced age. So, food should be cooked soft and delicious to be swallowed more easily. Dietary fiber includes soluble and insoluble dietary fiber. Food with soluble fiber usually tastes smooth and is rich in flavor. Besides, this kind of food can also be the substrate of intestinal flora as prebiotics and is especially suitable for the elderly. Thus, fresh fruits and vegetables which are rich in soluble dietary fiber, vitamins, and water should be an important part of senile CC patient's diet. As a natural soluble fiber extracted from chicory, inulin powder available in the market is a dietary fiber supplement of high quality,40, 41 which is typically suitable for senile constipation patients with dysphagia and tube feeding.
Sufficient fluid intake: The elderly should form habits of regular and initiative drinking and drink before feeling thirsty. Daily water intake is advised to be 1500‐1700 mL and 50‐100 mL each time. Warm water and light tea are recommended.
Proper exercise: Exercising with open forms should avoid falling down and overexercise. Long‐time sitting should also be avoided. To patients in bed, light activity such as sitting up, standing, and walking a little is helpful for defecation.
Form correct defecation habits: Jointly develop a defecation schedule with patients, help patients form defecation reflexes based on circadian rhythms, and cultivate a habit of regular defecation. As bowel movements reach highest in the morning or after meals, it is suggested to defecate within 2 hours after waking up or after meals. When defecating, patients should concentrate and minimize outside disruption.42
5.2. Pharmaceutical therapy
Bulk‐forming laxatives: Represented by psyllium seed husk, wheat bran, plantain herb, methylcellulose, and calcium polycarbophil,5, 43, 44, 45, 46, 47 bulk‐forming laxatives are commonly used drugs for CC in the elderly.28 Being poorly absorbed in the intestines, bulk laxatives can increase the bulk and moisture content of feces by luminal water binding, thus softening the stool and promoting bowel movements. Currently, they are mainly used for mild constipation treatment.12, 48 Adequate liquid should be supplied to avoid intestinal mechanical obstruction.49 Patients with stool impaction or suspected intestinal obstruction are not recommended. Taking together with warfarin, digoxin and antibiotics might affect their absorption.49, 50
Osmotic laxatives: Commonly used are lactulose, polyethylene glycol (PEG), and salinic laxatives (eg, magnesium sulfate). After oral administration, they can create an osmotic gradient by luminal water binding, increase stool bulk, and stimulate bowel movements. They are used for mild or moderate constipation.45, 47, 49, 50 Lactulose is also prebiotic, which can promote the growth of profitable strain. Generally, it can be administered safely for a long duration51 except a few cases that need dosage adjustment because of side effects, such as diarrhea and bloating. It is particularly suitable for senile CC patients complicated with chronic cardiac and renal dysfunctions.49 Overdosing of salinic laxatives can cause electrolyte imbalance (eg, magnesium sulfate can cause hypermagnesemia) and hence must be used with caution in the elderly and patients with compromised renal function.5, 49, 50
Stimulant laxatives: Including bisacodyl, castor oil, anthraquinones (eg, Chinese rhubarb, folium sennae, Maren pill, Muxiangliqi tablet, Congrong oral liquid, Dangguilonghui tablet, Tongbianning tablet, and other Chinese patent medicines), and phenolphthalein, these drugs are widely used in the clinic with quick laxative effects. By acting on the myenteric plexus, they can stimulate colonic motility and the secretion of intestinal fluid, thus shortening colonic transit time, increasing the exchanges of fluid and electrolyte, and finally promoting defecation.11, 45, 47, 49, 50, 52, 53 Despite quick and obvious effects, a long‐term use of these drugs will affect the absorption of water, electrolyte, and vitamins, lead to irreversible damage to the myenteric plexus, and even cause myasthenia of bowel, drug dependence, and fecal incontinence.54 Besides, a long‐term anthraquinone use may cause colon melanosis.46 Phenolphthalein agents were withdrawn from the market for the potential carcinogenesis discovered in some animal experiments.43 In summary, in spite of the strong effects of the stimulant laxatives, because of the above side effects, it is not recommended for the elderly to accept long‐term therapy of these drugs.5, 12, 49, 50
Lubricating agents: Including glycerin, liquid paraffin, and docusate sodium, this class of drugs are supplied in forms of oral liquid and enemas. They can soften stools and lubricate bowel wall, and can be applied to the frailty, the elderly, as well as those with hypertension and cardiac insufficiency. Apply 10‐15 mL of the enema to soften the stools, which is effective and safe,50, 55 and is especially suitable for outlet‐obstructed constipation and senile patients with hard stools or impaction.5 However, the liquid paraffin can decrease the absorption of fat‐soluble vitamins,42 and patients with dysphagia might have risk for aspiration pneumonia while taking liquid paraffin. Therefore, liquid paraffin should be avoided administered orally.
Prokinetic drugs: Currently, the commonly used prokinetic drugs are dopamine receptor antagonist, cholinesterase inhibitors (itopride), and 5‐HT receptor agonist (mosapride45, 56 and prucalopride46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57). In vivo and in vitro studies show that itopride can promote colonic motility.58, 59, 60, 61 Clinical research also shows that, when used singly or with lactulose, itopride works in CC patients and even in poststroke immobile patients.62, 63, 64 As a 5‐HT receptor agonist, mosapride acts on nerve endings, release excitatory neurotransmitters, and reverse the effect of inhibitory neurotransmitter. Or it can directly act on the smooth muscle, enhance the intestinal motility, and promote defecation. Now, it is mainly used in slow‐transit constipation patients with decreased defecation frequency and hard stools. Prucalopride is a highly selective 5‐HT4 receptor antagonist, which can promote colonic movements and decrease colonic transit time while having little effect on gastric emptying and small intestine transition. It can be used in the treatment of senile slow‐transit constipation.46, 57, 65 Oversea studies find that prucalopride is safe and well tolerated, with no significant association with cardiovascular events in the elderly.57, 66, 67, 68 But we lack data on safety in the Chinese elderly population.50 Common side effects of prokinetic drugs are diarrhea, abdominal pain, nausea, and headache.42, 51, 56
Secretagogues: Represented by lubiprostone69, 70 and linaclotide,71 secretagogues promote defecation by stimulating intestinal liquid secretion. In China, this class of drugs are not available in market yet.
Probiotics48, 72, 73, 74: Probiotics are beneficial for alleviating constipation by improving the intestinal micro‐ecology and bowel movements and can be applied as an adjuvant therapy for CC in the elderly. Recently, a meta‐analysis shows that, when combined with conventional laxatives, bifidobacterium triplex live bacteria preparation can enhance the efficacy on functional constipation and reduce recurrence rate.75 For the evidence‐based medical evaluation of some commonly used constipation drugs (Table 2).
When taking medicine, we should pay attention to the following aspects: (1) It must be based on the adjustment of lifestyle such as sufficient fluid and dietary fiber intake, proper exercise, and good bowel habit; (2) gradient medication : in sequence, bulking agents or osmotic laxatives, secretory stimulant, stimulant laxatives. Combination medication can be considered according to the patients' conditions: Patients with slow‐transit constipation can add prokinetic agents; patients with evacuation disorder, hard stool, or fecal impaction can be treated by enema together with drugs orally; (3) to patients with mild‐moderate chronic constipation, especially the elderly complicated with heart, renal insufficiency, or frailty, it is better to choose the mild and safe laxatives such as lactulose than those osmotic laxatives containing magnesium, phosphate, and sodium; and (4) to identify the pseudodiarrhea caused by fecal impaction. Pseudodiarrhea is usually happened in the weak elderly who suffer from fecal impaction in rectum ampullar region. Such fecal impaction may cause rectum ampullar expansion together with relaxation of rectal sphincter. Thus, the loose stool above the fecal blockage flows down just like diarrhea.
Table 2.
| Classification | Drugs | Recommendation level | Grade of evidence |
|---|---|---|---|
| Osmotic laxatives | Lactulose | Level II | Grade B |
| Polyethylene glycol | Level I | Grade A | |
| Bulking agents | Psyllium | Level II | Grade B |
| Bran | Level II | Grade C | |
| Methylcellulose | Level III | Grade C | |
| Calcium polycarbophil | Level III | Grade C | |
| Stimulant laxatives | Bisacodyl | Level II | Grade B |
| Senna | Level III | Grade C | |
| Wetting agents | Dioctyl sulfosuccinate | Level III | Grade C |
| Prokinetic agents | Prucalopride | Level I | Grade A |
| Secretory stimulant | Lubiprostone | Level I | Grade A |
| Linaclotide | Level II | Grade B |
5.3. Traditional Chinese medical therapy
Traditional Chinese medicine divides constipation into several types.11 Chinese medicine, acupuncture, and massage are effective to constipation. These methods have been used for thousands of years in China. For details, doctors can refer to the guideline or consensus laid down by the Association of Chinese Medicine and its branches.11 Meanwhile, it should be cautious to avoid the liver injury and other side effects resulted by taking Chinese medicine for long time.
5.4. Psychological treatment
By psychological counseling, make the patients with constipation know that constipation is preventable and treatable. Good psychological states, sleeping, and dietary habit are helpful to ease constipation. Those who have obvious psychological disorder should be recommended for drug treatment with antidepressants, while those who have severe mental disorder should be transferred to the psychiatric department for treatment.76
5.5. Improve social support
According to the social support assessment results, mobilize powers of different sectors to improve social support system and encourage patients to make use of this system.
5.6. Cognitive training
To the chronic constipation patients with cognitive dysfunction, cognitive training should be recommended including training on time, spatial orientation, and memory and communication skills. The successful cognition training should be advantageous to both the constipation therapy and the patient's life quality.1, 36
5.7. Biofeedback therapy
Biofeedback therapy may eliminate patients' paradoxical movement among abdominal muscles, pelvic muscles, and anal sphincters by repeated coordination exercises of the muscles to facilitate defecation. Thus, biofeedback therapy is especially appropriate to the patients with evacuation disorder73, 77, 78 and it is also the first‐line therapy for them.79 A successful biofeedback therapy may improve not only constipation, but also patients' psychological status and life quality1, 80 However, biofeedback is not suitable for the elderly with cognitive dysfunction, because they cannot grasp the skill of the exercises.
5.8. Surgery
It is applied for the refractory severe constipation for those who are not responding to normative nonsurgical treatment. Subtotal or total colectomy is performed in patients with refractory slow‐transit constipation. The indications are as follows49: (1) chronic refractory constipation patients with severe symptoms, long history of constipation, and no response to conventional therapy; (2) slow‐transit constipation; (3) constipation patients without pseudoileus confirmed by radiography or manometry; (4) excluding abdominal organic diseases which would result in constipation.
Surgeries for evacuation disorder are mainly aimed at rectal prolapse and rectocele77: (1)Surgeries via anus are more commonly performed for rectal prolapse, such as rectal mucosa folding and injection with sclerosing agents, PPH (procedure for prolapsed and hemorrhoids), and Delorme surgery.77 The technique named stapled transanal rectal resection (STARR) is simple and effective to remove rectal prolapse and rectocele.81 (2) Surgeries for rectocele including transanal or transvaginal rectocele repair, PPH, STARR, and so on.77
Transanal or transsacral puborectalis partial resection or fusion of musculus obturator internus and puborectalis77 may be suitable to relieve constipation symptoms of the patients with puborectal muscle syndrome caused by the spasm of puborectalis.82 Actually, very few patients benefit from surgery to treat constipation. In America, only 104 patients with slow‐transit constipation are treated by surgery 1 year.83 Considering the high risks and various complications of surgery to elderly, it should be cautious to make the decision of surgical treatment for constipation.5, 77
5.9. Treatment for different types of elderly chronic constipation
Treatment for chronic function constipation: Correct lifestyle is the fundamental therapy, including sufficient fluid and fiber intake, proper exercise, and regular defecation habit.5, 14, 48, 84 In medication, bulking agents or osmotic laxatives are the first choice. If bulking agents or osmotic laxatives fail, prokinetic agents can be used to promote bowel function.56, 57, 58, 59, 60, 61 Avoid long‐term application or abuse of stimulant laxatives. Enema or short time use of lubricant agents such as glycerinum and liquid paraffin5 is proper for evacuation disorder. Biofeedback therapy is also a reasonable choice for evacuation disorder patients without cognitive disorder.1, 80 Mixed‐constipation patients may need laxative combination of enema, bulking agents, osmotic laxatives, and prokinetic agents. Normal transit constipation patients with cognitive disorder are recommended cognitive training1 and psychological treatment if necessary. Improvement of social support may be effective to the patients who may have concerns.
Organic constipation: Treat the primary diseases and remove predisposing factors of organic constipation to relieve or reduce symptoms of constipation.
Drug‐induced constipation: Stop the medicine which may induce or aggravate constipation. Laxatives would be recommended to the patients who cannot stop the drugs concerned.
5.10. Graded approach to the treatment of chronic constipation in elderly
The treatment method may be decided by the constipation grade, type, severity, and the patient's condition.5, 15 Figure 1 shows the process of graded approach to the treatment of chronic constipation in elderly.85, 86
Figure 1.
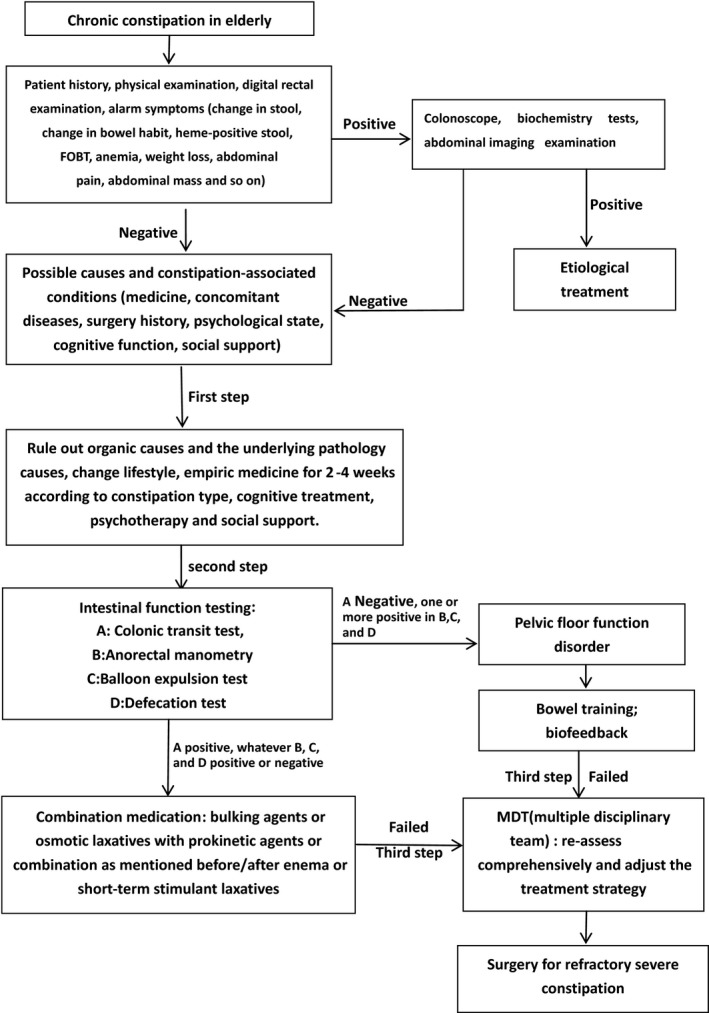
The process of graded approach to the treatment of chronic constipation in elderly
The first step in the graded approach:It is appropriate for mild‐moderate constipation. Organic constipation should be identified after asking case history, general physical examination, anorectal examination, FOBT, and other examinations if necessary. Drug‐induced constipation could be identified after asking medical history. The treatment in first step is based on recommending changes in lifestyle and diet, stopping or reducing medications that cause constipation, and administering fiber supplementation or other bulk‐forming agents and osmotic laxatives, adding prokinetic agents when necessary.5, 14, 48, 84 Cognitive training and psychological counseling or pharmacy treatment should be recommended for the patients with cognitive disorder. Reinforcement of social support may be considered to the patients concerned.
The second step in the graded approach: If the treatment of the first step fails, patients after re‐evaluated thoroughly would continue to do some specialized intestinal function testing, such as colonic transit test, anorectal manometry, and balloon expulsion test, to classify the types of constipation. The proper treatment measures would be taken according to the types of constipation. Combination of laxatives is usually recommended on the basis of changing lifestyle. Biofeedback therapy or short‐term stimulant laxatives may also be considered when necessary. Pay attention to the assessment of cognitive, psychology, and social support and treat if necessary.
The third step in the graded approach: If the treatment of the second step fails, the constipation patients must be re‐evaluated comprehensively, including lifestyle, diet, psychology, anorectal structure and function, organic abdominal diseases related to constipation. MDT (multiple disciplinary team) should be the choice for the patients in this step. Surgery may be considered for refractory serious constipation.
CONFLICT OF INTERESTS
There is no conflict of interest for this article.
APPENDIX 1.
1.1.
Writers: Zheng Songbai, Yao Jianfeng, Zhang Ying.
Academic Secretary: Li Xiaowen, Sun Tao, Zhang Xiaoli, Lu Meng.
Members of the Consensus Editorial Group (Alphabetical order by surname):Chen Xinyu (Zhejiang Hospital), Duan Chunbo (Beijing Hospital), Fang Jingyuan (Renji Hospital, Shanghai Jiaotong University School of Medicine), Gan Huatian (West China Hospital, Sichuan University), Guo Yonghong (Second Xiangya Hospital, Central South University), Jiang Hua (Oriental Hospital affiliated to Tong Ji University), Liu Ruixue (Liaoning People's Hospital), Liu Shixiong (The First Hospital of Lanzhou University), Luo Qingfeng (Beijing Hospital), Miao Lin (The Second Affiliated Hospital of Nanjing Medical University), Ruan Jigang (General Hospital of Ningxia Medical University), Shao Yun (The First Affiliated Hospital of Nanjing Medical University), Shi Liping (Shanxi Province People's Hospital), Wu Benyan (General Hospital of PLA), Wan J (General Hospital of PLA), Wang Gangshi (General Hospital of PLA), Wu Jing (Beijing Shijitan Hospital), Wang Ruiling (General Hospital of the PLA Rocket Force), Wang Fengyun (Xiyuan Hospital of China Academy of Chinese Medical Science), Wang Xiaozhong (Fujian Medical University, Union Hospital), Xu Le (Beijing Hospital), Xu Lishu (Guangdong General Hospital), Xu Shiping (General Hospital of PLA), Yang Shimin (Xinqiao Hospital of Third Military Medical University), Yan Xiang (The First Hospital of Lanzhou University), Yao Ping (The First Affiliated Hospital Of Xinjiang Medical University), Yao Jianfeng (Hua Dong Hospital affiliated to Fudan University), Yin Tiejun (Tongji Hospital affiliated to Tongji Medical College, Huazhong University of Science and Technology), Zhang Hangxiang (Xijing Hospital, the Fourth Military Medical University), Zheng Songbai (Hua Dong Hospital affiliated to Fudan University), Zhong Bihui (The First Affiliated Hospital of Sun Yat Sen University), Zhou Bingxi (Henan Provincial People's Hospital), Zhang Weisan (The General Hospital of TianJin Medical University), Zhu Yue (Hua Dong Hospital affiliated to Fudan University), Zhang Yu (Huashan Hospital affiliated to Fudan University), Zhang Ying (Hua Dong Hospital affiliated to Fudan University).
Zheng S, Yao J, for the Chinese Geriatric Society, Editorial Board of Chinese Journal of Geriatrics. Expert consensus on the assessment and treatment of chronic constipation in the elderly. Aging Med. 2018;1:8‐17. 10.1002/agm2.12013
Contributor Information
Songbai Zheng, Email: songbai1009@163.com.
Jianfeng Yao, Email: yjf1966@126.com.
REFERENCES
- 1. Ke MY, Wang YK. Epidemiology and research progress of chronic constipation in the elderly. Pract Geriatr. 2010;24:92‐94. [Google Scholar]
- 2. Fleming V, Wade WE. A review of laxative therapies for treatment of chronic constipation in older adults. Am J Geriatr Pharmacother. 2010;8:514‐550. [DOI] [PubMed] [Google Scholar]
- 3. Suares NC, Ford AC. Prevalence of, and risk factors for, chronic idiopathic constipation in the community: systematic review and meta analysis. Am J Gastroenterol. 2011;106:1582‐1591. [DOI] [PubMed] [Google Scholar]
- 4. Gallegos‐Orozco J, Foxx‐Orenstein A, Sterler S. Chronic constipation in the elderly. Am J Gastroenterol. 2012;107:18‐25. [DOI] [PubMed] [Google Scholar]
- 5. The Gastrointestinal Dynamics Group of Chinese Society of Gastroenterology, the Anus Colorectal Surgery Group of Surgery Academy of Chinese Medical Association . The guideline for diagnosis and treatment of chronic constipation in China. Chin J Dig. 2013;33:291‐297. [Google Scholar]
- 6. Mearin F, Lacy BE, Chang L, et al. Bowel disorders. Gastroenterology. 2016;150:1393‐1407. [DOI] [PubMed] [Google Scholar]
- 7. Chu H, Zhong L, Li H, et al. Epidemiology characteristics of constipation for general population, pediatric population, and elderly population in China. Gastroenterol Res Pract. 2014;2014:532734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vazquez RM, Bouras EP. Epidemiology and management of chronic constipation in elderly patients. Clin Interv Aging. 2015;10:919‐930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chu H, Hou X. Understanding of constipation symptoms and the diagnosis and management of constipation in Chinese physicians. PLoS ONE. 2016;11:e0152801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhang XL, Zheng SB. Epidemiology of chronic constipation: current status. Chin J Mult Organ Dis Elderly. 2014;13:178‐181. [Google Scholar]
- 11. The Spleen and Stomach Disease Academy of China Association of Chinese Medicine . Consensus on the diagnosis and treatment of chronic constipation with traditional Chinese medicine. Chin J Tradit West Med Dig. 2010;18:136‐139. [Google Scholar]
- 12. Gau J, Acharya UH, Khan MS, et al. Risk factors associated with lower defecation frequency in hospitalized older adults: a case control study. BMC Geriatr. 2015;15:1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Li XW, Zheng SB. Advances in studies on gastrointestinal dysmotility and its mechanisms in elderly subjects. Chin J Gastroenterol. 2014;19:746‐749. [Google Scholar]
- 14. Schuster BG, Kosar L, Kamrul R. Constipation in older adults stepwise approach to keep things moving. Can Farm Physician. 2015;61:152‐158. [PMC free article] [PubMed] [Google Scholar]
- 15. Bharucha AE, Wald AM. Anorectal disorders. Am J Gastroenterol. 2010;105:786‐794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Roberts M. Constipation, laxative use, and colon cancer in a North Carolina population. Am J Gastroenterol. 2003;98:857‐864. [DOI] [PubMed] [Google Scholar]
- 17. Tashiro N, Budhathoki S, Ohnaka K, et al. Constipation and colorectal cancer risk: the Fukuoka Colorectal Cancer Study. Asian Pac J Cancer Prev. 2011;12:2025‐2030. [PubMed] [Google Scholar]
- 18. Hu Z, Wang J. The harm and prevention of constipation in the elderly. Pract J Cardiac Cereb Pneum Vasc Dis. 2010;18:975. [Google Scholar]
- 19. Ye B, Chen CX. The anxiety depression and sleep condition of hospitalized elderly patients with chronic constipation. Chin J Gerontol. 2016;36:1996‐1998. [Google Scholar]
- 20. Yao JF, Yu Y, Zhang W, et al. Clinical characteristics of ischemic colitis in elderly accompanied with chronic constipation. Chin J Muh Organ Dis Elderly, 2014;13:165‐169. [Google Scholar]
- 21. Yang YX, Cao HY. Analysis of etiology and the causality for the changes of bowel obstruction. Modern Med J. 2011;39:312‐315. [Google Scholar]
- 22. Jao ZY. Clinical guideline of OMGE: constipation. J Gastroenterol Hepatol. 2002;11:382‐384. [Google Scholar]
- 23. Kyle GA. Guide to managing constipation: part two. Nurs Times. 2007;103:42‐43. [PubMed] [Google Scholar]
- 24. Locke GR, Pemberton JH, Phillips SF. AGA technical review on constipation. American Gastroenterological Association. Gastroenterology. 2000;119:1766‐1778. [DOI] [PubMed] [Google Scholar]
- 25. Yang RM. Constipation and behavior in the elderly. Geriatr Health Care. 2003;9:53‐54. [Google Scholar]
- 26. Chen CX, Li JM, Wang J, et al. Effect of long‐term history in taking medicine and anxiety on constipation of the aged. Modern Prev Med. 2008;35:101‐102. [Google Scholar]
- 27. Zhu LM, Fang XC, Liu S, et al. Multi‐centered stratified clinical studies for psychological and sleeping status in patients with chronic constipation in China. Natl Med J China. 2012;92:2243‐2246. [PubMed] [Google Scholar]
- 28. Van Oudenhove L, Vandenberghe J, Demyttenaere K, et al. Psychosocial factors, psychiatric illness and functional gastrointestinal disorders: a historical perspective. Digestion. 2010;82:201‐210. [DOI] [PubMed] [Google Scholar]
- 29. Han WT, Zhao XJ, Chen CX, et al. Effect of social support and life habits on constipation in the elderly of the nursing home. Chin J Gerontol. 2013;33:4866‐4867. [Google Scholar]
- 30. Zhao ZZ, Lin Z, Lin L, et al. Relationship of social support and quality of life in patients with chronic constipation. Jiangsu Med J. 2010;36:1640‐1642. [Google Scholar]
- 31. Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997;32:920‐924. [DOI] [PubMed] [Google Scholar]
- 32. Duan ZC, Xu Q. Evaluation and intervention for frailty in old adults (review). Chin J Rehabil Theory Pract. 2015;21:1282‐1286. [Google Scholar]
- 33. Li XW, Zheng SB. Frailty of the elderly. Int J Geriatr. 2014;35:75‐79. [Google Scholar]
- 34. Davis K, Kumar D. Posterior pelvic floor compartment disorders. Best Pract Res Clin Obstet Gynaecol. 2005;19:941‐958. [DOI] [PubMed] [Google Scholar]
- 35. Zhang YY, Ning XL, Lin LZ, et al. Application of cognitive behavioral intervention on senile habitual constipation. Med Innov China. 2015;12:106‐107. [Google Scholar]
- 36. Wang RT, Li Y. Analysis of cognitive function of old people with functional constipation. J Harbin Med Univ. 2011;45:603‐605. [Google Scholar]
- 37. Weinland SR, Morris CB, Hu Y, et al. Characterization of episodes of irritable bowel syndrome using ecological momentary assessment. Am J Gastroenterol. 2011;106:1813‐1820. [DOI] [PubMed] [Google Scholar]
- 38. Yang XC, He DH, Huang YN. Efficacy application toilet training method of treatment of functional constipation in elderly. Guide China Med. 2014;12:65‐66. [Google Scholar]
- 39. Chinese Nutrition Society . Chinese residents dietary guidelines (2016). Beijing: People's Medical Publishing House; 2016. [Google Scholar]
- 40. Marteau P, Jacobs H, Cazaubiel M, et al. Effects of chicory inulin in constipated elderly people: a double‐blind controlled trial. Int J Food Sci Nutr. 2011;62:164‐170. [DOI] [PubMed] [Google Scholar]
- 41. Collado Yurrita L, San Mauro Martin I, Ciudad‐Cabanas MJ, et al. Effectiveness of inulin intake on indicators of chronic constipation; a meta‐analysis of controlled randomized clinical trials. Nutr Hosp. 2014;30:244‐252. [DOI] [PubMed] [Google Scholar]
- 42. Hy L, Wei ZJ, Liu DQ. Diagnosis and management of opioid—induced constipation. Chin J Clin Oncol. 2015;42:603‐607. [Google Scholar]
- 43. Li QQ, Jiang H. Chronic constipation in the elderly: advances in medication treatment. Chin J Mult Organ Dis Elderly. 2014;13:182‐185. [Google Scholar]
- 44. Klaschik E, Nauck F, Ostgathe C. Constipation‐modern laxative therapy. Support Care Cancer. 2003;11:679‐685. [DOI] [PubMed] [Google Scholar]
- 45. Duan JL. Recent advances of diseases drugs in the treatment of digestive system. Eval Anal Drug‐Use Hosp China. 2007;7:401‐405. [Google Scholar]
- 46. Tack J, Mfiller‐Lissner S, Stanghellini V, et al. Diagnosis and treatment of chronic constipation–a European perspective. Neuro Gastroenterol Motil. 2011;23:697‐710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ramkumar D, Rao SS. Efficacy and safety of traditional medical therapies for chronic constipation: systematic review. Arn J Gastroenter. 2005;100:936‐971. [DOI] [PubMed] [Google Scholar]
- 48. Zheng SB, Chen MM. Treatment of chronic constipation for the elderly deserves great attention. Chin J Mult Organ Dis Elderly. 2014;13:161‐164. [Google Scholar]
- 49. Kurniawan I, Simadibrata M. Management of chronic constipation in the elderly. Acta Med Indones. 2011;43:195‐205. [PubMed] [Google Scholar]
- 50. Gallagher P, O'Mahony D. Constipation in old age. Best Pract Res Clin Gastroenterol. 2009;23:875‐887. [DOI] [PubMed] [Google Scholar]
- 51. Ford AC, Suares NC. Effect of laxatives and pharmacological therapies in chronic idiopathic constipation: systematic review and meta‐analysis. Gut. 2011;60:209‐218. [DOI] [PubMed] [Google Scholar]
- 52. Manabe N, Cremonini F, Camilleri M, et al. Effects of bisacodyl on ascending colon emptying and overall colonic transit in healthy volunteers. Aliment Pharmacol Ther. 2009;30:930‐936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Zhou Q, Chen YG. Clinical treatment of chronic functional constipation: research status. Chin J Integr Tradit West Med Dig. 2013;21:611‐613. [Google Scholar]
- 54. Kamm MA, Mueller Lissner S, Waid A, et al. Oral bisacodyl is effective and well—tolerated in patients with chronic constipation. Clin Gastroenterol Hepatol. 2011;9:577‐583. [DOI] [PubMed] [Google Scholar]
- 55. Vasanwala F. Management of chronic constipation in the elderly. Sing Fam Phys. 2009;35:84‐92. [Google Scholar]
- 56. Track J. Current and future therapies for chronic constipation. Best Pract Res Clin Gastroenterol. 2011;25:151‐158. [DOI] [PubMed] [Google Scholar]
- 57. Kanazawa M, Watanabe S, Tana C, et al. Effect of 5‐HT4 receptor agonist mosapride citrate on rectosigmoid sensorimotor function in patients with irritable bowel syndrome. Neurogastroenterol Motil. 2011;23:332‐754. [DOI] [PubMed] [Google Scholar]
- 58. Editorial Board of Chinese Journal of Geriatrics, Chinese Geriatric Society . The consensus on diagnosis and treatment of functional dyspepsia in the elderly. Chin J Geriatr. 2015;34:698‐705. [Google Scholar]
- 59. Xu DB, Ke MY. Itopride hydrochloride, a new gastrointestinal prokinetic agent. Chin J New Drugs. 2002;11:437‐439. [Google Scholar]
- 60. Tsubouchi T. Stimulatory action of Itopride hydrochloride on colonic motor activity in vitro and in vivo. J Pharmacol Exp Ther. 2003;306:787‐793. [DOI] [PubMed] [Google Scholar]
- 61. Hc L, Kim YG, Lim JH, et al. Effect of Itopride hydrochloride on the ileal and colonic motility in guinea pig in vitro. Yonsei Med J. 2008;49:472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Wang ZH. Clinical observation on 43 cases of the Itopride treatment of constipation. J Clin Intern Med. 2003;20:523. [Google Scholar]
- 63. Deng XP, Zhao LP, Wu ZJ, et al. Effect of Itopride in treatment of chronic constipation patients. Chin J Gastroenterol Hepatol. 2012;21:447‐449. [Google Scholar]
- 64. Wang L. Clinical observation on the treatment of constipation with itopride and lactulose in the elderly. China Prac Med. 2012;7:159‐160. [Google Scholar]
- 65. Bassotti G, Gambaccini D, Bellini M. Prucalopride succinate for the treatment of constipation: an update. Expert Rev Gastroenterol Hepatol. 2016;10:291‐300. [DOI] [PubMed] [Google Scholar]
- 66. Wong BS, Manabe N, Camilleri M. Role of prucalopride, a serotonin(5‐HT(4)) receptor agonist, for the treatment of chronic constipation. Clin Exp Gastroenterol. 2010;3:49‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Framptom J. Prucalopride. Drugs. 2009;69:02463‐02476. [DOI] [PubMed] [Google Scholar]
- 68. Camilleri M, Beyens G, Kerstens R, et al. Safety assessment of prucalopride in elderly patients with constipation: a double‐blind, placebo‐controlled study. Neurogastroenterol Motil. 2009;21:1117‐1256. [DOI] [PubMed] [Google Scholar]
- 69. Barish CF, Drossman D, Johanson JF, et al. Efficacy and safety of Lubiprostone in patients with chronic constipation. Dig Dis Sci. 2010;55:1090‐1097. [DOI] [PubMed] [Google Scholar]
- 70. Gonzalez‐Martinez MA, Ortiz‐Olvera NX, MendezNavarro J. Novel pharmacological therapies for management of chronic constipation. J Clin Gastroenterol. 2014;48:21‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Lembo AJ, Schneier HA, Shiff SJ, et al. Two randomized trials of linaclotide for chronic constipation. N Engl J Med. 2011;365:527‐536. [DOI] [PubMed] [Google Scholar]
- 72. Quigley EM. The enteric microbiota in the pathogenesis and management of constipation. Best Pract Res Clin Gastroenterol. 2011;25:119‐126. [DOI] [PubMed] [Google Scholar]
- 73. Leung L, Riutta T, Kotecha J, et al. Chronic constipation: an evidence‐based review. J Am Board Fam Med. 2011;24:436‐451. [DOI] [PubMed] [Google Scholar]
- 74. Hungin AP, Mulligan C, Pot B, et al. Systematic review: probiotics in the management of lower gastrointestinal symptoms in clinical practice‐an evidence based international guide. Aliment Pharmacol Ther. 2013;38:864‐886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Li H, Yang YZ, Yuan YZ, et al. Live combined Bifidobacterium, Lactobacillus and Enterococcus capsules/powder for the treatment of functional constipation: a meta analysis. Chin J Prac Int Med. 2016;36:724‐728. [Google Scholar]
- 76. Zhou L, Lin Z, Lin L, et al. Functional constipation: implications for nursing interventions. J Clin Nurs. 2010;19:1838‐1843. [DOI] [PubMed] [Google Scholar]
- 77. The Anus Colorectal Surgery Group of Surgery branch of Chinese Medical Association . The consensus on surgical diagnosis and treatment of constipation. Chin J Gastrointest Surg. 2010;13:546‐547. [Google Scholar]
- 78. Koh CE, Young CJ, Young JM, et al. Systematic review of randomized controlled trials of the effectiveness of biofeedback for pelvic floor dysfunction. Br J Surg. 2008;95:1079‐1087. [DOI] [PubMed] [Google Scholar]
- 79. Yu T, Lin L. Evaluation of efficacy of biofeedback therapy on chronic Constipation. Chin J Gastroenterol. 2016;21:104‐106. [Google Scholar]
- 80. Rao SS, Valestin J, Brown CK, et al. Long‐term efficacy of biofeedback therapy for dyssynergic defecation: randomized controlled trial. Am J Gastroenterol. 2010;105:890‐896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Wolff K, Marti L, Beutner U, et al. Functional outcome and quality of life after stapled transanal rectal resection for obstructed defecation syndrome. Dis Colon Rectum. 2010;53:881‐888. [DOI] [PubMed] [Google Scholar]
- 82. Liu YG, Zang JX, Li YW, et al. Treatment of musculi puborectalis syndrome with partial excision of musculi puborectalis: analysis in 149 cases. J Luoyang Med Coll. 2001;19:17‐18. [Google Scholar]
- 83. Dudekula A, Huftless S, Bielefeldt K. Colectomy for constipation: time trends and impact based on the US Nationwide Inpatient Sample, 1998‐2011. Aliment Pharmacol Ther. 2015;42:1281‐1293. [DOI] [PubMed] [Google Scholar]
- 84. Rao S, Go J. Update On the management of constipation in the elderly: new treatment options. Clin Interv Aging. 2010;9:163‐171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Lindberg G, Hamid SS, Malfertheiner P, et al. World Gastroenterology Organisation global guideline: constipation a global perspective. J Clin Gastroenterol. 2011;45:483‐487. [DOI] [PubMed] [Google Scholar]
- 86. Rao SS, Rattanakovit K, Patcharatrakul T. Diagnosis and management of chronic constipation in adults. Nat Rev Gastroenterol Hepatol. 2016;13:295‐305. [DOI] [PubMed] [Google Scholar]


