Abstract
The Fast Track (FT) intervention was a multimodal preventive intervention addressing antisocial development across 10 years of childhood and early adolescence. The intervention included parent management training, child social-cognitive skills training, peer coaching and mentoring, academic skills tutoring, and a classroom social-emotional learning program. While not specifically designed to target psychosis symptoms (e.g., social withdrawal, thought abnormalities), the present study aimed to examine whether the FT intervention prevented psychosis symptoms through childhood and adolescence and into adulthood. Participants included the FT intervention and high-risk control samples (N = 891; 69% male; M age = 6.58 years, SD = .48). Psychosis symptoms were assessed using the “thought problems” subscale of the parent-report Child Behavior Checklist during grades 1, 2, 4, 5, and 7, and the self-report Adult Behavior Checklist at age 25 years, in line with prior research using this measure. Growth models included the FT condition and covariates (i.e., initial risk screen score, cohort, socioeconomic status, rural/urban status, race, and sex) as predictors; and child, adolescent, and adult psychosis symptoms as outcomes. Intervention status was not significantly associated with the slope of psychosis symptoms; however, after controlling for concurrent cannabis use, intervention participants reported lower levels of psychosis symptoms over time. Findings suggest that interventions targeting antisocial behavior may prevent psychosis symptoms in the long term.
Keywords: Intervention, Prevention, Psychosis, Cannabis
Psychotic disorders include abnormalities in the following domains: delusions, hallucinations, disorganized thinking, disorganized motor behavior, and negative symptoms (e.g., diminished emotional expression, avolition; American Psychiatric Association 2013), and are associated with significant impairments in psychosocial functioning and neuropsychological deficits. For example, individuals with early onset schizophrenia (i.e., in adolescence) have higher ratings of deviant behavior during social interactions, poorer attention and set shifting, and slower acquisition of new intellectual information compared with healthy controls (Jepsen et al. 2010a, b; Vourdas et al. 2003). Additionally, longitudinal analyses of antisocial youth show greater psychosis symptoms in adulthood (Bor et al. 2010; Reef et al. 2010). Given the numerous negative consequences of psychotic disorders, emphasis has been placed on identifying early signs of these disorders. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association 2013) included Attenuated Psychosis Syndrome (APS) under “conditions for further study.” APS symptoms are similar to those identified in psychotic disorders (e.g., delusions, hallucinations); however, they are defined as less severe, more transient, and often precede a psychosis diagnosis. These symptoms have not yet been validated in children under the age of 12 years. Current psychopharmacological treatments for psychosis have shown limited efficacy (Yung and Nelson 2013), and thus, psychosocial interventions have been developed with the aim of modifying the course of psychosis symptoms among those at high risk.
Early interventions targeting psychosis symptoms have been found to reduce symptom severity and prognosis. A recent review and meta-analysis suggested that the most effective intervention for psychosis would combine cognitive-behavioral therapy with family therapy (Stafford et al. 2013). Whereas cognitive-behavioral therapy is beneficial among patients with early psychosis symptoms (Morrison et al. 2012) and for reducing symptoms of anxiety and depression (which are highly prevalent among this population; McGorry et al. 2002; Morrison et al. 2011), family interventions have been found to reduce relapse rates among first episode and established psychosis patients (National Institute for Clinical Excellence [NICE] 2009). Family-based interventions also provide a level of social support that is beneficial for both study participants and their caregivers. Yet other research has shown no evidence that any specific preventive intervention is more effective over other interventions in preventing the development of psychosis symptoms (Davies et al. 2018). Additionally, others suggest that psychosis preventive interventions should also be targeting other psychopathology (e.g., posttraumatic stress symptoms) given the high comorbidity among this population (van der Gaag et al. 2017). Thus, further research is needed examining the impact of early interventions in preventing transition to psychosis.
Early interventions targeting proximal (i.e., immediate) risk and protective factors have shown promise for long-term developmental outcomes, appearing to most benefit those individuals at greatest risk (Reider et al. 2014). However, preventive interventions can have positive impact on outcomes not specifically targeted by the intervention. A recent supplemental issue of Prevention Science examined “cross-over” effects of six longitudinal early interventions for preventing health-risking sexual behaviors. Findings demonstrated “collateral change” (i.e., reduced health-risking sexual behaviors) due to the interventions but not previously anticipated (Reider et al. 2014), supporting other past research examining unintended effects of intensive early intervention (Patterson et al. 2010). Similar intervention effects have recently been found for psychosis symptoms. For example, the Treatment Foster Care-Oregon (TFC-O) program designed to target chronic delinquency among adolescents who had been court-mandated to community-based, out-of-home care found reductions in psychosis symptoms in girls over a 24-month period (Poulton et al. 2014). The authors suggested that the unanticipated positive impact on psychotic symptoms may have been due to indirect mechanisms via a reduction in emotional reactivity, which is linked to cognitive distortions. Thus, the present study aimed to examine whether the Fast Track (FT) project (Conduct Problems Prevention Research Group [CPPRG] 2019)—a longitudinal investigation of the development and prevention of conduct problems (and not designed to target psychosis)—had cross-over effects in reducing psychosis symptoms.
The FT intervention aimed to test whether developmental outcomes of young children at high risk for antisocial behavior could be improved through a multimodal psychosocial intervention. Children randomly assigned to the intervention condition received 10 consecutive years of the intervention (grades 1–10). Based on developmental theory positing that there are multiple influences on the development of antisocial behavior, the preventive program addressed family and school risk factors and included communication between parents and schools. The elementary school component targeted cognitive, social, and emotional deficits associated with academic failure, peer victimization, and oppositional behavior toward teachers and parents. The middle and high school component targeted adolescent developmental issues (e.g., parent supervision and substance use). Recent analyses found that the intervention was effective in reducing externalizing and internalizing psychopathology, substance use problems, and drug and violent crimes at age 25 (Dodge et al. 2015); however, it is unknown whether the intervention had cross-over effects with respect to reducing psychosis symptoms.
Experiences of trauma, particularly maltreatment, and other dysfunctional home environments are a risk factor for the development of psychosis. For example, schizophrenic patients with positive symptoms (i.e., delusions, hallucinations, disorganized thoughts) reported a history of childhood trauma (Ross et al. 1994), and abused patients are likely to have experienced positive symptoms (Read and Argyle 1999). Further, among adults, childhood abuse was a significant predictor of hallucinations even in the absence of experiences of abuse in adulthood (Read et al. 2003). In addition to the parent training groups that taught behavior management skills and promoted the development of positive family-school relationships, the intervention also included home visits for the purpose of increasing parents’ problem-solving and life management skills. These components of the FT intervention may have improved the home environment for at-risk youth, and thus, may have reduced the risk for developing psychosis.
During the elementary school phase of the FT intervention, the children participated in “friendship groups” (Bierman et al. 2017) and an adapted PATHS (Promoting Alternative Thinking Strategies) curriculum (Greenberg et al. 2011), both of which aimed to promote social-cognitive skills. Social-cognitive functioning among psychosis patients is markedly impaired (Savla et al. 2012). Social cognition is comprised of four domains: theory of mind, social perception, attribution bias, and emotion processing (Green et al. 2008). Aspects of social cognition (e.g., theory of mind) are impaired among individuals at risk for developing psychosis and patients in their first episode of psychosis (Kim et al. 2011). Further, a recent meta-analysis found that individuals at high risk exhibited deficits in all four domains of social cognition compared with healthy controls (Lee et al. 2015). Findings from the FT intervention sample indicated that 27% of the intervention’s effect on the development of antisocial behavior in adolescence (grade 9) was mediated by social-cognitive processing (Dodge et al. 2013). Thus, through increasing social cognition skills, the FT intervention may also decrease risk for psychosis symptoms.
Extensive research has linked substance use, and specifically cannabis use, to psychosis symptoms (Oh and Devylder 2017). The majority of this research supports the vulnerability hypothesis that posits that cannabis use increases the risk of developing psychotic disorders (Bagot et al. 2015). One systematic review found an increased risk of psychosis symptoms among individuals who had used cannabis (Odds Ratio [OR] = 1.41; Moore et al. 2007). The authors also identified a dose-response effect, such that more frequent users were at greatest risk (OR = 2.09). Youth and young adults report the greatest rates of cannabis use with estimates between 13–29% of the population reporting use within the past year (Wu et al. 2014). Adolescence is a critical period for brain maturation and exposure to cannabis use during this time leads to chronic activation of the dopaminergic system, which may play a role in greater susceptibility to later psychosis symptoms (Laruelle 2000; Ujike 2002). Thus, controlling for cannabis use, and particularly during adolescence, is important in psychosis research.
The Present Study
Psychosis symptoms were assessed with the “thought problems” subscale of the Child Behavior Checklist (CBCL; Achenbach 1991) during grades 1, 2, 4, 5, and 7, and the self-report Adult Behavior Checklist (ASR; Achenbach 1997) at age 25 years. Past research has found that the CBCL did not predict psychosis symptoms within an adolescent clinical sample (Simeonova et al. 2011); however, it held promise among a high-risk general population sample of youth (Simeonova et al. 2014). Although the FT intervention was not designed to specifically target psychosis symptoms, intervention research has demonstrated unanticipated beneficial cross-over effects for a range of health outcomes. Further, the FT intervention contained components for decreasing stress within the home and increasing social-cognitive skills—two factors negatively associated with psychosis symptoms. Thus, the present study aimed to determine whether the FT intervention prevented psychosis symptoms through childhood and adolescence and into adulthood. It was hypothesized that the FT intervention would be negatively associated with psychosis symptoms. Further, given the association of cannabis use and psychosis symptoms, we also examined whether the intervention would be negatively associated with psychosis symptoms controlling for concurrent (i.e., assessed at the same time point; see Fig. 1) and adolescent (see Fig. 2) cannabis use. It was hypothesized that the FT intervention would be negatively associated with psychosis symptoms controlling for cannabis use; we were unsure whether this would include concurrent or adolescent cannabis use.
Fig. 1.
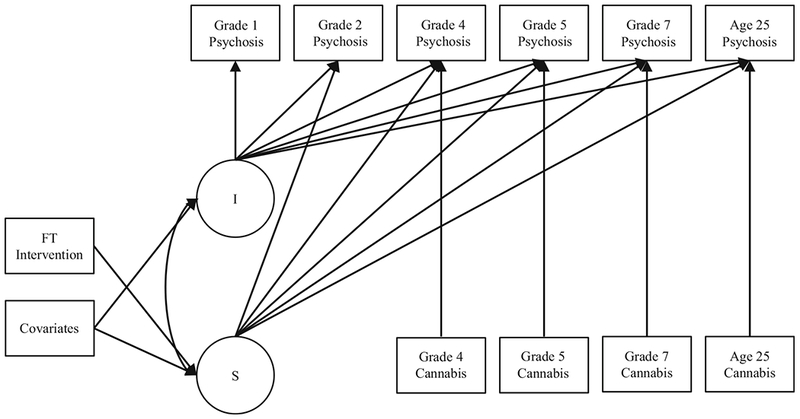
Growth model of psychosis symptoms (grades 1, 2, 4, 5, 7, and age 25) with concurrent cannabis use (grades 4, 5, 7, and age 25), and covariates.
Note: I, intercept; S, slope
Fig. 2.
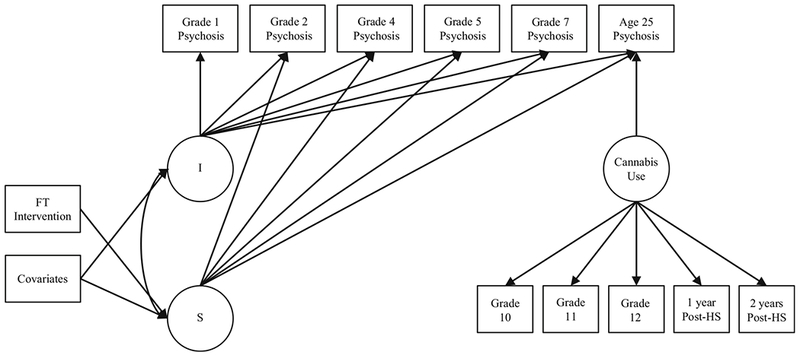
Growth model of psychosis symptoms (grades 1, 2, 4, 5, 7, and age 25) with adolescent cannabis use (grades 10–12, and 2 years post-high school), and covariates.
Note: I, intercept; S, slope; HS, high school
Method
Participants
Participants were from the FT project, a longitudinal, multisite (Durham, North Carolina; Nashville, Tennessee; Seattle, Washington; and rural Pennsylvania) investigation of the development and prevention of child conduct problems (CPPRG 2019). In 1991–1993, 9594 kindergarteners across three cohorts from 55 elementary schools in neighborhoods with high rates of crime and economic disadvantage were screened for classroom conduct problems by teachers using the Teacher Observation of Child Adjustment-Revised Authority Acceptance Score (Werthamer-Larsson et al. 1991). Those scoring in the highest 40% were then screened for home behavior problems by parents using a 22-item instrument based on the CBCL (Achenbach 1991). Teacher and parent scores were standardized within site and summed to yield a severity-of-risk screen score, and children were selected for the study based on this initial risk screening score. This multistage screening procedure identified children for the high-risk sample (control = 446; intervention = 445) and normative sample (n = 387). The present study used data from the intervention and high-risk control samples (N= 891; 69% male; M age = 6.58 years, SD = .48; 51% African American, 47% European American, 2% “other” race). Legal guardians provided consent and participants assented to procedures. Parents were compensated with $75 for completing each of the summer interviews, while teachers were compensated $10/child each year for completing classroom measures. At the age 25 assessment, condition-blinded adults were trained to interview participants in person or via telephone. Participants were paid $100 for the interview. All procedures were approved by the Institutional Review Boards of participating universities.
Intervention
Elementary School Phase (Grades 1–5)
During grades 1–5, intervention families participated in five programs including parent training groups promoting positive family-school relationships and teaching parents behavior management skills, home visits designed to advance parents’ problem-solving skills and life management, child social skill “friendship groups,” child reading tutoring, and child “peer pairing” classroom friendship development. These enrichment programs were held weekly during grade 1, biweekly during grade 2, and monthly during grades 3–5. Further, during grades 1–5, teachers implemented a FT adaptation of the PATHS social emotional learning curriculum (Greenberg et al. 2011) in all classrooms in intervention schools. PATHS addressed social-cognitive skill development to promote social-emotional competence.
Middle and Early High School Phase (Grades 6–10)
Tri-annual assessments were used to design individualized intervention plans that included attention to academic problems, antisocial behavior, social support, and family functioning. During grades 5 and 6, youth participated in a middle school transition program and in parent-youth groups on topics of adolescent development. During grades 7 and 8, youth forums addressed life skills and employment opportunities. Throughout grades 7–10, individualized interventions designed to strengthen protective factors or reduce risk factors in areas of need (e.g., social cognition, academic achievement, parent monitoring) were administered.
Measures
The present study included data collected from the following periods: covariates in kindergarten; psychosis symptoms during grades 1, 2, 4, 5, and 7, and at age 25 years; cannabis use during grades 4, 5, 7, and 10–12, at the 2 years post-high school, and at age 25 years.
Covariates
Measured in kindergarten, covariates included initial risk screen score, cohort, socioeconomic status (SES; M= 24.38; SD= 12.68; Hollingshead 1975), urban/rural status (urban = 74.7%), race (51% African American, 47% European American, 2% “other” race), and sex (male = 69%).
Psychosis Symptoms
Psychosis symptoms was assessed using the 7-item “thought problems” subscale of the parent-report version of the CBCL (Achenbach 1991) during grades 1, 2, 4, 5, and 7, and the ASR (Achenbach 1997) at age 25 years, in line with prior research using these measures (e.g., Simeonova et al. 2014). The 112-item CBCL is comprised of 8 narrow-band scales including aggressive behavior, anxious/depressed, attention problems, delinquent behavior, social problems, somatic complaints, thought problems, and withdrawn. The 132-item ASR is comprised of 10 narrow-band scales including aggressive behavior, anxious/depressed, attention problems, delinquent behavior, externalizing, internalizing, intrusive problems, social problems, somatic complaints, thought problems, and withdrawn. Items are scored on a three-point scale (0 “not true” to 2 “often true”). Internal consistency was adequate for the CBCL (α = .51–.70) and the ASR (α = .74) in the present study.
Cannabis Use
Cannabis use was assessed with different measures at different ages. The self-report Things That You Have Done from the National Youth Survey (Elliot et al. 1985) was administered in grades 4 and 5. The self-report Tobacco, Alcohol, and Drugs Survey from the National Longitudinal Study of Adolescent Health (Bureau of Labor Statistics, US Department of Labor, 2002) assessed cannabis use in grades 7, 10–12, and the 2 years post-high school, and the Tobacco, Alcohol, and Drugs Survey-Version 3 at age 25. The Things That You Have Done measure is comprised of 32 items assessing aggression, stealing, vandalism, and substance use. Items are coded as frequency of event in the past year and only the cannabis use item was used in the present study. The Tobacco, Alcohol, and Drugs Survey is a 57-item instrument assessing tobacco, alcohol, and illegal drug use. The present study included cannabis use over the past 30 days. Items were rated on a 7-point scale (0 “0 days” to 6 “all 30 days”).
Data Analyses
Descriptive statistics were conducted using SPSS version 24 (IBM Corp. 2013); all other analyses were conducted using Mplus 8 (Muthén and Muthén 2017). All models were estimated using full-information likelihood (FIML) to handle missing data (psychosis symptoms: grade 1 = 66.6%, 2 = 8.0%, 4 = 10.9%, 5 = 13.1%, 7 = 16.4%, age 25 = 19.2%; cannabis use: grade 4 = 12.7%, 5 = 14.9%, 7 = 17.2%, 10 = 26.9%, 11 = 28.8%, 12 = 27.3%, 1 year post-high school = 27.6%, 2 years post-high school = 23.9%, age 25 = 22.2%)1 (Rubin and Little 2002). Model fit criteria included chi-square (χ2) value, Root Mean Square Error of Approximation (RMSEA), and Comparative Fit Index (CFI). Models with non-significant χ2 value, RMSEA less than .06, and CFI greater than .90 indicate adequate fit; however, with larger sample sizes as per the present study, a non-significant χ2 value is not necessary (Hu and Bentler 1999). First, an unconditional growth model of psychosis symptoms using Z scores without covariates was fitted to determine the most parsimonious model. We then regressed the intercept and slope of psychosis symptoms onto covariates (i.e., initial risk screen score, cohort, SES, urban/rural status, race, and sex), and slope onto intervention status. Next, we examined whether concurrent cannabis use (i.e., assessed at the same time point) was a significant predictor by adding cannabis use at grades 4, 5, and 7 and at age 25 to the conditional model (Fig. 1). We also examined whether cannabis use in adolescence (i.e., grades 10–12, and the 2 years post-high school) was a significant predictor of age 25 psychosis symptoms modeled with a confirmatory factor analysis (Fig. 2).
Results
Descriptive Statistics
Rates of cannabis use increased through childhood (grade 4 = 0.6%, grade 5 = 1.4%, during the past year; grade 7 = 4.6% during the past 30 days) and adolescence (grade 10 = 16.6%, grade 11 = 17.0%, grade 12 = 23.3%, 1 year post-high school = 21.3%, 2 years post-high school = 19.7%, during the past 30 days) and into adulthood (age 25 = 22.7%, during the past 30 days). Means, standard deviations, and correlations of psychosis symptoms and cannabis use are presented in Table 1. Psychosis symptoms across the years were significantly associated. Cannabis use was significantly associated from grade 10 through age 25, with the exception of grade 10 and 1 year post-high school. Further, grade 1 psychosis symptoms were associated with grade 4 cannabis use; grades 2, 4, 5, and 7 psychosis symptoms were associated with 1 year post-high school cannabis use; and age 25 psychosis symptoms were associated with cannabis use in grades 11 and 12, and at age 25.
Table 1.
Descriptive statistics and correlations between study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | |||||||||||||||
| 1. G1 Psychosis symptoms | 1 | ||||||||||||||
| 2. G2 Psychosis symptoms | .37*** | 1 | |||||||||||||
| 3. G4 Psychosis symptoms | .36*** | .42*** | 1 | ||||||||||||
| 4. G5 Psychosis symptoms | .34*** | .31*** | .44*** | 1 | |||||||||||
| 5. G7 Psychosis symptoms | .18** | .25*** | .36*** | .37*** | 1 | ||||||||||
| 6. Age 25 Psychosis symptoms | .23*** | .14*** | .09* | .18*** | .18*** | 1 | |||||||||
| 7. G4 Cannabis use | .15* | .05 | .06 | .04 | −.02 | .05 | 1 | ||||||||
| 8. G5 Cannabis use | .00 | .02 | .02 | .00 | .00 | .03 | −.00 | 1 | |||||||
| 9. G7 Cannabis use | −.07 | .01 | −.07 | −.01 | .05 | .01 | .00 | .02 | 1 | ||||||
| 10. G10 Cannabis use | −.01 | −.01 | −.07 | .02 | −.01 | .03 | .04 | −.00 | .10* | 1 | |||||
| 11. G11 Cannabis use | .04 | .06 | −.02 | −.01 | .08 | .11* | .15*** | −.01 | .17*** | .31*** | 1 | ||||
| 12. G12 Cannabis use | .10 | .05 | .02 | .05 | .04 | .10* | −.02 | .01 | .04 | .26*** | .43*** | 1 | 1 | ||
| 13. 1 year post-HS Cannabis use | −.05 | .14*** | .10* | .10* | .11** | .02 | −.00 | −.01 | .03 | .04 | .19*** | .24*** | 1 | ||
| 14. 2 years post-HS Cannabis use | −.06 | −.05 | −.02 | −.02 | .01 | .05 | −.01 | −.00 | .15*** | .13** | .15** | .12** | .14** | 1 | |
| 15. Age 25 Cannabis use | .10 | −.01 | −.03 | .07 | −.02 | .14*** | −.02 | .08* | .01 | .11* | .23*** | .24*** | .21*** | .18*** | 1 |
| Descriptives | |||||||||||||||
| M | 1.27 | 1.48 | 1.17 | 1.00 | .96 | 4.66 | .01 | .09 | .27 | 3.40 | 2.47 | 3.26 | 4.04 | 4.01 | 4.01 |
| SD | 1.54 | 1.69 | 160 | 1.45 | 1.47 | 3.37 | .13 | 1.90 | 2.24 | 18.90 | 9.52 | 8.76 | 20.77 | 17.13 | 11.61 |
| Range | 0–10 | 0–11 | 0–10 | 0–11 | 0–10 | 0–20 | 0–3 | 0–52 | 0–40 | 0–299 | 0–100 | 0–50 | 0–420 | 0–300 | 0–120 |
G grade
p < .001
p < .01
p < .05
Growth Model
Unconditional Growth Model
Preliminary unconditional growth curve modeling of psychosis symptoms indicated that the model could not be identified with the inclusion of a quadratic term, and thus, a linear slope factor was specified. This unconditional growth model provided adequate fit to the data (χ2(16) = 45.300, p < .001, CFI = .949, RMSEA = .046, 90% CI [.030, .062]). Statistically significant variance estimates were found for the intercept (σ2 = .448, p < .001) and slope (σ2 = .001, p = .044).
Does the FT Intervention Prevent Later Psychosis Symptoms?
Next, the model was expanded to include covariates and intervention status, and this model provided adequate fit to the data (χ2(49) = 103.384, p < .001, CFI = .918, RMSEA = .036, 90% CI [.026, .046]). The initial risk screen score was significantly positively associated with intercept of psychosis symptoms (β = .231, B(SE) = .155(.029), p < .001), and SES was significantly negatively associated with intercept of psychosis symptoms (β = – .155, B(SE) = – .008(.002), p <.001). Intervention status was not significantly associated with the slope of psychosis symptoms; however, it approached significance (β = – .108, B(SE) = – .008(.004), p = .071).
Does the FT Intervention Prevent Later Psychosis Symptoms Controlling for Cannabis Use?
Next, we added concurrent cannabis use (i.e., assessed at the same time point) to the model (see Fig. 1); this model provided adequate fit to the data (χ2(69) = 113.033, p < .001, CFI = .913, RMSEA = .034, 90% CI [.022, .045]). Cannabis use was positively associated with psychosis symptoms at age 25 (β = .125, B(SE) = .010(.003), p = .002). With concurrent cannabis use included in the model, sex was significantly associated with the slope of psychosis symptoms; that is, male participants reported greater psychosis behavior over time (β = .277, B(SE) = .016(.007), p = .017). Further, intervention status was significantly negatively associated with the slope of psychosis symptoms (β = – .240, B(SE) = – .013(.005), p = .005), such that, after controlling for concurrent cannabis use, intervention participants reported lower levels psychosis symptoms over time.
Finally, we examined whether the FT intervention prevented later psychosis symptoms after controlling for adolescent cannabis use. First, we examined cannabis use during grades 10–12 and 2 years post-high school, with an unconditional confirmatory factor analysis, which provided adequate fit to the data (χ2(5) = 20.90, p <. 001, CFI = .940, RMSEA = .063, 90% CI [.037, .093]). This model was expanded to include covariates and intervention status (see Fig. 2) and it provided adequate fit to the data (χ2(123) = 223.796, p < .001, CFI = .897, RMSEA = .031, 90% CI [.024, .037]). Adolescent cannabis use was positively associated with psychosis symptoms at age 25 (β = .108, B(SE) = .011(.005), p = .024). Further, intervention status on the slope of psychosis symptoms approached significance (β = – .112, B(SE) = – .008(.004), p = .063).
Discussion
The present study examined whether the FT intervention reduced risk for psychosis symptoms through childhood and adolescence and into early adulthood. The multicomponent FT preventive intervention was not designed to target psychosis symptoms; however, present findings showed that receiving this intensive early intervention mitigated self-reported psychosis symptoms, but only when controlling for concurrent cannabis use. Our findings add to a dearth of research examining psychosis symptoms in childhood—an important avenue of research given the recent addition of APS in the DSM-5. Present findings support past research demonstrating that early preventive interventions can have unanticipated beneficial cross-over effects on later development. Mechanisms through which the FT intervention may have reduced psychosis symptoms include reducing stress within the home through parent training groups and FT staff home visits, and the development of child social-cognitive skills through friendship groups, peer pairing, and the PATHS social emotional learning curriculum. These are discussed further below.
The link between experiences of stress and the development of psychosis symptoms has long been noted; however, one recent line of research suggests that dysregulated emotion in the form of hypersensitivity to stress is an endophenotype for the development of psychosis (Myin-Germeys and van Os 2007). This “affective pathway to psychosis” purports that experiences of stress, often in the form of trauma, dysregulate the hypothalamic-pituitary-adrenal (HPA) axis and alter dopamine transmission, which is linked to increased emotional reactivity and positive symptoms of psychosis (e.g., delusions, hallucinations). The FT intervention focused on several avenues for reducing stress in the home and increasing emotion regulation skills. Within the context of the family, parents were provided training groups that taught behavior management skills to promote positive parent-child interactions and FT staff conducted home visits for the purpose of increasing parents’ problem-solving and life management skills. These aspects of the FT intervention were designed to foster a stable and nurturing home environment. Recent findings from the FT intervention sample showed that the intervention decreased parental harsh punishment and increased parental warmth which, in turn, decreased conduct disorder and callous-unemotional traits (i.e., lack of guilt, empathy, and deficient affect), respectively, in early adolescence (Pasalich et al. 2016). Thus, the present findings support recent meta-analytic studies pointing to the efficacy of family therapy for the treatment of psychosis symptoms (e.g., Stafford et al. 2013). Future research should examine whether parenting behaviors mediate the effect between early prevention interventions and later psychosis symptoms.
The FT intervention was designed with the aim of reducing conduct problems (e.g., aggression, destructive behavior, deceitfulness) by developing social and emotional skills. Longitudinal studies have linked antisocial behavior with psychosis symptoms (Bor et al. 2010; Reef et al. 2010). Another hypothesis for the development of psychosis symptoms is due to cognitive and social impairments (Garety et al. 2007). Garety and colleagues posited a cognitive-affective framework for the development of psychosis symptoms, and particularly positive symptoms. Among predisposed individuals, triggering events (e.g., trauma) disrupt cognitive and affective processes; these cognitive processes include biased conscious experiences and schemas of oneself and others, prompting externalizing appraisals (i.e., positive symptoms) that are worsened by a negative emotional state. Children in the intervention condition participated in “friendship groups” and an adapted PATHS curriculum, which aimed to promote social-cognitive skills. By ameliorating maladaptive cognitive, affective, and social states, the FT intervention may have indirectly reduced the prevalence of psychosis symptoms; however, unfortunately it is not possible to ascertain which components of the FT intervention may have contributed to present findings. Thus, an important line for future research would be to examine, like parenting behaviors, whether child social-cognitive skills also mediates the effect between participation in a comprehensive prevention intervention and the development of later psychosis symptoms.
One of the strongest risk factors for the development of psychosis is cannabis use. The present findings add to the research base that cannabis is associated with psychosis symptoms. Only after controlling for cannabis use was the FT intervention significantly associated with reduced psychosis symptoms. Extensive research has linked cannabis use to psychosis; however, there is still some debate about whether cannabis use and psychosis symptoms simply have a shared etiology or whether there is a direct causal relationship between these two factors. Recent evidence has provided further support for a temporal relationship between cannabis use in the 5 years prior to symptom onset (Kelley et al. 2016), which perhaps explains why we did not find a significant effect when controlling for adolescent cannabis use (i.e., age 15–20 years old). Future research should continue to examine this association given recent policy moves to change the legality of cannabis use in several countries.
The present findings must be considered within the context of several study limitations. First, our growth model included two measures of psychosis symptoms, with the CBCL assessing psychosis symptoms during grades 1, 2, 4, 5, and 7, and the ASR assessing psychosis symptoms at age 25. These measures have a different number of items on the “thought problems” subscale; however, we used Z scores in the growth model to address this methodological issue. Third, our measure of cannabis use assessed frequency of use in the past year during grades 4 and 5, and frequency of use in the past 30 days during grades 7–13 and at age 25. Thus, further longitudinal research should examine the impact of early interventions targeting antisocial behavior for the development of psychosis symptoms taking into account these methodological issues.
Present findings have important clinical implications, such that intensive multimodal early interventions may have unexpected beneficial effects for healthy development. The FT preventive intervention was guided by developmental theory that posits that there are multiple influences for the development of behavior. Although it was not designed to target psychosis symptoms, through its multicomponent approach the FT intervention reduced adult symptoms of psychosis when controlling for concurrent cannabis use. Through decreasing stress within the home and increasing emotion regulation and social-cognitive skills, interventions may indirectly reduce symptoms associated with a range of psychotic disorders. Psychotic disorders are associated with significant deficits in functioning and research shows that the longer the duration of untreated psychotic symptoms, the poorer the response to treatment across several domains (Marshall et al. 2005; Perkins et al. 2005). Thus, early comprehensive preventive measures may prove beneficial for long-term outcomes associated with psychotic disorders.
Acknowledgments
Members of the Conduct Problems Prevention Research Group, in alphabetical order, are Karen L. Bierman, Pennsylvania State University; John D. Coie, Duke University; D. Max Crowley, Pennsylvania State University; Kenneth A. Dodge, Duke University; Mark T. Greenberg, Pennsylvania State University; John E. Lochman, University of Alabama; Robert J. McMahon, Simon Fraser University and B.C. Children’s Hospital Research Institute; and Ellen E. Pinderhughes, Tufts University.
We are grateful for the collaboration of the Durham Public Schools, the Metropolitan Nashville Public Schools, the Bellefonte Area Schools, the Tyrone Area Schools, the Mifflin County Schools, the Highline Public Schools, and the Seattle Public Schools. We appreciate the hard work and dedication of the many staff members who implemented the project, collected the evaluation data, and assisted with data management and analyses.
Funding Information The Fast Track project has been supported by National Institute of Mental Health (NIMH) Grants R18MH48043, R18MH50951, R18MH50952, R18MH50953, R01MH062988, K05MH00797, and K05MH01027; National Institute on Drug Abuse (NIDA) Grants R01DA016903, K05DA15226, RC1DA028248, and P30DA023026; National Institute of Child Health and Human Development Grant R01HD093651; and Department of Education Grant S184U30002. The Center for Substance Abuse Prevention also provided support through a memorandum of agreement with the NIMH. Additional support for this study was provided by a B.C. Children’s Hospital Research Institute Investigator Grant Award and a Canada Foundation for Innovation Award to Robert J. McMahon.
Footnotes
Conflict of Interest Drs. Bierman, Coie, Dodge, Greenberg, Lochman, McMahon, and Pinderhughes are the Principal Investigators on the Fast Track Project and have a publishing agreement with Guilford Publications, Inc. Royalties from that agreement will be donated to a professional organization. They are also authors of the PATHS curriculum and donate all royalties from Channing-Bete, Inc. to a professional organization. Dr. Greenberg is a developer of the PATHS curriculum and has a separate royalty agreement with Channing-Bete, Inc. Bierman, Coie, Dodge, Greenberg, Lochman, and McMahon are the developers of the Fast Track curriculum and have publishing and royalty agreements with Guilford Publications, Inc. Dr. McMahon is a coauthor of Helping the Noncompliant Child and has a royalty agreement with Guilford Publications, Inc.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants in the study.
Analyses were repeated with grade 1 removed and findings remained the same with the exception of the final model (i.e., whether the FT intervention prevented later psychosis symptoms after controlling for adolescent cannabis use), which no longer provided adequate fit to the data (χ2(104) = 649.879, p < .001, CFI = .382, RMSEA = .078, 90% CI [.072, .084]).
References
- Achenbach TM (1991). Manual for the Child Behavior Checklist. Burlington, VT: University of Vermont, Department of Psychiatry. [Google Scholar]
- Achenbach TM (1997). Manual for the Young Adult Self-Report and Young Adult Behavior Checklist. Burlington, VT: University of Vermont Department of Psychiatry. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Bagot KS, Milin R, & Kaminer Y (2015). Adolescent initiation of cannabis use and early onset psychosis. Substance Abuse, 36, 524–533. 10.1080/08897077.2014.995332. [DOI] [PubMed] [Google Scholar]
- Bierman KL, Greenberg MT, Coie JD, Dodge KA, Lochman JE, & McMahon RJ (2017). Social and emotional skills training for children: The Fast Track Friendship Group Manual. New York, NY: Guilford Press. [Google Scholar]
- Bor W, McGee TR, Hayatbakhsh R, Dean A, & Najman JM (2010). Do antisocial females exhibit poor outcomes in adulthood? An Australian cohort study. Australian & New Zealand Journal of Psychiatry, 44, 648–657. 10.3109/00048671003631159. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics, US Department of Labor (2002). National Longitudinal Survey of Youth 1997 Cohort, 1997–2001. Washington, DC: US Department of Labor, Bureau of Labor Statistics. [Google Scholar]
- Conduct Problems Prevention Research Group. (2019). The Fast Track program for children at risk: Preventing antisocial behavior. New York: Guilford Press (in press). [Google Scholar]
- Davies C, Cipriani A, Ioannidis JP, Radua J, Stahl D, Provenzani U, et al. (2018). Lack of evidence to favor specific preventive interventions in psychosis: A network meta-analysis. World Psychiatry, 17, 196–209. 10.1002/wps.20526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodge KA, Godwin J, & the Conduct Problems Prevention Research Group. (2013). Social-information-processing patterns mediate the impact of preventive intervention on adolescent antisocial behavior. Psychological Science, 24, 456–465. 10.1177/0956797612457394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodge KA, Bierman KL, Coie JD, Greenberg MT, Lochman JE, McMahon RJ, & Pinderhughes EE (2015). Impact of early intervention on psychopathology, crime, and well-being at age 25. American Journal of Psychiatry, 172, 59–70. 10.1176/appi.ajp.2014.13060786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliot DS, Ageton SS, & Huizinga D (1985). Explaining delinquency and drug use. Beverly Hills, CA: Siegel. [Google Scholar]
- Garety PA, Bebbington P, Fowler D, Freeman D, & Kuipers E (2007). Implications for neurobiological research of cognitive models of psychosis: A theoretical paper. Psychological Medicine, 37, 1377–1391. 10.1017/S003329170700013X. [DOI] [PubMed] [Google Scholar]
- Green MF, Penn DL, Bentall R, Carpenter WT, Gaebel W, Gur RC, et al. (2008). Social cognition in schizophrenia: An NIMH workshop on definitions, assessment, and research opportunities. Schizophrenia Bulletin, 34, 1211–1220. 10.1093/schbul/sbm145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg MT, Kusche CA, & the Conduct Problems Prevention Research Group. (2011). Grade level PATHS Curriculum. South Deerfield, MA: Channing-Bete. [Google Scholar]
- Hollingshead AB (1975). Four factor index of social status. New Haven, CT: Yale University. Unpublished manuscript [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. 10.1080/10705519909540118. [DOI] [Google Scholar]
- IBM Corp. Released. (2013). IBM SPSS Statistics for Windows, Version 22.0. IBM Corp: Armonk, NY. [Google Scholar]
- Jepsen JRM, Fagerlund B, Pagsberg AK, Christensen AMR, Hilker RW, Nordentoft M, & Mortensen EL (2010a). Course of intelligence deficits in early onset, first episode schizophrenia: A controlled, 5-year longitudinal study. European Child & Adolescent Psychiatry, 19,341–351. 10.1007/s00787-009-0053-4. [DOI] [PubMed] [Google Scholar]
- Jepsen JRM, Fagerlund B, Pagsberg AK, Christensen AMR, Nordentoft M, & Mortensen EL (2010b). Deficient maturation of aspects of attention and executive functions in early onset schizophrenia. European Child & Adolescent Psychiatry, 19, 773–786. 10.1007/s00787-010-0126-4. [DOI] [PubMed] [Google Scholar]
- Kelley ME, Wan CR, Broussard B, Crisafio A, Cristofaro S, Johnson S, et al. (2016). Marijuana use in the immediate 5-year premorbid period is associated with increased risk of onset of schizophrenia and related psychotic disorders. Schizophrenia Research, 171, 62–67. 10.1016/j.schres.2016.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HS, Shin NY, Jang JH, Kim E, Shim G, Park HY, et al. (2011). Social cognition and neurocognition as predictors of conversion to psychosis in individuals at ultra-high risk. Schizophrenia Research, 130, 170–175. 10.1016/j.schres.2011.04.023. [DOI] [PubMed] [Google Scholar]
- Laruelle M (2000). The role of endogenous sensitization in the pathophysiology of schizophrenia: Implications from recent brain imaging studies. Brain Research Reviews, 31, 371–384. 10.1016/S0165-0173(99)00054-5. [DOI] [PubMed] [Google Scholar]
- Lee TY, Hong SB, Shin NY, & Kwon JS (2015). Social cognitive functioning in prodromal psychosis: A meta-analysis. Schizophrenia Research, 164, 28–34. https://doi.org/10.1016Zj.schres.2015.02.008. [DOI] [PubMed] [Google Scholar]
- Marshall M, Lewis S, Lockwood A, Drake R, Jones P, & Croudace T (2005). Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: A systematic review. Archives of General Psychiatry, 62, 975–983. 10.1001/archpsyc.62.9.975. [DOI] [PubMed] [Google Scholar]
- McGorry PD, Yung AR, Phillips LJ, Yuen HP, Francey S, Cosgrave EM, et al. (2002). Randomized controlled trial of interventions designed to reduce the risk of progression to first-episode psychosis in a clinical sample with subthreshold symptoms. Archives of General Psychiatry, 59, 921–928. 10.1001/archpsyc.59.10.921. [DOI] [PubMed] [Google Scholar]
- Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, & Lewis G (2007). Cannabis use and risk of psychotic or affective mental health outcomes: A systematic review. The Lancet, 370, 319–328. 10.1016/S0140-6736(07)61162-3. [DOI] [PubMed] [Google Scholar]
- Morrison AP, Stewart SL, French P, Bentall RP, Birchwood M, Byrne R, et al. (2011). Early detection and intervention evaluation for people at high-risk of psychosis-2 (EDIE-2): Trial rationale, design and baseline characteristics. Early Intervention in Psychiatry, 5, 24–32. 10.1111/j.1751-7893.2010.00254.x. [DOI] [PubMed] [Google Scholar]
- Morrison AP, French P, Stewart SL, Birchwood M, Fowler D, Gumley AI, et al. (2012). Early detection and intervention evaluation for people at risk of psychosis: Multisite randomised controlled trial. BMJ, 344, e2233 10.1136/bmj.e2233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén BO, & Muthén LK (2017). Mplus Version 8: User’s guide. Los Angeles, CA: Authors. [Google Scholar]
- Myin-Germeys I, & van Os J (2007). Stress-reactivity in psychosis: Evidence for an affective pathway to psychosis. Clinical Psychology Review, 27, 409–24. 10.1016/jxpr.206.09.005. [DOI] [PubMed] [Google Scholar]
- National Institute for Clinical Excellence (NICE). (2009). The NICE guideline on core interventions in the treatment and management of schizophrenia in adults in primary and secondary care—Updated edition. London, U.K.: Author. [Google Scholar]
- Oh H, & Devylder J (2017). Cannabis and psychotic experiences. Addiction, 112, 1688–1689. 10.1111/add.13885. [DOI] [PubMed] [Google Scholar]
- Pasalich DS, Witkiewitz K, McMahon RJ, Pinderhughes EE, & Conduct Problems Prevention Research Group. (2016). Indirect effects of the Fast Track intervention on conduct disorder symptoms and callous-unemotional traits: Distinct pathways involving discipline and warmth. Journal of Abnormal Child Psychology, 44, 587–597. 10.1007/s10802-015-0059-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson GR, Forgatch MS, & DeGarmo DS (2010). Cascading effects following intervention. Development and Psychopathology, 22, 949–970. 10.1017/S0954579410000568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins DO, Gu H, Boteva K, & Lieberman JA (2005). Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: A critical review and meta-analysis. American Journal of Psychiatry, 162, 1785–1804. 10.1176/appi.ajp.162.10.1785. [DOI] [PubMed] [Google Scholar]
- Poulton R, Van Ryzin MJ, Harold GT, Chamberlain P, Fowler D, Cannon M, et al. (2014). Effects of Multidimensional Treatment Foster Care on psychotic symptoms in girls. Journal of the American Academy of Child & Adolescent Psychiatry, 53, 1279–1287. 10.1016/jjaac.2014.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read J, & Argyle N (1999). Hallucinations, delusions, and thought disorder among adult psychiatric inpatients with a history of child abuse. Psychiatric Services, 50, 1467–1472. 10.1176/ps.50.11.1467. [DOI] [PubMed] [Google Scholar]
- Read J, Agar K, Argyle N, & Aderhold V (2003). Sexual and physical abuse during childhood and adulthood as predictors of hallucinations, delusions and thought disorder. Psychology and Psychotherapy: Theory, Research and Practice, 76, 1–22. 10.1348/14760830260569210. [DOI] [PubMed] [Google Scholar]
- Reef J, Diamantopoulou S, van Meurs I, Verhulst F, & van der Ende J (2010). Predicting adult emotional and behavioral problems from externalizing problem trajectories in a 24-year longitudinal study. European Child & Adolescent Psychiatry, 19, 577–585. 10.1007/s00787-010-0088-6. [DOI] [PubMed] [Google Scholar]
- Reider EE, Robertson EB, & Sims BE (2014). Does early intervention prevent health risking sexual behaviors related to HIV/AIDS? Prevention Science, 15, 1–5. 10.1007/s11121-013-0455-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross CA, Anderson G, & Clark P (1994). Childhood abuse and the positive symptoms of schizophrenia. Psychiatric Services, 45, 489–491. 10.1176/ps.45.5.489. [DOI] [PubMed] [Google Scholar]
- Rubin DB, & Little RJ (2002). Statistical analysis with missing data. Hoboken, NJ: Wiley. [Google Scholar]
- Savla GN, Vella L, Armstrong CC, Penn DL, & Twamley EW (2012). Deficits in domains of social cognition in schizophrenia: A meta-analysis of the empirical evidence. Schizophrenia Bulletin, 39, 979–992. 10.1093/schbul/sbs080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simeonova DI, Attalla A, Trotman H, Esterberg M, & Walker EF (2011). Does a parent-report measure of behavioral problems enhance prediction of conversion to psychosis in clinical high-risk adolescents? Schizophrenia Research, 130, 157–163. 10.1016/j.schres.2011.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simeonova DI, Nguyen T, & Walker EF (2014). Psychosis risk screening in clinical high-risk adolescents: A longitudinal investigation using the Child Behavior Checklist. Schizophrenia Research, 159, 7–13. https://doi.org/10.1016zj.schres.2014.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stafford MR, Jackson H, Mayo-Wilson E, Morrison AP, & Kendall T (2013). Early interventions to prevent psychosis: Systematic review and meta-analysis. BMJ, 346, f185 10.1136/bmj.f185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ujike H (2002). Stimulant-induced psychosis and schizophrenia: The role of sensitization. Current Psychiatry Reports, 4, 177–184. 10.1007/s11920-002-0024-7. [DOI] [PubMed] [Google Scholar]
- van der Gaag M, van den Berg D, & Ising H (2017). CBT in the prevention of psychosis and other severe mental disorders in patients with an at risk mental state: A review and proposed next steps. Schizophrenia Research. 10.1016/j.schres.2017.08.018. [DOI] [PubMed] [Google Scholar]
- Vourdas A, Pipe R, Corrigall R, & Frangou S (2003). Increased developmental deviance and premorbid dysfunction in early onset schizophrenia. Schizophrenia Research, 62, 13–22. 10.1016/S0920-9964(02)00429-2. [DOI] [PubMed] [Google Scholar]
- Werthamer-Larsson L, Kellam S, & Wheeler L (1991). Effect of first-grade classroom environment on shy behavior, aggressive behavior, and concentration problems. American Journal of Community Psychology, 19, 585–602. 10.1007/BF00937993. [DOI] [PubMed] [Google Scholar]
- Wu LT, Brady KT, Mannelli P, Killeen TK, & Workgroup NIDAAAPI (2014). Cannabis use disorders are comparatively prevalent among nonwhite racial/ethnic groups and adolescents: A national study. Journal of Psychiatric Research, 50, 26–35. 10.1016/jpsychires.2013.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yung AR, & Nelson B (2013). The ultra-high risk concept—A review. The Canadian Journal of Psychiatry, 58, 5–12. 10.1177/070674371305800103. [DOI] [PubMed] [Google Scholar]


