The economic burden of preeclampsia is significant, with the main cost drivers being infant health care costs associated with preterm birth.
Abstract
OBJECTIVE:
To provide U.S. case-based preeclampsia health care cost estimates for mothers and infants from a U.S. payer perspective, with comparisons with both uncomplicated and hypertensive pregnancies.
METHODS:
Electronic health record and billing data from a large regional integrated health care system in Pennsylvania were used to identify mother–singleton infant pairs with deliveries between 2010 and 2015. Data on clinical care and costs using actual payment amounts were compiled from 20 weeks of gestation to 6 weeks postdelivery for mothers and birth to 12 months for infants. Three defined pregnancy study cohorts, uncomplicated, hypertension and preeclampsia, were matched using a 1:1:1 ratio on the basis of maternal age, parity, body mass index, and comorbidities. Costs per pregnancy were calculated in 2015 dollars and preeclampsia incremental costs estimated by subtracting the average cost of the matched cohorts.
RESULTS:
The final study population included 712 matched mother–infant pairs in each cohort. The mean combined maternal and infant medical care costs in the preeclampsia cohort of $41,790 were significantly higher than those for the uncomplicated cohort of $13,187 (P<.001) and hypertension cohort of $24,182 (P<.001), and were largely driven by differences in the infant costs. The mean infant cost in the preeclampsia cohort were $28,898, in the uncomplicated cohort $3,669 and $12,648 in the hypertension cohort (P<.001). Mothers with preeclampsia delivered 3 weeks earlier (median 36.5 weeks of gestation) than women in the uncomplicated cohort and more than 2 weeks earlier than women in the hypertension cohort. A significantly larger percentage of women with preeclampsia and their infants experienced adverse events (13.9% for mothers and 14.6% for infants) compared with unaffected women (4.1% and 0.7%) and those with hypertension (9.4% and 4.8%), respectively (P<.001).
CONCLUSION:
The economic burden of preeclampsia health care is significant with the main cost drivers being infant health care costs associated with lower gestational age at birth and greater adverse outcomes.
FUNDING SOURCE:
This study is funded by Progenity, Inc.
Preeclampsia, which occurs in 2–8% of pregnancies, is one of the leading causes of prematurity,1–3 maternal and neonatal morbidity and mortality.4 The rate of preeclampsia and eclampsia in the United States has been increased by an estimated 21% from 2005 to 2014, consistent with increases in preeclampsia risk factors of obesity, maternal age and diabetes.5 The only consensus treatment is delivery, regardless of the gestational age.3,4 Development of preeclampsia (before 37 weeks of gestation) often results in preterm birth, which plays a primary role in perinatal morbidity and mortality6; thus, the extra days and weeks of gestational age are critical for infant health outcomes.
To date, there has been limited comprehensive evaluation of the economic burden of preeclampsia. Therefore, the objective of this study is to provide U.S. case-based preeclampsia maternal and infant medical care cost estimates compared with uncomplicated pregnancies and pregnancies in women with hypertension (but not preeclampsia) from a payer perspective using primary case data.
ROLE OF THE FUNDING SOURCE
The study was funded by Progenity, Inc. A contract was executed between Progenity, Inc. and Geisinger in the form of milestone payments for agreed on study activities. Payments made to Geisinger covered the salary of Geisinger research investigators and staff who are part of the research team of this study as well as indirect costs. Funding was also used to reimburse the 2018 International Society for Pharmacoeconomics and Outcomes Research conference expenses where the lead author presented preliminary findings of this study. Lastly, funding will be used to cover potential manuscript publication fees. The report and manuscript of this study and the study design have been reviewed and approved by Progenity, Inc. and they approved the decision to submit the article for publication, however they were not involved in the study design development and implementation, or the collection, analysis and interpretation of the data. I affirm that this manuscript is an honest, accurate, and transparent account of the study being reported.
The authors had access to relevant aggregated study data and other information (such as study protocol, analytic plan and report, validated data table, and clinical study report) required to understand and report research findings. The authors take responsibility for the presentation and publication of the research findings, have been fully involved at all stages of publication and presentation development, and are willing to take public responsibility for all aspects of the work. All individuals included as authors and contributors who made substantial intellectual contributions to the research, data analysis, and publication or presentation development are listed appropriately. The role of the sponsor in the design, execution, analysis, reporting, and funding is fully disclosed. The authors' personal interests, financial or nonfinancial, relating to this research and its publication have been disclosed.
METHODS
The study was conducted using data from retrospectively identified women who delivered at Geisinger Health System, an integrated delivery system in central and northeastern Pennsylvania. The data sources used included the health system's electronic health record and billing data for payment amounts received and payer information. The initial study inclusion criteria were all mother and infant pairs from singleton pregnancies at 20 weeks of gestation or greater starting January 1, 2010, with delivery dates on or before December 31, 2015. Mother–infant pairs were classified into three pregnancy cohorts: women with uncomplicated pregnancies, which was restricted to full-term pregnancies with no complications; women with hypertension; and women with preeclampsia. The approach used to define the three pregnancy cohorts was based on an unpublished study design by Phibbs and others (Appendix 1, available online at http://links.lww.com/AOG/B635).
Before development of the three pregnancy cohorts, exclusion criteria were applied based on the availability of the mother's weight and height to calculate maternal prepregnancy body mass index (BMI, calculated as weight in kilograms divided by height in meters squared) estimates (Appendix 2, available online at http://links.lww.com/AOG/B635). Patients with prepregnancy weight less than 80 pounds were excluded owing to possible data entry error. Additional inclusion and exclusion criteria arising from data validation processes were applied to all three cohorts by analyzing the distribution of costs and reviewing allowed amounts from Geisinger Health Plan claims data (Appendix 3, available online at http://links.lww.com/AOG/B635). Pregnancies were excluded if the mother's delivery encounter cost was less than $1,200 or greater than $30,000, or the infant's first hospitalization event cost was less than $100/day or greater than $1,000,000 in total. These cost exclusion criteria are consistent with earlier peer-reviewed published studies.7,8 Further, pregnancies were included only if there was a delivery encounter in both the mother and child encounter files. Also, if a mother had more than one pregnancy eligible for inclusion, only the first pregnancy was included. Finally, based on the results of a chart review of a sample of selected cases, pregnancies for which the initial diagnosis of preeclampsia or hypertension originated in the Emergency Department were excluded as they were consistently less accurately coded. We obtained Geisinger Institutional Review Board approval for this study.
We used a matched control cost-of-illness methodology9 to estimate the direct health care cost burden of preeclampsia. Three study cohorts were matched using a 1:1:1 ratio based on maternal age (younger than 20 years, 20–34 years, 35 years or older), parity, obesity status (BMI less than 30 or 30 or higher), and the mean of the Charlson Comorbidity Index scores. Age, parity and obesity are risk factors for preeclampsia and are associated with health care costs in pregnancy independent of developing preeclampsia.10,11 The Charlson Index Scores account for the patients' general comorbid conditions that are associated with costs not relevant to preeclampsia.
The study analytic horizon was from 20 weeks of gestation to 6 weeks postpartum for the mother and 12 months postdelivery for the infant. All maternal and infant costs per pregnancy were estimated using 2015 U.S. dollars. The differences between the mean maternal and infant costs in the preeclampsia cohort and the uncomplicated and hypertension cohorts were calculated to estimate the incremental cost of preeclampsia compared with uncomplicated pregnancies and women with hypertension, respectively. Pregnancy cases were also stratified by week of gestational age at birth and by payer (commercial, Medicaid, and other) to estimate and compare costs among the three cohorts. Besides costs, birth-related outcomes including gestational age at delivery, the frequency of adverse maternal outcomes during pregnancy and adverse infant outcomes of higher prevalence were reported using corresponding International Classification of Diseases, 9th Revision codes identified in a recently published preeclampsia cost study12 (Appendix 4, available online at http://links.lww.com/AOG/B635). Maternal adverse events in our analysis were limited to renal failure, eclamptic seizure, thrombocytopenia, and severe intrapartum and postpartum hemorrhage. The infant adverse events included delivery for fetal distress, respiratory distress syndrome, bronchopulmonary dysplasia, retinopathy of prematurity (stage greater than 3), necrotizing enterocolitis, Bell's (grade greater than 2), intraventricular hemorrhage (stage greater than 3), and sepsis. Finally, we compared delivery event length of stay (LOS) for both the mother and infant.
Costs for each of the three cohorts were compared using a generalized linear regression model with a log-link function and gamma distribution. Frequencies of cesarean delivery and adverse events were summarized and compared using χ2 tests, and the mean gestational age at delivery and LOS were compared using analyses of variance. Owing to small sample size, only descriptive statistics in subgroups stratified by gestational week were presented; inferential statistics to compare statistically significant differences among cohorts were only conducted on the 3 cohorts at the overall level.
RESULTS
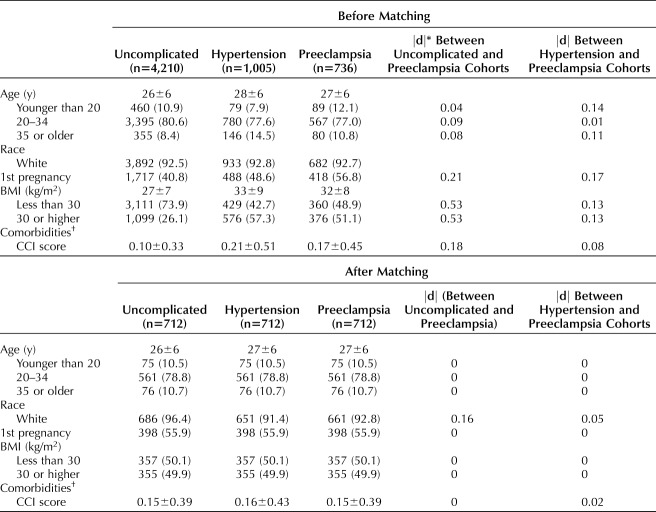
The initial study population included 16,545 mother–infant pairs. After applying all inclusion and exclusion criteria, the uncomplicated, hypertension, and preeclampsia cohorts were comprised of 4,210, 1,005, and 736 mother–infant pairs, respectively, before matching (Appendix 3, http://links.lww.com/AOG/B635), and the final study population contained 712 mother–infant pairs in each of the three cohorts after a 1:1:1 match. Overall before matching, the hypertension and preeclampsia cohorts had higher proportions of women aged 35 and over, obese women and first pregnancies, as well as a higher comorbidity index scores compared with the uncomplicated cohort. The results after matching demonstrate the elimination of heterogeneity for these characteristics across the three cohorts (Table 1).
Table 1.
Study Population Patient Characteristics Before and After Matching
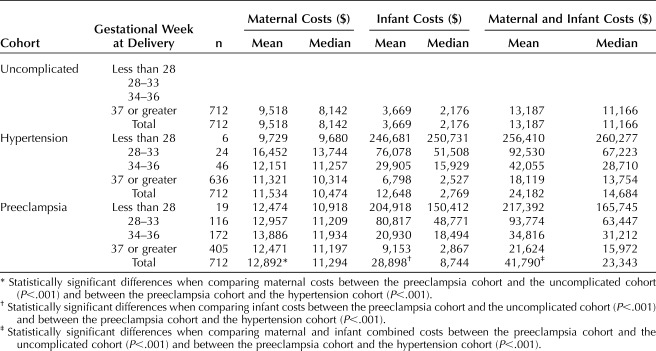
The mean combined maternal and infant medical care costs in the preeclampsia cohort of $41,790 were significantly higher than those for the uncomplicated cohort of $13,187 (P<.001) and hypertension cohort of $24,182 (P<.001) and were largely driven by differences in the infant costs (Appendix 5, available online at http://links.lww.com/AOG/B635). The mean infant cost in the preeclampsia cohort of $28,898 was almost 8 times greater than those for the uncomplicated cohort of $3,669 (P<.001) and more than double the mean infant cost for the hypertension cohort of $12,648 (P<.001) (Appendix 5, http://links.lww.com/AOG/B635).
The estimated total incremental costs of preeclampsia were $28,603 ($3,374 for mothers and $25,229 for infants) compared with the uncomplicated cohort and $17,608 ($1,358 for mothers and $16,250 for infants) compared with the hypertension cohort.
The mean cost per infant was dependent on gestational age, ranging from a mean of $214,941 at less than 28 weeks of gestation to $6,071 at full term of 37 or more weeks of gestation. Average maternal costs by gestational week at delivery were generally stable and did not exhibit an increasing or decreasing trend with gestational age in each of the three cohorts (Table 2, Appendix 6, available online at http://links.lww.com/AOG/B635). Commercial payments were substantially higher than Medicaid by about 2:1 overall (Appendix 7, available online at http://links.lww.com/AOG/B635).
Table 2.
Maternal, Infant, and Maternal and Infant Costs by Cohort and Gestational Week at Delivery (2015 U.S. Dollars)
Women with preeclampsia delivered at 36.5 gestational weeks on average, 3 weeks (95% CI 2.7–3.3) earlier than mothers with uncomplicated pregnancies, averaging 39.5 weeks of gestation, and slightly more than 2 weeks (1.9–2.5) earlier than mothers with hypertension, averaging 38.7 weeks of gestation. Women in the preeclampsia cohort had higher rates of cesarean delivery at 50.0% compared with 29.6% and 38.3% in the uncomplicated and hypertension cohorts, respectively, and greater rates of maternal adverse events. Infants in the preeclampsia cohort had higher rates of adverse events compared with the uncomplicated and hypertension cohorts with statistically significant differences (Appendix 8, available online at http://links.lww.com/AOG/B635). There was not a statistically significant difference between infant death rates in the uncomplicated (0.3%), hypertension (0.8%), and preeclampsia (0.7%) cohorts, which each had six or fewer observations.
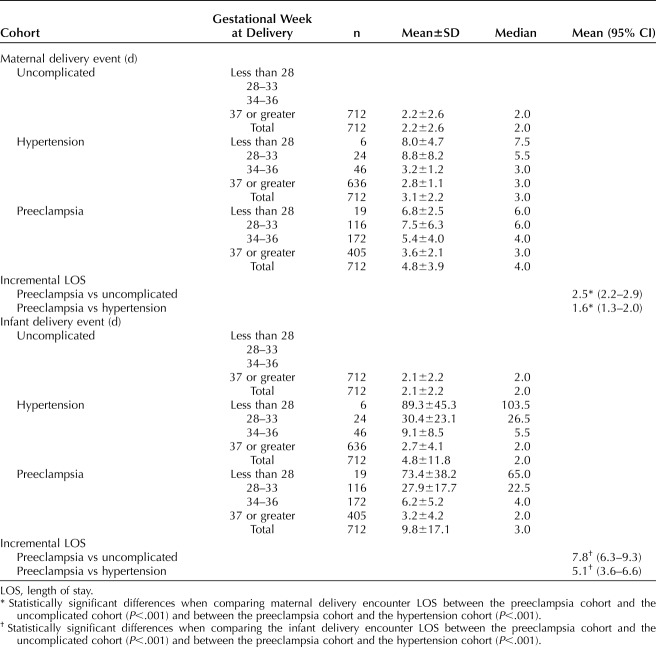
The mean LOS for mothers in the preeclampsia cohort was 4.8 days, which was, on average, 2.5 (2.2–2.9) days longer than women in the uncomplicated cohort (2.2 days) and 1.6 (1.3–2.0) days longer than women in the hypertension cohort (3.1 days). The average LOS for infants in the preeclampsia cohort was 9.8 days compared with 2.1 days for infants in the uncomplicated cohort (ie, 7.8, 6.3–9.3 days longer) and 4.8 days for hypertension cohort (ie, 5.1, 3.6–6.6 days longer) (Table 3).
Table 3.
Maternal and Infant Delivery Event Length of Stay by Cohort and Gestational Week at Delivery
DISCUSSION
The study shows that preeclampsia was associated with total estimated mean incremental costs of $28,603 per mother–infant pair compared with uncomplicated full-term pregnancies, and $17,608 compared with the pregnant women with hypertension (but not preeclampsia). Preeclampsia was also associated with lower gestational age at birth by approximately 3 weeks compared with mothers with uncomplicated pregnancies and 2.2 weeks for mothers with hypertension. The primary drivers of the incremental costs were high infant costs associated with preterm delivery and other infant adverse events. Women with preeclampsia had higher rates of cesarean delivery and maternal adverse events.
To date, Stevens et al12 is the only other study that comprehensively evaluated the medical care costs associated with preeclampsia for both mothers and infants (based on a PubMed search from January 1, 1990–August 31, 2019; English language; humans; title/abstract search terms: “preeclampsia” or “pre-eclampsia” and “cost”). Our total combined 2015 maternal and infant costs per preeclampsia birth of $43,009 were consistent with Stevens et al's 2012 cost, CPI-adjusted to 2015 U.S. dollars (multiplied by 1.0813) of $44,196. However, our maternal and infant cost estimates differed substantially with infants being the primary drivers of total incremental costs of preeclampsia. Specially, our incremental infant costs of $25,229 and $16,250 compared with uncomplicated pregnancies and pregnant women with hypertension, respectively, were 2–3 times higher than $7,938 (2015 U.S. dollars) compared with nonpreeclamptic pregnancies; our maternal cost estimates were substantially lower, at $3,374 and $1,358, less than one half to one fifth of $7,110 (2015 U.S. dollars). Another difference is that our maternal cost estimates did not show a decreasing trend with increased gestational age at delivery.
These cost-related differences are consistent with key differences in study methods, including our use of important variables associated with higher risk pregnancies and potential confounders of preeclampsia by matching cohorts compared with regression models; a maternal observation period starting point of 20 weeks of gestation,14 compared with 6 months before delivery12; a maternal observation period ending point based on the American College of Obstetricians and Gynecologists’ recommendation for a comprehensive postpartum visit within the first 6 weeks after birth,14 compared with 12 months postdelivery. As a result, our study's maternal cost estimates minimized the possibility of capturing costs unrelated to preeclampsia. In addition, we included two comparison cohorts: uncomplicated pregnancies, restricted to full-term delivery with no complications as an upper bound comparison, and pregnant women with hypertension as a lower bound, compared with all nonpreeclamptic pregnancies.12 Finally, we directly measured infant and maternal medical care costs using actual payment data independent of gestational age compared with imputed medical costs based on gestational week and adverse outcomes.
This study is the first cost-of-illness analysis of preeclampsia using primary data to provide directly observable U.S. case-based health care cost estimates for both mothers and infants from a payer perspective as a recent search revealed no other cases. The use of comprehensive electronic health record information allowed linking of mother infant-pairs to develop and match cohorts on key confounding variables, including age, parity, comorbidities and BMI based on actual weight and height information as opposed to self-reported prepregnancy weight, which is less accurate. The ability to link comprehensive billing and clinical data to capture actual costs is another important strength of our study, compared with imputed cost estimates based on secondary analysis of multiple data sets or cost-to-charge ratios to develop case-based estimates.
Our study addresses the limitation noted in the Stevens et al study,12 which did not incorporate a direct effect of preeclampsia on infant costs independent of gestational age, by using an actual matched study population including a diagnosed preeclampsia cohort and direct measurement of gestational age and medical care utilization and costs.
Limitations of our study include that the study population and data sources were from a single large integrated health system that had a modest sample size and may not be nationally representative, which limits subgroup analysis (eg, by geography or race) that could be of further interest to public health decisionmakers.9 The study's payer perspective limits the estimate of the preeclampsia cost burden to direct medical care costs compared with a comprehensive societal perspective, which would include additional cost components (direct nonmedical and indirect costs) and a longer time horizon when appropriate, especially for infant adverse outcomes. There is also the possibility that the medical cost estimates do not reflect all services as the data sources do not capture medical care services provided outside the single integrated health care system. In addition, we observed a lower percentage of Medicaid as the payer in the preeclampsia cohort; this may have contributed to increasing the estimated cost differences, because payments from Medicaid are lower those than from commercial insurers.
Preeclampsia cost of illness studies such as ours increase understanding of the substantial health and economic burden of preeclampsia and may provide useful information to health decision and policy makers.
Footnotes
This study is funded by Progenity, Inc.
Financial Disclosure Matthew Cooper is Chief Scientific Officer at Progenity, Inc., a biotechnology company conducting preeclampsia related research and development. He is also on the Board of Directors of the Preeclampsia Foundation, a patient advocacy group focused on hypertensive disorders of pregnancy. Jove Graham disclosed that money was paid to their institution by the Patient Centered Outcomes Research Institute, PA Department of Health, and Purdue Pharma. They received grant monies paid to their institution by Genentech Inc. (past), Medtronic Inc. (past), and Johnson & Johnson (past). Matthew Cooper disclosed that he is a paid employee of Progenity, who is currently working on a diagnostic product for preeclampsia. Susan R. Snyder disclosed that Progenity, Inc. and Geisinger had a research contract under which Progenity made payments for this research, which were primarily to cover expenses for the time and efforts of Geisinger employees. She was a salaried employee of Geisinger during the 36 months prior to submission. The other authors did not report any potential conflicts of interest.
Presented as a poster at the International Society of Pharmacoeconomics and Outcome Research's 23rd Annual International Meeting, May 19–23, 2018, Baltimore, Maryland; the AcademyHealth 2018 Annual Research Meeting, June 24–26, 2018, Seattle, Washington; and the Society for Maternal-Fetal Medicine’s 39th Annual Pregnancy Meeting, February 11–16, 2019, Las Vegas, Nevada.
The authors thank Drs. Ciaran Phibbs and Susan Schmitt from Stanford University for sharing criteria and ICD-9 codes for defining the three pregnancy study cohorts.
Peer reviews and author correspondence are available at http://links.lww.com/AOG/B636.
REFERENCES
- 1.Ananth CV, Keyes KM, Wapner RJ. Pre-eclampsia rates in the United States, 1980–2010: age-period-cohort analysis. BMJ 2013;347:f6564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.English FA, Kenny LC, McCarthy FP. Risk factors and effective management of preeclampsia. Integr Blood Press Control 2015;8:7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shih T, Peneva D, Xu X, Sutton A, Triche E, Ehrenkranz RA, et al. The rising burden of preeclampsia in the United States impacts both maternal and child health. Am J Perinatology 2016;33:329–38. [DOI] [PubMed] [Google Scholar]
- 4.Gestational hypertension and preeclampsia. ACOG Practice Bulletin No. 202. American College of Obstetricians and Gynecologists. Obstet Gynecol 2019;133:e1–25.30575675 [Google Scholar]
- 5.Fingar KR, Mabry-Hernandez I, Ngo-Metzger Q, Wolff T, Steiner CA, Elixhauser A. Delivery hospitalizations involving preeclampsia and eclampsia, 2005–2014. Available at: https://hcup-us.ahrq.gov/reports/statbriefs/sb222-Preeclampsia-Eclampsia-Delivery-Trends.jsp. Retrieved September 6, 2019. [PubMed] [Google Scholar]
- 6.Backes CH, Markham K, Moorehead P, Cordero L, Nankervis CA, Giannone PJ. Maternal preeclampsia and neonatal outcomes. J Pregnancy 2011;2011:214365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Russell RB, Green NS, Steiner CA, Meikle S, Howse JL, Poschman K, et al. Cost of hospitalization for preterm and low birth weight infants in the United States. Pediatrics 2007;120:e1–9. [DOI] [PubMed] [Google Scholar]
- 8.Phibbs CS, Schmitt SK. Estimates of the cost and length of stay changes that can be attributed to one-week increases in gestational age for premature infants. Early Hum Dev 2006;82:85–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Onukwugha E, McRae J, Kravetz A, Varga S, Khairnar R, Mullins CD. Cost-of-illness studies: an updated review of current methods. Pharmacoeconomics 2016;34:43–58. [DOI] [PubMed] [Google Scholar]
- 10.Wallis AB, Saftlas AF, Hsia J, Atrash HK. Secular trends in the rates of preeclampsia, eclampsia, and gestational hypertension, United States, 1987–2004. Am J Hypertens 2008;21:521–6. [DOI] [PubMed] [Google Scholar]
- 11.Duckitt K, Harrington D. Risk factors for pre-eclampsia at antenatal booking: systematic review of controlled studies. BMJ 2005;330:565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stevens W, Shih T, Incerti D, Ton TGN, Lee HC, Peneva D, et al. Short-term costs of preeclampsia to the United States health care system. Am J Obstet Gynecol 2017;217:237–48.e16. [DOI] [PubMed] [Google Scholar]
- 13.Bureau of Labor Statistics. CPI for all urban consumers 2019. Available at: https://data.bls.gov/timeseries/CUUR0000SAM?output_view=pct_12mths. Retrieved March 15, 2019. [Google Scholar]
- 14.Optimizing postpartum care. ACOG Committee Opinion No. 736. American College of Obstetricians and Gynecologists. Obstetrics Gynecol 2018;131:e140–50. [DOI] [PubMed] [Google Scholar]