Abstract
Hantaviruses are important zoonotic pathogens of public health importance that are found on all continents except Antarctica and are associated with hemorrhagic fever with renal syndrome (HFRS) in the Old World and hantavirus pulmonary syndrome (HPS) in the New World. Despite the significant disease burden they cause, no FDA-approved specific therapeutics or vaccines exist against these lethal viruses. The lack of available interventions is largely due to an incomplete understanding of hantavirus pathogenesis and molecular mechanisms of virus replication, including cellular entry. Hantavirus Gn/Gc glycoproteins are the only viral proteins exposed on the surface of virions and are necessary and sufficient to orchestrate virus attachment and entry. In vitro studies have implicated integrins (β1–3), DAF/CD55, and gC1qR as candidate receptors that mediate viral attachment for both Old World and New World hantaviruses. Recently, protocadherin-1 (PCDH1) was demonstrated as a requirement for cellular attachment and entry of New World hantaviruses In vitro and lethal HPS in vivo, making it the first clade-specific host factor to be identified. Attachment of hantavirus particles to cellular receptors induces their internalization by clathrin-mediated, dynamin-independent, or macropinocytosis-like mechanisms, followed by particle trafficking to an endosomal compartment where the fusion of viral and endosomal membranes can occur. Following membrane fusion, which requires cholesterol and acid pH, viral nucleocapsids escape into the cytoplasm and launch genome replication. In this review, we discuss the current mechanistic understanding of hantavirus entry, highlight gaps in our existing knowledge, and suggest areas for future inquiry.
1. Introduction
Hantaviruses are emerging rodent-borne pathogens whose accidental human transmission causes Hemorrhagic Fever with Renal Syndrome (HFRS) in the Old World and Hantavirus Pulmonary Syndrome (HPS) in the New World (Vaheri et al., 2013). HPS-causing hantaviruses are listed as Category A pathogens by the US National Institute of Allergy and Infectious Diseases (NIAID). Over 50,000 cases occur globally each year with fatality rates of up to 12% (HFRS) and 40% (HPS), depending on the infecting virus (Watson et al., 2014). The number of cases is predicted to increase as climate change and deforestation cause increases in rodent populations, bringing them into close proximity with human settlements (Guterres and de Lemos, 2018; Klempa, 2009). Despite the likelihood that the burden of hantavirus disease will increase, no FDA-approved vaccines or therapeutics exist against HFRS or HPS, in part due to a limited understanding of the viral life cycle. Although the discovery of HPS-causing hantaviruses in the 1990s significantly accelerated hantavirus research, the specific roles of host factors and the details of entry mechanisms remain poorly characterized. Here, we summarize the current understanding of hantavirus entry, including the structures of viral surface glycoproteins, the roles of candidate receptors in entry, pathogenesis, and host range. We also discuss surrogate systems to study hantavirus entry, and the targeting of hantavirus glycoproteins for the development of vaccines and antibody-based therapeutics. Finally, we highlight key questions that remain unanswered in the field.
2. Hantavirus ecology and diseases
Hantaviruses are members of the family Hantaviridae within the order Bunyavirales, which includes many viruses of medical, agricultural, and veterinary importance. Similar to some other bunyaviruses, hantaviruses are maintained and transmitted through many mammalian host reservoirs including bats (order Chiroptera), shrews and moles (order Soricomorpha), and rodents (order Rodentia) (Yanagihara et al., 2014; Zhang, 2014). Virus-host relationships appear to be specific—in general, each hantavirus associates with only one reservoir host (Table 1). Rodent-borne hantaviruses are classified into three clades based on their reservoir hosts: (1) New World viruses [e.g., Sin Nombre virus (SNV), New York-1 virus (NY-1V), and Andes virus (ANDV)] causing HPS that are carried by members of the Sigmodontinae sub-family, (2) Old World viruses [e.g., Hantaan virus (HTNV), Seoul virus (SEOV), and Dobrava-Belgrade virus (DOBV)] causing HFRS that are harbored in Murinae rodents, and (3) viruses found in the New or Old World that are associated with mild disease [Puumala virus (PUUV)] or are non-virulent [e.g., Prospect Hill virus (PHV) and Tula virus (TULV)] and are carried by Arvicolinae rodents (Meyer and Schmaljohn, 2000). Phylogenetic analyses suggest that hantaviruses originated in bats, shrews, or moles and later established persistent infections in rodents. Hantaviruses further diverged as rodent populations underwent geographic separation and divergent evolution (Witkowski et al., 2016; Yanagihara et al., 2014; Zhang, 2014). It is assumed that this co-evolution of virus and host ultimately led to the emergence of virulent hantaviruses, as only rodent-borne hantaviruses, found in the Orthohantavirus genus, are recognized to cause human disease (Forbes et al., 2018). However, there is evidence supporting the occurrence of shrew-borne hantavirus infection in humans (Heinemann et al., 2016; Okumura et al., 2007).
Table 1.
Selected hantaviruses and their reservoir hosts.
| Virus | Host sub-family | Host species | Distribution | Associated disease (fatality rate) |
|---|---|---|---|---|
| Hantaan | Murinae | Striped field mouse (Apodemus agrarius) | Asia and Russia | HFRS (10–15%) |
| Dobrava-Belgrade | Murinae | Yellow-necked mouse (Apodemus flavicollis) | Europe | HFRS (7–12%) |
| Seoul | Murinae | Norway rat (Rattus norvegicus) | Worldwide | HFRS (1–5%) |
| Puumala | Arvicolinae | Bank vole (Clethrionomys glareolus) | Europe | HFRS (0.1–0.4%) |
| Khabarovsk | Arvicolinae | Reed vole (Microtus fortis) | Russia | N/A |
| Prospect Hill | Arvicolinae | Meadow vole (Microtus pennsylvanicus) | North America | N/A |
| Tula | Arvicolinae | Common vole (Microtus arvalis) | Europe | Unknown |
| Isla Vista | Arvicolinae | California vole (Microtus californicus) | North America | N/A |
| Sin Nombre | Sigmodontinae | Deer mouse (Peromyscus maniculatus) | North America | HPS (40–60%) |
| Andes | Sigmodontinae | Long-tailed pygmy rice rat (Oligoryzomys longicaudatus) | South America | HPS (43–56%) |
| Black Creek Canal | Sigmodontinae | Hispid cotton rat (Sigmodon hispidus) | North America | HPS (>40%) |
| Rio Segundo | Sigmodontinae | Mexican harvest mouse (Reithrodontomys mexicanus) | Central America | Unknown |
| Laguna Negra | Sigmodontinae | Large vesper mouse (Calomys callosus) | South America | HPS (15%) |
Red lines separate the rodent-borne hantavirus clades. Viruses in each clade are carried by rodents of the same sub-family. Hantavirus species are found on most continents and display varied virulence in humans (Hardcastle et al., 2016; Jiang et al., 2017; Meyer and Schmaljohn, 2000).
Hantaviruses establish a persistent infection in their rodent hosts that is generally recognized as asymptomatic and can persist for months to the lifetime of the animal (Ermonval et al., 2016; Lee et al., 1978; Yanagihara et al., 1985). Once infected, the host will shed virus through its saliva, urine, and feces, allowing it to infect other rodents through bites or through its excrement, which can form aerosols inhaled by other rodents (Nuzum et al., 1988; Voutilainen et al., 2015). Human infection is considered a spillover event and the main transmission route is through inhalation of virus particles from contaminated rodent excrement (Johnson, 2001). There is some evidence that infection can also occur by the gastrointestinal route (Witkowski et al., 2017). Human-to-human transmission has only been documented for ANDV and occurs among those with fairly intimate contact, such as those who sleep in close proximity over a prolonged period (Martinez et al., 2005; Martinez-Valdebenito et al., 2014). It is suspected that ANDV can be transmitted through bodily fluids from infected individuals. Human infection is characterized by fever, muscle aches, gastrointestinal symptoms, and, most notably, vascular leakage (Sargianou et al., 2012). Due to similar underlying pathology and clinical features such as vascular leakage and thrombocytopenia, some have argued that HFRS and HPS are one disease, and not two (Clement et al., 2014; Rasmuson et al., 2011). However, renal involvement is more prominent in HFRS cases, resulting in oliguria and renal failure, and pulmonary symptoms are more pronounced in HPS cases and many patients experience pulmonary edema (Sargianou et al., 2012), raising the possibility that viral differences in host factor usage account, in part, for these differences in hantavirus pathogenesis.
3. Hantavirus particle and genes
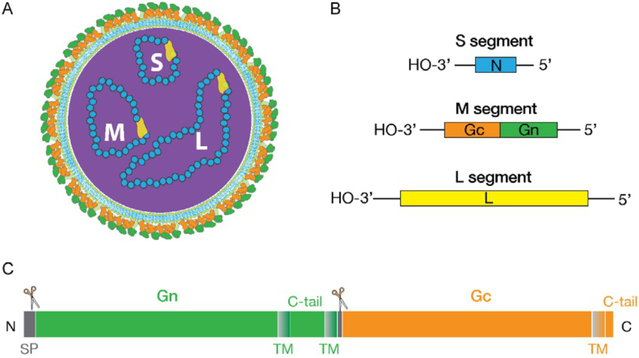
The infectious virions of hantaviruses are enveloped spherical particles with a diameter of 80–120nm (McCormick et al., 1982; Muyangwa et al., 2015) (Fig. 1A). The negative-strand RNA genomes of hantaviruses comprise three segments: a 1.8–2.1kb small segment (S), a 3.7–3.8kb medium segment (M), and a 6.5–6.6kb large segment (L) (Fig. 1B) (Hepojoki et al., 2012; Schmaljohn et al., 1983). Each segment has highly conserved 3′ and 5′ untranslated regions that contain complementary nucleotides (Chizhikov et al., 1995; Schmaljohn and Dalrymple, 1983). These regions recognize each other to form panhandle structures that give the RNA segments a circular appearance in some microscopic images. These panhandle structures are a hallmark of bunyaviruses (Elliott et al., 1991) and are thought to regulate viral transcription and replication, as demonstrated for other negative-strand RNA viruses, such as vesicular stomatitis virus (Wertz et al., 1994) and influenza A virus (Lee and Seong, 1996; Tiley et al., 1994). Viral RNA (vRNA) segments are each associated with an RNA-dependent RNA polymerase (RdRp) and are encased in nucleocapsid protein (Hepojoki et al., 2012; Mir et al., 2006). These are contained in a host-derived lipid envelope that is decorated with two glycoproteins, Gn (N-terminal subunit) and Gc (C-terminal subunit) (Fig. 1B).
Fig. 1.
Schematic representation of hantavirus particle and genes. (A) Hantaviruses carry a tri-segmented negative-sense RNA genome encased in a lipid envelope that is studded with surface spikes comprising the Gn and Gc glycoproteins. (B) Small (S), medium (M) and large (L) genome segments encode nucleoprotein (N), Gn/Gc glycoproteins and RNA-dependent RNA polymerase, respectively. (C) Linear representation of hantavirus Gn/Gc. Gn is proteolytically cleaved from Gc at the conserved WAASA site by the cellular signal protease complex (represented by scissors). SP, signal peptide; TM, transmembrane region (shown as shaded block); C-tail, cytoplasmic tail.
The L and S segments encode the 250-kDa RdRp and the 50-kDa nucleocapsid protein (N), respectively (Schmaljohn et al., 1983, 1986). The RdRp mediates transcription and replication of the hantavirus genome with its transcriptase, replicase, and endonuclease activities (Kukkonen et al., 2005; Muyangwa et al., 2015). The N protein coats the vRNA to protect it from cellular nucleases and works together with RdRp to ensure efficient replication of the viral genome (Mir and Panganiban, 2006; Mir et al., 2006). In addition, ANDV N protein enhances microvascular endothelial cell permeability (Gorbunova et al., 2016). It was also reported that N proteins help mediate viral immune evasion by protecting infected endothelial cells from T cell attack and by down-regulating the type I interferon response (Gupta et al., 2013; Pan et al., 2015). Akin to other bunyaviruses, hantaviruses harbored in Arvicolinae and Sigmodontinae rodents have an overlapping open reading frame (+1) in the S segment that encodes for a putative 7–10kDa non-structural protein NSS. However, only PUUV, TULV and ANDV are known to express it during infection (Jääskeläinen et al., 2007; Vera-Otarola et al., 2012). The reduced frequency of nucleotide substitutions in the predicted NSS coding region likely indicates a functional role for this protein—NSS has been proposed to inhibit the host’s interferon response (Jääskeläinen et al., 2007). However, the contribution of NSS during hantavirus pathogenesis and the reasons for its presence only in viruses infecting arvicoline and sigmodontine rodents are still unknown.
The M segment encodes a glycoprotein precursor (GPC) of 1133–1158 amino acids (Schmaljohn et al., 1987). A signal peptide at the N-terminus of GPC directs the translating ribosomes to the endoplasmic reticulum (ER), where GPC is co-translationally cleaved by the cellular signal peptidase complex at a conserved WAASA sequence to yield Gn and Gc (Fig. 1C) (Kamrud and Schmaljohn, 1994; Löber et al., 2001). Gn and Gc undergo N- and O-glycosylations and traffic together to the Golgi apparatus prior to their incorporation into viral particles. Gn and Gc are the only viral proteins on the surface of hantavirus virions and orchestrate viral entry into susceptible cells.
4. Hantavirus entry pathway
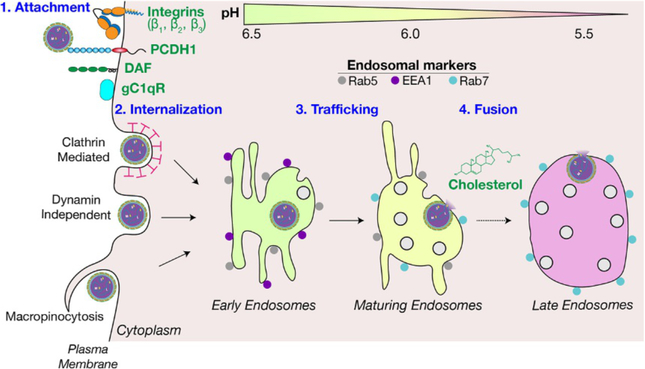
Although hantaviruses cause human diseases worldwide, our knowledge of their entry mechanisms remains limited. This lack of understanding presents one of the major obstacles to the development of new therapies. Viral attachment to the cell surface is the first essential step to establish infection; several cellular proteins have been implicated in mediating Old World and New World hantavirus attachment to cells (see Section 6 for more details, Fig. 2).
Fig. 2.
An overview of the hantavirus entry pathway. Host factors demonstrated or proposed to play a role in four stages of hantavirus entry, i.e., attachment, internalization, trafficking and membrane fusion are indicated. See the text for details.
Following attachment, hantaviruses are internalized, possibly through a variety of endocytic strategies including clathrin-mediated endocytosis and dynamin-independent pathways, depending on cell type and experimental conditions. Some studies suggest that Old World hantaviruses (HTNV, SEOV) are internalized via clathrin-mediated endocytosis (Jin et al., 2002), whereas studies with the New World hantavirus ANDV suggest a more complex picture (Chiang et al., 2016; Ramanathan and Jonsson, 2008). Specifically, Ramanathan and Jonsson described dynamin-independent uptake of ANDV, whereas a small interfering RNA (siRNA) screen in human lung microvascular cells identified genes encoding for dynamin, the clathrin heavy chain, and the adaptor protein AP2, three major components of the clathrin-dependent endocytosis pathway, as major hits for ANDV internalization (Chiang et al., 2016; Ramanathan and Jonsson, 2008). Further, ANDV was shown to be dependent on host factors implicated in dynamin-independent macropinocytosis, including cholesterol and the Rho GTPase Rac11 (Chiang et al., 2016; Torriani et al., 2019).
After internalization, viral particles are delivered to early endosomes and eventually trafficked to late endosomal and lysosomal compartments. One of the hallmarks of endosomal maturation is the decrease of their intra-luminal pH, from mildly acidic in early endosomes to strongly acidic in endo-lysosomes. Because hantaviruses require acid pH (5.8–6.3) to undergo membrane fusion (Arikawa et al., 1985; Cifuentes-Muñoz et al., 2011; Kleinfelter et al., 2015), they are generally assumed to traffic to early or late endosomes (Albornoz et al., 2016). However, details on the molecular mechanisms of hantavirus endocytic trafficking remain limited.
Viral entry culminates in fusion of the viral membrane with the endosomal membrane, followed by escape of the viral nucleocapsid payload into the cytoplasm. Hantavirus membrane fusion is driven by large conformational changes in the Gc protein. The site of hantavirus membrane fusion and the endosomal conditions required for fusion, other than luminal acid pH, are not well defined. Membrane fusion mediated by Gn/Gc of New World hantavirus ANDV has a pH threshold of 5.8, whereas that by Old World hantavirus HTNV Gn/Gc is 6.3 (Arikawa et al., 1985; Cifuentes-Muñoz et al., 2011; Kleinfelter et al., 2015), suggesting late and early endosomes as the sites of fusion, respectively. Although pH is a major determinant of the fusion site, a number of other class II viral glycoproteins (see below) have additional requirements that can influence the identity of the fusion compartment (Bitto et al., 2016; Bron et al., 1993; Dubé et al., 2014; Kielian and Helenius, 1984; Lu et al., 1999; Nieva et al., 1994; Zaitseva et al., 2010). To identify such host requirements for hantavirus entry, genome-wide loss-of-function genetic screens were performed in insect and human cells. These screens revealed the requirement of multiple genes involved in cholesterol sensing, regulation, and biosynthesis for Old and New World hantavirus entry and infection (Kleinfelter et al., 2015; Petersen et al., 2014). Mechanistic studies showed that the cholesterol content of target membranes strongly influences the efficiency of hantavirus Gn/Gc-mediated membrane fusion (Kleinfelter et al., 2015). While alphaviruses, such as Semliki Forest virus and Sindbis virus, require cholesterol in the target membrane for virus fusion (Bron et al., 1993; Kielian and Helenius, 1984; Lu et al., 1999), hantavirus membrane fusion and entry is exquisitely sensitive to small reductions in cellular cholesterol levels, underlining this key requirement (Kleinfelter et al., 2015). Following membrane fusion, the viral nucleocapsid is presumed to escape into the cytoplasm. The molecular details of viral “uncoating” and the delivery of nucleocapsid cores to intracellular sites of transcription and replication remain obscure, as is the potential involvement of host factors in these processes.
5. Structure and function of hantavirus glycoproteins
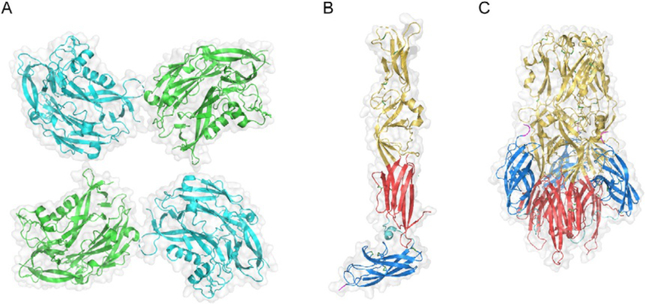
Hantavirus Gn/Gc are necessary and sufficient for cellular entry. On the viral membrane, Gn and Gc form a grid-like pattern that is a characteristic of hantaviruses (Huiskonen et al., 2010; Martin et al., 1985). Each square-shaped Gn/Gc spike has a fourfold symmetry and is composed of four copies each of Gn and Gc (Fig. 3A). The viral Gn is a ~70kDa protein composed of anti-parallel β sheets and α helices (Rissanen et al., 2017) (Fig. 3A). Fitting the crystal structure of PUUV Gn onto a cryo-electron tomography reconstruction of the TULV surface showed that Gn is distal to the viral membrane and sits atop Gc, probably protecting the target membrane-interacting region (TMIR) (Li et al., 2016). Gn contains seven disulfide bonds that stabilize the protein and that are conserved among hantaviruses (Li et al., 2016). In addition, Gn contains multiple N-linked glycans that project toward neighboring Gn proteins and may be important for Gn-Gn interactions. Although soluble Gn is monomeric and has limited Gn-Gn interactions, acidification is proposed to lead to the formation of compact Gn tetramers by locking a β-hairpin into a pocket on the adjacent Gn subunit (Rissanen et al., 2017). Gn is less conserved in amino acid sequence among hantaviruses than is Gc (e.g., 50% and 60% amino acid sequence identity between HTNV and PUUV Gn and Gc, respectively). Nevertheless, divergent Gn (and Gc) proteins share a common fold, suggesting that the overall architecture of Gn/Gc complexes is conserved among hantaviruses (Rissanen et al., 2017). Gn is proposed to bind to cell-surface receptors during entry based on its membrane-distal, solvent-exposed position on the spike and information derived from other bunyaviruses, although this has not been demonstrated experimentally. Given their variability in Gn sequence, different clades of hantaviruses are likely to use different attachment factors and/or receptors (Gavrilovskaya et al., 1998, 1999; Jangra et al., 2018).
Fig. 3.
Structure of hantavirus Gn and Gc. (A) Partial structural model for Gn tetramer derived by fitting the X-ray crystal structure of the N-terminal region of PUUV Gn (amino acid residues 29–383; PDB ID: 5FXU) into the cryo-electron tomography (cryo-ET)-derived density map of the TULV glycoprotein spike (PDB ID: 5FYN) (Li et al., 2016). Adjacent subunits are colored in cyan and green. Gray outlines in (A)–(C) represent surface-shaded views. En face view relative to the surface of the viral particle is shown. (B) X-ray crystal structure of the monomeric ectodomain of HTNV Gc in its putative pre-fusion conformation (PDB ID: 5LJY) (Guardado-Calvo et al., 2016). (C) X-ray crystal structure of the ectodomain of HTNV Gc in its trimeric post-fusion conformation (PDB ID: 5LK0) (Guardado-Calvo et al., 2016). (B) and (C) Gc is colored according to the convention for Class II fusion proteins: domains I, II, and III are shown in red, yellow, and blue, respectively. The DI–DIII linker is shown in cyan, and the beginning of the stem region at the C-terminus of the crystallized ectodomain constructs is shown in magenta. Disulfide bonds are shown as sticks, with sulfur atoms colored green. (C) The trimer is oriented axially to the viral and target membranes, with the fusion loops in domain II at the top of the structure.
The Gn cytoplasmic tail is 110 amino acids long and carries a single structured domain, a zinc finger, which likely plays a role in interactions with the N protein during virus assembly (Estrada et al., 2009, 2011; Wang et al., 2010), possibly in a manner functionally analogous to the matrix proteins of other viruses (Hepojoki et al., 2010a,b). The Gn cytoplasmic tails of virulent hantaviruses can also block the type I interferon response to limit the host immune response to infection (Alff et al., 2008; Shim et al., 2011).
Crystal structures of the pre-fusion ectodomain of Gc proteins from multiple hantaviruses reveal that Gc is a class II fusion protein similar in structure to the glycoproteins of flaviviruses, alphaviruses, Rubella virus, and phleboviruses (Guardado-Calvo and Rey, 2017; Guardado-Calvo et al., 2016; Willensky et al., 2016). Like these latter class II fusion proteins, hantavirus Gc comprises three domains of β strands and sheets: Domain I (DI) is the central domain, Domain II (DII) is located in the membrane-distal region and contains the TMIR, and Domain III (DIII) resides proximal to the viral membrane and connects to the stem and transmembrane domain (Fig. 3B). The hantavirus Gc structure also possesses certain unique features. The hantavirus ij loop on DII is unusually long, allowing the TMIR to consist of three fusion loops involving residues on the cd loop, ij loop, and bc loop (termed the α-αA loop on the PUUV Gc structure) (Guardado-Calvo et al., 2016; Willensky et al., 2016) (Fig. 3B). Gc also contains a conserved N-linked glycosylation site on DII, which is thought to help stabilize Gc interactions with DIII of neighboring Gc protomers during fusion (Willensky et al., 2016). Gc protomers mediate interactions at twofold Gc:Gc contacts between neighboring Gn/Gc spikes on the virion surface (Bignon et al., 2019; Guardado-Calvo et al., 2016; Willensky et al., 2016). Even at neutral pH, these spikes alternate between “open” (in which the TMIR is exposed) and “closed” (in which the TMIR is protected by Gn) conformations in a temperature-dependent manner and only the “closed” form is capable of inducing acid-pH-mediated membrane fusion (Bignon et al., 2019). Hantavirus Gc contains 26 conserved cysteine residues that form disulfide bonds, providing rigidity and stability to the TMIR (Willensky et al., 2016) (Fig. 3B). The Gc cytoplasmic tail is short (9–26 amino acid residues), and has no known function.
The post-fusion Gc structure also resembles those of other class II fusion proteins. DIII packs against the DI and DII junction, and DII hinges to project the fusion loop toward the target membrane (Fig. 3C). At acid pH, Gc forms trimers that are stabilized by salt bridges and a unique N-terminal tail (Acuña et al., 2015; Guardado-Calvo et al., 2016; Willensky et al., 2016). The Gc stem is vital for the formation of post-fusion conformation (Guardado-Calvo and Rey, 2017) and peptides corresponding to it block ANDV fusion (Barriga et al., 2016). The Gc sequence is fairly well-conserved among hantaviruses, consistent with its direct role in viral membrane fusion. ANDV and PUUV share 76% sequence identity and 89% sequence similarity, suggesting that the features seen in Old World hantavirus Gc crystal structures are also present in Gc proteins of New World hantaviruses. This is also supported by three-dimensional (3D) molecular modeling of ANDV Gc (Tischler et al., 2005).
As mentioned above, hantavirus Gn/Gc proteins undergo acid-induced conformational changes during fusion. Associations between Gn and Gc are pH-sensitive and dissociation begins at pH 6.4 for PUUV Gn/Gc (Hepojoki et al., 2010a,b). However, Gn/Gc dissociation is reversible and does not represent virus fusion triggering. Rather, Gn/Gc dissociation likely acts as a priming step that allows Gc to undergo subsequent fusion triggering. In the post-fusion state, spike proteins on the viral surface are composed of Gn tetramers and Gc trimers. Based on a comparison of TULV cryoEM structures at neutral and acid pH, and HTNV Gn crystal structure at acid pH, Rissanen and co-workers proposed that the formation of acid-induced, narrower, compact Gn tetramers detaches it from Gc and exposes otherwise-shielded hydrophobic fusion loops allowing the formation of an extended intermediate (Rissanen et al., 2017). However, structures of the Gn/Gc complexes at neutral and acid pH need to be solved to further test this model. Whether host factors, including the candidate receptors, play a role in the Gn/Gc conformational changes that eventually lead to the fusion of viral and endosomal membranes needs to be determined.
6. Candidate hantavirus receptors
The first proteins characterized as hantavirus entry factors were α5β1 and αVβ3 integrins. Integrins are heterodimeric transmembrane glycoproteins composed of alpha and beta subunits. To fulfill their cellular function, integrins bind to components of the extracellular matrix and link them to the actin cytoskeleton at focal adhesion sites, thus affording bidirectional signaling (Campbell and Humphries, 2011). Both non-enveloped (Guerrero et al., 2000; Jackson et al., 2000; Maginnis et al., 2006; Wickham et al., 1993) and enveloped viruses (Chu and Ng, 2004; Cseke et al., 2009; Feire et al., 2004; Gianni et al., 2010) use integrins for particle attachment or internalization into cells. Integrin-specific ligands and antibodies were evaluated for their effect on hantavirus infection (Gavrilovskaya et al., 1998, 1999). Pre-incubating human umbilical vein endothelial cells (HUVEC) or VeroE6 grivet monkey kidney epithelial cells with the αVβ3 ligand vitronectin reduced cellular susceptibility to multiple virulent New World (ANDV, SNV and NY-1V) and Old World hantaviruses (HTNV, SEOV and PUUV). Conversely, infection by the avirulent PHV was only reduced by the α5β1 ligand fibronectin (Gavrilovskaya et al., 1998, 1999). However, binding of vitronectin and fibronectin is not limited to αVβ3 and α5β1 integrins, respectively. For instance, αVβ3 integrin can recognize both fibronectin and vitronectin depending on its conformation (Boettiger et al., 2001; Van Agthoven et al., 2014). To provide additional specificity, antibodies against αVβ3 and α5β1 integrins were employed in infection-blocking experiments in HUVEC and VeroE6 cells, and were shown to selectively inhibit infections by virulent hantaviruses (ANDV, SNV, HTNV, DOBV and NY-1V), and avirulent PHV, respectively (Gavrilovskaya et al., 1998, 1999; Popugaeva et al., 2012). Many integrins recognize a tripeptide arginine-glycine-aspartate (RGD) motif that is essential for integrin-dependent cell adhesion. The RGD motif is found in fibronectin, vitronectin, fibrinogen, von Willebrand factor, and many other large glycoproteins (Ruoslahti, 1996). However, the lack of inhibition of NY-1V and SNV infection by soluble integrin-blocking RGD peptides and the absence of RGD motifs in hantavirus Gn/Gc proteins suggested a non-RGD-mediated interaction. Moreover, Chinese hamster ovary (CHO) cells expressing a mutated αVβ3 integrin were rendered incapable of binding its physiological ligands and were susceptible to hantavirus infection, further suggesting an RGD-independent mechanism (Gavrilovskaya et al., 1998, 1999).
Ectodomains of the β3 integrin subunit consist of a β-I domain, a hybrid domain, a plexin-semaphorin-integrin (PSI) domain, and four epidermal growth factor (EGF) modules (Campbell and Humphries, 2011; Xiong et al., 2001, 2002). The PSI domain is located at the apex of the β3 integrin protein in its bent/inactive conformation (Xiong et al., 2001). In vitro genetic complementation and neutralization studies mapped the αVβ3 integrin requirement for ANDV and NY-1V infection to the PSI domain (Matthys et al., 2010; Raymond et al., 2005). However, overexpression of human αVβ3 integrin in poorly permissive SupT1 cells failed to restore HTNV and PUUV infectivity (Higa et al., 2012), and a clear correlation between levels of αVβ3 expression and susceptibility to HTNV and PUUV infections was lacking (Higa et al., 2012; Müller et al., 2019) suggesting the existence of integrin-independent entry pathways. Although many studies have outlined the importance of β1/β3 integrins for cellular susceptibility to hantavirus infection, a direct interaction between hantavirus Gn/Gc and β1/β3 integrins has not yet been reported. Additionally, efforts to test the roles of αVβ3 and α5β1 integrins in vivo have been inconclusive. Treatment of newborn murine pups with antibodies targeting αVβ3 integrin after HTNV challenge afforded only a modest increase in survival time (Song et al., 2005). A similar, modest, increase in survival time was also reported when mice were injected with β1 integrin-specific antibodies (Song et al., 2005).
Raftery et al. suggested that hantaviruses use the αMβ2 and αXβ2 integrins to activate neutrophils resulting in the formation of neutrophil extracellular traps (Raftery et al., 2014). Overexpression of αMβ2 or αXβ2 integrin in CHO cells modestly increased HTNV infection suggesting their potential role in virus entry and infection (Raftery et al., 2014). Given that β2 integrins are exclusively expressed on leukocytes, their relevance as hantavirus receptors is unclear since hantavirus infection of neutrophils is nonproductive (Raftery et al., 2014).
Given their pulmonary route of infection in humans, initial infections by hantaviruses are likely to occur at the apical surface of the respiratory epithelium. In vitro studies showed that HTNV, PUUV and Black Creek Canal virus (BCCV) infected polarized epithelial cells predominantly via the apical surface (Krautkrämer and Zeier, 2008; Ravkov et al., 1997), whereas ANDV could infect via both, apical and basolateral surfaces (Rowe and Pekosz, 2006). It is unclear if αVβ3 integrins are expressed at the apical surface (Aplin et al., 1996; Conforti et al., 1992; Schoenenberger et al., 1994) suggesting other cell-surface receptors may mediate virus entry. Experiments to identify such molecules were carried out in polarized cells. Removal of glycosylphosphatidylinositol (GPI)-anchored proteins from the cell surface via phosphatidylinositol-specific phospholipase C treatment led to the identification of decay-accelerating factor (DAF/CD55) as a candidate receptor (Krautkrämer and Zeier, 2008). DAF/CD55 is a 70-kDa GPI-anchored protein localized exclusively to the apical surface of polarized epithelial cells and has been described as an important co-receptor for a number of enteroviruses (Bergelson et al., 1994; Karnauchow et al., 1996; Shafren et al., 1995). Treatment of polarized cells with DAF/CD55-specific antibodies or human recombinant DAF/CD55 ectodomain reduced infection of HTNV and PUUV in a concentration-dependent manner. A separate study confirmed the importance of DAF/CD55 for DOBV (Popugaeva et al., 2012). Other studies have described high-affinity binding of inactivated SNV particles to DAF/CD55 expressed on Tanoue B cells (Buranda et al., 2010, 2014). However, the relevance of DAF/CD55 as a hantavirus receptor in vivo and its role in viral pathogenesis remain unknown.
Proteomic approaches to identify HTNV-binding host factors revealed gC1qR as a candidate cell attachment factor (Choi et al., 2008). gC1qR, a 32-kDa glycoprotein, has no transmembrane domain, but associates with the cell surface through its interaction with other proteins, including integrins, and it can bind to the globular head domain of C1q, a complement protein (Feng et al., 2002). RNA interference-mediated suppression of gC1qR in human lung epithelial A549 cells reduced HTNV binding and infection. Similarly, ectopic expression of gC1qR in CHO cells conferred susceptibility to HTNV infection. However, the precise role of gC1qR in hantavirus entry and its in vivo relevance to viral infection and pathogenesis are unknown.
Using a genome-wide loss-of-function genetic screen in human haploid cells, we recently identified PCDH1 as a New World hantavirus receptor (Jangra et al., 2018). This type I transmembrane protein is a member of the cadherin superfamily and is composed of seven extracellular cadherin (EC) repeats, a transmembrane domain, and a cytoplasmic tail (Sotomayor et al., 2014). PCDH1 is highly expressed in neuronal cells during development, but is also expressed in airway endothelial cells (Faura Tellez et al., 2016; Koppelman et al., 2009; Kozu et al., 2015), which are the major target cells of hantavirus infection in vivo (Nolte et al., 1995; Zaki et al., 1995). Genetic knockout (KO) of PCDH1 in human cell lines and primary endothelial cells significantly reduced their susceptibility to multiple New World viruses, including ANDV, SNV, PHV and Maporal virus (MPRLV), but not to the Old World viruses HTNV and SEOV, providing evidence that PCDH1 is a hantavirus clade-specific entry factor (Jangra et al., 2018). The first extracellular cadherin repeat (EC1) of PCDH1 was found to be required for New World hantavirus entry. Further, treatment of cells with an antibody against the EC1 domain prior to virus exposure or preincubation of virus with a soluble version of PCDH1 reduced New World hantavirus infection in a dose-dependent manner. Importantly, multiple assays showed that New World hantavirus Gn/Gc proteins directly recognize EC1, and a biolayer interferometry-based assay with purified components indicated that these proteins interact with nanomolar affinity (Jangra et al., 2018). To test the in vivo relevance of PCDH1, PCDH1-KO Syrian golden hamsters were generated by CRISPR-Cas9 genome engineering, and WT and PCDH1-KO hamsters were challenged intranasally with a lethal dose of ANDV. Unlike their WT counterparts, the PCDH1-KO hamsters largely survived viral challenge and exhibited limited pathology. The PCDH1-KO hamsters also had lower viral loads in the lung than WT hamsters. Taken together, these findings validated the requirement of PCDH1 for ANDV entry, infection, and pathogenesis in vivo. However, genetic disruption of PCDH1-hantavirus Gn/Gc interaction did not completely inhibit New World hantavirus attachment and entry In vitro, and PCDH1 KO failed to completely eliminate viral replication and disease in hamsters, suggesting that PCDH1-independent entry pathways exist (Jangra et al., 2018). This work further underlines the complexity of the hantavirus entry process and points to the need to evaluate the interplay of different candidate receptors and other host factors in hantavirus entry.
7. Role of candidate receptors in pathogenesis
Although capillary endothelial cells are the major targets of hantavirus infection, viral replication does not appear to directly damage these cells or the vascular endothelium (Nolte et al., 1995; Zaki et al., 1995). Rather, the impairment of endothelial barrier integrity due to an excessive innate immune response is proposed to be central to pathogenesis (Hepojoki et al., 2014; Schönrich et al., 2015) and is a hallmark of hantavirus disease (Duchin et al., 1994; Spiropoulou and Srikiatkhachorn, 2013).
Vascular endothelial growth factor (VEGF), also known as vascular permeability factor, is a key regulator of endothelial permeability (Rahimi, 2017; Senger et al., 1983, 1986). β3 Integrin has been proposed as a host determinant of hantavirus pathogenesis (Mackow and Gavrilovskaya, 2009) given its link to the disruption of endothelial barrier function. VEGF binding to its receptor, VEGFR2, triggers a cascade of signaling events leading to the internalization of VE-cadherin, an adherens junctions protein, which then increases endothelial cell permeability and vascular leakage (Gavard and Gutkind, 2006). On endothelial cells, αVβ3 integrins regulate the permeabilizing effects of VEGF by forming a complex with VEGFR2 (Borges et al., 2000; Soldi et al., 1999). Angiogenic responses to hypoxia and vascular endothelial growth factor (VEGF) are enhanced when β3 integrins are knocked out In vitro and in vivo (Hodivala-Dilke et al., 1999; Reynolds et al., 2002; Su et al., 2012). Further, endothelial cells infected with pathogenic hantaviruses are able to recruit platelets via αIIβ3 integrin In vitro (Gavrilovskaya et al., 2010), which might contribute to the development of thrombocytopenia, another hallmark of hantavirus disease. However, β3 integrin-dependent hantaviruses differ greatly in their virulence in humans as well as experimental animals and cause distinct pathologies, suggesting a more complex picture (Hepojoki et al., 2014). Use of α5β1 integrin instead of αVβ3 integrin by some hantaviruses has been proposed as an explanation for their lack of virulence (Gavrilovskaya et al., 1998, 1999). However, Sangassou virus (SANGV), a β1 integrin-dependent hantavirus (Klempa et al., 2012), is capable of causing human infections, if not disease, in Africa (Klempa et al., 2010). Thus, β1 integrin usage by avirulent PHV and TULV may not be generalizable to all non-pathogenic hantaviruses, and evaluation of integrin usage of a larger group of hantaviruses is warranted. Engagement of another candidate receptor, β2 integrin, by hantaviruses on neutrophils has also been proposed and was implicated as the mechanism of recruitment and activation of neutrophils to the site of hantavirus replication and pathogenesis (Raftery et al., 2014; Schönrich et al., 2015).
In vivo studies with PCDH1-KO Syrian hamsters suggest that PCDH1 is an essential determinant of the severity of HPS (Jangra et al., 2018). As compared to WT animals, lungs from KO animals bore much lower levels of viral RNA and antigen following a lethal ANDV challenge. Moreover, only mild inflammation and tissue damage was seen in the PCDH1-KO animals (Jangra et al., 2018). The lower inflammation and tissue damage in PCDH1-KO animals may simply be a result of lower viral loads, but it is also conceivable that PCDH1 plays a more direct role in the pathogenesis of HPS. PCDH1 localizes to cell-cell contacts of epithelial cells and its knockdown compromises epithelial barrier function (Faura Tellez et al., 2016; Kozu et al., 2015). Thus, perturbation of PCDH1 expression or localization by viral infection may alter vascular permeability. Further, PCDH1 carries a long cytoplasmic tail that is involved in signaling (Kim et al., 2011). Those signaling events, poorly defined at present, may contribute to hantavirus infection and/or HPS pathogenesis. Regardless of the role of PCDH1 and other viral receptors and entry factors in the pathogenesis of HPS, current evidence indicates that the M genome segment, encoding the Gn/Gc proteins, is not the sole determinant of the difference in viral virulence between ANDV and SNV in Syrian hamsters (McElroy et al., 2004). Indeed, the capacity of virulent hantaviruses to delay the early induction of the interferon response (Geimonen et al., 2002; Hepojoki et al., 2014; Matthys and Mackow, 2012; Spiropoulou et al., 2007) is likely to play a role.
8. Candidate receptors as determinants of host range
Host range at a cellular level is determined by a combination of susceptibility, the ability of cells to allow entry of virions into the cytoplasm, and permissiveness, the capacity of cells to support cytoplasmic viral replication. Together with antiviral host factors that restrict viral replication, host factors required for viral entry and replication, including viral receptors, are key molecular determinants of host range for viruses. However, the roles of candidate hantavirus receptors as potential determinants of host range are poorly understood. An aspartate to asparagine (D39N) mutation at position 39 in human β3 integrin impedes NY-1V infection (Raymond et al., 2005). Moreover, a leucine residue at position 33 (L33) in the PSI domain of human β3 integrin has been proposed as a key determinant of ANDV infection and a proline mutation (L33P) in its bovine ortholog impairs ANDV infection (Matthys et al., 2010). Single-nucleotide polymorphisms (SNPs) with changes to valine and proline residues at L33 have been reported in human β3 integrin (Joutsi-Korhonen et al., 2004; Watkins et al., 2002). Based on a limited data set, ANDV-infected individuals were recently shown to have a higher prevalence of L33 (89%) than exposed but uninfected close-household contacts (60%) (Martínez-Valdebenito et al., 2019). By contrast, another study observed no effect of SNPs in αV or β3 integrins on HFRS susceptibility (Chen et al., 2017). However, the in vivo relevance of β3 integrin as a candidate receptor, its direct interaction with hantavirus glycoproteins and any effect of β3 integrin mutations on host range remain to be conclusively determined. Robust PUUV and HTNV infection of kidney cells derived from bank voles, the PUUV reservoir host, despite undetectable levels of β3 integrin (Müller et al., 2019) is suggestive of distinct receptor usage in these reservoir hosts and the identification of such factors will enhance our understanding of hantavirus biology.
9. Model systems to study hantavirus entry
The need for high-biocontainment facilities has challenged the study of entry by highly lethal hantaviruses. This roadblock has been eased by the development of surrogate viral systems bearing the hantavirus glycoproteins, Gn/Gc, which are necessary and sufficient for hantavirus entry. When co-expressed independent of other hantavirus proteins, Gn/Gc assemble into virus-like particles (VLPs) bearing heteromeric spikes similar to those on authentic virions, and resemble the latter in antigenicity (Acuña et al., 2014; Betenbaugh et al., 1995; Li et al., 2010). Although hantavirus VLPs have proven highly useful for studies of Gn/Gc organization and function (Acuña et al., 2014; Betenbaugh et al., 1995; Li et al., 2010), current approaches do not allow for the packaging of a reporter genome, and thus VLPs cannot be employed to assay productive viral entry at present.
To overcome this limitation, researchers have developed various surrogate systems that rely on replacing the native viral entry proteins of model viruses with hantavirus Gn/Gc. The latter can be provided either in trans (by ectopic Gn/Gc expression in infected cells) or in cis (by engineering the hantavirus M segment encoding Gn/Gc into the viral genome) to generate “sheep in wolf’s clothing” viral pseudotypes capable of single or multiple rounds of entry and infection, respectively. Several viruses have been employed to generate these pseudotypes, most notably the rhabdovirus vesicular stomatitis virus (VSV) (Brown et al., 2011; Jangra et al., 2018; Kleinfelter et al., 2015; Petersen et al., 2014; Slough et al., 2019) and several retroviruses (Cifuentes-Muñoz et al., 2010, 2011; Ma et al., 1999; Yu et al., 2013). Importantly, data obtained with such surrogate viral systems must be corroborated with the respective hantaviruses, and indeed, VLPs and pseudotyped viruses have both been shown to behave similarly to their authentic viral counterparts (Higa et al., 2012; Jangra et al., 2018; Kleinfelter et al., 2015; Paneth Iheozor-Ejiofor et al., 2016; Petersen et al., 2014; Ray et al., 2010).
The use of surrogate viruses has afforded the discovery of new mechanistic information regarding hantavirus entry. Because VSVs are cytolytic, they have been used to uncover host factors required for hantavirus entry in comprehensive genetic screens in human cells using cell survival as a selection and to dissect the entry-related roles of these host factors (Jangra et al., 2018; Kleinfelter et al., 2015; Petersen et al., 2014). This approach has uncovered the critical roles of host factors, including the New World hantavirus receptor, PCDH1 (Jangra et al., 2018), and cholesterol during virus entry and infection (Kleinfelter et al., 2015; Petersen et al., 2014). Pseudotyped VSVs have also enabled the production of large viral preparations necessary to efficiently evaluate neutralizing antibodies against both Old World and New World hantaviruses (Higa et al., 2012; Kallio-Kokko et al., 2001; Lee et al., 2006; Levanov et al., 2019; Ogino et al., 2003; Paneth Iheozor-Ejiofor et al., 2016) and immunization with these viruses induces production of neutralizing antibodies and protection in animal models (see Section 10 for details) (Brown et al., 2011; Lee et al., 2006; McClain et al., 2000; Prescott et al., 2014). Pseudotyped lentiviruses bearing hantavirus Gn/Gc proteins have been used to characterize the fusion loops within Gc (Cifuentes-Muñoz et al., 2011) and to selectively transduce vascular endothelial cells (Qian et al., 2006).
Not all hantavirus glycoproteins are amenable to efficient pseudotyping in VSV vectors, however, likely due to a mismatch in the sites of VSV and hantavirus budding within cells. Specifically, the VSV glycoprotein is targeted to the plasma membrane, which is the site of VSV budding (Brown and Lyles, 2003; Green et al., 1981; Johnson et al., 1998), whereas hantavirus Gn/Gc proteins are largely targeted to the Golgi complex (Deyde et al., 2005; Pensiero and Hay, 1992; Ruusala et al., 1992; Spiropoulou, 2001; Spiropoulou et al., 2003) and Old World hantaviruses bud into this organelle (Hung, 1988; Hung et al., 1983). Despite this mismatch, it has been possible to generate VSVs bearing Gn/Gc from ANDV and other New World hantaviruses (Brown et al., 2011; Jangra et al., 2018; Kleinfelter et al., 2015), likely because some Gn/Gc localizes to the plasma membrane (Deyde et al., 2005; Spiropoulou et al., 2003) and can be incorporated into budding virions (Goldsmith et al., 1995; Ravkov et al., 1997). By contrast, generating such VSVs bearing Old World hantavirus Gn/Gc has been more challenging, because little or none of these proteins localize to the plasma membrane (Ogino et al., 2003, 2004; Shi and Elliott, 2002). Recently, replication-competent VSVs were used in a forward genetic approach to identify key mutations in Old World HTNV and DOBV Gn/Gc that enhanced viral multiplication. These studies found that mutations in the cytoplasmic domain of Gn and in the membrane-proximal region of the Gc ectodomain acted synergistically to enhance Gn/Gc incorporation into VSV particles, primarily by increasing Gn/Gc cell surface expression (Slough et al., 2019). The use of similar strategies to generate VSVs expressing other hantavirus Gn/Gc that have been hard to produce is expected to facilitate studies on hantavirus entry. Moreover, similar forward genetic approaches with replication-competent VSVs could be employed to investigate the mechanisms of action of antiviral drugs and neutralizing antibodies through the selection of drug- and antibody-neutralization escape mutants.
10. Vaccines and neutralizing antibodies
No FDA-approved vaccines or specific therapeutics are available to prevent or treat hantavirus infection and/or disease. Studies in HPS (ANDV- or SNV-infected) as well as HFRS (PUUV-infected) convalescent patients suggest a direct correlation between the early mounting of an efficient neutralizing antibody (nAb) response and milder disease outcomes (Bharadwaj et al., 2000; Pettersson et al., 2014; Valdivieso et al., 2006). The protective efficacy of hyperimmune sera in animal models and humans further suggests that Gn/Gc-specific antibodies elicited by active or passive immunization may have utility in the treatment of hantavirus disease (Brocato et al., 2012, 2014; Hooper et al., 2008, 2014a,b; Klingström et al., 2008; Vial et al., 2015). Although numerous studies highlight the importance of nAbs for protection against hantaviruses, cDNA-based vaccination could protect Syrian hamsters from lethal ANDV challenge in the absence of any nAb activity suggesting that nAbs are sufficient but not essential (Brocato et al., 2013).
Vaccination is the most successful approach to induce a potent antiviral state and afford protection against viral infections and diseases. Over the last 20 years, numerous vaccine candidates and modalities have been evaluated for their efficiency against hantaviruses. Since 1990, a formalin-inactivated HTNV vaccine grown in suckling mouse brains (Hantavax™) has been marketed in the Republic of Korea (Cho et al., 2002; Yamanishi et al., 1988). However, due to the lack of well-designed clinical trials, its clinical efficacy and long-term immunogenicity have remained unclear. In a recent phase III clinical trial, high seroconversion but poor nAb generation was reported (Song et al., 2016). Another case-control study observed a moderate protective efficacy of Hantavax™, especially in high-risk populations (Jung et al., 2018). Despite the availability of Hantavax™, therefore, there is a clear and urgent need for new and more efficacious hantavirus vaccines.
As an alternative to inactivated vaccines, live-attenuated vaccines using recombinant VSV or adenovirus (AdV) vectors expressing hantavirus Gn/Gc have been developed. A single injection of a replication-competent VSV vector expressing ANDV Gn/Gc protected Syrian hamsters against lethal ANDV challenge as early as 3 days post immunization (Brown et al., 2011; Prescott et al., 2014). Protection lasted for up to 6 months and loss of protection at later time points correlated with a loss of nAb responses (Prescott et al., 2014). Vaccination of hamsters at 24h post-ANDV challenge was largely protective, suggesting that induction of a potent antiviral state by the recombinant vector itself may have contributed to protection (Brown et al., 2011; Prescott et al., 2014). Single-cycle VSVs carrying HTNV Gn/Gc also afforded protection against HTNV infection in a non-lethal Balb/c mouse model (Lee et al., 2006). Recombinant human AdV serotype 5 (Ad5V)-based vectors expressing ANDV Gn or Gc and recombinant canine AdV serotype 2-based vectors expressing SEOV Gn afforded protection of Syrian hamsters and Balb/c mice against lethal virus challenge, respectively (Safronetz et al., 2009; Yuan et al., 2009). Syrian hamsters vaccinated with a vaccinia virus vector expressing HTNV Gn/Gc and N proteins showed no viremia when challenged with HTNV or SEOV, but were partially susceptible to PUUV infection suggesting partial cross-protection between closely related hantaviruses, and the possibility that broadly protective hantavirus vaccines can be designed (Chu et al., 1995; Schmaljohn et al., 1992).
Although virus-based vaccine platforms have shown promise in animal models, their translation to human use has been complicated by several factors (Tatsis and Ertl, 2004). Pre-existing immunity to Ad5V and other common AdV serotypes might reduce vaccine efficacy. This problem can be avoided by establishing vectors based on rare human (Barouch et al., 2004; Lemckert et al., 2005) or animal adenovirus serotypes (Kobinger et al., 2006). Poor vaccine efficacy due to pre-existing immunity was also observed with vaccinia virus-based vectors: vaccinia viruses expressing HTNV Gn/Gc elicited HTNV-specific nAb titers in 72% of vaccinia virus-naïve patients, but only in 26% of vaccinia virus-immune patients (McClain et al., 2000). Although there is little pre-existing immunity against VSV in most human populations, the increasing popularity of VSV-based vaccines might alter this scenario in the future (Lévy et al., 2018; Regules et al., 2017; Suder et al., 2018).
DNA-based subunit vaccines comprising cDNA vectors encoding hantavirus Gn/Gc have also been evaluated. Immunization of Syrian hamsters with DNA vaccines encoding SEOV or HTNV Gn/Gc rendered them resistant to challenges with HTNV, SEOV and DOBV, but not with the more divergent PUUV (Hooper et al., 1999, 2001). PUUV and SNV Gn/Gc-based cDNA vaccines were also protective in Syrian hamsters (Brocato et al., 2013; Hooper et al., 2013). Unexpectedly, an equivalent ANDV cDNA vaccine was not immunogenic or protective in Syrian hamsters despite the generation of high nAb levels against ANDV as well as heterologous SNV in rhesus macaques (Custer et al., 2003). Passive transfer of sera conferred complete protection to Syrian hamsters even when carried out 4–5 days post-ANDV challenge and delayed HPS development when injected 1 day pre-challenge (Custer et al., 2003). In two phase I clinical studies, three vaccinations with cDNA vaccines expressing HTNV or PUUV Gn/Gc by particle-mediated epidermal delivery showed limited immunogenicity: only 30–56% of individuals developed a nAb response (Boudreau et al., 2012; Hooper et al., 2014a,b). cDNA electroporation improved nAb generation and resulted in nAb responses in up to 78% of individuals (Hooper et al., 2014a,b).
Passive transfer of polyclonal antibodies from animals immunized with hantavirus Gn/Gc-based vaccines conferred protection against lethal ANDV challenge in Syrian hamsters (Brocato et al., 2012, 2014; Haese et al., 2015; Hooper et al., 2008, 2014a,b). Importantly, passive transfusion of hyperimmune sera from ANDV convalescent donors to acute HPS patients improved disease outcomes and nAb titers were found to correlate inversely with HPS severity (Vial et al., 2015) suggesting that mAb-based anti-hantavirus therapeutics could be developed as a complement to vaccines.
For the development of mAb-based therapies, Garrido et al. isolated ANDV Gn/Gc-specific memory B cells from a HPS convalescent patient to generate recombinant human IgG antibodies and evaluated two potently neutralizing mAbs (JL16 and MIB22) for their post-exposure efficacy in Syrian hamsters (Garrido et al., 2018). All hamsters treated with the mAbs, alone or in combination, at 3 and 8 days post lethal ANDV challenge were protected. One of the two mAbs, JL16, cleared virus completely from the hamster lung despite its lower In vitro neutralization capacity, suggesting that antibody Fc-dependent effector functions, including antibody-dependent cellular cytotoxicity (ADCC), may play roles in hantavirus clearance in vivo.
11. Conclusions and future directions
Despite significant progress in understanding the biology of hantaviruses, the mechanisms by which these viruses enter cells and establish infection remain poorly understood. Many of the experiments describing hantavirus candidate receptors such as integrins (β1, β2 and β3), DAF/CD55, and gC1qR were performed before the advent of powerful experimental approaches for the genetic manipulation of cells and hosts, including RNA interference-mediated gene silencing and CRISPR-Cas9 genome engineering. Thus, genetic evidence to support a direct role of these and other candidate entry host factors is lacking. Further, little biochemical or structural evidence is currently available to support hypotheses that these candidate receptors directly engage the hantavirus Gn/Gc glycoproteins. Recent In vitro and in vivo studies provided genetic evidence that the cadherin-superfamily protein, PCDH1, plays a critical role in cell entry, infection, and disease by New World hantaviruses, and used a variety of approaches to demonstrate that PCDH1 directly interacts with hantavirus Gn and/or Gc.
Elucidation of the structures of hantavirus particles via cryo-electron microscopy and the X-ray crystal structures of isolated Gn and Gc subunits has helped characterize the conformational rearrangements required for hantavirus membrane fusion. However, structures of the entire Gn/Gc complex alone and bound to candidate receptors are needed to deepen our understanding of hantavirus entry. The lack of suitable animal models for most hantaviruses and genetic engineering tools to generate gene knockouts in Syrian hamsters, the only available small animal model for human hantavirus disease, until recently have further hampered the in vivo evaluation of host factors in hantavirus infection and disease. However, the wider availability of CRISPR-Cas9 tools, newly generated pseudotyped surrogate viruses for a number of hantaviruses, and recent discoveries of novel hantaviruses from a variety of non-rodent hosts have set the stage for more extensive investigations of hantavirus entry, infection and disease and may pave the way for the development of improved animal models for HPS and HFRS. Despite significant progress in the development of hantavirus vaccines, key features of the immunological mechanisms by which these vaccines afford protection, including the definition of protective epitopes in hantavirus Gn/Gc, remain poorly characterized. We anticipate that the new tools for hantavirus research mentioned above will accelerate the design of improved vaccine immunogens and the development of highly effective antibody therapies to prevent and treat hantavirus disease.
Box 1. Open questions.
Despite significant advances, many gaps exist in the understanding of how hantaviruses hijack host machinery to enter their target cells. Some key questions are:
What is the in vivo relevance of the candidate receptors β1, β2, and β3 integrins, DAF/CD55, and gC1qR, in hantavirus infection and disease?
What, if any, is the interplay among these candidate receptors and PCDH1 in hantavirus entry In vitro and in vivo?
What is the structure of the hantavirus Gn/Gc complex in the oligomeric state found in virions?
What are the structural bases of the interactions between Gn/Gc and its receptor(s)?
Are there conformational changes in hantavirus Gn and/or Gc upon receptor binding, and if so, are these changes required for subsequent membrane fusion?
How are the various pathways for hantavirus internalization into cells influenced by the type of virus, host, or cell type?
Do hantavirus receptors play a direct role in mediating the internalization of virus particles?
What are the endosomal sites of hantavirus membrane fusion and are they dependent on the type of virus or cell?
Does hantavirus membrane fusion require host factors other than acid pH and cholesterol?
Does host factor usage differ between human and natural reservoir hosts?
What are the differences in cellular entry between rodent-borne and non-rodent-borne hantaviruses?
Which, if any, entry host factors influence hantavirus host range and tissue tropism? How can we employ this knowledge to develop better animal models for hantaviruses?
What are the major antigenic sites in hantavirus Gn/Gc proteins, how do they differ among different hantaviruses, and can we exploit this knowledge to design broadly efficacious vaccines and therapeutics?
What is the relationship between nAbs and cell-mediated immunity in conferring protection against hantavirus infection and what role(s) do antibody Fc-effector functions play?
Acknowledgments
This work is supported by U.S. National Institute of Health grants R01 AI132633 and U19 AI142777 (to K.C.). M. Eugenia Dieterle, Ph.D., is a Latin American Fellow in the Biomedical Sciences, supported by the Pew Charitable Trusts.
Abbreviations
- Ad5V
adenovirus serotype-5
- ADCC
antibody-dependent cellular cytotoxicity
- AdV
adenovirus
- ANDV
Andes virus
- BCCV
Black Creek Canal virus
- cDNA
complementary DNA
- CHO
Chinese hamster ovary
- CRISPR
clustered regularly interspaced short palindromic repeats
- CryoEM
cryo-electron microscopy
- DAF/CD55
decay accelerating factor/cluster of differentiation-55
- DOBV
Dobrava-Belgrade virus
- EC1
first extracellular cadherin repeat
- EGF
epidermal growth factor
- ER
endoplasmic reticulum
- Fc
fragment crystallizable region
- FDA
United States Food and Drug Administration
- Gc
C-terminal glycoprotein subunit
- gC1qR
globular head of complement component 1 Q-subcomponent receptor
- Gn
N-terminal glycoprotein subunit
- GPC
glycoprotein precursor
- GPI
glycosylphosphatidylinositol
- HFRS
hemorrhagic fever with renal syndrome
- HPS
hantavirus pulmonary syndrome
- HTNV
Hantaan virus
- HUVEC
human umbilical vein endothelial cells
- KO
knockout
- mAb
monoclonal antibody
- MPRLV
Maporal virus
- N
nucleocapsid protein
- nAb
neutralizing antibody
- NIAID
United States National Institute of Allergy and Infectious Diseases
- NSs
hantavirus non-structural protein
- NY-1V
New York-1 virus
- PCDH1
protocadherin-1
- PHV
Prospect Hill virus
- PSI
plexin-semaphorin-integrin
- PUUV
Puumala virus
- RdRp
RNA-dependent RNA polymerase
- RGD
arginine-glycine-aspartate
- SANGV
Sangassou virus
- SEOV
Seoul virus
- siRNA
small interfering RNA
- SNV
Sin Nombre virus
- TMIR
target membrane-interacting region
- TULV
Tula virus
- VEGF
vascular endothelial growth factor
- VEGFR2
vascular endothelial growth factor receptor-2
- VLP
virus-like particle
- vRNA
viral RNA
- VSV
vesicular stomatitis virus
- WT
wild-type
References
- Acuña R, Cifuentes-Muñoz N, Márquez CL, Bulling M, Klingström J, Mancini R, Lozach P-Y, Tischler ND, 2014. Hantavirus Gn and Gc glycoproteins self-assemble into virus-like particles. J. Virol 88, 2344–2348. 10.1128/JVI.03118-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acuña R, Bignon EA, Mancini R, Lozach P-Y, Tischler ND, 2015. Acidification triggers Andes hantavirus membrane fusion and rearrangement of Gc into a stable post-fusion homotrimer. J. Gen. Virol 96, 3192–3197. 10.1099/jgv.0.000269. [DOI] [PubMed] [Google Scholar]
- Albornoz A, Hoffmann AB, Lozach P-Y, Tischler ND, 2016. Early bunyavirus-host cell interactions. Viruses 8, 143 10.3390/v8050143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alff PJ, Sen N, Gorbunova E, Gavrilovskaya IN, Mackow ER, 2008. The NY-1 hantavirus Gn cytoplasmic tail coprecipitates TRAF3 and inhibits cellular interferon responses by disrupting TBK1-TRAF3 complex formation. J. Virol 82, 9115–9122. 10.1128/JVI.00290-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aplin JD, Spanswick C, Behzad F, Kimber SJ, Vićovac L, 1996. Integrins beta 5, beta 3 and alpha v are apically distributed in endometrial epithelium. Mol. Hum. Reprod 2, 527–534. [DOI] [PubMed] [Google Scholar]
- Arikawa J, Takashima I, Hashimoto N, 1985. Cell fusion by haemorrhagic fever with renal syndrome (HFRS) viruses and its application for titration of virus infectivity and neutralizing antibody. Arch. Virol 86, 303–313. [DOI] [PubMed] [Google Scholar]
- Barouch DH, Pau MG, Custers JHHV, Koudstaal W, Kostense S, Havenga MJE, Truitt DM, Sumida SM, Kishko MG, Arthur JC, Korioth-Schmitz B, Newberg MH, Gorgone DA, Lifton MA, Panicali DL, Nabel GJ, Letvin NL, Goudsmit J, 2004. Immunogenicity of recombinant adenovirus serotype 35 vaccine in the presence of pre-existing anti-Ad5 immunity.J. Immunol 172, 6290–6297. [DOI] [PubMed] [Google Scholar]
- Barriga GP, Villalón-Letelier F, Márquez CL, Bignon EA, Acuña R, Ross BH, Monasterio O, Mardones GA, Vidal SE, Tischler ND, 2016. Inhibition of the hantavirus fusion process by predicted domain III and stem peptides from glycoprotein Gc. PLoS Negl. Trop. Dis 10 e0004799 10.1371/journal.pntd.0004799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergelson JM, Chan M, Solomon KR, St John NF, Lin H, Finberg RW, 1994. Decay-accelerating factor (CD55), a glycosylphosphatidylinositol-anchored complement regulatory protein, is a receptor for several echoviruses. Proc. Natl. Acad. Sci. U. S. A 91, 6245–6248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betenbaugh M, Yu M, Kuehl K, White J, Pennock D, Spik K, Schmaljohn C, 1995. Nucleocapsid- and virus-like particles assemble in cells infected with recombinant baculoviruses or vaccinia viruses expressing the M and the S segments of Hantaan virus. Virus Res 38, 111–124. 10.1016/0168-1702(95)00053-S. [DOI] [PubMed] [Google Scholar]
- Bharadwaj M, Nofchissey R, Goade D, Koster F, Hjelle B, 2000. Humoral immune responses in the hantavirus cardiopulmonary syndrome. J. Infect. Dis 182, 43–48. 10.1086/315657. [DOI] [PubMed] [Google Scholar]
- Bignon EA, Albornoz A, Guardado-Calvo P, Rey FA, Tischler ND, 2019. Molecular organization and dynamics of the fusion protein Gc at the hantavirus surface. Elife 8, e46028 10.7554/eLife.46028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitto D, Halldorsson S, Caputo A, Huiskonen JT, 2016. Low pH and anionic lipid-dependent fusion of uukuniemi phlebovirus to liposomes. J. Biol. Chem 291, 6412–6422. 10.1074/jbc.M115.691113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boettiger D, Lynch L, Blystone S, Huber F, 2001. Distinct ligand-binding modes for integrin alpha(v)beta(3)-mediated adhesion to fibronectin versus vitronectin. J. Biol. Chem 276, 31684–31690. 10.1074/jbc.M103997200. [DOI] [PubMed] [Google Scholar]
- Borges E, Jan Y, Ruoslahti E, 2000. Platelet-derived growth factor receptor beta and vascular endothelial growth factor receptor 2 bind to the beta 3 integrin through its extracellular domain. J. Biol. Chem 275, 39867–39873. 10.1074/jbc.M007040200. [DOI] [PubMed] [Google Scholar]
- Boudreau EF, Josleyn M, Ullman D, Fisher D, Dalrymple L, Sellers-Myers K, Loudon P, Rusnak J, Rivard R, Schmaljohn C, Hooper JW, 2012. A phase 1 clinical trial of Hantaan virus and Puumala virus M-segment DNA vaccines for hemorrhagic fever with renal syndrome. Vaccine 30, 1951–1958. 10.1016/j.vaccine.2012.01.024. [DOI] [PubMed] [Google Scholar]
- Brocato R, Josleyn M, Ballantyne J, Vial P, Hooper JW, 2012. DNA vaccine-generated duck polyclonal antibodies as a postexposure prophylactic to prevent hantavirus pulmonary syndrome (HPS). PLoS One 7, e35996 10.1371/journal.pone.0035996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brocato RL, Josleyn MJ, Wahl-Jensen V, Schmaljohn CS, Hooper JW, 2013. Construction and nonclinical testing of a Puumala virus synthetic M gene-based DNA vaccine. Clin. Vaccine Immunol 20, 218–226. 10.1128/CVI.00546-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brocato RL, Hammerbeck CD, Bell TM, Wells JB, Queen LA, Hooper JW, 2014. A lethal disease model for hantavirus pulmonary syndrome in immunosuppressed Syrian hamsters infected with Sin Nombre virus. J. Virol 88, 811–819. 10.1128/JVI.02906-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bron R, Wahlberg JM, Garoff H, Wilschut J, 1993. Membrane fusion of Semliki forest virus in a model system: correlation between fusion kinetics and structural changes in the envelope glycoprotein. EMBO J 12, 693–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown EL, Lyles DS, 2003. Organization of the vesicular stomatitis virus glycoprotein into membrane microdomains occurs independently of intracellular viral components. J. Virol 77, 3985–3992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KS, Safronetz D, Marzi A, Ebihara H, Feldmann H, 2011. Vesicular stomatitis virus-based vaccine protects hamsters against lethal challenge with Andes virus. J. Virol 85, 12781–12791. 10.1128/JVI.00794-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buranda T, Wu Y, Perez D, Jett SD, BonduHawkins V, Ye C, Edwards B, Hall P, Larson RS, Lopez GP, Sklar LA, Hjelle B, 2010. Recognition of decay accelerating factor and alpha(v)beta(3) by inactivated hantaviruses: toward the development of high-throughput screening flow cytometry assays. Anal. Biochem 402, 151–160. 10.1016/j.ab.2010.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buranda T, Swanson S, Bondu V, Schaefer L, Maclean J, Mo Z, Wycoff K, Belle A, Hjelle B, 2014. Equilibrium and kinetics of Sin Nombre hantavirus binding at DAF/CD55 functionalized bead surfaces. Viruses 6, 1091–1111. 10.3390/v6031091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell ID, Humphries MJ, 2011. Integrin structure, activation, and interactions. Cold Spring Harb. Perspect. Biol 3 10.1101/cshperspect.a004994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X-P, Xiong H-R, Zhu N, Chen Q-Z, Wang H, Zhong C-J, Wang M-R, Lu S, Luo F, Hou W, 2017. Lack of association between integrin αvβ3 gene polymorphisms and hemorrhagic fever with renal syndrome in Han Chinese from Hubei, China. Virol. Sin 32, 73–79. 10.1007/s12250-016-3888-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiang C-F, Flint M, Lin J-MS, Spiropoulou CF, 2016. Endocytic pathways used by Andes virus to enter primary human lung endothelial cells. PLoS One 11, e0164768 10.1371/journal.pone.0164768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chizhikov VE, Spiropoulou CF, Morzunov SP, Monroe MC, Peters CJ, Nichol ST, 1995. Complete genetic characterization and analysis of isolation of Sin Nombre virus. J. Virol 69, 8132–8136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho H-W, Howard CR, Lee H-W, 2002. Review of an inactivated vaccine against hantaviruses. Intervirology 45, 328–333. 10.1159/000067925. [DOI] [PubMed] [Google Scholar]
- Choi Y, Kwon Y-C, Kim S-I, Park J-M, Lee K-H, Ahn B-Y, 2008. A hantavirus causing hemorrhagic fever with renal syndrome requires gC1qR/p32 for efficient cell binding and infection. Virology 381, 178–183. 10.1016/j.virol.2008.08.035. [DOI] [PubMed] [Google Scholar]
- Chu JJ-H, Ng M-L, 2004. Interaction of West Nile virus with alpha v beta 3 integrin mediates virus entry into cells. J. Biol. Chem 279, 54533–54541. 10.1074/jbc.M410208200. [DOI] [PubMed] [Google Scholar]
- Chu YK, Jennings GB, Schmaljohn CS, 1995. A vaccinia virus-vectored Hantaan virus vaccine protects hamsters from challenge with Hantaan and Seoul viruses but not Puumala virus. J. Virol 69, 6417–6423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cifuentes-Muñoz N, Darlix J-L, Tischler ND, 2010. Development of a lentiviral vector system to study the role of the Andes virus glycoproteins. Virus Res 153, 29–35. 10.1016/j.virusres.2010.07.001. [DOI] [PubMed] [Google Scholar]
- Cifuentes-Muñoz N, Barriga GP, Valenzuela PDT, Tischler ND, 2011. Aromatic and polar residues spanning the candidate fusion peptide of the Andes virus Gc protein are essential for membrane fusion and infection. J. Gen. Virol 92, 552–563. 10.1099/vir.0.027235-0. [DOI] [PubMed] [Google Scholar]
- Clement J, Maes P, Van Ranst M, 2014. Hemorrhagic fever with renal syndrome in the new, and hantavirus pulmonary syndrome in the old world: paradi(se)gm lost or regained? Virus Res 187, 55–58. 10.1016/j.virusres.2013.12.036. [DOI] [PubMed] [Google Scholar]
- Conforti G, Dominguez-Jimenez C, Zanetti A, Gimbrone MA, Cremona O, Marchisio PC, Dejana E, 1992. Human endothelial cells express integrin receptors on the luminal aspect of their membrane. Blood 80, 437–446. [PubMed] [Google Scholar]
- Cseke G, Maginnis MS, Cox RG, Tollefson SJ, Podsiad AB, Wright DW, Dermody TS, Williams JV, 2009. Integrin alphavbeta1 promotes infection by human metapneumovirus. Proc. Natl. Acad. Sci. U. S. A 106, 1566–1571. 10.1073/pnas.0801433106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Custer DM, Thompson E, Schmaljohn CS, Ksiazek TG, Hooper JW, 2003. Active and passive vaccination against hantavirus pulmonary syndrome with Andes virus M genome segment-based DNA vaccine. J. Virol 77, 9894–9905. 10.1128/JVI.77.18.9894-9905.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deyde VM, Rizvanov AA, Chase J, Otteson EW, St Jeor SC, 2005. Interactions and trafficking of Andes and Sin Nombre Hantavirus glycoproteins G1 and G2. Virology 331, 307–315. 10.1016/j.virol.2004.11.003. [DOI] [PubMed] [Google Scholar]
- Dubé M, Rey FA, Kielian M, 2014. Rubella virus: first calcium-requiring viral fusion protein. PLoS Pathog 10, e1004530 10.1371/journal.ppat.1004530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duchin JS, Koster FT, Peters CJ, Simpson GL, Tempest B, Zaki SR, Ksiazek TG, Rollin PE, Nichol S, Umland ET, 1994. Hantavirus pulmonary syndrome: a clinical description of 17 patients with a newly recognized disease. The Hantavirus Study Group. N. Engl. J. Med 330, 949–955. 10.1056/NEJM199404073301401. [DOI] [PubMed] [Google Scholar]
- Elliott RM, Schmaljohn CS, Collett MS, 1991. Bunyaviridae genome structure and gene expression. Curr. Top. Microbiol. Immunol 169, 91–141. [DOI] [PubMed] [Google Scholar]
- Ermonval M, Baychelier F, Tordo N, 2016. What do we know about how hantaviruses interact with their different hosts? Viruses 8, 223 10.3390/v8080223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estrada DF, Boudreaux DM, Zhong D, St Jeor SC, De Guzman RN, 2009. The Hantavirus glycoprotein G1 tail contains dual CCHC-type classical zinc fingers. J. Biol. Chem 284, 8654–8660. 10.1074/jbc.M808081200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estrada DF, Conner M, Jeor SC, Guzman RND, 2011. The structure of the hantavirus zinc finger domain is conserved and represents the only natively folded region of the Gn cytoplasmic tail. Front. Microbiol 2, 251 10.3389/fmicb.2011.00251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faura Tellez G, Willemse BWM, Brouwer U, Nijboer-Brinksma S, Vandepoele K, Noordhoek JA, Heijink I, de Vries M, Smithers NP, Postma DS, Timens W, Wiffen L, van Roy F, Holloway JW, Lackie PM, Nawijn MC, Koppelman GH, 2016. Protocadherin-1 localization and cell-adhesion function in airway epithelial cells in asthma. PLoS One 11, e0163967 10.1371/journal.pone.0163967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feire AL, Koss H, Compton T, 2004. Cellular integrins function as entry receptors for human cytomegalovirus via a highly conserved disintegrin-like domain. Proc. Natl. Acad. Sci. U. S. A 101, 15470–15475. 10.1073/pnas.0406821101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng X, Tonnesen MG, Peerschke EIB, Ghebrehiwet B, 2002. Cooperation of C1q receptors and integrins in C1q-mediated endothelial cell adhesion and spreading. J. Immunol 168, 2441–2448. [DOI] [PubMed] [Google Scholar]
- Forbes KM, Sironen T, Plyusnin A, 2018. Hantavirus maintenance and transmission in reservoir host populations. Curr. Opin. Virol 28, 1–6. 10.1016/j.coviro.2017.09.003. [DOI] [PubMed] [Google Scholar]
- Garrido JL, Prescott J, Calvo M, Bravo F, Alvarez R, Salas A, Riquelme R, Rioseco ML, Williamson BN, Haddock E, Feldmann H, Barria MI, 2018. Two recombinant human monoclonal antibodies that protect against lethal Andes hantavirus infection in vivo. Sci. Transl. Med 10, eaat6420 10.1126/scitranslmed.aat6420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavard J, Gutkind JS, 2006. VEGF controls endothelial-cell permeability by promoting the beta-arrestin-dependent endocytosis of VE-cadherin. Nat. Cell Biol 8, 1223–1234. 10.1038/ncb1486. [DOI] [PubMed] [Google Scholar]
- Gavrilovskaya IN, Shepley M, Shaw R, Ginsberg MH, Mackow ER, 1998. Beta3 integrins mediate the cellular entry of hantaviruses that cause respiratory failure. Proc. Natl. Acad. Sci. U. S. A 95, 7074–7079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavrilovskaya IN, Brown EJ, Ginsberg MH, Mackow ER, 1999. Cellular entry of hantaviruses which cause hemorrhagic fever with renal syndrome is mediated by beta3 integrins. J. Virol 73, 3951–3959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavrilovskaya IN, Gorbunova EE, Mackow ER, 2010. Pathogenic hantaviruses direct the adherence of quiescent platelets to infected endothelial cells. J. Virol 84, 4832–4839. 10.1128/JVI.02405-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geimonen E, Neff S, Raymond T, Kocer SS, Gavrilovskaya IN, Mackow ER, 2002. Pathogenic and nonpathogenic hantaviruses differentially regulate endothelial cell responses. Proc. Natl. Acad. Sci. U. S. A 99, 13837–13842. 10.1073/pnas.192298899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gianni T, Cerretani A, Dubois R, Salvioli S, Blystone SS, Rey F, Campadelli-Fiume G, 2010. Herpes simplex virus glycoproteins H/L bind to cells independently of {alpha}V{beta}3 integrin and inhibit virus entry, and their constitutive expression restricts infection. J. Virol 84, 4013–4025. 10.1128/JVI.02502-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsmith CS, Elliott LH, Peters CJ, Zaki SR, 1995. Ultrastructural characteristics of Sin Nombre virus, causative agent of hantavirus pulmonary syndrome. Arch. Virol 140, 2107–2122. 10.1007/BF01323234. [DOI] [PubMed] [Google Scholar]
- Gorbunova EE, Simons MJ, Gavrilovskaya IN, Mackow ER, 2016. The Andes virus nucleocapsid protein directs basal endothelial cell permeability by activating RhoA. MBio 7, e01747–e01816. 10.1128/mBio.01747-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green RF, Meiss HK, Rodriguez-Boulan E, 1981. Glycosylation does not determine segregation of viral envelope proteins in the plasma membrane of epithelial cells. J. Cell Biol 89, 230–239. 10.1083/jcb.89.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guardado-Calvo P, Rey FA, 2017. The envelope proteins of the bunyavirales. Adv. Virus Res 98, 83–118. 10.1016/bs.aivir.2017.02.002. [DOI] [PubMed] [Google Scholar]
- Guardado-Calvo P, Bignon EA, Stettner E, Jeffers SA, Pérez-Vargas J, Pehau-Arnaudet G, Tortorici MA, Jestin J-L, England P, Tischler ND, Rey FA, 2016. Mechanistic insight into bunyavirus-induced membrane fusion from structure-function analyses of the hantavirus envelope glycoprotein Gc. PLoS Pathog 12, e1005813 10.1371/journal.ppat.1005813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrero CA, Méndez E, Zárate S, Isa P, López S, Arias CF, 2000. Integrin alpha(v)beta(3) mediates rotavirus cell entry. Proc. Natl. Acad. Sci. U. S. A 97, 14644–14649. 10.1073/pnas.250299897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S, Braun M, Tischler ND, Stoltz M, Sundström KB, Björkström NK, Ljunggren H-G, Klingström J, 2013. Hantavirus-infection confers resistance to cytotoxic lymphocyte-mediated apoptosis. PLoS Pathog 9, e1003272 10.1371/journal.ppat.1003272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guterres A, de Lemos ERS, 2018. Hantaviruses and a neglected environmental determinant. One Health 5, 27–33. 10.1016/j.onehlt.2017.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haese N, Brocato RL, Henderson T, Nilles ML, Kwilas SA, Josleyn MD, Hammerbeck CD, Schiltz J, Royals M, Ballantyne J, Hooper JW, Bradley DS, 2015. Antiviral biologic produced in DNA vaccine/goose platform protects hamsters against hantavirus pulmonary syndrome when administered post-exposure. PLoS Negl. Trop. Dis 9, e0003803 10.1371/journal.pntd.0003803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardcastle K, Scott D, Safronetz D, Brining DL, Ebihara H, Feldmann H, LaCasse RA, 2016. Laguna Negra virus infection causes hantavirus pulmonary syndrome in Turkish hamsters (Mesocricetus brandti). Vet. Pathol 53, 182–189. 10.1177/0300985815570071. [DOI] [PubMed] [Google Scholar]
- Heinemann P, Tia M, Alabi A, Anon J-C, Auste B, Essbauer S, Gnionsahe A, Kigninlman H, Klempa B, Kraef C, Krüger N, Leendertz FH, Ndhatz-Sanogo M, Schaumburg F, Witkowski PT, Akoua-Koffi CG, Krüger DH, 2016. Human infections by non-rodent-associated hantaviruses in Africa. J. Infect. Dis 214, 1507–1511. 10.1093/infdis/jiw401. [DOI] [PubMed] [Google Scholar]
- Hepojoki J, Strandin T, Vaheri A, Lankinen H, 2010a. Interactions and oligomerization of hantavirus glycoproteins. J. Virol 84, 227–242. 10.1128/JVI.00481-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hepojoki J, Strandin T, Wang H, Vapalahti O, Vaheri A, Lankinen H, 2010b. Cytoplasmic tails of hantavirus glycoproteins interact with the nucleocapsid protein. J. Gen. Virol 91, 2341–2350. 10.1099/vir.0.021006-0. [DOI] [PubMed] [Google Scholar]
- Hepojoki J, Strandin T, Lankinen H, Vaheri A, 2012. Hantavirus structure–molecular interactions behind the scene. J. Gen. Virol 93, 1631–1644. 10.1099/vir.0.042218-0. [DOI] [PubMed] [Google Scholar]
- Hepojoki J, Vaheri A, Strandin T, 2014. The fundamental role of endothelial cells in hantavirus pathogenesis. Front. Microbiol 5, 727 10.3389/fmicb.2014.00727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higa MM, Petersen J, Hooper J, Doms RW, 2012. Efficient production of Hantaan and Puumala pseudovirions for viral tropism and neutralization studies. Virology 423, 134–142. 10.1016/j.virol.2011.08.012. [DOI] [PubMed] [Google Scholar]
- Hodivala-Dilke KM, McHugh KP, Tsakiris DA, Rayburn H, Crowley D, Ullman-Culleré M, Ross FP, Coller BS, Teitelbaum S, Hynes RO, 1999. Beta3-integrin-deficient mice are a model for Glanzmann thrombasthenia showing placental defects and reduced survival. J. Clin. Invest 103, 229–238. 10.1172/JCI5487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper JW, Kamrud KI, Elgh F, Custer D, Schmaljohn CS, 1999. DNA vaccination with hantavirus M segment elicits neutralizing antibodies and protects against Seoul virus infection. Virology 255, 269–278. 10.1006/viro.1998.9586. [DOI] [PubMed] [Google Scholar]
- Hooper JW, Custer DM, Thompson E, Schmaljohn CS, 2001. DNA vaccination with the Hantaan virus M gene protects Hamsters against three of four HFRS hantaviruses and elicits a high-titer neutralizing antibody response in Rhesus monkeys. J. Virol 75, 8469–8477. 10.1128/JVI.75.18.8469-8477.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper JW, Ferro AM, Wahl-Jensen V, 2008. Immune serum produced by DNA vaccination protects hamsters against lethal respiratory challenge with Andes virus. J. Virol 82, 1332–1338. 10.1128/JVI.01822-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper JW, Josleyn M, Ballantyne J, Brocato R, 2013. A novel Sin Nombre virus DNA vaccine and its inclusion in a candidate pan-hantavirus vaccine against hantavirus pulmonary syndrome (HPS) and hemorrhagic fever with renal syndrome (HFRS). Vaccine 31, 4314–4321. 10.1016/j.vaccine.2013.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper JW, Brocato RL, Kwilas SA, Hammerbeck CD, Josleyn MD, Royals M, Ballantyne J, Wu H, Jiao J, Matsushita H, Sullivan EJ, 2014a. DNA vaccine-derived human IgG produced in transchromosomal bovines protect in lethal models of hantavirus pulmonary syndrome. Sci. Transl. Med 6, 264ra162 10.1126/scitranslmed.3010082. [DOI] [PubMed] [Google Scholar]
- Hooper JW, Moon JE, Paolino KM, Newcomer R, McLain DE, Josleyn M, Hannaman D, Schmaljohn C, 2014b. A phase 1 clinical trial of Hantaan virus and Puumala virus M-segment DNA vaccines for haemorrhagic fever with renal syndrome delivered by intramuscular electroporation. Clin. Microbiol. Infect 20 (Suppl. 5), 110–117. 10.1111/1469-0691.12553. [DOI] [PubMed] [Google Scholar]
- Huiskonen JT, Hepojoki J, Laurinmäki P, Vaheri A, Lankinen H, Butcher SJ, Grünewald K, 2010. Electron cryotomography of Tula hantavirus suggests a unique assembly paradigm for enveloped viruses. J. Virol 84, 4889–4897. 10.1128/JVI.00057-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung T, 1988. Atlas of Hemorrhagic Fever With Renal Syndrome. Science Press, Beijing. [Google Scholar]
- Hung T, Xia SM, Zhao TX, Zhou JY, Song G, Liao GXH, Ye WW, Chu YL, Hang CS, 1983. Morphological evidence for identifying the viruses of hemorrhagic fever with renal syndrome as candidate members of the bunyaviridae family. Arch. Virol 78, 137–144. 10.1007/BF01310869. [DOI] [PubMed] [Google Scholar]
- Jääskeläinen KM, Kaukinen P, Minskaya ES, Plyusnina A, Vapalahti O, Elliott RM, Weber F, Vaheri A, Plyusnin A, 2007. Tula and Puumala hantavirus NSs ORFs are functional and the products inhibit activation of the interferon-beta promoter. J. Med. Virol 79, 1527–1536. 10.1002/jmv.20948. [DOI] [PubMed] [Google Scholar]
- Jackson T, Sheppard D, Denyer M, Blakemore W, King AM, 2000. The epithelial integrin alphavbeta6 is a receptor for foot-and-mouth disease virus. J. Virol 74, 4949–4956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jangra RK, Herbert AS, Li R, Jae LT, Kleinfelter LM, Slough MM, Barker SL, Guardado-Calvo P, Román-Sosa G, Dieterle ME, Kuehne AI, Muena NA, Wirchnianski AS, Nyakatura EK, Fels JM, Ng M, Mittler E, Pan J, Bharrhan S, Wec AZ, Chandran K, 2018. Protocadherin-1 is essential for cell entry by New World hantaviruses. Nature 563, 559–563. 10.1038/s41586-018-0702-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang H, Zheng X, Wang L, Du H, Wang P, Bai X, 2017. Hantavirus infection: a global zoonotic challenge. Virol. Sin 32, 32–43. 10.1007/s12250-016-3899-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin M, Park J, Lee S, Park B, Shin J, Song K-J, Ahn T-I, Hwang S-Y, Ahn B-Y, Ahn K, 2002. Hantaan virus enters cells by clathrin-dependent receptor-mediated endocytosis. Virology 294, 60–69. 10.1006/viro.2001.1303. [DOI] [PubMed] [Google Scholar]
- Johnson KM, 2001. Hantaviruses: history and overview. Curr. Top. Microbiol. Immunol 256, 1–14. [DOI] [PubMed] [Google Scholar]
- Johnson JE, Rodgers W, Rose JK, 1998. A plasma membrane localization signal in the HIV-1 envelope cytoplasmic domain prevents localization at sites of vesicular stomatitis virus budding and incorporation into VSV virions. Virology 251, 244–252. 10.1006/viro.1998.9429. [DOI] [PubMed] [Google Scholar]
- Joutsi-Korhonen L, Preston S, Smethurst PA, Ijsseldijk M, Schaffner-Reckinger E, Armour KL, Watkins NA, Clark MR, de Groot PG, Farndale RW, Ouwehand WH, Williamson LM, 2004. The effect of recombinant IgG antibodies against the leucine-33 form of the platelet beta3 integrin (HPA-1a) on platelet function. Thromb. Haemost 91, 743–754. 10.1160/TH03-07-0484. [DOI] [PubMed] [Google Scholar]
- Jung J, Ko S-J, Oh HS, Moon SM, Song J-W, Huh K, 2018. Protective effectiveness of inactivated hantavirus vaccine against hemorrhagic fever with renal syndrome. J. Infect. Dis 217, 1417–1420. 10.1093/infdis/jiy037. [DOI] [PubMed] [Google Scholar]
- Kallio-Kokko H, Leveelahti R, Brummer-Korvenkontio M, Lundkvist A, Vaheri A, Vapalahti O, 2001. Human immune response to Puumala virus glycoproteins and nucleocapsid protein expressed in mammalian cells. J. Med. Virol 65, 605–613. 10.1002/jmv.2079. [DOI] [PubMed] [Google Scholar]
- Kamrud KI, Schmaljohn CS, 1994. Expression strategy of the M genome segment of Hantaan virus. Virus Res 31, 109–121. [DOI] [PubMed] [Google Scholar]
- Karnauchow TM, Tolson DL, Harrison BA, Altman E, Lublin DM, Dimock K, 1996. The HeLa cell receptor for enterovirus 70 is decay-accelerating factor (CD55). J. Virol 70, 5143–5152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kielian MC, Helenius A, 1984. Role of cholesterol in fusion of Semliki Forest virus with membranes. J. Virol 52, 281–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S-Y, Yasuda S, Tanaka H, Yamagata K, Kim H, 2011. Non-clustered protocadherin. Cell Adh. Migr 5, 97–105. 10.4161/cam.5.2.14374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinfelter LM, Jangra RK, Jae LT, Herbert AS, Mittler E, Stiles KM, Wirchnianski AS, Kielian M, Brummelkamp TR, Dye JM, Chandran K, 2015. Haploid genetic screen reveals a profound and direct dependence on cholesterol for hantavirus membrane fusion. MBio 6, e00801 10.1128/mBio.00801-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klempa B, 2009. Hantaviruses and climate change. Clin. Microbiol. Infect 15, 518–523. 10.1111/j.1469-0691.2009.02848.x. [DOI] [PubMed] [Google Scholar]
- Klempa B, Koivogui L, Sylla O, Koulemou K, Auste B, Krüger DH, ter Meulen J, 2010. Serological evidence of human hantavirus infections in Guinea, West Africa. J. Infect. Dis 201, 1031–1034. 10.1086/651169. [DOI] [PubMed] [Google Scholar]
- Klempa B, Witkowski PT, Popugaeva E, Auste B, Koivogui L, Fichet-Calvet E, Strecker T, Ter Meulen J, Krüger DH, 2012. Sangassou virus, the first hantavirus isolate from Africa, displays genetic and functional properties distinct from those of other murinae-associated hantaviruses. J. Virol 86, 3819–3827. 10.1128/JVI.05879-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klingström J, Stoltz M, Hardestam J, Ahlm C, Lundkvist A, 2008. Passive immunization protects cynomolgus macaques against Puumala hantavirus challenge. Antivir. Ther 13, 125–133. [PubMed] [Google Scholar]
- Kobinger GP, Feldmann H, Zhi Y, Schumer G, Gao G, Feldmann F, Jones S, Wilson JM, 2006. Chimpanzee adenovirus vaccine protects against Zaire Ebola virus. Virology 346, 394–401. 10.1016/j.virol.2005.10.042. [DOI] [PubMed] [Google Scholar]
- Koppelman GH, Meyers DA, Howard TD, Zheng SL, Hawkins GA, Ampleford EJ, Xu J, Koning H, Bruinenberg M, Nolte IM, van Diemen CC, Boezen HM, Timens W, Whittaker PA, Stine OC, Barton SJ, Holloway JW, Holgate ST, Graves PE, Martinez FD, Postma DS, 2009. Identification of PCDH1 as a novel susceptibility gene for bronchial hyperresponsiveness. Am. J. Respir. Crit. Care Med 180, 929–935. 10.1164/rccm.200810-1621OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozu Y, Gon Y, Maruoka S, Kazumichi K, Sekiyama A, Kishi H, Nomura Y, Ikeda M, Hashimoto S, 2015. Protocadherin-1 is a glucocorticoid-responsive critical regulator of airway epithelial barrier function. BMC Pulm. Med 15, 80 10.1186/s12890-015-0078-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krautkrämer E, Zeier M, 2008. Hantavirus causing hemorrhagic fever with renal syndrome enters from the apical surface and requires decay-accelerating factor (DAF/CD55). J. Virol 82, 4257–4264. 10.1128/JVI.02210-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kukkonen SKJ, Vaheri A, Plyusnin A, 2005. L protein, the RNA-dependent RNA polymerase of hantaviruses. Arch. Virol 150, 533–556. 10.1007/s00705-004-0414-8. [DOI] [PubMed] [Google Scholar]
- Lee YS, Seong BL, 1996. Mutational analysis of influenza B virus RNA transcription In vitro. J. Virol 70, 1232–1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee HW, Lee PW, Johnson KM, 1978. Isolation of the etiologic agent of Korean hemorrhagic fever. J. Infect. Dis 137, 298–308. 10.1093/infdis/137.3.298. [DOI] [PubMed] [Google Scholar]
- Lee B-H, Yoshimatsu K, Araki K, Okumura M, Nakamura I, Arikawa J, 2006. A pseudotype vesicular stomatitis virus containing Hantaan virus envelope glycoproteins G1 and G2 as an alternative to hantavirus vaccine in mice. Vaccine 24, 2928–2934. 10.1016/j.vaccine.2005.12.040. [DOI] [PubMed] [Google Scholar]
- Lemckert AAC, Sumida SM, Holterman L, Vogels R, Truitt DM, Lynch DM, Nanda A, Ewald BA, Gorgone DA, Lifton MA, Goudsmit J, Havenga MJE, Barouch DH, 2005. Immunogenicity of heterologous prime-boost regimens involving recombinant adenovirus serotype 11 (Ad11) and Ad35 vaccine vectors in the presence of anti-ad5 immunity. J. Virol 79, 9694–9701. 10.1128/JVI.79.15.9694-9701.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levanov L, Iheozor-Ejiofor RP, Lundkvist Å, Vapalahti O, Plyusnin A, 2019. Defining of MAbs-neutralizing sites on the surface glycoproteins Gn and Gc of a hantavirus using vesicular stomatitis virus pseudotypes and site-directed mutagenesis. J. Gen. Virol 100, 145–155. 10.1099/jgv.0.001202. [DOI] [PubMed] [Google Scholar]
- Lévy Y, Lane C, Piot P, Beavogui AH, Kieh M, Leigh B, Doumbia S, D’Ortenzio E, Lévy-Marchal C, Pierson J, Watson-Jones D, Nguyen V-K, Larson H, Lysander J, Lacabaratz C, Thiebaut R, Augier A, Ishola D, Kennedy S, Chêne G, Yazdanpanah Y, 2018. Prevention of Ebola virus disease through vaccination: where we are in 2018. Lancet 392, 787–790. 10.1016/S0140-6736(18)31710-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C, Liu F, Liang M, Zhang Q, Wang X, Wang T, Li J, Li D, 2010. Hantavirus-like particles generated in CHO cells induce specific immune responses in C57BL/6 mice. Vaccine 28, 4294–4300. 10.1016/j.vaccine.2010.04.025. [DOI] [PubMed] [Google Scholar]
- Li S, Rissanen I, Zeltina A, Hepojoki J, Raghwani J, Harlos K, Pybus OG, Huiskonen JT, Bowden TA, 2016. A molecular-level account of the antigenic hantaviral surface. Cell Rep 15, 959–967. 10.1016/j.celrep.2016.03.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löber C, Anheier B, Lindow S, Klenk HD, Feldmann H, 2001. The Hantaan virus glycoprotein precursor is cleaved at the conserved pentapeptide WAASA. Virology 289, 224–229. 10.1006/viro.2001.1171. [DOI] [PubMed] [Google Scholar]
- Lu YE, Cassese T, Kielian M, 1999. The cholesterol requirement for sindbis virus entry and exit and characterization of a spike protein region involved in cholesterol dependence. J. Virol 73, 4272–4278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma M, Kersten DB, Kamrud KI, Wool-Lewis RJ, Schmaljohn C, González-Scarano F, 1999. Murine leukemia virus pseudotypes of La Crosse and Hantaan Bunyaviruses: a system for analysis of cell tropism. Virus Res 64, 23–32. 10.1016/S0168-1702(99)00070-2. [DOI] [PubMed] [Google Scholar]
- Mackow ER, Gavrilovskaya IN, 2009. Hantavirus regulation of endothelial cell functions. Thromb. Haemost 102, 1030–1041. 10.1160/TH09-09-0640. [DOI] [PubMed] [Google Scholar]
- Maginnis MS, Forrest JC, Kopecky-Bromberg SA, Dickeson SK, Santoro SA, Zutter MM, Nemerow GR, Bergelson JM, Dermody TS, 2006. Beta1 integrin mediates internalization of mammalian reovirus. J. Virol 80, 2760–2770. 10.1128/JVI.80.6.2760-2770.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin ML, Lindsey-Regnery H, Sasso DR, McCormick JB, Palmer E, 1985. Distinction between Bunyaviridae genera by surface structure and comparison with Hantaan virus using negative stain electron microscopy. Arch. Virol 86, 17–28. 10.1007/BF01314110. [DOI] [PubMed] [Google Scholar]
- Martinez VP, Bellomo C, San Juan J, Pinna D, Forlenza R, Elder M, Padula PJ, 2005. Person-to-person transmission of Andes virus. Emerg. Infect. Dis 11, 1848–1853. 10.3201/eid1112.050501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Valdebenito C, Calvo M, Vial C, Mansilla R, Marco C, Palma RE, Vial PA, Valdivieso F, Mertz G, Ferrés M, 2014. Person-to-person household and nosocomial transmission of Andes hantavirus, Southern Chile, 2011. Emerg. Infect. Dis 20, 1629–1636. 10.3201/eid2010.140353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez-Valdebenito C, Angulo J, Le Corre N, Marco C, Vial C, Miquel JF, Cerda J, Mertz G, Vial P, Lopez-Lastra M, Ferrés M, 2019. A single-nucleotide polymorphism of αVβ3 integrin is associated with the Andes virus infection susceptibility. Viruses 11, 169 10.3390/v11020169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthys VS, Gorbunova EE, Gavrilovskaya IN, Mackow ER, 2010. Andes virus recognition of human and Syrian hamster beta3 integrins is determined by an L33P substitution in the PSI domain. J. Virol 84, 352–360. 10.1128/JVI.01013-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthys V, Mackow ER, 2012. Hantavirus regulation of type I interferon responses. Adv.Virol 2012, 524024 10.1155/2012/524024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClain DJ, Summers PL, Harrison SA, Schmaljohn AL, Schmaljohn CS, 2000. Clinical evaluation of a vaccinia-vectored Hantaan virus vaccine. J. Med. Virol 60, 77–85. . [DOI] [PubMed] [Google Scholar]
- McCormick JB, Sasso DR, Palmer EL, Kiley MP, 1982. Morphological identification of the agent of Korean haemorrhagic fever (Hantaan virus) as a member of the Bunyaviridae. Lancet 1, 765–768. [DOI] [PubMed] [Google Scholar]
- McElroy AK, Smith JM, Hooper JW, Schmaljohn CS, 2004. Andes virus M genome segment is not sufficient to confer the virulence associated with Andes virus in Syrian hamsters. Virology 326, 130–139. 10.1016/j.virol.2004.05.018. [DOI] [PubMed] [Google Scholar]
- Meyer BJ, Schmaljohn CS, 2000. Persistent hantavirus infections: characteristics and mechanisms. Trends Microbiol 8, 61–67. 10.1016/S0966-842X(99)01658-3. [DOI] [PubMed] [Google Scholar]
- Mir MA, Panganiban AT, 2006. Characterization of the RNA chaperone activity of hantavirus nucleocapsid protein. J. Virol 80, 6276–6285. 10.1128/JVI.00147-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mir MA, Brown B, Hjelle B, Duran WA, Panganiban AT, 2006. Hantavirus N protein exhibits genus-specific recognition of the viral RNA panhandle. J. Virol 80, 11283–11292. 10.1128/JVI.00820-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Müller A, Baumann A, Essbauer S, Radosa L, Krüger DH, Witkowski PT, Zeier M, Krautkrämer E, 2019. Analysis of the integrin β3 receptor for pathogenic orthohantaviruses in rodent host species. Virus Res 267, 36–40. 10.1016/j.virusres.2019.04.009. [DOI] [PubMed] [Google Scholar]
- Muyangwa M, Martynova EV, Khaiboullina SF, Morzunov SP, Rizvanov AA, 2015. Hantaviral proteins: structure, functions, and role in hantavirus infection. Front. Microbiol 6, 1326 10.3389/fmicb.2015.01326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nieva JL, Bron R, Corver J, Wilschut J, 1994. Membrane fusion of Semliki Forest virus requires sphingolipids in the target membrane. EMBO J 13, 2797–2804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolte KB, Feddersen RM, Foucar K, Zaki SR, Koster FT, Madar D, Merlin TL, McFeeley PJ, Umland ET, Zumwalt RE, 1995. Hantavirus pulmonary syndrome in the United States: a pathological description of a disease caused by a new agent. Hum. Pathol 26, 110–120. 10.1016/0046-8177(95)90123-X. [DOI] [PubMed] [Google Scholar]
- Nuzum EO, Rossi CA, Stephenson EH, LeDuc JW, 1988. Aerosol transmission of Hantaan and related viruses to laboratory rats. Am. J. Trop. Med. Hyg 38, 636–640. 10.4269/ajtmh.1988.38.636. [DOI] [PubMed] [Google Scholar]
- Ogino M, Ebihara H, Lee B-H, Araki K, Lundkvist A, Kawaoka Y, Yoshimatsu K, Arikawa J, 2003. Use of vesicular stomatitis virus pseudotypes bearing hantaan or Seoul virus envelope proteins in a rapid and safe neutralization test. Clin. Diagn. Lab. Immunol 10, 154–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogino M, Yoshimatsu K, Ebihara H, Araki K, Lee B-H, Okumura M, Arikawa J, 2004. Cell fusion activities of Hantaan virus envelope glycoproteins. J. Virol 78, 10776–10782. 10.1128/JVI.78.19.10776-10782.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okumura M, Yoshimatsu K, Kumperasart S, Nakamura I, Ogino M, Taruishi M, Sungdee A, Pattamadilok S, Ibrahim IN, Erlina S, Agui T, Yanagihara R, Arikawa J, 2007. Development of serological assays for Thottapalayam virus, an insectivore-borne Hantavirus. Clin. Vaccine Immunol 14, 173–181. 10.1128/CVI.00347-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan W, Bian G, Wang K, Feng T, Dai J, 2015. Effects of different doses of nucleocapsid protein from Hantaan virus A9 strain on regulation of interferon signaling. Viral Immunol 28, 448–454. 10.1089/vim.2015.0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paneth Iheozor-Ejiofor R, Levanov L, Hepojoki J, Strandin T, Lundkvist Å, Plyusnin A, Vapalahti O, 2016. Vaccinia virus-free rescue of fluorescent replication-defective vesicular stomatitis virus and pseudotyping with Puumala virus glycoproteins for use in neutralization tests. J. Gen. Virol 97, 1052–1059. 10.1099/jgv.0.000437. [DOI] [PubMed] [Google Scholar]
- Pensiero MN, Hay J, 1992. The Hantaan virus M-segment glycoproteins G1 and G2 can be expressed independently. J. Virol 66, 1907–1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen J, Drake MJ, Bruce EA, Riblett AM, Didigu CA, Wilen CB, Malani N, Male F, Lee F-H, Bushman FD, Cherry S, Doms RW, Bates P, Briley K, 2014. The major cellular sterol regulatory pathway is required for Andes virus infection. PLoS Pathog 10, e1003911 10.1371/journal.ppat.1003911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettersson L, Thunberg T, Rocklöv J, Klingström J, Evander M, Ahlm C, 2014. Viral load and humoral immune response in association with disease severity in Puumala hantavirus-infected patients—implications for treatment. Clin. Microbiol. Infect 20, 235–241. 10.1111/1469-0691.12259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popugaeva E, Witkowski PT, Schlegel M, Ulrich RG, Auste B, Rang A, Krüger DH, Klempa B, 2012. Dobrava-Belgrade hantavirus from Germany shows receptor usage and innate immunity induction consistent with the pathogenicity of the virus in humans. PLoS One 7, e35587 10.1371/journal.pone.0035587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prescott J, DeBuysscher BL, Brown KS, Feldmann H, 2014. Long-term single-dose efficacy of a vesicular stomatitis virus-based Andes virus vaccine in Syrian hamsters. Viruses 6, 516–523. 10.3390/v6020516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian Z, Haessler M, Lemos JA, Arsenault JR, Aguirre JE, Gilbert JR, Bowler RP, Park F, 2006. Targeting vascular injury using Hantavirus-pseudotyped lentiviral vectors. Mol. Ther 13, 694–704. 10.1016/j.ymthe.2005.11.016. [DOI] [PubMed] [Google Scholar]
- Raftery MJ, Lalwani P, Krautkrämer E, Peters T, Scharffetter-Kochanek K, Krüger R, Hofmann J, Seeger K, Krüger DH, Schönrich G, 2014. β2 integrin mediates hantavirus-induced release of neutrophil extracellular traps. J. Exp. Med 211, 1485–1497. 10.1084/jem.20131092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahimi N, 2017. Defenders and challengers of endothelial barrier function. Front. Immunol 8, 1847 10.3389/fimmu.2017.01847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramanathan HN, Jonsson CB, 2008. New and old world hantaviruses differentially utilize host cytoskeletal components during their life cycles. Virology 374, 138–150. 10.1016/j.virol.2007.12.030. [DOI] [PubMed] [Google Scholar]
- Rasmuson J, Andersson C, Norrman E, Haney M, Evander M, Ahlm C, 2011. Time to revise the paradigm of hantavirus syndromes? Hantavirus pulmonary syndrome caused by European hantavirus. Eur. J. Clin. Microbiol. Infect. Dis 30, 685–690. 10.1007/s10096-010-1141-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravkov EV, Nichol ST, Compans RW, 1997. Polarized entry and release in epithelial cells of Black Creek Canal virus, a new world hantavirus. J. Virol 71, 1147–1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray N, Whidby J, Stewart S, Hooper JW, Bertolotti-Ciarlet A, 2010. Study of Andes virus entry and neutralization using a pseudovirion system. J. Virol. Methods 163, 416–423. 10.1016/j.jviromet.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Raymond T, Gorbunova E, Gavrilovskaya IN, Mackow ER, 2005. Pathogenic hantaviruses bind plexin-semaphorin-integrin domains present at the apex of inactive, bent alphavbeta3 integrin conformers. Proc. Natl. Acad. Sci. U. S. A 102, 1163–1168. 10.1073/pnas.0406743102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regules JA, Beigel JH, Paolino KM, Voell J, Castellano AR, Hu Z, Muñoz P, Moon JE, Ruck RC, Bennett JW, Twomey PS, Gutiérrez RL, Remich SA, Hack HR, Wisniewski ML, Josleyn MD, Kwilas SA, Van Deusen N, Mbaya OT, Zhou Y, rVSVΔG-ZEBOV-GP Study Group, 2017. A recombinant vesicular stomatitis virus ebola vaccine. N. Engl. J. Med 376, 330–341. 10.1056/NEJMoa1414216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds LE, Wyder L, Lively JC, Taverna D, Robinson SD, Huang X, Sheppard D, Hynes RO, Hodivala-Dilke KM, 2002. Enhanced pathological angiogenesis in mice lacking beta3 integrin or beta3 and beta5 integrins. Nat. Med 8, 27–34. 10.1038/nm0102-27. [DOI] [PubMed] [Google Scholar]
- Rissanen I, Stass R, Zeltina A, Li S, Hepojoki J, Harlos K, Gilbert RJC, Huiskonen JT, Bowden TA, 2017. Structural transitions of the conserved and meta-stable hantaviral glycoprotein envelope. J. Virol 91, e00378–17. 10.1128/JVI.00378-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe RK, Pekosz A, 2006. Bidirectional virus secretion and nonciliated cell tropism following Andes virus infection of primary airway epithelial cell cultures. J. Virol 80, 1087–1097. 10.1128/JVI.80.3.1087-1097.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruoslahti E, 1996. RGD and other recognition sequences for integrins. Annu. Rev. Cell Dev. Biol 12, 697–715. 10.1146/annurev.cellbio.12.1.697. [DOI] [PubMed] [Google Scholar]
- Ruusala A, Persson R, Schmaljohn CS, Pettersson RF, 1992. Coexpression of the membrane glycoproteins G1 and G2 of Hantaan virus is required for targeting to the Golgi complex. Virology 186, 53–64. [DOI] [PubMed] [Google Scholar]
- Safronetz D, Hegde NR, Ebihara H, Denton M, Kobinger GP, St Jeor S, Feldmann H, Johnson DC, 2009. Adenovirus vectors expressing hantavirus proteins protect hamsters against lethal challenge with andes virus. J. Virol 83, 7285–7295. 10.1128/JVI.00373-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sargianou M, Watson DC, Chra P, Papa A, Starakis I, Gogos C, Panos G, 2012. Hantavirus infections for the clinician: from case presentation to diagnosis and treatment. Crit. Rev. Microbiol 38, 317–329. 10.3109/1040841X.2012.673553. [DOI] [PubMed] [Google Scholar]
- Schmaljohn CS, Dalrymple JM, 1983. Analysis of Hantaan virus RNA: evidence for a new genus of bunyaviridae. Virology 131, 482–491. 10.1016/0042-6822(83)90514-7. [DOI] [PubMed] [Google Scholar]
- Schmaljohn CS, Hasty SE, Harrison SA, Dalrymple JM, 1983. Characterization of Hantaan virions, the prototype virus of hemorrhagic fever with renal syndrome. J. Infect. Dis 148, 1005–1012. 10.1093/infdis/148.6.1005. [DOI] [PubMed] [Google Scholar]
- Schmaljohn CS, Jennings GB, Hay J, Dalrymple JM, 1986. Coding strategy of the S genome segment of Hantaan virus. Virology 155, 633–643. [DOI] [PubMed] [Google Scholar]
- Schmaljohn CS, Schmaljohn AL, Dalrymple JM, 1987. Hantaan virus M RNA: coding strategy, nucleotide sequence, and gene order. Virology 157, 31–39. [DOI] [PubMed] [Google Scholar]
- Schmaljohn CS, Hasty SE, Dalrymple JM, 1992. Preparation of candidate vacciniavectored vaccines for haemorrhagic fever with renal syndrome. Vaccine 10, 10–13. [DOI] [PubMed] [Google Scholar]
- Schoenenberger CA, Zuk A, Zinkl GM, Kendall D, Matlin KS, 1994. Integrin expression and localization in normal MDCK cells and transformed MDCK cells lacking apical polarity. J. Cell Sci 107 (Pt. 2), 527–541. [DOI] [PubMed] [Google Scholar]
- Schönrich G, Krüger DH, Raftery MJ, 2015. Hantavirus-induced disruption of the endothelial barrier: neutrophils are on the payroll. Front. Microbiol 6, 222 10.3389/fmicb.2015.00222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senger DR, Galli SJ, Dvorak AM, Perruzzi CA, Harvey VS, Dvorak HF, 1983. Tumor cells secrete a vascular permeability factor that promotes accumulation of ascites fluid. Science 219, 983–985. 10.1126/science.6823562. [DOI] [PubMed] [Google Scholar]
- Senger DR, Perruzzi CA, Feder J, Dvorak HF, 1986. A highly conserved vascular permeability factor secreted by a variety of human and rodent tumor cell lines. Cancer Res 46, 5629–5632. [PubMed] [Google Scholar]
- Shafren DR, Bates RC, Agrez MV, Herd RL, Burns GF, Barry RD, 1995. Coxsackieviruses B1, B3, and B5 use decay accelerating factor as a receptor for cell attachment. J. Virol 69, 3873–3877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi X, Elliott RM, 2002. Golgi localization of Hantaan virus glycoproteins requires coexpression of G1 and G2. Virology 300, 31–38. 10.1006/viro.2002.1414. [DOI] [PubMed] [Google Scholar]
- Shim SH, Park M-S, Moon S, Park KS, Song J-W, Song K-J, Baek LJ, 2011. Comparison of innate immune responses to pathogenic and putative non-pathogenic hantaviruses In vitro. Virus Res 160, 367–373. 10.1016/j.virusres.2011.07.013. [DOI] [PubMed] [Google Scholar]
- Slough MM, Chandran K, Jangra RK, 2019. Two point mutations in old world hantavirus glycoproteins afford the generation of highly infectious recombinant vesicular stomatitis virus vectors. MBio 10, e02372–e02418. 10.1128/mBio.02372-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soldi R, Mitola S, Strasly M, Defilippi P, Tarone G, Bussolino F, 1999. Role of alphavbeta3 integrin in the activation of vascular endothelial growth factor receptor-2. EMBO J 18, 882–892. 10.1093/emboj/18.4.882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song J-W, Song K-J, Baek L-J, Frost B, Poncz M, Park K, 2005. In vivo characterization of the integrin beta3 as a receptor for Hantaan virus cellular entry. Exp. Mol. Med 37, 121–127. 10.1038/emm.2005.16. [DOI] [PubMed] [Google Scholar]
- Song JY, Woo HJ, Cheong HJ, Noh JY, Baek LJ, Kim WJ, 2016. Long-term immunogenicity and safety of inactivated Hantaan virus vaccine (Hantavax™) in healthy adults. Vaccine 34, 1289–1295. 10.1016/j.vaccine.2016.01.031. [DOI] [PubMed] [Google Scholar]
- Sotomayor M, Gaudet R, Corey DP, 2014. Sorting out a promiscuous superfamily: towards cadherin connectomics. Trends Cell Biol 24, 524–536. 10.1016/j.tcb.2014.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiropoulou CF, 2001. Hantavirus maturation. Curr. Top. Microbiol. Immunol 256, 33–46. [DOI] [PubMed] [Google Scholar]
- Spiropoulou CF, Albariño CG, Ksiazek TG, Rollin PE, 2007. Andes and Prospect Hill hantaviruses differ in early induction of interferon although both can downregulate interferon signaling. J. Virol 81, 2769–2776. 10.1128/JVI.02402-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiropoulou CF, Srikiatkhachorn A, 2013. The role of endothelial activation in dengue hemorrhagic fever and hantavirus pulmonary syndrome. Virulence 4, 525–536. 10.4161/viru.25569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiropoulou CF, Goldsmith CS, Shoemaker TR, Peters CJ, Compans RW, 2003. Sin Nombre virus glycoprotein trafficking. Virology 308, 48–63. 10.1016/S0042-6822(02)00092-2. [DOI] [PubMed] [Google Scholar]
- Su G, Atakilit A, Li JT, Wu N, Bhattacharya M, Zhu J, Shieh JE, Li E, Chen R, Sun S, Su CP, Sheppard D, 2012. Absence of integrin αvβ3 enhances vascular leak in mice by inhibiting endothelial cortical actin formation. Am. J. Respir. Crit. Care Med 185, 58–66. 10.1164/rccm.201108-1381OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suder E, Furuyama W, Feldmann H, Marzi A, de Wit E, 2018. The vesicular stomatitis virus-based Ebola virus vaccine: from concept to clinical trials. Hum. Vaccin. Immunother 14, 2107–2113. 10.1080/21645515.2018.1473698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tatsis N, Ertl HCJ, 2004. Adenoviruses as vaccine vectors. Mol. Ther 10, 616–629. 10.1016/j.ymthe.2004.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiley LS, Hagen M, Matthews JT, Krystal M, 1994. Sequence-specific binding of the influenza virus RNA polymerase to sequences located at the 5’ ends of the viral RNAs. J. Virol 68, 5108–5116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tischler ND, Gonzalez A, Perez-Acle T, Rosemblatt M, Valenzuela PDT, 2005. Hantavirus Gc glycoprotein: evidence for a class II fusion protein. J. Gen. Virol 86, 2937–2947. 10.1099/vir.0.81083-0. [DOI] [PubMed] [Google Scholar]
- Torriani G, Mayor J, Zimmer G, Kunz S, Rothenberger S, Engler O, 2019. Macropinocytosis contributes to hantavirus entry into human airway epithelial cells. Virology 531, 57–68. 10.1016/j.virol.2019.02.013. [DOI] [PubMed] [Google Scholar]
- Vaheri A, Strandin T, Hepojoki J, Sironen T, Henttonen H, Mäkelä S, Mustonen J, 2013. Uncovering the mysteries of hantavirus infections. Nat. Rev. Microbiol 11, 539–550. 10.1038/nrmicro3066. [DOI] [PubMed] [Google Scholar]
- Valdivieso F, Vial P, Ferres M, Ye C, Goade D, Cuiza A, Hjelle B, 2006. Neutralizing antibodies in survivors of Sin Nombre and Andes hantavirus infection. Emerg. Infect. Dis 12, 166–168. 10.3201/eid1201.050930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Agthoven JF, Xiong J-P, Alonso JL, Rui X, Adair BD, Goodman SL, Arnaout MA, 2014. Structural basis for pure antagonism of integrin αVβ3 by a high-affinity form of fibronectin. Nat. Struct. Mol. Biol 21, 383–388. 10.1038/nsmb.2797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vera-Otarola J, Solis L, Soto-Rifo R, Ricci EP, Pino K, Tischler ND, Ohlmann T, Darlix J-L, López-Lastra M, 2012. The Andes hantavirus NSs protein is expressed from the viral small mRNA by a leaky scanning mechanism. J. Virol 86, 2176–2187. 10.1128/JVI.06223-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vial PA, Valdivieso F, Calvo M, Rioseco ML, Riquelme R, Araneda A, Tomicic V, Graf J, Paredes L, Florenzano M, Bidart T, Cuiza A, Marco C, Hjelle B, Ye C, Hanfelt-Goade D, Vial C, Rivera JC, Delgado I, Mertz GJ, Hantavirus Study Group in Chile, 2015. A non-randomized multicentre trial of human immune plasma for treatment of hantavirus cardiopulmonary syndrome caused by Andes virus. Antivir. Ther 20, 377–386. 10.3851/IMP2875. [DOI] [PubMed] [Google Scholar]
- Voutilainen L, Sironen T, Tonteri E, Bäck AT, Razzauti M, Karlsson M, Wahlstrom M, Niemimaa J, Henttonen H, Lundkvist Å, 2015. Life-long shedding of Puumala hantavirus in wild bank voles (Myodes glareolus). J. Gen. Virol 96, 1238–1247. 10.1099/vir.0.000076. [DOI] [PubMed] [Google Scholar]
- Wang H, Alminaite A, Vaheri A, Plyusnin A, 2010. Interaction between hantaviral nucleocapsid protein and the cytoplasmic tail of surface glycoprotein Gn. Virus Res 151, 205–212. 10.1016/j.virusres.2010.05.008. [DOI] [PubMed] [Google Scholar]
- Watkins NA, Smethurst PA, Allen D, Smith GA, Ouwehand WH, 2002. Platelet alphaIIbbeta3 recombinant autoantibodies from the B-cell repertoire of a post-transfusion purpura patient. Br. J. Haematol 116, 677–685. [DOI] [PubMed] [Google Scholar]
- Watson DC, Sargianou M, Papa A, Chra P, Starakis I, Panos G, 2014. Epidemiology of Hantavirus infections in humans: a comprehensive, global overview. Crit. Rev. Microbiol 40, 261–272. 10.3109/1040841X.2013.783555. [DOI] [PubMed] [Google Scholar]
- Wertz GW, Whelan S, LeGrone A, Ball LA, 1994. Extent of terminal complementarity modulates the balance between transcription and replication of vesicular stomatitis virus RNA. Proc. Natl. Acad. Sci. U. S. A 91, 8587–8591. 10.1073/pnas.91.18.8587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickham TJ, Mathias P, Cheresh DA, Nemerow GR, 1993. Integrins αvβ3 and αvβ5 promote adenovirus internalization but not virus attachment. Cell 73, 309–319. 10.1016/0092-8674(93)90231-E. [DOI] [PubMed] [Google Scholar]
- Willensky S, Bar-Rogovsky H, Bignon EA, Tischler ND, Modis Y, Dessau M, 2016. Crystal structure of glycoprotein C from a Hantavirus in the post-fusion conformation. PLoS Pathog 12, e1005948 10.1371/journal.ppat.1005948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkowski PT, Drexler JF, Kallies R, Ličková M, Bokorová S, Mananga GD, Szemes T, Leroy EM, Krüger DH, Drosten C, Klempa B, 2016. Phylogenetic analysis of a newfound bat-borne hantavirus supports a laurasiatherian host association for ancestral mammalian hantaviruses. Infect. Genet. Evol 41, 113–119. 10.1016/j.meegid.2016.03.036. [DOI] [PubMed] [Google Scholar]
- Witkowski PT, Perley CC, Brocato RL, Hooper JW, Jürgensen C, Schulzke J-D, Krüger DH, Bücker R, 2017. Gastrointestinal tract as entry route for hantavirus infection. Front. Microbiol 8, 1721 10.3389/fmicb.2017.01721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong JP, Stehle T, Diefenbach B, Zhang R, Dunker R, Scott DL, Joachimiak A, Goodman SL, Arnaout MA, 2001. Crystal structure of the extracellular segment of integrin alpha Vbeta3. Science 294, 339–345. 10.1126/science.1064535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J-P, Stehle T, Zhang R, Joachimiak A, Frech M, Goodman SL, Arnaout MA, 2002. Crystal structure of the extracellular segment of integrin alpha Vbeta3 in complex with an Arg-Gly-Asp ligand. Science 296, 151–155. 10.1126/science.1069040. [DOI] [PubMed] [Google Scholar]
- Yamanishi K, Tanishita O, Tamura M, Asada H, Kondo K, Takagi M, Yoshida I, Konobe T, Fukai K, 1988. Development of inactivated vaccine against virus causing haemorrhagic fever with renal syndrome. Vaccine 6, 278–282. [DOI] [PubMed] [Google Scholar]
- Yanagihara R, Amyx HL, Gajdusek DC, 1985. Experimental infection with Puumala virus, the etiologic agent of nephropathia epidemica, in bank voles (Clethrionomys glareolus). J. Virol 55, 34–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanagihara R, Gu SH, Arai S, Kang HJ, Song J-W, 2014. Hantaviruses: rediscovery and new beginnings. Virus Res 187, 6–14. 10.1016/j.virusres.2013.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu L, Bai W, Wu X, Zhang L, Zhang L, Li P, Wang F, Liu Z, Zhang F, Xu Z, 2013. A recombinant pseudotyped lentivirus expressing the envelope glycoprotein of hantaan virus induced protective immunity in mice. Virol. J 10, 301 10.1186/1743-422X-10-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan Z-G, Li X-M, Mahmmod YS, Wang X-H, Xu H-J, Zhang X-X, 2009. A single immunization with a recombinant canine adenovirus type 2 expressing the seoul virus Gn glycoprotein confers protective immunity against seoul virus in mice. Vaccine 27, 5247–5251. 10.1016/j.vaccine.2009.06.062. [DOI] [PubMed] [Google Scholar]
- Zaitseva E, Yang S-T, Melikov K, Pourmal S, Chernomordik LV, 2010. Dengue virus ensures its fusion in late endosomes using compartment-specific lipids. PLoS Pathog 6, e1001131 10.1371/journal.ppat.1001131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaki SR, Greer PW, Coffield LM, Goldsmith CS, Nolte KB, Foucar K, Feddersen RM, Zumwalt RE, Miller GL, Khan AS, 1995. Hantavirus pulmonary syndrome. Pathogenesis of an emerging infectious disease. Am. J. Pathol 146, 552–579. [PMC free article] [PubMed] [Google Scholar]
- Zhang Y-Z, 2014. Discovery of hantaviruses in bats and insectivores and the evolution of the genus Hantavirus. Virus Res 187, 15–21. 10.1016/j.virusres.2013.12.035. [DOI] [PubMed] [Google Scholar]