Abstract
Background
Poor patient experience, including long waiting time, is a potential reason for low healthcare utilisation. In this study, we evaluate the impact of appointment scheduling on waiting time and utilisation of antenatal care.
Methods
We implemented a pilot study in Mozambique introducing appointment scheduling to three maternity clinics, with a fourth facility used as a comparison. The intervention provided women with a return date and time for their next antenatal care visit. Waiting times and antenatal care utilisation data were collected in all study facilities. We assessed the effect of changing from first come, first served to scheduled antenatal care visits on waiting time and complete antenatal care (≥4 visits during pregnancy). Our primary analysis compared treatment facilities over time; in addition, we compared the treatment and comparison facilities using difference in differences.
Results
We collected waiting time data for antenatal care from 6918 women, and antenatal care attendance over the course of pregnancy from 8385 women. Scheduling appointments reduced waiting time for antenatal care in treatment facilities by 100 min (95% CI −107.2 to -92.9) compared with baseline. Using administrative records, we found that exposure to the scheduling intervention during pregnancy was associated with an approximately 16 percentage point increase in receipt of four or more antenatal care visits during pregnancy.
Conclusions
Relatively simple improvements in the organisation of care that reduce waiting time may increase utilisation of healthcare during pregnancy. A larger scale study is needed to provide information about whether appointment scheduling can be sustained over time.
Trial registration number
Keywords: quality of care, antenatal care, maternal health, health systems, health policy
Key questions.
What is already known?
Long waiting time for care is a commonly reported problem in public health facilities in sub-Saharan Africa, and may reduce utilisation of healthcare.
This study is the first to evaluate the effect of an appointment scheduling intervention on both waiting time and completion of recommended care.
What are the new findings?
Appointment scheduling decreased waiting time for antenatal care by over 1 hour (100 min), and increased the per cent of women who completed four or more antenatal care visits during pregnancy.
What do the new findings imply?
Relatively simple improvements in the organisation of care that reduce waiting time may increase utilisation of healthcare during pregnancy.
Background
Antenatal care (ANC) represents a critical introduction to the continuum of maternal and newborn healthcare.1 High-quality ANC informs women about potential danger signs during pregnancy and provides treatment and prevention for illnesses that adversely affect infant health. With adequate ANC coverage, an estimated 283 000 lives could be saved annually.2 WHO guidelines published in 2002 recommended that women receive at least four ANC visits during pregnancy. In Mozambique, only 55% of pregnant women receive complete ANC (four visits over the course of their pregnancy), and only 13% of women start ANC in the first trimester of pregnancy.3 4 In 2016, new WHO guidelines recommending that women attend at least eight ANC visits during pregnancy replaced the earlier recommendation.5 In 2015 in Mozambique, only 3% of women obtained eight or more visits. Meeting these new coverage targets will require a better understanding of barriers to utilisation and the effectiveness of interventions to address these barriers.
It is increasingly recognised that high-quality healthcare, in addition to improved coverage of maternal and child health services, is necessary to achieve the Sustainable Development Goal’s target reductions in maternal and child mortality.6 The ongoing ‘quality revolution’7 in global health emphasises the need for successful health systems to deliver on various dimensions of quality, including providing patient-centred care, or care that is responsive to the preferences of users.8
Abundant evidence has shown that public clinics in sub-Saharan Africa are not organised around the preferences of patients9–15 in particular with respect to the amount of time spent waiting at facilities.16 In Mozambique, attending ANC typically involves arriving early in the morning only to spend most of the day waiting for care. Previous studies have shown that waiting time for ANC is perceived as a significant barrier to seeking care and is associated with decreased satisfaction with ANC.17–19 Long queues and the resulting crowded facilities may also decrease technical quality if health workers rush through key procedures.
Recent evidence demonstrates that comprehensively improving technical and non-technical quality can influence choice of delivery location.20 Furthermore, non-technical quality care (including patient responsiveness) has been shown to influence utilisation decisions.21 However, more evidence is needed to understand whether improving patient experience alone can drive changes in utilisation of care. We partnered with the Ministry of Health in Mozambique to conduct a pilot study of a scheduling intervention in three high-volume public health clinics in Mozambique with a fourth high-volume facility serving as a comparison. We examine the relationship between the introduction of the scheduling system and changes in waiting time and utilisation of ANC. We also examine the effect of the scheduling system on the quality of ANC, the study’s secondary outcome. While one previous study demonstrated that scheduling systems can reduce waiting times even in contexts of limited state capacity,22 our study is the first to analyse the relationship between introduction of a scheduling system and healthcare utilisation.
Local context: ANC scheduling
The large majority (almost 99%) of women in Mozambique receive ANC in public health facilities.4 Before the study intervention, women were assigned their next antenatal appointment 30 days from the date of their visit in public clinics, without any specified time. Pregnant women typically arrived early in the morning to wait for ANC and consultation order was determined by type of visit (first vs follow-up) and the order of patient arrival (first come, first served). Facility organisation varied; in some facilities, women coming for their initial ANC visit were seen first, while in others priority was given to follow-up visits.
Scheduling intervention design
The evaluation study took place between September 2016 and July 2017. All of the study health facilities were high-volume (ie, 21–40 ANC patients per day) public health facilities. In treatment clinics, patients receiving ANC were asked to select a return time on the date of their next appointment. Patients were informed that if they returned at their scheduled date and time they would be seen within 1 hour by clinic staff. Nurses recorded the appointment date and time on a scheduling card provided to patients and in an appointment book provided to facilities.
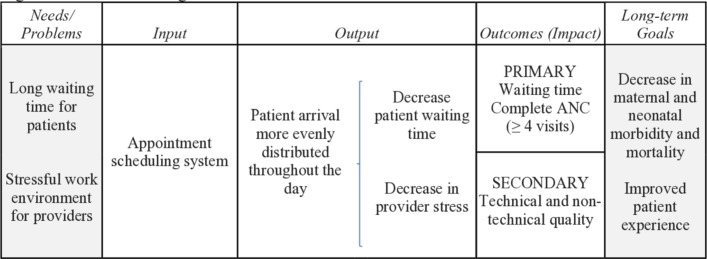
Theory of change
The intervention could decrease waiting time by more evenly distributing patient arrival throughout the day (figure 1). The intervention could increase utilisation if decreased waiting time makes it easier for patients to attend their appointment, if having a specific time makes the patient feel more responsible for returning on their scheduled date, or if the appointment serves as a signal that the health system is responsive to patients. Managing long patient queues may increase health worker stress. Therefore, the intervention could improve technical and non-technical quality by reducing health worker stress and improving the technical content and interpersonal quality of their communication with patients. Scheduled appointments might also increase visit duration, which could give nurses more time to complete recommended tests and counselling. Alternatively, appointment scheduling could decrease quality if nurses dislike the new system, or if needing to see patients at specific times increased health worker stress.
Figure 1.
Intervention logic framework. ANC, antenatal care.
Study population
Scheduling interventions were implemented in three clinics. Two intervention clinics were located in urban Maputo (Boane and Malhangalene). A third intervention clinic, Quissico, located in rural Inhambane Province, was included to test scheduling in a rural environment where employment and transportation might differ. A fourth clinic, Machava II, located in urban Maputo, was used as a comparison. We selected clinics with high ANC volume and accessibility to a main road.
Methods
Study outcomes
The primary study outcomes were (1) waiting time for ANC as measured by patient-reported survey data collected by our study team, and (2) receipt of complete ANC defined as four or more ANC visits during pregnancy. The number of visits was obtained from administrative data contained in facility registers. The secondary outcomes were (1) an index of technical quality and (2) an index of non-technical quality of care measured using variables collected in survey data. Technical quality was measured using an index measuring self-reported receipt of the technical components of ANC recommended by the WHO for all ANC visits (abdominal examination, measurement of uterine height, provision of folic acid, provision of malaria prophylaxis and discussion of signs of pregnancy complications). Non-technical quality was defined by an index of patient satisfaction with interpersonal quality including an indicator for any experience of disrespect or abuse, as well as Likert scales for the communication skills, friendliness and respectfulness of health workers. Online supplementary table 1 describes the definition and data source for each outcome.
bmjgh-2019-001788supp001.pdf (839.8KB, pdf)
Data sources
Waiting time data collection
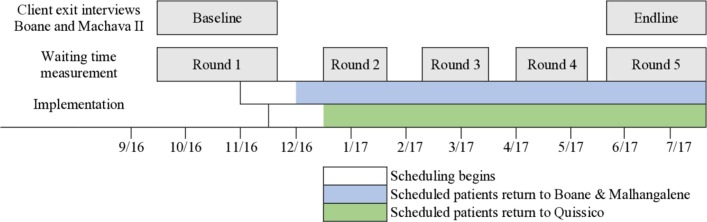
Starting at 07:30, enumerators recorded the time that all ANC patients arrived, the time their consultation began and the time their consultation ended. Waiting time data were collected using an electronic application at baseline, and all subsequent rounds of waiting time data collection used paper forms. As many women arrive before 07:30, and the enumerator can only record information from one woman at a time, study enumerators also recorded the patient’s self-reported arrival time. Four consecutive weeks of baseline waiting time data was collected in all four study facilities with staggered start dates. Following the introduction of the scheduling intervention, waiting time was measured bimonthly for a period of 2 weeks in all intervention and control facilities. Finally, 4 weeks of data were collected at endline (round 5) (see figure 2 for a general timeline, the online supplementary appendix for detailed waiting time data collection procedures and the online supplementary table 2 for a detailed timeline).
Figure 2.
Study timeline.
As the same nurses providing ANC also provide family planning and postpartum care, it is possible that ANC scheduling affected the amount of time health workers spent seeing other types of patients. To examine whether appointment scheduling for ANC had the unintended consequence of diverting resources away from other services, we tested whether scheduling appointments for ANC resulted in nurses spending less time with patients seeking family planning. To do this, enumerators collected waiting time from five randomly selected women who received family planning services during both baseline and endline data collection in the control facility and in Boane, one of the treatment facilities. Finally, enumerators also recorded the number of staff providing ANC on each day of waiting time data collection.
ANC and delivery exit interviews
We conducted baseline and endline exit surveys in Boane (T) and Machava II (C). We conducted ANC client exit interviews to obtain detailed demographic data and information on the quality of ANC from a sample of women attending the study clinics for ANC. We collected delivery exit interviews to obtain information on the location of all ANC visits during pregnancy from women who delivered at the health facility. Nearly all women obtained ANC at the same health facility during pregnancy, which gave us confidence that the administrative data we extract from clinic records provide a complete picture of ANC utilisation. ANC exit interviews recorded patient demographics and the self-reported content of, and satisfaction with, the ANC visit that occurred on the day of data collection. Delivery exit interviews recorded the self-reported content of, and satisfaction with, the most recent ANC visit before delivery. For ANC exit interviews, study enumerators recruited women attending ANC who were ≥18 years old and whose gestational age was between 16 and 22 weeks. For the delivery exit interviews, all women ≥18 years of age who delivered during the weeks of enrolment were invited to participate.
Administrative data collection
We recorded the dates of all ANC visits from all women whose first ANC visit took place between April 2016 and April 2017 from facility registers. We started the date range in April 2016 as a new ANC register, which tracks women over the course of pregnancy, began to be used by public health facilities in April 2016. We transcribed data from registers during the month of November 2017 for this study. As we wanted to be able to observe all visits during the course of pregnancy for all women included in the study, we restricted data collection to include any woman with a first visit between April 2016 and April 2017 (eg, a woman who began ANC in April 2017 when she was 2 months pregnant with an estimated delivery date in November 2017 would have all her visits recorded in the facility register).
We used these data to construct a variable measuring exposure to the scheduling system in the following way. We assume that women will have 40 weeks of pregnancy in which they may experience scheduled visits. Women whose entire pregnancy took place before the start of the intervention would be assigned 0 exposure weeks. Women whose pregnancy overlapped with the intervention would be assigned the number of pregnancy weeks remaining after the start of the intervention. Any woman whose entire pregnancy took place after the start of the intervention would be assigned 40 weeks of exposure.
Pre-post analysis within treatment facilities
Our main analyses are conducted with data only from treated facilities. In order to visualise changes in waiting time over the study period, we graphically present average waiting time in each of the five rounds of waiting time data collection in all of the study facilities. In this graph, the x axis measures study round by facility, and the y axis measures average waiting time pooling individual-level data from each facility’s data collection round. Facility-specific results are presented in online supplementary figure 1. We also graph the distribution of arrival times at baseline and in the four rounds of follow-up data collection after the start of the intervention. We then regressed waiting time on a post indicator variable identifying observations after the start of appointment scheduling and 4 day of the week dummy variables (regression equation 1 in the online supplementary appendix). We use self-reported arrival time since some patients arrived at the facility before the enumerator in the morning. We present several robustness checks including estimating waiting time with observed instead of self-reported waiting time, adjusting the waiting time outcome for censoring and accounting for clustering in SEs23 in online supplementary tables 3–5.
To check patients’ adherence to the new scheduling system, we calculated the difference between patient arrival time and the time of the scheduled appointment. To check providers’ compliance with the scheduling system, we calculated the difference between the patient’s appointment time and the time they were seen by a nurse.
To examine utilisation, we tested whether exposure to scheduling, defined as the number of weeks of pregnancy remaining after the start of the scheduling intervention, increased the likelihood that women obtained complete ANC (regression equation 2 in the online supplementary appendix). We used a generalised linear model for a binomial outcome with an identity link function. The model included facility fixed effects, and robust SEs. The results of this analysis using wild bootstrap SEs are presented in online supplementary table 3. To examine changes in the utilisation outcome over time, we also plot the percentage of women with complete ANC by month of the first ANC visit.
Difference-in-differences analysis in intervention and comparison facilities
To understand whether our findings were driven by changes unrelated to scheduling during the study period, we conducted a difference-in-differences analysis to compare the change in the study outcomes in the three intervention clinics with the change in the comparison clinic. We use difference-in-differences regression analysis to assess the effect of scheduling on waiting time for ANC, ANC utilisation, waiting time for family planning, and technical and non-technical quality of ANC. We present findings for these analyses excluding Quissico, the only rural health facility, in the online supplementary table 6. For the two quality outcomes, and the analysis of waiting time for family planning, we include only Boane (treatment) and Machava II (comparison) in the difference-in-differences analysis as data collection for these outcomes only took place in these two facilities. Waiting time and quality regressions used ordinary least squares and the utilisation regression used a generalised linear model for a binomial outcome with an identity link function. All analyses included a postvariable identifying observations after scheduling and an indicator of exposure to scheduling. An interaction term between these two variables was used to assess the effect of scheduling on the study outcomes (regression equations 3 and 4 in the online supplementary appendix). We also present findings from the same regression for the individual components of the quality scores in online supplementary table 7.
Human subjects approval and study registration
This study received human subjects approval from the authors’ institutes. The study has been registered at ClinicalTrials.gov.
Patient and public involvement statement
The study was informed by previous research showing that waiting time is perceived by patients as an important barrier to healthcare receipt in low-income countries. Patients were included in ANC and delivery care exit surveys but were not directly involved in the design of this study. Information on appointment scheduling and the results of this study may be distributed to patients by the Ministry of Health through media announcements.
Results
Table 1 displays baseline levels of facility and patient characteristics.
Table 1.
Health facility and patient characteristics at baseline
| Boane (T) Urban n (%)/mean (SD) |
Malhangalene (T) Urban n (%)/mean (SD) |
Quissico (T) Rural n (%)/mean (SD) |
Machava II (C) Urban n (%)/mean (SD) |
|
| Facility characteristics* | ||||
| Mean ANC nurses† | 2.4 (1.0) | 1.6 (0.5) | 1.9 (0.4) | 2.6 (0.9) |
| Mean ANC auxiliary nurses | 2.2 (0.6) | 1.2 (0.4) | 4.1 (0.9) | 2.3 (0.5) |
| Number of ANC visits per day | 25.4 (7.9) | 21.2 (8.7) | 22.9 (12.9) | 40.0 (19.0) |
| n | 20 | 18 | 20 | 20 |
| Patient characteristics‡ | ||||
| Mean age | 23.4 (5.0) | 24.5 (5.5) | 26.6 (5.5) | 23.5 (4.1) |
| Mean travel time to facility (min) | 47.8 (29.9) | 33.6 (35.7) | 70.5 (39.8) | 36.2 (23.2) |
| Mean household size | 5.2 (2.6) | 6.0 (3.0) | 5.1 (2.8) | 4.7 (2.2) |
| Per cent married | 26 (90) | 21 (75) | 26 (81) | 22 (73) |
| Per cent worked for money | 8 (28) | 8 (29) | 17 (53) | 7 (23) |
| Per cent responsible for child care§ | 16 (55) | 13 (46) | 23 (72) | 11 (37) |
| n | 29 | 28 | 32 | 30 |
| Study outcomes at baseline | ||||
| Mean waiting time | 281.6 (126.3) | 178.8 (87.1) | 128.2 (86.7) | 175.6 (93.0) |
| n¶ | 505 | 377 | 433 | 432 |
| Per cent with ≥4 ANC visits | 490 (52) | 236 (39) | 528 (58) | 1380 (70) |
| n** | 941 | 605 | 911 | 1976 |
*Staff and ANC visit numbers collected during round 1 of waiting time data collection.
†Included both nurses employed by the Ministry of Health who are permanently based at the health facility and temporary staff employed by non-governmental organisations.
‡Data from women ≥18 years old between 16 and 22 weeks pregnant surveyed during round 1 of ANC exit interviews.
§Survey question included both the respondent’s own children and other children.
¶Round 1 of waiting time data among women who received antenatal care in September/October 2016 in Malhangalene and in October/November 2016 in Boane, Machava II and Quissico.
**Administrative data from facility records documenting the number of antenatal care visits obtained during pregnancy among women who came for their first antenatal care visit between 1 April and 31 October 2016.
ANC, antenatal care.
Scheduling system implementation
Appointment scheduling shifted the distribution of arrival times for ANC towards later arrival (figure 3). Before scheduling, 62% of women seeking ANC in treatment facilities arrived before 08:00, when the facility opened. During follow-up rounds, this percentage declined to 22% (figure 3). Forty-eight per cent of patients arrived before their hour-long appointment window (online supplementary figure 2). However, 58% of patients overall, and 51% who arrived on time, were seen by nurses after the end of their window (online supplementary figure 3).
Figure 3.
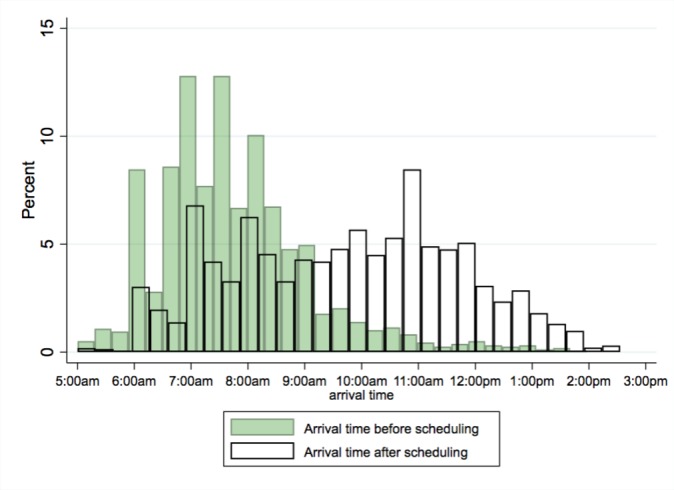
Distribution of patient arrival times for antenatal care before and after scheduling. Source: Waiting time data collection rounds 1–5. White bars capture rounds 2–5.
The average of mean daily waiting time across the three facilities at baseline was 182 min. Average waiting time after scheduling ranged from 85 to 107 min, a decrease between 41% and 53% from baseline (figure 4).
Figure 4.

Waiting time for antenatal care visits. Source: Waiting time data collected from 19 September to 18 November 2016 (round 1), 12 December 2016 to 20 January 2017 (round 2), 6 February to 10 March 2017 (round 3), 27 March to 28 April 2017, (round 4) and 22 May to 14 July 2017 (round 5).
Impact on utilisation
Pre-post analysis within treatment facilities
Our regression analysis, which controls for day of the week effects, shows that waiting time declined by 100.0 min after scheduling (95% CI −107.2 to −92.9, p<0.0001) (table 2, panel A). The decline in waiting time was largest in Boane (−144.8, 95% CI −156.9 to −132.8), where baseline waiting time was longest. The decrease in waiting time was more modest in Quissico (−47.1, 95% CI −56.0 to −38.3), the rural treatment facility with the shortest baseline waiting time. These results remain consistent when using observed waiting time and censored waiting time in place of self-reported arrival time (online supplementary tables 4 and 5).
Table 2.
Pre-post analysis examining change in waiting time and ANC utilisation among treatment facilities
| Boane (T) |
Malhangalene (T) |
Quissico (T) |
Pooled treatment facility results | |
| β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | |
| Panel A: waiting time†‡ | ||||
| Post indicator | −144.8*** (–156.9 to –132.8) |
−88.9*** (–98.6 to –79.2) |
−47.1*** (–56.0 to –38.3) |
−100.0*** (–107.2 to –92.9) |
| Baseline mean | 281.6 | 178.8 | 128.2 | 201.6 |
| n | 1709 | 1579 | 1702 | 4990 |
| Panel B: ≥4 ANC visits§¶ | ||||
| Weeks exposed | 0.004*** (0.003 to 0.006) |
0.008*** (0.006 to 0.009) |
0.003*** (0.001 to 0.004) |
0.004*** (0.004 to 0.005) |
| Constant | 0.504*** (0.467 to 0.542) |
0.294*** (0.248 to 0.340) |
0.570*** (0.535 to 0.605) |
0.499*** (0.469 to 0.528) |
| n | 1742 | 1201 | 1921 | 4864 |
***p<0.01.
†Source: Five rounds of waiting time data collection (one round before treatment and four rounds in post-treatment).
‡Ordinary least squares regression models comparing baseline waiting time with waiting time during four rounds of follow-up waiting time data collected after the start of the scheduling intervention. 95% CIs in parentheses. Regressions are adjusted for day or the week.
§Source: Administrative data from facility records documenting the number of antenatal care visits obtained during pregnancy among women who came for their first antenatal care visit between 1 April 2016 and 30 April 2017.
¶Generalised linear model for a binomial outcome with an identity link function. 95% CI in parentheses.
ANC, antenatal care.
We find that exposure to scheduling increased receipt of complete ANC by 0.004 percentage points each week in the pooled treatment facilities (95% CI 0.004 to 0.005, p<0.001) (table 2, panel B). This coefficient is equivalent to a 16 percentage point or 32% increase among women who were exposed to scheduling during all 40 weeks of pregnancy. The trend in complete ANC increased dramatically in treatment facilities after the start of scheduling but began to decline in January 2017 (online supplementary figure 4). Qualitatively similar results for waiting time and ANC utilisation from the same regressions using wild bootstrap SEs are presented in the online supplementary table 3.
Difference-in-differences analysis in intervention and comparison facility pair
We find that appointment scheduling decreased waiting time and increased ANC utilisation in our difference-in-differences analysis, confirming the results we found in the pre-post analysis (table 3, panel A). The results of these analyses are very similar after excluding Quissico, the intervention facility located in a rural area (online supplementary table 6). Furthermore, ANC scheduling did not affect waiting time for other services offered in the same health unit such as family planning (−0.94, 95% CI −37.64 to 35.76, p=0.515) (table 3, panel B).
Table 3.
Difference-in-difference analysis examining change in waiting time, ANC utilisation and service quality in all study facilities
| Panel A: analysis in all study facilities | Waiting time for ANC†‡ (min) |
4 ANC visitsठ| |
| β (95% CI) | β (95% CI) | ||
| Treatment*post | −80.03*** (−92.12 to −67.94) | Treatment*exposure weeks | 0.004** (0.002 to 0.005) |
| Treatment | 26.15*** (15.14 to 37.15) | Treatment | −0.175** (−0.210 to −0.141) |
| Post | −19.78*** (−29.55 to −10.00) | Exposure weeks | 0.001 (−0.001 to 0.002) |
| Baseline control mean | 175.5 | Baseline in control group | 0.60 |
| n | 6918 | n | 8385 |
| Panel B: analysis in Boane (treatment) and Machava II (control) only | Technical quality index‡¶†† | Non-technical quality index‡¶‡‡ | Waiting time for family planning†‡ |
| β (95% CI) | β (95% CI) | β (95% CI) | |
| Treatment*post | −0.01 (−0.08 to 0.06) | 0.07 (−0.03 to 0.16) | −0.94 (−37.64 to 35.76) |
| Treatment | 0.05** (0.00 to 0.11) | −0.01 (−0.09 to 0.07) | −20.04 (−54.44 to 14.37) |
| Post | 0.03 (−0.02 to 0.08) | 0.00 (−0.07 to 0.07) | −18.80 (−45.12 to 7.53) |
| Baseline control mean | 0.74 | 0.89 | 140.1 |
| n | 315 | 315 | 425 |
**p<0.05; ***p<0.01.
†Source: Five rounds of waiting time data collection (one round before treatment and four rounds in post-treatment) among women waiting to receive antenatal care in treatment facilities (Boane, Malhangalene, Quissico) and the comparison facility (Machava II), and women waiting to receive family planning in Boane (treatment) and Machava II (comparison).
‡Ordinary least squares regression model. Difference-in-differences analysis controlling for day of the week. 95% CIs in parentheses.
§Source: Administrative data from facility records documenting the dates of all antenatal visits among women who came for their first antenatal care visit between 1 April 2016 and 30 April 2017 in treatment facilities (Boane, Malhangalene, Quissico) and the comparison facility (Machava II).
¶Source: Round 1 (pretreatment) and round 2 (post-treatment) antenatal exit interviews conducted among women who attended antenatal care in Boane (treatment) and Machava II (comparison) on the day of the survey, and round 1 (pretreatment) and round 2 (post-treatment) delivery exit interviews conducted among women who delivered in Boane (treatment) and Machava II (comparison).
††The technical quality index was constructed using the mean of the non-missing values of the following variables: (1) abdominal exam, (2) measurement of uterine height, (3) provision of folic acid, (4) provision of malaria prophylaxis, and (5) discussion of the signs of pregnancy complications.
‡‡The non-technical quality index was constructed using the mean of the non-missing values of the following four variables: (1) respectfulness of health workers, (2) good communication skills of the healthcare workers, (3) good friendliness of healthcare workers, and (4) never felt humiliated or disrespected at any point during antenatal care.
ANC, antenatal care.
Scheduling did not change the technical quality of ANC visits (−0.01, 95% CI −0.08 to 0.06, p=0.689) or non-technical quality of care (0.07, 95% CI −0.03 to 0.16, p=0.178) (table 3, panel B). Regression results for the individual components of the technical and non-technical indices are shown in online supplementary table 7.
Discussion
This study presents evidence that scheduling appointments reduced waiting time for ANC. The decline in waiting time was largest where baseline waiting time was longest (table 2). Despite concerns that even after scheduling, patients might continue to arrive early in the morning to guarantee a place in line, we found that most patients arrive before or during their scheduled time. We found that waiting time decreased more after the intervention in higher volume facilities, and that baseline waiting time was lower in the single rural health facility. While a larger sample would be needed to better understand heterogeneity in treatment effects, it may be that the intervention would be more effective in facilities closer to urban areas that are likely to have high patient volumes.
We estimate that scheduling increased receipt of complete ANC during pregnancy by 16 percentage points, a 32% increase. Though one previous study demonstrated that scheduling can reduce waiting time,22 our study provides the first evidence that appointment scheduling can increase service utilisation, suggesting that poor patient experience may be unpleasant and may contribute to poor health outcomes by decreasing utilisation.
We do not find evidence that reducing waiting times changes the technical and non-technical contents of an ANC visit. While it is reassuring that we do not find that exposure to a scheduling system reduced the likelihood of receiving key elements of care, our findings suggest that a more significant investment is needed to improve the content of ANC, and without this investment, changes in utilisation may not yield better health.
We find that the effect of the intervention on ANC utilisation decreases over time (online supplementary figure 4). This may be due to poor compliance among nurses who often saw patients over an hour after their scheduled visit hour. More evidence is needed to understand whether the potential benefits of the intervention attenuate over time and whether attenuation could be mitigated by better management and supervision of nurses to more closely adhere to scheduled times. Future research should use a larger trial to investigate whether appointment scheduling can be effectively supervised and sustained at a larger scale.
This study has several limitations. Though we observe no change in patient volume over the study period (online supplementary figure 5), it is possible that other changes occurred at the same time as our intervention, confounding our results. To address this concern, we conducted a difference-in-differences analysis. While this analysis is consistent with findings from our main specification, the comparison clinic had important baseline differences, including higher volume and a lower staff-to-patient ratio than the intervention clinics. Differences in baseline waiting time and patient volume between the facilities remain a limitation and we are unable to evaluate the assumption of parallel trends in the study outcomes because of a limited period of data collection prior to the intervention. Therefore, despite the inclusion of a comparison facility to control for changes affecting the study outcomes that were not due to the intervention, it is possible that the observed increase in ANC utilisation resulted from other changes in the treatment clinics after the start of the intervention.
Another limitation is that administrative records used to assess utilisation only document care that was obtained in that facility. While it is possible that women could have visited other facilities during their pregnancy, 96% of women responding to our exit survey report receiving all ANC at the same facility. Finally, our sample size for the quality outcomes is relatively small, and the quality outcomes are based on patient reports which may be upwardly biased if patients were worried that their responses will not remain confidential.24
Interventions that reorganise the process of care may have important unintended consequences, such as decreased resources to non-targeted services or adverse changes to intrafacility relationships or health worker motivation. We find no negative relationship between ANC scheduling and waiting time for family planning, another health service offered in the maternal and child health unit. We also find that scheduling did not adversely affect the technical quality of care provided by health workers. However, there are other potential negative side effects of scheduling that we cannot address. For example, in some health facilities, group counselling occurs before the start of ANC consultations. In future research, it will be valuable to consider the impact of scheduling on patient knowledge of key health information during pregnancy.
The quality of healthcare has recently taken central stage in the international health systems agenda with the 2018 publication of the Lancet Global Health Commission’s Report on High-Quality Health Systems,25 which aims to ensure that the quality of healthcare increases alongside global coverage targets set by the Sustainable Development Goals. Future interventions targeting healthcare quality should consider incorporating improvements in the management of patient flows as they may offer a low-cost, high-impact avenue for improving patient experience.
Conclusion
We demonstrate that relatively simple improvements in the organisation of care that reduce waiting time can increase utilisation of healthcare during pregnancy. Our evidence suggests that patient experience is an important consideration for its own sake, and it may play an important role in shaping utilisation patterns.
Acknowledgments
The authors thank all the participants for their participation in the study. The authors also thank Carla Alberto for her excellent research assistance and all of the study enumerators who worked to collect the data reported in this study.
Footnotes
Handling editor: Seye Abimbola
Contributors: MM and SS co-led the study design and supervised data analysis. MS, JD, AA, SC, ESG, SS and MM contributed to the study design. MS conducted data analysis and drafted the manuscript. All authors contributed to the interpretation of data, reviewed and approved the final version of the manuscript.
Funding: This study was funded by the Abdul Latif Jameel Poverty Action Lab’s (J-PAL) Urban Services Initiative and the International Growth Center. MS was supported by the NIH training grant (T32 HD007338) and other NIH support (P2C HD041020).
Disclaimer: The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: This study received human subjects approval from Harvard TH Chan’s Institutional Review Board (IRB16-0344), the London School of Economics Ethics Committee and from the Mozambican Ministry of Health’s Comité Institucional de Bioética do Instituto Nacional de Saúde. Study participants who completed interviews provided written consent. A waiver of consent was approved for the administrative data collected in this study as these data contained no individual identifying information and was considered minimal risk. This study was registered at ClinicalTrials.gov.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request.
References
- 1. Lawn J, Kerber K. Opportunities for Africas newborns: practical data policy and programmatic support for newborn care in Africa, 2006. [Google Scholar]
- 2. Bhutta ZA, Das JK, Bahl R, et al. . Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet 2014;384:347–70. 10.1016/S0140-6736(14)60792-3 [DOI] [PubMed] [Google Scholar]
- 3. Instituto Nacional de Saúde (INS) Instituto Nacional de Estatística (INE) and ICF Inquérito de Indicadores de Imunização, Malária E HIV/SIDA em Moçambique (IMASIDA 2015). Maputo, Moçambique. Rockville, Maryland, 2017. [Google Scholar]
- 4. Ministerio da Saude (MISAU) Instituto Nacional de Estatística (INE) and ICF International (ICFI) Moçambique Inquérito Demográfico E de Saúde 2011. Calverton, Maryland, USA: MISAU, INE and ICFI, 2012. [Google Scholar]
- 5. The World Health Organization Who recommendations on antenatal care for a positive pregnancy experience. Geneva, Switzerland: The World Health Organization, 2016. [PubMed] [Google Scholar]
- 6. Kruk ME, Gage AD, Arsenault C, et al. . High-quality health systems in the sustainable development goals era: time for a revolution. Lancet Glob Health 2018;6:e1196–252. 10.1016/S2214-109X(18)30386-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kruk ME, Larson E, Twum-Danso NAY. Time for a quality revolution in global health. Lancet Glob Health 2016;4:e594–6. 10.1016/S2214-109X(16)30131-0 [DOI] [PubMed] [Google Scholar]
- 8. Larson E, Vail D, Mbaruku GM, et al. . Moving toward patient-centered care in Africa: a discrete choice experiment of preferences for delivery care among 3,003 Tanzanian women. PLoS One 2015;10:e0135621 10.1371/journal.pone.0135621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jallow IK, Chou Y-J, Liu T-L, et al. . Women's perception of antenatal care services in public and private clinics in the Gambia. Int J Qual Health Care 2012;24:595–600. 10.1093/intqhc/mzs033 [DOI] [PubMed] [Google Scholar]
- 10. Kigenyi O, Tefera GB, Nabiwemba E, et al. . Quality of intrapartum care at Mulago national referral Hospital, Uganda: clients' perspective. BMC Pregnancy Childbirth 2013;13:162 10.1186/1471-2393-13-162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Peltzer K. Patient experiences and health system responsiveness in South Africa. BMC Health Serv Res 2009;9:117 10.1186/1472-6963-9-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hasumi T, Jacobsen KH. Healthcare service problems reported in a national survey of South Africans. Int J Qual Health Care 2014;26:482–9. 10.1093/intqhc/mzu056 [DOI] [PubMed] [Google Scholar]
- 13. Asefa A, Bekele D. Status of respectful and non-abusive care during facility-based childbirth in a hospital and health centers in Addis Ababa, Ethiopia. Reprod Health 2015;12:33 10.1186/s12978-015-0024-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ishola F, Owolabi O, Filippi V. Disrespect and abuse of women during childbirth in Nigeria: a systematic review. PLoS One 2017;12:e0174084 10.1371/journal.pone.0174084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rosen HE, Lynam PF, Carr C, et al. . Direct observation of respectful maternity care in five countries: a cross-sectional study of health facilities in East and southern Africa. BMC Pregnancy Childbirth 2015;15:306 10.1186/s12884-015-0728-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Afrobarometer Afrobarometer data, Mozambique, round 5, 2015. [Google Scholar]
- 17. Mason L, Dellicour S, Ter Kuile F, et al. . Barriers and facilitators to antenatal and delivery care in Western Kenya: a qualitative study. BMC Pregnancy Childbirth 2015;15:26 10.1186/s12884-015-0453-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Do M, Wang W, Hembling J, et al. . Quality of antenatal care and client satisfaction in Kenya and Namibia. Int J Qual Health Care 2017;29:183–93. 10.1093/intqhc/mzx001 [DOI] [PubMed] [Google Scholar]
- 19. Okonofua F, Ogu R, Agholor K, et al. . Qualitative assessment of women’s satisfaction with maternal health care in referral hospitals in Nigeria. Reprod Health 2017;14:44 10.1186/s12978-017-0305-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Larson E, Mbaruku G, Mbatia R, et al. . Can investment in quality drive use? A cluster-randomised controlled study in rural Tanzania. Lancet Glob Health 2018;6 10.1016/S2214-109X(18)30138-4 [DOI] [Google Scholar]
- 21. Cohen J, Rothschild C, Golub G, et al. . Measuring The Impact Of Cash Transfers And Behavioral ‘Nudges’ On Maternity Care In Nairobi, Kenya. Health Aff 2017;36:1956–64. 10.1377/hlthaff.2017.0537 [DOI] [PubMed] [Google Scholar]
- 22. Atnafu A, Haile Mariam D, Wong R, et al. . Improving adult art clinic patient waiting time by implementing an appointment system at gondar university teaching Hospital, Northwest Ethiopia. Advances in Public Health 2015;2015:1–5. 10.1155/2015/892464 [DOI] [Google Scholar]
- 23. Cameron AC, Gelbach JB, Miller DL. Bootstrap-based improvements for inference with clustered errors. Review of Economics and Statistics 2008;90:414–27. 10.1162/rest.90.3.414 [DOI] [Google Scholar]
- 24. Dunsch F, Evans DK, Macis M, et al. . Bias in patient satisfaction surveys: a threat to measuring healthcare quality. BMJ Glob Health 2018;3:e000694 10.1136/bmjgh-2017-000694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kruk ME, Gage AD, Arsenault C, et al. . High-Quality health systems in the sustainable development goals era: time for a revolution. Lancet Glob Health 2018;6:e1196–252. 10.1016/S2214-109X(18)30386-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2019-001788supp001.pdf (839.8KB, pdf)