Introduction
Radiologically, white matter hyperintensities (WMHs) are defined as confluent hyperintensities on T2-weighted and fluid attenuated inversion recovery (FLAIR) sequences, and generally thought to be the result of irreversible small-vessel disease secondary to arteriosclerosis. However, though rare and infrequent, the reversibility of WMHs has been reported.1 The transient disruption of the blood–brain barrier, small vessel ischemia, endothelial dysfunction and venous pressure has also been proposed to be the possible mechanism, but none of these hypotheses have been verified.
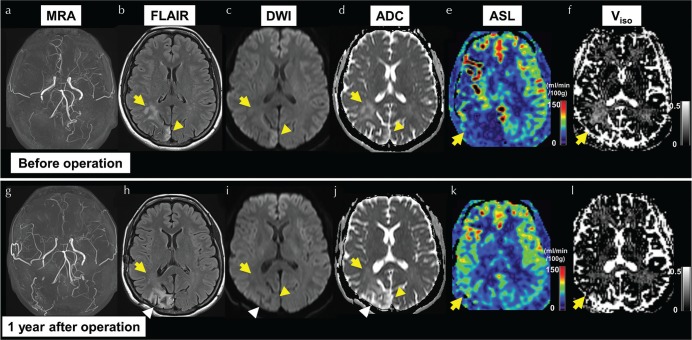
A 41-year-old female without significant past medical history suddenly developed visual impairment of the left lower part of the visual field. MRI in a local clinic revealed acute cerebral infarction of the right occipital cortex (Fig. 1, arrowhead) and WMH of the right occipital lobe (Fig. 1, arrow) adjacent to the infarction. MRA showed multiple intracranial arterial stenosis consistent with Moyamoya disease (Fig. 1a). After a detailed workup in our university hospital, she was diagnosed as Moyamoya disease with severe stenosis of the right posterior cerebral artery (Suzuki stage 4/3), and her right hemisphere suffered misery perfusion (Fig. 1e). Neurite orientation dispersion and density imaging (NODDI)2 revealed increased isotropic volume fraction (Viso), which reflects water components of the brain parenchyma, in the most affected right occipital lobe where the infarction and WMH existed (Fig. 1f). Three months later, she underwent the indirect bypass surgery on the right side to improve her hemodynamic condition, which resulted in a new infarction (Fig. 1h–1j, white arrowhead). Two months after the operation, dramatic improvement of the perfusion of the right hemisphere was observed; at the same time, the WMH of the right occipital lobe had disappeared. The increase in Viso observed before the operation had also been subsided (Fig. 1l, arrow).
Fig. 1.
Comparison of the MR images obtained before (a–f) and 1 year after the indirect bypass surgery (g–l). After the restoration of the hemodynamic impairment (e and k), the white matter hyperintensity (WMH) (arrow) adjacent to the occipital infarction (arrowhead) has completely disappeared, as well as the increase of Viso (f and I). ADC, apparent diffusion coefficient; ASL, arterial spin labeling; DWI, diffusion weighted image; FLAIR, fluid attenuated inversion recovery; Viso, isotropic volume fraction.
Considering the disappearance of increased Viso, we would like to propose dysfunction of the glymphatic system3 as a possible mechanism of the observed reversibility in our patient. In this water exchange system, cerebral arterial pulsatility has been demonstrated as a key driver of paravascular influx, which is likely impaired in Moyamoya disease.
Footnotes
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.Adachi M, Sato T. Characterization of the growth of deep and subcortical white matter hyperintensity on MR imaging: a retrospective cohort study. Magn Reson Med Sci 2017; 16:238–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang H, Schneider T, Wheeler-Kingshott CA, Alexander DC. NODDI: practical in vivo neurite orientation dispersion and density imaging of the human brain. Neuroimage 2012; 61:1000–1016. [DOI] [PubMed] [Google Scholar]
- 3.Naganawa S, Nakane T, Kawai H, Taoka T. Gd-based contrast enhancement of the perivascular spaces in the basal ganglia. Magn Reson Med Sci 2017;16:61–65. [DOI] [PMC free article] [PubMed] [Google Scholar]