Abstract
PURPOSE
This study aims to describe the pattern of presentation of Iraqi female patients with breast cancer by assessing the grades and stages of their cancers at the time of presentation, to identify patients’ main complaints, and to discover whether there is any difference in presentation between patients in Iraq and those in other countries.
PATIENTS AND METHODS
This is a retrospective cross-sectional study that was performed in the National Center of Cancer in 2018. The target population was female patients with breast cancer who came to the Center for treatment and follow-up. A sample of 171 patients was drawn from this population. Self-evaluation forms were used in interviews with the patients to collect personal and sociodemographic data; clinical and histologic characteristics of the patients’ tumors were obtained from their medical records. Ethical approval was obtained.
RESULTS
Forty-five percent of the patients were younger than age 50 years, and 25% were younger than age 45 years. In all, 42.9% of the patients were diagnosed with stage III and 25% with stage IV cancer, and metastasis was diagnosed in 24.1%. In our study population, 53.4% of the tumors were found in the right breast, and 3.9% of patients had bilateral breast tumors. The most common histopathologic type was invasive ductal carcinoma (81.4%) followed by invasive lobular carcinoma (6.9%) and tubular carcinoma (5.9%). The patients’ most common complaints were breast lump (71.3%) and pain (18.9%). No correlation was found between tumor stage and breast self-examination, family history, education, occupation, histopathology, or grade.
CONCLUSION
Most of the patients are diagnosed at a late stage when treatment is less effective.
INTRODUCTION
Cancer is the second leading cause of death worldwide, according to the WHO. Cancer was responsible for 8.8 million deaths in 2015, and it was the cause of about 1 in 6 deaths worldwide.1 Within the Eastern Mediterranean Region, cancer is the fourth-ranked cause of death after cardiovascular diseases, infectious diseases, and injuries.2 In 2008, the average cancer incidence in industrialized countries was more than 80 per 100,000, but it was less than 40 per 100,000 in developing countries.3 The Iraqi Cancer Registry revealed that in 2012, among an estimated population of 32,500,000, a total of 21,101 new cases of cancer were registered; 9,268 were in men and 11,833 were in women.4
Globally, breast cancer is the most frequent cancer among women and accounts for about 23% of all female cancers.5 Breast cancer is the second leading cause of death among all types of cancers in women (15% of all cancer deaths) after lung cancer (26% of all cancer deaths).6 According to Alwan,7 breast cancer is the most common type of cancer in Iraq. The Global Burden of Cancer 20138 study showed that breast cancer has the highest incidence and mortality rate of all cancers in women. According to the WHO, the incidence of breast cancer is increasing in developing countries, which may be the result of increased urbanization, increased life expectancy, and adoption of western lifestyles.1
Early detection of breast cancer in Iraq was established in 2001 by the Ministry of Health. Their efforts were then supported by other ministries and by the development of the National Cancer Research Program. The latest report from the International Union Against Cancer showed that Iraq has made significant progress toward providing cancer health services by extending the Iraqi National Registry to become a population-based registry, launching public campaigns that encourage early detection, encouraging physical activity and control of tobacco use, and providing better access to cancer diagnosis and treatment service free of charge.9 Many new centers were built in Baghdad and other provinces to provide better services and easier access to health care for patients throughout the country. With the expansion of the National Cancer Control Program, new studies are now being conducted to evaluate the breast cancer screening program in Iraq. A study in 201810 showed that the breast cancer screening program in Baghdad had a coverage rate ranging from 63% to 77% with detection ability ranging from 1% to 10%.
When a patient presents with breast cancer, the usual pattern of intake includes gathering data to construct sociodemographic, clinical, and pathologic profiles. Here, we describe the clinical profile or the patient’s history, which includes tumor history, past medical and surgical history, social history, family history, gynecologic history, and tumor stage. The pathologic profile captures the histopathologic type of malignancy, tumor grade, and molecular subtype. Staging of the tumor is also essential for proper treatment and for determining survival rates.11
Identifying the pattern of presentation of patients with breast cancer is a key part of developing effective methods of cancer control and patient management programs in Iraq. These patterns include collecting data regarding the patient’ age and the pathologic and clinical features of the tumor.
Multiple studies have been conducted in Iraq to determine the clinicopathologic features of breast cancer, and they have shown that incidence, stage, treatment, and survival are affected by the ethnic variation of the population.12 Thus, identifying how the characteristics of Iraqi patients with breast cancer deviate from the general trends for this disease may provide a guide for better treatment and early detection. The results of previous studies show variance in patients’ presentation in different timeframes, so this study is intended to provide information about patients in the National Center of Cancer during the last year to determine whether the patients’ presentations vary from those in previous studies. Most of the previous studies focused on a narrow scope of information with little regard for other types of data, such as when a study provided clinical data but had incomplete information about the patients’ sociodemographic status or vice versa. Thus, our data collection efforts included sociodemographic status; clinical, histopathologic, and molecular data; nutritional status (as indicated by body mass index [BMI]); and whether or not patients performed breast self-examination (BSE). Thus, this study provides a broader description of Iraqi patients than previous studies did.
This study was performed after the latest war and migration to show the effects of migration on patient characteristics. The International Organization for Migration in 2017 registered more than 3 million internally displaced people, which had an adverse effect on Iraq’s Ministry of Health.9
This study aims to describe the patterns of presentation for Iraqi females with breast cancer by assessing the grade and stage of their tumors at the time of presentation and by identifying the patients’ main complaints to determine whether any differences have cropped up over time in Iraqi patients’ presentations.
PATIENTS AND METHODS
This is a retrospective cross-sectional study that was carried out in the Oncology Teaching Hospital and National Center of Cancer during the 4 months between April 2018 and the beginning of August 2018. Eligibility requirements for the study included being female and being a patient with breast cancer who regularly came to the hospital and the National Center of Cancer for treatment and follow-up. The only inclusion criterion was being a patient diagnosed on the basis of the following assessments: breast physical examination, mammography, and histopathology (for confirmation). A sample of 171 patients was drawn from this target population.
Patients were interviewed, and self-evaluation forms were used to capture data regarding sociodemographics (ie, age, occupation, marital status, number of children, and residency), the number of times a woman had been pregnant, the number of pregnancies that reached a viable gestational age (including live births and stillbirths), time of menarche, time of menopause, family history of breast cancer, main complaint (ie, a lump discovered by BSE or during checkup or pain as the reason for the first visit), previous visit to a physician for consultation regarding a breast problem, and breast augmentation surgery. Clinical and pathologic characteristics (grade, TNM stage, metastasis, recurrence, tumor size, and histopathologic type of malignancy) were obtained from patients’ medical records.
Most of the data were collected by using the QuickTapSurvey app on smartphone devices; paper-based forms were rarely used. Data were collected from patients while they were receiving treatment, and all patients had invasive ductal carcinoma. In some situations, the data were collected from first-degree relatives. The mean amount of time required for collecting data from patients was 8.5 minutes. Exclusion criteria included having mental problems, having mental deficits, or having records with incomplete information. Informed consent was provided by all patients using forms provided by the hospital. Each patient’s data were covered by full privacy policies, and each patient’s identity and profile will be fully protected. SPSS v.24 (SPSS, Chicago, IL) was used for processing all statistical data. All statistical tests were performed at a 95% level of significance and were two-sided; a P value < .05 indicated statistical significance. Descriptive statistics in the form of mean, median, mode, standard deviation (SD), and quartiles were used for quantitative data, and proportions were used for qualitative data. For analysis, χ2, one-way analysis of variance, t test, and binary logistic regression were used to determine significant correlations.
RESULTS
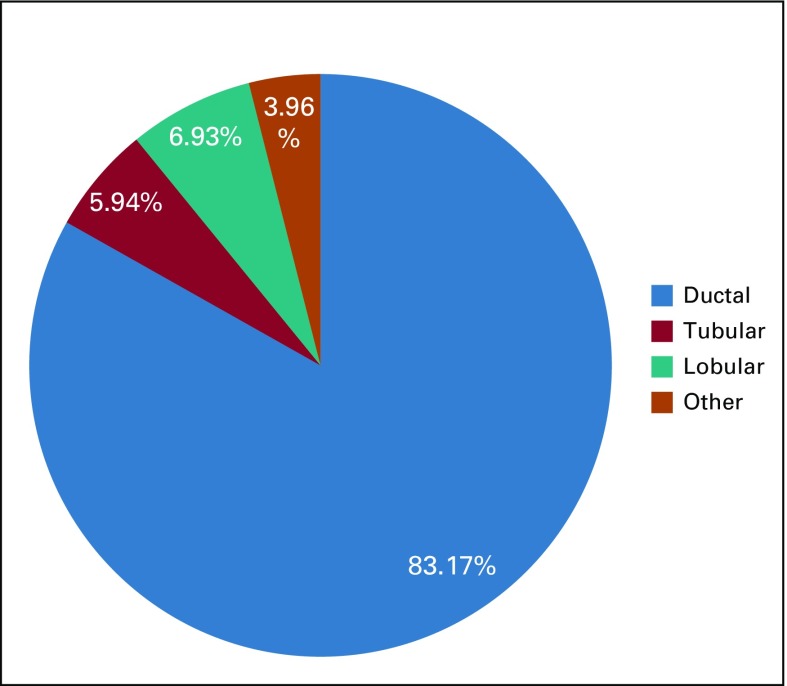
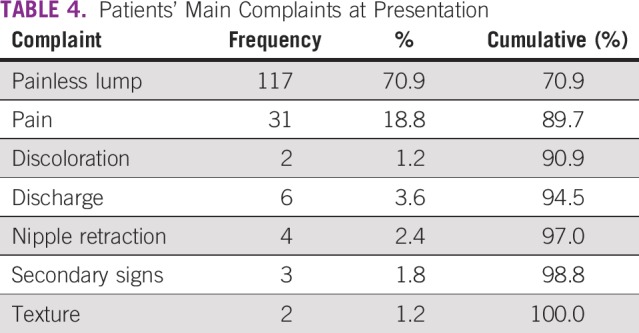
The mean patient age was 51.6 years (SD, 10.88 years; Table 1), and three quarters of the patients were younger than age 59 years. Table 2 lists the characteristics of the patients and their tumors, and Table 3 describes the pathologic and clinical features of the malignant tumors. More than 67% of the patients had advanced stage (III or IV) cancer. No significant correlation was found between molecular subtypes and tumor grade (P = .09). The mean BMI was 29.82 (SD, 6.2). About 75% had a BMI above 25, which means that three quarters of the patients were either overweight or obese; 7.6% were morbidly obese. Only 20% performed BSE regularly. Those with a higher level of education were more likely to perform BSE, and this was statistically significant (P = .006); however, there was no significant correlation between BSE and early diagnosis of the disease (P = .63). The histopathologic subtypes are shown in Figure 1, with invasive ductal carcinoma being the most common subtype (83.17%). No significant correlation was found between histopathologic subtype and disease stage, recurrence, laterality, or tumor grade. The main complaints at the time of presented are listed in Table 4, with painless lump being the most common (70.9%). Statistics showed no significant correlation between main complaints and disease stage.
TABLE 1.
Patient Age at Time of Diagnosis
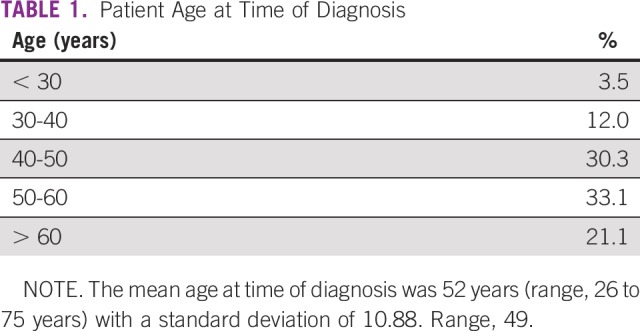
TABLE 2.
Patient and Disease Characteristics
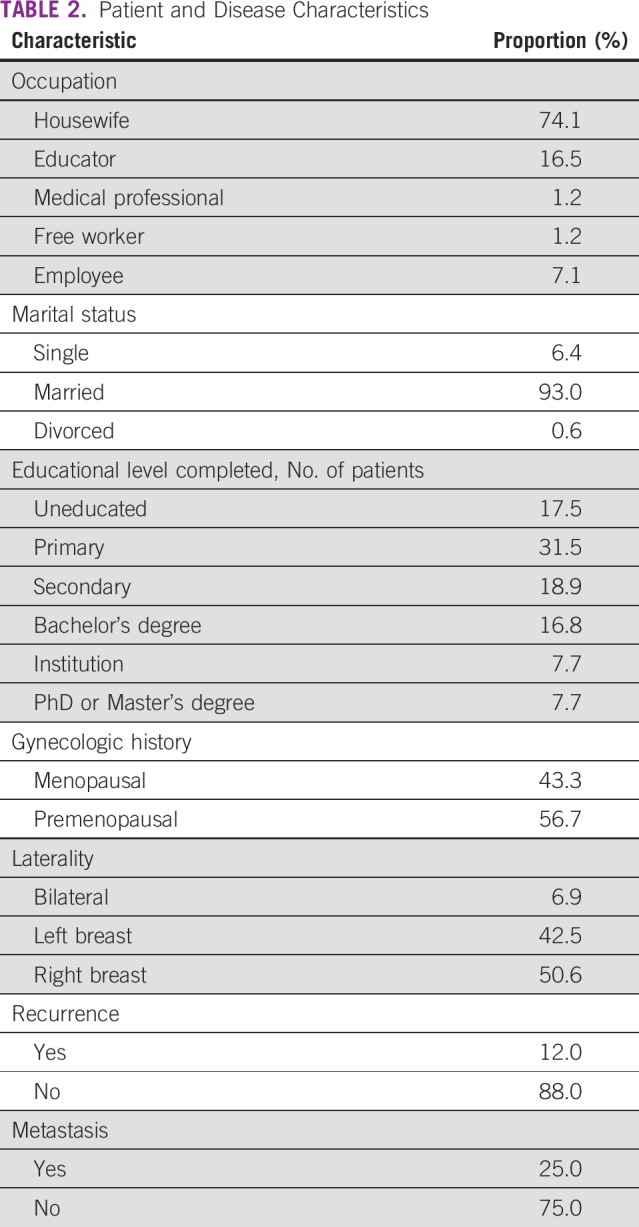
TABLE 3.
Clinical and Histopathologic Characteristics of Patients’ Breast Cancer
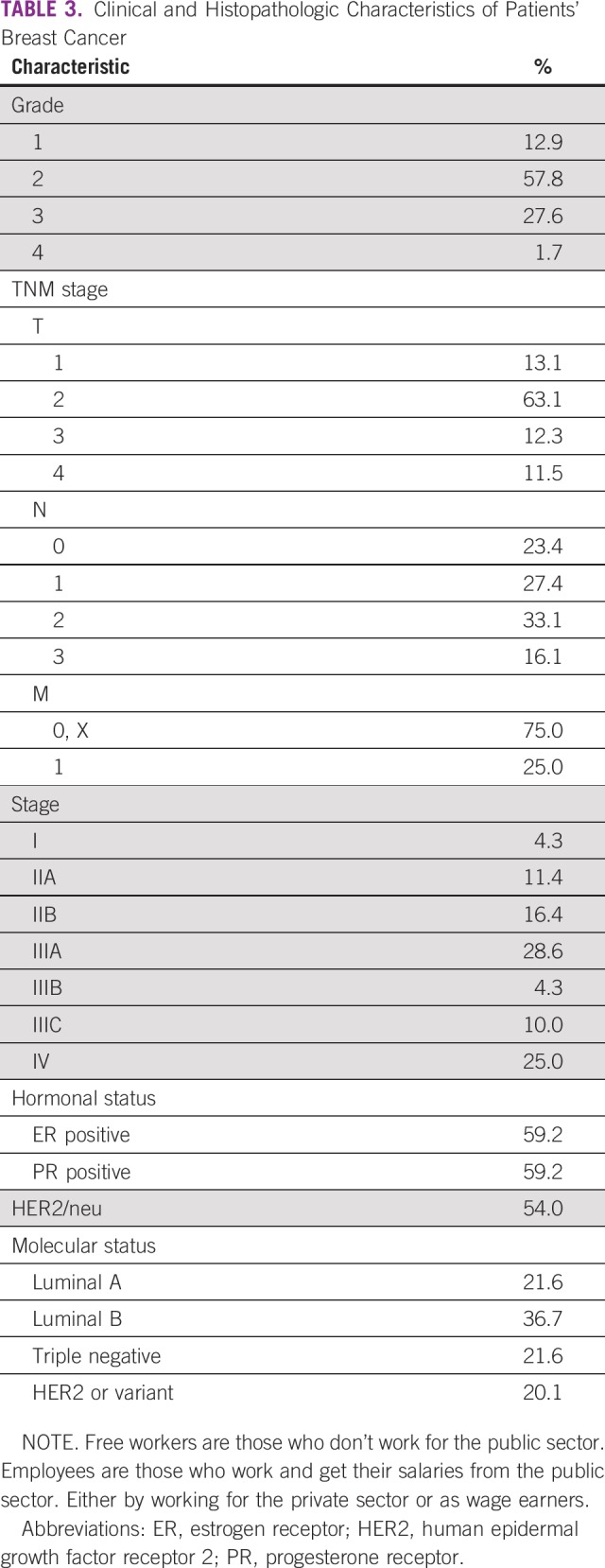
FIG 1.
Occurrence of main histopathologic subtypes of tumors.
TABLE 4.
Patients’ Main Complaints at Presentation
DISCUSSION
The clinical outcome of breast cancer is affected by the age of the patient at presentation. Breast cancer in young age groups is associated with more aggressive types of cancer, and many studies report that young age at diagnosis is associated with a high risk of recurrence and death.13 Age distribution showed that 45% of patients with invasive carcinoma were younger than age 50 years, which reflects a difference in the distribution of cancer among age groups in Iraq compared with that in other societies. This difference was also found in another study conducted between 2004 and 2008 in Iraq, in which 54.1% of the patients were found to be younger than age 50 years.7 According to the American Cancer Society, in the United States between 2017 and 2018, only 19% of patients with breast cancer were younger than age 50 years.14 This difference may be because of the younger demographic profile in the Arab population, as suggested by WHO collaborative work.14 In the developing countries, advanced stage at diagnosis is the major contributor to the higher rates of morbidity and mortality.14 In this study, 65% of the patient sample had stage III to IV cancer (late presentation), which explains why the mortality rate in developing countries is high.
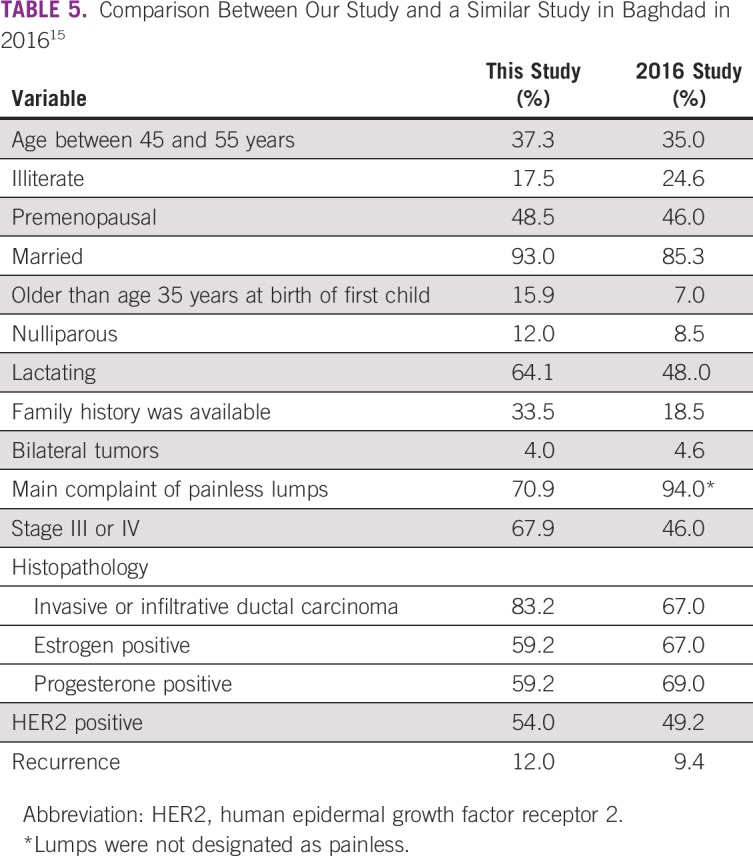
Late presentation was also found in another Iraqi study15 in which 47% of the patients presented with advanced stages of the disease; only 9.8% presented at stage I (Table 5). In a recent study published in 2018,16 50.5% of patients had tumor stage III or IV. A study conducted in Maysan governorate in southern Iraq showed that stage II was the most common (52.9%) followed by stage III (29.4%), which also indicates that most of the patients presented with advanced-stage disease.17 Another study18 conducted in 2010 in the Northern region of Nigeria included 103 patients and showed that most (62%) presented with advanced-stage disease. Late presentation can be attributed to the lack of knowledge and awareness of the disease and failure to identify the warning signs, because 29.5% did not seek medical attention until they felt pain or noticed abnormal discharge, ulceration, or a change in breast texture. Late presentation may also be attributed to a delay in deciding to visit the doctor after noticing warning signs.19 The women may be afraid of a cancer diagnosis20 or they might have thought that the signs were not serious. It is also possible that their religious beliefs were the cause for the delay.21
TABLE 5.
Comparison Between Our Study and a Similar Study in Baghdad in 201615
In addition, lack of effective screening programs causes late presentations. Accordingly, there is a need to develop effective screening programs that could help reduce late presentations and thereby achieve better prognosis. Even though BSE is not really a screening strategy, it is considered to be valuable for encouraging breast awareness. It is not surprising that BSE alone does not necessarily have an impact on stage at presentation, as the results have shown.
In this study, a family history of breast cancer was found in 33.5% of patients. In a study conducted in 2015, 30% of the patients had a family history of breast cancer, whereas studies from the United Kingdom revealed that family history was present in only 15% of the patients.22 There is a need to investigate the wide variation in the presence of family history between Iraqis and other populations.
This study showed that a lump in the breast was the most common feature at presentation (71.3%) compared with another study that analyzed data from the English National Audit of Cancer Diagnosis in Primary Care (2009-2010), which showed that about 83% of female patients presented with a lump.23 This is a characteristic sign of the disease, and it has been noted that patients tend to request a breast consultation if they have a lump rather than other abnormalities.23 In our study, a triple-negative molecular subtype was found in 21.6% of patients whereas in American patients with breast cancer, only 12% of the total number of patients had triple-negative disease.24 Triple-negative disease has been correlated with a high mortality rate because of the lack of targeted therapy.25 This could explain the high mortality rate observed among Iraqi patients in addition to late discovery of the disease discussed earlier.
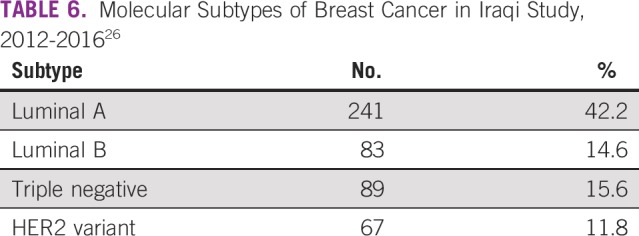
In comparison with another study7 of patients presenting with breast cancer, which had a sample size of 570 females (Table 6), our study showed that the molecular subtype with the highest proportion was luminal B, while in that study, it was luminal A, with a large difference between the two proportions. As the data in (Table 6) reflects the results of the study which was conducted on 2016, in which, luminal A had the highest proportion. While in our study, luminal B had the highest proportion. In a recent study, luminal A was the most common type in 47.4% of the patients, luminal B in 13.7%, human epidermal growth factor receptor 2 (HER2)–enriched cancer in 10.7%, and triple-negative in 14.7%.26
TABLE 6.
Molecular Subtypes of Breast Cancer in Iraqi Study, 2012-201626
Some studies showed that invasive lobular carcinoma was more likely to be advanced stage, low grade, estrogen receptor and progesterone receptor positive, and have higher incidence in contralateral breast cancer,27,28 but was not significant in this study.
In conclusion, most of the patients in Iraq who have breast cancer present at a late stage, and their most common complaint was a painless breast lump. The age of patients at the time of diagnosis was younger than that in other populations.
ACKNOWLEDGMENT
We thank Mustafa Majid Hameed, Ali Abdulmortafea Aljabery, Sara Shihab, and Munwar Alnaqash who helped us with this study, and members of the Community Department in the College of Medicine, University of Baghdad, especially Batool Ali Galib, Tariq A. Mutar, Seemaa Albahrani, Saleh I. Goyani, Siham Jalal, and Mohammed Almawashee, for their support.
Footnotes
Presented as an oral presentation at Baghdad College of Medicine 17th Scientific Conference, Baghdad, Iraq, November 28-29, 2018; and as a poster presentation at 30th European Students’ Conference ESC, Berlin, Germany, September 25-28, 2019.
AUTHOR CONTRIBUTIONS
Conception and design: All authors
Financial support: All authors
Administrative support: Mohammed Tareq Mutar, Mohammed Saleh Goyani, Ali Mohammed Hadi
Provision of study materials or patients: Mohammed Tareq Mutar, Mohammed Saleh Goyani, Ali Mohammed Hadi
Collection and assembly of data: Mohammed Tareq Mutar, Ali Mohammed Hadi
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jgo/site/misc/authors.html.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
No potential conflicts of interest were reported.
REFERENCES
- 1.World Health Organization Cancer. 2018 https://www.who.int/en/news-room/fact-sheets/detail/cancer/ September 12,
- 2.World Health Organization, Regional Office for the Eastern Mediterranean Towards a strategy for cancer control in the Eastern Mediterranean Region. http://applications.emro.who.int/dsaf/dsa1002.pdf
- 3.Ferly J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 4.Iraqi Cancer Board . Results of the Iraqi Cancer Registry 2009. Baghdad, Iraq: Iraqi Cancer Registry Center, Ministry of Health; 2015. https://moh.gov.iq/upload/upfile/ar/833.pdf [Google Scholar]
- 5.Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010 doi: 10.1002/ijc.25516. https://onlinelibrary.wiley.com/doi/full/10.1002/ijc.25516 [DOI] [PubMed] [Google Scholar]
- 6.Kumar V, Abbas A, Aster J, et al. Robbins Basic Pathology(ed 9)Philadelphia, PA: Saunders; 2013. pp 170, 208 [Google Scholar]
- 7.Alwan NA. Breast cancer: Demographic characteristics and clinico-pathological presentation of patients in Iraq. East Mediterr Health J. 2010;16:1159–1164. [PubMed] [Google Scholar]
- 8.Global Burden of Disease Cancer Collaboration. Fitzmaurice C, Dicker D, et al. The global burden of cancer 2013. JAMA Oncol. 2015;1:505–527. doi: 10.1001/jamaoncol.2015.0735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alwan N, Kerr D. Cancer control in war-torn Iraq. Lancet Oncol. 2018;19:291–292. doi: 10.1016/S1470-2045(18)30135-9. [DOI] [PubMed] [Google Scholar]
- 10.Alkhazrajy LA, Souza AM. Effectiveness and results of Iraqi breast cancer screening program applied at primary health care centers. https://www.ijmrhs.com/medical-research/effectiveness-and-results-of-iraqi-breast-cancer-screening-program-applied-at-primary-health-care-centers.pdf
- 11.National Cancer Institute, Surveillance, Epidemiology, and End Results (SEER) Program Cancer of the Breast (Female), in Cancer Stat Facts. https://seer.cancer.gov/statfacts/html/breast.html
- 12.Jack RH, Davies EA, Møller H. Breast cancer incidence, stage, treatment and survival in ethnic groups in South East England. Br J Cancer. 2009;100:545–550. doi: 10.1038/sj.bjc.6604852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reyna C, Lee MC. Breast cancer in young women: Special considerations in multidisciplinary care. J Multidiscip Healthc. 2014;7:419–429. doi: 10.2147/JMDH.S49994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Cancer Society Cancer Facts & Figures 2018. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2018/cancer-facts-and-figures-2018.pdf
- 15.Alwan NAS. Breast cancer among Iraqi women: Preliminary findings from a regional comparative breast cancer research project. J Glob Oncol. 2016;2:255–258. doi: 10.1200/JGO.2015.003087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alwan NAS. Tumor characteristics of female breast cancer: Pathological review of mastectomy specimens belonging to Iraqi patients. World J Breast Cancer Res. 2018;1:1006. [Google Scholar]
- 17.Alhelfi HSQ, Alhashimi RAH. Pattern of presentation of breast cancer in Missan’s women . Int J Basic Appl Sci. 2015;4:162–167. [Google Scholar]
- 18.Kene TS, Odigie VI, Yusufu LM, et al. Pattern of presentation and survival of breast cancer in a teaching hospital in north Western Nigeria. Oman Med J. 2010;25:104–107. doi: 10.5001/omj.2010.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gangane N, Anshu, Manvatkar S, et al. Prevalence and risk factors for patient delay among women with breast cancer in rural India. Asia Pac J Public Health. 2016;28:72–82. doi: 10.1177/1010539515620630. [DOI] [PubMed] [Google Scholar]
- 20.Maghous A, Rais F, Ahid S, et al. Factors influencing diagnosis delay of advanced breast cancer in Moroccan women. BMC Cancer. 2016;16:356. doi: 10.1186/s12885-016-2394-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Odongo J, Makumbi T, Kalungi S, et al. Patient delay factors in women presenting with breast cancer in a low income country. BMC Res Notes. 2015;8:467. doi: 10.1186/s13104-015-1438-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brewer HR, Jones ME, Schoemaker MJ, et al. Family history and risk of breast cancer: An analysis accounting for family structure. Breast Cancer Res Treat. 2017;165:193–200. doi: 10.1007/s10549-017-4325-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koo MM, von Wagner C, Abel GA, et al. Typical and atypical presenting symptoms of breast cancer and their associations with diagnostic intervals: Evidence from a national audit of cancer diagnosis. Cancer Epidemiol. 2017;48:140–146. doi: 10.1016/j.canep.2017.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ghodsi Z, Hojjatoleslami S. Breast self examination and mammography in cancer screening: Women health protective behavior. J Prev Med Hyg. 2014;55:46–49. [PMC free article] [PubMed] [Google Scholar]
- 25.Bianchini G, Balko JM, Mayer IA, et al. Triple-negative breast cancer: Challenges and opportunities of a heterogeneous disease. Nat Rev Clin Oncol. 2016;13:674–690. doi: 10.1038/nrclinonc.2016.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alwan NAS, Mualla FH, Al Naqash M, et al. Clinical and pathological characteristics of triple positive breast cancer among Iraqi patients. Gulf J Oncolog. 2017;1:51–60. [PubMed] [Google Scholar]
- 27.Arpino G, Bardou VJ, Clark GM, et al. Infiltrating lobular carcinoma of the breast: Tumor characteristics and clinical outcome. Breast Cancer Res. 2004;6:R149–R156. doi: 10.1186/bcr767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Glas NA, Engels CC, Bastiaannet E, et al. Contralateral breast cancer risk in relation to tumor morphology and age-in which patients is preoperative MRI justified? Breast Cancer Res Treat. 2015;150:191–198. doi: 10.1007/s10549-015-3294-6. [DOI] [PMC free article] [PubMed] [Google Scholar]