Abstract
Background:
Building on several decades of innovative HIV prevention and treatment programming in San Francisco, in 2014, a small group of academic, civic, and community leaders launched Getting to Zero San Francisco (GTZ-SF), a city-wide consortium focused on getting to zero HIV infections, zero HIV-related deaths, and zero HIV stigma and discrimination.
Setting:
San Francisco city and county
Methods:
The consortium operates under the principles of collective impact, comprised of five components: a common agenda, shared measurement, mutually reinforcing activities, continuous communication, and organization backbone. Two flagship initiatives are described: citywide scale-up of pre-exposure prophylaxis and rapid antiretroviral therapy upon diagnosis.
Results:
The number of new HIV diagnosis declined by over 50% from 399 to 197 from 2013 to 2018; the time from diagnosis to viral suppression decreased from 134 to 62 days during that time period. However, continued racial/ethnic disparities in new HIV diagnoses and viral suppression rates point to the need for the GTZ-SF committees to focus on racial/ethnic equity as a primary focus. Cis- and transgender women, people who inject drugs, and people who are homeless also have lower viral suppression rates; and ongoing initiatives are attempting to address these disparities.
Conclusion:
A collective impact implementation strategy that operates by unifying municipal organizations towards a common goal was associated with citywide gains in reducing new HIV diagnosis and time to viral suppression in San Francisco. Formal evaluation of this strategy will help elucidate under which conditions this approach is most likely to succeed.
Keywords: Getting to Zero, San Francisco, collective impact, fast track cities, 90-90-90
San Francisco, a hub of the HIV epidemic in the United States, is home to 12% of all persons living with HIV in California, but accounts for only 2.2 % of the state’s population. From the beginning of the HIV epidemic, the city of San Francisco was a “first responder” and has pursued a series of innovative programs and policies to address an array of ever-evolving challenges. HIV testing services were massively expanded starting in 2010, beginning with scale-up in clinical settings and moving to community- based and mobile services that were much more accessible than health facilities for testing and re-testing for at-risk populations. In 2010, prior to US national HIV treatment guideline changes, San Francisco was the first jurisdiction to offer antiretroviral treatment to all persons living with HIV, not restricting eligibility by CD4 cell count. In 2012, shortly after the US Food and Drug Administration approved use of Truvada® for pre-exposure prophylaxis (PrEP), San Francisco launched the first demonstration project for PrEP1, paving the way for future expansion.
In 2013, on the heels of the UNAIDS “Getting to Zero” campaign—calling for zero new infections, zero deaths and zero stigma-- a small group of academic and community leaders, persons living with HIV and local politicians sponsored a Town Hall “San Francisco Getting to Zero- Where are We?” at the San Francisco LGBT Community Center. Declines in new HIV infections and deaths from the previous year appeared to have stalled—despite the increase in HIV testing, FDA approval of PrEP and universal eligibility for antiretroviral therapy. What became clear at this Town Hall meeting was that programs in prevention and treatment were moving forward in a fragmented, rather than a coordinated fashion, enabled by compartmentalized funding streams. Meeting attendees recognized and were in agreement that much more could be gained with the interventions and resources at hand if we coordinated efforts under a broader organizational structure.
Thus, in 2014, following the Town Hall, we established a new free-standing entity—Getting to Zero San Francisco (GTZ-SF)—a multi-sector consortium that operates under the principles of collective impact. GTZ-SF importantly was not a “competitor” to the many existing community-based organizations nor an entity directly under the San Francisco Department of the Public Health (SFDPH). Rather, our organization was an independent body that sought and leveraged the expertise of the community in the broadest sense, and collectively advocated and advised for resources from the public and private sector to support programming to meet its goals. “Successes” of GTZ-SF were those of the city as a whole; the Mayor as the highest city official was critical to the mission. As cities and local municipalities consider how to respond to new national targets for HIV epidemic control, and as researchers evaluate results of these approaches, San Francisco is one of several models in the United States that has made measurable gains.2 Here we describe the GTZ-SF collective impact implementation strategy and two flagship initiatives within a health equity framework. We discuss an analytic approach to understand the relationship between the organization and outcomes and comment on the generalizability of this approach for other communities or regions.
Collective Impact
Collective impact is an implementation strategy used in health and other sectors that brings together organizations to align their efforts towards a common goal—that typically alone, each organization would be unable to reach3,4. GTZ-SF’s approach was built on the five core principles of collective impact (Table 1). The first and critical component for collective impact is the common agenda. A tri-part mission to reduce new HIV infections, deaths and stigma was unanimously adopted by the core members. Our steering group developed, vetted and distributed a strategic plan community-wide to work towards these goals with three initial flagship projects, to expand 1) PrEP, 2) RAPID (treatment upon HIV diagnosis), and 3) Retention and reengagement in care.
Table 1.
Components of Collective Impact
| Component | Implementation |
|---|---|
| Common Agenda | Getting to Zero SF has a strategic plan to reduce HIV infections, death and stigma in San Francisco endorsed by broad base of constituents. Accountability to the targets are reviewed annually. |
| Shared Measurement | San Francisco Department of Public Health collects and reports annual metrics on HIV infections, death and other outcomes of interest such as antiretroviral therapy start and viral suppression |
| Mutually Reinforcing Activities | San Francisco organizations act and contribute at policy, program and community level guided by the strategy and GTZ-SF committees such as PrEP, RAPID, and housing |
| Continuous Communication | GTZ-SF holds thrice yearly consortium, hosts active web site, sends updates to members and conducts ongoing reporting to Mayors Office, Director of Department of Public Health, City Health Commission |
| Organization Backbone | GTZ-SF has Steering committee (multi-sector volunteers), meets monthly and administrative staff (1 full time, 1 part time position) that support and coordinate activities and events inclusive of the committees. |
Shared measurement, the second component of the collective impact framework, was necessary if the GTZ-SF consortium was to set and evaluate implementation targets. The key outcomes of annual new HIV diagnosis and deaths were already captured in the San Francisco HIV Epidemiology Annual Report; thus, the consortium did not need to set up a new measurement system. Having this information was invaluable to steer interventions and investments toward persons at greatest risk for new HIV infection or those living with HIV who had fallen out of care. Process measures for the three flagship projects, however, were not explicitly included in the annual report. Thus, GTZ-SF worked closely with San Francisco HIV Surveillance Section to incorporate new metrics for PrEP and to track the time from diagnosis to antiretroviral start. The role of the consortium was to collaborate and advocate for resources for the Surveillance Section to adapt these metrics, which are now included in the Annual Report.5
The third core component of a collective impact-structured organization is to catalyze mutually reinforcing activities towards the common goal. Much of this work is done through the committees, starting with the PrEP, Rapid, and Re-engagement in Care Committees. Each of these groups has broad membership from multiple community-based organizations as well as SFDPH, which funds many initiatives. A fourth group, a Housing Task Force, was created by GTZ-SF to address the remarkably low viral suppression rates among people with housing instability. Activities included 1) a consortium meeting where city leaders, housing advocacy organizations, and affected community members discussed short- and long-term solutions for housing for the HIV community; 2) organizations and members organized sign-on to San Francisco ballot initiatives to expand supportive housing; 3) GTZ-SF developed its own housing policy statement, and participated in Mayoral Housing Task Force meetings; 4) one community-based organization (the San Francisco AIDS Foundation) launched a formal HIV and housing needs assessment; 5) the “front line providers” group organized a new communication strategy for rapidly evolving housing allocation policies; and 6) the public HIV clinic at San Francisco General Hospital launched a new program to improve care for unstably housed persons. Each of these activities are examples of GTZ-SF member organizations aligning efforts in response the consortium’s call to action for the extraordinarily complex challenge of inadequate housing.
The fourth component of collective impact relies on strategic and ongoing communication. GTZ-SF has consortium-wide meetings thrice yearly. At these meetings, the consortium is provided with policy updates, progress on key initiatives and a discussion of a key topic with a community-focused panel. GTZ-SF has a website that includes committee meeting summaries, protocols for the PrEP and RAPID programs, materials developed by each of the GTZ-SF committees, and a list serve where members can share updates of interest (e.g. policy or funding from the state or national level, articles of interest). Social media is used to disseminate updates on policy, meetings and events. Each year, the San Francisco Health Commission receives an update on progress of GTZ-SF, and the steering committee communicates regularly with the Mayor’s Office, Supervisors, and Director of Public Health.
The administrative backbone of GTZ-SF, the fifth component of collective impact, is very streamlined, consisting of 1.2 full-time dedicated staff and a small budget for food at the consortium events and committee meetings. The bulk of the planning, reports and work of the committees is donated time by its more than 250 member cadre of volunteer providers, community members, public and private sector organizations and political leaders. A Steering Committee, directed by 2 co-chairs and comprised of representatives of the SFDPH, University, providers, leads of community-based organizations, and community members of diverse backgrounds, set the strategic vision for the consortium. They guide the committee work, identify policy issues that need to be addressed, communicate with high level City officials and mobilize funding to support initiatives of the committees.
Mutually Reinforcing activities
PrEP
At the launch of Getting to Zero San Francisco, PrEP scale-up was just beginning, with a demonstration project conducted at the municipal sexually transmitted disease clinic (San Francisco City Clinic – SFCC), and a nascent program at Kaiser Permanente, the largest Health Maintenance Organization in the city. Most clinicians in the community were reluctant to prescribe PrEP, because of concerns of risk compensation and for fear that they would be inundated with patients seeking PrEP. When the PrEP committee launched in 2014, they recognized the need to increase both PrEP supply and demand, as well as to track PrEP uptake. The committee established 3 subcommittees, each tackling their unique need.
The subcommittee focused on increasing PrEP supply, began working with many providers and organizations to launch PrEP initiatives over the next several years. PrEP protocols were developed, disseminated at SFDPH clinics, and posted on the GTZ-SF website. GTZ-SF advocated to the SFDPH to fund a nurse practitioner and part-time physician to develop materials and conduct PrEP academic detailing with providers throughout the city. A member of the PrEP committee launched pleaseprepme.org, an online tool to list providers willing to provide PrEP, so that potential PrEP users could identify a potential PrEP care provider; this project was later expanded nationally. PrEP-dedicated clinics were launched or expanded: at SFCC (after the demonstration project had ended), at Magnet (a men’s sexual health clinic run by one of the largest HIV-related community-based organizations in San Francisco), as well as at the HIV clinic based at the public health hospital (Ward 86). PrEP navigators were hired using city general fund and federal dollars, and placed at community-based organizations and the SFDPH clinics thought to have the greatest potential to provide PrEP to their patient population. Navigators across the city and in other jurisdictions were trained through PrEP “boot camps” to ensure the most up-to-date and comprehensive information was available about PrEP-related resources. A PrEP providers group was formed that met monthly to brainstorm strategies to provide PrEP to populations with lower PrEP uptake, including trans- and cis-gender women and people who inject drugs (PWID). A fund was established to purchase Truvada® for youth under 18 years, as they were not eligible for Gilead’s Patient Assistance Program and were often uncomfortable or unable to use their parents’ insurance; additional funding was provided for transportation of youth to PrEP clinics. A GTZ-SF member, in collaboration with SFCC, launched a novel community-based pharmacy-delivered PrEP model in the city’s Mission district,6 a neighborhood traditionally serving a large Latinx population.
The subcommittee focused on increasing PrEP demand was tasked with increasing outreach to communities in need of PrEP. Several social media campaigns were launched. The first campaign focused on the joyfulness of PrEP; a follow-up campaign used African American and transgender community members who discussed how PrEP supports their creativity, intelligence, and other positive attributes. Online and radio advertising encouraged people with PrEP questions to get in touch with a centralized PrEP navigator, who was able to provide education and linkage to services. The San Francisco SFDPH issued 4 requests for proposals, and in turn, funded 4 community-based organizations to increase interest in 4 communities that the data demonstrated were under-served by PrEP: African Americans, Latinx, youth, and transgender women. (The group funded to increase PrEP awareness in the Latinx community won an award from POZ magazine for the best HIV prevention media campaign of 20187). A PrEP demonstration project was launched for transgender women in which gender-affirming care was integrated with PrEP care. SFDPH staff integrated PrEP counseling into partner notification services for partners of persons with newly diagnosed HIV or syphilis; a “data to PrEP” program also provided PrEP outreach to persons with newly acquired syphilis or rectal gonorrhea or chlamydia. A PrEP ambassadors program was launched, in which PrEP users were trained to go out speak with other community members at street fairs and other events about their experiences using PrEP.
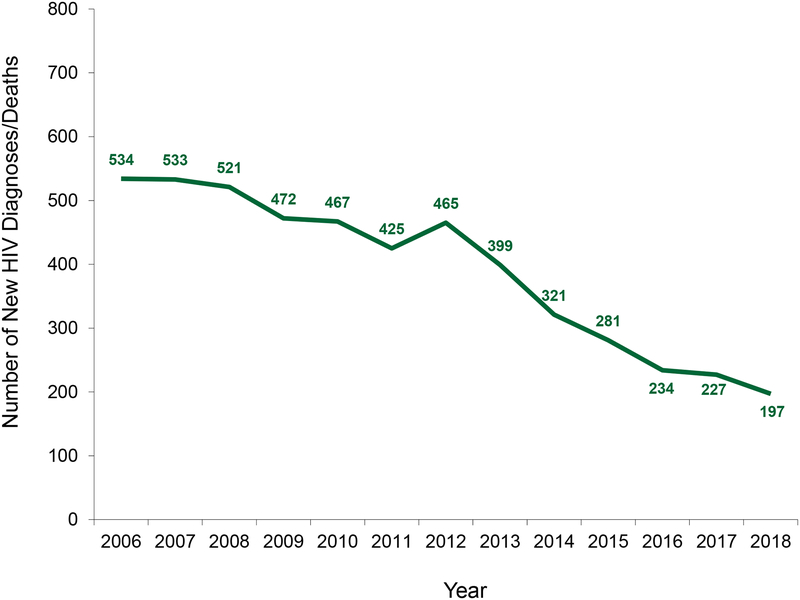
The third subcommittee launched several initiatives to measure PrEP uptake in the community. SFDPH began tracking PrEP provided by each of the community-based organizations they funded, using a centralized scorecard that identified the number of PrEP starts, by age and race/ethnicity. Kaiser analyzed data from their own program,8 as has Magnet and SFCC. A quarterly mobile survey was advertised online and recruited approximately 900 MSM and transgender women in San Francisco to measure all stages in the PrEP cascade.9 To develop an overall estimate of PrEP uptake among MSM in San Francisco, data were used from 2 population-based surveys: the National HIV Behavioral Surveillance system10 and the STOP AIDS Project survey. These two surveys provided estimates of the proportion of HIV negative MSM or those with unknown serostatus who reported using PrEP from 2014 to 2017. These proportions were multiplied by the estimated size of the HIV negative population in San Francisco11 to estimate the total number of MSM on PrEP during those years. We estimate that the overall number of MSM using PrEP increased from approximately 4400 in 2014 to between 16,300 and 20,000 in 2017. This coincides with a 58% decline in new HIV diagnoses from the year PrEP was first rolled out, in 2012, to 2018 (Figure 1).
Figure 1.
Number of new HIV diagnoses in San Francisco from 2006 (the first year of HIV case reporting) through 2018.5
RAPID
GTZ-SF’s RAPID committee, comprised of providers from public and private sectors and the SFDPH, took a number of specific steps to support the city-wide expansion of San Francisco General Hospital pilot RAPID program, offering HIV treatment upon diagnosis. Three major levels of change were required to expand and disseminate the RAPID approach to ART start. First, health systems needed to develop protocols to provide flexible scheduling to see newly diagnosed patients, including insurance enrollment for persons not previously in a health system. Second, providers needed to be comfortable with and have access to offering treatment on diagnosis and be assured that follow-up counseling, laboratory assessments and adherence support could be provided in this framework. Third, patients needed to understand the rationale for rapid ART start and their autonomy in decision-making. National guidelines for rapid ART start have only recently changed, thus these efforts preceded guideline changes by approximately 5 years.12
The RAPID committee started by developing a city-wide protocol. This protocol was built on the San Francisco General Hospital program,13 with the intent for individual clinical programs to adapt this protocol for their specific setting. Next, GTZ-SF successfully obtained 1-year funding through the SFDPH for a part-time physician and a full-time program staff to do academic detailing on the rationale and logistics of RAPID implementation to health systems and clinics around the city. Of note, all detailing materials and protocols are posted and updated by the RAPID committee on the GTZ -SF website to provide local, national and global access. The RAPID team also worked to connect testing sites to clinics that had the capacity for RAPID ART starts. After this surge activity, the RAPID committee began hosting a monthly case-centered meeting where providers and program representatives across the city discussed successes and challenges of RAPID programming. This was later expanded to include discussion of PrEP successes and challenges. Finally, the committee worked with the SFDPH surveillance team to augment metrics to measure the performance of RAPID with the targeted program expansion. From 2013 to 2016, health providers and systems under the GTZ-SF consortium started implementing a RAPID approach to ART start. Consumer demand for rapid ART increased. The median time from new HIV care to ART start decreased by over 90% from 27 to 0 days; the time from HIV diagnosis to viral suppression decreased by over 50% from 134 to 62 days (Table 2). These metrics and those from San Francisco General Hospital showing 95.8% of participants in the RAPID program had ever achieved viral suppression by 1 year14 were reported at the consortium meetings, providing accountability and reinforcement.
Table 2.
Median number of days from HIV Diagnosis to Care Indicators
| Indicator | 2013 (median days) | 2017 (median days) |
|---|---|---|
| First medical care to ART* start | 27 | 0 |
| ART start to first viral suppression | 71 | 46 |
| HIV diagnosis to first medical care | 8 | 4 |
| HIV diagnosis to first viral suppression | 134 | 62 |
ART: antiretroviral therapy
Outcomes viewed through a health equity lens
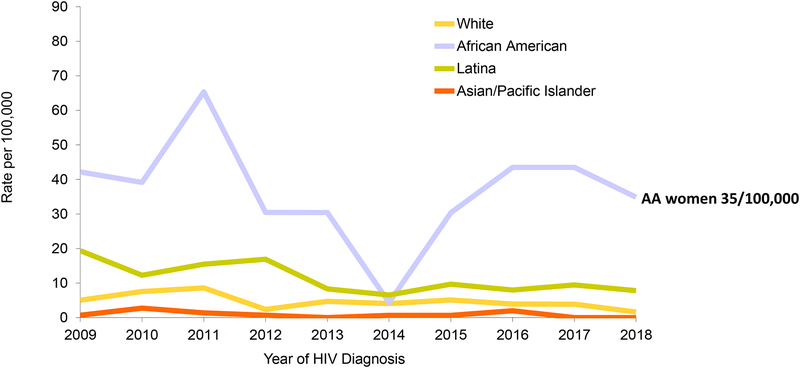
Overall, since 2012, the number of new HIV diagnosis in San Francisco has declined by 58%; this compares with a national decline of only 7% over that time period. One of the key components of a successful collective impact approach is equity and inclusion. The GTZ-SF consortium had access to disaggregated data – one way to assess its progress through this lens. Our analyses showed striking health disparities across many metrics, including HIV diagnosis rates by race/ethnicity (Figure 2). From 2006 to 2018, the annual rate of HIV diagnoses per 100,000 population declined among all racial/ethnic groups, but disparities remain, with infection rates highest in African American men and women and Latino men (Figure 2). In fact, despite women accounting for only 12% of new HIV diagnoses in 2017, rates in African American women exceeded those in White men. Rates of viral suppression were also lower among cis- and transgender women than cis-gender men, African American and Latinx persons than White and Asian persons, persons under 50 years than older persons; and people who inject drugs than among men who have sex with men who did not inject drugs (Table 3). Viral suppression rates were lowest among people who were homeless.15,16
Figure 2.
Annual new HIV diagnosis rates per 100,000 a) men and b) women from 2009 through 2018, San Francisco.5 AA: African American. API: Asian/Pacific Islander
Table 3.
Demographic characteristics of people living with HIV in San Francisco
| Demographic | Number of living cases | % virally suppressed (<200 copies/mL) |
|---|---|---|
| Overall | 12,778 | 74% |
| Gender | ||
| Cisgender men | 11,688 | 74% |
| Cisgender women | 725 | 66% |
| Transgender women | 360 | 68% |
| Race/Ethnicity | ||
| White | 7,095 | 76% |
| African American | 1,606 | 68% |
| Latinx | 2,742 | 70% |
| Asian/Pacific Islander | 815 | 77% |
| Other/Unknown | 520 | 74% |
| Age | ||
| 13–24 | 83 | 80% |
| 25–29 | 382 | 69% |
| 30–39 | 1,175 | 67% |
| 40–49 | 2,804 | 67% |
| 50–59 | 4,542 | 75% |
| 60–69 | 2,548 | 81% |
| 70+ | 704 | 83% |
| Transmission category | ||
| MSM* | 9,263 | 76% |
| TWSM# | 207 | 71% |
| PWID& | 745 | 65% |
| MSM-PWID | 1,719 | 68% |
| TWSM-PWID | 151 | 64% |
| Heterosexual | 470 | 70% |
| Other/Unidentified | 223 | 51% |
| Housing status, most recent | ||
| Housed | 12,447 | 75% |
| Homeless | 331 | 33% |
| Country of birth | ||
| US | 9,321 | 75% |
| Non-US | 2,201 | 69% |
| Unknown | 1,256 | 76% |
MSM: men who have sex with men
TWSM: transgender women who have sex with men
PWID: people who inject drugs
With this information, our steering committee charged each of the committees to address these disparities in the work they do, with a particular focus on racial/ethnic disparities, which underlie most of the other disparities. To address disparities in HIV diagnoses, initiatives have been launched to increase PrEP uptake particularly among African Americans, Latinx, transgender women, and youth, as described previously. The RAPID program has the potential to undo racial/ethnic disparities in the speed with which people achieve viral suppression, as all newly diagnosed persons have access to this program. Two GTZ-SF consortium meetings have focused on issues facing African Americans and Latinx at risk for and living with HIV;17,18 other consortium meetings have focused on cis- and transgender women,19,20 people who are homeless,21 people who use drugs,22 and youth.23 The GTZ-SF steering committee and other committee leadership is undertaking racial equity training. We are developing African American and Latinx community groups to make develop innovative racial equity programs to address these disparities in HIV infection rates and HIV outcomes. We have much work to do, and are trying to innovate within each of the committees to address these disparities.
Collective Impact Evaluation
Methods to evaluate the effect of collective impact are in the early stages of development.24–26 “Process tracing” is one proposed approach described by Stachowiak and Gase.27 The central hypothesis is that the initiatives developed and implemented under a collective impact approach can explain the resulting outcomes. In order to test this hypothesis, one needs to assess the degree to which initiatives are associated with desired outcomes and the degree to which the activities undertaken under collective impact uniquely explain the result. Process tracing requires gathering data from stakeholders; it starts by creating and refining a model, testing hypothesis and assessing the strength and relationship between collective impact activities and outcomes.
Using process evaluation to assess the effect of collective impact on 25 initiatives ranging from health to the environment, Stachowiak and Gase found that of the 5 components of collective impact, having backbone support and a common agenda were most frequently prioritized among collective impact initiatives that achieved change in their target populations.28 Without these, it is difficult to foster mutually reinforcing activities, or maintain the continuous communication required to be successful. Some other key findings from their work are a) collective impact contributes to desired changes in outcomes, but that the degree to which they contributed in this analysis varied across projects; b) the quality of the implementation matters, with more complete implementation of the 5 components resulting in greater impact; c) change takes time, with the time between inception and impact ranging from 4 to 24 years across projects; d) achieving equity requires deliberate effort and actions;29 and e) much more research and data are needed to define, refine and compare this to other approaches.
Although we do see an ecologic association between the start of GTZ-SF and our priority outcomes, we have not yet applied process tracing to formally assess the impact of GTZ-SF. We are, however, well positioned to do so with our collective impact structure, programming and objective outcomes. This would indeed be important to do for own group, the field of collective impact and to address and legitimate criticisms waged against the collective impact approach.30,31
Implications
A combination of new approaches will be needed for the United States to end HIV as an epidemic by 2030.32,33 GTZ-SF’s collective impact implementation strategy may provide a model for other municipalities, and contribute to the larger global “Fast-track cities” effort.34 Our progress was clearly facilitated by having an integrated City and County (with a single, strong health department) and extensive HIV surveillance system. Geopolitical boundaries with different levels of political engagement, funding streams and health system reporting can pose huge barriers for collaboration. San Francisco also has a highly effective and collaborative network of community-based organizations, academic advocates, political support for HIV services, and a large and politically active base of persons affected by HIV—which may not be present in other jurisdictions. On the other hand, high housing costs, mobile populations, and high rates of methamphetamine use35,36 as well as inadequate mental health programs37 pose a huge and complex barriers for persons with or at risk for HIV that may not be present in other cities.38 The genesis of GTZ-SF was the recognition that unified efforts under a common goal could accelerate HIV epidemic control better than a fragmented approach. We conclude that GTZ-SF’s collective impact implementation strategy is addressing this gap and could be an asset to other municipalities or geographic units. Much more research needs to be done on methods to understand the effect of collective impact and under which conditions it is most likely to succeed.
Acknowledgments:
SF-GTZ co-founders and supporters Jeff Sheehy, Neil Giuliano, Scott Wiener, Barbara Garcia, Shannon Weber, Diane Jones, the late San Francisco Mayor Ed Lee; the SF-GTZ steering committee, volunteer working committees and members; Courtney Liebi, Mary-Lawrence Hicks, San Francisco Mayor London Breed, and Department of Health Director Grant Colfax.
Footnotes
Conflicts of interest: SB and DH have been investigators on studies for which Gilead Sciences has donated study drug.
References
- 1.Liu A, Cohen S, Vittinghoff E, et al. Preexposure Prophylaxis for HIV Infection Integrated with Municipal- and Community-Based Sexual Health Services. JAMA Intern Med. 2015;176:In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scheer S, Hsu L, Schwarcz S, et al. Trends in the San Francisco Human Immunodeficiency Virus Epidemic in the “Getting to Zero” Era. Clin Infect Dis. 2018;66(7):1027–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kania JKM. Collective Impact. Stanford Social Innovation Review. (Winter 2011):38–41. [Google Scholar]
- 4. https://ssir.org/articles/entry/collective_impact.
- 5.SFDPH. HIV Epidemiology Annual Report. 2018.
- 6.Lopez MI, Cocohoba J, Cohen SE, Trainor N, Levy MM, Dong BJ. Implementation of pre-exposure prophylaxis at a community pharmacy through a collaborative practice agreement with San Francisco Department of Public Health. J Am Pharm Assoc (2003). 2019. [DOI] [PubMed] [Google Scholar]
- 7. https://www.poz.com/article/poz-awards-2018-media-prevention.
- 8.Marcus JL, Hurley LB, Hare CB, Silverberg MJ, Volk JE. Disparities in Uptake of HIV Preexposure Prophylaxis in a Large Integrated Health Care System. Am J Public Health. 2016;106(10):e2–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu A C K, Walker N, Vittinghoff E, Turner C, Vinson J, Quinonez C, Gardner E, Raymand HF, Buchbinder S, Lightfoot M, Scheer S, Arayasirikul S, Wilson EC. Assessing the PrEP Continuum in the San Francisco Bay Area: The Quickie Mobile Survey. Conference on Retroviruses and Opportunistic Infections 2019;#973. [Google Scholar]
- 10.Finlayson T, Cha S, Xia M, et al. Changes in HIV Preexposure Prophylaxis Awareness and Use Among Men Who Have Sex with Men - 20 Urban Areas, 2014 and 2017. MMWR Morb Mortal Wkly Rep. 2019;68(27):597–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hughes AJ, Chen YH, Scheer S, Raymond HF. A Novel Modeling Approach for Estimating Patterns of Migration into and out of San Francisco by HIV Status and Race among Men Who Have Sex with Men. J Urban Health. 2017;94(3):350–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saag MS, Benson CA, Gandhi RT, et al. Antiretroviral Drugs for Treatment and Prevention of HIV Infection in Adults: 2018 Recommendations of the International Antiviral Society-USA Panel. JAMA. 2018;320(4):379–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pilcher CD, Ospina-Norvell C, Dasgupta A, et al. The Effect of Same-Day Observed Initiation of Antiretroviral Therapy on HIV Viral Load and Treatment Outcomes in a US Public Health Setting. J Acquir Immune Defic Syndr. 2017;74(1):44–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coffey S, Bacchetti P, Sachdev D, et al. RAPID antiretroviral therapy: high virologic suppression rates with immediate antiretroviral therapy initiation in a vulnerable urban clinic population. AIDS. 2019;33(5):825–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clemenzi-Allen A, Geng E, Christopoulos K, et al. Degree of Housing Instability Shows Independent “Dose-Response” With Virologic Suppression Rates Among People Living With Human Immunodeficiency Virus. Open forum infectious diseases. 2018;5(3):ofy035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Riley ED, Vittinghoff E, Koss CA, et al. Housing First: Unsuppressed Viral Load Among Women Living with HIV in San Francisco. AIDS Behav. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCree DH, Williams AM, Chesson HW, et al. Changes in Disparities in Estimated HIV Incidence Rates Among Black, Hispanic/Latino, and White Men Who Have Sex With Men (MSM) in the United States, 2010–2015. J Acquir Immune Defic Syndr. 2019;81(1):57–62. [DOI] [PubMed] [Google Scholar]
- 18.Sullivan PS, Purcell DW, Grey JA, et al. Patterns of Racial/Ethnic Disparities and Prevalence in HIV and Syphilis Diagnoses Among Men Who Have Sex With Men, 2016: A Novel Data Visualization. Am J Public Health. 2018;108(S4):S266–S273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.May S, Murray A, Sutton MY. HIV infection among women in the United States: 2000–2017. AIDS Care. 2019:1–8. [DOI] [PubMed] [Google Scholar]
- 20.Baguso GN, Turner CM, Santos GM, et al. Successes and final challenges along the HIV care continuum with transwomen in San Francisco. J Int AIDS Soc. 2019;22(4):e25270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clemenzi-Allen A, Neuhaus J, Geng E, et al. Housing Instability Results in Increased Acute Care Utilization in an Urban HIV Clinic Cohort. Open forum infectious diseases. 2019;6(5):ofz148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Broz D, Wejnert C, Pham HT, et al. HIV infection and risk, prevention, and testing behaviors among injecting drug users -- National HIV Behavioral Surveillance System, 20 U.S. cities, 2009. MMWR Surveill Summ. 2014;63(6):1–51. [PubMed] [Google Scholar]
- 23.Mitsch A, Singh S, Li J, Balaji A, Linley L, Selik R. Age-Associated Trends in Diagnosis and Prevalence of Infection with HIV Among Men Who Have Sex with Men - United States, 2008–2016. MMWR Morb Mortal Wkly Rep. 2018;67(37):1025–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Preskill H P M, Splansky Juster J. Guide to Evaluating Collective Impact: Learning and Evaluation in the Collective Impact Context. Collective Impact Forum. [Google Scholar]
- 25.Preskill H P M, Splansky Juster J. Guide to Evaluating Collective Impact: Assessing Progress and Impact. Collective Impact Forum. [Google Scholar]
- 26.Preskill H P M, Splansky Juster J. Guide to Evaluating Collective Impact: Sample Questions, Outcomes, and Indicators. Collective Impact Forum. [Google Scholar]
- 27.Stachowiak S G L. Does collective impact really make an impact? Stanford Social Innovation Review. [Google Scholar]
- 28.Stachowiak S L J. When collective impact has an impact. 2018.
- 29.Kania J K M. The equity imperative in collective impact. Stanford Social Innovation Review.pp. 36–41. [Google Scholar]
- 30.Wolff T. Ten places where collective impact gets it wrong. GJCPP. 2016;7(1). [Google Scholar]
- 31.Weaver L. The promise and peril of collective impact. The Philanthropist. 2014;26:11–19. [Google Scholar]
- 32.Havlir DV, Buchbinder SP. Ending AIDS in the United States-If Not Now, When? JAMA Intern Med. 2019. [DOI] [PubMed] [Google Scholar]
- 33.Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV Epidemic: A Plan for the United States. JAMA. 2019;321(9):844–845. [DOI] [PubMed] [Google Scholar]
- 34.Fast track to 2030: granularity at a global scale. The lancet HIV. 2015;2(1):e1. [DOI] [PubMed] [Google Scholar]
- 35.Carrico AW, Hunt PW, Neilands TB, et al. Stimulant Use and Viral Suppression in the Era of Universal Antiretroviral Therapy. J Acquir Immune Defic Syndr. 2019;80(1):89–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jin H, Ogunbajo A, Mimiaga MJ, et al. Over the influence: The HIV care continuum among methamphetamine-using men who have sex with men. Drug Alcohol Depend. 2018;192:125–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Riley ED, Moore K, Sorensen JL, Tulsky JP, Bangsberg DR, Neilands TB. Basic subsistence needs and overall health among human immunodeficiency virus-infected homeless and unstably housed women. Am J Epidemiol. 2011;174(5):515–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wohl AR, Benbow N, Tejero J, et al. Antiretroviral Prescription and Viral Suppression in a Representative Sample of HIV-Infected Persons in Care in 4 Large Metropolitan Areas of the United States, Medical Monitoring Project, 2011–2013. J Acquir Immune Defic Syndr. 2017;76(2):158–170. [DOI] [PubMed] [Google Scholar]