Abstract
Primary pyogenic ventriculitis is more commonly manifested in children. Its presentation in adults due to Streptococcus pneumonia is rarely reported. It is mainly due to adequate vaccination cover and initiation of appropriate antibiotics. Ventriculitis is one of the complications of bacterial meningitis, requires long-term antibiotics and surgical intervention. Here, we are reporting a 67-year-old diabetic lady presented with a decrease in sensorium, seizure, and fever, diagnosed as bacterial ventriculitis. Her cerebro spinal fluid (CSF) picture suggestive of pyogenic meningitis, CSF, blood culture grew Streptoccous pneumoniae; MRI revealed –ventriculitis. She was treated with Injection Ceftriaxazone for 6 week duration. Serial MRI showed clearing of ventricular debris and she improved. This highlights the atypical presentation of pyogenic meningitis without nuchal rigidity, status epilepticus, and clinical improvement without the need of surgical intervention.
Keywords: Pyogenic meningitis, streptococus pneumoniae, ventriculitis
Case Details
A 66-year-old lady brought to an emergency with a history of decrease in sensorium since morning for the last 5 h duration; She had 1 episode of vomiting. On arrival to the emergency room, she had 1 episode of seizure with worsening of sensorium. There was no history of fever, headache, blurring of vision, and weakness of limbs preceding the event. She was known diabetic and on regular medication.
On examination – she was moving her limbs with painful stimuli, no spontaneous eye-opening, not responding to oral commands. Her BP was 130/90 mmHg, pulse-110/min, Temperature-1000 F. Considering her low GCS continuous seizure, she was paralyzed, intubated, and mechanical ventilation was given. Her pupils were bilaterally reacting to light. Fundus showed bilateral early papilledema. There was no neck stiffness. Deep tendon reflexes were diminished. Bilateral plantar was no response. Diabetic patient with acute onset decrease in sensorium andseizure –we considered massive cerebrovascular event at this point. Her emergency computed tomography (CT) of the brain was done, which ruled out intracranial bleed. She was admitted in the intensive care unit and was on ventilatory support. Her blood investigation revealed-elevated total counts 23,000 cells/cumm with neutrophilic predominance. Hence, suspected of pyogenic meningitis. Cerebrospinal fluid (CSF) analysis was done, which was turbid and showed elevated total counts 5,760 cells with polymorphic predominance, low glucose 2 mg/dL with elevated protein-277 gm% suggestive of pyogenic meningitis. She was initiated on Injection Ceftriaxazone 2 gm iv twice daily and Injection Dexamethzone 6 gm iv thrice daily for 3 days. She underwent magnetic resonance imaging (MRI) of brain –which showed intraventricular T2/FLAIR hyperintensity with mild diffusion restriction and fluid-fluid level in the dependant portion of the occipital horn of bilateral ventricles - which was suggestive of ventriculitis [Figure 1].
Figure 1.
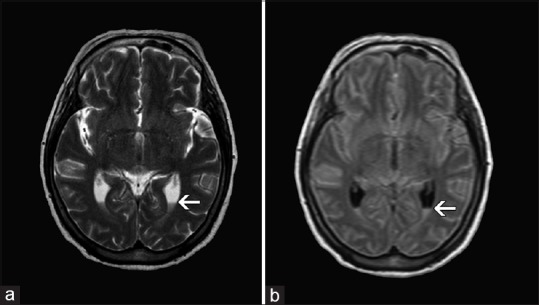
Magnetic resonance imaging of brain T2W image (a), FLAIR image (b) showing intra ventricular hyperintensity and fluid level in the dependent portion of occipital horn of bilateral lateral ventricle
CSF gram stain showed plenty of polymorphs and gram-positive capsulated cocci in pairs suggestive of Streptococcal pneumoniae. Injection Penicillin 4 mU q 4 hourly was given for 14 days. Her blood culture also grew S. pneumoniae, which was sensitive to Injection Ceftriaxazone. Considering her prolong ventilator support, treacheostomy was done. As there was not much of clinical improvement, repeat cerebrospinal fluid analysis was done after 2 week, which revealed a decrease in total counts 28 cells/cumm. Repeat MRI brain was done after 3 week, which showed resolving ventriculitis [Figure 2].
Figure 2.
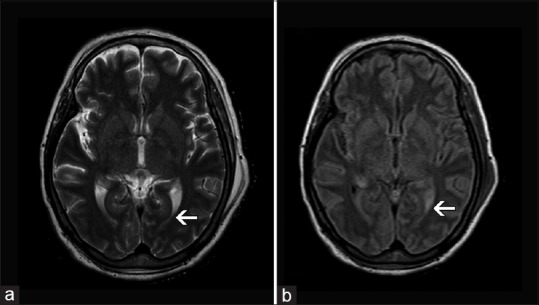
Magnetic resonance imaging of brain T2W image (a), FLAIR image (b) showing clearing of fluid level-ventriculitis
Her parenteral antibiotics Injection Ceftriaxazone was continued for 6 week period. From 3 rd week onwards, her sensorium gradually improved; she was weaned from ventilator and discharged at the fourth week. On discharge, she was moving all four limbs, responding to commands, continued physiotherapy for ambulation.
Discussion
Ventriculitis is a suppurative infection of ventricles usually occurring secondary to shunt/catheter-related infections. It is also known as ventricular empyema, pyocephalus, and ependymitis. Common causes of ventriculitis are post-trauma, ventricular drain, shunt, surgery, ruptured abscess, immunocompromised patients. It can also occur as a complication of meningitis. Primary bacterial ventriculitis is commonly reported in children.[1] In adults, it is rarely reported.
Gronthoud et al., has reported six cases of primary pyogenic ventriculitis in adult.[2] Primary pyogenic ventriculitis due to streptococcus pneumoniae in an adult with full clinical recovery is not reported earlier.
This present case does not present with classical signs of meningeal involvement-nuchal rigidity. Even clinical signs of meningitis were reported in 76% of cases with ventriculitis.[3] At primary care level, the presentation of pyogenic meningitis without signs of meningeal irritation should be highlighted, so that the need of CSF analysis and initiation of appropriate antibiotics would not be delayed. Among the reported six cases of pyogenic ventriculitis in adults, only one patient had nuchal rigidity.[2] Hence, in all pyogenic meningitis not responding to initial antibiotics or poor GCS at presentation as in our patient should undergo evaluation for underlying ventriculitis complicating pyogenic meningitis.
Among the reported cases of ventriculitis, gram-negative organism was 60% in nosocomial ventriculitis, followed by staphylococcus species.[4] ventriculitis complicating meningitis was commonly presented in neonates. Organism commonly reported in neonates are Streptococus bovis, S. gallolyticus, and S. intermedius.[5,6,7] In adults, primary ventriculitis caused by Nisseria meningitis,[3,8] Streptococus acidominicus,[9] and S. agalactiae[10] has been reported.
MRI brain has a major role in diagnosing ventriculitis. MRI features specific for ventriculitis are ventricular debris, hydrocephalus, periventricular hyperintense signals, and ependymal enhancement. Among these MRI findings, irregular ventricular debris is seen commonly (94%) and ependymal enhancement manifest less frequently (60%).[11] In diagnosed case of pyogenic meningitis, if there is not much of improvement, we should suspect ventriculitis. Because patients with ventriculitis require long-term antibiotics, 4–6 weeks duration may require surgical intervention for obstructive hydrocephalus. If it is not suspected earlier, the mortality and neurological sequelae related to the infection is more.
Specific guidelines are available for health care-associated ventriculitis. However, in primary bacterial ventriculitis, the decision of antibiotics and duration depends upon the organism and clinical response to the antibiotics. In all reported cases, the duration of antibiotics was decided according to clinical recovery and CSF and MRI resolution, which was ranging from 3 to 6 weeks period. In a Japanese report, even 49 days of antibiotics for penicillin-sensitive Streptococcus pneumoniae did not show clinical recovery, as there was a low conscious level at initiation of antibiotics.[12] Streptococcal infection is commonly treated with Injection Ceftriaxazone and Injection Penicillin.[13] The reported Neissieria related ventriculitis was treated with parenteral third-generation cephalosporin for 2 weeks followed by oral Tablet Levofloxacon and Tablet Moxifloxacin for 4 weeks showed marked clinical recovery.[3] Prevention of infection is the most important aspect of management. High-risk patients, all diabetic patients more than 60 years of age should be advised for the pneumococcal vaccine as part of adult vaccination policy.
Conclusion
The classical teaching of meningitis is signs of meningial irritation - nuchal rigidity. Our case highlights the rare presentation of pyogenic meningitis without nuchal rigidity and role of MRI imaging to identify the complications of pyogenic meningitis such as ventriculitis. Initiation of appropriate earlier antibiotics for longer durations has favorable outcomes without the need of neurosurgical intervention.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We wish to thank the Department of Microbiology and Radiology for their support in diagnosis.
References
- 1.Harris L, Munakomi S. Ventriculitis. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. 2019. [Updated 2019 Sep 12]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544332 .
- 2.Gronthoud F, Hassan I, Newton P. Primary pyogenic ventriculitis caused byNeisseria meningitis: Case report and review of the literature. JMM Case Rep. 2017;4:e005078. doi: 10.1099/jmmcr.0.005078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lesourd A, Magne N, Soares A, Lemaitre C, Taha MK, Gueit I, et al. Primary bacterial ventriculitis in adults, an emergent diagnosis challenge: Report of ameningoccal case and review of the literature. BMC Infect Dis. 2018;18:226. doi: 10.1186/s12879-018-3119-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agrawal A, Cincu R, Timothy J. Current concepts and approach to ventriculitis. Infect Dis Clin Pract. 2008;16:100–4. [Google Scholar]
- 5.Seimiya Y, Ohshima K, Itoh H, Ogasawara N, Okutomo M, Tanaka S. Clinicopathology of meningoventriculitis due to Streptococcus bovis infection in neonatal calves. J Vet Med Sci. 1992;54:871–4. doi: 10.1292/jvms.54.871. [DOI] [PubMed] [Google Scholar]
- 6.Yamamura Y, Mihara Y, Nakatani K, Nishiguchi T, Ikebe T. Unexpected ventriculitis complication of neonatal meningitis caused by Streptococcus gallolyticussubsp.pasteurianus: ACase Report. Jpn J Infect Dis. 2018;71:68–71. doi: 10.7883/yoken.JJID.2017.053. [DOI] [PubMed] [Google Scholar]
- 7.Vajramani G, Akrawi H, Jones G, Sparrow O. Primary ventriculitis caused byStreptococcus intermedius. Br J Neurosurg. 2007;21:293–6. doi: 10.1080/02688690701246129. [DOI] [PubMed] [Google Scholar]
- 8.Bajaj D, Agrawal A, Gandhi D, Varughese R, Gupta S, Regelmann D. Intraventricular empyema caused byNeisseria meningitidis. IDCases. 2019;15:e00503. doi: 10.1016/j.idcr.2019.e00503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shah GS. Pyogenic ventriculitis and meningitis caused by Streptococcus acidominimus in humans: A case report. Am J Case Rep. 2018;19:329–34. doi: 10.12659/AJCR.908000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ito T, Koiwa H, Watanabe K, Yoshida T, Hamada K, Ito A. Life-threatening pyogenic ventriculitis, complicating endocarditis, presenting as sudden hearing loss. Oxf Med Case Rep2019. 2019 doi: 10.1093/omcr/omz044. omz044.doi: 10.1093/omcr/omz044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fukui MB, Williams RL, Mudigonda S. CT and MR imaging features of pyogenic ventriculitis. Am J Neuroradiol. 2001;22:1510–6. [PMC free article] [PubMed] [Google Scholar]
- 12.Tokimura R, Iguchi M, Ito E, Murakami T, Ugawa Y. The duration of antibiotic therapy in bacterial meningitis with pyogenic ventriculitis. RinshoShinkeigaku. 2019;59:133–8. doi: 10.5692/clinicalneurol.cn-001210. [DOI] [PubMed] [Google Scholar]
- 13.Farooq H, HtunZM Pyogenic ventriculitis: An unusual complication of streptococcal meningitis. Crit Care Med. 2019;47:275. [Google Scholar]


