Abstract
China has stepped into an aging society. The social service development statistical bulletin 2015 published in July 2016 by Ministry of Civil Affairs showed that till the end of 2015, the amount of people ≥60 years of age had already approached to 222 million, which comprised 16.1% of the Chinese population, while the amount of people ≥65 years of age comprised 10.5% of the Chinese population was 143 million.1 Hypertension is an independent risk factor for cardio‐cerebral‐vascular diseases and is a primary and contributory cause for death and disability in the elderly. A large number of epidemiological and clinical studies have shown that the risk of target organ damage of hypertension such as ischemic heart disease, cardiac insufficiency, stroke, chronic kidney disease, and aortic and peripheral artery diseases significantly increases with aging. Blood pressure control plays a significant role in reducing cardio‐cerebral‐vascular events and all‐cause mortality.2 Compared to younger patients with similar blood pressure elevation, the risks of cardiovascular and cerebrovascular events significantly increase in the elderly. Because of specialties in the pathogenesis and clinical manifestation in older patients with hypertension, physicians should pay more attention to the population characteristics and individual treatments.
Keywords: elderly, hypertension
1. INTRODUCTION
China has stepped into an aging society. The social service development statistical bulletin 2015 published in July 2016 by Ministry of Civil Affairs showed that till the end of 2015, the amount of people ≥60 years of age had already approached to 222 million, which comprised 16.1% of the Chinese population, while the amount of people ≥65 years of age comprised 10.5% of the Chinese population was 143 million.1 Hypertension is an independent risk factor for cardio‐cerebral‐vascular diseases and is a primary and contributory cause for death and disability in the elderly. A large number of epidemiological and clinical studies have shown that the risk of target organ damage of hypertension such as ischemic heart disease, cardiac insufficiency, stroke, chronic kidney disease, and aortic and peripheral artery diseases significantly increases with aging. Blood pressure control plays a significant role in reducing cardio‐cerebral‐vascular events and all‐cause mortality.2 Compared to younger patients with similar blood pressure elevation, the risks of cardiovascular and cerebrovascular events significantly increase in the elderly. Because of specialties in the pathogenesis and clinical manifestation in older patients with hypertension, physicians should pay more attention to the population characteristics and individual treatments.
Since the publication of guideline for hypertension prevention and management in China (2010)3 and Chinese expert consensus on the diagnosis and treatment of hypertension in the elderly (2008, 2011),4, 5 multiple guidelines have been updated accordingly and further improved the strategy of hypertension prevention and control. For instance, 2013 European Society of Hypertension (ESH)/European Society of Cardiology (ESC) guidelines for the management of arterial hypertension,6 2014 evidence‐based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC‐8),7 the Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2014),8 2015 guidelines of the Taiwan Society of Cardiology and the Taiwan Hypertension Society for the management of hypertension,9 and Hypertension Canada's 2017 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults.10 These updated guidelines further improved the prevention and control strategy of hypertension. Recently, the American College of Physicians (ACP) and the American Academy of Family Physicians (AAFP) have published their joint guidelines for management and target of blood pressure control in patients ≥60 years of age.11 Based on this, Chinese expert consensus on the diagnosis and treatment of hypertension in the elderly (2011) is updated as to facilitate the prevention and management of hypertension in Chinese elderly.
2. DEFINITION AND MEASUREMENT OF HYPERTENSION IN THE ELDERLY
2.1. Definition of hypertension in the elderly
A clinical diagnosis of hypertension in the elderly is established by demonstrating apersistent or at least 3 times in different days systolic blood pressure (SBP) ≥ 140 mm Hg (1 mm Hg = 0.133 kpa) and/or a diastolic blood pressure (DBP) ≥ 90 mm Hg in sitting position in patients ≥ 60 years of age. In addition, isolated systolic hypertension is defined as SBP ≥ 140 mm Hg and DBP < 90 mm Hg.
2.2. Blood pressure measurement in the elderly
It is very important to measure BP accurately in the diagnosis and management of hypertension in the elderly, and the followings should be attentioned: (i) Patients should sit calmly for 5 minutes before BP measurement, usually in sitting position, with cuff at heart level; (ii) compared with office BP measurement, out‐of‐office BP monitoring (especially home blood pressure monitoring, HBPM) represents a more reliable assessment of actual BP; (iii) patient BP should be measured in both arms during the initial visit;(iv) BP should be measured at 1‐minute and 3‐minute intervals after assumption of standing position to make sure if there is orthostatic hypotension during the initial visit or after management adjustment; (v) HBPM could be measured 2‐3 times and then averaged; and (vi) pulse rate should be measured while BP measurement.
Cutoff values of BP by different measuring methods: Office BP < 140/90 mm Hg, HBPM < 135/85 mm Hg, ABPM < 130/80 mm Hg, and daytime ABPM < 135/85 mm Hg.
In recent years, automated office blood pressure using oscillometric devices is recommended, and hypertension is defined as values ≥ 135 mm Hg in SBP or ≥85 mm Hg in DBP. A study in Canada showed that in community‐dwelling residents aged ≥ 65 years untreated for hypertension, relative to the reference BP categories of 110‐119 mm Hg SBP and 60‐69 mm Hg DBP, cardiovascular risk was significant elevated at a SBP of 135‐144 mm Hg (HR 1.66, 95% CI 1.09, 2.54; P = .02), at a DBP of 80‐89 mm Hg (HR 1.72, 95% CI 1.21, 2.45; P = .003)12 HBPM is very important in BP monitoring and treatment evaluation for elderly patients with hypertension, so they should be encouraged to master the basic measuring method of cuff‐electronic sphygmomanometer and to enhance self‐management of BP. However, HBPM is not recommended in elderly patients with mental stress or anxiety. ABPM could be used in patients with a large blood pressure variability or with poor controlled BP, and it could be used as a routine examine tool in the diagnosis and efficacy monitoring in elderly hypertensive patients if possible. However, more large‐scale clinical trials are needed to establish the normal range of ambulatory blood pressure in the elderly.
3. EPIDEMIOLOGY AND STATUS OF PREVENTION AND TREATMENT IN HYPERTENSIVE ELDERLY
Comprehensive report on national nutrition and health status survey 2002 showed that the prevalence of hypertension in Chinese population older than 60 is around 49.1% in 2002,13 but the prevalence moved up to 58.9% in 2012 according to Report on nutrition and chronic diseases in China 2015,14 and the rising range is approximately 20%. The prevalence of hypertension progressively increases with age, and approximately 3 in 5 elderly people suffer from hypertension in China. American data in 2011‐2014 demonstrated that in 65‐ to 74‐year‐old people, hypertension prevalence was 63.4% in men and 64.3% in women, and in people ≥75 years of age, the prevalence was 72.3% in men and 79.9% in women.15 Compared to middle‐aged and young patients, the risk of cardiovascular and cerebrovascular events, target organ damage, and other diseases increases in the elderly. A research on risk factors and treatment status of clinic patients with hypertension and other cardiovascular diseases demonstrated16 that about 42.6% of hypertensive patients were combined with other clinical diseases, approximately 90% had more than one risk factor, and 13.2% were combined with target organ damage. About 78.4% of hypertensive patients ≥65 years of age were on high‐ or very high‐risk level. A systematic analysis for the global burden of disease study on global, regional, and national comparative risk assessment of behavioral, environmental, and occupational, and metabolic risks demonstrated that hypertension was at top of the list.17 In addition, hypertension is the most important risk factor for stroke.18
In recent years, the rate of awareness, treatment, and control for hypertension in China has been improved, which was 53.7%, 48.8%, and 16.1%, respectively, in ≥60 years hypertensive patients in 2012,14 but there still remains a wide range with western developed countries. The rate of awareness, treatment, and control of hypertension was 86.1%, 82.2%, and 50.5%, respectively, in the USA 2011‐2012.19
4. CHARACTERISTICS OF HYPERTENSION IN THE ELDERLY
4.1. Pathophysiological characteristics20
Age‐associated fatigue fracture of elastin and collagen deposition increase atherosclerotic arterial diseases, hypertrophy, and sclerosis of muscular arteries and arterioles, and these vascular changes lead to the following: (i) Large vessels become less distensible, resulting in increasing in the left ventricular ejection resistance and late systolic blood pressure (SBP) augmentation; (ii) the decreased arterial compliance and the ability to buffer the blood pressure, which promotes the early return of the reflected waves from the diastole to the systolic period, cause an increase in systolic pressure and pulse pressure but a fall in diastolic pressure; (iii) reduction in the elasticity of the aorta, vascular elasticity, and reserve capacity, which results in the increase in systolic blood flow from ventricle to peripheral artery and the decrease in blood volume in elastic reserve vessels at early diastolic period, causes decrease in diastolic blood pressure (DBP); and (iv) the lumen of arterioles is narrowed or even closed because of the age‐related small arteries arteriosclerosis, which causes a significantly increase in total peripheral resistances.
Cardiac structural aging changes, such as left ventricular myocardial fibrosis, ventricular wall thickening, and compliance decline, may lead to both cardiac systolic and diastolic function decrease, left ventricular systolic pressure increase, cardiac load increase and atrial enlargement, and thus cardiac insufficiency and arrhythmia. Progressive renal structure changes with aging induce a reduction in renal plasma flow and glomerular filtration rate (GFR), damage of renal tubule concentration and secretion, reduction in kidney drain function, and increase in salt sensitivity, which cause extracellular capacity expansion and water‐sodium retention. Chronic hypertension increases the threshold value of renal self‐regulative perfusion and renal impairment.
The sensitivity of the pressure receptor decreased in elderly hypertensive patients, which reduces the blood pressure fluctuation buffer ability and adjustment ability. The increase in vascular stiffness, compliance declines, and endothelial dysfunction decline the ability of adjusting pressure changes in blood vessels. The impairment of blood pressure regulation increases the blood pressure variability in elderly patients with hypertension. Besides that, elderly patients with hypertension are often accompanied with atherosclerotic cardiovascular disease (ASCVD), and the risk of cardiovascular events elevates when blood pressure fluctuates acutely. Many diseases coexist in elderly patients, and their reciprocal causation will increase cardiovascular and cerebrovascular events. Furthermore, high‐salt diet in the elderly can result in increased capacity load; low blood volume easily occurs because of the insensitivity of the thirsty central; blood pressure fluctuations and adverse drug reactions are commonduring the antihypertensive therapy.
4.2. Clinical characteristics of hypertension in the elderly21
Isolated systolic hypertension: The systolic hypertension in the elderly increases with age, while DBP declines slightly after 60 years old. Compared with DBP, SBP is more closely related to the target organ damage, and it is a stronger independent risk factor for incident cardiovascular events.
Increased pulse pressure: Pulse pressure is a measure of vascular stiffness, which is associated with physiological aging and various diseases that lead to vascular aging. Pulse pressure augmentation is a characteristic in the elderly hypertension, which is defined as pulse pressure >40 mm Hg. For the elderly, the pulse pressure can be as high as 50‐100 mm Hg. Multiple studies demonstrated that pulse pressure in the elderly is positively correlated with all‐cause death, cardiovascular death, stroke, and coronary heart disease.22, 23, 24, 25 However, another research showed that, for predicting cardiovascular events in elderly patients, pulse pressure is no better than SBP.26
Blood pressure fluctuation: With the increase in age, blood pressure in elderly patients with hypertension tends to fluctuate significantly with mood, season, and body position. The early morning hypertension surge tends to occur most frequently in the elderly. Blood pressure fluctuation in the elderly increases the difficulty of blood pressure treatment. In addition, elderly hypertensive patients are often coexisted with coronary artery, renal artery, carotid artery, and intracranial arterial disease, when blood pressure fluctuates sharply, cardiovascular events and target organ damage can be significantly increased.
Orthostatic hypotension: Orthostatic hypotension is defined as a reduction of ≥20 mm Hg in SBP or ≥10 mm Hg in DBP from lying to standing position within 3 minutes, with insufficient perfusion symptoms, such as dizziness or syncope.3 Orthostatic hypotension is common in the elderly because of age‐related blood vessel stiffness and autonomic neuropathy, especially when accompanied with diabetes mellitus, hypovolemia, use of diuretic, vasodilator, and psychotropic medicine. Therefore, lying and standing blood pressure should be measured during the diagnosis and treatment of hypertension in the elderly.
Postprandial hypotension (PPH): It is defined as systolic blood pressure dropped ≥ 20 mm Hg within 2 hours after meal, or preprandial SBP ≥ 100 mm Hg, and postprandial SBP < 90 mm Hg with symptoms of dizziness, fainting, angina pectoris, and other hypotensive symptoms after eating.27
Abnormal blood pressure circadian rhythm: An adult's BP normally decreases during the night, and a nighttime BP fall of 10%‐20% of daytime values is defined as dipper type blood pressure rhythm. Elderly patients often have abnormal circadian rhythm of blood pressure, such as a nighttime BP fall < 10% (nondipping pattern) or >20% (extreme‐dipping pattern), and even a reverse‐dipping pattern which nighttime BP reversely increases. In patients with abnormal blood pressure circadian rhythm, it is more likely to develop heart, brain, or kidney damage.28 The incidence of nondipping pattern blood pressure in elderly patients can reach to 60% or more. Compared to younger patients, the circadian abnormality of blood pressure is more closely related to the damage of target organs in the elderly.
Office hypertension: White‐coat hypertension is defined as SBP greater than 140 mm Hg or DBP greater than 90 mm Hg measured by a doctor or nurse in the clinic together with a normal daytime by ambulatory BP monitoring or home blood pressure measurements. White‐coat hypertension is common in the elderly and may lead to overtreatment. For patients with office hypertension, it is encouraged to strengthen the blood pressure monitoring and family self‐test. When necessary, ABPM is used to assess the presence of office hypertension. It is recommended to check the blood pressure gauge if necessary to avoid measurement errors. Besides that, patients with office hypertensive are often associated with metabolic abnormalities, which increases the cardio‐cerebral‐vascular risks.
Multiple diseases coexistence and many complications: Elderly hypertension is often associated with ASCVD and other risk factors for cardiovascular and cerebrovascular diseases, and some patients suffer from multiple diseases meanwhile. If BP cannot be well controlled long term, it is more likely to cause or aggravate target organ damage and increase the mortality of cardio‐cerebral‐vascular diseases and total mortality significantly. However, symptoms of hypertension or accompanying diseases in some elderly patients are not typical, which can easily lead to missed diagnosis, so comprehensive evaluation should be carried out to establish reasonable treatment measures. Cerebrovascular disease is common in elderly patients, which needs more attention to screening and evaluation. If the patient has bilateral carotid stenosis (≥70%) or severe intracranial arterial stenosis, excessive reduction or fluctuation of blood pressure may increase the risk of ischemic stroke.
-
Types of hypertension that may be missed or misdiagnosed:
-
a
Secondary hypertension: Secondary hypertension is commonly reported in the elderly population, including renal vascular hypertension, renal hypertension, primary hyperaldosteronism, and pheochromocytoma. Secondary hypertension should be suspected in patients with sudden onset or worsening of hypertension, or poor BP response to various antihypertensive drugs therapy. Obstructive sleep apnea hypopnea syndrome (OSAHS) in elderly can lead to or aggravate hypertension, which can be seen as the rising of nocturnal sleep or early morning blood pressure and the changing of blood pressure circadian rhythm.
-
b
Masked hypertension: Masked hypertension is characterized by normal office BP values, but elevated BP values from out‐of‐office (ABPM/HBPM) readings. Diagnostic criteria: Office blood pressure <140/90 mm Hg, while systolic blood pressure ≥ 135 mm Hg and/or diastolic blood pressure ≥ 85 mm Hg by HBPM; daytime systolic blood pressure ≥ 135 mm Hg; and/or diastolic blood pressure ≥ 85 mm Hg by ABPM. The risk of target organ damage increases in patients with masked hypertension.
-
c
Pseudohypertension: Pseudohypertension is defined that the blood pressure measured by cuff is higher than that measured within the arterial, with the elevation of SBP ≥ 10 mm Hg or DBP ≥ 15 mm Hg, which is commonly seen in elderly patients with severe atherosclerosis. In the elderly, the brachial arteries may become very thickened and stiff due to arterial medial sclerosis and calcification, which is hard to be compressed, while the cuff is inflating, so the BP reading measured with indirect techniques may be falsely higher than the actual intra‐arterial pressure. Pseudohypertension should be suspected in elders with refractory hypertension without obvious target organ damage or hypotension symptoms after antihypertensive medication and continuous elevation of cuff blood pressure. Accurate blood pressure can be obtained by the determination of noninvasive central arterial pressure or direct measurement of intra‐arterial pressure.
-
a
| Key point 1. Clinical features of hypertension in the elderly |
|---|
| Isolated systolic hypertension |
| Increased pulse pressure |
| Blood pressure variability |
| Liable to occur orthostatic hypotension |
| Combined with postprandial hypotension |
| Abnormal blood pressure circadian rhythm |
| Multiple diseases coexistence and many complications |
| Office hypertension |
| Secondary hypertension is easily missed |
5. THE MAIN CLINICAL EVIDENCE FOR THE TREATMENT OF HYPERTENSION IN ELDERLY PATIENTS
Researches including systolic hypertension in the elderly program (SHEP),29 Swedish trail in old patients with hypertension (STOP‐H),30 systolic hypertension in Europe (Syst‐Eur),24 and the study on cognition and prognosis in the elderly (SCOPE)31 had confirmed that antihypertensive treatment of elderly hypertension reduces the incidence and mortality of cardio‐cerebral‐vascular disease, as well as the risk of cognitive decline and cardiovascular events. Elderly men over the age of 70 with high pulse pressure and cardiovascular complications have more benefit. Systolic hypertension in China (Syst‐China)23 demonstrated that antihypertensive therapy reduces mortality by 55% in elderly hypertensive patients. Subgroup analysis in HOT‐CHINA32 showed that antihypertensive therapy for 3050 very elderly patients (aged between 80 and 90 (82.6 ± 2.5)) has high control rate, low incidence of adverse events accompany with good efficacy, safety, and compliance. Hypertension in the very elderly trial (HYVET)33 was a large‐scale, randomized, double‐blind, placebo‐controlled study of hypertension patients over 80 years old, and a total of 3845 very elderly patients (age between 80 and 105, mean age 83.6 years) were enrolled, including 1526 Chinese patients, and median follow‐up was 1.8 years (1‐5 years). In the active‐treatment group, the average blood pressure was 144/78 mm Hg compared with 161/84 mm Hg of placebo group. In an intention‐to‐treat analysis, active treatment was associated with a 21% reduction in the rate of death from any cause (P = .019), a 30% reduction in the rate of stroke (P = .06), a 39% reduction in the rate of death from stroke (P = .05), a 64% reduction in the rate of heart failure (P < .001), and a 34% reduction in the rate of severe cardiovascular events (P < .001). The Felodipine Event Reduction (FEVER) trial34 was a prospective, multicenter, randomized, double‐blind controlled trial. A total of 9711 randomly assigned Chinese patients aged 50‐79 years were included in the intention‐to‐treat analysis. The subgroup analysis of elderly35 included 3179 patients showed that in hypertensive patients aged >65 years, significant reductions in stroke were found in elderly hypertensive patients (−44%, P < .001) when their SBP was lowered to a mean just <140 mm Hg (rather than 145 mm Hg), significant reductions (−47%, −51%, −36%, and −49%, P =< .001, 0.002, 0.013, and 0.004) were also found in cardiovascular events, cardiac events, all deaths, and cardiovascular death. However, the results in Japanese trial to assess optimal systolic blood pressure in elderly hypertensive patients (JATOS)36 indicated that strict treatment (reduce SBP to 138 mm Hg) for elderly hypertensive patients has no more clinical benefits as compared with mild treatment (reduce SBP to 147 mm Hg). Valsartan in the elderly isolated systolic hypertension study (VALISH)37 was a prospective, randomized, open‐label, blinded endpoint study; 3260 patients aged 70‐84 years with isolated systolic hypertension (SBP 160‐199 mm Hg) were enrolled. Valsartan was administrated as the first‐step therapy, and the population was divided into strict BP control group (SBP < 140 mm Hg) and moderate BP control group (SBP 140‐150 mm Hg). After average follow‐up of 3.07 years, BP reached 136.6/74.8 mm Hg and 142.0/76.5 mm Hg, respectively. There were no statistical significances on the overall rate of the primary composite endpoint and rate of adverse event. The result proved that strict BP control (SBP to <140 mm Hg) may not enhance the clinical benefit in the prevention of cardiovascular events as compared with that of moderate BP control (SBP 140‐150 mm Hg). The international verapamil SR/trandolapril study (INVEST)38 involved 22 576 clinically stable hypertensive coronary artery disease patients. The patients were grouped by age in 10‐year increments (aged ≥ 80, n = 2180; 70‐79, n = 6126; 60‐69, n = 7602; <60, n = 6668) with an average follow‐up of 2.7 years. Compared with the subgroup which SBP reduces to less than 130 mm Hg, the risks of death, myocardial infarction, and stroke are lower in the 70‐ to 79‐year subgroup which average SBP reduces to 135 mm Hg and 140 mm Hg in the subgroup ≥80 years old. Systolic blood pressure intervention trial (SPRINT) assigned 9361 persons more than 50 years old with a systolic blood pressure of 130 mm Hg or higher and an increased cardiovascular risk, excluding diabetes mellitus, stroke, acute renal insufficiency (eGFR < 20 mL/min/1.73 m2), recent acute coronary syndrome, hospitalization for heart failure, and patients whose SBP were lower than 110 mm Hg in 1 minute when changed to standing position. Patients used automatic sphygmomanometer to test blood pressure by themselves, throughout the 3.26 years of follow‐up; the mean systolic blood pressure was 121.5 mm Hg in the intensive‐treatment group and 134.6 mm Hg in the standard‐treatment group, and the result showed that enhanced antihypertensive therapy can reduce the major cardiovascular events and all‐cause death further.39The elderly patients (≥75 years old) benefit from the enhanced antihypertensive treatment with no significant increase in severe adverse effects.40 Heart outcomes prevention evaluation‐3 trial (HOPE‐3)41 was a large‐scale international multicenter, randomized, double‐blind, placebo‐controlled, and comparison from a 2‐by‐2 factorial trial, which was designed to observe the effects of antihypertension (candesartan 16 mg plus hydrochlorothiazide 12.5 mg/d), lipids‐lowering (rosuvastatin 10 mg/d) therapy separated and combined on cardiovascular endpoints in participants at intermediate risk who did not have cardiovascular disease. A total of 12 705 patients were enrolled in the trial, 29% of them were Chinese. The mean age was 65.7 years old with a baseline of BP 138.1/81.9 mm Hg. After 5.6‐year follow‐up, the SBP decreased to 128.2 mm Hg and 133.9 mm Hg in the candesartan plus hydrochlorothiazide group and the placebo group, respectively. The decrease in blood pressure was 6.0/3.0 mm Hg greater in the active‐treatment group than in the placebo group, but there were no significant differences in the incidence of the outcome. Participants in the subgroup for the upper third of systolic blood pressure who were in the active‐treatment group had significantly lower rates of the first cardiovascular outcomes, as well as the therapy of statins. The prospective observational longitudinal registry of patients with stable coronary artery disease (CLARIFY)42 enrolled 22 672 patients (mean age 65.2) with stable coronary artery disease and treated for hypertension. The result showed in patients with hypertension and coronary artery disease, systolic blood pressure of less than 120 mm Hg, and diastolic blood pressure of less than 70 mm Hg for DBP was each associated with adverse cardiovascular outcomes.
6. GOALS AND PROCEDURES OF DIAGNOSIS AND TREATMENT IN THE ELDERLY
The goals of antihypertensive treatment in the elderly are to protect the target organs and minimize the risks and mortality of cardio‐cerebral‐vascular disease. The general recommended BP target in patients more than 65 years of age is <150/90 mm Hg, and the final target level of BP control is <140/90 mm Hg if tolerated. Antihypertensive medications may be considered for elderly patients with systolic blood pressure of 140‐149 mm Hg, and it is necessary to monitor BP changes and the clinical manifestations of cardiac, cerebral, and renal hypoperfusion during the treatment.
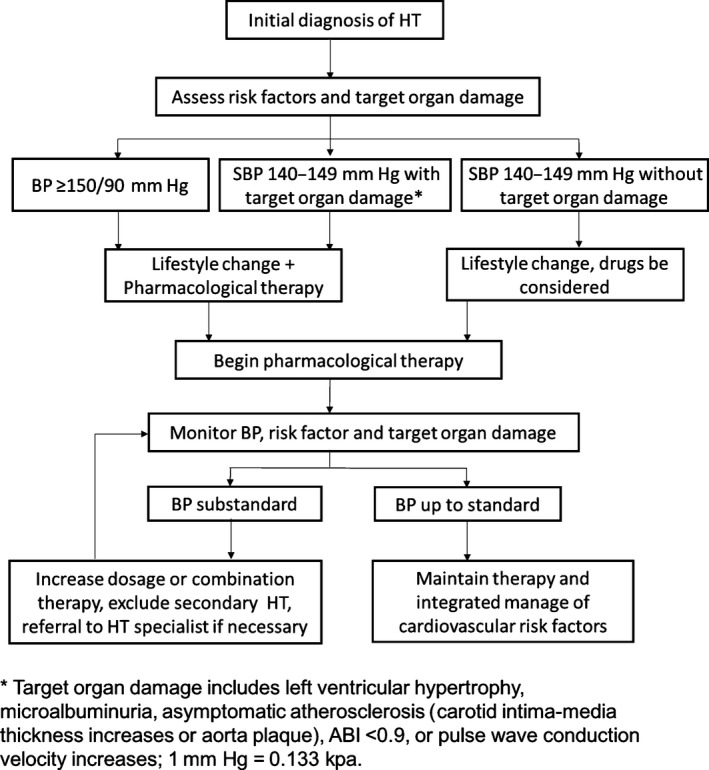
It is suggested to adopt individualized and graded treatment strategies for elderly patients with high blood pressure combined with target organ damages including heart, brain, and kidney: to lower BP of <150/90 mm Hg at first, and then to <140/90 mm Hg for the well‐tolerated people. For those patients whose age <80 years old with well‐tolerance and good condition, BP can be reduced to <130/80 mm Hg. For the patients aged ≥ 80 years old, it is recommended to reduce BP to <150/90 mm Hg at first and then to <140/90 mm Hg if tolerated. Antihypertensive therapy is particularly important in preventing stroke because of the high prevalence of stroke in China compared with western population. Antihypertensive therapy should be carefully chosen for patients suffering from symptomatic carotid stenosis, and BP should not be reduced too excessively and too fast. It is suggested to decrease BP to <140/90 mm Hg if tolerated. Excessive reduction in blood pressure is adverse to the blood perfusion of important organs, which increases the risk of syncope, fall, fracture, and death of the elderly. For elderly hypertensive patients with ischemic heart disease, physicians should pay attention to DBP while strengthening the control of SBP, and the SBP target should be gradually achieved under close monitoring when DBP is lower than 60 mm Hg. The range of blood pressure reduction should be associated with baseline of BP, the higher the baseline blood pressure, the greater the depressurizing range is. Antihypertensive drugs lower the systolic blood pressure more efficiently than diastolic blood pressure. It is emphasized to ensure SBP to reach the target and to decrease BP gradually if tolerated for elderly patients rather than too fast and excessively.
Elderly hypertensive patients are often combined with multiple diseases and many ASCVD risk factors and/or target organ damages, and most of them need two or more antihypertensive drugs for combination therapy to achieve the target. The antihypertensive drugs should be rationally selected according to the patient's individual characteristics, coexisting clinical diseases, and the combination of medication, and the risk factors for cardiovascular and cerebrovascular diseases should be evaluated and interfered. Antihypertensive drugs should begin with the minimum dose, gradually increased the dosage or type to achieve the BP target. During the therapy, BP should not be reduced too fast. Physicians should pay closely attention for the presence of symptoms of antihypertensive‐treatment related cerebral or myocardial ischemia and adverse drug reactions to avoid orthostatic hypotension or the harm of excessive depressurization. It is recommended to measure BP in standing, lying, and recumbent position for patients with significant change of postural blood pressure.
7. TREATMENTS OF HYPERTENSION IN THE ELDERLY
7.1. Lifestyle therapy
Nonpharmacological therapy is the cornerstone for the treatment of hypertension, patients should be encouraged to change lifestyles.
-
a.
Salt restriction It is very important to limit salt intake; salt‐sensitive hypertension is common in the elderly. Daily salt intake less than 6 g is recommended43 However, too aggressive salt restriction may cause hyponatremia.
-
b.
Balanced diet Elderly patients should be encouraged to eat all kinds of fresh vegetables, fruits, fish, beans and bean products, whole grains, skimmed milk, and other foods rich in potassium, calcium, dietary fiber, and polyunsaturated fatty acids.
-
c.
Quit smoking and avoid secondhand smoke Smoking causes an increase in the incidence and mortality of cardiovascular events, so it is suggested to quit smoking or avoid exposure to secondhand smoke.
-
d.
Alcohol limitation Elderly people are not encouraged to drink. It is generally agreed that alcohol intake should be limited to <25 g/d in men and <15 g/d in women. Besides that, it should be noticed that alcohol intake may affect the drug efficacy. Amount of pure alcohol (g) = Alcohol consumption (mL)* alcohol degree (%)*0.8
-
e.
Moderate body weight reduction Body weight reduction is followed by a decrease in BP. For controlling hypertension, the ideal body weight index (BMI) is ≤ 25 kg/m2.
-
f.
Regular aerobic physical exercise Regular aerobic exercise is beneficial for treatment of hypertension. Patients should be advised to participate in dynamic aerobic exercise such as brisk walking last on 30‐60 min/session, 5 sessions per week according to personal interests and physical conditions.
-
g.
Keep psychological health It is suggested to avoid mood swings and stress, maintain mental well‐being, psychological balance and regular life, and treat mental disorders such as anxiety and depression. Attention: Too aggressive diet control and salt restriction may lead to malnutrition and electrolyte disorder (such as hyponatremia, hypokalemia) for elderly patients (especially for the very old population). It will affect their life quality and cause other diseases which are induced by low immunity, if the elderly patients lose their weight fast and excessively. The blood pressure of the aged is affected by seasonal changes, with a characteristic of low BP in summer and high BP in winter. It is necessary to monitor blood pressure changes and adjust the antihypertensive drugs in time.
| Key point 2. Treatment strategies of hypertension in the elderly |
|---|
| Drugs used from small dosage to lower BP smoothly |
| Choose antihypertensive drugs carefully and observe closely |
| Combination therapy to achieve the target gradually Individualized treatment |
| Monitor standing position BP to avoid postural hypotension |
| Appreciate home BP monitoring and 24‐h BP monitoring |
| Key point 3. Nonpharmacological therapy |
|---|
| Salt restriction |
| Balanced diet |
| Reduce fat and saturated fat intake |
| Increase unsaturated fatty acid intake |
| Increase dietary fiber intake |
| Quit smoking or avoid secondhand smoke |
| Alcohol limitation |
| Moderate body weight reduction |
| Regular aerobic physical exercise |
| Keep psychological health |
7.2. Pharmacological therapy
Appropriate antihypertensive drugs can improve the control rate of hypertension, reduce the morbidity and mortality of cardiovascular and cerebrovascular diseases, and prevent the damages of target organ (stroke, coronary heart disease, heart failure, and renal insufficiency). The ideal antihypertensive drugs for the treatment of senile hypertension should meet the following requirements: (i) to lower blood pressure smoothly and effectively; (ii) with good safety and less adverse reactions; and (iii) easy to take and associated with good compliance.
-
a.
Antihypertensive drugs The current guidelines reconfirm that calcium antagonists, diuretics, angiotensin‐converting enzyme inhibitors (ACEI) and angiotensin receptor blockers (ARB), and beta‐blockers are all suitable for the initiation antihypertensive treatment in the elderly. Individual characteristics including target organ damage, coexisting disease, and risk factors for cardio‐cerebrovascular diseases should be taken into account when choosing antihypertensive drugs.
CCB: Long‐effect dihydropyridine CCB has potent BP‐lowering effect with no absolute contraindication and less adverse reactions, which is suitable for patients with low renin or low sympathetic activity. The major adverse reactions include edema, headache, flushing, gingival hyperplasia, and constipation. Nondihydropyridine CCB such as verapamil, diltiazem should be used with caution in patients with heart failure, cardiac atrioventricular conduction abnormality, and pathological sinus syndrome. Nifedipine should be used with caution in patients with tachycardia, acute coronary syndrome, and cardiac insufficiency.44
Diuretics: Diuretics are recommended for initial and combined antihypertensive therapy for elderly patients, especially suitable for elderly patients with heart failure and edema. Small dosage of thiazide diuretics (hydrochlorothiazide 6.25‐12.5 mg/d or indapamide 1.25‐2.5 mg/d) are commonly used. The adverse effects of diuretics are dose‐dependent and high‐dose diuretic for a long‐term use increases the risk of electrolyte, blood glucose, and lipid profile metabolic disorders, so physicians should monitor the renal function and electrolytes levels to avoid hypokalemia and hyperuricemia. Loop diuretics such as torsemide or furosemideare recommended in patients with severe chronic kidney disease (eGFR < 30 mL/min/1.73 m2). For the treatment of secondary or refractory hypertension, potassium‐sparing diuretics such as spironolactone, eplerenone, and amiloride should be individualized used according to the specific situation. In the application, it is necessary to monitor renal function and serum potassium level. Potassium‐sparing diuretics are prohibited when serum potassium >5.5 mmol/L and should be used with caution for patients with chronic kidney disease stage 4 (eGFR < 30 mL/min/1.73 m2).
ACEI or ARBs: ACEI or ARBs are preferred in elderly hypertensive patients with diabetes mellitus, chronic renal disease, or proteinuria, which has little effect on glucose and lipid metabolism with less side effects. When using ACEI or ARBs, bilateral renal artery stenosis should be excluded first, and physicians should monitor serum potassium, creatinine, and eGFR. ACEI or ARBs are prohibited when serum potassium >5.5 mmol/L, and it should be used with caution in patients with chronic kidney disease stage 4 (eGFR < 30 mL/min/1.73 m2). ACEI is recommended for elderly hypertensive patients with coronary heart disease and heart failure. ARBs are considered as an alternative to ACEI in patients who cannot tolerate ACEI. The major side effects of ACEIare cough and rash, rarely allotriogeustia and angioedema. The major dangerous side effect of ACEI is angioedema, and severe angioedema can be life‐threatening. ARB has fewer side effects such as coughing, an dangioneurotic edema is rare.
Beta‐blockers: Beta‐blockers can inhibit sympathetic activity, myocardial contractility, and slow heart rate, which are recommended for elderly hypertensive patients with coronary heart disease, chronic cardiac insufficiency, tachyarrhythmia, drastic blood pressure fluctuation, and high sympathetic nerve activity if no contraindications exist. The initial use of beta‐blocker should be started at the lowest dose, and adjustment should be made subsequently depending on blood pressure and heart rate. However, it is contraindicated for patients with sick sinus syndrome, II degree, or above atrioventricular block and bronchial asthma. Elderly patients often suffer from sinus bradycardia and sinus node dysfunction, so beta‐blockers should be used according to the specific situation of the patients.
Alpha‐blockers: Alpha‐blockers can be used for elderly hypertensive patients with symptoms of prostatic hyperplasia and should be taken at bed‐time from small dosage and adjustment should be made subsequently depending on blood pressure. Blood pressure in standing position should be measured to detect postural hypotension in time.
-
b.
Combination therapy Combining drugs with different antihypertensive mechanisms may be more effective than titrating doses of a single agent, with less side effects and better target organ protection. Combination therapy should be used when BP cannot reach the target with monotherapy. Elderly patients often need to take two or more antihypertensive drugs. The antihypertensive drugs can be chosen according to the characteristics of aged individuals to synergistically increase the effects and reduce the adverse reactions. In determining the combined treatment regimen, the baseline blood pressure level, coexisting cardiovascular risk factors, and target organ damage should be considered. Fixed‐dose combination is helpful to improve adherence.
7.3. The BP target and drug selection in elderly hypertensive patients with coexisting diseases
Elderly hypertensive patients are often associated with coronary heart disease, cardiac dysfunction, cerebrovascular disease, chronic kidney disease, and diabetes mellitus, so antihypertensive drugs should be chosen based on the individual characteristics (Table 1).
Table 1.
The BP target and drug selection in elderly patients
| Concomitant diseases | Antihypertensive target and drug recommendation |
|---|---|
| Stroke | BP‐lowering therapy for patients with acute ischemic stroke should be carefully performed in the first week, and it is suggested to deal with anxiety, pain, nausea, vomiting, and higher cranial pressure first. If BP constantly increases to ≥200/110 mm Hg, antihypertensive drug should be used to reduce BP gradually (the reduction <15% over the first 24 h), and BP changes should be closely observed |
| For patients with ischemic stroke eligible for thrombolytic therapy, BP should be controlled within 180/100 mm Hg | |
| The patient with acute ischemic stroke can restore the antihypertensive drugs which used before the onset of stroke or initiate antihypertensive therapy several days after the onset of the disease when in stable condition and BP consistently >140/90 mm Hg | |
| The long‐term control target of BP for patients with ischemic stroke is <140/90 mm Hg. In patients with lacunar cerebral infarction recently, a lower level <130/80 mm Hg should be targeted if possible | |
| Early positive antihypertensive therapy in patients with acute intracerebral hemorrhage may improve the prognosis, and blood pressure can be reduced to 140/90 mm Hg if no contraindications present. Antihypertensive therapy should be initiated when blood pressure ≥180/100 mm Hg with intracranial pressure increased, and the target BP is 160/90 mm Hg | |
| The target of BP in patients with intracerebral hemorrhage is <130/80 mm Hg | |
| Coronary heart disease | The target of BP control should be <140/90 mm Hg in principle and even < 130/80 mm Hg if can be tolerant. There are greater benefits from beta‐blockers and ACE inhibitors, and ARBs can be chosen when ACEI is intolerant. Calcium antagonists are to be preferred for patients with angina or uncontrolled hypertension. Physicians should be cautious when DBP < 60 mm Hg and closely monitor the BP to achieve the target |
| Chronic heart failure | The target of BP control is <130/80 mm Hg and <140/90 mm Hg for very elderly patients. Beta‐blockers, ACE inhibitors, diuretics, and aldosterone antagonist are recommended as first choice if no contraindication. ARBs can be chosen when ACEI is intolerant |
| Renal insufficiency | The target of BP control is <130/80 mm Hg and <140/90 mm Hg for very elderly patients. ACEI and ARBs are recommended as first choice if no contraindication. It is suggested to take drugs from small dosage and monitor the changes of kidney function and potassium. CCB, loop diuretics, and alpha‐ and beta‐blockers can be used for patients with CKD Stage 4 (eGFR < 30 mL/min/1.73 m2),ACEI and ARBs should be used with caution |
| Diabetes mellitus | The recommendation is to lower BP < 140/90 mm Hg and even <130/80 mm Hg if tolerant, and ACEI and ARBs are recommended as first choice |
7.4. Antihypertensive therapy for very elderly and frail senile patients with hypertension
Very elderly patients are defined as patients more than 80 years old. It is recommended to control BP < 150/90 mm Hg for very elderly patients whom in good health condition, and BP can be reduced to <140/90 mm Hg if tolerant.45 The clinical manifestations are complex, and adverse drug reactions easily occur in very elderly patients because of the presence of other comorbidities and multiple drugs combination. Physicians should pay attention to the impact of the associated disease and strengthen the protection of target organs while lowering blood pressure to the recommended targets, to avoid the excessive lowering of blood pressure. Physicians should be more cautious in the selection of antihypertensive drugs for very elderly patients, starting from small dosage to avoid blood pressure lowering too fast and drastic fluctuations as far as possible, be alert for postural hypotension and postprandial hypotension, and adjusting the dosage or switching other drugs according to the patient's response. It is suggested to make blood pressure reach the target gradually under the condition that patients have good tolerance to the antihypertensive therapy. Physicians should reduce the dosage of antihypertensive drugs and seek possible inducement if dizziness, angina pectoris or other symptoms of insufficient of the cardiovascular and cerebrovascular perfusion occurs during the treatment.
The definition of frailty in elderly patients is not unified, but it generally refers to conditions meeting more than 3 of the following clinical characteristics meanwhile: (i) weight loss ≥5 kg in 1 year with unknown cause; (ii) exhaustion; (iii) weakness: grip strength decreased; (iv) slow walking speed; and (v) decreased physical activity. It is recommended for physicians to evaluate the frail conditions and then to make the treatment protocols for the elderly patients before starting antihypertensive therapy. For the frail elderly, physicians should make antihypertensive treatment protocols according to the result of evaluation. Frail elderly patients, especially those who are institutionalized must be evaluated and treated individually. Some frail elderly may require higher blood pressures for tissues and organ perfusion via stiff arteriosclerotic vessels and should avoid excessive blood pressure and excessive fluctuation of blood pressure46, 47
8. GENERAL MANAGEMENT OF ELDERLY HYPERTENSIVE PATIENTS
Many risk factors for other diseases or cardio‐cerebral‐vascular diseases commonly coexist in elderly patients with hypertension; thus, comprehensive management should be strengthened. The principles of lipid profile, blood glucose management, and antithrombotic therapy in elderly patients with hypertension are similar to those of the general adult population, which can be seen in related guidelines. Attention should be paid to the particularity of elderly patients: (i) Elderly hypertensive patients with dyslipidemia may benefit from statin therapy. In general, small to medium dosage of statin therapy can decrease total cholesterol and LDL cholesterol level to the target in most elderly patients. Besides that, it is suggested to pay attention to the drug interactions and to monitor adverse reactions as the elderly patients often take multiple drugs meanwhile. (ii) Hypoglycemia is more harmful to the elderly; therefore, elderly patients with diabetes mellitus should strengthen blood glucose monitoring when using hypoglycemic drugs and try to avoid hypoglycemic drugs which are prone to hypoglycemia. For patients in good health with long life expectancy and no hypoglycemiahistory, the control target of HbA1c is <7%, and the target of HbA1c can be adjusted to 7.5%‐8% for patients in poor health. (iii) It is recommended for the elderly hypertensive patients with high risk of cardio‐cerebral‐vascular disease to take low‐dose aspirin to reduce the risk of cardio‐cerebral‐vascular events, but aspirin should be used under carefully evaluation when benefits overweigh risks, no presence of high bleeding risk exists, and blood pressure is well controlled (<150/90 mm Hg). The bleeding tendency and adverse effects should be monitored during medication.
9. EPILOGUE
Antihypertensive therapy of elderly hypertensive patients reduces the risk of target organ damage, cardiovascular events, and death. At present, the treatment, control, and target rate of elderly hypertensive patients in China are generally low. We hope that more elderly hypertensive patients could benefit from the antihypertensive treatment through the spread of the Chinese expert consensus on the diagnosis and treatment of hypertension, to improve the prevention and control strategy of cardiovascular and cerebrovascular diseases.
CONFLICTS OF INTEREST
Chinese Expert Consensus on the Diagnosis and Treatment of Hypertension in the Elderly (2017) makes every effort to avoid any actual or potential conflicts of interest that might arise as a result of an outside relationship or personal interest of a member of the writing panel.
TASK FORCE FOR THE CHINESE EXPERT CONSENSUS ON THE DIAGNOSIS AND TREATMENT OF HYPERTENSION IN THE ELDERLY (2017) 1.
1.1.
Da‐Yi Hu (Chairperson).
Mei‐Lin Liu,Yi‐Fang Guo (Author).
ADVISORY BOARD MEMBERS FOR THE CHINESE EXPERT CONSENSUS ON THE DIAGNOSIS AND TREATMENT OF HYPERTENSION IN THE ELDERLY (2017) 1.
1.1.
(In Chinese Pinyin alphabetical order) Qi Bi (Beijing), Hai‐Ping Chen (Beijing), Hong Chen (Beijing), Shu‐Yan Chen (Shanghai), Xiao‐Ping Chen (Sichuan), Ya‐Hong Chen (Beijing), Bei‐Cheng (Sichuan), Yun‐Lin Cheng (Jiangsu), Jing‐Ru Chi (Harbin), Ai‐Min Dang (Beijing), Ning‐Yuan Fang (Shanghai), Ming Feng (Beijing), Jun Fu (Jilin), Yan Fu (Beijing), Zhi‐Fang Fu (Beijing), Lu Gan (Harbin), Xiu‐Rong Gao (Harbin), Hai‐Qing Gao (Shandong), Yan Guo (Jiangsu), Yi‐Fang Guo (Hebei), Ying Guo (Hunan), Zhi‐Gang Guo (Guangdong), Qing He (Beijing), Zhao‐Chu He (Guangdong), Mao‐Lin He (Beijing), Da‐Yi Hu (Beijing), Qi Hua (Beijing), Ruo‐Wen Huang (Shanxi), Meng‐Jue Lei (Jiangxi), Hang Li (Beijing), Hua Li (Henan), Min Li (Beijing), Xiao‐Ying Li (Beijing), Yong Li (Shanghai), Cheng‐Yun Liu (Shanghai), Mei‐Lin Liu (Beijing), Wen‐Juan Liu (Harbin), Lei‐Ming Luo (Beijing), Ji‐Cheng Lv (Beijing), Yong‐Jun Mao (Shandong), Shu‐Hua Mi (Beijing), Da‐Peng Mo (Beijing), Ben‐Ling Qi (Shanghai), Guo‐Xian Qi (Shenyang), Yun‐Yun Qi (Beijing), Ming‐Zhao Qin (Beijing), Pei‐Yan Shan (Shandong), Qian‐Mei Sun (Beijing), Yong‐An Sun (Beijing), Hai‐Qin Sun (Anhui), Xin‐Hua Tang (Zhejiang), Gui‐Zhou Tao (Liaoning), Jun Tao (Guangdong), Tao Tian (Shandong), Jian‐Li Tian (Tianjin), Feng‐Ling Wang (Heilongjiang), Jian‐Chang Wang (Beijing), Ji‐Guang Wang (Shanghai), Jie Wang (Beijing), Li‐Na Wang (Heilongjiang), Wei Wang (Beijing), Xiao‐Ming Wang (Shanxi).
Liu M, Committee of cardio‐cerebro‐vascular Disease of China Association of Gerontology and Geriatrics, Chinese College of Cardiovascular Physician of Chinese Medical Doctor Association . Chinese expert consensus on the diagnosis and treatment of hypertension in the elderly (2017). Aging Med. 2018;1:106‐116. 10.1002/agm2.12020
Translation: Xiting Wang, Qin Zheng,Tianxu Fu, Meilin Liu
REFERENCES
- 1. Ministry of Civil Affairs of the People's Republic of China , The social service development statistical bulletin 2015. http://www.mca.gov.cn/article/sj/tjgb/201607/20160700001136.shtml. Accessed July 11, 2016.
- 2. Rahimi K, Emdin CA, MacMahon S. The epidemiology of blood pressure and its worldwide management. Circ Res. 2015;116:925‐936. [DOI] [PubMed] [Google Scholar]
- 3. 2010 Chinese guidelines for the management of hypertension Writing Group . 2010 Chinese guidelines for the management of hypertension. Chin J Cardiol. 2011;39:579‐616. [PubMed] [Google Scholar]
- 4. Chinese Expert Consensus on the Diagnosis and Treatment of Hypertension in the Elderly (2008). Chin J Intern Med. 2008;47:1046‐1050. [Google Scholar]
- 5. Chinese Expert Consensus on the Diagnosis and Treatment of Hypertension in the Elderly (2011). Chin J Intern Med. 2012;51:76‐82. [Google Scholar]
- 6. Mancia G, Fagard R, Narkiewicz K, et al. ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the management of Arterial Hypertension of the European Society of Hypertension(ESH) and of the European Society of Cardiology(ESC). Eur Heart J. 2013;34:2159‐2219. [DOI] [PubMed] [Google Scholar]
- 7. James PA, Oparil S, Carter BL, et al. Evidence‐based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee(JNC 8). JAMA. 2014;311:507‐520. [DOI] [PubMed] [Google Scholar]
- 8. Shimamoto K, Ando K, Fujita T, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res. 2014;37:253‐390. [DOI] [PubMed] [Google Scholar]
- 9. Chiang CE, Wang TD, Ueng KC, et al. 2015 guidelines of the Taiwan Society of Cardiology and the Taiwan Hypertension Society for the management of hypertension. J Chin Med Assoc. 2015;78:147. [DOI] [PubMed] [Google Scholar]
- 10. Leung AA, Daskalopoulou SS, Dasgupta K, et al. Hypertension Canada's 2017 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults. Can J Cardiol. 2017;33:557‐576. [DOI] [PubMed] [Google Scholar]
- 11. Qaseem A, Wilt TJ, Rich R, et al. Pharmacologic treatment of hypertension in adults aged 60 years or order to higher versus lower blood pressure targets: a clinical practice guideline from the American college of physicians and the American academy of family physicians. Ann Intern Med. 2017;166:430‐437. [DOI] [PubMed] [Google Scholar]
- 12. Myers MG, Kaczorowski J, Paterson JM, et al. Thresholds for diagnosing hypertension based on automated office blood pressure measurements and cardiovascular risk. Hypertension. 2015;66:489‐495. [DOI] [PubMed] [Google Scholar]
- 13. Wang LD. Report on nutrition and health status of Chinese residents: 2002 comprehensive report. Beijing:People's Medical Publishing House. 2005;53‐57.
- 14. National Health and Family Planning Commission Disease Prevention and Control Bureau . Report on nutrition and chronic diseases of Chinese residents (2015). . Beijing: People's Medical Publishing House. 2015;33‐50.
- 15. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics . Health, United States, 2015; with special feature on racial and ethnic health disparities. Washington DC: Government Printing Office, 2016;203. [PubMed]
- 16. Liu J, Wang W, Liu J, et al. Clustering of cardiovascular risk factors and hypertension control status among hypertensive patients in the outpatient setting. Chin J Cardiol. 2013;41:1050‐1054. [PubMed] [Google Scholar]
- 17. Forouzanfar MH, Alexander L, Anderson HR, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990‐2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:2287‐2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Feigin VL, Roth GA, Naghavi M, et al. Global burden of stroke and risk factors in 188 countries, during 1990‐2013: a systematic analysis for the global burden of disease study 2013. Lancet Neurol. 2016;15:913‐924. [DOI] [PubMed] [Google Scholar]
- 19. Nwankwo T, Yoon SS, Burt V, et al. Hypertension among adults in the United States: national health and nutrition examination survey, 2011‐2012. NCHS Data Brief. 2013;1‐8. [PubMed] [Google Scholar]
- 20. Du JL, Liu ML. The pathophysiological characteristics of hypertension in the elderly. Chin J Mult Organ Dis in the Elder. 2011;10:196‐199. [Google Scholar]
- 21. Geriatrics Medicine Branch of the Chinese Medical Association, Hypertension Proffessional Committee of Chinese Medical Doctor Association . The recommendation of characteristics and management diagram in elderly hypertension. Chin J Geriatr. 2014;33:689‐701. [Google Scholar]
- 22. Franklin SS, Larson MG, Khan SA, et al. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham heart study. Circulation. 2001;103:1245‐1249. [DOI] [PubMed] [Google Scholar]
- 23. Wang JG, Staessen JA, Gong L, et al. Chinese trial on isolated systolic hypertension in the elderly. Systolic Hypertension in China (Syst‐China) Collaborative Croup. Arc Intern Med. 2000;160:211‐220. [DOI] [PubMed] [Google Scholar]
- 24. Staessen JA, Fagard R, Thijs L, et al. Randomised double‐blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The systolic hypertension in Europe (Syst‐Eur) trial investigators. Lancet. 1997;350:757‐764. [DOI] [PubMed] [Google Scholar]
- 25. Staessen J. Mortality and treated blood pressure in patients of the European Working Party on high blood pressure in the elderly. Am J Med. 1991;90:60S‐61S. [DOI] [PubMed] [Google Scholar]
- 26. Lewington S, Clarke R, Qizilbash N, et al. Age‐specific relevance of usual blood pressure to vascular mortality: a metaanalysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903‐1913. [DOI] [PubMed] [Google Scholar]
- 27. Van Orshoven NP, Jansen PA, Oudejans I, et al. Postprandial hypotension in clinical geriatric patients and healthy elderly: prevalence related to patient selection and diagnostic criteria. J Aging Res. 2010;2010:243752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kario K, Shimada K. Risers and extreme‐dippers of nocturnal blood pressure in hypertension: antihypertensive strategy for nocturnal blood pressure. Clin Exp Hypertens. 2004;26:177‐189. [DOI] [PubMed] [Google Scholar]
- 29. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the systolic hypertension in the elderly program (SHEP). SHEP Cooperative Research Group. JAMA.1991;265:3255‐3264. [PubMed] [Google Scholar]
- 30. Dahlöf B, Lindholm LH, Hansson L, et al. Morbidity and mortality in the Swedish trial in old patients with hypertension (STOP‐Hypertension). Lancet. 1991;338:1281‐1285. [DOI] [PubMed] [Google Scholar]
- 31. Degl'Innocenti A, Elmfeldt D, Hansson L, et al. Cognitive function and health‐related quality of life in elderly patients with hypertension‐baseline data from the study on cognition and prognosis in the elderly (SCOPE). Blood Press. 2002;11:157‐165. [DOI] [PubMed] [Google Scholar]
- 32. Liu LS, Zhang WZ, Hao JS, et al. Slow releasing Felodipine in blood pressure lowering treatment: rate of reaching target blood pressure and safety. Chin J Cardiol. 2004;32:291‐294. [Google Scholar]
- 33. Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887‐1898. [DOI] [PubMed] [Google Scholar]
- 34. Liu L, Zhang Y, Liu G, et al. The felodipine event reduction (FEVER) study: a randomized long‐term placebo‐controlled trial in Chinese hypertensive patients. J Hypertens. 2005;23:2157‐2172. [DOI] [PubMed] [Google Scholar]
- 35. Zhang Y, Zhang X, Liu L, et al. Is a systolic blood pressure target<140 mmHg indicated in all hypertensives? Subgroup analyses of findings from the randomized FEVER trial. Eur Heart J. 2011;32:1500‐1508. [DOI] [PubMed] [Google Scholar]
- 36. Rakugi H, Ogihara T, Goto Y, et al. Comparison of strict and mild blood pressure control in elderly hypertensive patients: a per‐protocol analysis of JATOS. Hypertens Res. 2010;33:1124‐1128. [DOI] [PubMed] [Google Scholar]
- 37. Ogihara T, Saruta T, Rakugi H, et al. Target blood pressure for treatment of isolated systolic hypertension in the elderly:valsartan in elderly isolated systolic hypertension study. Hypertension. 2010;56:196‐202. [DOI] [PubMed] [Google Scholar]
- 38. Denardo SJ, Gong Y, Nichols WW, et al. Blood pressure and outcomes in very old hypertensive coronary artery disease patients: an INVEST substudy. Am J Med. 2010;123:719‐726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wright JT, Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood‐pressure control. N Engl J Med. 2015;373:2103‐2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Williamson JD, Supiano MA, Applegate WB, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≧ 75 years: a randomized clinical trial. JAMA. 2016;315:2673‐2682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lonn EM, Bosch J, Lopez‐Jaramillo P, et al. Blood‐pressure lowering in intermediate‐risk persons without cardiovascular disease. N Engl J Med. 2016;374:2009‐2020. [DOI] [PubMed] [Google Scholar]
- 42. Vidal‐Petiot E, Ford I, Greenlaw N, et al. Cardiovascular event rates and mortality according to achieved systolic and diastolic blood pressure in patients with stable coronary artery disease: an international cohort study. Lancet. 2016;388:2142‐2152. [DOI] [PubMed] [Google Scholar]
- 43. Chinese Society of Nutrition . Dietary guidelines for Chinese residents (2016). Beijing: People's Medical Publishing House. 2016.
- 44. Aronow WS, Fleg JL, Pepine CJ, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus documents developed in collaboration with the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension. J Am Coll Cardiol. 2011;57:2037‐2114. [DOI] [PubMed] [Google Scholar]
- 45. Hypertension Branch of Chinese Geriatric Medical Association . China experts consensus on the management of hypertension in the very old people. Chin J Cardiovasc Med. 2015;6:401‐409. [Google Scholar]
- 46. Materson BJ, Garcia‐Estrada M, Preston RA. Hypertension in the frail elderly. J Am Soc Hypertens. 2016;10:536‐541. [DOI] [PubMed] [Google Scholar]
- 47. Benetos A, Bulpitt CJ, Petrovic M, et al. An expert opinion from the European Society of Hypertension‐European Union Geriatric Medicine Society Working Group on the management of hypertension in very oldfrail subjects. Hypertension. 2016;67:820‐825. [DOI] [PubMed] [Google Scholar]


