Abstract
Study Design:
Retrospective cohort study.
Objective:
To evaluate differences in patient factors, procedural factors, early outcomes and safety in mutlilevel anterior cervical discectomy and fusion (ACDF) in the inpatient versus outpatient setting.
Methods:
Patient demographics, operative factors, and outcomes of multilevel ACDF performed in an inpatient and outpatient setting were compared using Fisher’s exact test for categorical and Student’s t test for continuous variables.
Results:
Fifty-seven patients had surgery on an outpatient and 46 on an inpatient basis. Inpatients were older (56.7 vs 52.2 years, P = .012) and had a higher ASA (American Society of Anesthesiologists) class (P = .002). Sixty percent of 2-level cases were outpatient surgeries, compared with 35% of 3-level cases (P = .042). Outpatients had shorter operative times (71.26 vs 83.59 minutes, P < .0001) and shorter lengths of stay (8.51 vs 35.76 hours, P < .0001), lower blood loss (33.04 vs 45.87 mL, P = .003), and fewer in-hospital complications (5.3% vs 37.0%, P < .0001). Outpatients had better early outcomes in terms of 6-week Neck Disability Index (NDI) (27.97 vs 37.59, P = .014), visual analogue scale (VAS) neck (2.92 vs 4.02, P = .044), and Short Form–12 Physical Health Score (SF-12 PHS) (35.66 vs 30.79, P = .008). However, these differences did not persist at 6 months.
Conclusions:
The results of our study suggest that multilevel ACDF can be performed safely in the outpatient setting without an increased risk of complications compared with the inpatient setting in an appropriately selected patient. Specifically, patients’ age, ASA class, and number of levels being fused should be taken into consideration. At our institution, ASA class 3, body mass index >40 kg/m2, age >80 years, intubation time >2.5 hours, or not having a responsible adult with the patient warrant inpatient admission. Importantly, the setting of the surgery does not affect patient-reported outcomes.
Keywords: ACDF, anterior cervical discectomy and fusion, multilevel, outpatient surgery, outcomes, safety, complications, patient-reported outcomes
Introduction
The overall rates of cervical spine surgeries performed in the United States have shown consistent growth over the past several years.1,2 Simultaneously, due to low complication rates, short operative times, and moderate postoperative pain, anterior cervical discectomy and fusion (ACDF) is specifically being done increasingly in an outpatient setting. Previously authors have documented safety and maintenance of excellent outcomes in single-level ACDF surgery.3 Given the ever increasing health care expenditure in the United States and an increasing shift toward a value-based system that emphasizes cost reduction, there is increasing pressure to perform more surgeries on an outpatient basis.4,5 Currently anterior cervical fusions account for up to 80% of all cervical spine surgeries performed in the United States.6
The majority of studies that have reported on outcomes of outpatient cervical fusion surgery focus on single-level procedures. Those that have included multilevel cervical fusions have generally combined them with single-level fusions, and single-level fusions have accounted for about 60% of cases in those reports. It is our belief that there is a lack of studies that evaluate the safety and outcomes of multilevel ACDF performed in an outpatient setting. Given the fact that more of these surgeries will be performed on an outpatient basis, we feel it is important to understand which differences, if any, exist between patients undergoing multilevel ACDF on outpatient versus inpatient basis.
The purpose of our study was to describe our experience with multilevel ACDF performed in the inpatient versus outpatient setting and examine which differences exist in terms of patient and procedural factors between outpatient and inpatient multilevel ACDF, as well as identify any differences in early clinical and patient-reported outcomes (PROs).
Methods
A full institutional review board approval was obtained prior to collecting surgical data and an expedited institutional review board approval was obtained for the retrospective review and analysis of this data.
Study Design and Population
A retrospective review of prospectively collected data from a single surgeon surgical database was performed. The surgical database includes data on patient demographics, comorbidities, various intraoperative variables and post-operative outcomes. This database was queried for patients who underwent 2-level or more ACDF. Patients who underwent revision surgery or combined anterior-posterior surgery were excluded from the analysis.
Extracted Data
Selected patients were divided into 2 groups based on whether they were outpatient surgeries (ie, hospital length of stay ≤23 hours) or they were admitted as inpatients (ie, hospital length of stay >23 hours). Outpatient surgeries included both, those performed at an Ambulatory Surgery Center and those performed in the hospital setting having a length of stay ≤23 hours. Patient selection for outpatient versus inpatient performance of surgery was based on a mutual decision made by the surgeon and anesthesiologist, as well as postoperative clinical evaluation. Baseline characteristic, including demographics and comorbidities, operative data and outcomes between the 2 groups were compared.
Patient data extracted for analysis included patient age at the time of surgery, sex, body mass index (BMI), smoking status, American Society of Anesthesiologists (ASA) classification and comorbidities. Surgical data that was analyzed includes number of levels operated, estimated blood loss, procedure time (in minutes) and length of stay in the hospital (in hours). PROs that were collected preoperatively, and at 6 weeks and 6 months postoperatively include Neck Disability Index (NDI, reported as %), visual analogue scale (VAS) for neck pain and arm pain (reported on a scale of 0-10), and Short Form–12 (SF-12) Physical (PHS) and Mental (MHS) Health Scores. In addition, any complications occurring during the index hospitalization were recorded.
Evaluation for immediate postoperative dysphagia was done using clinical swallowing evaluation performed by postanesthesia care unit nursing staff. During the mandatory 5-hour observation period in the postanesthesia care unit, patients were encouraged to swallow early, and had to complete 2 swallowing tests (ie, patient has to eat twice) before being discharged. Patients were deemed to have dysphagia if the clinical swallowing evaluation confirmed that they had dysphagia, or if they required intravenous fluid hydration or tube feeding due to dysphagia.
Assessment of dysphagia was also performed in the clinic preoperatively, and at 6 and 12 weeks postoperatively using the Swallowing Quality of Life (SWAL-QOL) Questionnaire.7 The SWAL-QOL questionnaires contains 44 items divided into various domains. Each item is given a score from 1 to 5 (worse to best). Scoring in each domain is calculated by the sum of the scores for each item in that domain expressed as a percentage of the maximum possible domain score. In addition to the domain scores, a total SWAL-QOL can also be derived by summing each domain score and dividing by 10.
The Frequency of Symptoms domain of the SWAL-QOL was used for this study. This domain contains 14 items that pertain to the frequency of symptoms such as coughing, choking when taking food or liquids, drooling etc. occurring as a result of the patient’s swallowing program. Each item’s response is recorded on a 5-point scale ranging from “Almost Always” to “Never.” The dysphagia rate is reported as the sum of the scores for each of the 14 items in this domain, expressed as a percentage of the maximum possible domain score of 70. Thus, the final score is reported as a percentage, with a score of 100 indicating no dysphagia and a progressively lower score indicating increasing frequency and severity of dysphagia symptoms. With the use of the SWAL-QOL, there is no predetermined score that differentiates those with dysphagia from those without. Rather, the results, which are reported on a continuous scale, reflect the severity of the impact on the patient’s quality of life from the patient’s perspective.
Statistical Analysis
Descriptive statistics were summarized using Fisher’s exact test for categorical variables, and independent-samples Student’s t test was used to compare means of continuous variables.
Paired-samples Student’s t test was used to analyze the change in PROs from the preoperative visit to the 6-month follow-up.
In addition, the percentage of patients experiencing an improvement greater than the minimum clinically important difference (MCID) at 6 weeks and 6 months postoperatively was calculated. The published values for MCID in patients with cervical spinal disease vary greatly depending on the population, the intervention and the method used for calculation.8 In our study, the MCID for NDI was calculated using a weighted average (based on sample size) of MCID values reported in 4 studies9-12 that focus on patients with degenerative conditions of the cervical spine undergoing surgical intervention, which in a majority of cases was an ACDF surgery. The MCID values reported in these studies ranged from 12.08 to 17.3, and yielded a weighted average of 14.8. For VAS neck pain and arm pain, the MCID of 2.5 reported by Carreon et al10 was selected as the threshold.
Statistical significance was defined with a P value set at <.05 and all P values were 2-tailed. All analyses were performed using the IBM Statistical Package for the Social Sciences (SPSS) version 25 (IBM Corp, Armonk, NY).
Surgical Technique
Standard ACDF was carried out through a transverse anterior approach. Disc space preparation was conducted per the operative surgeon’s preference, but included curette and burr usage. Following implantation of a zero-profile device or a plate-graft construct, the wound was irrigated. Local administration of steroid was achieved by spraying 1 mL of 40 mg/mL of Kenalog directly onto the esophagus and wound bed using a standard syringe and blunt hypodermic needle. Layered closure completed the surgery.
Results
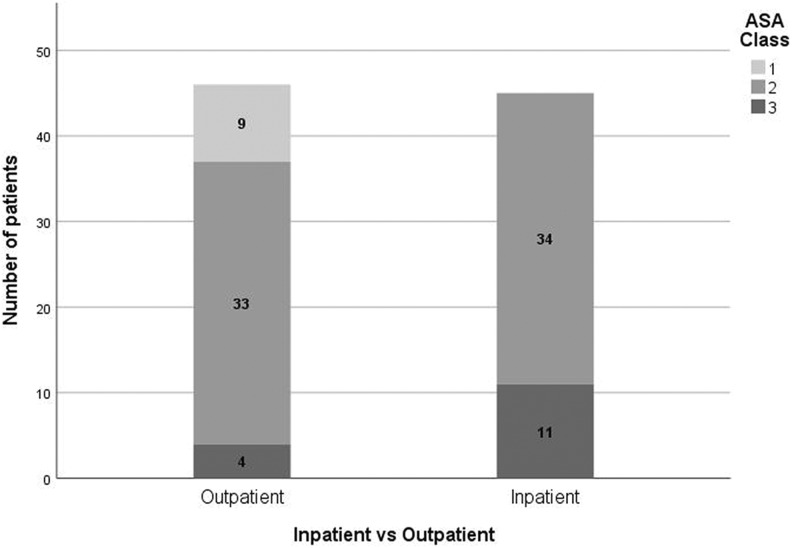
A total of 103 patients were included in this study, of whom 57 underwent outpatient procedures and 46 were treated on an inpatient basis. Of the 57 outpatient procedures, 26 (45.6%) were performed at a stand-alone Ambulatory Surgery Center and 31 (54.4%) were performed in a hospital. Patients undergoing outpatient procedures were younger (P = .012), with a mean age of 52.2 ± 7.5 years compared with 56.7 ± 10.5 years for the inpatient group. The outpatient group comprised 33 males (57.9%) and 24 females (42.1%), whereas the inpatient group included 28 males (60.9%) and 18 females (39.1%), thus showing no significant difference in this regard (P = .76). The BMI was not significantly different between the 2 groups (28.28 ± 5.63 kg/m2 in outpatients vs 29.99 ± 5.36 kg/m2 in inpatients, P = .12). Seven patients in each group were smokers (P = .67). Although there was no significant difference in the number of patients with diabetes (10.5% of outpatients vs 17.4% of inpatients, P = .390), the difference in the number of patients with hypertension approached statistical significance (24.6% of outpatients vs 43.5% of inpatients, P = .058). Additionally, a significant difference was seen in the Charlson Comorbidity Index (CCI) (1.56 ± 1.45 for outpatients vs 2.26 ± 1.57 for inpatients, P = .021) (Table 1). As seen in Figure 1, the inpatient group had an overall higher ASA class (P = .002), with no patients being ASA class 1 and 11 patients being ASA class 3. In the outpatient group, 9 patients were ASA class 1 and only 4 patients were ASA class 3.
Table 1.
Demographics and Preoperative Variables.
| Outpatient | Inpatient | P a | |
|---|---|---|---|
| No. of cases, n | 57 | 46 | |
| Age, years, mean ± SD | 52.19 ± 7.47 | 56.72 ± 10.48 | .012 |
| Gender, n (%) | .76 | ||
| • Male | 33 (57.9) | 28 (60.9) | |
| • Female | 24 (42.1) | 18 (39.1) | |
| Type of insurance, n (%) | .429 | ||
| • Medicare/Medicaid | 1 (1.8) | 3 (6.5) | |
| • Workers Compensation | 15 (26.3) | 13 (28.3) | |
| • Private/other | 41 (71.9) | 30 (65.2) | |
| Body mass index, kg/m2, mean ± SD | 28.28 ± 5.63 | 29.99 ± 5.36 | .12 |
| Current smoker (within 1 year), n (%) | 7 (12.3) | 7 (15.2) | .67 |
| Diabetes, n (%) | 6 (10.5) | 8 (17.4) | .390 |
| Hypertension, n (%) | 14 (24.6) | 20 (43.5) | .058 |
| Charlson Comorbidity Index, mean ± SD | 1.56 ± 1.45 | 2.26 ± 1.57 | .021 |
| ASA classification, n | .002 | ||
| • Class 1 | 9 | 0 | |
| • Class 2 | 33 | 34 | |
| • Class 3 | 4 | 11 |
Abbreviation: ASA, American Society of Anesthesiologists.
a P values in boldface indicate statistical significance (P < .05).
Figure 1.
American Society of Anesthesiologists (ASA) class of the outpatient and inpatient cohorts.
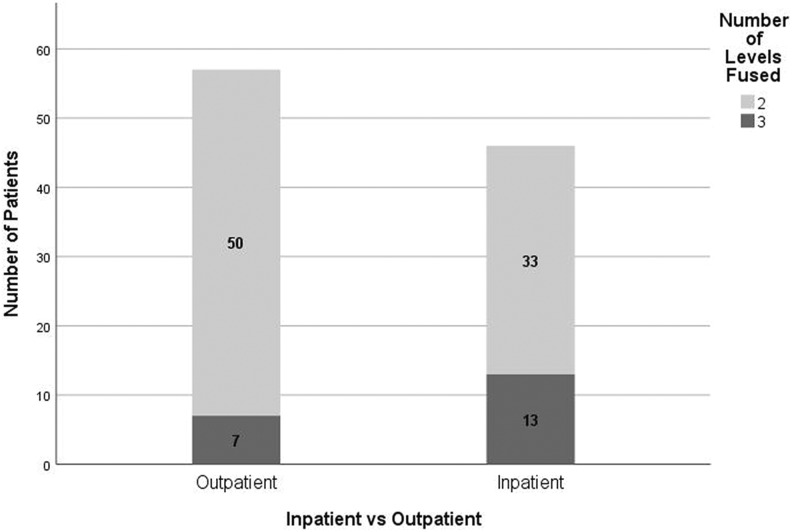
In terms of operative factors, 60% of the 2-level cases were performed as outpatient surgeries, compared with only 35% of the 3-level surgeries (P = .042) (Figure 2). Outpatients had significantly shorter operative times (71.26 ± 12.48 vs 83.59 ± 20.71 minutes in the inpatient group, P < .0001), and shorter total length of stay (8.51 ± 4.39 vs 35.76 ± 15.41 hours, P < .0001). In addition, outpatients had a lower estimated blood loss (33.04 ± 13.57 vs 45.87 ± 27.41 mL, P = .003) and fewer in-hospital complications (5.3% vs 37.0%, P < .0001). In addition, 1 patient in the inpatient group required reintubation for a postoperative hematoma. The 2 groups had similar postoperative day zero pain scores (4.96 ± 2.07 in the outpatient group vs 4.89 ± 1.47 in the inpatient group, P = .84) (Table 2).
Figure 2.
Number of Levels operated in the outpatient and inpatient cohorts.
Table 2.
Operative and Postoperative Factors.
| Outpatient | Inpatient | P a | |
|---|---|---|---|
| No. of levels operated, n | .042 | ||
| • 2 levels (n = 83) | 50 | 33 | |
| • 3 levels (n = 20) | 7 | 13 | |
| Procedure time, min, mean ± SD | 71.26 ± 12.48 | 83.59 ± 20.71 | <.0001 |
| Total length of stay, hours, mean ± SD | 8.51 ± 4.39 | 35.76 ± 15.41 | <.0001 |
| Estimated blood loss, mL, mean ± SD | 33.04 ± 13.57 | 45.87 ± 27.41 | .003 |
| In-hospital complications, n (%) | 3 (5.3) | 17 (37.0) | <.0001 |
| • Aspiration/reintubation | 0 (0.0) | 1 (2.2) | .447 |
| • Urinary retention requiring catheterization | 2 (3.5) | 16 (34.8) | <.0001 |
| • Epidural hematoma | 0 (0.0) | 1 (2.2) | .447 |
| • Ileus | 0 (0.0) | 1 (2.2) | .447 |
| • Dysphagia (intravenous fluid hydration, tube feeding, clinical swallowing evaluation) | 0 (0.0) | 2 (4.3) | .197 |
| Postoperative day zero average pain scores, mean ± SD | 4.96 ± 2.07 | 4.89 ± 1.47 | .84 |
a Pvalues in boldface indicate statistical significance (P < .05).
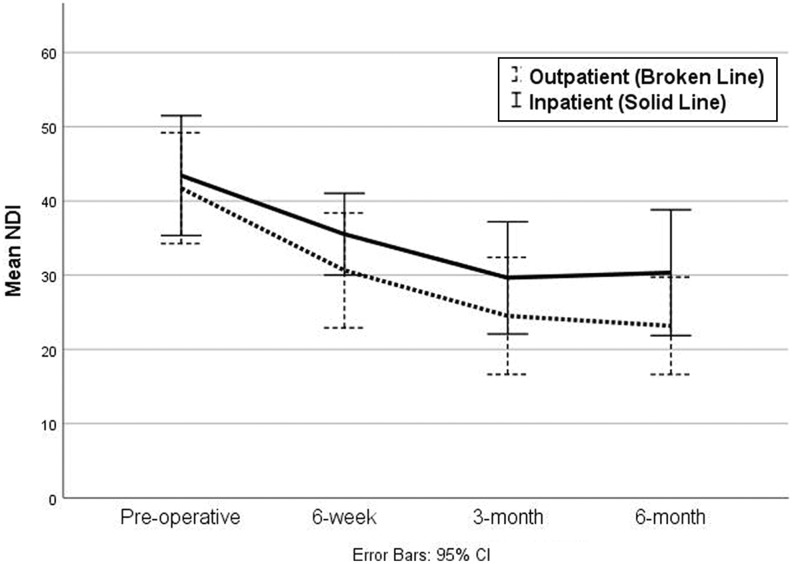
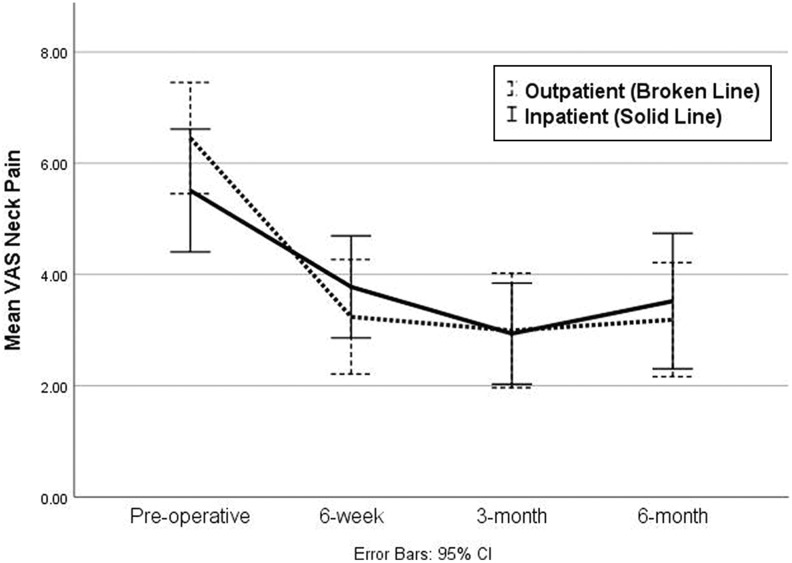
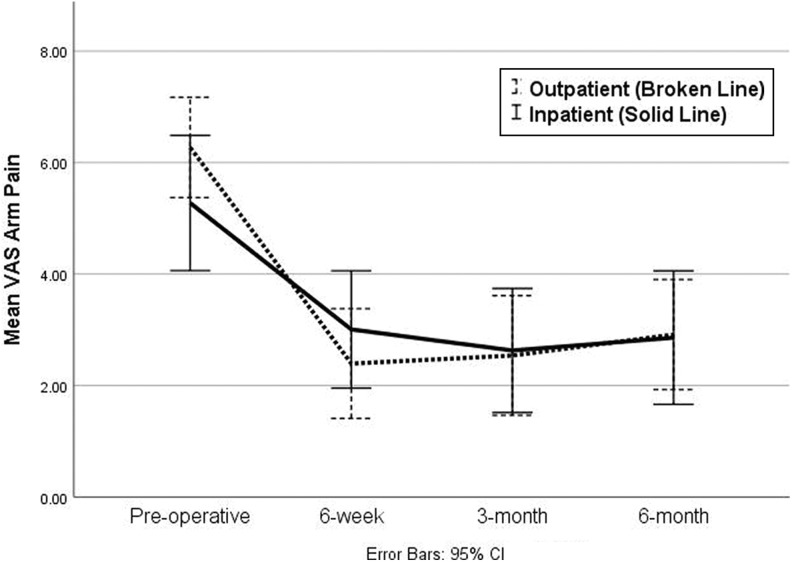
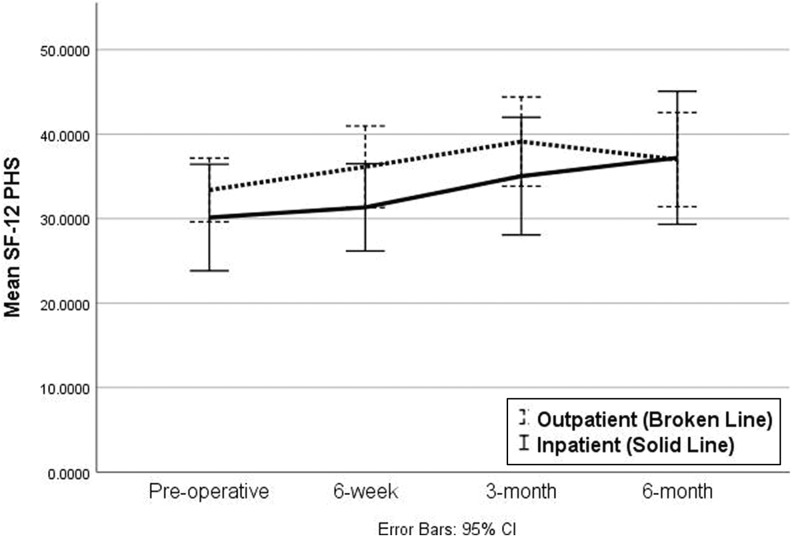
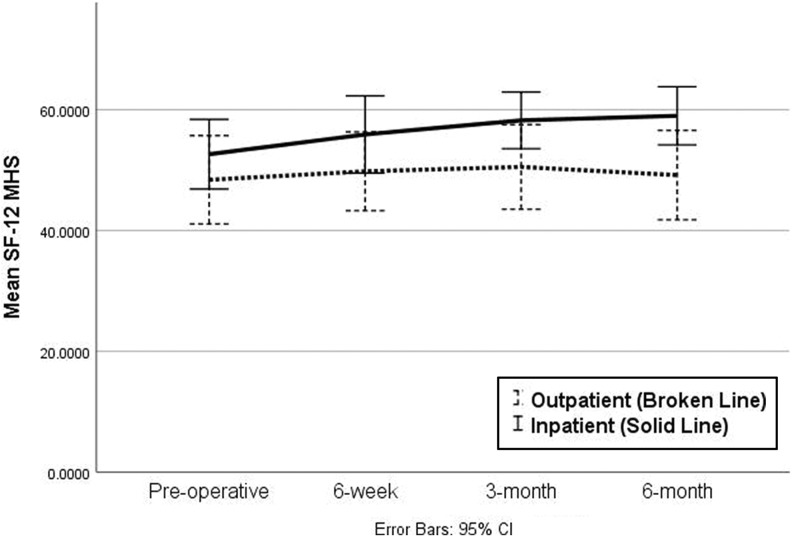
The NDI improved from 39.45 ± 18.92 preoperatively to 21.94 ± 17.49 at 6 months in the outpatient group (P < .0001), and from 46.06 ± 23.11 to 31.00 ± 20.60 (P = .001) in the inpatient group (Figure 3). Similarly, the VAS neck score improved from 6.16 ± 2.70 preoperatively to 2.99 ± 2.68 at 6 months in the outpatient group (P < .0001) and from 7.89 ± 11.32 to 3.67 ± 2.94 in the inpatient group (P = .089) (Figure 4). VAS arm score also improved from 5.86 ± 2.57 preoperatively to 2.82 ± 2.58 at 6 months in the outpatient group (P < .0001), and from 5.78 ± 2.89 to 3.67 ± 2.94 in the inpatient group (P = .002) (Figure 5). The SF-12 PHS improved from 34.4 ± 7.92 preoperatively to 39.7 ± 11.38 at 6 months in the outpatient group (P = .029), and from 30.11 ± 8.72 to 34.73 ± 10.12 in the inpatient group (P = .005) (Figure 6). Although, the SF-12 MHS improved in both groups, this change was not statistically significant in either group, with the score improving from 44.21 ± 14.52 preoperatively to 51.10 ± 11.05 at 6 months in the outpatient group (P = .169), and from 44.76 ± 11.74 to 48.52 ± 13.56 in the inpatient group (P = .064) (Figure 7).
Figure 3.
Mean Neck Disability Index (NDI) preoperatively and at each follow-up.
Figure 4.
Mean visual analogue scale (VAS) neck pain score preoperatively and at each follow-up.
Figure 5.
Mean visual analogue scale (VAS) arm pain score preoperatively and at each follow-up.
Figure 6.
Mean Short Form–12 (SF-12) physical health score (PHS) preoperatively and at each follow-up.
Figure 7.
Mean Short Form–12 (SF-12) mental health score (MHS) preoperatively and at each follow-up.
In terms of difference in PROs between the 2 groups, preoperatively, inpatients and outpatients were similar in terms of NDI, VAS neck, VAS arm, and SF-12 MHS. SF-12 PHS was worse in the inpatient group preoperatively (30.11 ± 8.72 vs 34.4 ± 7.92, P = .024) and this difference persisted at 6 weeks (30.79 ± 6.69 vs 35.66 ± 7.16, P = .008) but was not apparent at the 6 months follow-up (34.73 ± 10.12 vs 39.7 ± 11.38, P = .12). The outpatient group appeared to have better early outcomes in terms of 6-week NDI (27.97 ± 17.92 vs 37.59 ± 17.40, P = .014), VAS neck (2.92 ± 2.46 vs 4.02 ± 2.51, P = .044), and SF-12 PHS (35.66 ± 7.16 vs 30.79 ± 6.69, P = .008). However, these differences did not persist at 6 months, with both groups showing similar outcomes. There were no significant differences between the groups in terms of dysphagia, as evaluated by the SWAL-QOL at 6 or 12 weeks postoperatively (Table 3).
Table 3.
Patient-Reported Outcomes.
| Outpatient | Inpatient | P a | |
|---|---|---|---|
| NDI | |||
| • Preoperative | 39.45 ± 18.92 | 46.06 ± 23.11 | .15 |
| • 6 weeks | 27.97 ± 17.92 | 37.59 ± 17.40 | .014 |
| • 6 months | 21.94 ± 17.49 | 31.00 ± 20.60 | .058 |
| VAS neck pain | |||
| • Preoperative | 6.16 ± 2.70 | 7.89 ± 11.32 | .3 |
| • 6 weeks | 2.92 ± 2.46 | 4.02 ± 2.51 | .044 |
| • 6 months | 2.99 ± 2.68 | 3.67 ± 2.94 | .33 |
| VAS arm pain | |||
| • Preoperative | 5.86 ± 2.57 | 5.78 ± 2.89 | .9 |
| • 6 weeks | 2.54 ± 2.57 | 3.52 ± 2.87 | .097 |
| • 6 months | 2.82 ± 2.58 | 3.21 ± 2.78 | .55 |
| SF-12 PHS | |||
| • Preoperative | 34.4 ± 7.92 | 30.11 ± 8.72 | .024 |
| • 6 weeks | 35.66 ± 7.16 | 30.79 ± 6.69 | .008 |
| • 6 months | 39.70 ± 11.38 | 34.73 ± 10.12 | .12 |
| SF-12 MHS | |||
| • Preoperative | 44.21 ± 14.52 | 44.76 ± 11.74 | .86 |
| • 6 weeks | 51.31 ± 10.60 | 50.11 ± 12.74 | .68 |
| • 6 months | 51.10 ± 11.05 | 48.52 ± 13.96 | .47 |
| SWAL-QOL | |||
| • Preoperative | 92.20 ± 9.66 | 90.24 ± 12.38 | .473 |
| • 6 weeks | 89.21 ± 11.18 | 86.07 ± 15.89 | .365 |
| • 12 weeks | 93.83 ± 8.00 | 89.45 ± 13.89 | .309 |
Abbreviations: NDI, Neck Disability Index; VAS, visual analogue scale; SF-12; Short Form–12; PHS, physical health score; MHS, mental health score; SWAL-QOL, Swallowing Quality of Life questionnaire.
a P values in boldface indicate statistical significance (P < .05).
As seen in Table 4, there were also no significant differences between the inpatient and outpatient cohorts in terms of the percentage of patients achieving an improvement >MCID for NDI, VAS arm pain, and VAS neck pain at either the 6-week or the 3-month follow-up.
Table 4.
Percentage of Patients Experiencing an Improvement Greater Than Minimum Clinically Important Difference on the Neck Disability Index (NDI) and Visual Analog Scale (VAS).
| Outpatient, % | Inpatient, % | P | |
|---|---|---|---|
| NDI | |||
| • 6 weeks | 42.2 | 43.8 | .894 |
| • 3 months | 52.4 | 40.0 | .300 |
| VAS neck pain | |||
| • 6 weeks | 53.3 | 48.4 | .672 |
| • 3 months | 57.1 | 48.3 | .462 |
| VAS arm pain | |||
| • 6 weeks | 57.8 | 54.8 | .799 |
| • 3 months | 59.5 | 55.2 | .715 |
Discussion
Discogenic neck pain due to degenerative disc disease, including symptomatic myelopathy and/or radiculopathy, is becoming an increasingly common problem and ultimately a financial burden to the healthcare system. Since its introduction by Smith and Robinson,13 and Cloward14 in 1958, ACDF has become the gold standard surgical treatment for single and multilevel cervical degenerative disc disease because it results in improved clinical and radiographic outcomes.15-18
It is well-known that the current level and growth of US health care expenditure is unsustainable.19 More so, a significant portion of this expenditure has been shown to be cost-ineffective.19 Thus, in recent years there has been a trend toward emphasizing and promoting value-based health care, while reducing associated costs. This emphasis on reducing health care costs has led to numerous surgeries across specialties being performed on an outpatient basis.2 Because of relatively short operative times, moderate postoperative pain, and little need for postoperative wound care, 1-level ACDF is one of the most common spine surgeries that is currently performed on an outpatient basis. Despite the success of 1-level ACDF in the outpatient setting, concerns over increased postoperative complications, including respiratory compromise has curtailed the performance of multilevel ACDF in the same setting.
The results of our study show that patients undergoing outpatient surgery were younger, in better overall physical health, as evidenced by the lower ASA class and CCI, and had fewer levels operated. These findings are reflective of the criteria used at our institution for selection of patients for inpatient versus outpatient performance of surgery. In our practice, the decision on when to admit a patient after surgery is made mutually by the surgeon and anesthesiologist. In general, ASA class 3 or higher, BMI of >40 kg/m2, age >80 years, intubation time >2.5 hours, or not having a responsible adult with the patient warrant inpatient admission.
Postoperative retropharyngeal hematoma resulting in acute airway obstruction is one of the most catastrophic complications of ACDF surgery that can potentially be fatal if it is not detected and managed in a timely manner. Although these hematomas can occur up to several days after surgery, Lied et al20 and Garringer and Sasso21 found that all potentially life-threatening neck hematomas were detected within 4 to 6 hours of surgery. This suggests that discharge after 6-hour observation period is likely to be as safe as inpatient observation of longer duration. However, Lied et al20 did not report the number of levels operated and Garringer and Sasso21 only included single-level fusions. Thus, it is unknown whether a greater number of operative levels is likely to result in an increased risk of complications and warrant a longer observation period, including inpatient admission. In contrast to the studies by Lied et al20 and Garringer and Sasso,21 a recent report by Song et al22 found that 33% of postoperative hematomas occurred at a median of 72 hours after surgery. However, the latter included patients undergoing ACDF due to both, degenerative and traumatic conditions of the spine. If we only consider those who underwent surgery due to degenerative pathology, the 4 postoperative hematomas occurred between 4 to 8 hours postoperatively, which is similar to prior reports.
While there have been numerous reports on 1-level ACDF on an outpatient basis, evidence for multilevel ACDF in the same setting is limited. The few studies that include outpatient multilevel fusions also include 1-level fusions, which account for a majority of the study population.3,23-32
A number of large database studies, which include nation-wide and state-wide data, have studied the outcomes and safety of 1- and 2-level ACDF in the outpatient setting. These include studies by McGirt et al30 and Fu et al31 who reported on the complications and outcomes of outpatient versus inpatient 1- and 2-level ACDF in the National Surgical Quality Improvement Program (NSQIP) database, McClelland et al23,32 who reported on the complications and re-admissions data of outpatient 1- and 2- level ACDF in the State Ambulatory Services Data (SASD) for New Jersey and compared it with an inpatient population undergoing the same procedure from the Nationwide Inpatient Sample (NIS) data, and Arshi et al25 who reported in the risk of revision surgery and perioperative complications in outpatient 1- and 2-level ACDF in the PearlDiver Humana insurance records database. Consistent with the findings of our study, all these studies found that outpatient ACDF patients were younger and had fewer comorbidities than their inpatient counterparts. This finding is not surprising, given that age is a known risk factor for peri-complications in spine surgery25,33 and the presence of comorbidities may increase the risk anesthetic or other perioperative complications, and thus these patients are likely to be selected for inpatient procedures to allow for prolonged monitoring. Although these studies included 1- and 2- level cases in contrast to our study, which included 2- and 3- level cases, the findings of our study are consistent with the results reported by McGirt et al,30 Fu et al,31 and McClelland et al,23,32 which showed that ACDF can be safely performed in the outpatient setting, with no increase in complication rates in appropriately selected patients. In contrast, Arshi et al25 found a greater risk of perioperative complications, including the need for revision surgeries, as well as a higher risk of postoperative acute renal failure in the outpatient setting; the reason for this concerning finding is unclear.
A few smaller studies have also reported on the feasibility and safety of 1- and 2-level ACDF on an outpatient basis26 and in outpatient ambulatory surgery centers.3,24 These studies also found no increase in complication rates in the outpatient setting.
To our knowledge, only 2 studies,3,29 with a total of 10 cases have reported 3-level ACDF being performed in an outpatient setting. While Adamson et al3 had 6 reports of >2 levels being performed as outpatient ACDF, these cases comprised only 0.6% of their study population and hence were excluded from further analysis. Their findings for the remaining 1- and 2-level cases (with about 60% of cases being 1-level) performed in an outpatient ambulatory surgery center showed a <1% rate of surgical complications, which could be appropriately diagnosed and managed in a 4-hour postoperative monitoring window. Similar to the findings of our study, they found that the length of hospital stay, estimated blood loss, and duration of the procedure were greater in the inpatient cohort, and there was no difference in complications or surgical morbidity in either 1- or 2-level cases. Villavicencio et al29 reported their experience with 1-, 2-, and 3-level ACDF performed on an outpatient or 23-hour observation period basis and compared their complication rates to those reported in the literature. In this study as well, about 60% of cases were single-level fusions and only 4 were 3-level fusions. While 1- and 2-level fusions were discharged after an average hospital stay of 8 hours (range 2-15 hours), all the 3-level cases were discharged after a 23-hour observation period. They found no increase in overall or hardware-related complications in these patients undergoing outpatient surgery compared to complication rates reported in the literature.
A meta-analysis27 on outpatient ACDF also reported that nearly two-thirds of outpatient ACDFs are single-level procedures with just 0.5% extending beyond 2 levels. This study also reported a low readmission rate and complication rates comparable to inpatient procedures.
Even though the findings of our study are consistent with these reports in the literature, an important distinction is that all of these studies comprised 60% 1-level fusions, which have been shown to be safe in the outpatient setting. As a result, the low incidence of complications and readmissions can be attributed to the large number of single-level cases and may not be applicable to multi-level fusions.
Although the complication rate of 5.3% in the outpatient group and 37% in the inpatient group reported in our study is higher than the complication rates reported in the literature, a majority of these were due urinary retention, and not directly related to the procedure or hardware. In addition, retropharyngeal soft-tissue hematoma requiring reintubation was reported in only 1 patient and postoperative dysphagia was reported in 2 patients, all occurring in the inpatient group. The higher complication rate in the inpatient cohort may be attributable to baseline differences between the groups in terms of age, as well as CCI and ASA class, with the inpatient group having significantly higher scores on both these indices. In addition, there were differences in the duration of the surgical procedure and blood loss. Since patient selection for inpatient versus outpatient performance of surgery was based on surgeon preference, it is possible that the inpatient cohort had a poorer overall health and/or more complex cases, which could account for the higher complication rate and worse early PROs. Ultimately, it is critical that the patient undergoing surgery be aware and informed of all potential complications and make an informed decision as to the setting of surgery.
To our knowledge, this is the first report to focus solely on multilevel ACDF in the outpatient setting, and assess safety, outcomes and complications in these patients. In addition, no prior studies included PROs. As we move toward patient-centric value-based care, assessing patients’ health status and efficacy of interventions from the patient’s perspective is becoming increasingly important. Thus, incorporation of PROs in our study adds an important dimension to the analysis and interpretation of outcomes, which have thus far been limited to clinical or radiographic measures that may not necessarily reflect the patient’s perspective.
Limitations
The findings of this study should be interpreted with the inherent limitations and weaknesses in mind. This study was a retrospective review of prospectively collected data and thus selection bias cannot be completely eliminated. Criteria for patient selection could not be elucidated from retrospective analysis of the data. Thus patient selection for inpatient versus outpatient procedure could have been a result of surgeon preference due to technical difficulty or case complexity, unanticipated admission following planned outpatient surgery due to intra- or postoperative complications, or other administrative factors, such as insurance or staffing concerns.
A further limitation is that patients who were included in our study cohort may not necessarily be representative of all patients undergoing this surgical procedure. In addition, all patients did not have complete follow-up, and this could be a potential source of bias as well.
Patients included in the study were limited to those with degenerative conditions of the cervical spine who underwent minimally invasive ACDF, and hence these findings may not be applicable to other populations. Additionally, although our study population included 2- and 3-level fusions, the number of 3-level cases was quite small and may not have been sufficient to assess the outcomes of interest.
Additionally, radiographic outcomes were not analyzed and their correlation with clinical and PROs was not assessed.
While outpatient surgery has been shown to be associated with lower costs, the costs associated with these procedures were not analyzed in this study, and hence the cost saving could not be directly assessed.
Conclusion
The results of our study suggest that multi-level ACDF can be performed safely in the outpatient setting without an increased risk of complications compared with the inpatient setting in an appropriately selected patient. Importantly, the setting of the surgery does not affect patient reported outcomes. However, it is critical that the patient undergoing surgery be aware and informed of all potential complications and make an informed decision as to the setting of surgery. In our cohort, patients undergoing outpatient surgery were younger and were in better overall health, as evidenced by a lower CCI and ASA class. Outpatient surgery was related to fewer levels being fused, lower estimated blood loss and shorter procedure time. Criteria typically used to select patients for inpatient admission at our institution include ASA class 3 or higher, BMI >40 kg/m2, age >80 years, intubation time >2.5 hours, or not having a responsible adult with the patient. Ultimately patient selection is done on a case-by-case basis and will depend on numerous factors including but not limited to patient and surgeon comfort with the surgical setting, patient demographics and comorbidities, magnitude of the procedure and surgical technique, institutional policy, social support, and access to emergency care. Thus, while our results demonstrate that multilevel ACDF can be safely done in the outpatient setting, safety and feasibility very much depend on the individual case, comfort of the care team with early discharge, and resources for emergency care and ancillary support services; appropriate patient selection and surgical technique are of utmost importance.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr Kern Singh is a current Board Member of Vital 5 LLC, TDi LLC, Minimally Invasive Spine Study Group; takes part in Editorial Board at Contemporary Spine Surgery, Orthopedics Today, and Vertebral Columns; receives consultant fees from Zimmer Biomet, K2M; receives royalties from Zimmer Biomet, Stryker, RTI Surgical, Lippincott Williams and Wilkins, Thieme, Jaypee Publishing, Slack Publishing; and receives grants from Cervical Spine Research Society. Dr Sheeraz Qureshi currently receives consulting fees from Zimmer Biomet, Stryker Spine, Globus Medical, Inc; has shareholder interest in Avaz Surgical; and receives royalties from RTI, Zimmer Biomet, and Stryker Spine.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Oglesby M, Fineberg SJ, Patel AA, Pelton MA, Singh K. Epidemiological trends in cervical spine surgery for degenerative diseases between 2002 and 2009. Spine (Phila Pa 1976). 2013;38:1226–1232. doi:10.1097/BRS.0b013e31828be75d [DOI] [PubMed] [Google Scholar]
- 2. Baird EO, Egorova NN, Mcanany SJ, Qureshi SA, Hecht AC, Cho SK. National trends in outpatient surgical treatment of degenerative cervical spine disease. Global Spine J. 2014;4:143–150. doi:10.1055/s-0034-1376917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Adamson T, Godil SS, Mehrlich M, Mendenhall S, Asher AL, McGirt MJ. Anterior cervical discectomy and fusion in the outpatient ambulatory surgery setting compared with the inpatient hospital setting: analysis of 1000 consecutive cases. J Neurosurg Spine. 2016;24:878–884. doi:10.3171/2015.8.SPINE14284 [DOI] [PubMed] [Google Scholar]
- 4. Ban D, Liu Y, Cao T, Feng S. Safety of outpatient anterior cervical discectomy and fusion: a systematic review and meta-analysis. Eur J Med Res. 2016;21:34 doi:10.1186/s40001-016-0229-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sivaganesan A, Hirsch B, Phillips FM, McGirt MJ. Spine surgery in the ambulatory surgery center setting: value-based advancement or safety liability? Neurosurgery. 2018;83:159–165. doi:10.1093/neuros/nyy057 [DOI] [PubMed] [Google Scholar]
- 6. Liu CY, Zygourakis CC, Yoon S, et al. Trends in utilization and cost of cervical spine surgery using the National Inpatient Sample Database, 2001 to 2013. Spine (Phila Pa 1976). 2017;42: E906–E913. doi:10.1097/BRS.0000000000001999 [DOI] [PubMed] [Google Scholar]
- 7. McHorney CA, Robbins J, Lomax K, et al. The SWAL-QOL and SWAL-CARE outcomes tool for oropharyngeal dysphagia in adults: III. Documentation of reliability and validity. Dysphagia. 2002;17:97–114. doi:10.1007/s00455-001-0109-1 [DOI] [PubMed] [Google Scholar]
- 8. Chung AS, Copay AG, Olmscheid N, Campbell D, Walker JB, Chutkan N. Minimum clinically important difference: current trends in the spine literature. Spine (Phila Pa 1976). 2017;42:1096–1105. doi:10.1097/BRS.0000000000001990 [DOI] [PubMed] [Google Scholar]
- 9. Parker SL, Godil SS, Shau DN, Mendenhall SK, McGirt MJ. Assessment of the minimum clinically important difference in pain, disability, and quality of life after anterior cervical discectomy and fusion: clinical article. J Neurosurg Spine. 2013;18:154–160. doi:10.3171/2012.10.SPINE12312 [DOI] [PubMed] [Google Scholar]
- 10. Carreon LY, Glassman SD, Campbell MJ, Anderson PA. Neck Disability Index, Short Form–36 physical component summary, and pain scales for neck and arm pain: the minimum clinically important difference and substantial clinical benefit after cervical spine fusion. Spine J. 2010;10:469–474. doi:10.1016/j.spinee.2010.02.007 [DOI] [PubMed] [Google Scholar]
- 11. Auffinger B, Lam S, Shen J, Roitberg BZ. Measuring surgical outcomes in subaxial degenerative cervical spine disease patients. Neurosurgery. 2014;74:206–214. doi:10.1227/NEU.0000000000000247 [DOI] [PubMed] [Google Scholar]
- 12. Auffinger BM, Lall RR, Dahdaleh NS, et al. Measuring surgical outcomes in cervical spondylotic myelopathy patients undergoing anterior cervical discectomy and fusion: assessment of minimum clinically important difference. PLoS One. 2013;8:e67408 doi:10.1371/journal.pone.0067408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40-A:607–624. [PubMed] [Google Scholar]
- 14. Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15:602–617. doi:10.3171/jns.1958.15.6.0602 [DOI] [PubMed] [Google Scholar]
- 15. Fraser JF, Härtl R. Anterior approaches to fusion of the cervical spine: a metaanalysis of fusion rates. J Neurosurg Spine. 2007;6:298–303. doi:10.3171/spi.2007.6.4.2 [DOI] [PubMed] [Google Scholar]
- 16. Song KJ, Taghavi CE, Lee KB, Song JH, Eun JP. The efficacy of plate construct augmentation versus cage alone in anterior cervical fusion. Spine (Phila Pa 1976). 2009;34:2886–2892. doi:10.1097/BRS.0b013e3181b64f2c [DOI] [PubMed] [Google Scholar]
- 17. Yun DJ, Lee SJ, Park SJ, et al. Use of a zero-profile device for contiguous 2-level anterior cervical diskectomy and fusion: comparison with cage with plate construct. World Neurosurg. 2017;97:189–198. doi:10.1016/j.wneu.2016.09.065 [DOI] [PubMed] [Google Scholar]
- 18. Li Z, Zhao Y, Tang J, et al. A comparison of a new zero-profile, stand-alone Fidji cervical cage and anterior cervical plate for single and multilevel ACDF: a minimum 2-year follow-up study. Eur Spine J. 2017;26:1129–1139. doi:10.1007/s00586-016-4739-2 [DOI] [PubMed] [Google Scholar]
- 19. Reilley BM, Evans AT. Much ado about (doing) nothing. Ann Intern Med. 2009;150:270–271. doi:10.7326/0003-4819-150-4-200902170-00008 [DOI] [PubMed] [Google Scholar]
- 20. Lied B, Sundseth J, Helseth E. Immediate (0-6 h), early (6-72 h) and late (>72 h) complications after anterior cervical discectomy with fusion for cervical disc degeneration; discharge six hours after operation is feasible. Acta Neurochir (Wien). 2008;150:111–118. doi:10.1007/s00701-007-1472-y [DOI] [PubMed] [Google Scholar]
- 21. Garringer SM, Sasso RC. Safety of anterior cervical discectomy and fusion performed as outpatient surgery. J Spinal Disord Tech. 2010;23:439–443. doi:10.1097/BSD.0b013e3181bd0419 [DOI] [PubMed] [Google Scholar]
- 22. Song KJ, Choi BW, Lee DH, Lim DJ, Oh SY, Kim SS. Acute airway obstruction due to postoperative retropharyngeal hematoma after anterior cervical fusion: a retrospective analysis. J Orthop Surg Res. 2017;12:19 doi:10.1186/s13018-017-0517-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McClelland S, 3rd, Passias PG, Errico TJ, Bess RS, Protopsaltis TS. Inpatient versus outpatient anterior cervical discectomy and fusion: a perioperative complication analysis of 259 414 patients from the Healthcare Cost and Utilization Project Databases. Int J Spine Surg. 2017;11:11 doi:10.14444/4011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Stieber JR, Brown K, Donald GD, Cohen JD. Anterior cervical decompression and fusion with plate fixation as an outpatient procedure. Spine J. 2005;5:503–507. doi:10.1016/j.spinee.2005.01.011 [DOI] [PubMed] [Google Scholar]
- 25. Arshi A, Wang C, Park HY, et al. Ambulatory anterior cervical discectomy and fusion is associated with a higher risk of revision surgery and perioperative complications: an analysis of a large nationwide database. Spine J. 2018;18:1180–1187. doi:10.1016/j.spinee.2017.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Trahan J, Abramova MV, Richter EO, Steck JC. Feasibility of anterior cervical discectomy and fusion as an outpatient procedure. World Neurosurg. 2011;75:145–148. doi:10.1016/j.wneu.2010.09.015 [DOI] [PubMed] [Google Scholar]
- 27. McClelland S, 3rd, Oren JH, Protopsaltis TS, Passias PG. Outpatient anterior cervical discectomy and fusion: a meta-analysis. J Clin Neurosci. 2016;34:166–168. doi:10.1016/j.jocn.2016.06.012 [DOI] [PubMed] [Google Scholar]
- 28. Sheperd CS, Young WF. Instrumented outpatient anterior cervical discectomy and fusion: is it safe? Int Surg. 2012;97:86–89. doi:10.9738/CC35.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Villavicencio AT, Pushchak E, Burneikiene S, Thramann JJ. The safety of instrumented outpatient anterior cervical discectomy and fusion. Spine J. 2007;7:148–153. doi:10.1016/j.spinee.2006.04.009 [DOI] [PubMed] [Google Scholar]
- 30. McGirt MJ, Godil SS, Asher AL, Parker SL, Devin CJ. Quality analysis of anterior cervical discectomy and fusion in the outpatient versus inpatient setting: analysis of 7288 patients from the NSQIP database. Neurosurg Focus. 2015;39:E9 doi:10.3171/2015.9.FOCUS15335 [DOI] [PubMed] [Google Scholar]
- 31. Fu MC, Gruskay JA, Samuel AM, et al. Outpatient anterior cervical discectomy and fusion is associated with fewer short-term complications in one- and two-level cases. Spine (Phila Pa 1976). 2017;42:1044–1049. doi:10.1097/BRS.0000000000001988 [DOI] [PubMed] [Google Scholar]
- 32. McClelland S, 3rd, Passias PG, Errico TJ, Bess SS, Protopsaltis TS. Outpatient anterior cervical discectomy and fusion: an analysis of readmissions from the New Jersey State Ambulatory Services Database. Int J Spine Surg. 2017;11:3 doi:10.14444/4003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Buerba RA, Giles E, Webb ML, Fu MC, Gvozdyev B, Grauer JN. Increased risk of complications after anterior cervical discectomy and fusion in the elderly: an analysis of 6253 patients in the American College of Surgeons National Surgical Quality Improvement Program database. Spine (Phila Pa 1976). 2014;39:2062–2069. doi:10.1097/BRS.0000000000000606 [DOI] [PubMed] [Google Scholar]