Abstract
This study aims to establish the range of exophthalmometry values (EV) in the adult Hong Kong (HK) Chinese population, its relationship with various anthropometric parameters, and to compare it with the EV in different ethnic groups.
About 1485 adult HK Chinese were drawn from a random sample from the community-based FAMILY Cohort. Participants were interviewed, and comprehensive ophthalmological assessments were conducted. EV was measured using the Hertel's exophthalmometer.
EV of both eyes from 630 male (42.4%) and 855 female (57.6%) participants, mean age 54 ± 17.2 and 52 ± 16 respectively were analyzed. The mean EV were found to be 15.3 ± 2.8 mm in the right eye, 15.2 ± 2.9 mm in the left eye for men and 14.4 ± 2.7 mm in the right eye, 14.3 ± 2.7 mm in the left eye for women. There were no differences in the EV between right and left eyes (P > .05). Men had significantly higher EV than women (P < .05) and age was found to be negatively correlated to EV (P < .05). Body height (r = 0.20), weight (r = 0.25), waist (r = 0.11), hip circumference (r = 0.15), body mass index (r = 0.17), interpupillary distance (r = 0.54), and axial length (AL) (r = 0.20) were all found to have statistically significant positive correlations with EV (P < .01). Spherical equivalent was found to have statistically significant negative correlation with EV (P < .01).
Our study provides normative data on EV in the HK Chinese population. Height, weight, interpupillary distance, waist, hip circumference, and AL had positive correlations with EV. Spherical equivalent had negative correlation with EV. There was no significant difference in EV between the right and left eye. Age and gender had significant effect on EV.
Keywords: Chinese, epidemiology, exophthalmometry values, Hertel's, proptosis
1. Introduction
Proptosis, forward displacement of the globe, can be a manifestation of various orbital pathologies, namely thyroid eye disease, tumor, trauma, and craniofacial abnormalities. As the various literature has demonstrated heterogenicity in exophthalmometric values (EV) across race and geographical locations, establishing a population specific set of normal value is critical for diagnosis, gauging severity, monitoring treatment, and guiding craniofacial plastic and reconstruction surgery.[1]
From clinical exophthalmometry to orbital computed tomography, modern technology has enabled a variety of means to measure the axial position of the globe. Despite possible inter-observer and inter-instrumental variability, the Hertel's exophthalmometry is simple and easy to operate, hence widely applied in clinical practice.[2,3] Distance between the vertex of the cornea to the anterior aspect of the lateral orbital margin is measured, giving rise to absolute (with reference to measurements of the general population), relative (with reference to the contralateral eye), and comparative (with reference to earlier measurements) values.[2]
Clinicians and scientists have been trying to establish normal EV for different populations for many decades. Studies have shown that EV may differ between various ethnicities due to differences in anatomy. This study reports on the range of globe position in the adult Hong Kong (HK) Chinese population and its relationship with various parameters including gender, age, height, weight, body mass index (BMI), hip, and waist circumference. No prior studies on Asian population has established the preliminary relationships between EV and anthropometric measurements.
2. Methods
The Department of Ophthalmology of the Li Ka Shing Faculty of Medicine and the School of Public Health at the University of Hong Kong, in conjunction with the FAMILY Cohort,[4] launched a comprehensive eye survey nested within the large, population-based FAMILY Cohort. These participants have been part of the Cohort since 2008, with known background demographic data available. The study design, cohort characteristics, inclusion, and exclusion criteria of the FAMILY Cohort have been previously reported.[4]
For this current study, participants from the FAMILY Cohort were drawn from a random core sample and were recruited by telephone invitation. All participants recruited were ≥18 years old. After obtaining written consent, subjects were interviewed, and thorough ophthalmological assessments were performed. The height, weight, hip, and waist circumference of each participant was measured and recorded. Their BMI was then calculated using the formula: weight (kg)/square of height (meters2). Subjective refraction was measured by a certified optometrist and the axial length (AL) was measured using ocular biometer (AL-Scan, Nidek, Gamagori, Japan).
The position of the globe was measured using the Hertel's exophthalmometer (Oculus 52400). The measurement was taken in a well-lit room with subjects sitting up right. The Hertel's exophthalmometer rested on the lateral orbital rims with the subject's eyes directed forwards. Through the system of mirrors and a millimeter scale, the protrusion of the corneal apex relative to the outer orbital margin in the sagittal plane was measured and recorded.
Data analysis was done using SPSS software (version 25, Chicago, IL). The mean and standard deviations were calculated. Statistical significance between male and female EV readings was calculated using the Mann–Whitney U test. Comparisons of EV between different age groups were performed using the Kruskal–Wallis test. Correlations between different parameters with EV were tested by Pearson correlation test. A P-value less than .05 was considered statistically significant.
3. Results
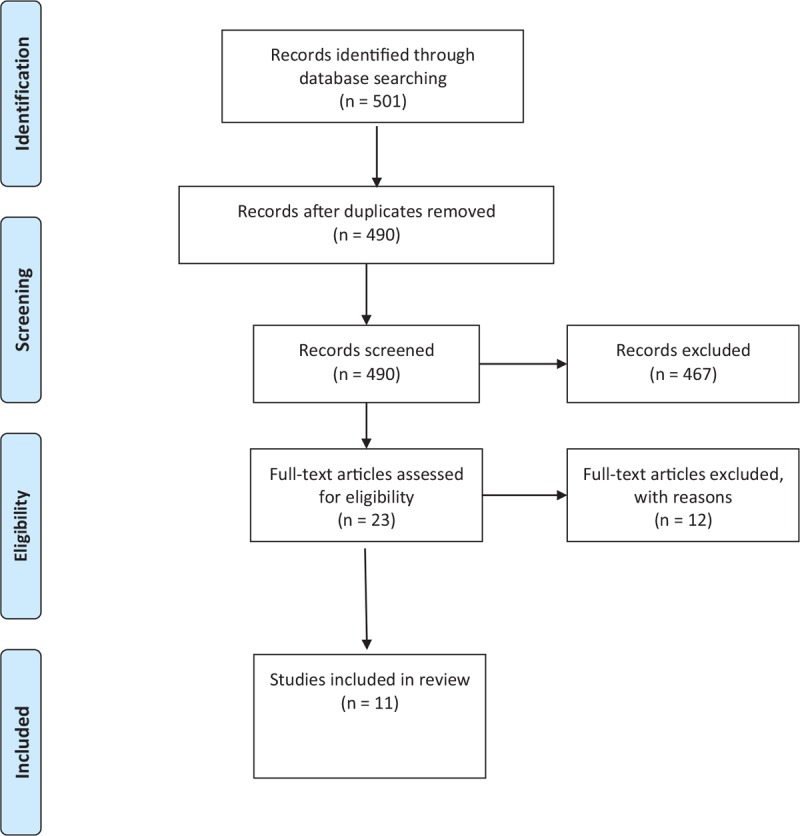
A total of 1517 participants out of 2202 eligible subjects were recruited from February 6, 2017 to December 31, 2017. Among these 1517 participants, 32 were excluded due to myopia or hyperopia greater than 6D, missing exophthalmometric readings for either one or both eyes, and one subject was excluded for having an erroneous reading for one eye. A total of 1485 participants’ data were analysed, including 630 males (42.4%) and 855 females (57.6%) (see Fig. 1).
Figure 1.
Flow diagram of participant recruitment.
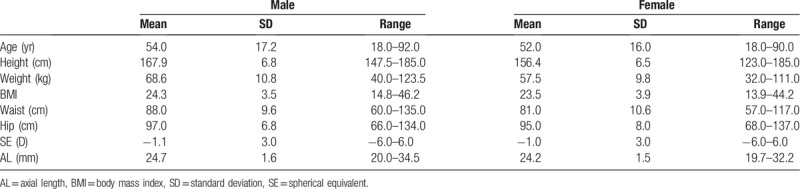
The mean age of male participants was 54 years old (range 18–92 years old) and mean age of female participants was 52 years old (range 18–90 years old). Table 1 summarizes the age, anthropometric measurements (including the height, weight, BMI, waist circumference, and hip circumference), spherical equivalent (SE), and AL.
Table 1.
Age, anthropometric measurements, refraction, and eyeball axial length.
Subjects were divided into 4 age groups: 18–40, 41–60, 61–80, and >80 and the mean EV and the reference range using the 95% confidence interval within the different age groups were calculated (see Table 2).
Table 2.
Mean, standard deviations, and 95% confidence interval of EV of different age groups.
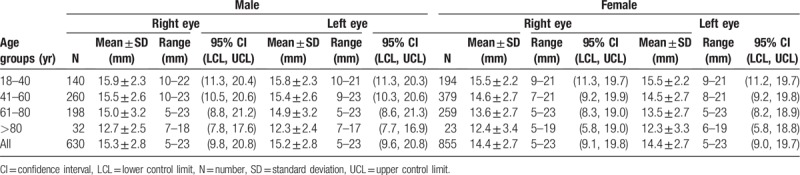
There was no statistically significant difference between the two eyes when compared independently among the male and female participants. EV in male participants was 15.3 mm on the right and 15.2 mm on the left, with no statistically significant difference (P > .05). That of female participants was 14.4 mm on the right and 14.3 mm on the left, also with no statistical significance (P > .05). However, male participants had significantly higher EV compared with female participants (P < .001).
The difference in EV between the different age groups in both eyes for male and female participants was significantly different (P < .001) (see Fig. 2). There was a negative correlation between age and EV, indicating EV decreased with increasing age and the correlation was statistically significant (P < .001).
Figure 2.
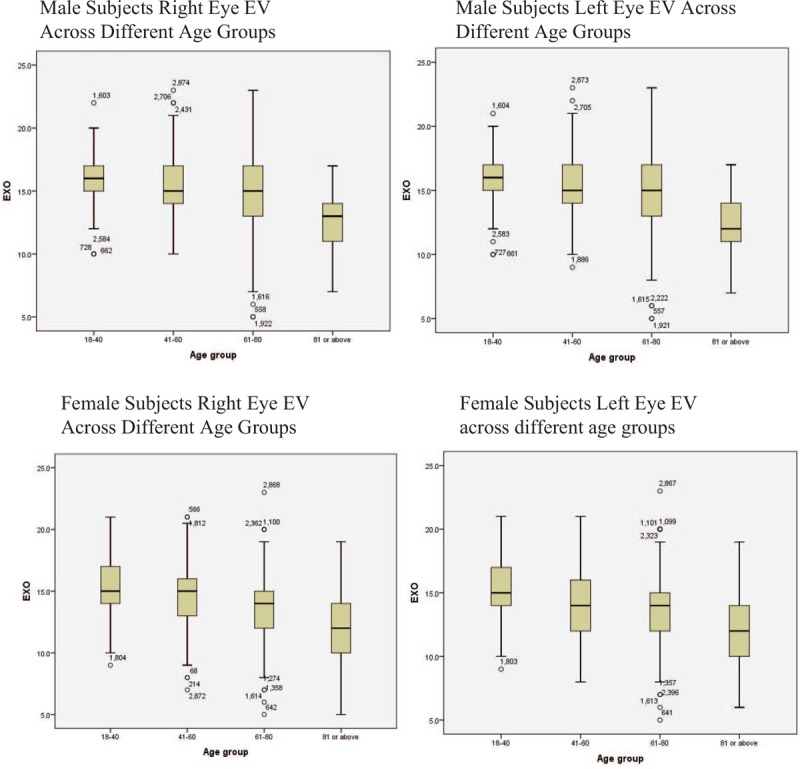
Male and female subjects exophthalmometric values of right and left eyes across different age groups.
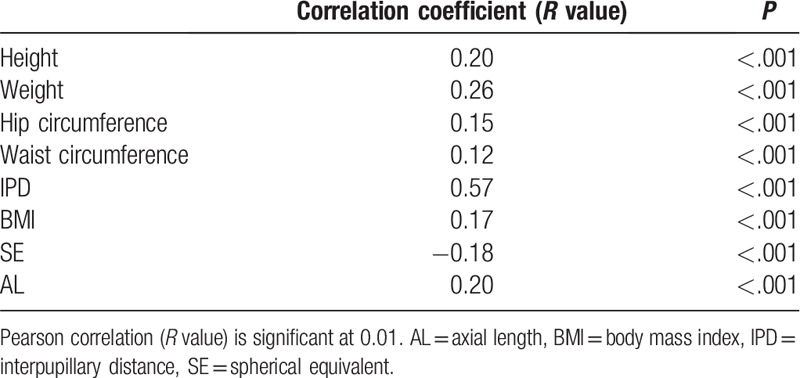
Body height, weight, waist circumference, hip circumference, BMI, interpupillary distance, and AL were all found to have statistically significant positive correlations with EV, while SE had statistically significant negative correlation with EV (P < .001). Table 3 summarizes correlation coefficient and P-values of these parameters.
Table 3.
Correlation coefficient and P-value of relationship between body height, weight, hip circumference, waist circumference, interpupillary distance, body weight index, spherical equivalent, and axial length with EV.
4. Discussion
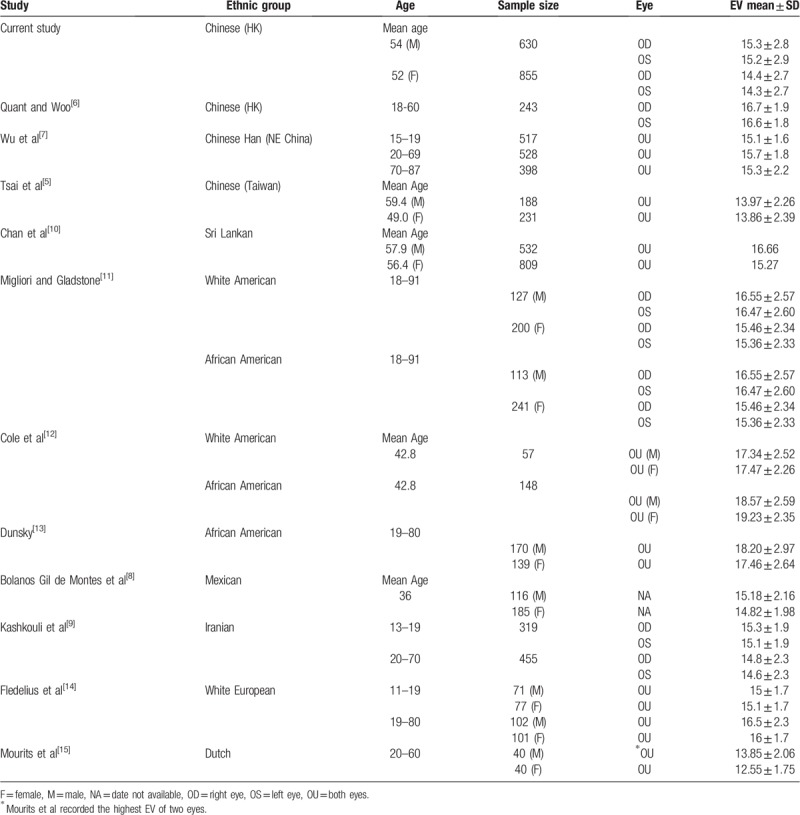
A systematic review of the literature according to The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was used to identify studies for comparison with our data results (see Fig. 3). Studies with only participants below 18 years old were not included since our study does not have the relevant data for comparison. Table 4 is a summary of the 11 studies included.
Figure 3.
PRISMA flowchart.
Table 4.
Comparison of Hertel's EV among different ethnic populations.
Proptosis is defined as a measurement 2 mm greater than the normal upper limit as suggested by Tsai et al.[5] The primary aim of this study is to look into the EV of HK Chinese adults. The closest study in terms of subject ethnicity and geographical location was published in 1992 by Quant and Woo,[6] in which 243 HK Chinese aged 18 to 60 were recruited. While participants in our study were randomly selected, Quant and Woo[6] did not outline the mechanism of subject selection in their study. This suggests that our study has an additional methodological advantage in addition to a larger sample size of 1517 participants. Quant and Woo did not document the refraction and AL of their participants, while our study did, with a mean SE of –1.1D and –1.0D and mean AL of 24.7 mm and 24.2 mm, in male and female participants, respectively. Interestingly, despite a rising trend of myopia in Hong Kong, EV demonstrated in this study were lower than that in Quant and Woo's study. The mean ages of male and female participants were 54 and 52 years old, respectively, in this study, which is much older than that of the Quant and Woo[6] study with mean ages at 25 and 29, respectively. Mean EV in male participants (right eye) was 15.3 ± 2.79 mm in this study and that of the Quant and Woo[6] study was 16.73 ± 1.90 mm. Such difference is consistent with our finding that older age is associated with lower EV. Table 5 summarizes the important differences between the two studies.
Table 5.
Comparison of Hertel's EV among Hong Kong Chinese population.
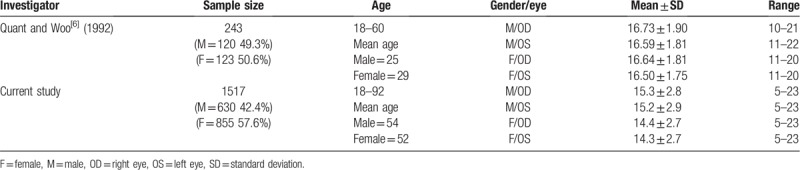
Quant and Woo[6] put forth 95% confidence limits for EV of normal subjects. It was suggested that values of less than 12 mm should be defined as enophthalmos and values more than 20.5 mm warranted further investigation. Based on such definitions, around 21% of our subjects have enophthalmos in either one or both eyes whereas 4 and 13 subjects were found to have unilateral and bilateral EV readings above 20.5 mm, respectively. These could have been normal variants instead. From our data, the 95% confidence limit for EV of normal subjects was 9.5 mm to 20.9 mm in male participants and 9 mm to 19.7 mm in female participants. In view of the large sample size, the data distribution can be assumed normal and therefore the reference range can be derived from the 95% confidence limits. In our study, the mean SE was –1.1 ± 3D and –1.0 ± 3D, and mean AL was 24.7 ± 1.6 mm and 24.2 ± 1.5 mm, in male and female, respectively. This was not documented in the study by Quant and Woo,[6] which may contribute to differences in EV.
Two studies conducted in Taiwan[5] and Northeastern China[7] also investigated the normal EV of Chinese participants. Both studies compared their findings with the normal EV reported in various studies that included participants of different ethnic groups and found considerable racial differences in the values.
Our study demonstrates that HK Chinese participants have similar EV to that of Northeastern Han Chinese,[7] Mexican,[8] and Iranian.[9] Sri Lankan,[10] White, and African American,[11–13] and White European[14] have significantly higher EV than our HK Chinese participants, whereas Taiwanese[5] and Dutch[15] have lower EV readings.
There are mixed conclusions regarding the relationship between refraction and AL with EV. Some studies[10,14] did not find significant correlation between SE and EV, yet our study is in agreement with Karti et al[16] in finding a significant negative correlation between SE and EV. Some studies eliminate data from subjects with myopia more than –6D[9] to exclude possibility of high myopia affecting EV. In our locality, there is high prevalence of high myopia,[17] we have similarly excluded subjects with SE greater than –6D. It is noteworthy that AL was shown to correlate with EV in our study and it should be taken into account in exophthalmometer measurements.[16]
Factors including age, gender, height, weight, and BMI are also known to contribute to differences in EV.[16] Earlier studies have demonstrated a negative correlation between EV and age starting from 20 years old,[9,18,19] which is consistent with our findings; this may be due to orbital soft tissue atrophy. The mean EV in the >80 years old group were significantly lower when compared to other age groups across both eyes and gender. Kashkouli et al[9] and Nath et al[19] included children and teenagers in their study and found EV to significantly increase as they grow older into adulthood. Fledelius and Stubgaard,[14] however, found EV to remain static after late teenage years. Chan et al[10] demonstrated in their study that EV were not statistically different across all age groups in both genders. Karti et al[16] commented in their study that the relationship between gender and EV is controversial. Bilen et al[20] and Kashkouli et al[9] did not find any statistically significant gender differences in EV in their study. Two older studies,[11,13] however, reported significantly higher EV in male than in females, which is in keeping with our findings. Fledelius and Stubgaard[14] attributed the higher male EV to the larger body structure.
According to the results of our study, anthropometric measurements like height, weight, hip, and waist circumference are positively related to EV. However, only a few previous studies have investigated into and discussed the reason for the correlation. Males in general are taller, heavier with larger hip and waist circumference, and are likely to have higher EV.[14] Smolders et al[21] found that obese patients have significantly higher EV. Their male and female obese participants had a mean BMI of 39.0 and 36.5, respectively. On top of the increased deposition of excess body fat in the retrobulbar fat-pads, medial rectus muscle enlargement was also found to be a contributing factor.
While the absolute EV is useful in diagnosing bilateral proptosis, relative EV measures the asymmetry of protrusion between the two eyes, hence useful in diagnosing unilateral proptosis.[9] Statistically significant differences between the two eyes has been reported in some studies,[22–24] but this was not demonstrated in our study. Some consider relative EV exceeding 2 mm to be clinically significant.[9] The findings from our study are useful in providing information to support further research in orbital conditions, particularly bilateral conditions such as thyroid eye disease where the fellow eye cannot be used as a normal baseline. Our study can provide local reference values to assess disease severity, and monitor progression and treatment response in future research.
Limitations were identified in our study. First, participants <18 years old were not included. It would be clinically relevant to conduct another study to establish a set of normal EV in this age group. Second, the study was solely conducted on Chinese residing in HK. It may not represent other ethnic populations and may not even fully represent the whole Chinese population. There may be geographical variations among the Chinese population. However, this was not seen when comparing our results from HK which lies in Southern China with the results from Chinese population residing in the Northeastern part of China.
5. Conclusion
Knowledge on normal EV has important implications on the diagnosis and management of ocular and orbital diseases of various etiologies. Ethnicity, age, and gender were all shown to affect EV in our study. Elementary relationships between height, weight, waist and hip circumference, AL and SE with EV were observed, warranting further studies to explicate these associations.
Author contributions
Conceptualization: Janice J.C. Cheung, Michael Y. Ni, Jimmy S.M. Lai, Ian Y.H. Wong.
Data curation: Janice J.C. Cheung, Jonathan C. Chan, Bonnie N.K. Choy, Kendrick C. Shih, Jasper K.W. Wong, Alex L.K. Ng, Jennifer W.H. Shum, Ian Y.H. Wong.
Formal analysis: Janice J.C. Cheung, Dulcia L. Chang, Ian Y.H. Wong.
Funding acquisition: Michael Y. Ni, Gabriel M. Leung, Ian Y.H. Wong.
Investigation: Janice J.C. Cheung, Jonathan C. Chan, Bonnie N.K. Choy, Kendrick C. Shih, Jasper K.W. Wong, Alex L.K. Ng, Jennifer W.H. Shum, Ian Y.H. Wong.
Methodology: Janice J.C. Cheung.
Project administration: Janice J.C. Cheung, Jonathan C. Chan, Bonnie N.K. Choy, Kendrick C. Shih, Jasper K.W. Wong, Alex L.K. Ng, Jennifer W.H. Shum, Michael Y. Ni, Jimmy S.M. Lai, Ian Y.H. Wong.
Resources: Ian Y.H. Wong.
Supervision: Jimmy S.M. Lai, Gabriel M. Leung, Ian Y.H. Wong.
Writing – original draft: Janice J.C. Cheung, Dulcia L. Chang.
Writing – review & editing: Janice J.C. Cheung, Dulcia L. Chang, Michael Y. Ni, Gabriel M. Leung, Ian Y.H. Wong.
Janice J.C. Cheung: 0000-0003-1216-729X.
Footnotes
Abbreviations: AL = axial length, BMI = body mass index, EV = exophthalmometry values, HK = Hong Kong, PRISMA = The Preferred Reporting Items for Systematic Reviews and Meta-Analyses, SE = spherical equivalent.
How to cite this article: Cheung JJC, Chang DL, Chan JC, Choy BNK, Shih KC, Wong JKW, Ng ALK, Shum JWH, Ni MY, Lai JSM, Leung GM, Wong IYH. Exophthalmometry values in the Hong Kong Chinese adult population from a population-based study. Medicine. 2019;98:47(e17993).
The study protocol was approved by the local institutional research ethics committee, Institutional Review Board of the Hospital Authority Hong Kong West Cluster (Ethics reference number: UW16-2038). The study firmly adhered to the tenets of the 1964 Helsinki declaration and its later amendments.
Financial support for this study was received from: the ‘Chloe Ho Safeguarding Vision Initiative,’ which was funded by The Jessie & George Ho Charitable Foundation and Hong Kong Jockey Club Charities Trust, which funded the establishment of the FAMILY Cohort from 2007 to 2014. The funding organization had no role in the design or conduct of this research.
The authors have no conflicts of interest to disclose.
References
- [1].Farkas LG, Posnick JC, Hreczko TM. Anthropometric growth study of the head. Cleft Palate Craniofac J 1992;29:303–8. [DOI] [PubMed] [Google Scholar]
- [2].Choi KJ, Lee MJ. Comparison of exophthalmos measurements: Hertel exophthalmometer versus orbital parameters in 2-dimensional computed tomography. Can J Ophthalmol 2018;53:384–90. [DOI] [PubMed] [Google Scholar]
- [3].Campi I, Vannucchi GM, Minetti AM, et al. A quantitative method for assessing the degree of axial proptosis in relation to orbital tissue involvement in Graves’ orbitopathy. Ophthalmology 2013;120:1092–8. [DOI] [PubMed] [Google Scholar]
- [4].Leung GM, Ni MY, Wong PT, et al. Cohort profile: FAMILY Cohort. Int J Epidemiol 2017;46:e1. [DOI] [PubMed] [Google Scholar]
- [5].Tsai CC, Kau HC, Kao SC, et al. Exophthalmos of patients with Graves’ disease in Chinese of Taiwan. Eye (Lond) 2006;20:569–73. [DOI] [PubMed] [Google Scholar]
- [6].Quant JR, Woo GC. Normal values of eye position in the Chinese population of Hong Kong. Optom Vis Sci 1992;69:152–8. [DOI] [PubMed] [Google Scholar]
- [7].Wu D, Liu X, Wu D, et al. Normal values of Hertel exophthalmometry in a Chinese Han population from Shenyang, Northeast China. Sci Rep 2015;5:8526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Bolaños Gil de Montes F, Pérez Resinas FM, Rodríguez Garcia M, et al. Exophthalmometry in Mexican adults. Rev Invest Clin 1999;51:341–3. [PubMed] [Google Scholar]
- [9].Kashkouli MB, Nojomi M, Parvaresh MM, et al. Normal values of hertel exophthalmometry in children, teenagers, and adults from Tehran, Iran. Optom Vis Sci 2008;85:1012–7. [DOI] [PubMed] [Google Scholar]
- [10].Chan W, Madge SN, Senaratne T, et al. Exophthalmometric values and their biometric correlates: the Kandy Eye Study. Clin Exp Ophthalmol 2009;37:496–502. [DOI] [PubMed] [Google Scholar]
- [11].Migliori ME, Gladstone GJ. Determination of the normal range of exophthalmometric values for black and white adults. Am J Ophthalmol 1984;98:438–42. [DOI] [PubMed] [Google Scholar]
- [12].Cole HP, 3rd, Couvillion JT, Fink AJ, et al. Exophthalmometry: a comparative study of the Naugle and Hertel instruments. Ophthalmic Plast Reconstr Surg 1997;13:189–94. [PubMed] [Google Scholar]
- [13].Dunsky IL. Normative data for hertel exophthalmometry in a normal adult black population. Optom Vis Sci 1992;69:562–4. [DOI] [PubMed] [Google Scholar]
- [14].Fledelius HC, Stubgaard M. Changes in eye position during growth and adult life as based on exophthalmometry, interpupillary distance, and orbital distance measurements. Acta Ophthalmol (Copenh) 1986;64:481–6. [DOI] [PubMed] [Google Scholar]
- [15].Mourits MP, Lombardo SH, van der Sluijs FA, et al. Reliability of exophthalmos measurement and the exophthalmometry value distribution in a healthy Dutch population and in Graves’ patients. An exploratory study. Orbit 2004;23:161–8. [DOI] [PubMed] [Google Scholar]
- [16].Karti O, Selver OB, Karahan E, et al. The effect of age, gender, refractive status and axial length on the measurements of hertel exophthalmometry. Open Ophthalmol J 2015;9:113–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Mak CY, Yam JC, Chen LJ, et al. Epidemiology of myopia and prevention of myopia progression in children in East Asia: a review. Hong Kong Med J 2018;24:602–9. [DOI] [PubMed] [Google Scholar]
- [18].Kaye SB, Green JR, Luck J, et al. Dependence of ocular protrusion, asymmetry of protrusion and lateral interobital width on age. Acta Ophthalmol (Copenh) 1992;70:762–5. [DOI] [PubMed] [Google Scholar]
- [19].Nath K, Gogi R, Rao GS, et al. Normal exophthalmometry. Indian J Ophthalmol 1977;25:47–52. [PubMed] [Google Scholar]
- [20].Bilen H, Gullulu G, Akcay G. Exophthalmometric values in a normal Turkish population living in the northeastern part of Turkey. Thyroid 2007;17:525–8. [DOI] [PubMed] [Google Scholar]
- [21].Smolders MH, Graniewski-Wijnands HS, Meinders AE, et al. Exophthalmos in obesity. Ophthalmic Res 2004;36:78–81. [DOI] [PubMed] [Google Scholar]
- [22].Kashkouli MB, Beigi B, Noorani MM, et al. Hertel exophthalmometry: reliability and interobserver variation. Orbit 2003;22:239–45. [DOI] [PubMed] [Google Scholar]
- [23].Musch DC, Frueh BR, Landis JR. The reliability of Hertel exophthalmometry. Observer variation between physician and lay readers. Ophthalmology 1985;92:1177–80. [DOI] [PubMed] [Google Scholar]
- [24].Lang J, Schäfer WD, Grafen W, et al. [Side differences in the position of the corneal apex in relation to the lateral orbital margin (measurements with the Hertel exophthalmometer)]. Klin Monbl Augenheilkd 1985;187:521–4. [DOI] [PubMed] [Google Scholar]


