Abstract
Objective:
Our goal was to evaluate knowledge and testing preferences for Chlamydia trachomatis (CT) Neisseria gonorrhoeae (NG), and Trichomonas vaginalis (TV) infections.
Participants:
We surveyed female undergraduates attending the University of California, Los Angeles, in May 2017.
Methods:
Using an online survey, we collected demographic information and information on 793 participants’ health care seeking behavior, sexual activity, sexually transmitted infection (STI) knowledge, and STI screening preferences. We used conjoint analysis to evaluate testing preferences of hypothetical STI tests.
Results:
On knowledge questions of CT and NG infections, 193 (27.7%) participants scored >80% correct. Cost had the largest impact on willingness to use a hypothetical STI test, accounting for 41.5% of preference, followed by specimen type (17.4%), and location of testing (16.4%).
Conclusions:
Knowledge regarding STIs was low. Educational programs implemented through the university health center might increase testing rates. A free, urine-based, home STI test may be desirable for undergraduate females.
Keywords: Conjoint analysis, Chlamydia trachomatis, Neisseria gonorrhoeae, Trichomonas vaginalis, testing, knowledge
Chlamydia trachomatis (CT), Neisseria gonorrhoeae (NG), and Trichomonas vaginalis (TV) are common infections that disproportionately affect individuals aged 15–24 years. Even though both men and women are affected by sexually transmitted infections (STIs), young women can face serious long-term health consequences and infertility due to untreated STIs.1 Currently, the Centers for Disease Control and Prevention recommend annual screening for CT and NG in sexually active women under the age of 25 years.1 However, many young women are not screened regularly.2 Studies have revealed that STI positivity among college females may actually be higher than previously believed compared with the general age-matched population.3 Younger students may also be more likely to be infected than older students.4 As STI rates continue to rise in the United States, greater understanding about the cause of the high infection rates and low screening rates among adolescents is needed.
Increasing knowledge of STIs on college campuses may increase uptake of screening services, therefore helping to increase case findings of CT, NG, and TV infections. Prior studies have explored undergraduate knowledge of STIs in university settings outside of the United States.5–8 One study investigating sexual behavior and knowledge about STIs among undergraduate students in São Paulo, Brazil, revealed limited knowledge about the sexual transmissibility of common STIs including CT and TV.6 Additionally, at Birmingham University in England, a survey was conducted regarding knowledge about CT infection, including its transmission and screening practices. Overall knowledge scores revealed student misconceptions about CT infection and researchers recommended increasing both overall knowledge and knowledge about the screening services offered.8
In the United States, a previous study found that around 20% of adolescents believed STIs were only transmissible with symptoms, and around 25% were unaware that STIs could cause infertility.9 Those findings are consistent with other studies revealing serious limitations in STI knowledge.10,11 A previous study found that knowledge about STIs motivated adolescents to seek STI testing, and those adolescents also reported a desire for greater STI knowledge as they believed it would lead to increases in their own testing practices.12 Those findings support a connection between STI knowledge and testing.
Along with increasing knowledge, point of care (POC) testing, which occurs at the clinic or location where care is given, may help increase testing. POC testing offers the possibility for more widespread access and availability of testing for STIs and can reduce the need for follow up visits, thus reducing cost and burden of multiple clinic visits for patients.13,14 Furthermore, a study at Pennsylvania State University shows that self-testing programs may be an effective way to test at-risk males and females as well as identify asymptomatic cases.15 However, even with greater availability and participant interest for self-testing, one’s intention to use a test may not always translate into action.16 Conjoint analysis is a method used in market-based research to assess acceptability of hypothetical products with varying attributes and attribute values that can allow for estimation of features that are most important to the consumers. An acceptable test, by determining preferable attributes and identifying potential barriers to testing, is important for future efforts to increase the testing and treatment of STIs. Since tradeoffs of specific product attributes must be made when creating rapid tests, conjoint analysis can help identify which attributes are most important.
This study aimed to evaluate knowledge of CT, NG, and TV infections among female undergraduates at the University of California, Los Angeles (UCLA), along with current screening behavior. Additionally, we assessed preferences for STI testing to determine test attributes most associated with willingness to test for CT, NG, and TV infections.
Methods
Study population and data collection
We aimed to conduct a representative survey of female undergraduate students at UCLA. We worked with the UCLA Registrar office to determine a method for distributing an online survey link to students and create a sample population. The UCLA Registrar office created a list of 5,000 randomly selected female students (out of the 17,512 total female students enrolled at UCLA17). We selected a sample size of 5,000 to have adequate power to provide precise estimates of knowledge measures based on a response rate of approximately 15%. Participants were eligible to receive the link if they were full-time undergraduate female students attending UCLA in Spring 2017 as registered by the UCLA Registrar office. In May 2017, the Registrar sent out the survey request twice, 2 weeks apart, to the same population to increase the response rate. In the email, participants were informed on the purpose of the study, what would be asked of them if they chose to participate, and on the confidentiality of the results. We incentivized participation using a lottery system which participants could enter to win an Amazon gift card (one worth $50 and ten worth $25). Participants were asked to respond to each question but were not required to answer all questions, thus statistics are calculated per question among those that responded.
Measures
In the survey, participants were first asked to provide their age, year in school, ethnicity, use of the student health center on campus, sexual activity (ie, currently are, or have ever been sexually active), and testing history of the three infections (ie, have previously tested for the infections). Participant knowledge of CT, NG, and TV infections was assessed through a series of survey questions based on the California Women’s Health Survey11 and a survey which was created through literature reviews and a pilot study.8 The survey asked questions regarding testing, treatment, and effects of the three infections (eg, CT is only transmitted by vaginal sex? CT can be treated with antibiotics? Most individuals with CT do not display symptoms?). Participants could select “True,” “False,” or “I don’t know” as an answer choice and were not required to answer any question. Answer choices of “I don’t know” were considered incorrect during analysis.
Participants were further asked to rate their likelihood of using eight hypothetical STI tests for chlamydia, gonorrhea, and trichomoniasis that varied in five attributes. The five test attributes included cost (free vs. $20), collection method (urine vs. vaginal swab), time of results (20min vs. 3 days), test location (clinic vs. home), or number of tests (one test vs. three tests). Scenarios for the tests were created which described all possible combinations of attributes. The scenarios were then reduced to eight hypothetical tests using fractional factorial design.18 For example, the question describing one of the hypothetical tests asks participants how likely they would be to test for chlamydia, gonorrhea, and trichomoniasis if the test: requires a sample that is collected using a small amount of urine in a cup, is free, will provide the results of this diagnosis in 3 days, will be performed in a clinic or in a clinic’s laboratory, and each of the three infections will be tested separately (requiring three tests total) [full conjoint survey questions included in supplemental material]. That conjoint survey design with eight hypothetical test profiles is 100% efficient, balanced and orthogonal. Participants were asked to select how likely they would be to use each test on a 5-point Likert scale ranging from highly unlikely (1) to highly likely (5).
Statistical analyses
Descriptive statistics were used to summarize the demographic characteristics and knowledge of infections as well as sexual history and STI testing history using mean values, standard deviation, and percentages. To assess differences in the distribution of those characteristics and knowledge responses between sexually active and nonsexually active individuals, we used t-tests for continuous variables (eg, age, knowledge scores) and Fisher’s exact test and chi-square tests for categorical variables (eg, knowledge category and race/ethnicity). We performed both univariable and multivariable logistical regression to examine associations between knowledge and prior STI testing as well as analyze the participants who scored ≥ 80% correct on knowledge questions for CT and NG infections. To assess the association and interaction between STI knowledge and sexual activity on the STI testing history, the multivariable logistic regression model was used to estimate odds ratios (ORs) and 95% confidence intervals (CIs). We controlled for race/ethnicity and year in education to reduce the potential confounding effects from these variables.19
To evaluate STI knowledge, a score was created based on the 23 knowledge-related questions from the survey. Each question was equally scored and multiple-choice questions were scored one point if all correct answers were selected and no incorrect answer was selected (eg, a diagnostic method question). The STI knowledge score was classified into four categories using quartiles as a cutoff. Participant knowledge of the three STIs was also assessed by determining the proportion of participants within each category (year in school, ethnicity, sexual activity, and testing history) who scored ≥80% correct on the knowledge questions. A score of 80% was classified as sufficient knowledge based on usual academic standards equaling a “B-” or better and has been used in previous studies assessing knowledge.20 In addition, a score of 80% represents the rounded value for the top interquartile range. We further calculated the ORs of the association between STI testing history and knowledge score categories (≤ 10; 11–13; 14–16; 17–23 questions answered correctly). The association was modified by sexually active status. We additionally compared the ethnicities of our study population to that of the overall UCA female undergraduate population.
To determine the importance of each attribute, we used metric conjoint analysis.21 Ratings of preference on the 5-point Likert scale were then converted to a 100-point preference score using multiplication where higher scores imply an increased willingness to use the test. Participant data were excluded for the conjoint survey if participants did not answer one or more of the conjoint survey questions or if they provided the same Likert preference scale value for all eight hypothetical test profiles. We calculated part-worth utility values for each level of attribute by scaling the values to an arbitrary constant within each attribute and scaling all attributes to zero. Part-worth utility values measure how much attribute and level influenced the participants’ willingness to test. To characterize relative importance, we analyzed how each attribute could affect the total utility. Attributes with the largest part-worth utility range are considered the most important in predicting preference. The conjoint analysis model was fit separately for each participant using the main-effects analysis of variance with attributes as independent variables, the participant ratings as the dependent variable and the part-worth utilities represented by the b terms. We then calculated the attribute importance using the percentages from relative ranges in the attribute’s utility values. Results were summarized across participants and averages were reported.
All data analyses were conducted using SAS software v9.4 (Cary, NC).
Ethical consideration
The UCLA Institutional Review Board approved the study under application #17–000404. Informed consent was obtained from all participants at the start of the online survey.
Results
Of the 5,000 participants who received the survey link, 793 (15.9%) responded. Demographic information, health care seeking behavior, sexual activity, and prior testing history for the participants is provided in Table 1. Our sample had slightly younger participants (mean age 20.6 vs. 21.4years), more first year students (32.9% vs. 17.0%), more Latinas (27.6% vs. 23.0%), fewer Blacks (3.4% vs. 7.2%), and Asian or Pacific Islanders (36.2% vs. 41.1%) than the overall UCLA female undergraduate population. However, except for year in school, the absolute differences were less than 5%.
Table 1.
Select characteristics, including demographic information, sexual activity, and history of Chlamydia trachomatis (CT), Neisseria gonorrhoeae (NG), and Trichomonas vaginalis (TV) infection among female undergraduate participants attending the University of California, Los Angeles, 2017.
| Demographics | % (n) | ||
|---|---|---|---|
| Participants | 793 | ||
| Age, years | |||
| Mean, ± SD | 20.3 (SD = ±2.7) | ||
| Year in University | |||
| 1st | 32.1% (224) | ||
| 2nd | 20.4% (142) | ||
| 3rd | 26.0% (181) | ||
| 4th | 19.1% (133) | ||
| 5+ | 2.4% (17) | ||
| Latina ethnicity | 27.1% (189) | ||
| Origin | |||
| White or Caucasian | 36.3% (233) | ||
| Black or African American | 2.7% (17) | ||
| Asian or Asian American | 35.9% (230) | ||
| American Indian, Alaska Native, Native Hawaiian or other Pacific Islander | 2.5% (16) | ||
| Mixed | 8.9% (57) | ||
| Unavailable/Unknown | 8.0% (51) | ||
| Decline to answer | 5.8% (37) | ||
| Has visited the university health center before | 81.5% (568) | ||
| Been sexually active? | |||
| Yes | 68.1% (474) | ||
| No | 30.0% (209) | ||
| Choose not to answer | 1.9% (13) | ||
| Sexually Active | Not Sexually Active | ||
| Has been tested for CT infection | 42.2% (288) | 1.3% (9) | |
| Has been tested for NG infection | 37.9% (259) | 0.7% (5) | |
| Has been tested for TV infection | 8.4% (57) | 0 | |
| Has tested positive for CT infection | 4.5% (29) | 0 | |
| Has tested positive for NG infection | 0.2% (1) | 0 | |
| Has tested positive for TV infection | 0 | 0 | |
Note. SD = standard deviation; n = the number of participants who selected the answer.
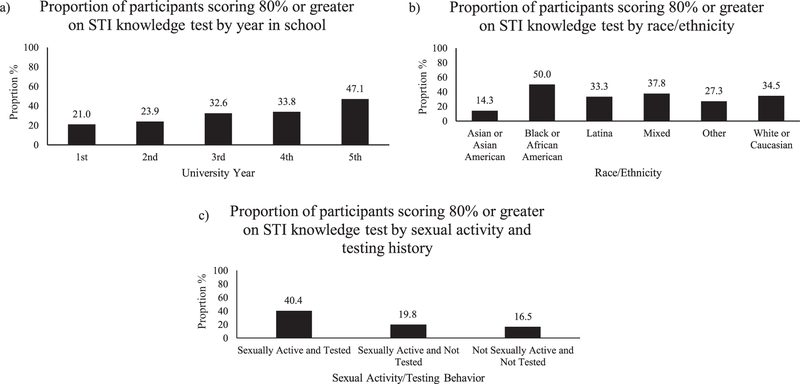
Participant responses regarding knowledge about the diagnostics, symptoms, and treatment of the infections are shown in Table 2. Of the 698 (88.0%) participants who responded to all 23 knowledge questions, only 25 (3.6%) scored ≥ 80% correct. On knowledge questions of only CT and NG infections, 193 (27.7%) participants scored ≥ 80% correct. Figure 1 shows the proportion of participants in categories (year in school, ethnicity, sexual activity/STI testing history) who scored ≥ 80% on the knowledge questions for CT and NG. Participants in a later year in university appeared to have increased STI knowledge as students in university year five or greater had the highest odds of scoring ≥80% compared with first year students (OR: 3.35, 95% CI 1.23, 9.15). Additionally, sexually active participants who had been tested for either CT, NG, or TV were more likely to score ≥ 80% compared with nonsexually active participants who had not been tested (OR: 3.43, 95% CI 2.21, 5.33). There was a similar proportion of participants who were sexually active who had not been tested previously that scored ≥ 80% on the knowledge test (19.8%) compared with nonsexually active participants who had not been tested (16.5%) (OR: 1.25, 95% CI .74, 2.1).
Table 2.
Knowledge of Chlamydia trachomatis (CT), Neisseria gonorrhoeae (NG), and Trichomonas vaginalis (TV) infections including diagnostics, symptoms, and treatment among female undergraduate participants attending the University of California, Los Angeles, 2017.
| % of participants that correctly answered the knowledge question |
||||
|---|---|---|---|---|
| Sexually active % (N = 474) | Not sexually active % (N = 209) | p valuea | Total % (N = 698)b | |
| Has heard of chlamydia | 98.1% (463) | 89.5% (187) | <0.001 | 95.3% (663) |
| Chlamydia is only transmitted by vaginal sex? (F) | 63.3% (292) | 54.0% (109) | 0.029 | 60.0% (406) |
| Most people with chlamydia do not have symptoms? (T) | 58.6% (270) | 46.0% (93) | 0.004 | 54.8% (371) |
| Once infected, you cannot get rid of chlamydia? (F) | 75.0% (345) | 51.7% (104) | <0.001 | 68.0% (458) |
| Chlamydia can be treated with antibiotics? (T) | 68.5% (313) | 50.2% (101) | <0.001 | 62.6% (421) |
| Chlamydia can only be caught once? (F) | 70.1% (321) | 55.7% (112) | <0.001 | 65.5% (441) |
| Has heard of gonorrhea | 98.3% (466) | 93.8% (196) | 0.004 | 96.8% (676) |
| Gonorrhea is only transmitted by vaginal sex? (F) | 65.3% (301) | 55.0% (111) | 0.015 | 61.7% (418) |
| Most people with gonorrhea do not have symptoms? (T) | 31.2% (144) | 26.7% (54) | 0.283 | 29.7% (201) |
| Once infected, you cannot rid of gonorrhea? (F) | 64.1% (295) | 48.3% (97) | <0.001 | 59.1% (399) |
| Gonorrhea can be treated with antibiotics? (T) | 56.8% (262) | 41.8% (84) | <0.001 | 52.2% (353) |
| Gonorrhea can only be caught once? (F) | 62.6% (286) | 54.2% (109) | 0.054 | 59.7% (401) |
| Chlamydia/Gonorrhea can lead to infertility/other reproductive health issues? (T) | 80.1% (366) | 67.7% (136) | <0.001 | 75.9% (510) |
| Has heard of trichomoniasis | 33.1% (156) | 22.6% (47) | 0.008 | 29.4% (204) |
| Trichomoniasis is only transmitted by vaginal sex? (F) | 30.0% (138) | 30.7% (62) | 0.931 | 29.9% (202) |
| Most people with trichomoniasis do not have symptoms? (T) | 11.7% (54) | 13.4% (27) | 0.646 | 12.1% (82) |
| Once infected, you cannot get rid of trichomoniasis? (F) | 21.1% (97) | 16.4 % (33) | 0.195 | 19.3% (130) |
| Trichomoniasis can be treated with antibiotics? (T) | 15.8% (73) | 16.9% (34) | 0.816 | 16.0% (108) |
| Trichomoniasis can only be caught once? (F) | 28.2% (129) | 27.9% (56) | 0.999 | 27.6% (186) |
| If your partner is diagnosed, you need to be treated? (T) | 71.1% (328) | 60.7% (122) | 0.011 | 67.9% (459) |
| % of participants that selected each diagnostic method | ||||
| Chlamydia can be diagnosed using | ||||
| Urine test* | 44.8% (206) | 33.2% (66) | 0.007 | 41.3% (278) |
| Self-collected vaginal swab* | 56.3% (259) | 39.2% (78) | <0.001 | 51.3% (345) |
| Blood test | 32.8% (151) | 29.6% (59) | 0.476 | 32.1% (216) |
| Gonorrhea can be diagnosed using | ||||
| Urine test* | 41.8% (192) | 29.4% (59) | 0.003 | 37.8% (255) |
| Self-collected vaginal swab* | 52.7% (242) | 35.8% (72) | <0.001 | 47.3% (319) |
| Blood test | 31.2% (143) | 25.4% (51) | 0.159 | 29.1% (196) |
| Trichomoniasis can be diagnosed using | ||||
| Urine test* | 14.3% (66) | 12.5% (25) | 0.610 | 13.6% (92) |
| Self-collected vaginal swab* | 20.2% (93) | 16.5% (33) | 0.313 | 18.8% (127) |
| Blood test | 14.8% (68) | 18.5% (37) | 0.278 | 15.9% (107) |
Correct diagnostic method.
Note. T = true; F = false; the correct answer is indicated in parenthesis; n = number of participants.
p values calculated using chi square test.
Total includes “choose not to answer” sex group.
Figure 1.
The proportion (%) of participants within each category ((a) year in school, (b) race/ethnicity, (c) sexual activity/sexually transmitted infection (STI) testing history) who scored ≥80% correct on Chlamydia trachomatis (CT) and Neisseria gonorrhoeae (NG) knowledge questions.
Additionally, sexually active participants had higher odds of prior testing for CT, NG, or TV as knowledge score categories increased. When we adjusted for year in education and race/ethnicity, participants in the highest knowledge quartile had three times the odds of prior testing for at least one of CT, NG, or TV, (aOR: 3.74, 95% CI 2.02, 6.96) compared with those in the lowest knowledge quartile.
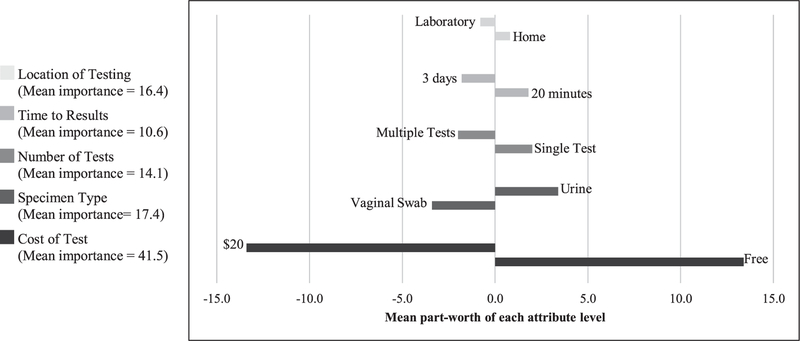
Figure 2 shows the conjoint analysis results regarding participant willingness to use a hypothetical STI test. For the sample population, cost (free vs. $20) had the largest impact on willingness to use the test and on average accounted for 41.5% of test type preference, followed by specimen type (urine vs. vaginal swab; 17.4%), location of testing (home vs laboratory; 16.4%), number of tests required (one vs three tests; 14.1%), and time to results (20min vs. 3 days; 10.6%).
Figure 2.
Average impact of chlamydia, gonorrhea, and trichomoniasis test attributes on hypothetical test acceptability among a total sample of undergraduate females attending University of California, Los Angeles, using metric conjoint analysis, 2017.
Finally, most participants would prefer a test which directly provided them with results at home, 83.4% (n = 527) versus having to collect the specimen and mail them to a laboratory for results 16.7% (n = 103). For communication of results, most participants would prefer a test which would automatically send results to the doctor 62.9% (n = 388), followed by manually sending the results to a doctor via an online message 15.7% (n = 96), sharing results in person 13.5% (n = 84), and uploading results to an app which a doctor could access 8.7% (n = 54).
Comments
We surveyed undergraduate females at a large university and assessed knowledge about CT, NG, and TV infections and preferences for STI testing. Overall, we found that participants had more knowledge about CT and NG infections compared with TV infection. Over half of the participants had never heard of TV infection. For other questions regarding the symptoms, diagnosis, and transmission of TV infection, most respondents selected “I don’t know” as their answer choice. Those results suggest there is a lack of awareness or knowledge regarding TV infection compared with other STIs, even though it is one of the most common STIs.1
While participants had a greater awareness and knowledge of both CT and NG infections, there were still gaps in knowledge as overall only 27.7% of participants scored ≥ 80% correct on the questions regarding CT and NG infections. Additionally, participant knowledge of the diagnosis of the infections was limited as around 30% of participants for both CT and NG incorrectly answered that a blood test could be used for routine diagnosis. Many participants were also unaware that most people infected with CT or NG are asymptomatic. Without an awareness of the asymptomatic nature of those infections, individuals may not know the need to follow the annual screening recommendations of the Centers for Disease Control and Prevention,1 leading to under detection and treatment. The higher the year in university, the more likely a participant was to score ≥ 80% on knowledge questions for CT and NG infections. Additionally, participants who had previously been tested and sexually active were most likely to score ≥ 80% correct. While the directionality of the association cannot be determined, those findings suggest that implementing educational programs for undergraduate females may help increase screening and testing of STIs. Conversely, STI testing itself might result in increased STI knowledge and further increase STI testing.
We also determined the factors associated with participant willingness to use hypothetical STI tests. The cost of the test was the most impactful attribute as most participants unsurprisingly preferred a free test compared with one that cost $20. That result supports the need for further education to ensure that participants are made aware that screening for STIs is covered by most insurance. Along with cost, participant preferences in attributes support a single, urine-based, home STI test that will provide the patient with results in 20 min.
Strengths of this study include the large sample size, range of knowledge measures, and novel use of conjoint analysis to determine STI testing preferences. Previous studies found that 98% of university students found it easy to understand self-collected vaginal instructions, revealing that home based tests might be a viable, and preferred option for STI testing.22 Additionally, the preference of urine samples versus self-collected vaginal samples from participants in our survey was consistent with some,23,24 but not all, prior studies.22,25,26 It is important to continue to offer choices for STI specimens among undergraduate students. Prior studies have surveyed the prevalence of CT infection among females and found that women with CT were more likely to be younger, nonwhite, and have lower socioeconomic status.27 Those findings suggest that future research about STIs among undergraduate female students should also consider their socioeconomic status when comparing differences among knowledge or testing preferences. Future studies could also explore the testing preferences and knowledge of STIs among male university students.
Limitations
Using an online survey resulted in less than 100% participation, subjecting the findings to nonresponse bias. We were unable to compare all the characteristics of respondents to nonrespondents, therefore the knowledge, screening practices, and preferences among those who did respond may be different than those who did not respond. Additionally, due to the large size of the university, we found small but statistically significant differences between our sample population and the base population of UCLA female undergraduates. The population from our study was female students at UCLA and these students may not be representative of other populations. The survey also did not distinguish participants based on any socioeconomic factors such as household income or parental education level. Furthermore, using an online survey format does not allow for participants to clarify or ask questions. Participants also were not required to answer all questions, so some questions have less than the total sample size response. To create an overall knowledge score, each question was weighted equally which may not capture the importance of knowledge in particular areas. While our overall sample size was large, due to small sample sizes within some ethnic and age groups, we were limited in our ability to draw conclusions. For the conjoint analysis, attribute preferences depend on the particular attribute levels chosen for the study, thus with a narrower range for cost, for example, this attribute may have been rated as less important. Finally, sexual activity was defined by the respondent, so some participants may have a more expansive definition of sexual activity than others.
Conclusion
Undergraduate female survey participants had greater knowledge about CT and NG infections compared with TV infection. However, overall knowledge was strikingly low as many participants had incorrect knowledge in their understanding about the diagnostic methods, frequency of symptoms, and treatment of the three infections. Additionally, having a prior history of STI testing appeared to be a major contributor to differences in knowledge. Our findings reveal a need to improve knowledge of STIs among undergraduate females. As we found that female undergraduate students were more likely to have higher knowledge of CT and NG if they are in a later year in university, interventions should be targeted toward first year students entering university to have the greatest impact. The university health center may be a successful place for interventions to increase education and awareness of STIs as most participants reported having used the university health center.
Offering guideline-directed education for providers and staff in health centers has been shown to increase screening for CT and NG.28 During meetings, college health providers were educated on the Centers for Disease Control and Prevention recommendations for STI screening for all sexually active adults 25 years or younger as well as strategies for discussing sexual health and history with patients. Along with educating providers, a flag was placed on patients’ electronic charts who were sexually active adults 25 years or younger, providing a short questionnaire in the exam room regarding sexual health.
Another study found that undergraduate females had sustained improvements in STI knowledge after attending a single intervention session where they learned about STI transmission, consequences, and misconceptions.29 That strategy of focused educational interventions may be incorporated into students’ regular visits to the university health center.
Finally, as youth behavior continues to be increasingly influenced by social media, providers should use social media to educate university students.30,31 Our study revealed modest STI knowledge and screening frequency among undergraduate females. New educational strategies coupled with convenient STI testing options may improve sexual health among university students.
Supplementary Material
Acknowledgments
We thank our participants for their participation in the survey as well as UCLA Registrar office.
Funding
This work was supported by Team Klausner Saving Lives, National Institutes of Health: Center for AIDS Research (5P30AI028697), and Center for HIV, Identification, Prevention and Treatment Services (MH58107).
Footnotes
Conflict of interest disclosure
The authors have no conflicts of interest to report. The authors confirm that the research presented in this article met the ethical guidelines, including adherence to the legal requirements, of the United States and received approval from the Institutional Review Board of the University of Los Angeles, California.
References
- 1.CDC (Centers for Disease Control and Prevention) Sexually Transmitted Diseases Treatment Guidelines. Morbidity and Mortality Recommendations and Reports. 2015;64 (3):1–134. [Google Scholar]
- 2.Cuffe KM, Newton-Levinson A, Gift TL, et al. Sexually transmitted infection testing among adolescents and young adults in the United States. J Adolescent Health. 2016;58(5):512–519. doi: 10.1016/j.jadohealth.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 3.Habel MA, Leichliter JS, Torrone E. Exploring chlamydia positivity among females on college campuses, 2008–2010. J Am Coll Health. 2016;64(6):496–501. doi: 10.1080/07448481.2015.1117470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.James AB, Simpson TY, Chamberlain WA. Chlamydia prevalence among college students: reproductive and public health implications. Sex Transm Dis. 2008;35(6):529–532. doi: 10.1097/0LQ.0b013e3181676697. [DOI] [PubMed] [Google Scholar]
- 5.Lorimer K, Hart GJ. Knowledge of Chlamydia trachomatis among men and women approached to participate in community-based screening, Scotland, UK. BMC Public Health 2010; 10(1):794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caetano ME, Linhares IM, Pinotti JA, et al. Sexual behavior and knowledge of sexually transmitted infections among university students in Sao Paulo, Brazil. Obstet Gynecol Int J. 2010;110(1): 43–46. doi: 10.1016/j.ijgo.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 7.Ekşi Z, Kömürcü N. Knowledge level of university students about sexually transmitted diseases. Procedia-Social Behav Sci. 2014;122:465–472. doi: 10.1016/j.sbspro.2014.01.1374. [DOI] [Google Scholar]
- 8.Greaves A, Lonsdale S, Whinney S, Hood E, Mossop H, Olowokure B. University undergraduates’ knowledge of chlamydia screening services and chlamydia infection following the introduction of a National Chlamydia Screening Programme. Eur J Contracept Reprod Health Care. 2009;14(1):61–68. doi: 10.1080/13625180802434884. [DOI] [PubMed] [Google Scholar]
- 9.Hoff T, Greene L, Davis J. National survey of adolescents and young adults: sexual health knowledge, attitudes and experiences. Menlo Park, CA: Henry J. Kaiser Family Foundation; 2003. [Google Scholar]
- 10.Toews ML, College YA. students’ knowledge, attitudes, and behaviors regarding sex and contraceptives. J Fam Consum Sci. 2012;104(3):16–23. [Google Scholar]
- 11.Chase J, Chow JM, Lifshay J, et al. STD/HIV knowledge, care-related behaviors, and morbidity. Women’s Health. 2003;4: 1–8. Available at: https://www.dhcs.ca.gov/dataandstats/reports/Documents/0WHReports/CWHS_97-03Report.pdf. Accessed April 15, 2018. [Google Scholar]
- 12.Denison HJ, Bromhead C, Grainger R, et al. What influences university students to seek sexually transmitted infection testing?: a qualitative study in New Zealand. Sexual Reprod Healthcare. 2018;16:56–60. doi: 10.1016/j.srhc.2018.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tucker JD, Bien CH, Peeling RW. Point-of-care testing for sexually transmitted infections: recent advances and implications for disease control. Curr Opin Infect Dis. 2013;26(1):73–79. doi: 10.1097/QC0.0b013e32835c21b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. Mapping the Landscape of Diagnostics for Sexually Transmitted Infections: Key Findings and Recommendations. Geneva, Switzerland: World Health 0rganization; 2004. [Google Scholar]
- 15.Habel M, Brookmeyer K, Haffner S, et al. Creating innovative STD testing options for University Students: the impact of a STD self-testing program. Sex Transm Dis. 2016;43:S134–S135. doi: 10.1097/0LQ.0000000000000733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McRee AL, Esber A, Reiter PL. Acceptability of home-based chlamydia and gonorrhea testing among a national sample of sexual minority young adults. Perspect Sex Reprod Health. 2015; 47(1):3–10. doi: 10.1363/47e2715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.UCLA Academic Resources and Planning. Undergraduate profile (2016-2017). Available at: https://www.apb.ucla.edu/Portals/90/25.Documents/Campus%20Stats/UGProfile16-17.pdf. Accessed April 15, 2018.
- 18.Bristow CC, Lee SJ, Severe L, et al. Attributes of diagnostic tests to increase uptake of dual testing for syphilis and HIV in Port-26. au-Prince, Haiti. Int J STD AIDS. 2017;28(3):259–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.James TG, Sadie RJ. Differences in STI knowledge accuracy and STI/HIV testing among a random sample of college students: a secondary survey analysis. SocArXiv 2017:1–21. doi: 10.31235/osf.io/uycjs.27. [DOI] [Google Scholar]
- 20.Gebremedhn EG, Gebregergs GB, Anderson BB. The knowledge level of final year undergraduate health science students and medical interns about cardiopulmonary resuscitation at a university teaching hospital of Northwest Ethiopia. World J Emerg Med. 2014;5(1):29. doi: 10.5847/wjem.j.issn.1920-8642.2014.01.005.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kuhfeld W. Marketing Research Methods in SAS. 2nd ed., Vol. 9 Cary, NC: SAS Institute Inc; 2010. [Google Scholar]
- 22.Fielder RL, Carey MP, Carey KB. Acceptability of STD Testing 29. Using Self-collected Vaginal Swabs Among College Women. Ann BehavMed. 2011;41(1):S232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Serlin M, Shafer MA, Tebb K, et al. What sexually transmitted 30. disease screening method does the adolescent prefer? Adolescents’ attitudes toward first-void urine, self-collected vaginal swab, and pelvic examination. Arch Pediatr Adolesc Med. 31. 2002;156(6):588–591. doi: 10.1001/archpedi.156.6.588. [DOI] [PubMed] [Google Scholar]
- 24.Hsieh YH, Howell MR, Gaydos JC, et al. Preference among female Army recruits for use of self-administrated vaginal swabs or urine to screen for Chlamydia trachomatis genital infections. Sex Transm Dis. 2003;30(10):769–773. doi: 10.1097/01.OLQ.0000079048.11771.46. [DOI] [PubMed] [Google Scholar]
- 25.Gaydos CA, Dwyer K, Barnes M, et al. Internet-based screening for Chlamydia trachomatis to reach non-clinic populations with mailed self-administered vaginal swabs. Sex Transm Dis. 2006; 33(7):451–457. doi: 10.1097/01.olq.0000200497.14326.fb. [DOI] [PubMed] [Google Scholar]
- 26.Newman SB, Nelson MB, Gaydos CA, Friedman HB. Female prisoners’ preferences of collection methods for testing for Chlamydia trachomatis and Neisseria gonorrhoeae infection. Sex Transm Dis. 2003;30(4):306–309. doi: 10.1097/00007435-200304000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Klausner JD, McFarland W, Bolan G, et al. Knock-knock: a population-based survey of risk behavior, health care access, and Chlamydia trachomatis infection among low-income women in the San Francisco Bay area. J Infect Dis. 2001;183(7):1087–1092. doi: 10.1086/319276. [DOI] [PubMed] [Google Scholar]
- 28.Myers A, McCaskill SP, Van Ravenstein K. Improving STD screening rates on a university campus. J Community Health. 2017;42(6):1247–1254. doi: 10.1007/s10900-017-0377-9. [DOI] [PubMed] [Google Scholar]
- 29.Jaworski BC, Carey MP. Effects of a brief, theory-based STD-prevention program for female college students. J Adolesc Health. 2001;29(6):417–425. doi: 10.1016/S1054-139X(01)00271-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Landry M, Turner M, Vyas A, Wood S. Social media and sexual behavior among adolescents: is there a link? JMIR Public Health Surveill. 2017;3(2):e28. doi: 10.2196/publichealth.7149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stevens R, Gilliard-Matthews S, Dunaev J, Todhunter-Reid A, Brawner B, Stewart J. Social media use and sexual risk reduction behavior among minority youth: seeking safe sex information. Nurs. Res. 2017;66(5):368–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.