A healthy 18-year-old white woman presented for evaluation of skin roughness of her hands for 2 years. Both palmar and dorsal surfaces were affected. Short immersion in water or hand washing produced excessive, but asymptomatic wrinkling, which disappeared 10 to 15 minutes after drying. The patient denied any other systemic complaints.
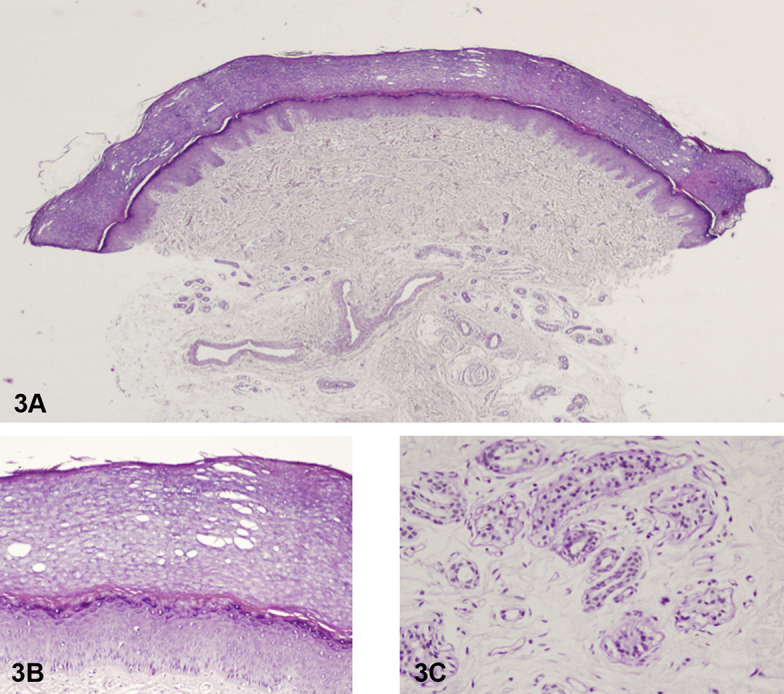
Physical examination found normal palm appearance with slightly hyperkeratotic fingertips before water immersion (Fig 1) and excessive wrinkling and rapid development of white flat-topped papules with papillomatous appearance 3 to 4 minutes after water exposure (Fig 2, A and B). Punch biopsy of the patient's palm was performed (Fig 3, A-C).
Fig 1.
Fig 2.
Fig 3.
Question 1: What is the most likely clinical diagnosis?
-
A.
Dyshidrotic hand dermatitis
-
B.
Acquired aquagenic keratoderma (AAK)
-
C.
Hereditary papulotranslucent acrokeratoderma
-
D.
Aquagenic urticaria
-
E.
Aquagenic pruritus
Answers:
-
A.
Dyshidrotic hand dermatitis – Incorrect. Dyshidrotic hand dermatitis is a relatively common, chronic palmoplantar eczematous dermatosis, characterized by firm, pruritic vesicles on the palms and sides of the fingers. Patients often have underlying atopic dermatitis or, less often, a manifestation of allergic contact dermatitis.1
-
B.
AAK – Correct. AAK is a rare condition characterized by a transient and recurrent keratoderma on the palms, and occasionally the soles of the feet after brief exposure to water.2 Histologically, AAK is characterized by orthohyperkeratosis, increased thickness of the stratum corneum (Fig 3, A), dilated intracorneal acrosyringia (Fig 3, B), and hyperplasia of eccrine coils in the dermis, often with a crenulated or vacuolar appearance (Fig 3, C).
-
C.
Hereditary papulotranslucent acrokeratoderma—Incorrect. AAK should be differentiated from the hereditary papulotranslucent acrokeratoderma, which shows similar characteristics, but is a congenital condition with suspected autosomal dominant inheritance pattern and persistent lesions.2
-
D.
Aquagenic urticaria – Incorrect. Aquagenic urticaria is a rare subtype of physical urticaria marked by immediate contact with water.3
-
E.
Aquagenic pruritus – Incorrect. Aquagenic pruritus is characterized by immediate development of intense pruritus, stinging, or burning sensation, without any visible skin changes, after contact with water.3
Question 2: What disorder is this condition most likely associated with?
-
A.
Polycythemia vera (PcV)
-
B.
Myelodysplastic syndrome
-
C.
Bernard-Soulier syndrome (BSS)
-
D.
Cystic fibrosis (CF)
-
E.
Hepatitis C
Answers:
-
A.
PcV – Incorrect. Aquagenic pruritus is a characteristic symptom found in many patients with PcV. A recent study found that about two-thirds of patients with PcV had aquagenic pruritus.3
-
B.
Myelodysplastic syndrome – Incorrect. Myelodysplastic syndrome is reported to be associated with aquagenic pruritus and may precede the diagnosis by several years.3
-
C.
BSS – Incorrect. BSS is a rare autosomal recessive disorder caused by mutations in the GPIbα, GPIbβ, and GPIX genes. BSS has been associated with prolonged bleeding as well as aquagenic urticaria.3
-
D.
CF – Correct. AAK is often reported to be associated with CF, as a large number of patients with AAK exhibit mutations of the CF transmembrane conductance regulator (CFTR) gene.4 In fact, AAK is proposed as a possible sign of CF, with an estimation that between 44% and 80% of patients with CF has AAK.4 Our patient, however, did not have a known history of CF. Interestingly, AAK can be found in 10% to 25% of asymptomatic, heterozygous carriers of the CFTR gene mutation.1
-
E.
Hepatitis C – Incorrect. Hepatitis C is reported to be associated with aquagenic pruritus, not with AAK.3
Question 3: Which of the following has been found to be aberrantly expressed in this condition?
-
A.
Aquaporin 5 (AQP5)
-
B.
Connexin 26
-
C.
Keratin 9
-
D.
Histamine
-
E.
Vasoactive intestinal peptide
Answers:
-
A.
AQP5 – Correct. The pathogenesis of AAK is unknown, but it is believed that aberrant function of the sweat glands may be involved in the clinical phenotype. On a molecular level, the dysregulation of the sweating mechanisms of AAK may be due in part to an aberrant expression of AQP5.5 Aquaporins are membrane proteins that are responsible for osmotic water trafficking across the plasma membrane in response to osmotic gradients produced by salt transport.5 AQP5 is present in the dark cells of sweat glands of healthy donors; however, in patients with AAK, there is an aberrant expression of AQP5 that also extends to the clear cells of the sweat glands.5 Clear cells are considered to be the source of focal hyperhidrosis.4
-
B.
Connexin-26 – Incorrect. Connexin-26 is expressed in the palmoplantar epidermis, sweat glands, and inner ear cochlea. It is encoded by gap junction β-2 gene (GJB2), which is mutated in Vohwinkel syndrome (an autosomal dominant diffuse palmoplantar keratoderma characterized by “starfish” keratoses on the knuckles and sensorineural hearing loss).1
-
C.
Keratin 9 – Incorrect. Patients with diffuse epidermolytic palmoplantar keratoderma have mutations in KRT1 and KRT9 genes, the latter of which encodes keratin 9.1
-
D.
Histamine – Incorrect. Histamine release is found to be implicated in aquagenic urticaria and possibly in aquagenic pruritus.3
-
E.
Vasoactive intestinal peptide – Incorrect. Increased release of vasoactive intestinal peptide has been reported in patients with aquadynia, a variant of aquagenic pruritus.3
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Bolognia J.L., Schaffer J.V., Cerroni L., editors. Dermatology. Chapter 58. Elsevier Limited; 2018. [Google Scholar]
- 2.Yan A.C., Aasi S.Z., Alms W.J. Aquagenic palmoplantar keratoderma. J Am Acad Dermatol. 2001;44:696–699. doi: 10.1067/mjd.2001.113479. [DOI] [PubMed] [Google Scholar]
- 3.Wang F., Zhao Y.K., Luo Z.Y. Aquagenic cutaneous disorders. J Dtsch Dermatol Ges. 2017;15(6):602–608. doi: 10.1111/ddg.13234. [DOI] [PubMed] [Google Scholar]
- 4.Tchernev G., Semkova K., Cardoso J., Ananiev J., Wollina U. Aquagenic keratoderma. Two new case reports and a new hypothesis. Indian Dermatol Online. 2014;5:30–33. doi: 10.4103/2229-5178.126025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kabashima K., Shimauchi T., Kobayashi M. Aberrant aquaporin 5 expression in the sweat gland in aquagenic wrinkling of the palms. J Am Acad Dermatol. 2008;59(2):28–32. doi: 10.1016/j.jaad.2008.04.023. [DOI] [PubMed] [Google Scholar]




