Abstract
A 70-year-old female patient, known to be diabetic and hypertensive, was diagnosed with coronary artery disease and severe aortic stenosis aortic valve area 0.5 cm, peak gradient of 110 mmHg, mean gradient 55 mmHg). This patient underwent coronary artery bypass graft with two grafts and artery bypass grafting in 2012. She received a sutureless Perceval aortic valve with good postoperative results except for a small jet of paravalvular leak. She did well for 5 years until she began experiencing dyspnea on exertion. The patient was found to have moderate to severe aortic regurgitation and moderate aortic stenosis which progressed over the years with multiple admissions for heart failure and pulmonary edema. The patient was considered high risk for operative treatment. Therefore, she was treated by percutaneous valve-in-valve technique using S3 Edward valve with excellent results.
Keywords: Aortic regurgitation, aortic stenosis, aortic valve replacement, degenerated prosthetic aortic valve, paravalvular leak, valve in valve
INTRODUCTION
Transcatheter aortic valve implantation (TAVI) procedures are becoming more popular in the last 10 years worldwide. It is now considered a common Cath lab procedure in most countries.
The degeneration of prosthetic tissue valves is a very well-known phenomenon, which may result in aortic stenosis, aortic regurgitation, or combined valve pathology.
The same mechanism of degeneration may occur when the surgeons use sutureless valves in surgical aortic valve replacement (SAVR). We propose a possible treatment of such patients by using TAVI and Valve-in-Valve (ViV) technique.
CASE PRESENTATION
A 70-year-old female patient, known to be diabetic and hypertensive, was diagnosed with coronary artery disease, and severe aortic stenosis (AVA 0.5 cm, Peak gradient of 110 mmHg, Mean gradient 55 mmHg). In 2012, this patient underwent coronary artery bypass graft with two grafts and artery bypass grafting. She received a sutureless Perceval valve of medium size [Figure 1], with good postoperative results despite a small jet of Paravalvular Leak (PVL) which was seen at the anterior aspect. The Aortic valve showed a peak gradient of 27 mmHg and a mean gradient of 13 mmHg.
Figure 1.
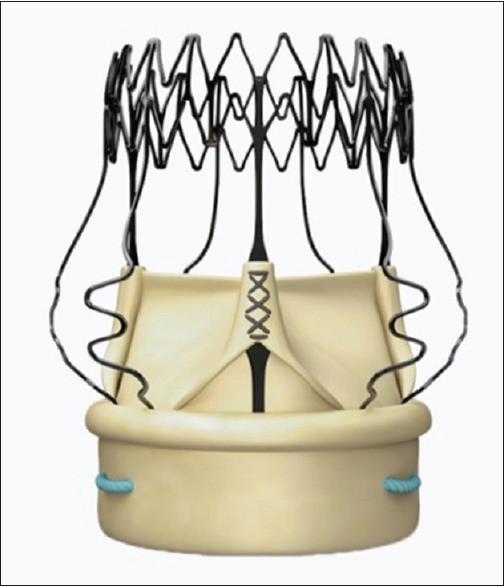
Perceval is the 100% sutureless valve for aortic valve replacement, with the unique characteristic of allowing sutureless positioning and anchoring at the implant site
She did well over 5 years until she began experiencing more dyspnea on exertion. The patient was found to have moderate aortic regurgitation and moderate aortic stenosis [Figure 2], which progressed over the years with multiple admissions for heart failure and pulmonary edema. The case was investigated, a coronary and graft angiogram was done. The left mammary artery graft to left anterior descending artery was patent and the saphenous vein graft to obtuse marginal was also patent.
Figure 2.
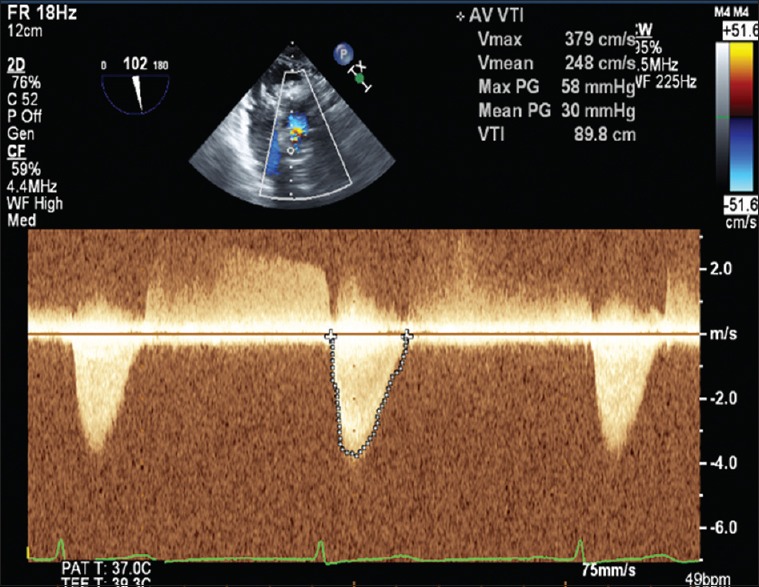
Echo Doppler shows aortic stenosis with PG 58 mmHg and PG 30 mmHg with moderate AR
Echocardiogram findings have shown the following: Normal ejection fraction, moderate aortic regurgitation with PVL [Figure 3], moderate to severe aortic stenosis with aortic valve (AV)-peak gradient of 80 mmHg and a mean Gradient 35 mmHg.
Figure 3.
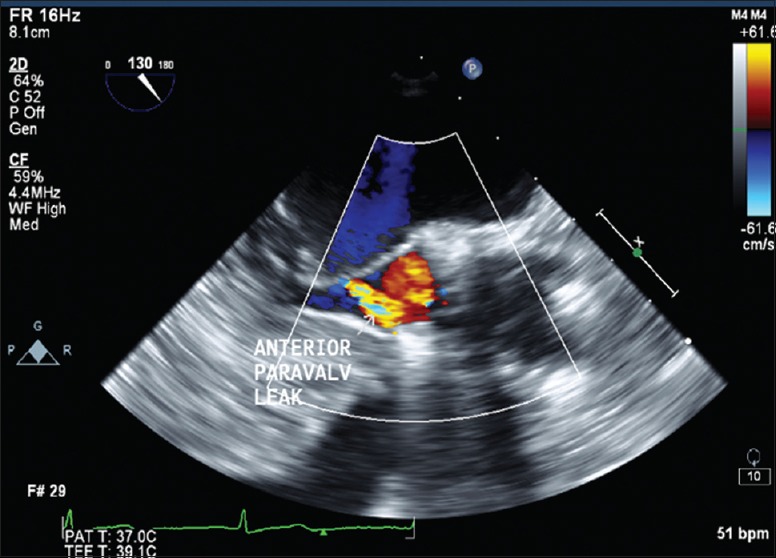
Showed an anterior paravalvular leak (moderate AR)
This case was discussed in the heart team meeting, and she was labeled as high risk for operative treatment. Risks and benefits were explained to the patient and her family.
The patient underwent a TAVI procedure through the right femoral approach [Figure 4]. We used the ViV technique. According to the original valve size, our computed tomography-scan measurement, and sizing an S3 size 26 mm. Edward valve was deployed with excellent final results [Figures 5 and 6]. The echocardiogram showed no PVL and the gradient was 15 mmHg [Figure 7]. The patient was discharged from hospital after 2 days in a very good condition.
Figure 4.
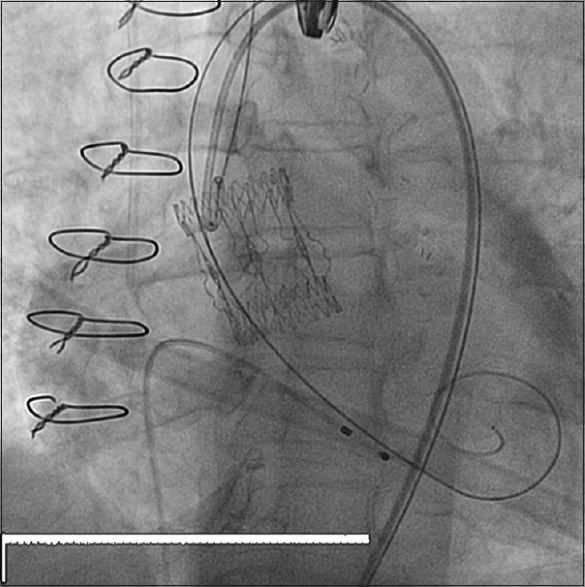
Showed a Perceval (Sutureless valve) by fluoroscopy
Figure 5.
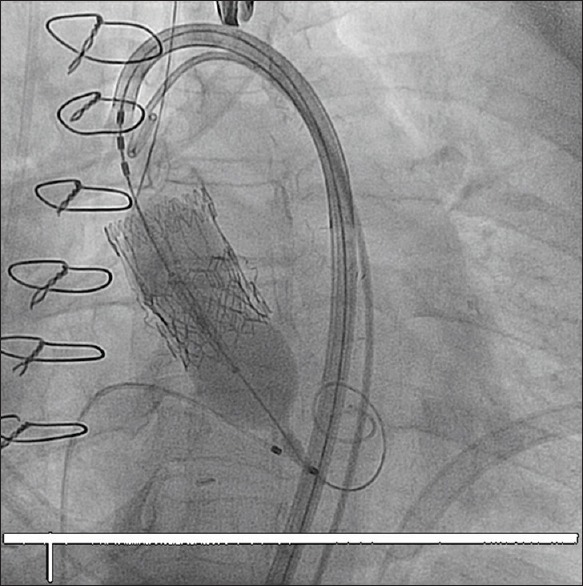
Showed A valve in valve deployment, using an Edward S3 during balloon inflation
Figure 6.
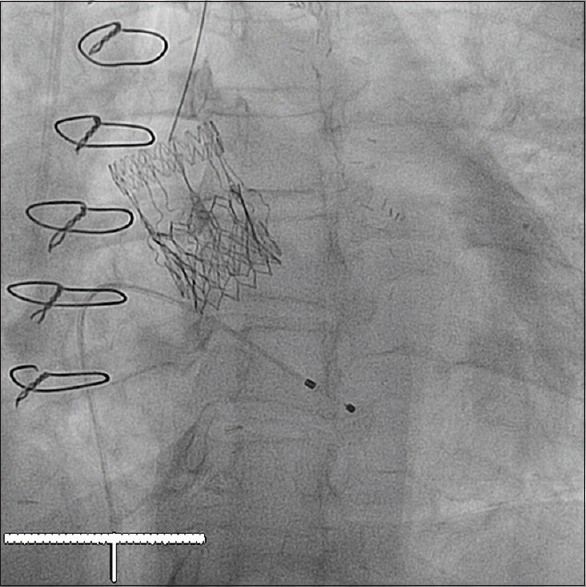
Showed a final result of valve-in-valve deployment (S3 Edward valve inside the sutureless valve)
Figure 7.
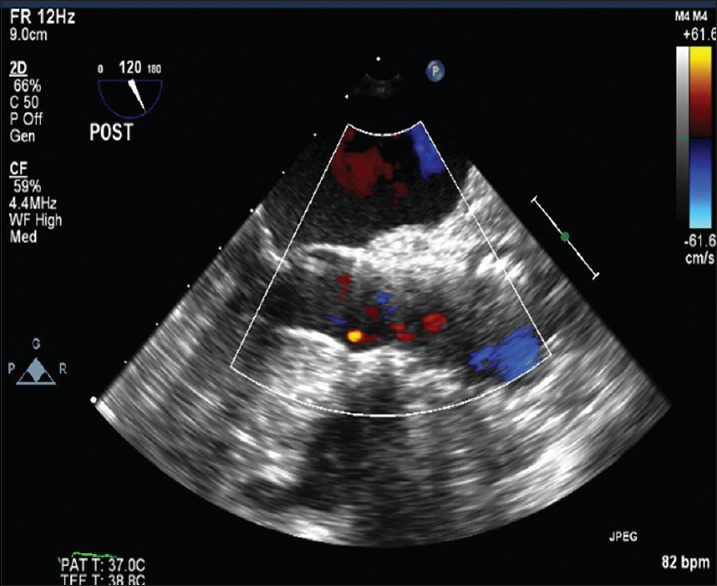
Showed a final result of valve in valve, color Doppler with paravalvular leak
DISCUSSION
TAVI, has become more popular in the last decade as an alternative to surgical aortic valve replacement for high risk patients with severe symptomatic aortic stenosis. Recently, TAVI is debated in replacing surgery for both intermediate and low-risk patients.[1]
This new technology of sutureless (self-expandable aortic valve), has been adopted by some cardiac surgeons as an alternative to the conventional bioprosthetic aortic valve replacement,[2] because surgeons prefer decreasing the cross-clamp time and shortening cardiopulmonary bypass time, and the sutureless valve may achieve better hemodynamic parameters.[3,4]
This new procedure was utilized by a small number of cardiac surgeons in the Middle East. In our cardiac center, about 90 cases were done over the last 8 years. We monitored those patients with regular follow-up visits in the cardiac clinics and echocardiography studies.[5] In our center, we noticed so far two cases of symptomatic degeneration of Perceval valve, one is this patient, and the second is a lady with moderate PVL with controlled symptoms on optimal medical therapy.
In general, surgical aortic bioprosthetic valves show degeneration over time, which could result in either aortic stenosis, aortic regurgitation, or a combination of both lesions. This may occur over a period of 7–10 years in most cases. Most of such patients may require subsequent interventions.[6,7]
Since the start of the TAVR program, the ViV option was used during percutaneous procedures for the treatment of PVL due to either low or high positioned valve. Nowadays, the aortic ViV technique is accepted, and became a routine procedure. This method was approved by the FDA as a percutaneous procedure for the treatment of degenerated failed bioprosthetic valves, mainly in patients with a high surgical risk.[8] The ViV technique was used also for the treatment of degenerated homografts. Many recent new studies showed that TAVI is superior to medical therapy in high-risk inoperable patients, due to the increase in survival rate and the cost-effectiveness using this procedure.[9,10]
Regarding ViV technique for degenerated sutureless (Perceval), the number of cases done by this method is small, and the long-term benefit is unknown. Because of the difference in structure, such as a large nitinol stent with a soft ring, this may lead to less support for an additional device inside this type of valve.[11,12]
Most of studies and case reports about treating degenerated surgical aortic bioprosthetic valve using (ViV) technique originated from Western countries. We are lacking similar data from Middle East countries. We describe here our first degenerated sutureless valve in our cardiac center, this patient was treated successfully with the ViV technique. The patient was discharged in a very good condition and had two follow up visits so far.
CONCLUSION
TAVI procedure has become a regular and safe procedure in the Cardiac Cath Lab as reported in major clinical trials. It is now approved to treat degeneration of aortic bioprosthetic valve by ViV technique. The new surgical technique of using sutureless valves is feasible. If the same phenomenon of degeneration would happen with this type of valve, ViV technique may be the optimal treatment of choice.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Barker CM, Reardon MJ. Should TAVR replace surgery for aortic stenosis in low – To intermediate-risk patients? Can J Cardiol. 2017;33:1124–8. doi: 10.1016/j.cjca.2017.06.013. [DOI] [PubMed] [Google Scholar]
- 2.Takagi H, Umemoto T. A meta-analysis of sutureless or rapid-deployment aortic valve replacement. Thorac Cardiovasc Surg. 2016;64:400–9. doi: 10.1055/s-0035-1566130. [DOI] [PubMed] [Google Scholar]
- 3.Fischlein T, Meuris B, Hakim-Meibodi K, Misfeld M, Carrel T, Zembala M, et al. The sutureless aortic valve at 1 year: A large multicenter cohort study. J Thorac Cardiovasc Surg. 2016;151:1617–26, e4. doi: 10.1016/j.jtcvs.2015.12.064. [DOI] [PubMed] [Google Scholar]
- 4.Santarpino G, Pfeiffer S, Jessl J, Dell'Aquila AM, Pollari F, Pauschinger M, et al. Sutureless replacement versus transcatheter valve implantation in aortic valve stenosis: A propensity-matched analysis of 2 strategies in high-risk patients. J Thorac Cardiovasc Surg. 2014;147:561–7. doi: 10.1016/j.jtcvs.2013.10.025. [DOI] [PubMed] [Google Scholar]
- 5.Pfeiffer S, Fischlein T, Santarpino G. Sutureless sorin perceval aortic valve implantation. Semin Thorac Cardiovasc Surg. 2017;29:1–7. doi: 10.1053/j.semtcvs.2016.02.013. [DOI] [PubMed] [Google Scholar]
- 6.Salaun E, Mahjoub H, Dahou A, Mathieu P, Larose É, Després JP, et al. Hemodynamic deterioration of surgically implanted bioprosthetic aortic valves. J Am Coll Cardiol. 2018;72:241–51. doi: 10.1016/j.jacc.2018.04.064. [DOI] [PubMed] [Google Scholar]
- 7.Salaun E, Clavel MA, Rodés-Cabau J, Pibarot P. Bioprosthetic aortic valve durability in the era of transcatheter aortic valve implantation. Heart. 2018;104:1323–32. doi: 10.1136/heartjnl-2017-311582. [DOI] [PubMed] [Google Scholar]
- 8.Dvir D, Webb JG, Bleiziffer S, Pasic M, Waksman R, Kodali S, et al. Transcatheter aortic valve implantation in failed bioprosthetic surgical valves. JAMA. 2014;312:162–70. doi: 10.1001/jama.2014.7246. [DOI] [PubMed] [Google Scholar]
- 9.Reynolds MR, Magnuson EA, Wang K, Lei Y, Vilain K, Walczak J, et al. Cost-effectiveness of transcatheter aortic valve replacement compared with standard care among inoperable patients with severe aortic stenosis: Results from the placement of aortic transcatheter valves (PARTNER) trial (Cohort B) Circulation. 2012;125:1102–9. doi: 10.1161/CIRCULATIONAHA.111.054072. [DOI] [PubMed] [Google Scholar]
- 10.Finch J, Roussin I, Pepper J. Failing stentless aortic valves: Redo aortic root replacement or valve in a valve? Eur J Cardiothorac Surg. 2013;43:495–504. doi: 10.1093/ejcts/ezs335. [DOI] [PubMed] [Google Scholar]
- 11.Landes U, Sagie A, Kornowski R. Transcatheter aortic valve implantation in degenerative sutureless perceval aortic bioprosthesis. Catheter Cardiovasc Interv. 2018;91:1000–4. doi: 10.1002/ccd.26576. [DOI] [PubMed] [Google Scholar]
- 12.Andreas M, Coti I, Laufer G, Kastner J. Valve-in-valve transcatheter aortic valve implantation into a novel, sutureless bioprosthesis: Technical considerations. EuroIntervention. 2018;13:1902–3. doi: 10.4244/EIJ-D-17-00578. [DOI] [PubMed] [Google Scholar]


