Abstract
Objective:
The Course and Outcome of Bipolar Youth study (Birmaher and colleagues) found that children and adolescents with bipolar spectrum disorders followed one of four distinct mood trajectories over 8 years of follow-up, with as many as 25% showing a predominantly euthymic course. We evaluated whether similar patterns of illness course are observed in adolescents with bipolar I and II disorder who participated in a 2-year clinical trial.
Method:
144 adolescents with bipolar I or II disorder, identified shortly after a mood episode, were assessed over a 2-year period. Participants were randomly assigned to one of two psychosocial family treatments during the first 9 months of the study, and pharmacotherapy was provided throughout the two years. Using latent class growth analyses (LCGA), we classified participants into distinct courses of illness based on mood ratings collected over the two years. We examined demographic and illness variables as predictors of these course classifications.
Results:
LCGA indicated four mood trajectories: “predominantly euthymic” (29.9% of sample), “ill with significantly improving course” (11.1%), “moderately euthymic” (26.4%), and “ill with moderately improving course” (32.6%). Adolescents in these classes were euthymic 77.7%, 53.6%, 44.1%, and 18.6% of the weeks of follow-up, respectively. Psychosocial treatment condition and baseline medication exposure were not associated with trajectories. However, youth with more severe baseline depressive symptoms, suicidality, lower quality of life scores, and minority race had more symptomatic courses of illness over time.
Conclusion:
A substantial proportion (25%-30%) of youth with bipolar I or II disorder maintain euthymic states over extended periods of follow-up. Identifying youth who are more and less likely to remain stable over time may help guide psychosocial and pharmacological treatments after an illness episode.
Keywords: latent class growth analysis, quality of life, early-onset, euthymic, recovery
Introduction
Individuals who develop bipolar disorder (BD) typically experience their first mood symptoms in childhood or adolescence, and 60-70% have initial onset before age 18.1 Following recovery from a mood episode, up to 80% of youth with BD experience a mood recurrence within the next 3-5 years,2-4 and subsyndromal or syndromal mood symptoms (particularly depression or mixed symptoms) characterize up to 60% of follow-up periods.5 Despite a commonly chronic course of mood symptoms, however, the length of symptomatic and asymptomatic periods are highly variable across patients.6-8
Historical accounts of BD from the pre-pharmacological era indicated that a proportion of patients have extended periods – even decades – without major mood recurrences.9 More recently, longitudinal studies have found that 15-30% of adults and youth with BD maintain states of recovery over 3-5 year periods.2-5,7,8 To account for a portion of this heterogeneity, developmental subtypes of BD have been proposed.10,11 For example, patients with early ages of onset (i.e., <18 years) may form a subgroup that experiences more severe mood symptoms, rapid cycling and fewer periods of remission over time.12,13
To our knowledge, only one study has distinguished course subtypes based on prospective data in pediatric BD. In a sample of youth with BD I, II and not otherwise specified (NOS), the Course and Outcome of Bipolar Youth (COBY) study examined the naturalistic course of mood symptoms over 8 years, with trajectories based on the amount of time youth spent in euthymic states.14 Using latent classification analysis, they observed four distinct course trajectories: “predominantly ill,” “ill with improving course,” “moderately euthymic,” and “predominantly euthymic.” Earlier age of onset, more severe baseline mood symptoms, suicidality, sexual abuse, and family history of BD and substance abuse were associated with poorer courses of illness. Twenty-four percent of adolescents were predominantly euthymic throughout the 8-year study and 19% achieved and maintained euthymic status over the final years of follow-up. Thus, a significant proportion (42%) of early-onset patients with BD have extended periods of recovery.
It is unclear whether the trajectories found in COBY replicate in other pediatric BD samples. In this study, we used the same assessment measures and procedures as in COBY, and examined whether distinct courses of illness could be identified in an older group of adolescents with bipolar I or II disorder followed over 2 years. Unlike the COBY sample, the participants were patients in a 9-month randomized trial of family-focused treatment or a brief educational control treatment who were then followed for an additional 15 months. Pharmacotherapy was provided by study psychiatrists who followed treatment guidelines for childhood BD.15 Using latent class growth modeling, we identified classes of mood trajectories over the two-year study. We then examined the association between specific demographic, longitudinal mood symptoms, and clinical variables measured at baseline and class membership. Following from the COBY findings, we expected four classes of illness course to best fit the data. We also hypothesized that earlier age of onset, more severe baseline symptoms, suicidality at baseline, a family history of BD, and lower quality of life scores at baseline would be associated with poorer courses of illness.
Method
The study enrolled adolescents between the ages of 12 years, 0 months and 18 years, 1 month. Eligibility criteria included: a DSM-IV-TR diagnosis of bipolar I or II disorder; a hypomanic, manic or mixed episode of at least 1 week’s duration or a major depressive episode of at least 2 weeks duration within the 3 months prior to randomization; mood symptoms of at least moderate severity (≥17 on the Kiddie Schedule for Affective Disorders and Schizophrenia Mania Rating Scale (KMRS)16 or ≥16 on the K-SADS Depression Rating Scale (KDRS)17) for at least 1-2 weeks during the previous month; willingness to engage in pharmacotherapy with a study psychiatrist; and at least one caregiver willing to participate in family treatment. The cut points on the KMRS and KDRS represent clinically significant levels of symptom severity.18 Participants with a current substance abuse disorder or pervasive developmental disorder were excluded.
The study was conducted at three university centers - University of Colorado, Boulder, the University of Pittsburgh School of Medicine, and the Cincinnati Children’s Hospital Medical Center. Participants were randomized to 21 sessions of family-focused therapy for adolescents (FFT-A) over 9 months, consisting of psychoeducation, communication enhancement training, and problem-solving skills training; or 3 weekly sessions of family psychoeducation (enhanced care, or EC). Participants received pharmacotherapy from a study psychiatrist for the duration of involvement in the study. Study outcome assessments were conducted by an examiner who was unaware of psychosocial treatment conditions. Assessments occurred at a pretreatment baseline (covering the 3 months prior to randomization) and at months 3, 6, 9, 12, 18, and 24 following randomization. Participation throughout the study was not contingent upon trial involvement; all participants who entered the study were actively encouraged to continue in the follow-up even if they did not complete their psychosocial treatment.
At baseline, adolescents were interviewed about current and lifetime psychiatric disorders using the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS).19 One primary parent/caregiver was interviewed separately about the adolescent using the K-SADS, with final K-SADS scores based on a consensus between adolescent and parent/caregiver reports. The KMRS and KDRS were used in place of the K-SADS mood module, enabling examiners to rate symptoms on 6- or 7-point scales of severity and impairment. The K-SADS assessed the most symptomatic 1-2-week(s) period in the past month (baseline rating) as well as the most symptomatic period in the patient’s lifetime. Additionally, the K-SADS interviewer obtained the age of first onset of mood symptoms that affected functioning, ages of first major depressive episode and first manic or hypomanic episodes, the number of lifetime depressive and (hypomanic) episodes, suicidal ideation, and the number of hospitalizations.
The Adolescent Longitudinal Interval Follow-Up Evaluation (A-LIFE) was administered at each follow-up point. Weekly Psychiatric Status Ratings (PSRs) of depression, mania, and hypomania quantified the severity of and impairment caused by symptoms over the course of the 24-month study. 20 Data were collected from the patient and primary caregiver separately, with final ratings made based on a consensus between the reports. To help improve the adolescents’ and parents’ memory for retrospective moods changes, participants were provided with a calendar and asked to use “landmark events” (e.g., birthday, holidays, start of an academic year) to trace mood states over week-to-week intervals. PSR scores ≤ 2 were used to indicate euthymic mood, 3-4 to indicate subsyndromal symptoms, and ≥ 5 to indicate syndromal symptoms that would meet DSM-5 criteria for a depressive or manic/hypomanic episode. Time to recovery was calculated as the number of weeks from randomization until weekly PSR depression, mania, and hypomania ratings were ≤ 2 for at least 8 weeks. Time to recurrence was calculated as weeks from the point of recovery to the point where the patient had a PSR score of ≥ 5 for at least 1 week for (hypo)mania or 2 weeks for depression.
Assessments with the K-SADS and A-LIFE were conducted by trained masters/doctoral-level research staff. Reliabilities (intraclass correlations), calculated across 11 raters at the 3 sites, averaged 0.89 for the KDRS scores, 0.81 for KMRS scores, and 0.74 for the 1-6 depression and (hypo)mania PSR scales.
Socioeconomic status (SES) was gathered using the Hollingshead Scale.21 A family history of psychiatric diagnoses in first-degree relatives of the adolescent was assessed using the Family History Screen.22 Expressed emotion (EE), a measure of critical, hostile, or emotionally overinvolved attitudes in parents, was assessed using the Five-Minute Speech Sample.23 Adolescents and parents also completed the Kiddo-KINDL-R Questionnaire (KINDL), a 24-item self-report scale measuring the child’s quality of life and well-being in the domains of physical, emotional, self-esteem, social, family, and school functioning.24 Parent and adolescent scores on this scale were significantly correlated (Pearson rs ranging from .22 to .45, ps<0.05). To reduce the number of comparisons, parent and adolescent scores were averaged.
Statistical Analyses
Week-by-week PSR scores were aggregated for each assessment point to create total mood scores at baseline, 3, 6, 9, and 12 months (covering the prior 3 months), and 18 and 24-months (covering the prior 6 months). Following the methods of COBY,1 the percentage of weeks that participants were euthymic (PSR ≤ 2) during each assessment interval was calculated. Using latent class growth modeling in Mplus,25,26 classes of euthymic mood trajectories were modeled starting from one class and sequentially testing the model fit of adding an additional class. Full information maximum likelihood (the default in Mplus) was used to handle missing data, which uses all available data in the model to estimate parameters and assigns each participant with any available data a class membership. The final number of classes for the latent class growth analysis was determined by (1) successful convergence of the model (i.e., the statistical program arriving at a replicable and stable model), (2) a significant value derived from Mplus’ bootstrap likelihood ratio test (BLRT), and (3) clinical interpretability of the classes. The BLRT tests whether the current model’s fit is significantly improved from the previous model, and has been identified as the best fit index for latent class growth modeling in Mplus.27
Once a final model was derived, the class assignment for each participant was extracted. Using univariate analyses of variance and chi-square tests, we compared classes on baseline demographic and family variables (i.e., age, sex, race, SES, parental history of BD, and parental EE) as well as treatment and longitudinal course variables (i.e., psychosocial treatment condition, recruitment site, duration of follow-up, percentage of time with at least subthreshold PSR symptoms, and mean PSR mood symptom ratings). Survival analyses by the Kaplan-Meier method were used to compare classes on weeks to recovery from randomization until recovery from the index mood episode (censored for patients who did not recover) and weeks to relapse following recovery (censored for patients who recovered but did not relapse over the study period). Second, classes were compared on baseline K-SADS mood, ages of onset (i.e., first mood symptoms that affected functioning, ages of first depressive and (hypo)manic episodes, number of lifetime mood episodes, number of hospitalizations, weeks until mood episode recovery, weeks until a mood relapse following initial recovery, comorbid psychiatric disorders, baseline medication exposure, and quality of life.
Results
A total of 447 individuals were screened for eligibility, of which 168 were deemed ineligible based on a phone screen, 70 declined to participate, and 209 were invited for a full intake assessment; of these 209, 145 were randomized to treatments. Baseline mood data were available for 144 participants, 76 of whom had bipolar I disorder and 68 of whom had bipolar II disorder. For the follow-up, data were available on 111 participants at 3 months, 108 at 6 months, 89 at 9 months, 91 at 12 months, 76 at 18 months and 74 at 24 months. Participants were followed for an average of 82.7 weeks (SD=33.9). The mean age at baseline was 15.6 years (SD=1.4); 54.9% were female, 16.7% were non-White, and 8.3% were Hispanic. The mean Hollingshead SES score was 3.7 (SD=1.2), indicating middle-to-upper educational and occupational status. All participants entered the study with active (subsyndromal or syndromal) mood symptoms. Of the 144, 37 (25.5%) entered in a bipolar I or II depressive episode, 71 (49.7%) in a manic or hypomanic episode, and 36 (24.8%) in a mixed or subthreshold mixed episode. Further details on the design, CONSORT information, sample, and treatment outcomes can be found in a prior publication on this trial.18
Latent Class Growth Analyses
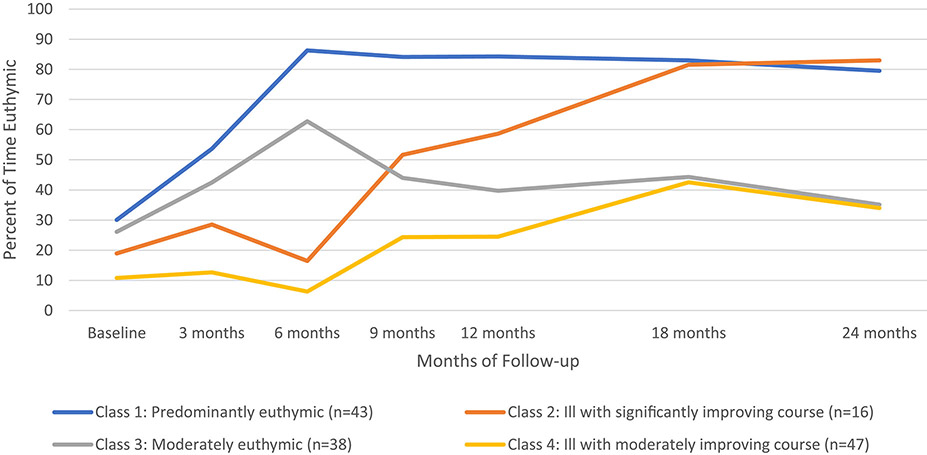
When examining the aggregated week-by-week PSR scores over the two-year study, a four-class model best fit the data (see Figure 1 for trajectories of euthymic mood). The BLRTs showed a significant log-likelihood difference for the two-class model (log-likelihood difference=98.25; p<0.001), the three-class model (log-likelihood difference=37.67; p<0.001), and the four-class model (log-likelihood difference=15.10; p=0.01), indicating a significantly better fit for each successive model. A five-class model would not converge despite attempts to increase start values and iterations.
Figure 1.
Percent Time Spent Euthymic Among Adolescents With Bipolar Disorder Over 2 Years
Class 1 (“predominantly euthymic”; n=43, 29.9%) consisted of participants who improved within the first 6 months following the index study episode to a mostly euthymic state, and consistently maintained euthymic mood throughout the remaining follow-up period. Class 2 (“ill with significantly improving course”; n=16, 11.1%) indicated participants who were symptomatic without improvement over the first 6 months following the index episode, followed by significant improvement over the next year, and maintaining mostly euthymic mood through the last 6 months of follow-up. Participants in class 3 (“moderately euthymic”; n=38, 26.4%) showed initial improvement in the first six months, but then had a return of symptoms that persisted for the remainder of follow-up. Finally, class 4 (“ill with moderately improving course”; n=47, 32.6%) indicated participants who started with a high level of symptoms, had a poor course over the first 12 months and improved only to a moderately euthymic level by 18 months. Within classes, participants spent 77.7%, 53.6%, 44.1%, and 18.6% percent of the follow-up weeks in euthymic states, respectively. Classes 1, 2 and 4 all showed significant improvements in euthymic mood from baseline to 24-months (ps<0.05).
Demographic Variables as Predictors of Class Membership
Demographic variables as they relate to class membership are presented in Table 1. Age at baseline, SES, gender, ethnicity, history of mood disorders in biological parents, and parental EE did not relate to class assignment. However, race did relate to class assignment: the group who were ill with a moderately improving course (class 4) consisted of more nonwhite patients relative to adolescents who were predominantly euthymic (class 1) and adolescents who were moderately euthymic (class 3).
Table 1.
Demographics and Longitudinal Clinical Characteristics by Class Assignment
| Class 1: Predominantly euthymic (n=43) |
Class 2: Ill with significantly improving course (n=16) |
Class 3: Moderately euthymic (n=38) |
Class 4: Ill with moderately improving course (n=47) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Demographics | |||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | p | |
| Age (years) | 15.8 | 1.5 | 15.5 | 1.3 | 15.5 | 1.5 | 15.6 | 1.4 | 0.8 |
| Hollingshead SES | 3.7 | 1.2 | 3.3 | 1.1 | 3.7 | 1.2 | 3.7 | 1.3 | 0.7 |
| N | % | N | % | N | % | N | % | p | |
| Female Participants | 20 | 46.5 | 8 | 50.0 | 25 | 65.8 | 26 | 55.3 | 0.4 |
| Nonwhite Participants | 5 | 11. 6a | 2 | 12.5a,b | 3 | 7.9a | 14 | 29.7b | 0.03 |
| Hispanic Participants | 4 | 9.3 | 1 | 6.3 | 3 | 7.9 | 4 | 8.5 | 1.0 |
| Bio Parent Mood Hx | |||||||||
| Depressive episode | 19 | 44.1 | 8 | 50.0 | 19 | 50.0 | 17 | 36.2 | 0.6 |
| (Hypo)manic episode | 11 | 25.6 | 3 | 18.8 | 7 | 18.4 | 11 | 23.4 | 0.9 |
| High Baseline Caregiver EE | 16 | 37.2 | 5 | 31.3 | 12 | 31.6 | 17 | 36.2 | 0.7 |
| Longitudinal Clinical Characteristics | |||||||||
| N | % | N | % | N | % | N | % | p | |
| Randomized to FFT | 18 | 41.9 | 9 | 56.3 | 17 | 44.7 | 28 | 59.6 | 0.3 |
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | p | |
| Weeks of follow-up | 86.4 | 30.9 | 84.4 | 34.7 | 86.4 | 32.8 | 73.8 | 37.5 | 0.4 |
| Psychotherapy visits during study | 9.1 | 9.4 | 11.7 | 8.7 | 11.1 | 11.3 | 8.8 | 9.6 | 0.6 |
| Medication visits during study | 10.5 | 7.1 | 13.4 | 6.7 | 11.3 | 7.6 | 8.6 | 7.6 | 0.1 |
| Longitudinal Mean PSR: | |||||||||
| Depressive symptoms | 1.7a | 0.4 | 2.1b | 0.5 | 2.4b | 0.6 | 3.1c | 0.7 | <0.001 |
| (Hypo)manic symptoms | 1.5a | 0.5 | 1.7a,b | 0.5 | 1.9b | 0.6 | 2.2c | 0.7 | <0.001 |
| Survival Analyses | |||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | p | |
| Weeks to Recovery | 20.1a | 12.6 | 38.0b | 14.1 | 50.4b | 33.5 | 80.5c | 20.9 | <0.001 |
| N | % | N | % | N | % | N | % | ||
| Recovered from baseline mood episode | 36 | 83.7 | 13 | 81.3 | 25 | 65.8 | 13 | 27.7 | |
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | p | |
| Weeks to Relapse Post-Recovery | 75.6a | 29.2 | 63.1a | 33.6 | 28.3b | 27.5 | 23.5b | 19.2 | <0.001 |
| N | % | N | % | N | % | N | % | ||
| Relapse post-recovery / Recovered from mood episode | 14 | 38.9 | 6 | 46.2 | 21 | 84.0 | 9 | 69.2 | |
Note: Each superscript letter within a row denotes classes whose column proportions or means do not significantly differ from each other at the p < .05 level. Bio Parent Mood Hx = biological parent mood history; EE = Expressed Emotion; PSR = Psychiatric Scale Rating; SES = socioeconomic status
Treatment and Longitudinal Mood Symptoms
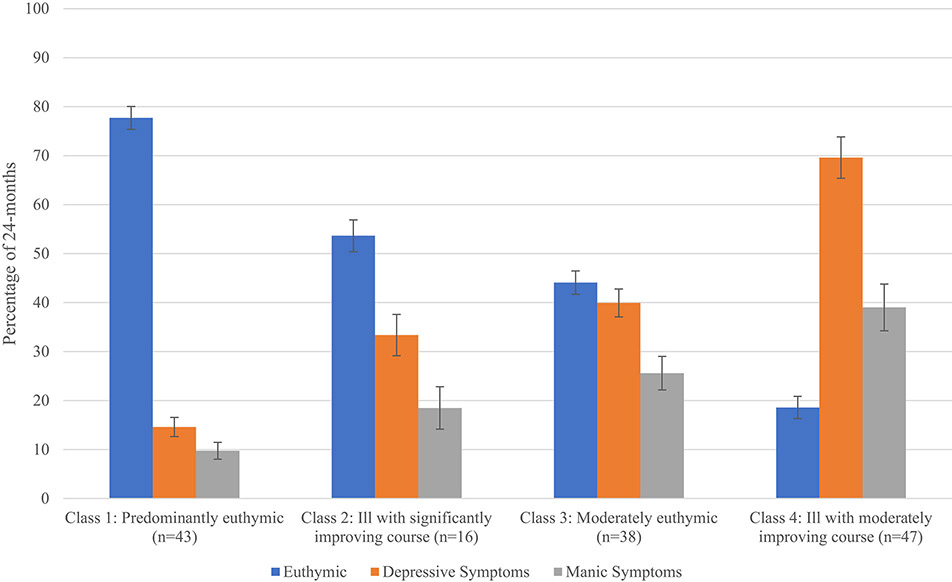
As shown in Table 1, neither psychosocial treatment assignment nor number of psychotherapy sessions obtained during the study predicted membership in the four longitudinal course classes. Class membership also did not relate to study site or weeks of follow-up. As expected, adolescents in class 4 had fewer weeks euthymic, a greater percentage of weeks with depressive and (hypo)manic symptoms, and had the greatest number of weeks to recovery from the index mood episode compared to all other classes (see Figure 2). They also had higher total mean PSR (hypo)mania and depression scores over the 2-year study than the other three classes (see Table 1). Conversely, adolescents in class 1 recovered from the index mood episode in fewer weeks, had a higher percentage of time euthymic, a lower percentage of time with depressive or (hypo)manic symptoms, and lower 2-year mean PSR depressive and (hypo)manic severity scores compared to adolescents in the other classes. Additionally, after recovering from the index episode, classes 1 and 2 remained in recovery for more weeks prior to the next mood episode compared to classes 3 and 4 (see Table 1 for weekly recovery and recurrence values).
Figure 2.
Total Percentage of Time Euthymic With Depressive and Manic Symptoms Over 2-Years by Class
Note: Error bars indicate the standard error of the mean.
Baseline Illness Variables
Baseline illness variables stratified by class designation are presented in Table 2. Adolescents in class 1 had less severe baseline depressive symptoms (average weekly rating for the 12 weeks prior to random assignment) than adolescents who were in classes 3 and 4. Adolescents in class 2 also had less severe baseline depressive symptoms compared to adolescents in class 4. Additionally, adolescents in classes 1 and 2 had a lower proportion of adolescents with suicidal ideation at baseline compared to adolescents in class 4. There were no differences between classes in the severity of baseline (hypo)manic symptoms. There were also no differences in age of onset for mood symptoms or mood episodes, number of lifetime mood episodes or number of prior hospitalizations, nor were there differences in proportion of patients in each group with bipolar I versus II disorder, depressive vs. manic vs. mixed baseline polarities, comorbid psychiatric disorders (including combined ADHD-ODD; χ2(3)=1.65, p=0.65), or parental EE.
Table 2.
Baseline Illness Variables Based on Class Assignment
| Class 1: Predominantly euthymic (n=43) |
Class 2: Ill with significantly improving course (n=16) |
Class 3: Moderately euthymic (n=38) |
Class 4: Ill with moderately improving course (n=47) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | p | |
| KDRS | 21.7a | 11.9 | 23.1a,b | 8.6 | 26.3b,c | 11.3 | 29.2c | 10.3 | 0.007 |
| KMRS | 29.0 | 10.3 | 24.2 | 11.8 | 28.9 | 12.2 | 29.5 | 11.3 | 0.4 |
| Age of onset of any mood symptoms | 11.8 | 3.1 | 11.3 | 3.1 | 10.6 | 3.9 | 11.3 | 2.8 | 0.5 |
| Age of onset of MDE | 13.8 | 2.1 | 13.9 | 1.3 | 13.9 | 2.6 | 13.2 | 2.7 | 0.7 |
| Age of onset of H/ME | 14.1 | 2.5 | 13.7 | 2.7 | 13.8 | 3.0 | 13.5 | 2.8 | 0.8 |
| Prior number of hospitalizations | 1.5 | 3.1 | 1.2 | 1.6 | 0.9 | 1.2 | 1.3 | 2.0 | 0.7 |
| Prior number of MDE | 6.8 | 17.2 | 6.5 | 12.8 | 5.3 | 8.4 | 4.2 | 4.2 | 0.7 |
| Prior number of HME | 9.4 | 14.2 | 14.6 | 22.7 | 15.1 | 21.6 | 8.7 | 8.3 | 0.3 |
| N | % | N | % | N | % | N | % | p | |
| Bipolar I Disorder | 23 | 53.4 | 9 | 56.3 | 20 | 52.6 | 24 | 51.1 | 1.0 |
| Suicidal Ideation | 14 | 32.6a | 4 | 25.0a | 13 | 34.2a,b | 27 | 57.4b | 0.05 |
| Baseline Polarity | 0.1 | ||||||||
| Manic | 15 | 34.9 | 6 | 37.5 | 7 | 18.4 | 8 | 17.0 | |
| Hypomanic | 8 | 18.6 | 3 | 18.8 | 14 | 36.8 | 10 | 27.0 | |
| Depressive | 8 | 18.6 | 6 | 37.5 | 9 | 23.7 | 14 | 29.7 | |
| Mixed | 12 | 27.9 | 1 | 6.3 | 8 | 21.1 | 15 | 31.9 | |
| Comorbid Disorders | |||||||||
| Anxiety Disorder | 14 | 32.6 | 5 | 31.2 | 18 | 47.4 | 20 | 42.6 | 0.5 |
| ADHD | 14 | 32.6 | 6 | 37.5 | 11 | 28.9 | 17 | 36.2 | 0.9 |
| Conduct Disorder | 2 | 4.7 | 1 | 6.3 | 4 | 10.5 | 1 | 2.1 | 0.4 |
| ODD | 11 | 25.6 | 3 | 18.8 | 8 | 21.1 | 13 | 27.7 | 0.8 |
| Medications | |||||||||
| Any psychotropic | 38 | 88.4 | 14 | 87.5 | 33 | 86.8 | 36 | 76.6 | 0.4 |
| Antipsychotic | 28 | 65.1a,b | 8 | 50.0a | 30 | 78.9b | 25 | 53.2a | 0.06 |
| Antidepressant | 7 | 16.3 | 4 | 25.0 | 10 | 26.3 | 6 | 12.8 | 0.4 |
| Mood stabilizer | 31 | 72.1 | 10 | 62.5 | 31 | 81.6 | 31 | 66.0 | 0.4 |
| Lithium | 7 | 16.3 | 2 | 12.5 | 3 | 7.9 | 12 | 25.5 | 0.2 |
| Stimulant | 6 | 14.0 | 2 | 12.5 | 6 | 15.8 | 5 | 10.6 | 0.9 |
Note: Each superscript letter within a row denotes classes whose column proportions or means do not significantly differ from each other at the p<0.05 level. ADHD = attention-deficit/hyperactivity disorder; H/ME = hypomanic or manic episode; KDRS = K-SADS Depressive Rating Scale; KMRS = K-SADS Mania Rating Scale; MDE = major depressive episode; ODD = oppositional defiant disorder.
Baseline medication exposure (i.e., any psychotropic exposure, antipsychotic, antidepressant, mood stabilizer, and stimulant medication) was compared by class. Adolescents in class 3 were marginally more likely to be prescribed antipsychotics compared to adolescents in class 2 and class 4, but not class 1 (see Table 2). There were no other differences among course classifications in baseline medication exposure.
Quality of Life
Adolescents’ quality of life at baseline (averaging adolescent and parent reports) significantly predicted class membership (see Table 3). In the total score and across four of the six KINDL subscales, adolescents in classes 1 and 2 reported higher quality of life scores than adolescents in class 4. Class 1 adolescents also had higher KINDL subscale scores (except for family well-being) compared to class 3. Interestingly, adolescents in class 2 (ill with significantly improving course) had the highest baseline family well-being scores compared to adolescents of every other class, and had greater school well-being scores compared to adolescents in classes 3 and 4. Differences between course classifications in quality of life remained significant when controlling for baseline K-SADS depression severity, with the exception of physical well-being, which no longer differed across classes. Additionally, class membership related to quality of life over time, such that classes 1 and 2 had greater KINDL scores compared to classes 3 and 4 at the 24-month follow-up even when controlling for baseline KINDL scores (F(3,53)=2.96, p=0.04).
Table 3.
Quality of Life (KINDL) by Class Assignment
| Class 1: Predominantly euthymic (n=43) |
Class 2: Ill with significantly improving course (n=16) |
Class 3: Moderately euthymic (n=38) |
Class 4: Ill with moderately improving course (n=47) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | p | |
| KINDL-total-100 | 60.3a | 16.2 | 62.9a | 17.0 | 49.0b | 15.4 | 45.1b | 14.8 | <0.001 |
| KINDL-physical-100 | 65.1a | 17.3 | 56.7a,b | 21.6 | 54.5b | 21.1 | 53.2b | 21.1 | 0.04 |
| KINDL-emotional-100 | 64.5a | 23.1 | 63.4a,b | 24.6 | 53.7b,c | 24.1 | 46.7c | 21.6 | 0.003 |
| KINDL-self-esteem-100 | 50.0a | 22.6 | 52.2a | 30.7 | 35.0b | 23.2 | 30.2b | 22.8 | <0.001 |
| KINDL-family-100 | 61.3b | 26.1 | 76.8a | 15.2 | 53.1b,c | 22.7 | 49.5c | 25.0 | 0.002 |
| KINDL-friends-100 | 68.1a | 22.9 | 68.3a | 20.9 | 54.4b | 21.5 | 49.5b | 23.7 | 0.001 |
| KINDL-school-100 | 51.9a,b | 19.8 | 60.3a | 25.4 | 43.0b | 22.8 | 44.1b | 18.8 | 0.03 |
Note: Each superscript letter within a row denotes classes whose means do not significantly differ from each other at the p <.05 level. All scores were transformed to a range of 0 - 100 for ease of interpretation, with 0 being the lowest quality of life and 100 being the highest. As reference values, the KINDL manual presents total quality of life scores of 70.78 (SD = 10.01) for healthy boys and 73.54 (SD = 8.83) for healthy girls (N = 583 adolescents 14 – 17 years old; scores transformed to a base of 100).22
Discussion
This study identified four distinct mood trajectories of adolescent bipolar I and II disorder based on the amount of time adolescents spent in euthymic states. The most favorable course pattern, predominantly euthymic (class 1), was identified in 29.9% of adolescents; these patients were euthymic 77.7% of the time over an average of 86.4 weeks of follow-up. On the other end of the spectrum were 32.6% of adolescents who were ill with moderately improving course (class 4) and had the lowest percentage of time euthymic (18.6% of the follow-up). Between these two courses of illness were 11.1% of adolescents who were ill with significantly improving course (class 2) and 26.4% who were moderately euthymic (class 3) and spent 53.3% and 44.1% of the study period in euthymic states, respectively.
Despite methodological differences and a shorter period of follow-up, identifying these four distinct trajectories replicates findings from the COBY study,14 and provides further evidence of a more positive prognosis of pediatric bipolar illness than is often considered. While the disorder can be chronic and debilitating for periods of time, a substantial number of adolescents in this study (29.9% to 41%) recovered within 6 months after an episode and maintained mostly euthymic mood for up to 18 months. In the COBY study, between 24.0% and 43.1% recovered and became mostly euthymic over an 8-year period.
We used assessments batteries and metrics for determining euthymic mood that were identical to those of the COBY study. However, there were a number of study differences. The COBY study used a naturalistic design to track participants over an 8-year period. COBY included a wider range of the BD spectrum, including individuals with BD NOS. Additionally, participants in COBY began the study in early adolescence (mean age of 13.6 years). In contrast, the present study used structured treatment protocols (FFT-A or enhanced care in conjunction with study-based pharmacotherapy) and followed adolescents (mean age of 15.6 years) for a maximum of two years. Compared to the COBY study,14 it is possible that the earlier improvement was due to the active and structured psychotherapy and psychopharmacology protocols offered in this study. Additionally, exclusion of youth with substance disorders may have played a role in the earlier improvements; however, it is notable that we observed the same course trajectories as the COBY investigation despite these protocol differences.
Greater baseline depressive severity and suicidal ideation were associated with less favorable course designations. Several longitudinal studies have found that depression severity predicts poorer outcomes in bipolar disorder to a greater extent than manic symptoms.2,6,14,28-30 Manic symptoms, especially at a syndromal level, have been shown to be less frequent in the course of pediatric bipolar illness, possibly because manic symptoms are more responsive to pharmacological treatment than depressive symptoms.31,32 Previous work in adults with major depressive disorder has found that when patients are not treated to remission, they are more likely to relapse and have a decreased likelihood of remission in later treatment.33 Together, these findings highlight the importance of treating depression to remission in adolescents following a mood episode.
Greater baseline quality of life was a strong predictor of a more favorable course of illness, even after controlling baseline depression severity. Quality of life continued to relate to the symptomatic course of illness at the end of the two-year follow-up. These findings are consistent with previous research that has found quality of life to be linked to symptomatic outcomes among youth and adults with bipolar illness.34-36 Higher self-reported quality of life may be indicative of social adeptness and better premorbid adjustment, which is a well-established predictor of symptomatic outcome in bipolar disorder and schizophrenia.37-39 Further, in adults with BD, the presence of social supports affects the course of depressive symptoms more than the course of manic symptoms.40
The family and school quality of life subscales distinguished adolescents in class 2, as these youth were reported to have better family relationships than youth in the other classes and better school functioning compared to adolescents with poorer illness courses. Previous work has found that conflictual family environments and low maternal warmth are predictive of recurrence in bipolar adults and youth.4,41-43 This study extends these findings to suggest that adolescents’ perceptions of a positive family environment may serve as a buffer against worsening mood symptoms and may contribute to a more favorable course of illness over time. Alternatively, families with higher quality relationships may provide more instrumental support by connecting the youth with treatment and encouraging school engagement, which in turn may enhance the youth’s sense of agency and control.44 It is noteworthy that parental expressed emotion, as coded by a clinical observer, was not associated with illness course in this study, perhaps suggesting the greater importance of the adolescents’ and parents’ perceptions of the family as a prognostic indicator.
There were no differences between the course trajectories in the length or number of psychiatric treatment sessions or exposure to medications at baseline. Delay of treatment in pediatric bipolar disorder has been found to predict a poorer illness course.45 We were not able to address whether individuals with a poorer illness course were more delayed in receiving treatment. Further, racial disparities in mental health access and treatment46 and in the success of treatments47 may have contributed to the observation that minority individuals had a poorer course of illness. Increasing access to early intervention is especially critical for individuals with demographic and symptomatic/illness profiles that bode poorly for long-term outcome.
This study was designed as a treatment study. Thus, the observed mood trajectories – although independent of treatment assignment - may have been influenced by selection biases related to randomized trials, such as the possibility of greater motivation for psychosocial treatment. Further, the sample size, especially for small subgroup comparisons, limited our ability to detect differences. The generalizability of the findings pertain mostly to older adolescents with bipolar disorder. Finally, recall and hindsight bias, particularly for recalling number of mood episodes and the cycling of mood symptoms over 6-month retrospective periods, are limitations of this study’s design. Decreased reliability of data derived from retrospectively-recalled history may help explain why these previously identified prognostic variables were not associated with long-term outcome in this study.
To be clinically useful to the patient, family, and provider, patients’ course designations need to be ascertained prior to treatment. For example, knowing that a patient’s course subtype is likely to be predominantly euthymic may provide relief to the patient and family, and may indicate that shorter courses of psychoeducation and/or lower doses of psychotropic medications may suffice, in comparison to those with more chronic courses. In parallel, more intensive psychosocial treatments and/or medication regimens may be most helpful to individuals with BD who have not been able to obtain a consistently remitted state. Future research should attempt to determine whether predictors of course classifications – such as baseline depression and quality of life – can reliably elucidate the expected trajectory of illness and guide treatment for youth early in the course of bipolar illness.
Acknowledgments
Financial support for this study was provided by the National Institute of Mental Health (NIMH) grants R01MH093676, R01MH073871, R01MH073817, R01MH074033, R34MH077856, and R34117200.
Disclosures and Acknowledgements
Dr. Weintraub reports no competing interests. Dr. Schneck receives research support from the NIMH and the Ryan White HIV/AIDS Treatment Extension Act. Dr. Axelson receives royalties from UpToDate and has served as a consultant for Janssen Research. Dr. Kowatch is on the Data Safety Monitoring Committees of Pfizer and Forest Pharmaceuticals. Dr. Birmaher has received research support from NIMH and receives royalties from Random House, Lippincott Williams & Wilkins, and UpToDate. Dr. Miklowitz has received research funding from the NIMH, Brain and Behavior Research Foundation, Attias Family Foundation, Danny Alberts Foundation, Carl and Roberta Deutsch Foundation, Kayne Family Foundation, Max Gray Foundation, American Foundation for Suicide Prevention, and AIM for Mental Health. He receives book royalties from Guilford Press and John Wiley & Sons.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: Dr. Schneck has received research support from the NIMH and the Ryan White HIV/AIDS Treatment Extension Act. Dr. Axelson has received royalties from UpToDate and has served as a consultant for Janssen Research. Dr. Birmaher has received research support from NIMH and has received royalties from Random House, Lippincott Williams and Wilkins, and UpToDate. Dr. Kowatch has served on the Data Safety Monitoring Committees of Pfizer and Forest Pharmaceuticals. Dr. Miklowitz has received research funding from the NIMH, the Brain and Behavior Research Foundation, the Attias Family Foundation, the Danny Alberts Foundation, the Carl and Roberta Deutsch Foundation, the Kayne Family Foundation, the Max Gray Foundation, the American Foundation for Suicide Prevention, and AIM for Mental Health. He has received book royalties from Guilford Press and John Wiley and Sons. Dr. Weintraub reports no biomedical financial interests or potential conflicts of interest.
Clinical Trial Registration Information: Effectiveness of Family-Focused Treatment Plus Pharmacotherapy for Bipolar Disorder in Adolescents; https://clinicaltrials.gov/; NCT00332098
Contributor Information
Marc J. Weintraub, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles..
Christopher D. Schneck, School of Medicine, the University of Colorado, Aurora..
David A. Axelson, Nationwide Children’s Hospital and The Ohio State University College of Medicine, Columbus, OH..
Boris Birmaher, University of Pittsburgh Medical Center, Pittsburgh, PA..
Robert A. Kowatch, Nationwide Children’s Hospital and The Ohio State University College of Medicine, Columbus, OH..
David J. Miklowitz, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles..
References
- 1.Perils RH, Dennehy EB, Miklowitz DJ, et al. Retrospective age at onset of bipolar disorder and outcome during two-year follow-up: results from the STEP-BD study. Bipolar Disord. 2009;11(4):391–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DelBello MP, Hanseman D, Adler CM, Fleck DE, Strakowski SM. Twelve-month outcome of adolescents with bipolar disorder following first hospitalization for a manic or mixed episode. Am J Psychiatry. 2007;164(4):582–590. [DOI] [PubMed] [Google Scholar]
- 3.Birmaher B, Axelson D, Strober M, et al. Clinical course of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry. 2006;63(2):175–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Geller B, Tillman R, Bolhofner K, Zimerman B. Child bipolar I disorder: prospective continuity with adult bipolar I disorder; characteristics of second and third episodes; predictors of 8-year outcome. Arch Gen Psychiatry. 2008;65(10):1125–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Birmaher B, Axelson D, Goldstein B, et al. Four-year longitudinal course of children and adolescents with bipolar spectrum disorders: the Course and Outcome of Bipolar Youth (COBY) study. Am J Psychiatry. 2009;166(7):795–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goodwin FK, Jamison KR. Manic-depressive illness: bipolar disorders and recurrent depression. Vol 1: Oxford University Press; 2007. [Google Scholar]
- 7.Judd LL, Akiskal HS, Schettler PJ, et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry. 2002;59(6):530–537. [DOI] [PubMed] [Google Scholar]
- 8.Angst J, Sellaro R. Historical perspectives and natural history of bipolar disorder. Biol Psychiatry. 2000;48(6):445–457. [DOI] [PubMed] [Google Scholar]
- 9.Kraepelin E Manic-depressive illness and paranoia. Livingstone, Edinburgh: 1921. [Google Scholar]
- 10.Cicero DC, Epler AJ, Sher KJ. Are there developmentally limited forms of bipolar disorder? J Abnorm Psychol. 2009;118(3):431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Biederman J, Mick E, Faraone SV, Spencer T, Wilens TE, Wozniak J. Pediatric mania: a developmental subtype of bipolar disorder? Biol Psychiatry. 2000;48(6):458–466. [DOI] [PubMed] [Google Scholar]
- 12.Goldstein BI, Levitt AJ. Further evidence for a developmental subtype of bipolar disorder defined by age at onset: results from the national epidemiologic survey on alcohol and related conditions. Am J Psychiatry. 2006;163(9):1633–1636. [DOI] [PubMed] [Google Scholar]
- 13.Coryell W, Endicott J, Keller M. Rapidly cycling affective disorder. Arch Gen Psychiatry. 1992;49:126–131. [DOI] [PubMed] [Google Scholar]
- 14.Birmaher B, Gill MK, Axelson DA, et al. Longitudinal trajectories and associated baseline predictors in youths with bipolar spectrum disorders. Am J Psychiatry. 2014;171(9):990–999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kowatch RA, Fristad M, Birmaher B, Wagner KD, Findling RL, Hellander M. Treatment guidelines for children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2005;44(3):213–235. [DOI] [PubMed] [Google Scholar]
- 16.Axelson D, Birmaher BJ, Brent D, et al. A preliminary study of the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children mania rating scale for children and adolescents. J Child Adolesc Psychopharm. 2003;13(4):463–470. [DOI] [PubMed] [Google Scholar]
- 17.Chambers WJ, Puig-Antich J, Hirsch M, et al. The assessment of affective disorders in children and adolescents by semistructured interview: test-retest reliability of the Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present Episode Version. Arch Gen Psychiatry. 1985;42(7):696–702. [DOI] [PubMed] [Google Scholar]
- 18.Miklowitz DJ, Schneck CD, George EL, et al. Pharmacotherapy and family-focused treatment for adolescents with bipolar I and II disorders: a 2-year randomized trial. Am J Psychiatry. 2014;171(6):658–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaufman J, Birmaher B, Brent D, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–988. [DOI] [PubMed] [Google Scholar]
- 20.Keller MB, Lavori PW, Friedman B, et al. The Longitudinal Interval Follow-up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44(6):540–548. [DOI] [PubMed] [Google Scholar]
- 21.Hollingshead AB. Four factor index of social status. 1975. [Google Scholar]
- 22.Weissman MM, Wickramaratne P, Adams P, Wolk S, Verdeli H, Olfson M. Brief screening for family psychiatric history: the family history screen. Arch Gen Psychiatry. 2000;57(7):675–682. [DOI] [PubMed] [Google Scholar]
- 23.Magaña AB, Goldstein MJ, Karno M, Miklowitz DJ, Jenkins J, Falloon IR. A brief method for assessing expressed emotion in relatives of psychiatric patients. Psychiatry Res. 1986;17(3):203–12. [DOI] [PubMed] [Google Scholar]
- 24.Ravens-Sieberer U, Bullinger M. KINDL-R. Questionnaire for measuring health-related quality of life in children and adolescents, revised version. Manual. Recuperado de https://www.kindl.org/english/manual/[Links]. 2000. Accessed February 25, 2018. [Google Scholar]
- 25.Jung T, Wickrama K. An introduction to latent class growth analysis and growth mixture modeling. Soc Pers Psychol Compass. 2008;2(1):302–317. [Google Scholar]
- 26.Muthén LK, Muthén BO. Mplus: Statistical analysis with latent variables: User's guide. Muthén & Muthén Los Angeles; 2005. [Google Scholar]
- 27.Nylund KL, Asparouhov T, Muthen BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Struct Equat Modeling. 2007;14(4):535–569. [Google Scholar]
- 28.Goldberg JF, Perlis RH, Bowden CL, et al. Manic symptoms during depressive episodes in 1,380 patients with bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2009; 166(2):173–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oquendo MA, Waternaux C, Brodsky B, et al. Suicidal behavior in bipolar mood disorder: clinical characteristics of attempters and nonattempters. J Affect Disord. 2000;59(2):107–117. [DOI] [PubMed] [Google Scholar]
- 30.Nolen WA, Luckenbaugh DA, Altshuler LL, et al. Correlates of 1-year prospective outcome in bipolar disorder: results from the Stanley Foundation Bipolar Network. Am J Psychiatry. 2004;161(8):1447–1454. [DOI] [PubMed] [Google Scholar]
- 31.Geller B, Luby JL, Joshi P, et al. A randomized controlled trial of risperidone, lithium, or divalproex sodium for initial treatment of bipolar I disorder, manic or mixed phase, in children and adolescents. Arch Gen Psychiatry. 2012;69(5):515–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Correll CU, Sheridan EM, DelBello MP. Antipsychotic and mood stabilizer efficacy and tolerability in pediatric and adult patients with bipolar I mania: a comparative analysis of acute, randomized, placebo-controlled trials. Bipolar Disord. 2010;12(2):116–141. [DOI] [PubMed] [Google Scholar]
- 33.Rush AJ. STAR* D: what have we learned? Am J Psychiatry. 2007;164(2):201–204. [DOI] [PubMed] [Google Scholar]
- 34.Perlis RH, Miyahara S, Marangell LB, et al. Long-term implications of early onset in bipolar disorder: data from the first 1000 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD). Biol Psychiatry. 2004;55(9):875–881. [DOI] [PubMed] [Google Scholar]
- 35.Michalak EE, Yatham LN, Lam RW. Quality of life in bipolar disorder: a review of the literature. Health Qual Life Outcomes. 2005;3(1):72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.de Abreu LN, Nery FG, Harkavy-Friedman JM, et al. Suicide attempts are associated with worse quality of life in patients with bipolar disorder type I. Compr Psychiatry. 2012;53(2):125–129. [DOI] [PubMed] [Google Scholar]
- 37.Rea MM, Tompson MC, Miklowitz DJ, Goldstein MJ, Hwang S, Mintz J. Family-focused treatment versus individual treatment for bipolar disorder: results of a randomized clinical trial. J Consult Clin Psychol. 2003;71(3):482. [DOI] [PubMed] [Google Scholar]
- 38.Cannon M, Jones P, Gilvarry C, et al. Premorbid social functioning in schizophrenia and bipolar disorder: similarities and differences. Am J Psychiatry. 1997;154(11):1544–1550. [DOI] [PubMed] [Google Scholar]
- 39.Houlihan JP. Heterogeneity among schizophrenic patients: Selective review of recent findings (1970–75). Schizophr Bull. 1977;3(2):246. [DOI] [PubMed] [Google Scholar]
- 40.Johnson SL, Meyer B, Winett C, Small J. Social support and self-esteem predict changes in bipolar depression but not mania. J Affect Disord. 2000;58(1):79–86. [DOI] [PubMed] [Google Scholar]
- 41.Geller B, Tillman R, Craney JL, Bolhofner K. Four-Year Prospective Outcome and Natural History of Mania in Children With a Prepubertal and Early Adolescent Bipolar Disorder Phenotype. Arch Gen Psychiatry. 2004;61(5):459–467. [DOI] [PubMed] [Google Scholar]
- 42.Butzlaff RL, Hooley JM. Expressed emotion and psychiatric relapse: a meta-analysis. Arch Gen Psychiatry. 1998;55(6):547–552. [DOI] [PubMed] [Google Scholar]
- 43.Kim EY, Miklowitz DJ. Expressed emotion as a predictor of outcome among bipolar patients undergoing family therapy. J Affect Disord. 2004;82(3):343–352. [DOI] [PubMed] [Google Scholar]
- 44.Harrow M, Hansford BG, Astrachan-Fletcher EB. Locus of control: Relation to schizophrenia, to recovery, and to depression and psychosis—A 15-year longitudinal study. Psychiatry Res. 2009;168(3):186–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Post RM, Leverich GS, Kupka RW, et al. Early-onset bipolar disorder and treatment delay are risk factors for poor outcome in adulthood. J Clin Psychiatry. 2010;71(7):864–872. [DOI] [PubMed] [Google Scholar]
- 46.Creedon TB, Cook BL. Access to mental health care increased but not for substance use, while disparities remain. Health Affairs. 2016;35(6):1017–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Maura J, Weisman de Mamani A. Mental Health Disparities, Treatment Engagement, and Attrition Among Racial/Ethnic Minorities with Severe Mental Illness: A Review. J Clin Psychol Med Settings. 2017;24(3-4):187–210. [DOI] [PubMed] [Google Scholar]