Abstract
Background:
The healthcare reforms have led to the development of new primary care systems. These models allowed responding to people's needs but with problems in maintaining the relational continuity between the patient and therapist.
Materials and Methods:
We performed a survey on 12 May 2018, in Messina (Sicily, Italy), during an informational event. Participants were invited to fill in a self-reported Italian questionnaire composed of 12 multiple-choice questions, specifically created by the authors. The tool included the assessment of the social status, the presence of chronic diseases, preference in health care, and evaluation of the services offered in the territory.
Results:
As for the territorial services, we observed that the general practitioner (GP) was the most appreciated healthcare provider, followed by the nurse.
Conclusions:
We believe that nurses can represent the most appropriate healthcare figure to potentiate GP's patient management in primary territorial care.
Keywords: Healthcare system, nurse, patients preferences, primary care, telemedicine
Introduction
In the last few years, new healthcare reforms in western Europe has changed the primary care systems.[1] In particular, many countries encouraged the promotion of interprofessional teamwork, fundamental to improve the patients’ care and support the diffusion of knowledge.[2,3,4] This innovative process also hit Italy, where the primary care system’ organization models changed to incentivize the continuity and the therapies’ accessibility and to foster the fruition of nursing care and health services, both of which allow cooperation in the multi-professional team. It was underlined how it is very important to redefine these models on the basis of the population's needs and necessities.[5] The local health authorities, in fact, tried to change the traditional models, mainly based on the “isolation” of general practitioner (GP), encouraging cooperation among all the health service players.[6] These innovative programs aimed at fostering health continuity.[7,8] The chance to have a continuity of the treatment, which can also build a dialog among healthcare professionals, can allow benefiting from new diagnostic and therapeutic technologies, such as telerehabilitation.[9,10] This could be useful in earlier identification of the disease and guarantee both home and hospital rehabilitation, to avoid nonurgent access to the emergency services, reduce remarkably the number of unnecessary returns to the specialists, and permit a reduction in the healthcare costs.[11,12,13,14] Therefore, it is very important to evaluate all the aspects concerning the healthcare models in terms of effectiveness of the therapies, costs and benefits, and relational continuity for the patient and his/her professional therapist, also taking into account patient's preference.[8] The primary care models’ characteristics should be considered, especially when the users/patients ask for some enhancements.[5] In the literature, some surveys about the preferences of the patients and the suppliers exist,[15,16,17,18] and concern the characteristics related to the access to services, the kind of specialist that has been consulted, and the continuity of treatment.[19] Nonetheless, even if the concept of satisfaction/preference of the patient is generously evaluated, the studies suggest that this concept is not coherent enough, as it is not properly correlated as to how the patients evaluate the health care system.[20]
The purpose of this study is to find out the preferences of an Italian sample concerning the point of access to local health services and propose an innovative solution to overcome healthcare costs and resource allocation disparities.
Materials and Methods
We performed a survey on the 12 May 2018, in Messina (Sicily, Italy), during an informational event related to the “International Nursing Day”. Participants were asked to complete a questionnaire. Although 500 people attended the event, less than half of them entered the study. They were adequately informed about the study and offered their collaboration and written consent.
The Local Ethics Committee of the IRCCS Centro Neurolesi “Bonino-Pulejo” approved the study (ID: 28/2018).
The sample included 203 Sicilian individuals (102 females and 101 males) aged 18–88 years (mean age 38.12 ± 18.93 years), mainly single (61.58%), and with a middle-high educational level, as shown in Table 1. The self-reported Italian questionnaire was composed of 12 multiple-choice questions, specifically created by the authors. The tool included the assessment of the social status, the presence of chronic diseases, preference in health care, and evaluation of the services offered in the territory (see Appendix 1).
Table 1.
Demographical description of the sample
| Males | Females | All | |
|---|---|---|---|
| Participants | 101 (49.75%) | 102 (50.25%) | 203 (100%) |
| Age (years) | 41.91±15.29 | 34.37±21.43 | 38.12±18.93 |
| Education | |||
| None | 1 (0.99%) | 1 (0.98%) | 2 (0.98%) |
| Primary school | 2 (1.98%) | 2 (1.96%) | 4 (1.97%) |
| Middle school | 19 (18.81%) | 8 (7.84%) | 27 (13.30%) |
| High school | 47 (46.53%) | 61 (59.80%) | 108 (53.20%) |
| Vocational school | 5 (4.95%) | 2 (1.96%) | 7 (3.45%) |
| University | 27 (26.73%) | 28 (27.45%) | 55 (27.09%) |
| Marital Status | |||
| Single | 61 (60.40%) | 64 (62.75%) | 125 (61.58%) |
| Married | 30 (29.70%) | 24 (23.53%) | 54 (26.60%) |
| Divorced | 2 (1.98%) | 5 (4.90%) | 7 (3.45%) |
| Living with partner | 2 (1.98%) | 5 (4.90%) | 7 (3.45%) |
| Widowed | 6 (5.94%) | 4 (3.92%) | 10 (4.92%) |
| Job | |||
| Not stated | 1 (0.99%) | - | 1 (0.49%) |
| Pensioned | 23 (22.78%) | 4 (3.92%) | 27 (13.30%) |
| Unemployed | 10 (9.90%) | 7 (6.86%) | 17 (8.37%) |
| Housewife | - | 5 (4.90%) | 5 (2.46%) |
| Student | 29 (28.71%) | 44 (43.14%) | 73 (35.96%) |
| Construction worker | 3 (2.97%) | 6 (5.88%) | 9 (4.43%) |
| Office worker | 20 (19.80%) | 19 (18.63%) | 39 (19.21%) |
| Teacher | 2 (1.98%) | 1 (0.98%) | 3 (1.48%) |
| Freelance professional | 5 (4.95%) | 9 (8.82%) | 14 (6.90%) |
| Artisan/Trader | 1 (0.99%) | - | 1 (0.49%) |
| Other | 7 (6.93%) | 7 (6.86%) | 14 (6.90%) |
Quantitative variables are in mean±standard deviation; qualitative variables are in frequencies (n) and percentage
Statistical analysis were performed by using the 3.2.3 version of the open-source software R. Results for continuous variables were expressed in mean ± standard deviation, whereas categorical variables were expressed in frequencies and percentages.
Since this was an epidemiological study, we followed the STROBE checklist, instead of CONSORT, which refers to randomized clinical trials (see Appendix 1).
Results
We found a few comorbidities in the population that we screened. The mean number of chronic diseases per subject was 0.88 ± 1.36, higher in men (0.96 ± 1.54) than in women (0.79 ± 1.61), being headache the most prevalent (11.33%), followed by arthrosis and hypertension (10.84%), anxiety/depression, and respiratory disease (9.85%).
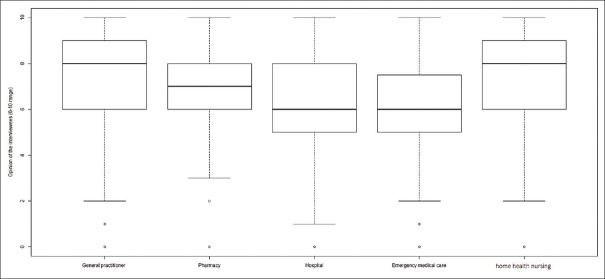
As for the territorial services, we observed that GP was the most appreciated (with a mean score of 7.27 in a range of 0–10), followed by the home health nursing (with a mean score of 7.19 in a range of 0–10), the pharmacy (with a mean score of 6.68 in a range of 0–10), the hospital and the emergency medical care (each with a mean score of 5.75 in a range of 0–10), as showed in Figure 1. Moreover, around 70% of the sample declared to refer to their GP in case of need. The reasons for this prevalence seem to be the confidence established with the GP over time (49.32%), his knowledge of the clinical history of the patient (21.92%), and the convenience of being close to home (28.76%). On the contrary, the hospital is chosen mainly for emergencies (11.82%), whereas familiars/friends (11.33%), and private doctors (6.90%) are preferred to avoid waiting queue. Significantly, 50.25% of the people interviewed reported long waiting queue as the first problem of the hospital, followed by the need for more attention to the patient (42.36%), and a better staff training (7.39%).
Figure 1.
Community preferences for the different territorial services and health professionals in Messina (Sicily)
Overall, about 40% of the subjects declared having met the GP in the last month, 18.72% in the last trimester, and 41.87% of not having met the GP for more than 3 months. The main reason for visiting GP was flu (45.83%), get a routine examination (36.46%), or require a prescription for a specialist examination (17.71%). For 88.18% of the subjects, GP was kind and attentive to the patient's needs. However, 28.57% declared that the GP should increase their reception hours, besides to keep updated on new clinical practices.
Discussion
The continuity of care (i.e. the relationship between individual patients and their physicians over time, includes both the interpersonal aspects of care and the quality and cost-effectiveness of care) is one of the main purposes of the Italian SSN.[21] In the territory, GP and another healthcare professional of the SSN work together to build on the integrated network, giving a central role to the patient.[22] The results of our study showed the community preferences for the different territorial services in Sicily, an Italian region located in the south of the country. It is based on the fact that involving citizens in the decision-making of the care, in terms of preference, allows empowerment and compliance to the patient's care, with a consequent increase in the healthcare provision.[23,24] In line with the literature,[15,16,25] our data reveals a clear appreciation for consultation with GP. Therefore, citizens identify their GP as the preferred point of access to local health services compared to other health professionals.[15,25] However, the actual health policies encounter many difficulties in the territorial patient's management, and they do not guarantee the relational-continuity with the GP.[8,26] To this end, there are at least two different organizational models for patient management in the territory. Segheri et al. underline that it is still difficult to establish the best model that can maximize the healthcare advantages, especially to respond to the patient's preference and needs in context with limited resources.[5] In fact, some surveys point out that the healthcare reform, with regard to Italy, gave priority to health structures for patient care and cure. Nevertheless, the care-giving teams should guarantee assistance to the chronicity and serious health problems.[27] In particular, according to Lamarche et al.,[8] these models may obtain various positive outcomes but they find it difficult to preserve the relational continuity between the patient and the health professionals, limiting access to the treatment.[15,16,25] However, the second model, as it is described in other surveys, remarks a different direction of the government.[28] In fact, most of the developed countries adopted the figure of the GP as a kind of “guardian” of the healthcare territorial systems. This model gives a role of responsibility to the GP for both the patients’ health and prescribed treatment costs. The results of our survey show a preference for the second model. The reasons seem to be the confidence established with the GP over time and the convenience of being close to home. On the other hand, the application of the model is limited by an overload of the GP. In fact, the GP may have difficulty to carry out the needs of a vast territory.[29,30,31] In reality, it is known that the highest number of patients the GP can take care of is 1500, even if some GP has more than 1800 patients in charge.[32] Thus, the GP cannot guarantee adequate high-quality care for the patient. As suggested by our survey, it could be useful to introduce the nurse to collaborate with the GP in the territorial management of the patient. The nurse has the ability to respond adequately to the needs of the healthy or sick individual and establish an empathic communication aimed at understanding the wellbeing. The collaboration between these healthcare professionals could respond effectively to the critical issues that have emerged in the territory, as evidenced by our data (accessibility to treatment and the reduction of health response times). The nurse could enhance the patient's cure and increase the continuity of care.[23] Some countries (i.e. the United Kingdom, Australia, Canada, and the USA) have just introduced nurses in the routine management of primary care. In specific circumstances, there are available proofs that this model can potentially optimize the relationship between GP and patients on the territory and it can reduce the health care costs without compromising on the quality of care.[14,24] Laurant et al. highlighted that if the nurse is properly trained, then he/she might be able to furnish high-quality care and reach good health results for the patients. In particular, the authors have noticed a high level of satisfaction in the patient and the highest number of programed follow-ups.[32] From the future perspective, it is our opinion that the nurse, a case manager (CM), should be employed in a multimodal approach, combining his/her specific expertise with innovative technologies for health care [Figure 2].[33] In fact, the skills of CM represent the evolution of nursing professional functions, as CM takes care of the health of the individual and the well-being of the community in the territory. The CM carries outpatient management, health planning, coordination of the multidisciplinary team, and can actively collaborate with the GP, playing the linking role in the territorial network. Moreover, in our opinion, the use of telemedicine could maximize patient management in the local health service, in situations wherein GP and patient are not in the same place.[34,35]
Figure 2.

Innovative approach to overcome disparities in healthcare allocations. The GP collaborates with different CM, located in strategic positions in the rural areas of the city, to guarantee better assistance. CM, by means of telemedicine, can immediately respond to the needs of patients, and have direct contact with GP, in situations where GP/CM/patient are not in the same place
CM could use telemedicine to support GP in supervising the patient's clinical pathway (therapeutic counseling, diagnosis, and rehabilitation at home). This innovation could facilitate the delivery of healthcare services in the territory, permitting a reduction of inappropriate health-service access and direct/indirect health costs.[10,13,36] Finally, CM could promote the empowerment of patients and caregivers in a family environment.[37] Therefore, it is important that GP and nurses, as primary care providers especially for rural and disadvantaged populations, collaborate and develop the knowledge, skills, and attitudes necessary to use information and communication technology, and in particular telemedicine, in their clinical practices.[38]
This study proposes an innovative clinical pathway for patient management in territorial services, considering citizens’ preferences. CM could represent a valid collaborator of the GP, improving the relationship between operator/patient/family and maintaining unaltered quality of treatments. Finally, CM could be useful to improve continuity and personalization of care, especially in patients affected by chronic neurological disorders. The investigation of this innovative path, considering the complex socio-economic and geographic territorial problems of Sicily, could make the local health service more equitable and accessible, to guarantee containment of healthcare-costs, and improve resource allocation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient (s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Appendix 1: Shows the semistructured interview we administered during the International Nursing Day.
1. Patient's civil status (married, single, divorced, widowed)
2. Education (primary school, secondary school, high school diploma, bachelor's degree, doctoral degree, others)
3. Job (pensioner, unemployed, student, office worker, housewife, teacher, businessman, others)
4. Do you have one of the following illness? Hypertension, diabetes, heart or lung disease, kidney or liver disease, osteo-arthrosis/arthritis/porosis, stroke, tumor, depression and/or anxiety.
5. When you feel seek, you refer to. (General practioner, Physician on call, pharmacist, home health nurse, emergency physician, ambulatory specialists, private physician, relatives and friends)
6. Please, specify the reason why you choose to this person
7. When was the last time do you refer to a physician? (today/yesterday, some day ago, 1–2 weeks ago, 3–4 weeks ago, 1–3 months ago, more than 3 months ago, last year)
8. Please specify the reason why you went to the doctor/hospital
9. Do you think that helthcare service was of adeguate quality?
10. Explain your answer
11. Give a score in a 0 (the worst) to 10 (the best) scale to the following healthcare professionals: General practitioner, Physician on call, pharmacist, home health nurse, emergency physician, ambulatory specialists
12. Please, give some advice to improve the service.
References
- 1.Rico A, Saltman RB, Boerma WG. Organizational restructuring in European health systems: The role of primary care. Social Policy Adm. 2003;37:592–608. [Google Scholar]
- 2.Saltman R, Bankauskaite V, Vrangbaek K. UK: McGraw-Hill Education; 2005. Primary Care in the Driver's Seat? Organizational Reform in European Primary Care. [Google Scholar]
- 3.Schäfer WL, Boerma WG, Spreeuwenberg P, Schellevis FG, Groenewegen PP. Two decades of change in European general practice service profiles: Conditions associated with the developments in 28 countries between 1993 and 2012. Scand J Prim Health Care. 2016;34:97–110. doi: 10.3109/02813432.2015.1132887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Levesque JF, Harris MF, Scott C, Crabtree B, Miller W, Halma LM, et al. Dimensions and intensity of inter-professional teamwork in primary care: Evidence from five international jurisdictions. Fam Pract. 2018;35:285–94. doi: 10.1093/fampra/cmx103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seghieri C, Mengoni A, Nuti S. Applying discrete choice modelling in a priority setting: An investigation of public preferences for primary care models. Eur J Health Econ. 2014;15:773–85. doi: 10.1007/s10198-013-0542-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fattore G, Frosini F, Salvatore D, Tozzi V. Social network analysis in primary care: The impact of interactions on prescribing behaviour. Health Policy. 2009;92:141–8. doi: 10.1016/j.healthpol.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 7.De Cola MC, Lo Buono V, Mento A, Foti M, Marino S, Bramanti P, et al. Unmet needs for family caregivers of elderly people with dementia living in Italy: What do we know so far and what should we do next? Inquiry. 2017;54:46958017713708. doi: 10.1177/0046958017713708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lamarche PA, Beaulieu MD, Pineault R, Contandriopoulos AP, Denis JL, Haggerty J. Ottawa: Canadian Health Services Research Foundation; 2003. Choices for Change: The Path for Restructuring Primary Healthcare Services in Canada. [Google Scholar]
- 9.Calabrò RS, Bramanti A, Garzon M, Celesti A, Russo M, Portaro S, et al. Telerehabilitation in individuals with severe acquired brain injury: Rationale, study design, and methodology. Medicine (Baltimore) 2018;97:e13292. doi: 10.1097/MD.0000000000013292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bramanti A, Manuli A, Calabrò RS. Stroke telerehabilitation in Sicily: A cost-effective approach to reduce disability? Innov Clin Neurosci. 2018;15:11–5. [PMC free article] [PubMed] [Google Scholar]
- 11.De Cola MC, De Luca R, Bramanti A, Bertè F, Bramanti P, Calabrò RS. Tele-health services for the elderly: A novel southern Italy family needs-oriented model. J Telemed Telecare. 2016;22:356–62. doi: 10.1177/1357633X15604290. [DOI] [PubMed] [Google Scholar]
- 12.Gilboa Y, Maeir T, Karni S, Eisenberg ME, Liebergall M, Schwartz I, et al. Effectiveness of a tele-rehabilitation intervention to improve performance and reduce morbidity for people post hip fracture-study protocol for a randomized controlled trial. BMC Geriatr. 2019;19:135. doi: 10.1186/s12877-019-1141-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Luca R, Bramanti A, De Cola MC, Trifiletti A, Tomasello P, Torrisi M, et al. Tele-health-care in the elderly living in nursing home: The first Sicilian multimodal approach. Aging Clin Exp Res. 2016;28:753–9. doi: 10.1007/s40520-015-0463-8. [DOI] [PubMed] [Google Scholar]
- 14.Maresca G, De Cola MC, Caliri S, De Luca R, Manuli A, Scarcella I, et al. Moving towards novel multidisciplinary approaches for improving elderly quality of life: The emerging role of telemedicine in Sicily. J Telemed Telecare. 2018 doi: 10.1177/1357633X17753057. doi: 10.1177/1357633X17753057. [DOI] [PubMed] [Google Scholar]
- 15.Gerard K, Salisbury C, Street D, Pope C, Baxter H. Is fast access to general practice all that should matter? A discrete choice experiment of patients’ preferences. J Health Serv Res Policy. 2008;13(Suppl 2):3–10. doi: 10.1258/jhsrp.2007.007087. [DOI] [PubMed] [Google Scholar]
- 16.Hole AR. Modelling heterogeneity in patients’ preferences for the attributes of a general practitioner appointment. J Health Econ. 2008;27:1078–94. doi: 10.1016/j.jhealeco.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 17.Pedersen LB, Kjær T, Kragstrup J, Gyrd-Hansen D. Do general practitioners know patients’ preferences? An empirical study on the agency relationship at an aggregate level using a discrete choice experiment. Value Health. 2012;15:514–23. doi: 10.1016/j.jval.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 18.Caldow J, Bond C, Ryan M, Campbell NC, Miguel FS, Kiger A, Lee A. Treatment of minor illness in primary care: A national survey of patient satisfaction, attitudes and preferences regarding a wider nursing role. Health Expect. 2007;10:30–45. doi: 10.1111/j.1369-7625.2006.00422.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Turner D, Tarrant C, Windridge K, Bryan S, Boulton M, Freeman G, et al. Do patients value continuity of care in general practice? An investigation using stated preference discrete choice experiments. J Health Serv Res Policy. 2007;12:132–7. doi: 10.1258/135581907781543021. [DOI] [PubMed] [Google Scholar]
- 20.Batbaatar E, Dorjdagva J, Luvsannyam A, Amenta P. Conceptualisation of patient satisfaction: A systematic narrative literature review. Perspect Public Health. 2015;135:243–50. doi: 10.1177/1757913915594196. [DOI] [PubMed] [Google Scholar]
- 21.Kumar R, Chattu VK. What is in the name? Understanding terminologies of patient-centered, person-centered, and patient-directedcare! J Family Med Primary Care. 2018;7:487–8. doi: 10.4103/jfmpc.jfmpc_61_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Purdy D, Hardwick C. Seeing double: Expanding GP capacity through teamwork and redesign. Br J Gen Pract. 2018;68:29. doi: 10.3399/bjgp17X694217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chin WY, Lam CL, Lo SV. Quality of care of nurse-led and allied health personnel-led primary care clinics. Hong Kong Med J. 2011;17:217–30. [PubMed] [Google Scholar]
- 24.Starfield B, Horder J. Interpersonal continuity: Old and new perspectives. Br J Gen Pract. 2007;57:527–9. [PMC free article] [PubMed] [Google Scholar]
- 25.Rubin G, Bate A, George A, Shackley P, Hall N. Preferences for access to the GP: A discrete choice experiment. Br J Gen Pract. 2006;56:743–8. [PMC free article] [PubMed] [Google Scholar]
- 26.Bellentani M, Di Stanislao F, Padovano P, Visca M, Pecci F, Mannucci F, et al. Italy: Agenas; 2009. Stato di attuazione dei modelli innovativi di assistenza primaria nelle Regioni italiane. [Google Scholar]
- 27.Wilton P, Smith RD. Primary care reform: A three country comparison of ‘budget holding’. Health Policy. 1998;44:149–66. doi: 10.1016/s0168-8510(98)00020-7. [DOI] [PubMed] [Google Scholar]
- 28.Gerard K, Lattimer V, Surridge H, George S, Turnbull J, Burgess A, et al. The introduction of integrated out-of-hours arrangements in England: A discrete choice experiment of public preferences for alternative models of care. Health Expect. 2006;9:60–9. doi: 10.1111/j.1369-7625.2006.00365.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Scott A, Watson MS, Ross S. Eliciting preferences of the community for out of hours care provided by general practitioners: A stated preference discrete choice experiment. Soc Sci Med. 2003;56:803–14. doi: 10.1016/s0277-9536(02)00079-5. [DOI] [PubMed] [Google Scholar]
- 30.Gerard K, Lattimer V, Turnbull J, Smith H, George S, Brailsford S, et al. Reviewing emergency care systems 2: Measuring patient preferences using a discrete choice experiment. Emerg Med J. 2004;21:692–7. doi: 10.1136/emj.2002.003707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.ISTAT AS. Istituto Nazionale di statistica. 2015 [Google Scholar]
- 32.Geurts-Laurant MG, Reeves D, Hermens RP, Braspenning JC, Grol RP, Sibbald BS. Substitution of doctors by nurses in primary care. Cochrane Database Syst Rev. 2005:CD001271. doi: 10.1002/14651858.CD001271.pub2. [DOI] [PubMed] [Google Scholar]
- 33.Tahan HM. To exist as a case manager is to constantly change; to be successful, you must constantly adapt. Prof Case Manag. 2018;23:103–6. doi: 10.1097/NCM.0000000000000287. [DOI] [PubMed] [Google Scholar]
- 34.Beijer LJ, Rietveld AC. Asynchronous telemedicine applications in the rehabilitation of acquired speech-language disorders in neurological patients. Smart Homecare Technol Telehealth. 2015;3:39–48. [Google Scholar]
- 35.Scriven H, Doherty DP, Ward EC. Evaluation of a multisite telehealth group model for persistent pain management for rural/remote participants. Rural Remote Health. 2019;19:4710. doi: 10.22605/RRH4710. [DOI] [PubMed] [Google Scholar]
- 36.Weinstein RS, Lopez AM, Joseph BA, Erps KA, Holcomb M, Barker GP, et al. Telemedicine, telehealth, and mobile health applications that work: Opportunities and barriers. Am J Med. 2014;127:183–7. doi: 10.1016/j.amjmed.2013.09.032. [DOI] [PubMed] [Google Scholar]
- 37.Flodgren G, Rachas A, Farmer AJ, Inzitari M, Shepperd S. Interactive telemedicine: Effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2015:CD002098. doi: 10.1002/14651858.CD002098.pub2. doi: 10.1002/14651858.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rutledge CM, Kott K, Schweickert PA, Poston R, Fowler C, Haney TS. Telehealth and eHealth in nurse practitioner training: Current perspectives. Adv Med Educ Pract. 2017;8:399–409. doi: 10.2147/AMEP.S116071. [DOI] [PMC free article] [PubMed] [Google Scholar]