Abstract
Study Design:
Technical note.
Objectives:
Coccygectomy for chronic coccydynia has a high rate of successful clinical outcome. However, the procedure is associated with increased incidence of wound dehiscence and surgical site infection. The main objective was to evaluate the clinical outcomes of coccygectomy using the Z plasty technique of wound closure.
Methods:
Patients with chronic coccydynia refractory to conservative treatment underwent coccygectomy followed by Z plasty technique of wound closure between January 2013 and February 2018. Primary outcome measure was evaluation of the wound healing in the postoperative period and at follow-up; secondary outcome measure included visual analogue scale (VAS) score for coccygeal pain.
Results:
Ten patients (male:female 6:4) fulfilled the inclusion criteria. The mean age of patients was 40.78 years (range 19-55 years). The mean follow-up was 1.75 years (range 6 months to 5 years). All wounds healed well with no incidence of wound dehiscence or surgical site infections. The mean VAS improved from 7.33 ± 0.5 to 2.11 ± 1.2 (P < .05). Nine patients reported excellent outcomes and 1 patient reported poor outcome with regards to relief from coccydynia.
Conclusion:
Z plasty technique of wound closure is recommended as procedure of choice to avoid wound healing problems and surgical site infections associated with coccygectomy. Coccygectomy remains a successful treatment modality for chronic coccydynia.
Keywords: coccydynia, coccygectomy, Z plasty, wound dehiscence, surgical site infections
Introduction
Coccydynia is a painful condition characterized by pain in the region of coccyx. It is typically exhibited as discomfort in sitting position. Coccydynia was first defined in 1859 by Simpson. It is not an uncommon condition without any universally accepted treatment protocol. As a result, management of these patients presents a unique challenge. Coccygectomy performed for patients with chronic coccydynia has met with considerable success, with success rate as high as 90%.1 However, the procedure is associated with infection rate as high as 30% with the standard midline incision approach.2-7 The prolonged nature of disease, uncertain treatment protocols and high rate of wound complications associated with the surgery can lead to a poor quality of life.
Z plasty with transposition of flaps has been highly successful in treatment of pilonidal sinus and contracted scars.8-10 The aim of this study was to evaluate the clinical outcomes of Z plasty for coccygectomy in minimizing the wound healing problems and surgical site infections.
Materials and Methods
This study is a retrospective case series. Consecutive patients with chronic coccydynia refractory to conservative treatment were operated between January 2013 and February 2018 were part of the study. All patients were given a nonoperative trial. First line of nonoperative treatment included nonsteroidal anti-inflammatory drugs, hot baths, ring-shaped cushions, and postural changes. Local steroid injection was given as second line of nonoperative regimen. Patients with failed conservative trial underwent coccygectomy. Sacrococcygeal dynamic X-rays were done to rule out instability/fracture in patients with history of trauma. Magnetic resonance imaging was done to rule out infection, local tumor pathology, or metastatic bone disease. Patients with concomitant low back pain were not considered for surgery. Approval from institutional review board was taken and written informed consent taken from patients for publication of images.
Surgical Technique
All cases were operated upon by the lead author. With the patient in the prone position and the buttocks strapped laterally using adhesive tape, a 5 to 6 cm vertical midline incision was made directly over the coccyx (Figure 1). Dissection was carried down to the bone, followed by release of the anococcygeal ligaments using a pair of scissors. The distal part of the coccyx could then be elevated using a towel clip. A subperiosteal plane was developed on the anterior surface with great care to stay well clear of the rectum. Coccyx was amputated at the level of sacrococcygeal joint and a total coccygectomy was performed and meticulous hemostasis achieved. At the time of closure, the vertical incision was extended in the shape of a “Z”; considering the vertical incision as central limb of the “Z,” extension of incision was done in opposite directions at an angle of 60° (Figures 2 and 3). Flaps were raised such that the surgical wound looked like a parallelogram now (Figure 4). Flaps were mobilized and then transposed with their position approximately adjusted with interrupted subcutaneous 2/0 Vicryl stitches (Figure 5). Meticulous apposition was sought without the flaps being under tension. Skin was closed with subcuticular 3/0 Monocryl sutures (Figure 6) without a drain. Figure 7 shows the excised coccyx. Patients were mobilized immediately after the procedure within the limits of pain. All patients received intravenous Cefuroxime 30 minutes preoperatively and 1 dose after 6 hours following the operation. Assessment of wound healing was performed after 2 weeks postsurgery (Figure 8).
Figure 1.

Vertical midline Incision.
Figure 2.

Overlay of Z incision.
Figure 3.

Z incision.
Figure 4.
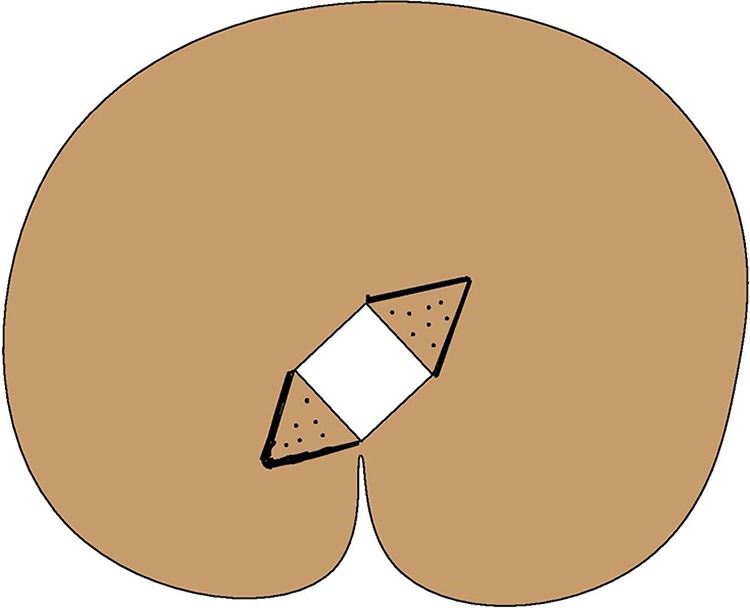
Illustrated version showing raised flaps.
Figure 5.

Transposition of flaps.
Figure 6.

Skin closure and the “Z”.
Figure 7.

Excised coccyx.
Figure 8.

Healed surgical wound after 2 weeks.
The patients were followed up at intervals of 6 weeks, 3 months, and 6 months and were assessed for wound healing and visual analogue scale (VAS) score for pain. Paired-samples t tests were used for comparisons of continuous variables like VAS. All statistical analyses were performed using IBM SPSS software version 15.0. A probability value of P < .05 was considered statistically significant. An excellent outcome was defined as being pain free or with significantly decreased pain, with a maximum VAS score of 2, and a major improvement in activities of daily living, including sitting and standing. Poor outcome was defined as no decrease of pain (VAS score more than 5) and no or marginal improvement in the activities of daily living, including sitting and standing.
Results
Ten patients underwent the procedure. The female to male ratio was 3:2 and the mean age of patients was 40.78 years (range 19-55 years). The mean duration of symptoms was 163.3 days (range 125-190 days). Mean duration of surgery was 60 minutes (range 50-80 minutes) and blood loss was 50 mL (range 45-80 mL). The mean follow-up was 1.75 years (range 6 months to 5 years). The mean VAS score for coccygeal pain improved from 7.33 ± 0.5 to 2.11 ± 1.2 (P < .05). None of the patients had wound dehiscence or surgical site infections (0.0%). Nine patients reported excellent outcome and 1 patient reported poor outcome at the last follow-up. The patient with poor outcome continued to have pain and tenderness in the amputated region of the sacrococcygeal junction.
Discussion
Coccydynia is usually associated with direct trauma, repetitive microtrauma, postnatal period, spasm of pelvic floor muscles, local tumors, degenerative disc disease, post–weight loss/bariatric surgery or could be idiopathic in nature.3,6,11-14 It is most commonly seen in females and is associated with obesity.11 The classical presentation of coccydynia is localized pain over the coccyx. Pain worsens with prolonged sitting, leaning back while seated, prolonged standing, and rising from a seated position.6,11,14,15 The condition appears to be emerging as a major problem in the current millennium with an increasing population base that sits in front of computers for extended periods. Many patients also experience pain with sexual intercourse or defecation.14 Specific point tenderness over coccyx is diagnostic, nontender coccygeal pain almost rules out coccydynia.6
First line of treatment includes nonsteroidal anti-inflammatory drugs, sitting aids, warm bath, and physiotherapy.6,11,14 This nonoperative management is effective in only 60% to 66% of cases.1,13,16 When the first line of treatment fails, local steroid injection and coccyx manipulation have variable success rate between 75% and 85%.1,3,13,17 Coccygectomy is a valid surgical alternative in patients who fail to respond to conservative methods of treatment. 89.9% of our patients reported excellent results after coccygectomy. This is in concurrence with previous published literature.1,13,15,17,18
The vertical midline incision approach described by Key19 is the most common approach used by majority of surgeons. The infection rates associated with conventional approach of coccygectomy have ranged from 14% to 30%, comprising superficial and deep infections and wound dehiscence.2-7 This can lead to repeated debridements, prolonged antibiotic usage, protracted recovery and hospital stay, finally affecting the clinical outcomes.4 There are numerous studies published to minimize the infection rate associated with coccygectomy employing multiple techniques; however, most have met with limited outcomes.2,4,15,18,20 Many authors recommend antibiotic prophylaxis beyond 48 hours postoperatively.2,4,5,12,16 Sehirlioglu et al20 recommend a constipating or low-residue diet to prevent postoperative wound infection. Fogel et al15 recommend oral mechanical bowel preparation such as polyethylene glycol solution, the day before surgery. Doursounian et al21 in their comparative study showed the decrease in infection rate to 0% by using skin adhesive, 2 prophylactic antibiotics for 48 hours, preoperative rectal enema, and closure of the incision in 2 layers as compared with infection rate of 1.5% with the use of topical skin adhesive alone.
Z plasty in treatment of pilonidal sinus is associated with a high success rate.8,9 The authors employed this technique of wound closure based on the various factors that act at the sacrococcygeal area making it prone to increased infections with conventional approach. Z plasty is a procedure that involves the transposition of 2 interdigitating triangular flaps. The name derives from the “Z” shape seen when the three limbs of the flaps are drawn out on the skin. Transposition of the flaps leads to gain in length and change in the direction of the central limb of Z.22 The length of flaps taken is equal in size and angles of Z are taken at 60°. Studies have shown that the angle at 60° is associated with adequate gain in length and optimum blood supply of the flap.22 Angles less than 30° are associated with decreased gain in length and associated with poor blood supply to flap and angles more than 60° is associated with increased tension in the surrounding tissues making it difficult to bring the flaps in transposed position.22 As a result, angle at 60° is considered as standard.
With the standard midline incision, there is excessive wound tension, especially when the patient sits with centrifugal forces acting at wound site making it prone for wound dehiscence and infection.2 By executing a Z plasty, we alter the forces acting at the surgical site and the natal environment. It also obliterates the crease, which minimizes friction and reduces the accumulation of debris.23 The infection rate/wound-related problem in this study was 0.0% and this can be attributed to elimination of various factors involved in wound dehiscence and surgical site infections.
Patients with coccydynia face a lot of stigma due to trivialization of symptoms, disbelief against a physical etiology (“it’s all in your head”), and defeatism (“there’s nothing you can do for it”).24,25 Coccydynia cannot be regarded as a hysterical or a neurotic condition.24 Moreover, the chronic nature of disease, uncertain clinical outcomes, wound complications associated with surgery have led to increased disease burden, sickness absenteeism, and health care expenditure. Consequently, patients with coccydynia end up having poor quality of life.26 Hence, coccygectomy along with measures to decrease the infection rates as described in this article would be hugely beneficial to curtail the course of the disease course and improving the quality of life.
Limitations of the Study
Retrospective case series with single center, single surgeon analysis, and lack of control group is a major limitation of this study. However, this is not a commonly performed surgery and hence the numbers of subjects that are eligible and willing for surgery are less. A large majority of patients get better with conservative treatment and some of the patients that are deserving candidates for surgery are anxious about complications such as wound dehiscence and bowel incontinence. Hence, the numbers of subjects in this series are limited; this can be considered as a pilot study and can form a basis for larger study with multicentric trials.
Conclusion
Z plasty technique of wound closure seems to be a good alternative to conventional midline incision with the potential to reduce the rate of delayed wound healing and wound infection. The superiority of this technique to decrease wound related complications in patients following coccygectomy for chronic coccydynia has to be further elaborated in multicenter randomized controlled trials. Coccygectomy remains to be an effective surgical alternative to patients with chronic coccydynia nonresponsive to conservative treatment.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: The study is approved by institutional review board (approval vide BHIRB7948), Bombay Hospital and Medical Research Centre.
References
- 1. Wray CC, Easom S, Hoskinson J. Coccydynia. Aetiology and treatment. J Bone Joint Surg Br. 1991;73:335–338. [DOI] [PubMed] [Google Scholar]
- 2. Wood KB, Mehbod AA. Operative treatment for coccygodynia. J Spinal Disord Tech. 2004;17:511–515. [DOI] [PubMed] [Google Scholar]
- 3. Bayne O, Bateman JE, Cameron HU. The influence of etiology on the results of coccygectomy. Clin Orthop Relat Res. 1984;(190):266–227. [PubMed] [Google Scholar]
- 4. Doursounian L, Maigne JY, Faure F, Chatellier G. Coccygectomy for instability of the coccyx. Int Orthop. 2004;28:176–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cebesoy O, Guclu B, Kose KC, Basarir K, Guner D, Us AK. Coccygectomy for coccygodynia: do we really have to wait? Injury. 2007;38:1183–1188. [DOI] [PubMed] [Google Scholar]
- 6. Sarmast AH, Kirmani AR, Bhat AR. Coccydynia: a story retold. Austin J Surg. 2016;3:1091. [Google Scholar]
- 7. Kleimeyer JP, Wood KB, Lønne G, et al. Surgery for refractory coccygodynia: operative versus nonoperative treatment. Spine (Phila Pa 1976). 2017;42:1214–1219. [DOI] [PubMed] [Google Scholar]
- 8. Monro RS, Mc Dermott FT. The elimination of causal factors in pilonidal sinus: treated by Z-plasty. Br J Surg. 1965;52:177–181. [DOI] [PubMed] [Google Scholar]
- 9. Fazeli MS, Adel MG, Lebaschi AH. Comparison of outcomes in Z-plasty and delayed healing by secondary intention of the wound after excision of the sacral pilonidal sinus: results of a randomized, clinical trial. Dis Colon Rectum. 2006;49:1831–1836. [DOI] [PubMed] [Google Scholar]
- 10. Hundeshagen G, Zapata-Sirvent R, Goverman J, Branski LK. Tissue rearrangements: the power of the Z-plasty. Clin Plast Surg. 2017;44:805–812. [DOI] [PubMed] [Google Scholar]
- 11. Maigne JY, Doursounian L, Chatellier G. Causes and mechanisms of common coccygodynia: role of body mass index and coccygeal trauma. Spine (Phila Pa 1976). 2000;25:3072–3079. [DOI] [PubMed] [Google Scholar]
- 12. Duncan GA. A painful coccyx. Arch Surg. 1937;34:1088–1104. [Google Scholar]
- 13. Perkins R, Schofferman J, Reynolds J. Coccygectomy for severe refractory sacrococcygeal joint pain. J Spinal Disord Tech. 2003;16:100–103. [DOI] [PubMed] [Google Scholar]
- 14. Nathan ST, Fisher BE, Roberts CS. Coccydynia: a review of pathoanatomy, aetiology, treatment and outcome. J Bone Joint Surg Br. 2010;92:1622–1627. [DOI] [PubMed] [Google Scholar]
- 15. Fogel G, Cunningham PY, 3rd, Esses SI. Coccygodynia: evaluation and management. J Am Acad Orthop Surg. 2004;12:49–54. [DOI] [PubMed] [Google Scholar]
- 16. Hodges SD, Eck JC, Humphreys SC. A treatment and outcomes analysis of patients with coccydynia. Spine J. 2004;4:138–140. [DOI] [PubMed] [Google Scholar]
- 17. Ramsey ML, Toohey JS, Neidre A, Stromberg LJ, Roberts DA. Coccygodynia: treatment. Orthopedics. 2003;26:403–405. [DOI] [PubMed] [Google Scholar]
- 18. Balain B, Eisenstein SM, Alo GO, et al. Coccygectomy for coccydynia: case series and review of literature. Spine (Phila Pa 1976). 2006;31:E414–E420. [DOI] [PubMed] [Google Scholar]
- 19. Key JA. Operative treatment of coccygodynia. J Bone Joint Surg Am. 1937;19:759–764. [Google Scholar]
- 20. Sehirlioglu A, Ozturk C, Oguz E, Emre T, Bek D, Altinmakas M. Coccygectomy in the surgical treatment of traumatic coccygodynia. Injury. 2007;38:182–187. [DOI] [PubMed] [Google Scholar]
- 21. Doursounian L, Maigne JY, Cherrier B, Pacanowski J. Prevention of post-coccygectomy infection in a series of 136 coccygectomies. Int Orthop. 2011;35:877–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McGregor AD, McGregor IA. The Z-plasty In: Fundamental Techniques of Plastic Surgery and Their Surgical Applications. 10th ed London, England: Churchill Livingstone; 2000:21–34. [Google Scholar]
- 23. Dogra S, Rao PP. Z-plasty: a rational and effective technique for pilonidal sinus. Hellenic J Surg. 2014;86:208–211. [Google Scholar]
- 24. Foye PM. Stigma against patients with coccyx pain. Pain Med. 2010;11:1872. [DOI] [PubMed] [Google Scholar]
- 25. Slade SC, Molloy E, Keating JL. Stigma experienced by people with nonspecific chronic low back pain: a qualitative study. Pain Med. 2009;10:143–154. [DOI] [PubMed] [Google Scholar]
- 26. Foye PM. Coccydynia: tailbone pain. Phys Med Rehabil Clin N Am. 2017;28:539–549. [DOI] [PubMed] [Google Scholar]


