Abstract
Objective:
To document the rates of intentional self-harm and mental disorders among youths aged 13 to 17 years visiting Ontario emergency departments (EDs) from 2003-2017.
Methods:
This was a repeated cross-sectional observational design. Outcomes were rates of adolescents with (1) at least 1 self-harm ED visit and (2) a visit with a mental disorder code.
Results:
Rates of youths with self-harm visits fell 32% from 2.6/1000 in 2003 to 1.8 in 2009 but rose 135% to 4.2 by 2017. The slope of the trend in self-harm visits changed from –0.18 youths/1000/year (confidence interval [CI], –0.24 to –0.13) during 2003 to 2009 to 0.31 youths/1000/year (CI, 0.27 to 0.35) during 2009 to 2017 (P < 0.001). Rates of youths with mental health visits rose from 11.7/1000 in 2003 to 13.5 in 2009 (15%) and to 24.1 (78%) by 2017. The slope of mental health visits changed from 0.22 youths/1000/year (CI, 0.02 to 0.42) during 2003 to 2009 to 1.84 youths/1000/year (CI, 1.38 to 2.30) in 2009 to 2017 (P < 0.001). Females were more likely to have self-harm (P < 0.001) and mental health visits (P < 0.001). Rates of increase after 2009 were greater for females for both self-harm (P < 0.001) and mental health (P < 0.001).
Conclusions:
Rates of adolescents with self-harm and mental health ED visits have increased since 2009, with greater increases among females. Research is required on the determinants of adolescents’ self-harm and mental health ED visits and how they can be addressed in that setting. Sufficient treatment resources must be supplied to address increased demands for services.
Keywords: child and adolescent psychiatry, self-harm, suicide, emergency service, hospital, mental health, sex differences
Abstract
Objectif:
Documenter les taux d’automutilation intentionnelle et des troubles mentaux chez les adolescents de 13 à 17 ans qui se sont présentés aux services d’urgence (SU) de l’Ontario entre 2003 et 2017.
Méthodes:
Il s’agit d’une étude transversale répétée par observation. Les résultats étaient les taux des adolescents ayant a) au moins une visite au SU pour automutilation et b) une visite pour un code de trouble mental.
Résultats:
Les taux des visites d’adolescents pour automutilation ont chuté de 32%, de 2,6/1000 en 2003 à 1,8 en 2009, mais ont augmenté de 135% pour atteindre 4,2 en 2017. La pente de la ligne de tendance des visites pour automutilation est passée de -0,18 adolescents/1000/année (IC = [-0,24 à -0,13]) pour la période de 2003 à 2009, à 0,31 adolescents/1000/année (IC = [0,27 à 0,35]) de 2009 à 2017 (P < 0,001). Les taux des visites d’adolescents pour raison de santé mentale ont augmenté de 11,7/1000 en 2003 à 13,5 en 2009 (15%) et à 24,1 (78%) en 2017. La pente des visites pour santé mentale est passée de 0,22 adolescents/1000/année (IC = [0,02 à 0,42]) pour la période de 2003 à 2009 à 1,84 adolescents/1000/année (IC = [1,38 à 2,30]) de 2009 à 2017 (P < 0,001). Les filles étaient plus susceptibles de présenter l’automutilation (P < 0,001) et des visites pour santé mentale (P < 0,001). Les taux d’augmentation d’après 2009 étaient plus élevés chez les filles tant pour l’automutilation (P < 0,001) que la santé mentale (P < 0,001).
Conclusions:
Les taux des adolescents comptant des visites au SU pour raisons d’automutilation et de santé mentale se sont accrus depuis 2009, et ces augmentations sont plus marquées chez les filles. Il faut une recherche sur les déterminants des visites au SU des adolescents pour raison d’automutilation et de santé mentale et sur la manière de les aborder dans ce contexte. Des ressources de traitement suffisantes doivent être fournies pour répondre aux demandes de services accrues.
Background
Self-harm is the deliberate attempt to injure oneself, regardless of intent.1 Adolescents who self-harm are at risk for repeated self-harm or suicide.2–6 Adolescent emergency department (ED) visits with self-harm have been increasing in recent years in many jurisdictions,7–9 including Canada.10 ED visits by adolescents for mental disorders have likewise been increasing in many countries,11–14 including Canada.15,16 The increasing numbers of adolescents who access the ED following self-harm or for mental disorders are of concern because the ED is not an ideal setting for delivery of mental health care or for care of adolescents who have self-harmed. Studying population trends in visits for self-harm or mental disorders is also important because fluctuations in these trends may reflect significant changes in the social conditions affecting adolescent health and may provide direction for targeted interventions.
Hence, the objectives of this study were to examine temporal trends in rates of youths having self-harm and mental health ED visits in Ontario, a large Canadian province with centralized administrative records of all ED visits. Because sex effects are pronounced in adolescent self-harm17,18 and mental health,19 for both objectives, we fit models that permitted us to identify sex and sex by time effects.
Method
Study Design, Setting, and Participants
This is a repeated annual cross-sectional study of Ontario ED visits by youths aged 13 to 17 years (inclusive) between 2003 and 2017. We chose this age range because it falls clearly in adolescence, the period in which self-harming behaviors are believed to be the most common.20 In a previous Canadian study of self-harm,21 the mean age of onset of self-harm was 15.2 years. Participants were all such adolescents with an Ontario Health Insurance Plan number presenting to a provincial ED. This research was approved by the Children’s Hospital of Eastern Ontario Research Ethics Board.
Variables and Data Sources
Data on ED visits were obtained from the Canadian National Ambulatory Care Reporting System (NACRS) database from the Canadian Institute for Health Information, using the International Classification of Diseases, 10th Revision (ICD-10).22 The data were accessed through health administrative databases at ICES (Toronto, Ontario). NACRS records are produced by coders who abstract the documentation generated by ED clinicians.23 These records are subject to several forms of error, including inaccurate or incomplete documentation of problems by physicians and errors in coding and abstraction of data from clinical records. Gibson and her colleagues23 studied the quality of NACRS data by carrying out reabstractions of charts at several Ontario EDs and found agreement rates for ICD-10 codes that ranged from 86% to 90%. Chart review studies indicate that some injuries and poisonings that are coded as having an undetermined cause are actually instances of intentional self-harm.24,25 Moreover, NACRS coders may record only the main diagnostic code that led to the ED visit, meaning that a mental health disorder or a self-injury might be omitted if another medical problem took precedence. This means that estimates of the prevalence of diagnoses in the ED setting are likely biased downwards.
The Registered Persons Database was used to link ED youth records with demographic information including age, sex, rurality, neighborhood income quintile, and postal code. The Ontario population by year, age, and sex was obtained from the intercensal and postcensal population estimates for census divisions by Statistics Canada held by the Ontario Ministry of Health and Long-Term Care. These data sets were linked using unique encoded identifiers and analyzed at ICES.
In this study, self-harm visits had ICD-10 codes X7 or X80-X84 (self-injuries) or X6 (self-poisoning). Mental health visits had any ICD-10 F code.
Statistical Methods
Rates of youths with self-harm and mental health ED visits were calculated per 1000 adolescents in the population. For example, the dependent variable of rates of youths with at least 1 self-harm visit in year t was calculated for the years 2003 through 2017 as follows:
Rates of mental health visits were defined similarly.
Exploratory data analyses suggested that the trends in self-harm and mental health visits changed slope on or around 2009. To model this, we created 2 time variables:
and
and enabled us to capture changes in trajectory occurring in 2009 using discontinuity models.26 We also included and terms in our regressions to capture nonlinear time trends. The quadratic terms were nonsignificant except for rates of youths with mental health ED visits during 2009 to 2017 and were dropped from the other regressions. To examine sex effects, we created a dummy variable, S, which was 1 for females and –1 for males. Sex × Time interaction terms were created by multiplying S by the time variables. To check for serial correlation, we fit each regression using generalized least squares with an autoregressive lag-1 covariance structure in the residuals. The 95% confidence intervals for the coefficient of serial correlation () always included zero, so we have reported ordinary least squares results (which were nearly identical to generalized least squares estimates).
Models were fit using R 3.5.1.27 All confidence intervals are 95%, and all P values are 2-tailed.
Results
Participants
From 2003 to 2017, an average of 190,384 (SD = 4662) Ontario adolescents visited Ontario EDs in a given year. Table 1 reports demographic characteristics for adolescents who had or did not have a self-harm visit in the years 2003, 2009, and 2017. Table 2 presents demographic characteristics for adolescents who had or did not have a mental health visit.
Table 1.
Ontario Adolescents with a Self-Harm Emergency Department (ED) Visit.
| 2003 | 2009 | 2017 | |||||
|---|---|---|---|---|---|---|---|
| Self-Harm Code on Visit? | Self-Harm Code on Visit? | Self-Harm Code on Visit? | |||||
| Yes | No | Yes | No | Yes | No | ||
| n | 1592 | 172,447 | 1094 | 186,486 | 2295 | 167,264 | |
| Age, y, mean ± SD | 15.44 ± 1.24 | 15.03 ± 1.44 | 15.52 ± 1.23 | 15.08 ± 1.43 | 15.44 ± 1.28 | 15.04 ± 1.44 | |
| Neighborhood income quintile, n (%) | Missing | 25 (1.6) | 1,922 (1.1) | 15 (1.4) | 1,979 (1.1) | 23 (1.0) | 712 (0.4) |
| 1 | 310 (19.5) | 32,017 (18.6) | 255 (23.3) | 34,942 (18.7) | 556 (24.2) | 30,864 (18.5) | |
| 2 | 343 (21.5) | 33,025 (19.2) | 222 (20.3) | 35,316 (18.9) | 397 (17.3) | 30,325 (18.1) | |
| 3 | 316 (19.8) | 34,677 (20.1) | 204 (18.6) | 37,525 (20.1) | 455 (19.8) | 33,417 (20.0) | |
| 4 | 296 (18.6) | 35,871 (20.8) | 208 (19.0) | 39,113 (21.0) | 438 (19.1) | 34,955 (20.9) | |
| 5 | 302 (19.0) | 34,935 (20.3) | 190 (17.4) | 37,611 (20.2) | 426 (18.6) | 36,991 (22.1) | |
| Sex, n (%) | Female | 1182 (74.2) | 79,135 (45.9) | 816 (74.6) | 88,642 (47.5) | 1837 (80.0) | 82,537 (49.3) |
| Male | 410 (25.8) | 93,312 (54.1) | 278 (25.4) | 97,844 (52.5) | 458 (20.0) | 84,727 (50.7) | |
| Rural, n (%) | Missing | 15 (0.9) | 1,263 (0.7) | 7 (0.6) | 750 (0.4) | 22 (1.0) | 665 (0.4) |
| No | 1294 (81.3) | 128,438 (74.5) | 855 (78.2) | 146,031 (78.3) | 1853 (80.7) | 138,213 (82.6) | |
| Yes | 283 (17.8) | 42,746 (24.8) | 232 (21.2) | 39,705 (21.3) | 420 (18.3) | 28,386 (17.0) | |
The table reports demographic characteristics of adolescents who had at least 1 ED visit during the years 2003, 2009, and 2017. Demographics are reported separately for adolescents with at least 1 self-harm visit and separately for all other youths with ED visits. The years 2003 and 2017 were selected because they were the starting point and endpoint of our data series, and 2009 was selected because it was the year when the slope of the trend changed. However, our regression models in Tables 3 and 4 and Figure 1 are based on the entire series of annual rates from 2003 to 2017.
Table 2.
Ontario Adolescents with a Mental Health Emergency Department (ED) Visit.
| 2003 | 2009 | 2017 | |||||
|---|---|---|---|---|---|---|---|
| Mental Health Code on Visit? | Mental Health Code on Visit? | Mental Health Code on Visit? | |||||
| Yes | No | Yes | No | Yes | No | ||
| n | 9131 | 172,447 | 11,223 | 186,486 | 17,696 | 167,264 | |
| Age, y, mean ± SD | 15.40 ± 1.31 | 15.03 ± 1.44 | 15.46 ± 1.30 | 15.08 ± 1.43 | 15.43 ± 1.33 | 15.04 ± 1.44 | |
| Neighborhood income quintile, n (%) | Missing | 122 (1.3) | 1922 (1.1) | 184 (1.6) | 1979 (1.1) | 140 (0.8) | 712 (0.4) |
| 1 | 1960 (21.5) | 32,017 (18.6) | 2468 (22.0) | 34,942 (18.7) | 3857 (21.8) | 30,864 (18.5) | |
| 2 | 1909 (20.9) | 33,025 (19.2) | 2212 (19.7) | 35,316 (18.9) | 3372 (19.1) | 30,325 (18.1) | |
| 3 | 1799 (19.7) | 34,677 (20.1) | 2109 (18.8) | 37,525 (20.1) | 3451 (19.5) | 33,417 (20.0) | |
| 4 | 1702 (18.6) | 35,871 (20.8) | 2196 (19.6) | 39,113 (21.0) | 3403 (19.2) | 34,955 (20.9) | |
| 5 | 1639 (17.9) | 34,935 (20.3) | 2054 (18.3) | 37,611 (20.2) | 3473 (19.6) | 36,991 (22.1) | |
| Sex, n (%) | Female | 5335 (58.4) | 79,135 (45.9) | 6460 (57.6) | 88,642 (47.5) | 11,048 (62.4) | 82,537 (49.3) |
| Male | 3796 (41.6) | 93,312 (54.1) | 4763 (42.4) | 97,844 (52.5) | 6648 (37.6) | 84,727 (50.7) | |
| Rural, n (%) | Missing | 69 (0.8) | 1,263 (0.7) | 69 (0.6) | 750 (0.4) | 132 (0.7) | 665 (0.4) |
| No | 7,413 (81.2) | 128,438 (74.5) | 9,202 (82.0) | 146,031 (78.3) | 14,910 (84.3) | 138,213 (82.6) | |
| Yes | 1,649 (18.1) | 42,746 (24.8) | 1,952 (17.4) | 39,705 (21.3) | 2,654 (15.0) | 28,386 (17.0) | |
This table reports demographic characteristics of adolescents who had at least 1 ED visit during the years 2003, 2009, and 2017. Demographics are reported separately for adolescents with at least 1 mental health visit and separately for all other youths with ED visits. The years 2003 and 2017 were selected because they were the starting point and endpoint of our data series, and 2009 was selected because it was the year when the slope of the trend changed. However, our regression models in Tables 3 and 4 and Figure 1 are based on the entire series of annual rates from 2003 to 2017.
Self-Harm Visit Rates
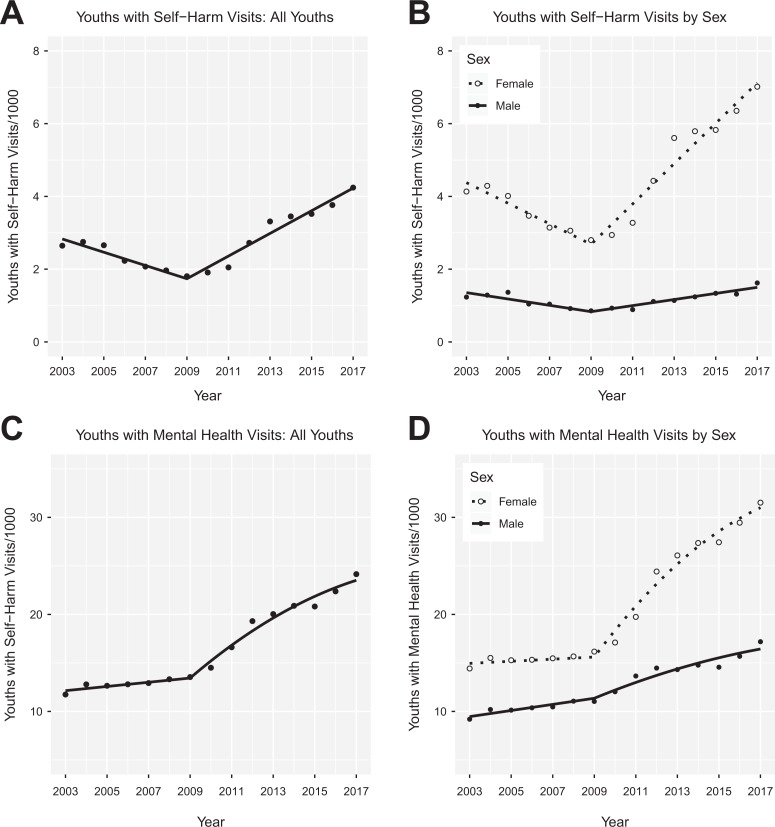
Figure 1A shows the trends for rates of adolescents having at least 1 self-harm ED visit. From 2003 to 2017, in an average year, 2.7 adolescents/1000 had an ED visit with intentional self-harm (CI, 2.1 to 3.5). Rates of youths with self-harm visits fell 32% from 2.6/1000 youths in 2003 to 1.8/1000 youths in 2009 and then rose 135% to 4.2/1000 youths from 2009 to 2017. The “All Youths” column in Table 3 presents the results of a regression discontinuity model fit to these data. From 2003 to 2009, the rate of adolescents with self-harm visits declined by –0.18 youths/1000/year (CI, –0.24 to –0.13), whereas from 2009 to 2017, they rose by 0.31 youths/1000/year (CI, 0.27 to 0.35). The change in the slope at 2009 was 0.49 youths/1000/year2 (CI, 0.41 to 0.58; P < 0.001).
Figure 1.
Rates of adolescents with self-harm emergency department (ED) visits: 2003 to 2017. (A) Rates of adolescents having a self-harm ED visit, per thousand adolescents in the population, as a function of time. The fitted lines are from the discontinuity regression reported in the “All Youths” columns of Table 3. (B) Rates of adolescents having a self-harm ED visit by sex. The fitted lines are from the regression reported in the “By Sex” columns of Table 3. (C) Rates of adolescents having a mental health ED visit. The fitted lines are from the regression reported in the “All Youths” columns of Table 4. A quadratic term is included in the regression model for mental health visits for year ≥2009. (D) Rates of adolescents having a self-harm ED visit by sex. The fitted lines are from the regression reported in the “By Sex” columns of Table 4.
Table 3.
Discontinuity Regressions for Rates of Youths with Self-Harm Visits.
| All Youths | By Sex | |||||
|---|---|---|---|---|---|---|
| Covariate | B | SE | P | B | SE | P |
| Tpre | –0.18 | 0.03 | <0.001 | –0.18 | 0.03 | <0.001 |
| Tpost | 0.31 | 0.02 | <0.001 | 0.32 | 0.02 | <0.001 |
| Sex | 0.93 | 0.09 | <0.001 | |||
| Sex × Tpre | –0.10 | 0.03 | 0.001 | |||
| Sex × Tpost | 0.24 | 0.02 | <0.001 | |||
Adjusted R 2 = 0.98.
Figure 1B shows how the trends in youths with self-harm visits differed by sex. From 2003 to 2017, there were higher rates of females with at least 1 self-harm visit (mean = 4.4/1000; CI, 3.7 to 5.1) compared with males (mean = 1.2/1000; CI, 1.0 to 1.3). The difference between the rates of self-harm visits for females and males was smallest in 2009, when females had 1.85 visits/1000/year (CI, 1.61 to 2.09; P < 0.001) more self-harm visits than males (see the “By Sex” column in Table 3). The significant interaction in Table 2 indicates that the rates of self-harm visits fell faster for females before 2009. Similarly, the significant interaction indicates that the rates rose faster for females after 2009. The change in slopes for males in 2009 (i.e., in Table 2) was 0.17 visits/1000/year2 (CI, 0.06 to 0.28; P = 0.001). However, the change in slopes for females (i.e., ) was 0.84 visits/1000/year2 (CI, 0.72 to 0.95; P < 0.001), 4.9 times larger than the change for males.
Mental Health Visit Rates
In an average year, 16.6 adolescents/1000 had an ED visit with a mental health code (CI, 14.4 to 18.9). Rates of youths with mental health visits rose 15% from 11.7/1000 youths in 2003 to 13.5/1000 youths in 2009, then rose 78% to 24.1/1000 youths in 2017 (Figure 1C). For all adolescents, Table 4 shows that from 2003 to 2009, the rate of adolescents with mental visits increased by 0.22 youths/1000/year (CI, 0.02 to 0.42), whereas from 2009 to 2017, they rose by 1.84 youths/1000/year (CI, 1.38 to 2.30). The change in the slope at 2009 was 1.62 youths/1000/year2 (CI, 1.02 to 2.22; P < 0.001).
Table 4.
Discontinuity Regressions for Rates of Youths with Mental Health Visits.
| All Youths | By Sex | |||||
|---|---|---|---|---|---|---|
| Covariate | B | SE | P | B | SE | P |
| Tpre | 0.22 | 0.10 | 0.058 | 0.21 | 0.09 | 0.025 |
| Tpost | 1.84 | 0.23 | <0.001 | 1.87 | 0.20 | <0.001 |
| Tpost 2 | –0.07 | 0.03 | 0.035 | –0.07 | 0.03 | 0.009 |
| Sex | 2.12 | 0.31 | <0.001 | |||
| Sex × Tpre | –0.10 | 0.09 | 0.256 | |||
| Sex × Tpost | 1.00 | 0.20 | <0.001 | |||
| Sex × Tpost 2 | –0.04 | 0.03 | 0.104 | |||
Adjusted R 2 = 0.99.
Figure 1D presents the rates of youths with self-harm visits by sex. From 2003 to 2017, rates of adolescents with at least 1 self-harm visit were higher for females (mean = 20.7/1000, CI, 17.5 to 24.0) than males (mean = 12.6/1000, CI, 11.3 to 13.9). The rates of females and males with mental health visits increased slowly (0.21 youths/1000/year; CI, 0.04 to 0.39; P = 0.025) and nearly in parallel before 2009 (i.e., is nonsignificant in the “By Sex” column of Table 4). The trend in rates of mental health visits accelerated after 2009 and was nonlinear, with slope 1.87 2⋅–0.07 . The significant interaction indicates that the rates rose faster for females after 2009. The change in slopes for males in 2009 (i.e., in Table 4) was 0.56 visits/1000/year2 (CI, –0.17 to 1.29; P = 0.066). However, the change in slopes for females (i.e., ) was 2.76 visits/1000/year2 (CI, 2.03 to 3.49; P < 0.001). As a result, the rate of mental health visits for females rose 95% from 2009 to 2017, compared with 56% for males.
Interpretation
This study examined parallel time series of rates of self-harm and mental health ED visits using methods that could identify discontinuous or nonlinear changes in rates of change, that is, accelerations or decelerations in rates. We found that from 2003 to 2009, rates of adolescents with self-harm visits declined for both sexes. Rates of adolescents with mental health visits increased only slightly. Starting in 2009, however, rates of adolescent ED visits for both self-harm and mental health concerns have increased rapidly in Ontario. These rates were higher and increased faster among females. These findings are consistent with extensive prior literature on adolescent ED visits for self-harm2–4,10 and mental health conceerns11–16 In particular, rates of suicidal attempts and suicidal ideation among US children and adolescents almost doubled over the period from 2007 to 2015.28 Likewise, from 2011 to 2015, there was a 28% increase in psychiatric ED visits per 1000 youth in the United States.29
So, what happened starting in 2009? Our data provide no evidence about this, but we see at least 2 non–mutually-exclusive explanations to be explored in future research. First, rates of self-harming behavior and mental disorders may have increased in the Ontario adolescent population. If more adolescents self-harmed or became mentally ill, then it is likely that more youths would visit the ED. There are 2 social factors starting about this time that might have increased the stress experienced by adolescents. On one hand, there might have been familial stress associated with the financial crisis of 2008. On the other hand, the iPhone first appeared in 2007, and the use of smartphones has increased greatly since that time. Engagement with social media could lead to increased rates of self-harm, at least for vulnerable adolescents,30 in several ways: by normalizing it, by triggering it, by eliciting emulation of self-harming behaviors, or by exposing youths to cyber bullying.31–35 Conversely, social media may also benefit troubled adolescents by providing them with opportunities to mitigate social isolation and find encouragement for seeking treatment.31,33,34,36,37
Second, independent of the population rates of self-harm and mental disorder, adolescents with these problems may have become more likely to visit the ED after 2009. Geulayov et al.38 estimated that for each youth who presents at a hospital with self-harm, there are several hundred who self-harm but do not present. If so, even a small increase in the proportion of such youths who present at the ED would greatly increase rates of ED visits. There were intensive anti-stigma campaigns during this period.39 These efforts to destigmatize mental illness might have helped adolescents seek care for mental health problems or helped families seek care for them, whether or not the adolescents sought it.40,41 To the degree that increasing ED visits for these problems reflects increased care seeking for acute problems, the increased rate of youths visiting the ED could be viewed as positive, compared with the potential consequences of distressed youths not seeking care at all.
Implications
With these increasing rates of adolescents presenting to the ED for self-harm or mental disorders and the importance of ensuring they receive good care, we need to find better ways to connect adolescents to mental health and social services during or following their visit.42 Possible solutions include integration of psychiatric emergency services into regional EDs43 and/or better integration between ED and community mental health services.44 Unfortunately, many hospitals do not have access to local mental health consultants, particularly in sparsely populated regions.45,46 Therefore, some youths receive limited emergency mental health assessments and/or follow-up outpatient mental health care.47–49 This gap might be addressed by using videoconferencing technology to facilitate assessments in the ED setting by mental health specialists located in other settings.50 Community mental health follow-up after self-harm has been associated with reduced likelihood of repeat self-harm,51 but evidence on whether youths can be successfully connected to mental health services from the ED is mixed.47,52,53 Efforts should be made to increase the supply and accessibility42 of evidence-based treatments54–56 for adolescents who self-harm or have mental health problems and where possible to deliver these services to them before they present to the ED. The development and implementation of such intervention strategies should be informed by research on the specific care that youths with self-harm or mental health disorders received before, during, and following their presentations to the ED. Our results suggest that Ontario’s destigmatization campaigns may have succeeded in increasing adolescent ED access for self-harm and mental illness. This is a great accomplishment, but unfortunately, it is not clear that there was an adequate increase in mental health treatment capacities to accommodate the surge in adolescents presenting at EDs with self-harm or mental health disorders. Finally, the concurrence of the inflection points in both time series with the advent of internet-connected mobile devices should prompt increased research on the psychological impacts of social media.
Limitations
This was an observational study using administrative data, and it was subject to the weaknesses of such data.57 Administrative records have limited information about many factors relevant to explaining self-harming behavior, including gender identification (as opposed to sex), sexual preference, fine-grained information about economic disadvantage, racial and ethnic affiliations, or scores on validated measures of mental disorders. Coders have less than perfect agreement in assigning ICD-10 codes to ED visits, and they likely undercount the prevalence of some problems. Likewise, these records lack information about the patient’s motivation for visiting the ED, in particular, whether the youth was seeking help or was brought unwillingly by others. In addition, many of the ICD-10 codes reported here have limited validation in the ED setting, particularly for this population, and therefore cases may be misclassified. Indeed, the codes for both self-harm and mental disorders likely undercount both problems in the ED population.24,25,58,59 There could also have been variability over time in how ICD-10 codes for self-harm were used. If so, some of the historical changes in the rates of self-harming behavior may have reflected changes in the understanding of self-harm by ED personnel. In particular, destigmatization campaigns may also have affected ED physicians, raising their awareness of the prevalence of self-harm and mental health problems. It is possible that physicians may “see” and therefore code more self-harm or mental health problems. To our knowledge, no one has investigated how destigmatization affects physicians’ practice. Finally, the data are from Ontario and may not generalize to other jurisdictions.60
Conclusions
Rates of adolescent ED visits for self-harm and mental disorders have more than doubled since 2009 in Ontario. More research is required on the factors that may promote the risks of self-harm and mental health disorders, including the social determinants of health. More research is also required to understand the factors affecting which of the many adolescents who self-harm or who suffer from mental disorders will present to the ED and the causes of sex differences in these uses of the ED. Finally, there is an urgent need for strategies to connect adolescents who visit the ED with appropriate treatments and services.
Supplemental Material
Supplemental Material, RECORD_Checklist_2019-04-28 for Changing Rates of Self-Harm and Mental Disorders by Sex in Youths Presenting to Ontario Emergency Departments: Repeated Cross-Sectional Study by William Gardner, Kathleen Pajer, Paula Cloutier, Roger Zemek, Lisa Currie, Simon Hatcher, Ian Colman, Dayna Bell, Clare Gray, Mario Cappelli, Daniel Rodriguez Duque and Isac Lima in The Canadian Journal of Psychiatry
Acknowledgements
We thank Paul Kurdyak, MD, for serving as the ICES scientist on this project. Parts of this material are based on data and/or information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions, and statements expressed in the material are those of the authors and not necessarily those of CIHI.
Data Access: Daniel Rodriguez Duque and Isac Lima had full access to the data in the study. The data set from this study is held securely in coded form at ICES. While data-sharing agreements prohibit ICES from making the data publicly available, access may be granted to those who meet prespecified criteria for confidential access, available at www.ices.on.ca/DAS. See https://www.ices.on.ca/Data-and-Privacy/Privacy-at-ICES for a discussion of how ICES handles data privacy. The R code used to model the aggregate rates is available from the corresponding author.
Disclosure: The authors have no financial relationships with any organizations that might have an interest in the submitted work and no other relationships or activities that could appear to have influenced the research.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by a grant from the ScotiaBank Foundation. ScotiaBank had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication. This study was also supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results, and conclusions reported in this article are those of the authors and are independent from the funding sources. No endorsement by ICES or the MOHLTC is intended or should be inferred.
ORCID iD: William Gardner  https://orcid.org/0000-0003-1918-3540
https://orcid.org/0000-0003-1918-3540
Ian Colman  https://orcid.org/0000-0001-5924-0277
https://orcid.org/0000-0001-5924-0277
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Posner K, Brodsky B, Yershova K, et al. The classification of suicidal behavior In: Nock M, ed. The Oxford Handbook of Suicide and Self-injury. Oxford (UK: ): Oxford University Press; 2014:7–22. [Google Scholar]
- 2. Whitlock J, Muehlenkamp J, Eckenrode J, et al. Nonsuicidal self-injury as a gateway to suicide in young adults. J Adolesc Health. 2013;52(4):486–492. [DOI] [PubMed] [Google Scholar]
- 3. Mars B, Heron J, Crane C, et al. Clinical and social outcomes of adolescent self harm: population based birth cohort study. BMJ. 2014;349:g5954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Olfson M, Wall M, Wang S, et al. Suicide after deliberate self-harm in adolescents and young adults. Pediatrics. 2018;141(4): e20173517. [DOI] [PubMed] [Google Scholar]
- 5. Georgiades K, Boylan K, Duncan L, et al. Prevalence and correlates of youth suicidal ideation and attempts: evidence from the 2014 Ontario Child Health Study. Can J Psychiatry. 2019;64(4):265–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rhodes AE, Sinyor M, Boyle MH, et al. emergency department presentations and youth suicide: a case-control study. Can J Psychiatry. 2019;64(2):88–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cutler GJ, Flood A, Dreyfus J, et al. Emergency department visits for self-inflicted injuries in adolescents. Pediatrics. 2015;136(1):28–34. [DOI] [PubMed] [Google Scholar]
- 8. Herbert A, González-Izquierdo A, McGhee J, et al. Time-trends in rates of hospital admission of adolescents for violent, self-inflicted or drug/alcohol-related injury in England and Scotland, 2005–11: population-based analysis. J Public Health. 2016;39(1):65–73. [DOI] [PubMed] [Google Scholar]
- 9. Perera J, Wand T, Bein KJ, et al. Presentations to NSW emergency departments with self-harm, suicidal ideation, or intentional poisoning, 2010-2014. Med J Aust. 2018;208(8):348–353. [DOI] [PubMed] [Google Scholar]
- 10. Rhodes AE, Bethell J, Carlisle C, et al. Time trends in suicide-related behaviours in girls and boys. Can J Psychiatry. 2014;59(3):152–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Simon AE, Pastor PN, Reuben CA, et al. Use of mental health services by children ages six to 11 with emotional or behavioral difficulties. Psychiatr Serv. 2015;66(9):930–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mapelli E, Black T, Doan Q. Trends in pediatric emergency department utilization for mental health-related visits. J Pediatr. 2015;167(4):905–910. [DOI] [PubMed] [Google Scholar]
- 13. Sheridan DC, Spiro DM, Fu R, et al. Mental health utilization in a pediatric emergency department. Pediatr Emerg Care. 2015;31(8):555–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hiscock H, Neely RJ, Lei S, et al. Paediatric mental and physical health presentations to emergency departments, Victoria, 2008-15. Med J Aust. 2018;208(8):343–348. [DOI] [PubMed] [Google Scholar]
- 15. Gandhi S, Chiu M, Lam K, et al. Mental health service use among children and youth in Ontario: population-based trends over time. Can J Psychiatry. 2016;61(2):119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Newton AS, Rosychuk RJ, Niu X, et al. Emergency department use and postvisit care for anxiety and stress disorders among children: a population-based cohort study in Alberta, Canada. Pediatr Emerg Care. 2016;32(10):658–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bethell J, Bondy SJ, Lou WYW, et al. Emergency department presentations for self-harm among Ontario youth. Can J Public Health. 2013;104(2):e124–e130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bresin K, Schoenleber M. Gender differences in the prevalence of nonsuicidal self-injury: a meta-analysis. Clin Psychol Rev. 2015;38:55–64. [DOI] [PubMed] [Google Scholar]
- 19. Merikangas K, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the adolescent supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Whitlock J, Selekman M. Non-suicidal self-injury across the lifespan In: Nock MK, ed. The Oxford Handbook of Suicide and Self-injury. Oxford (UK: ): Oxford University Press; 2014:61–81. [Google Scholar]
- 21. Nixon M, Cloutier P, Jannsson S. Nonsuicidal self-harm in youth: a population-based survey. CMAJ. 2008;178(3):306–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) Geneva (Switzerland): World Health Organization; 2016. [Google Scholar]
- 23. Gibson D, Richards H, Chapman A. The national ambulatory care reporting system: factors that affect the quality of its emergency data. Int J Inform Qual. 2008;2(2):97–114. [Google Scholar]
- 24. Rhodes AE, Links PS, Streiner DL, et al. Do hospital E-codes consistently capture suicidal behaviour? Chronic Dis Can. 2002;23(4):139–145. [PubMed] [Google Scholar]
- 25. Bethell J, Rhodes AE. Identifying deliberate self-harm in emergency department data. Health Rep. 2009;20(2):35–42. [PubMed] [Google Scholar]
- 26. Imbens G, Lemieux T. Regression discontinuity designs: a guide to practice. J Econometrics. 2008;142(2):615–635. [Google Scholar]
- 27.R Core Team. R: The R Project for Statistical Computing. Vienna: R Core Team; 2018. https://www.r-project.org. [Google Scholar]
- 28. Burstein B, Agostino H, Greenfield B. Suicidal attempts and ideation among children and adolescents in US emergency departments, 2007-2015. JAMA Pediatr. 2019; 173(6): 598–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kalb LG, Stapp EK, Ballard ED, et al. Trends in psychiatric emergency department visits among youth and young adults in the US. Pediatrics. 2019:143(4);e20182192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Odgers C. Smartphones are bad for some teens, not all. Nature. 2018;554(7693):432–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Whitlock J, Powers J, Eckenrode J. The virtual cutting edge: the internet and adolescent self-injury. Develop Psychol. 2006;42(3):407–417. [DOI] [PubMed] [Google Scholar]
- 32. Lewis SP, Heath NL, Michal NJ, et al. Non-suicidal self-injury, youth, and the internet: what mental health professionals need to know. Child Adolesc Psychiatry Ment Health. 2012;6(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Daine K, Hawton K, Singaravelu V, et al. The power of the web: a systematic review of studies of the influence of the internet on self-harm and suicide in young people. PloS One. 2013;8(10):e77555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lewis SP, Seko Y. A double-edged sword: a review of benefits and risks of online nonsuicidal self-injury activities. J Clin Psychol. 2015;72(3):249–262. [DOI] [PubMed] [Google Scholar]
- 35. Twenge J, Joiner T, Rogers M, et al. Increases in depressive symptoms, suicide-related outcomes, and suicide rates among U.S. adolescents after 2010 and links to increased new media screen time. Clin Psychol Sci. 2017;1–15. [Google Scholar]
- 36. Seko Y, Kidd SA, Wiljer D, et al. On the creative edge: exploring motivations for creating non-suicidal self-injury content online. Qual Health Res. 2015;25(10):1334–1346. [DOI] [PubMed] [Google Scholar]
- 37. Marchant A, Hawton K, Stewart A, et al. A systematic review of the relationship between internet use, self-harm and suicidal behaviour in young people: the good, the bad and the unknown. PloS One. 2017;12(8):e0181722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Geulayov G, Casey D, McDonald KC, et al. Incidence of suicide, hospital-presenting non-fatal self-harm, and community-occurring non-fatal self-harm in adolescents in England (the iceberg model of self-harm): a retrospective study. Lancet Psychiatry. 2017;5(2):167–174. [DOI] [PubMed] [Google Scholar]
- 39. Bell Canada. Bell Let’s Talk. 2018. https://letstalk.bell.ca/en/.
- 40. Cheng J, Benassi P, De Oliveira C. Impact of a mass media mental health campaign on psychiatric emergency department visits. Can J Public Health. 2016;107(3):e303–e311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Booth RG, Allen BN, Bray Jenkyn KM, et al. Youth mental health services utilization rates after a large-scale social media campaign: population-based interrupted time-series analysis. JMIR Ment Health. 2018;5(2):e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Renaud J, Seguin M, Lesage AD, et al. Service use and unmet needs in youth suicide: a study of trajectories. Can J Psychiatry. 2014;59(10):523–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Zeller S, Calma N, Stone A. Effects of a dedicated regional psychiatric emergency service on boarding of psychiatric patients in area emergency departments. West J Emerg Med. 2014;15(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Jabbour M, Reid S, Polihronis C, et al. Improving mental health care transitions for children and youth: a protocol to implement and evaluate an emergency department clinical pathway. Implement Sci. 2016;11(1):90–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Kurdyak P, Stukel TA, Goldbloom D, et al. Universal coverage without universal access: a study of psychiatrist supply and practice patterns in Ontario. Open Med. 2014;8(3):e87–e99. [PMC free article] [PubMed] [Google Scholar]
- 46. Kelleher KJ, Gardner W. Out of sight, out of mind—behavioral and developmental care for rural children. N Engl J Med. 2017;376(14):1301–1303. [DOI] [PubMed] [Google Scholar]
- 47. Bridge JA, Marcus SC, Olfson M. Outpatient care of young people after emergency treatment of deliberate self-harm. J Am Acad Child Adolesc Psychiatry. 2012;51(2):213–222. [DOI] [PubMed] [Google Scholar]
- 48. Sobolewski B, Richey L, Kowatch RA, et al. Mental health follow-up among adolescents with suicidal behaviors after emergency department discharge. Arch Suicide Res. 2013;17(4):323–334. [DOI] [PubMed] [Google Scholar]
- 49. Zanus C, Battistutta S, Aliverti R, et al. Adolescent admissions to emergency departments for self-injurious thoughts and behaviors. PloS One. 2017;12(1):e0170979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Narasimhan M, Druss BG, Hockenberry JM, et al. Impact of a telepsychiatry program at emergency departments statewide on the quality, utilization, and costs of mental health services. Psychiatric Serv. 2015;66(11):1167–1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Bilén K, Pettersson H, Owe-Larsson B, et al. Can early follow-up after deliberate self-harm reduce repetition? A prospective study of 325 patients. J Affect Disord. 2014;152-154(1):320–325. [DOI] [PubMed] [Google Scholar]
- 52. Cappelli M, Cloutier P, Newton A, et al. Evaluating mental health service use during and after emergency department visits in a multisite cohort of Canadian children and youth. Can J Emerg Med. 2019;21(1):75–86. [DOI] [PubMed] [Google Scholar]
- 53. Morgan C, Webb R, Carr M, et al. Incidence, clinical management, and mortality risk following self harm among children and adolescents: cohort study in primary care. BMJ. 2017;359:j4351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Brent D, McMakin DL, Kennard BD, et al. Protecting adolescents from self-harm: a critical review of intervention studies. J Am Acad Child Adolesc Psychiatry. 2013;52(12):1260–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Mehlum L, Tormoen AJ, Ramberg M, et al. Dialectical behavior therapy for adolescents with repeated suicidal and self-harming behavior: a randomized trial. J Am Acad Child Adolesc Psychiatry. 2014;53(10):1082–1091. [DOI] [PubMed] [Google Scholar]
- 56. Asarnow JR, Hughes JL, Babeva KN, et al. Cognitive-behavioral family treatment for suicide attempt prevention: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2017;56(6):506–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Benchimol EI, Smeeth L, Guttmann A, et al. The REporting of studies conducted using observational routinely-collected health data (RECORD) statement. PloS Med. 2015;12(10):e1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Clements C, Turnbull P, Hawton K, et al. Rates of self-harm presenting to general hospitals: a comparison of data from the multicentre study of self-harm in England and hospital episode statistics. BMJ Open. 2016;6(2):e009749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Randall JR, Roos LL, Lix LM, et al. Emergency department and inpatient coding for self-harm and suicide attempts: validation using clinician assessment data Int J Methods Psychiatr Res. 2017;26(3). doi:10.1002/mpr.1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Renaud J, Lesage A, Gagné M, et al. Regional variations in suicide and undetermined death rates among adolescents across canada. J Can Acad Child Adolesc Psychiatry. 2018;27(2):112–121. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, RECORD_Checklist_2019-04-28 for Changing Rates of Self-Harm and Mental Disorders by Sex in Youths Presenting to Ontario Emergency Departments: Repeated Cross-Sectional Study by William Gardner, Kathleen Pajer, Paula Cloutier, Roger Zemek, Lisa Currie, Simon Hatcher, Ian Colman, Dayna Bell, Clare Gray, Mario Cappelli, Daniel Rodriguez Duque and Isac Lima in The Canadian Journal of Psychiatry