Abstract
PURPOSE
Misconceptions associated with radiotherapy (RT) may affect the patient’s choice to undergo or not undergo RT. In this study, the level of awareness and perceptions about radiation and RT, as well as their impact on the use of RT, were assessed.
MATERIALS AND METHODS
A cross-sectional survey was conducted in the city of Dar es Salaam, Tanzania, between November 2018 and March 2019. Stratified sampling was used to obtain a sample of 629 participants from 4 strata, including 53 patients with cancer, 129 health professionals, 127 medical and nursing students, and 320 respondents from the general public. A questionnaire with 13 items measuring awareness and 8 items measuring perceptions was used for data collection. The Kruskal-Wallis test and χ2 test were used to test association between predictor and outcome variables. Statistical analyses were performed using statistical software.
RESULTS
The percentage of right responses was < 50% in all 13 awareness items. Only 16.9% of respondents were aware that RT would not reduce their lifespan. Only 34.5% of respondents had positive perceptions of RT. Awareness was higher among medical/nursing students, younger respondents, single or cohabiting respondents, and those who had attained a college or higher education. Overall, 52% would accept receiving RT if recommended as part of their treatment. Those who would accept undergoing RT were more likely to have higher awareness and a positive perception of RT.
CONCLUSION
Public awareness of RT in Dar es Salaam is low, and negative perceptions prevail. Low levels of awareness and negative perceptions have a negative effect on the use of RT.
INTRODUCTION
Radiotherapy (RT) remains an important modality in the management of cancer because approximately half of all newly diagnosed patients with cancer require RT at some point during the course of their disease.1,2 RT is a highly cost-effective treatment modality, accounting for only 5% of the total cost of cancer care.3 It can be used either alone or in combination with other treatment modalities, such as chemotherapy and hormonal therapy, in a variety of tumor sites.
Optimal RT use (oRTU), defined as the proportion of all patients with cancer with an indication for RT, varies between countries, depending on case mix of the cancer types and stages at presentation. Evidence-based estimates of oRTUs range from approximately 47% to 56%, regardless of the level of economic development.4,5 Actual RT use rates, however, vary widely, depending on the level of economic development, with rates ranging from 9% to 46% in low- and middle-income countries (LMICs)6 and 54% to 108% in high-income countries.5
Access to RT is the main barrier to oRTU in LMICs with alarming scarcity in radiation oncology resources. Only approximately 40% of LMICs had infrastructures for radiation oncology in 2013.8,9 In studies in African countries, RT accessibility ranged from 0% to 88%,9 and approximately 60% of all radiation oncology resources were located in only 2 countries, Egypt and South Africa.10 Even in countries with nearly adequate resources, resources tend to be located in large urban centers, creating a geographic barrier to RT access.11
Although RT access is recognized as the main barrier to the use of RT, other factors that are not directly related to access may affect the use of RT.12 Patients’ or carers’ awareness and perceptions about RT are part of consumer-level factors that might affect the use of RT. Patients with cancer who would benefit from RT may opt for complementary and alternative therapies because they believe that RT is less beneficial and riskier.13,14
CONTEXT
Key Objective
To assess awareness and perceptions of radiotherapy (RT) among residents of Dar es Salaam and how awareness and perceptions affect RT uptake.
Knowledge Generated
We found that the level of RT awareness among respondents was low, and a large proportion had negative perceptions about RT. Low awareness and negative perceptions were found to be significant barriers to RT use.
Relevance
One of the objectives of the national cancer control strategy (2013-2022) is to ensure that quality RT services are accessible to all patients with cancer. To achieve this objective, the government is committed to investing in modern RT infrastructures, as well as establishing more RT centers. However, to ensure that investment in RT infrastructures is translated to increased RT use, gaps in awareness and negative perceptions must be addressed because low awareness and negative perceptions can significantly affect RT use.
Public awareness about RT and its importance in cancer management is low. A survey on the public awareness of RT in the United Kingdom revealed that only 10% of people were aware that RT can cure a large proportion of cancers, and approximately 40% had negative perceptions about RT.15 These negative perceptions are exacerbated by information from the media, such as links to nuclear power plant accidents, nuclear weapons, and secondhand experiences.16 They increase anxiety about RT and may lead to delay in seeking care or refusal of treatment.17
Like other low-income countries, Tanzania had only 2 cobalt-60 units serving a population of about 47 million in 2012.18,19 In this situation, a national cancer control strategy (2013-2022) was developed to address problems in cancer control, and among its objectives were ensuring timely access to optimal treatment.20 Implementation of this strategy has resulted in an increase in the number of teletherapy units from 2 in 2012 to 7 in 2017, as well as establishment of RT services in one zonal hospital. Therefore, in light of the benefits of this investment in RT infrastructures, other factors that might affect the use of RT must be addressed. In this study, we assessed the influence of awareness and perception of RT on RT uptake among people of diverse sociocultural backgrounds in the city of Dar es Salaam, Tanzania.
MATERIALS AND METHODS
Setting
The study was conducted in the Dar es Salaam region in Tanzania. Dar es Salaam is the largest and major industrial city in Tanzania, located along the Indian Ocean. It has a population of approximately 5.5 million,21 which constitutes approximately 10% of the population of Tanzania. Dar es Salaam is a metropolitan city, with a mixture of people from all ethnic groups, with the highest (compared to all other cities in Tanzania) in-migration rate of about 31%.22 The major health services facilities, including the Muhimbili National Hospital and the Ocean Road Cancer Institute (ORCI), are located in Dar es Salaam.
Study Population
A cross-sectional survey was conducted in the Dar es Salaam region in Tanzania between November 2018 and March 2019. Stratified sampling was used to obtain a sample of 629 respondents, which included 53 patients with cancer, 129 health professionals, 127 medical/nursing students, and 320 individuals from the general public.
Patients with cancer were randomly sampled from newly diagnosed patients referred to the ORCI for treatment, whereas respondents from the general public were randomly sampled from both slum and nonslum areas of the city. Health professionals were randomly sampled from both public and private hospitals in Dar es Salaam. Final-year medical and nursing students were randomly sampled from both public and private medical universities in Dar es Salaam.
Data Collection Tools
A list of misconceptions about RT was created by asking radiotherapists, radiation oncologists, and nurses involved in caring for patients with cancer about mistaken perceptions. Additional items were added to the list by asking a small sample of members of the public about RT. The list was presented to a panel of 5 experts, consisting of radiotherapists and radiation oncologists, for their input, and a final list of 21 items was obtained and used to create questionnaires. Thirteen items associated with a definite piece of information were categorized under “knowledge,” and the remaining 8 items not associated with a definite answer were categorized under “perception.” The questionnaire had a section with questions about sociodemographic characteristics and RT uptake. Questionnaires were administered to 10 potential respondents to test whether the questions captured the intended information.
Quality Control
Data collectors were trained to ensure they understood the meaning of every survey question, procedures during data collection, and how to respond to the participants’ questions. Items and response choices were read to respondents who had difficulty reading because of illiteracy or poor vision.
All respondents in this study signed a written informed consent form. Ethical clearance was obtained from the ORCI Academics, Research, Publications, and Ethics Committee.
Data Analysis
Each right response to the 13 awareness items was given a score of 1. Overall awareness scores below the 25th percentile, between the 25th and 75th percentiles, and above the 75th percentile were grouped as low, medium, and high awareness, respectively.
Responses from 8 perception items were given scores of 1 if the respondent agreed, −1 if the respondent disagreed, and 0 it the respondent neither agreed nor disagreed. The overall perception score was the sum of scores for all 8 questions. Overall scores at or above the 25th percentile were grouped as negative; those between the 25th and 75th percentiles were taken as neutral, whereas those above the 75th percentile were taken as positive.
The Kruskal-Wallis and χ2 tests were used to explore the association between overall awareness, perception and RT uptake, and sociodemographic characteristics. A P value < .05 was considered statistically significant. Statistical analyses were performed using Statistical Package for Social Sciences for Windows software (version 23.0; SPSS, Chicago, IL).
RESULTS
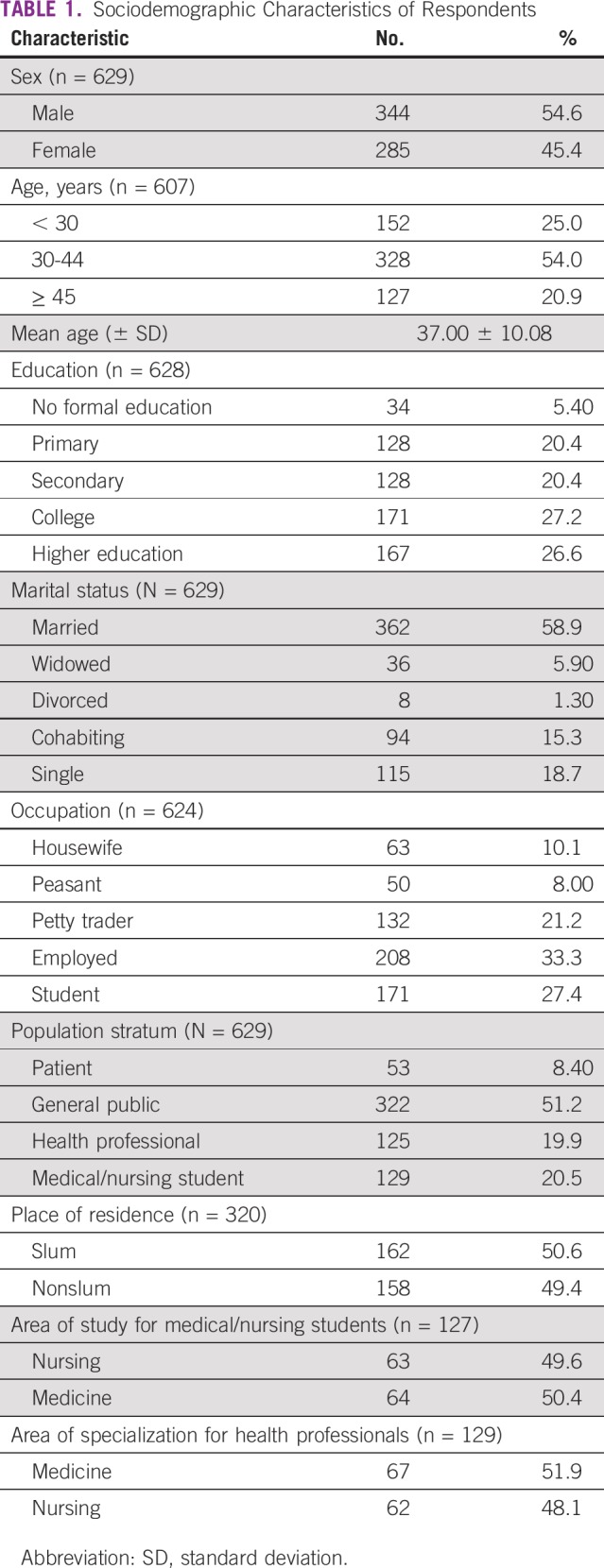
Sociodemographic Characteristics of Respondents
A total of 629 participants were included: 53 patients with cancer, 320 participants from the general population, 129 health professionals, and 127 students. There were 344 male respondents (54.6%), and 285 female respondents (45.4%). The majority of the respondents (54%) were 30-44 years of age. A total of 594 (94.6%) had formal education, and more than 50% had acquired a diploma or degree. Sociodemographic characteristics are summarized in Table 1.
TABLE 1.
Sociodemographic Characteristics of Respondents
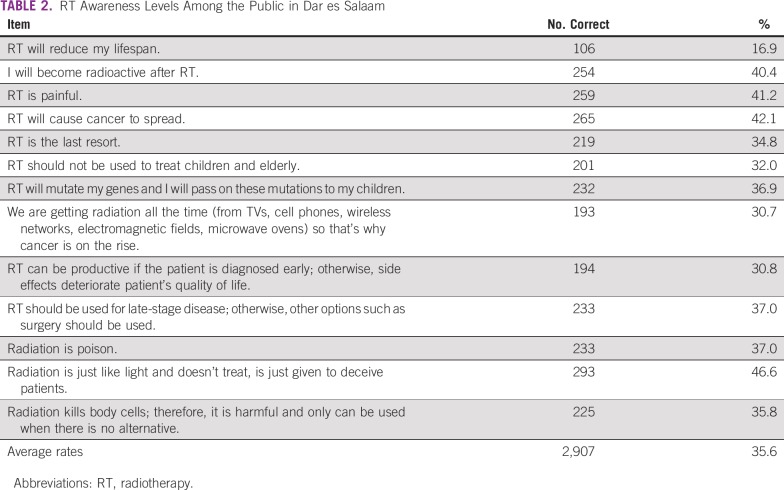
Awareness of RT
The average rate of right responses from all 13 awareness items was 35.6%. The majority of respondents (83.1%) believed that RT would reduce their lifespan. The highest rate of correct responses was recorded for the item, “Radiation is just like light and doesn’t treat, is just given to deceive patients,” which had a correct score of 46.6% (Table 2). The results revealed that 33.9% of respondents had low levels of awareness about RT, whereas 42.8% and 23.2% had medium and high levels of awareness, respectively.
TABLE 2.
RT Awareness Levels Among the Public in Dar es Salaam
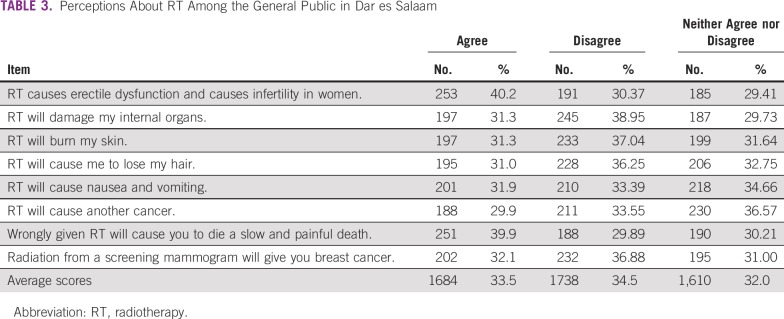
Perception of RT
Average scores for the 88 items regarding RT perceptions were 33.5% for agree, 34.5% for disagree, and 32.0% for neither agree nor disagree. The highest agree rate of 40.2% was recorded for the item “RT causes erectile dysfunction and causes infertility in women.”
The lowest agreement rate was recorded for the item “RT will cause another cancer,” with an agree score of 29.9% (Table 3). The expected response for a respondent with positive perceptions was “disagree” for all 8 perception items. Overall, 37.4% of respondents had a negative perception score, whereas 28.3% had a positive perception score.
TABLE 3.
Perceptions About RT Among the General Public in Dar es Salaam
Factors Influencing Awareness of RT
The association between awareness and respondent sociodemographic characteristics is summarized in Table 4.
TABLE 4.
Factors Influencing Radiotherapy Awareness
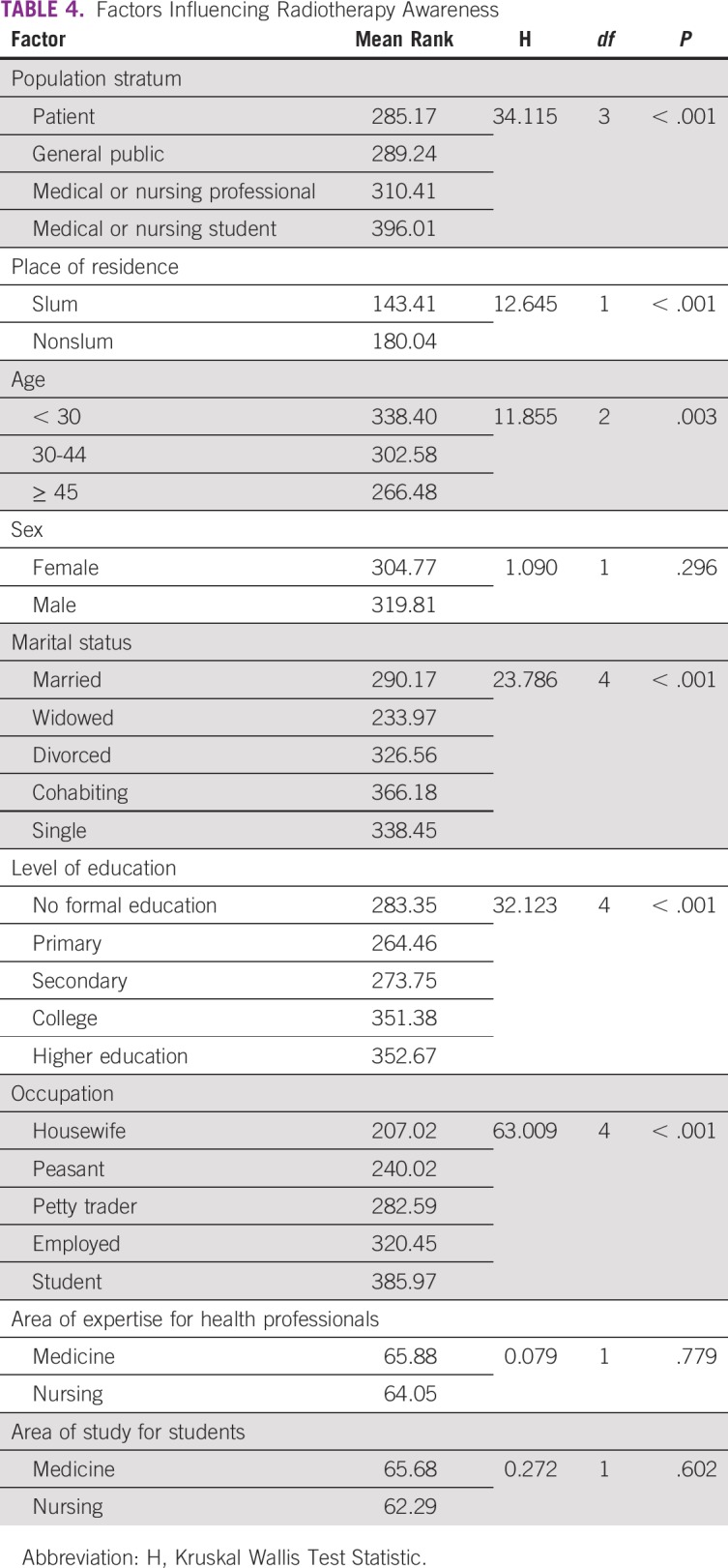
Population stratum.
The Kruskal-Wallis test provided strong evidence of a difference between mean ranks of at least 1 pair of groups in the population stratum (χ23 = 34.115; P < .001). Pairwise comparisons showed evidence of statistically significant differences between patients with cancer and medical/nursing students (P < .001), as well as patients with cancer and the general public (P < .001). The median awareness score was 5.00 for medical/nursing students and 4.00 for both patients with cancer and the general public.
Place of residence.
There was strong evidence for a difference between mean ranks of slum and nonslum areas (χ21 = 12.645; P < .001). The median awareness scores were 3.00 and 5.00 for slum and nonslum areas, respectively.
Age.
The Kruskal-Wallis test provided strong evidence of a difference between mean ranks of at least 1 pair of age groups (χ22 = 12.368; P = .002). There was evidence of a statistically significant difference between the > 45 years of age and < 30 years of age groups. The median awareness scores were 4.00 and 5.00 for > 45 years and < 45 years of age groups, respectively.
Marital status.
There was strong evidence of a difference between mean ranks of at least 1 pair of groups in marital status (χ24 = 23.573; P < .001). Statistically significant differences were found in 3 pairs, which included widowed/single (P = .019), widowed/cohabiting (P = .001), and married/cohabiting (P = .002). The median awareness scores were 4.00 and 5.00 for widowed/cohabiting and widowed/single, respectively.
Level of education.
The Kruskal-Wallis test provided strong evidence of a difference between mean ranks of at least 1 pair of groups in the level of education (χ24 = 31.78; P < .001). Four pairs of groups, including primary/college (P < .001), primary/higher education (P = .001), secondary/college (P = .002), and secondary/higher education (P = .002), showed statistically significant differences. Median scores were 4.00 for primary and secondary, and 5.00 for college and higher education.
Occupation.
There was strong evidence of a difference between mean ranks of at least 1 pair of groups in occupation (χ24 = 62.006; P < .001). There were statistically significant differences between students and petty traders (P < .001), peasants (P < .001), housewives (P < .001), and those employed (P = 0.004). Statistically significant differences were also observed between employed individuals and peasants (P = .043), as well as employed individuals and housewives (P < .001). The median awareness scores were 6.00 for students, 3.00 for housewives, 3.50 for peasants, 4.00 for petty traders, and 5.00 for employed individuals.
Factors Influencing the Perception of RT
The association between perception of RT and sociodemographic characteristics is presented in Table 5.
TABLE 5.
Factors Influencing the Perception of Radiotherapy
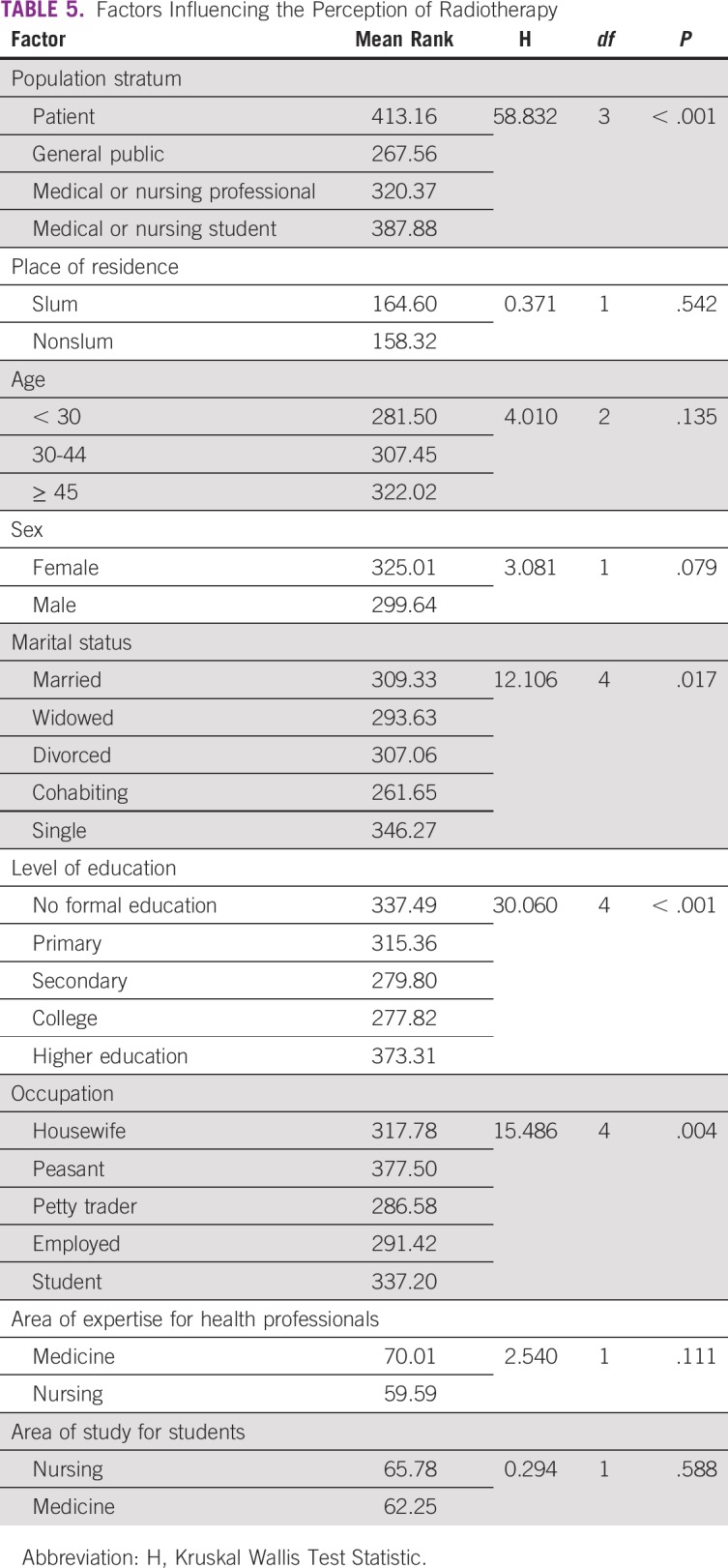
Population stratum.
There was strong evidence of a difference between mean ranks of at least 1 pair of groups in the population stratum (χ23 = 58.322; P < 0.001). There was strong evidence of a difference between the general public and health professionals (P = .034), students (P < .001), and patients with cancer (P < .001). Furthermore, there was evidence of a statistically significant difference in perception scores between health professionals and students (P = .018), as well as health professionals and patients with cancer (P = .010). The median perception scores for the 4 groups were 2.00 for patients with cancer, −1.00 for the general public, 0.00 for health professionals, and 2.00 for students. There was no evidence of a statistically significant difference between the medical/nursing student and patient with cancer pair (P = 1.000).
Level of education.
There was strong evidence of a difference between the mean ranks of at least 1 pair of groups in level of education (χ24 = 30.060; P < 0.001). Pairwise comparisons showed strong evidence of a difference in perception scores in 2 pairs, between secondary and higher education (P < .001) and between college and higher education (P < .001). The median perception scores were −1.00 for secondary as well as college education and 0.00 for higher education. There was no evidence of a statistically significant difference between the other pairs.
Marital status.
There was strong evidence of a difference between mean ranks of at least 1 pair of groups in marital status (χ24 = 12.106; P = .017). There was strong evidence of a statistically significant difference between cohabiting and being single (P = .006). The median perception scores were −2.00 and 0.00 for cohabiting and being single, respectively. There was no evidence of a statistically significant difference between the other pairs.
Occupation.
There was strong evidence of a difference between mean ranks of at least 1 pair of groups in occupation (χ24 = 15.486; P = 0.004). Pairwise comparisons showed statistically significant differences between those employed and peasants (P = .023) and petty traders and peasants (P = .023). Median scores were −1.00 for petty traders and being employed, as well as 1.00 for peasants.
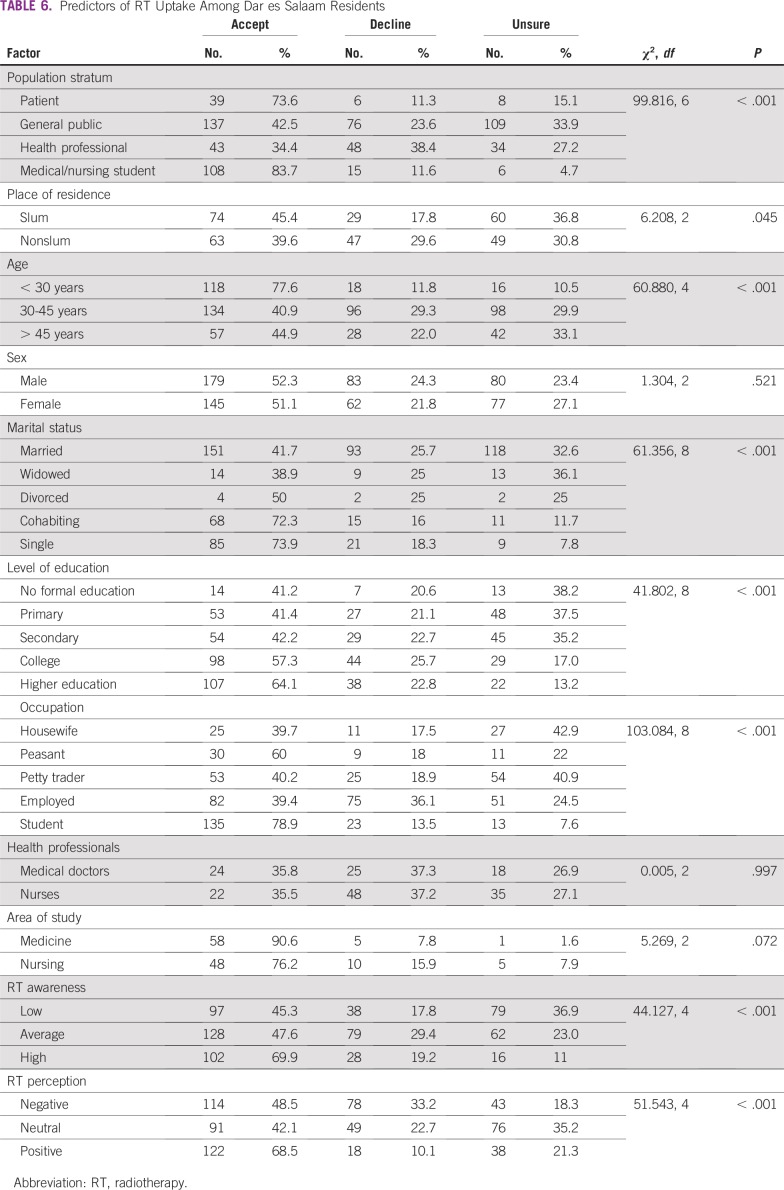
Predictors of the Use of RT
Results showed that 52% of respondents would accept RT, whereas 23.1% would decline it. Statistically significant associations were found between RT uptake and the following factors (Table 6): population stratum (P < .001), place of residence (P < .045), age (P < .001), marital status (P < .001), level of education (P < .001), RT awareness (P < .001), and perceptions of RT (P < .001).
TABLE 6.
Predictors of RT Uptake Among Dar es Salaam Residents
DISCUSSION
Despite the fact that RT continues to be an important modality in cancer management, its public image remains negative.23 This has led to underuse of RT, even in patients in whom it can provide substantial benefit in terms of achieving cure or palliation. This study explored public awareness and perceptions about radiation and RT, which are key issues concerning the use of RT.
We found that the level of RT awareness among respondents was low. The majority of respondents (83.1%) believed that RT would reduce their lifespan, and approximately 60% thought they would become radioactive after RT. More than 60% of respondents were not aware that RT could be used to treat advanced cancer, children, and older patients. The levels of awareness found in this study are consistent with those reported in previous literature.24-26 RT awareness was influenced by population category, place of residence, age, marital status, level of education, and occupation. As previously reported,26 awareness was lower in the general public and patients with cancer compared with other categories of the population.
Furthermore, approximately one third of respondents in this study had negative perceptions about RT, and only approximately one quarter had positive perceptions. Approximately 40% of respondents perceived that RT would cause erectile dysfunction and infertility, whereas approximately 30% believed that RT would cause another cancer. Approximately 31% of respondents perceived that RT would cause early side effects, including skin burns, hair loss, and nausea and vomiting. These results are consistent with those reported by Gillan et al,16 who found that approximately one third of the public had negative perceptions about RT.16 Shaverdian et al24 found that negative perceptions were fueled by concerns about side effects, such as skin burns, hair loss, and nausea and vomiting. Perceptions about RT were most negative in the general public and most positive in patients with cancer and medical/nursing students.
In this study, approximately half of respondents would accept RT if recommended as part of their treatment, whereas nearly a quarter would reject it. The choice of whether to have or not to have RT was found to be influenced by age, education, marital status, awareness, and perception about RT. The proportion of patients with cancer who would accept RT found in this study was consistent with proportions reported in other publications.17,27 However, the proportion of health professionals who would accept RT was surprisingly low. This has wider implications in the use of RT because patients’ choice of either to have or not to have RT is influenced by the recommendation of health professionals.28 Patients may go back to their general practitioners to obtain their opinions on whether to undergo RT or not after consultation with the radiation oncologist; therefore it is important that health professionals have awareness and positive perceptions about RT to help patients make a decision.
RT awareness and perceptions were found to be significant predictors of RT uptake. Nearly 70% of respondents with high awareness would be willing to accept RT, whereas only approximately 45% of respondents with low awareness would be willing to accept it. Low awareness of and negative perceptions about RT may affect its use by fueling concerns such as side effects among referring physicians, patients, and their families.29 Sharma and Malik30 explored perceptions, attitudes, and knowledge of RT among referring physicians and found that 18% of physicians did not refer patients for RT because of concerns about side effects. To bridge this gap, cancer treatment centers should take responsibility to ensure that basic understanding of RT and available infrastructures are present among referring physicians by offering facility visits as well as continuing medical education workshops. Furthermore, concerns about side effects were found to be significant consumer-related barriers to the use of RT in several studies.16,17,19,31-33 The majority of patients with prostate cancer who declined treatment mentioned concerns about side effects, including impotence and incontinence, as the main reasons for their choice.34
A lack of understanding of the potential benefits of treatment as a result of low awareness can have a significant impact on the use of RT. Among black African patients with breast cancer in Cape Town, South Africa, refraining from RT was linked to a belief that RT would scar and cover their tumors, making them inaccessible to traditional medicines.32 These concerns can only be alleviated by efforts to improve RT awareness among the public.
In conclusion, public awareness toward RT in Dar es Salaam is not only low, but negative perceptions also prevail. Low levels of awareness and negative perceptions are significant barriers to the use of RT. To realize the benefits of investment in RT infrastructures in Tanzania as stipulated in the national cancer control strategy, public education on RT should be provided to improve awareness and perceptions about it to increase its uptake.
Footnotes
Supported by the Ocean Road Cancer Institute through the Academics, Research, and Publications Unit.
AUTHOR CONTRIBUTIONS
Conception and design: All authors
Financial support: Anthony B. Burambo
Administrative support: Anthony B. Burambo
Provision of study materials or patients: Anthony B. Burambo
Collection and assembly of data: Geofrey F. Soko, Anthony B. Burambo, Mpanda M. Mngoya
Data analysis and interpretation: Geofrey F. Soko, Anthony B. Burambo
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jgo/site/misc/authors.html.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
No potential conflicts of interest were reported.
REFERENCES
- 1.Delaney G, Jacob S, Featherstone C, et al. The role of radiotherapy in cancer treatment: Estimating optimal utilization from a review of evidence-based clinical guidelines. Cancer. 2005;104:1129–1137. doi: 10.1002/cncr.21324. [DOI] [PubMed] [Google Scholar]
- 2.Hortobagyi GN, El-Saghir NS, Cufer T, et al. The American Society of Clinical Oncology’s efforts to support global cancer medicine. J Clin Oncol. 2016;34:76–82. doi: 10.1200/JCO.2015.61.7696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ringborg U, Bergqvist D, Brorsson B, et al. The Swedish Council on Technology Assessment in Health Care (SBU) systematic overview of radiotherapy for cancer including a prospective survey of radiotherapy practice in Sweden 2001—summary and conclusions. Acta Oncol. 2003;42:357–365. doi: 10.1080/02841860310010826. [DOI] [PubMed] [Google Scholar]
- 4.Rosenblatt E, Barton M, Mackillop W, et al. Optimal radiotherapy utilisation rate in developing countries: An IAEA study. Radiother Oncol. 2015;116:35–37. doi: 10.1016/j.radonc.2015.06.012. [DOI] [PubMed] [Google Scholar]
- 5.Borras JM, Lievens Y, Dunscombe P, et al. The optimal utilization proportion of external beam radiotherapy in European countries: An ESTRO-HERO analysis. Radiother Oncol. 2015;116:38–44. doi: 10.1016/j.radonc.2015.04.018. [DOI] [PubMed] [Google Scholar]
- 6.Rosenblatt E, Fidarova E, Zubizarreta EH, et al. Radiotherapy utilization in developing countries: An IAEA study. Radiother Oncol. 2018;128:400–405. doi: 10.1016/j.radonc.2018.05.014. [DOI] [PubMed] [Google Scholar]
- 7. Reference deleted.
- 8.Abdel-Wahab M, Bourque JM, Pynda Y, et al. Status of radiotherapy resources in Africa: An International Atomic Energy Agency analysis. Lancet Oncol. 2013;14:e168–e175. doi: 10.1016/S1470-2045(12)70532-6. [DOI] [PubMed] [Google Scholar]
- 9.Datta NR, Samiei M, Bodis S. Radiation therapy infrastructure and human resources in low- and middle-income countries: Present status and projections for 2020. Int J Radiat Oncol Biol Phys. 2014;89:448–457. doi: 10.1016/j.ijrobp.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 10.Grover S, Xu MJ, Yeager A, et al. A systematic review of radiotherapy capacity in low- and middle-income countries. Front Oncol. 2015;4:380. doi: 10.3389/fonc.2014.00380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Atun R, Jaffray DA, Barton MB, et al. Expanding global access to radiotherapy. Lancet Oncol. 2015;16:1153–1186. doi: 10.1016/S1470-2045(15)00222-3. [DOI] [PubMed] [Google Scholar]
- 12.Sundaresan P, Stockler MR, Milross CG. What is access to radiation therapy? A conceptual framework and review of influencing factors. Aust Health Rev. 2016;40:11–18. doi: 10.1071/AH14262. [DOI] [PubMed] [Google Scholar]
- 13.Citrin DL, Bloom DL, Grutsch JF, et al. Beliefs and perceptions of women with newly diagnosed breast cancer who refused conventional treatment in favor of alternative therapies. Oncologist. 2012;17:607–612. doi: 10.1634/theoncologist.2011-0468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deng G, Cassileth B. Complementary or alternative medicine in cancer care-myths and realities. Nat Rev Clin Oncol. 2013;10:656–664. doi: 10.1038/nrclinonc.2013.125. [DOI] [PubMed] [Google Scholar]
- 15. James S: A guide to modern radiotherapy. London, United Kingdom, Society and College of Radiographers, 2013. [Google Scholar]
- 16.Gillan C, Abrams D, Harnett N, et al. Fears and misperceptions of radiation therapy: Sources and impact on decision-making and anxiety. J Cancer Educ. 2014;29:289–295. doi: 10.1007/s13187-013-0598-2. [DOI] [PubMed] [Google Scholar]
- 17.Sundaresan P, King M, Stockler M, et al. Barriers to radiotherapy utilization: Consumer perceptions of issues influencing radiotherapy-related decisions. Asia Pac J Clin Oncol. 2017;13:e489–e496. doi: 10.1111/ajco.12579. [DOI] [PubMed] [Google Scholar]
- 18.Avery S, Kenton O, bin Dachi J, et al. Radiation oncology solutions in Tanzania. Int J Radiat Oncol Biol Phys. 2015;93:961–962. doi: 10.1016/j.ijrobp.2015.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. The Foundation for Cancer Care in Tanzania: Meeting the challenge of cancer care in northern Tanzania. https://s3-eu-west-1.amazonaws.com/s3.sourceafrica.net/documents/117849/FCCT-White-Paper-V4-1-Compressed.pdf.
- 20. United Republic of Tanzania, Ministry of Health and Social Welfare: National cancer control strategy (2013-2022). https://www.iccp-portal.org/system/files/plans/NCSS%20Book.pdf.
- 21.NBS . Tanzania total population by district - regions -2016-2017. National Bureau of Statistics; 2018. http://www.nbs.go.tz/nbstz/index.php/english/statistics-by-subject/population-and-housing-census/844-tanzania-total-population-by-district-regions-2016. [Google Scholar]
- 22.NBS . Migration and urbanization report. The United Republic of Tanzania; 2015. https://www.nbs.go.tz/nbs/takwimu/census2012/Migration_and_Urbanisation_Monograph.pdf. [Google Scholar]
- 23.Watts G. Radiotherapy in UK is feared and underused. BMJ. 2011;342:d616. doi: 10.1136/bmj.d616. [DOI] [PubMed] [Google Scholar]
- 24.Shaverdian N, Wang X, Hegde J V., et al. The patient’s perspective on breast radiotherapy: Initial fears and expectations versus reality. Cancer. 2018;124:1673–1681. doi: 10.1002/cncr.31159. [DOI] [PubMed] [Google Scholar]
- 25.Hammick M, Tutt A, Tait DM. Knowledge and perception regarding radiotherapy and radiation in patients receiving radiotherapy: A qualitative study. Eur J Cancer Care (Engl) 1998;7:103–112. doi: 10.1046/j.1365-2354.1998.00072.x. [DOI] [PubMed] [Google Scholar]
- 26.Lawler G. Knowledge and awareness of radiation therapy in the general Irish population and a population of health professionals. Radiother Oncol. 2012;92:S157. [Google Scholar]
- 27.O’Connell RL, Mohammed K, Gui GPH, et al. A case-control study of treatment choices made by doctors diagnosed with early breast cancer. Int J Surg. 2015;17:19–23. doi: 10.1016/j.ijsu.2015.02.014. [DOI] [PubMed] [Google Scholar]
- 28.Sundaresan P, Milross CG, Smith A, et al. Factors influencing the use of RT in NSW: A qualitative study exploring consumer and health professional perspectives. J Med Imaging Radiat Oncol. 2014;58:625–632. doi: 10.1111/1754-9485.12198. [DOI] [PubMed] [Google Scholar]
- 29.Maliti BK. Management of retinoblastoma in Zambia. Asia Pac J Oncol Nurs. 2017;4:184–186. doi: 10.4103/apjon.apjon_24_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sharma K, Malik A. Perception, attitude and knowledge regarding radiotherapy among physicians at a tertiary care center. J Curr Oncol. 2019;2:6. [Google Scholar]
- 31.Haileselassie W, Mulugeta T, Tigeneh W, et al. The situation of cancer treatment in Ethiopia: Challenges and opportunities. J Cancer Prev. 2019;24:33–42. doi: 10.15430/JCP.2019.24.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wright SV. An investigation into the causes of absconding among black African breast cancer patients. S Afr Med J. 1997;87:1540–1543. [PubMed] [Google Scholar]
- 33.Livergant J, Howard M, Klein J. Barriers to referral for palliative radiotherapy by physicians: A systematic review. Clin Oncol (R Coll Radiol) 2019;31:e75–e84. doi: 10.1016/j.clon.2018.09.009. [DOI] [PubMed] [Google Scholar]
- 34.White MA, Verhoef MJ. Decision-making control: Why men decline treatment for prostate cancer. Integr Cancer Ther. 2003;2:217–224. doi: 10.1177/1534735403256411. [DOI] [PubMed] [Google Scholar]