Abstract
A 67-year-old woman presented to our vein clinic for chronic left lower extremity edema, pain, and varicosities. After failed conservative management, a computed tomography scan revealed central venous stenosis secondary to compression of the left common iliac vein by a large osteophyte along the anterolateral aspect of the L5-S1 disk space. An anterior osteophytectomy was performed, followed by iliac venous stenting at a 1-month interval. The patient had resolution of symptoms and remains symptom free at 15 months of follow-up. This report describes a spinal exostosis causing symptomatic venous compression successfully relieved by surgical decompression.
Keywords: Iliac vein, Exostosis, Limb swelling, Venous obstruction
Iliac vein compression syndrome is a condition in which obstruction of the venous outflow from the lower extremity may cause lower extremity venous congestion, leading to discomfort, swelling, or venous thrombosis. It is more commonly seen as the classic May-Thurner syndrome, in which the left common iliac vein is compressed by the right common iliac artery. Other rare and less frequent causes of extrinsic compression of the iliac veins have been described.1, 2 Venous outflow obstruction in combination with repetitive microtrauma to the iliac vein predisposes patients to recurrent venous thrombosis or nonthrombotic symptoms. Patients may present with acute iliofemoral venous thrombosis or with symptoms of chronic lower extremity venous insufficiency, such as unilateral pain, edema, ulcers, skin hyperpigmentation, varicosities, and venous claudication.3, 4, 5 Detailed history and physical examination are typically followed by ultrasound evaluation for venous thrombosis and insufficiency. Any suspicion of central venous compression should trigger further investigation with either axial imaging (computed tomography [CT] or magnetic resonance imaging) or conventional venography combined with intravascular ultrasound. Treatment of compression-induced central thrombosis commonly consists of endovascular therapy (ie, catheter-directed thrombolysis or pharmacomechanical thrombectomy) and anticoagulation, followed by luminal restoration with iliac venoplasty and stenting.6
We describe a rare cause of extrinsic central venous compression by lumbosacral exostosis resulting in a large bone osteophyte compressing the left common iliac vein. Osteophytes are a type of exostosis, or abnormal bone growth, that project along joint margins and are common sequelae of osteoarthritis throughout the body. They present along joints that experience chronic mechanical stress, like those of the hip, knee, and vertebral bodies. Vertebral osteophytes are present in 20% to 30% of the geriatric population, although only a small proportion of these produce clinical symptoms. Symptoms are usually based on the location of the osteophyte and the surrounding structures it compresses. For example, osteophytes at the level of the cervical spine are manifested with dysphagia or dysarthria when there is compression of the pharynx, larynx, or esophagus.7 Osteophytes of the thoracic spine may lead to compression of the splanchnic nerves or the sympathetic trunk. Lumbar osteophytes are capable of decreasing venous outflow to the inferior vena cava. Osteophytes throughout the spine frequently compress the exiting nerve in the cervical spine and traversing nerves in the thoracic and lumbar spine, causing radiculopathy. Our patient presented with symptoms of iliac vein compression syndrome secondary to left iliac vein compression by a large anterolateral osteophyte of the lumbosacral spine.
The patient about whom this case report is written was made aware that data concerning her diagnosis and treatment would be submitted for publication. She provided consent.
Case report
Our patient, a 67-year-old woman, first presented to the vascular clinic complaining of chronic left lower extremity edema, pain, and venous stasis changes. The patient was also found to have large painful varicosities. Her physical examination demonstrated significant pitting edema above and below the level of the popliteal fossa. She underwent a duplex ultrasound examination, which showed reflux in the small saphenous vein, mild reflux in the great saphenous vein, and post-thrombotic changes in the popliteal vein. Interestingly, the patient reported that she underwent surgery for veins in Mexico about 20 years ago, when a vein in her right leg was transferred to her left. Unfortunately, she was unable to recall the details of the procedure. Surgical records from this operation are not available; however, her bilateral groin scars, right great saphenous vein harvest scar, and subsequent CT imaging indicate that a Palma procedure, which had thrombosed at some point, was likely to have been performed. The patient was prescribed compression stockings and was given follow-up at 3 months.
At 3-month follow-up, the patient was dutifully wearing her compression stockings; however, she continued to have significant lower extremity edema and pain. With the suspicion of central compression or stenosis, a venous-phase contrast-enhanced CT scan was obtained. The CT study revealed high-grade stenosis and compression of the left common iliac vein (Figs 1 and 2) by a large anterolateral vertebral osteophyte complex off the L5-S1 disk space.
Fig 1.
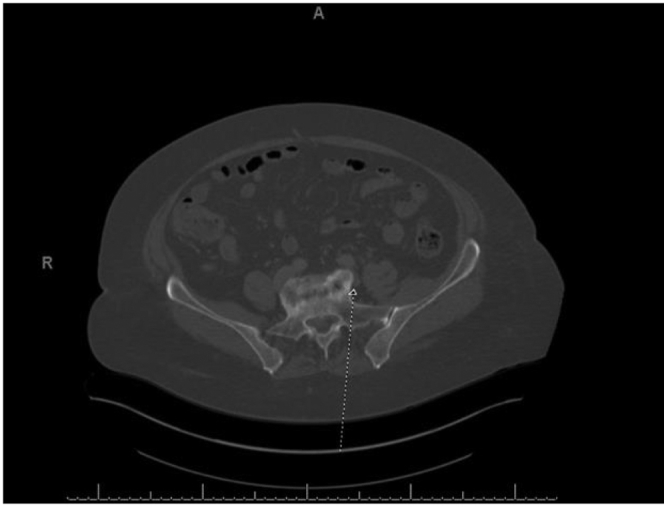
Axial view of the large left-sided L5-S1 osteophyte resulting in extrinsic compression of the left common iliac vein.
Fig 2.
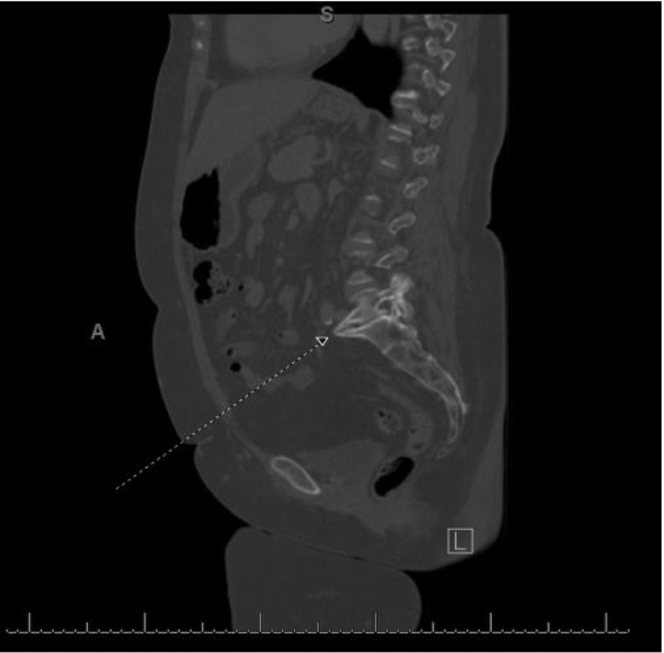
Sagittal view of the large left-sided L5-S1 osteophyte invading the left common iliac vein.
After orthopedic spine consultation, it was agreed that the osteophyte complex was the cause of compression of the common iliac vein. The patient then agreed to undergo resection of the anterior osteophyte at L5-S1 through a left extraperitoneal approach standard for L5-S1 anterior exposure. On exploration, the common iliac vein was noted to be densely adherent to the exostosis with severe scarring. The vein was carefully mobilized, and a small injury to the scarred vein was repaired by direct lateral venorrhaphy. The osteophyte was completely resected off the joint space. Venolysis was performed, resulting in wide decompression of the iliac vein; however, the vein was scarred with about 50% residual stenosis. On postoperative day 1, the patient was found to have dramatically resolved lower extremity edema. Despite the resolution of edema and pain, there was a clinical suspicion of residual significant stenosis, given the intraoperative scarred and stenotic appearance of the common iliac vein. After the operation, the patient continued anticoagulation with the concern that the injured and stenotic vein may thrombose. Scheduled venography 1 month after surgery showed there was about 70% diameter focal stenosis in the common iliac vein with a septation. This was treated with venoplasty and stenting using a 20-mm × by 6-cm self-expanding stent (Wallstent; Boston Scientific, Marlborough, Mass) and a 16-mm balloon. Anticoagulation was continued for 6 months and then stopped. Duplex ultrasound imaging at 3-, 6-, 12-, and 15-month follow-up revealed the vein and stent to be widely patent. The patient remains symptom free without any residual pain or edema at 15 months of follow-up.
Discussion
Cases of osteophytes causing vascular compression and subsequent vascular compromise are common in the literature. For example, cases of Paget-Schroetter syndrome, thrombosis of the abdominal aorta, and compression of femoral vessels by osteophyte complexes have been reported.8, 9, 10 Surgical treatment typically consists of relieving the symptoms of vessel compression while reducing the chances of recurrent compromise or thrombosis. Thus, if the osteophytes are accessible, they are typically excised. Endovascular therapy in the form of angioplasty and stenting may be needed to treat residual stenosis after external decompression or as a primary revascularization if external decompression is not to be performed. In our patient, surgical decompression with resection of osteophyte and venolysis successfully resulted in complete resolution of lower extremity edema and pain. Given residual stenosis in the traumatized iliac vein, we initially kept her anticoagulated and then stented it to restore complete patency for an improved long-term outcome.
Our case outlines that although it is rare, external compression by bone exostosis and osteophytes should be on the list of differentials when patients present to the clinic for chronic lower extremity edema or thrombotic symptoms. This diagnosis may be particularly important in elderly patients with risk factors for spinal osteoarthritis and osteoporosis.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Shin D.S., Mokkarala M., Allison S., Monroe E.J. Osteophytic iliac venous compression: technical considerations for a bony May-Thurner syndrome variant. J Clin Interv Radiol ISVIR. 2018;2:95–100. [Google Scholar]
- 2.Ou-Yang L., Lu G. Underlying anatomy and typing diagnosis of May-thurner syndrome and clinical significance: an observation based on CT. Spine (Phila Pa 1976) 2016;41:E1284. doi: 10.1097/BRS.0000000000001765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Knuttinen M.G., Naidu S., Oklu R., Kriegshauser S., Eversman W., Rotellini L. May-Thurner: diagnosis and endovascular management. Cardiovasc Diagn Thera. 2017;7:S159–S164. doi: 10.21037/cdt.2017.10.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaltenmeier C.T., Erben Y., Indes J., Lee A., Dardik A., Sarac T. Systematic review of May-Thurner syndrome with emphasis on gender differences. J Vasc Surg Venous Lymphat Disord. 2018;6:399–407.e4. doi: 10.1016/j.jvsv.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 5.Ahsan I., Qureshi B.G., Ghani A.R., Malik F., Arif Z. An extensive unprovoked left lower extremity deep vein thrombosis secondary to an anatomical anomaly: a case of May-Thurner syndrome. Clin Pract. 2017;7:938. doi: 10.4081/cp.2017.938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lugo-Fagundo C., Nance J.W., Johnson P.T., Fishman E.K. May-Thurner syndrome: MDCT findings and clinical correlates. Abdom Radiol. 2016;41:2026–2030. doi: 10.1007/s00261-016-0793-9. [DOI] [PubMed] [Google Scholar]
- 7.Seo J.W., Park J.W., Jang J.C., Kim J.W., Lee Y.G., Kim Y.T. Anterior cervical osteophytes causing dysphagia and paradoxical vocal cord motion leading to dyspnea and dysphonia. Ann Rehabil Med. 2013;37:717–720. doi: 10.5535/arm.2013.37.5.717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Werner-Gibbings K., Dubenec S. Medial clavicular osteophyte: a novel cause of Paget-Schroetter syndrome. Case Rep Vasc Med. 2015;2015:723182. doi: 10.1155/2015/723182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pinkerton G.E. Thrombosis of the abdominal aorta: apparently caused by pressure from a vertebral osteophyte. Lancet. 1948;252:811. [PubMed] [Google Scholar]
- 10.Takasago T., Goto T., Tsutsui T., Kondo K., Hamada D., Tonogai I. A huge capital drop with compression of femoral vessels associated with hip osteoarthritis. Case Rep Orthop. 2015;2015:709608. doi: 10.1155/2015/709608. [DOI] [PMC free article] [PubMed] [Google Scholar]


