Abstract
We reviewed the role of telemedicine in multidisciplinary team (MDT) meetings, which play an important role in the provision of effective and tailored patient care in diverse clinical settings. This article is based on conducted search in PubMed. Search terms included “telemedicine,” “multidisciplinary team,” and “(telemedicine) and (multidisciplinary team).” Telemedicine provides an important advantage in the provision of MDT meeting comparing with traditional settings. Those include improved access to and collaboration of medical experts. This resulted in increased levels of medical competence and improved provisions of diagnosis, treatment, and follow-up to patients irrespective of location.
Keywords: Digital pathology, multidisciplinary team meeting, remote diagnostics, telemedicine, video interpretation
INTRODUCTION
Telemedicine is defined as remote use of communication technology in health-care exchange of medical information for diagnosis, prevention, evaluation, research, administration, examination, treatment, follow-up, and education. It has found its way to nearly all medical settings in both primary, secondary, and tertiary care.[1,2,3,4,5] A multidisciplinary team (MDT) consists of specialists in different medical fields and supporting medical staff providing final expert opinion services [Figure 1]. MDT meetings are found to be necessary to failsafe diagnosis, treatment, and follow-up.[6,7,8] The concept of MDT meetings is not new, but has evolved and been revolutionized by the introduction of telemedicine.[9,10] Telemedicine has improved provisions of MDT meetings in diverse clinical settings [Table 1].[11,12,13] We reviewed the role of telemedicine in MDT meetings based on literature search.
Figure 1.
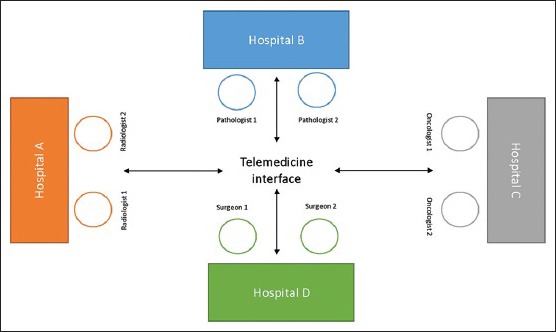
Schematic presentation of multidisciplinary team meetings via telemedicine
Table 1.
Effects of multidisciplinary team meeting via telemedicine on key health care elements
| Quality | Cost | Accessibility | Organisation | Acceptability | |
|---|---|---|---|---|---|
| For the state | ↑Quality of health care | ↓Expenditure | ↑Better regional access | ↑Management of health care | ↑Support for e-health |
| For the hospital | ↑Recruitment and reputation | ↓Cost of hospitalisation | ↑Hospital services | ↑Efficiency and cooperation | ↑Development |
| For physicians | ↑Quality of practice | ↓Travel and lodging costs | ↑Access to patient data | ↑Collaboration and traning | ↑Utilisation |
| For patients | ↑Quality of life and care | ↓Cost of tranfer | ↑ Access to care | ↑Care choices | ↑Confidence |
METHODS
The methods used in this review article are based on conducted search in PubMed. Search terms included “telemedicine,” “multidisciplinary team” and “(telemedicine) and (multidisciplinary team).” We have used MeSH terms to conduct the search. Inclusion criteria were English-written papers and publication to the present day. We have found 137 publications, of which 133 publications were available as full text. Out of those 133 articles, we focused on 32 review articles. Some articles were dropped either because of similarities in their objectives, design, and results or having focused on telemedicine or MDT (and not both) or not having MDT via telemedicine as their primary subject.
DISCUSSION
General considerations on technology, design, oversight, implementation, and recommendations from literature review (specialty unrelated or multiple specialties)
In this article, we have peer-reviewed literature on the use of telemedicine in MDT meetings. Analysis shows successful implementation of telemedicine in diverse aspects of MDT meetings, in both primary and secondary health care. Advantages are multiple and overweigh disadvantages. Two mainly used methods include video and telephone conferencing.[14,15,16,17,18,19] Key findings from the reviewed articles are summarized in Table 2.
Table 2.
Summary of key findings on multidisciplinary team meetings via telemedicine in reviewed articles
| References | Specialties | Conclusions |
|---|---|---|
| Tensen E, etal.[1] | Dermatology | Reduces travel, waiting time, unnecessary dermatologic visits, and improves access of care to underserved patients |
| WHO[2] | General | Benefits of health telematics include reduced costs, hospitalization, waiting times, and isolation of patients, improves training, education and diagnostics |
| Voran D[3] | General | Policy, regulatory status, legislative, interstate licensing and reimbursement initiatives are important to future telemedicine trends with special attention to mobile devices |
| Chaet D, etal.[4] | General | Input from oversight institutions such as AMA Council on Ethical and Judicial Affairs on ethical practice in telehealth and telemedicine plays crucial roles for maintaining and updating the code of conduct |
| Bartz CC, etal.[5] | General | Developments in telemedicine accessible to all patients and healthcare professionals, enable expert advice to be provided remotely and ensure continuity of care for all patients in need |
| Wood L. etal.[6] | Psychology and psychiatry | Psychology was valued source of support for skilling-up and offering reflective space to MDT |
| Song P, etal.[7] | Cancer Services | Possible problems in constructing scientifically best cancer treatment models include medical care insurance systems, public hospitals reform, hospital management approaches, personnel framework, concern with patients’ psychology |
| Abdulrahman GO Jr[8] | Cancer Services | Barriers to effectiveness included importance of nontechnical skills, organizational support, good relationships between team members, recording of disagreements and importance of patient-centered information in relation to team-decision making; central role of clinical nurse specialists as the patient’s advocates, complementing the role of physicians in relation to patient centeredness |
| Stalfors J, etal.[9] | Cancer Services | Cost analysis showed that FTF presentation cost versus telemedicine was not significant, however physician accompanied only fraction of patients when presented |
| Slusser W, etal.[10] | Nutritional medicine | Chart review indicated trend for decreased or stabilized body mass index and blood pressure |
| Demartines N, etal.[11] | General | Telemedicine augments exchange of scientific information, remote diagnosis and therapy, remote education and training, simplifying and expanding access to remote interdisciplinary expertise |
| Haines A, etal.[12] | Psychology & psychiatry | While direct (video) observations were very difficult to achieve in secure settings, they enabled unmediated access to how people conducted themselves rather than having to rely only on their subjective accounts (interviews) |
| Davison AG, etal.[13] | Cancer Services | Annual resection rate increased by 30%, reductions of mean time (from first consultation in the clinic to surgery), estimated annual saving of three working weeks of thoracic surgical time |
| Woods L, etal.[14] | Cardiology | Method was considered inadequately comprehensive for use in needs analysis with patients and family, which encourages further research evaluating in-hospital processes for co-designed health technologies |
| De Jong CC, etal.[15] | Neurology | Professionals used Congredi adequately in MDT care of patients with dementia because changing involvement of caregivers and level of care activities were reflected in use of Congredi |
| Geronimo A, etal.[16] | Neurology | Telehealth removed burdens of travel, resulting in lower stress and interactions that are more comfortable |
| Giordano A, etal.[17] | Orthopedics | Economic evaluation could provide information about cost-effectiveness and effects on quality of life |
| Emerson JF, etal.[18] | Nutritional medicine | MDT care could increase access to intensive primary care services in vulnerable population |
| Comín-Colet J, etal.[19] | Cardiology | Addition of telemedicine resulted in better outcomes and reduction of costs |
| Cuperus N, etal.[20] | Pharmacology | Non-pharmacologic, FTF treatment program for patients with GOA was likely to be cost effective, relative to a tele-phonebased program |
| Cuperus N, etal.[21] | Pharmacology | No differences found in treatment effect between patients with GOA (nonpharmacological multidisciplinary FTF self-management program vs. telephone-delivered program), limited benefits of selfmanagement program for individuals with GOA |
| Vermeulen J, etal.[22] | General | Broader insights into similarities and differences can improve understanding between team members from different backgrounds, optimizing collaboration during the development of user-centered telecare products and services |
| Stern A, etal.[23] | Dermatology | Economic evaluation demonstrated mean reduction in direct care costs with telemedicine |
| Watanabe SM, etal.[24] | Cancer Services | Delivery of specialist multidisciplinary PC consultation by videoconferencing is feasible, may improve symptoms, results in cost savings to patients and families, and is satisfactory to users |
| Miller DM, etal.[25] | Neurology | e-PHR-enabled self-management did not augment multidisciplinary MS center-based care, possibly because differences between interventions were not great enough |
| Huis in ‘t Veld RM, etal.[26] | General | Clear guidlines required to overcome lack of user acceptance because of knowledge gaps medical and technical experts, language gaps, and methodological gaps in applying requirement methods to multidisciplinary scientific matters |
| Castelnuovo G, etal.[27] | Nutritional medicine | A comprehensive two-phase stepped down program enhanced by telemedicine for the long-term treatment of obese people with type 2 diabetes seeking intervention for weight loss was developed |
| Washington KT, etal.[28] | Cancer Services | Nursing and administrative staff members will likely more readily accept telehospice interventions, while those employees who address primarily psychosocial issues may be reluctant to use such technology |
| Kunkler IH, etal.[29] | Cancer Services | Proposed comprehensive methodology to assess clinical and economic effectiveness of telemedicine in this setting was encouraging |
| Delaney G, etal.[31] | Cancer Services | Regular MDT reduced travel for patients, increased access to expert opinion, and reduced delay in implementing treatment |
| Simpson S, etal.[32] | Nutritional medicine | Patients have consistently rated high levels of satisfaction with all aspects of video-therapy, and after their last session majority preferred video-therapy to FTF therapy |
| Axford AT, etal.[33] | Cancer Services | Reduced travel for patients, increased access to expert opinion and reduced delay in implementing treatment |
AMA - American Medical Association; ePHR - electronic personal health record; FTF - face-to-face; GOA - generalized osteoarthritis; MDT - multidisciplinary team; MS - multiple sclerosis; WHO - World Health Organization
While technology's potential has been recognized to be of value in MDT meetings, the findings in this review suggest that there is little research focused on how telemedicine can be effectively be implemented in MDT.[10,20,21,22] The most investigated area was the use of video and teleconferencing technology to support MDT meetings in diverse clinical settings. Telemedicine solutions are used to either link specialist teams, geographically dispersed, or create closer relationships between primary, secondary, and tertiary health care and patients.[23,24,25,26]
Telemedicine has been a very efficient tool in fighting patient disparity and physician shortages. Advantages of using telemedicine in MDT meetings are multiple. Increased productivity, remote reporting, better ergonomics, access to medical settings, reduced time for diagnostics and treatment, increased flexibility, and reduced travel expenses are the most encouraging. Telemedicine MDT services have also shown to be time effective, reduce overtime, build stable competence network, and increase expertise. This literature review has identified availability and quality of IT infrastructure, lack of acceptance, licensure, and costs as the most important barriers to the wider implementation of telemedicine in MDT meetings. Although the service is better and more efficient than traditional settings, the implementation of technological aspects of telemedicine can be too expensive for smaller health-care organizations. Telemedicine can open up many treatment doors, but it is not the same as a medical service up close.[9,27,28,29] As shown in our work in the implementation of routine remote digital pathology services, minimum network speed necessary for seamless viewing of digital images was 20 Mbps. We believe that this would also serve as the reference for videoconferencing and telemedicine. Network speeds of 100 Mbps are standard worldwide today, although access can vary including levels of network stability. For remote communities and areas with undeveloped IT infrastructure, satellite solutions are of interest and available, potential short- or long-term options, not necessarily costly by default. Through our digital pathology, we have also investigated novel ways of financing such projects. Regional IT budget, where hospitals in the same region contribute, was our way forward to secure the funding. Although it comes from all regional hospitals, this model gives more flexibility in selection and execution of projects throughout the region or nationally.[30]
Technology has a very important role in further advancing of the health sector by supporting collaboration of highly specialized teams through MDT meetings and connects patients with the specialist needs. A limited number of articles presented findings on the implementation of telemedicine in MDT meetings. This review revealed that research into telemedicine applications in MDT meetings focused largely on development rather than implementation.
Multiple reviews investigated various forms of telemedicine, policy and regulatory status, legislative, interstate licensing and reimbursement initiatives, and future telemedicine trends with special attention to mobile devices.[3] Input from oversight institutions such as the American Medical Association's Council on Ethical and Judicial Affairs (CEJA) on ethical practice in telehealth and telemedicine plays crucial roles in maintaining and updating the code of conduct. The CEJA strives to articulate expectations for conduct that are as independent of specific technologies or models of practice as possible. The present report provides broad guidance for ethical conduct relating to key issues in telemedicine.[4] Developments in telemedicine are now accessible to all patients and health-care professionals. These tools enable expert advice provided remotely and ensure a continuity of care for all patients in need. Telemedicine is developing across the world, as are networks of medical professionals who practice it and researchers who analyze the results.[5]
User-centered design (UCD) methodologies can help take the needs and requirements of potential end users into account during the development of innovative telecare products and services. Understanding how members of multidisciplinary development teams experience the UCD process might help gain insight into factors that members with different backgrounds consider critical during the development of telecare products and services. Experiences of participants related to creating a development team, expectations regarding responsibilities and roles, translating user requirements into technical requirements, technical challenges, evaluation of developed products and services, and valorization. MDT members from different backgrounds often reported similar experienced barriers and facilitators. However, only certain groups of participants reported some experienced barriers and facilitators. For example, only managers reported the experience that having different ideas about what a good business case is within one development team was a barrier, whereas only end users emphasized the facilitating role of project management in end user participation and the importance of continuous feedback from researchers on input of end users. Broader insights into these similarities and differences can improve understanding between team members from different backgrounds, which can optimize collaboration during the development of telecare products and services.[22]
Although the lack of user acceptance of telemedicine services is an important barrier to its wider implementation and deployment, the involvement of users in the service development process of telemedicine services is difficult because of knowledge gaps between the expertise of medical and technical experts, language gaps, and methodological gaps in applying requirement methods to multidisciplinary scientific matters. Clear guidelines, in which the medical and technical domains meet, would lead to the development of scenarios to elicit requirements. The approach provides an arena for different stakeholders to take part in the early stages of the design process, which should increase the chance of user acceptance and thus smoother adoption of the service.[26]
Telemedicine augments the exchange of scientific information, whereas its applications in the fields of patient care and medical education cover remote diagnosis and therapy as well as remote education and training. Its application to specialties such as anesthesiology, dermatology, medicine, surgery, and pathology at the University Hospital of Basel, Switzerland, has led to simplifying and expanding access to remote interdisciplinary expertise, as well as improving medical education in a number of specialties.[11]
Specialty-specific experiences from literature review
Dermatology
Teledermatology has been one of the first telemedicine services in use. It is an efficient and effective health-care service compared to in-person care. Use of teledermatology reduces travel and waiting time, reduces unnecessary dermatologic visits, and improves access of care to underserved patients.[1]
The clinical and cost-effectiveness of enhanced multidisciplinary teams versus “usual care” for the treatment of pressure ulcers in long-term care (LTC) facilities in Ontario, Canada, was studied. The economic evaluation demonstrated a mean reduction in direct care costs compared to “usual care.” The qualitative study suggested that onsite support by wound specialists was welcomed and is responsible for reduced costs through discontinuation of expensive nonevidence-based treatments. Insufficient allocation of nursing home staff time to wound care may explain the lack of impact on healing. Enhanced multidisciplinary wound care teams were cost-effective, with most benefit through cost reduction initiated, but did not improve the treatment of pressure ulcers in nursing homes. Policy makers should consider the potential yield of strengthening evidence-based primary care within LTC facilities, through outreach by nursing staff.[23]
Cancer services
The treatment model of malignant tumors has changed from single-subject treatment to multidisciplinary collaboration treatment led by MDT. This concept strengthens the focus of malignant tumor treatment by not only improving cure rate and extending life span, but also paying close attention to patients’ actual demands to improve their quality of life. Many hospitals have investigated and practiced MDT models. Possible problems in constructing scientifically best malignant tumor treatment models, which conform to national conditions, include medical care insurance systems, public hospitals reform, hospital management approaches, personnel framework, and concern with patients’ psychosis and psychology.[7]
MDT for decisions on cancer management is a cornerstone of UK cancer policy. A proposed comprehensive methodology to assess the clinical and economic effectiveness of telemedicine in this setting, tested in a randomized breast cancer trial, was encouraging.[29]
Integrated cancer service is an accepted approach worldwide. The proposed models may be, however, difficult to introduce in rural areas, where health-care sites and staff are far apart. In the study from Wales, during the 1st year, videoconferencing MDT meetings discussed colorectal, breast, and lung cancers. There was only one aborted session, which was due to a line fault. The average attendance at the meetings increased beyond essential team members. Regular MDT reduced the need for patients to travel. They also increased access to expert opinion and reduced the delay in implementing treatment.[31]
Various studies measured the effectiveness of MDT in the management of cancer patients and identified some of the barriers to MDT. Those included the importance of nontechnical skills, organizational support, and good relationships between team members for effective team working; recording of disagreements and the importance of patient-centered information in relation to team decision-making; the central role of clinical nurse specialists as the patient's advocates; and complementing the role of physicians in relation to patient centeredness.[8]
Studies from Sweden analyzed the costs of presenting patients face-to-face (FTF) versus via telemedicine based on the questionnaires completed by patients presented at the head and neck cancer MDT meeting. Although the cost analysis showed that FTF presentation cost versus telemedicine was not significant, the difference related to the fact that the responsible physician accompanied only a fraction of patients when presented FTF. However, when presented via telemedicine, the responsible physician always participated. A sensitivity analysis revealed that if the responsible physician always accompanied individual patients for presentation of FTF, the cost would be much higher per patient.[9]
Although lung cancer MDT should review all lung cancer cases prospectively and thoracic surgeons be readily available to liaise with the MDT, there is a shortage of thoracic surgeons in the UK. The annual resection rate increased by 30% in one district general hospital following the introduction of the telemedicine MDT meetings. This has led to reductions of the mean time (from first consultation in the clinic to surgery) from 69 to 54 days. The estimation is that the telemedicine meetings saved over three working weeks of thoracic surgical time during the year.[13]
A trial of videoconferencing of multidisciplinary breast cancer clinical meetings between three public hospitals was also conducted in an attempt to increase attendance by medical staff at the meetings and thus facilitate multidisciplinary care for breast cancer patients. The videoconferences were compared with the previously existing FTF clinical meetings through questionnaires, attendance, number of cases discussed, and anthropological analysis. Although more people attended the videoconferences than the FTF meetings, most of the participants in the trial preferred the FTF meetings to the videoconferences. The mean number of cases discussed at the videoconferences was significantly less than the mean number of cases presented at FTF clinical meetings. FTF meetings were informal, spontaneous, and conducive to open discussion. In contrast, the videoconferences were formal and regimented. However, multidisciplinary case discussion can be facilitated by videoconferencing, and some of the negative experiences encountered could be overcome with changes in meeting format.[30]
Palliative care (PC) and palliative radiotherapy consultation are integral to the care of patients with advanced cancer. These services are not universally available in rural areas and travel to urban centers to access them can be burdensome for patients and families. Experience from rural Alberta, Canada, showed that delivery of specialist multidisciplinary PC consultation by videoconferencing is feasible, may improve symptoms, results in cost savings to patients and families, and is satisfactory to users.[24]
Telehospice, the delivery of end-of-life care using telecommunications technologies, allows increased interaction between providers and patients. Professionals must first accept it as a useful and user-friendly method of service delivery. Results indicate that acceptance was moderately high overall, although significant differences existed among individuals from different disciplines, with nurses and administrators generally indicating higher levels of acceptance than social workers and chaplains. Findings demonstrate that nursing and administrative staff members will likely more readily accept telehospice interventions, while those employees who address primarily psychosocial issues may be reluctant to use such technology.[28]
Cardiology
The role of telemedicine in the management of patients with chronic heart failure (HF) has not been fully elucidated. The telemedicine group experienced a significant mean net reduction in direct hospital costs per patient and 6 months of follow-up. Among patients managed in the setting of a comprehensive HF program, the addition of telemedicine resulted in better outcomes and reduction of costs. In development of applications for HF self-management, the authors conducted a needs analysis with clinicians. The objectives were to define the features and support self-management and the clinical requirements in preparation for its implementation as an adjunct to existing multidisciplinary care. This method was considered inadequately comprehensive for use in the needs analysis with patients and family, which encourages further research evaluating in-hospital processes for codesigned health technologies.[14,19]
Neurology
The use of a professional e-communication tool, Congredi, for patients with dementia has been evaluated. The patients were divided into low-complex care and high-complex care groups. Professionals used Congredi adequately in the multidisciplinary care of patients with dementia because the changing involvement of caregivers and the level of care activities were reflected in the use of Congredi.[15]
The practice of telehealth in the care of patients with amyotrophic lateral sclerosis (ALS) has received little attention, but has the potential to change the multidisciplinary care model. Patients and caregivers engaged in live telehealth videoconferencing from their homes with members of a multidisciplinary ALS care team. All patients and caregivers, and most health care providers (HCPs), agreed that the system allowed for good communication, description of concerns, and provision of care recommendations. The most common sentiment conveyed by each group was that telehealth removed the burdens of travel, resulting in lower stress and interactions that are more comfortable. Caregivers and HCPs expressed more concerns than patients did about the ways in which telehealth fell short of in-person care. ALS patients, caregivers, and MDT members generally viewed telehealth favorably.[16]
Studies have addressed the use of electronic personal health records (e-PHRs) for self-management in complex neurological disorders such as multiple sclerosis (MS). Self-management support is an emerging aspect of chronic care management. The authors established the feasibility of conducting a randomized, controlled trial using e-PHRs for patient self-management. However, e-PHR-enabled self-management did not augment multidisciplinary MS center-based care, possibly because the differences between interventions were not great enough.[25]
Nutritional medicine
Telemedicine has been effective for rural populations, but little has been reported on pediatric obesity care via telemedicine in urban settings. The aims were to assess feasibility and acceptability of multidisciplinary pediatric obesity care via telemedicine within the same metropolitan area in terms of information technology, coordination, patient care, and clinical outcomes. Based on the questionnaires, 93% of responding patients and 88.3% of referring providers felt satisfied with the appointment. Chart review indicated a trend for decreased or stabilized body mass index and blood pressure. Implementation of telemedicine for tertiary multidisciplinary pediatric obesity care in urban settings is both feasible and acceptable to patients and HCPs.[10]
Advances in technology are likely to provide new approaches to address health-care disparities for high-risk populations. A high-risk cohort of uninsured, poorly controlled diabetic patients was identified and then randomized preconsent with stratification by geographic region to receive either the intervention or usual care. Multidisciplinary care that utilizes health coach-facilitated virtual visits is an intervention that could increase access to intensive primary care services in a vulnerable population. The methods tested are feasible and should be tested in a pragmatic randomized controlled trial to evaluate the impact on patient-relevant outcomes across multiple chronic diseases.[18]
Obesity is one of the most important medical and public health problems of our time, and therefore, it is imperative that enduring and low-cost clinical programs for obesity and related comorbidities are developed and evaluated. A comprehensive two-phase stepped down program enhanced by telemedicine for the long-term treatment of obese people with type 2 diabetes seeking intervention for weight loss was developed.[27]
Many remote communities were unable to access specialist eating disorder services. Researchers from Scotland have developed a video therapy service that offers specialist psychological and nutritional therapy for sufferers of eating disorders. Patients have consistently rated high levels of satisfaction with all aspects of video therapy, and after their last session, 67% preferred video therapy to FTF therapy. A number of patients commented that, compared with FTF therapy, they felt more in control and less intimidated in video therapy. There was also a trend for patients to become more comfortable with video therapy over the course of treatment. Nutritional knowledge increased for all patients, and the nutritional content of dietary intake markedly improved over the course of therapy.[32]
Pharmacology
The cost utility and cost-effectiveness of a nonpharmacologic FTF treatment program was compared with a telephone-based treatment program for patients with generalized osteoarthritis (GOA). This economic evaluation from a societal perspective showed that a nonpharmacologic, FTF treatment program for patients with GOA was likely to be cost-effective, relative to a telephone-based program.[20]
The effectiveness of a nonpharmacological multidisciplinary FTF self-management treatment program with a telephone-based program on daily function in patients with GOA was also addressed. Although the authors found no differences in treatment effect between patients with GOA who followed a nonpharmacological multidisciplinary FTF self-management program and those who received a telephone-delivered program, limited benefits of a self-management program for individuals with GOA were also demonstrated.[21]
Psychology and psychiatry
Psychologists routinely work in psychiatric inpatient settings and cannot work in isolation from the MDT. The analysis identified two key themes: “psychological treatments,” which describes the perceived function of psychology on the ward, and “integrated psychological working” outlining key issues that psychologists should consider when working in MDTs. MDT members see psychology as an integral, but not first-line, treatment option in the psychiatric inpatient setting. Multidisciplinary staff participants valued both direct and indirect work. Education dialogue about the role is sometimes required. The MDT values the role of psychology in the psychiatric inpatient setting. Psychology was a valued source of support for skilling-up and offering reflective space to the MDT. Psychologists need to better promote their role and their skills to the MDT.[6]
The operation of MDT meetings within a forensic hospital in England, UK, has shown that while direct (video) observations were very difficult to achieve in secure settings, they enabled unmediated access to how people conducted themselves rather than having to rely only on their subjective accounts (from the interviews).[12]
Orthopedics
Fall incidents are the third cause of chronic disablement in the elderly according to the World Health Organization. Recent meta-analyses show that multifactorial falls risk assessment and management programs are effective in all older population studied. However, the application of these programs may not be the same in all national health- care setting and consequently needs evaluation by cost-effectiveness studies before planning this intervention in regular care. Experiences from Italy showed that structured collaboration between hospital staff and primary care was generally lacking and the role of Information and Communication Technologies in a fall prevention program at home has never been explored. The program is expected to be feasible in terms of intensity and characteristics, but particularly in terms of patient and provider compliance. The results of the economic evaluation could provide information about the cost-effectiveness of the intervention and the effects on quality of life. In case of shown effectiveness and cost-effectiveness, the program could be implemented into health services settings.[17]
The technology is developing rapidly, and both researchers and medical professionals are responsible for wider and faster implementation of telemedicine in the health care for the benefit to our patients. The findings suggest that health-care professionals largely support the use of telemedicine in MDT meetings, but are also resistant to closer, wider, and faster integration into the health practices. Despite some difficult barriers, majority of published literature on the subject recognizes the benefits of using technology to support MDT meetings for both patients and health-care professionals. It is the researchers’ responsibility to provide medical professionals with guidance on how to incorporate the technology into the health-care sector in the best possible way. It is important that further research is conducted on telemedical design, evaluation, and long-term sustainability of MDT meetings.[13,31,32,33]
Contributing factors to professional, financial, and health benefits of MDT meetings via telemedicine are summarized in Figure 2.
Figure 2.
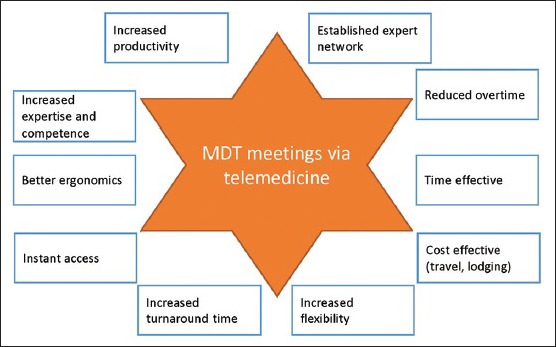
Contributing factors to professional, financial, and health benefits of multidisciplinary team meetings via telemedicine
CONCLUSION
Telemedicine has improved provisions of expert, time, and cost-effective MDT meetings benefiting patients irrespective of location, compared to traditional settings. Technology plays a crucial role in further development of the patient-centered health care. It is important to support collaboration of specialist teams through MDT meetings and address special needs of patients. Further research needs to concentrate on telemedical design, evaluation, and long-term sustainability in MDT meetings.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This review did not receive any specific grant from any funding agency in the public or commercial.
Footnotes
Available FREE in open access from: http://www.jpathinformatics.org/text.asp?2019/10/1/35/271206
REFERENCES
- 1.Tensen E, van der Heijden JP, Jaspers MW, Witkamp L. Two decades of teledermatology: Current status and integration in national healthcare systems. Curr Dermatol Rep. 2016;5:96–104. doi: 10.1007/s13671-016-0136-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Geneva, Switzerland: World Health Organization; 1998. A Health Telematics Policy in Support of WHO's Health-For-All Strategy for Global Health Development: Report of the WHO Group Consultation on Health Telematics. 1997 December 11–16. [Google Scholar]
- 3.Voran D. Telemedicine and beyond. Mo Med. 2015;112:129–35. [PMC free article] [PubMed] [Google Scholar]
- 4.Chaet D, Clearfield R, Sabin JE, Skimming K Council on Ethical and Judicial Affairs American Medical Association. Ethical practice in telehealth and telemedicine. J Gen Intern Med. 2017;32:1136–40. doi: 10.1007/s11606-017-4082-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bartz CC. Nursing care in telemedicine and telehealth across the world. Soins. 2016;61:57–9. doi: 10.1016/j.soin.2016.09.013. [DOI] [PubMed] [Google Scholar]
- 6.Wood L, Williams C, Billings J, Johnson S. The role of psychology in a multidisciplinary psychiatric inpatient setting: Perspective from the multidisciplinary team. Psychol Psychother. 2018 Oct 11; doi: 10.1111/papt.12199. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 7.Song P, Wu Q, Huang Y. Multidisciplinary team and team oncology medicine research and development in China. Biosci Trends. 2010;4:151–60. [PubMed] [Google Scholar]
- 8.Abdulrahman GO., Jr The effect of multidisciplinary team care on cancer management. Pan Afr Med J. 2011;9:20. doi: 10.4314/pamj.v9i1.71195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stalfors J, Björholt I, Westin T. A cost analysis of participation via personal attendance versus telemedicine at a head and neck oncology multidisciplinary team meeting. J Telemed Telecare. 2005;11:205–10. doi: 10.1258/1357633054068892. [DOI] [PubMed] [Google Scholar]
- 10.Slusser W, Whitley M, Izadpanah N, Kim SL, Ponturo D. Multidisciplinary pediatric obesity clinic via telemedicine within the Los Angeles metropolitan area: Lessons learned. Clin Pediatr (Phila) 2016;55:251–9. doi: 10.1177/0009922815594359. [DOI] [PubMed] [Google Scholar]
- 11.Demartines N, Battegay E, Liebermann J, Oberholzer M, Rufli T, Harder F. Telemedicine: Perspectives and multidisciplinary approach. Schweiz Med Wochenschr. 2000;130:314–23. [PubMed] [Google Scholar]
- 12.Haines A, Perkins E, Evans EA, McCabe R. Multidisciplinary team functioning and decision making within forensic mental health. Ment Health Rev (Brighton) 2018;23:185–96. doi: 10.1108/MHRJ-01-2018-0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davison AG, Eraut CD, Haque AS, Doffman S, Tanqueray A, Trask CW, et al. Telemedicine for multidisciplinary lung cancer meetings. J Telemed Telecare. 2004;10:140–3. doi: 10.1258/135763304323070779. [DOI] [PubMed] [Google Scholar]
- 14.Woods L, Cummings E, Duff J, Walker K. Partnering in digital health design: Engaging the multidisciplinary team in a needs analysis. Stud Health Technol Inform. 2018;252:176–81. [PubMed] [Google Scholar]
- 15.de Jong CC, Ros WJ, van Leeuwen M, Witkamp L, Schrijvers G. Professionals’ use of a multidisciplinary communication tool for patients with dementia in primary care. Comput Inform Nurs. 2018;36:193–8. doi: 10.1097/CIN.0000000000000414. [DOI] [PubMed] [Google Scholar]
- 16.Geronimo A, Wright C, Morris A, Walsh S, Snyder B, Simmons Z. Incorporation of telehealth into a multidisciplinary ALS clinic: Feasibility and acceptability. Amyotroph Lateral Scler Frontotemporal Degener. 2017;18:555–61. doi: 10.1080/21678421.2017.1338298. [DOI] [PubMed] [Google Scholar]
- 17.Giordano A, Bonometti GP, Vanoglio F, Paneroni M, Bernocchi P, Comini L, et al. Feasibility and cost-effectiveness of a multidisciplinary home-telehealth intervention programme to reduce falls among elderly discharged from hospital: Study protocol for a randomized controlled trial. BMC Geriatr. 2016;16:209. doi: 10.1186/s12877-016-0378-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Emerson JF, Welch M, Rossman WE, Carek S, Ludden T, Templin M, et al. A multidisciplinary intervention utilizing virtual communication tools to reduce health disparities: A pilot randomized controlled trial. Int J Environ Res Public Health. 2015;13:31. doi: 10.3390/ijerph13010031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Comín-Colet J, Enjuanes C, Verdú-Rotellar JM, Linas A, Ruiz-Rodriguez P, González-Robledo G, et al. Impact on clinical events and healthcare costs of adding telemedicine to multidisciplinary disease management programmes for heart failure: Results of a randomized controlled trial. J Telemed Telecare. 2016;22:282–95. doi: 10.1177/1357633X15600583. [DOI] [PubMed] [Google Scholar]
- 20.Cuperus N, van den Hout WB, Hoogeboom TJ, van den Hoogen FH, Vliet Vlieland TP, van den Ende CH. Cost-utility and cost-effectiveness analyses of face-to-face versus telephone-based nonpharmacologic multidisciplinary treatments for patients with generalized osteoarthritis. Arthritis Care Res (Hoboken) 2016;68:502–10. doi: 10.1002/acr.22709. [DOI] [PubMed] [Google Scholar]
- 21.Cuperus N, Hoogeboom TJ, Kersten CC, den Broeder AA, Vlieland TP, van den Ende CH. Randomized trial of the effectiveness of a non-pharmacological multidisciplinary face-to-face treatment program on daily function compared to a telephone-based treatment program in patients with generalized osteoarthritis. Osteoarthritis Cartilage. 2015;23:1267–75. doi: 10.1016/j.joca.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 22.Vermeulen J, Verwey R, Hochstenbach LM, van der Weegen S, Man YP, de Witte LP. Experiences of multidisciplinary development team members during user-centered design of telecare products and services: A qualitative study. J Med Internet Res. 2014;16:e124. doi: 10.2196/jmir.3195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stern A, Mitsakakis N, Paulden M, Alibhai S, Wong J, Tomlinson G, et al. Pressure ulcer multidisciplinary teams via telemedicine: A pragmatic cluster randomized stepped wedge trial in long term care. BMC Health Serv Res. 2014;14:83. doi: 10.1186/1472-6963-14-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Watanabe SM, Fairchild A, Pituskin E, Borgersen P, Hanson J, Fassbender K. Improving access to specialist multidisciplinary palliative care consultation for rural cancer patients by videoconferencing: Report of a pilot project. Support Care Cancer. 2013;21:1201–7. doi: 10.1007/s00520-012-1649-7. [DOI] [PubMed] [Google Scholar]
- 25.Miller DM, Moore SM, Fox RJ, Atreja A, Fu AZ, Lee JC, et al. Web-based self-management for patients with multiple sclerosis: A practical, randomized trial. Telemed J E Health. 2011;17:5–13. doi: 10.1089/tmj.2010.0133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huis in ‘t Veld RM, Widya IA, Bults RG, Sandsjö L, Hermens HJ, Vollenbroek-Hutten MM. A scenario guideline for designing new teletreatments: A multidisciplinary approach. J Telemed Telecare. 2010;16:302–7. doi: 10.1258/jtt.2010.006003. [DOI] [PubMed] [Google Scholar]
- 27.Castelnuovo G, Manzoni GM, Cuzziol P, Cesa GL, Tuzzi C, Villa V, et al. TECNOB: Study design of a randomized controlled trial of a multidisciplinary telecare intervention for obese patients with type-2 diabetes. BMC Public Health. 2010;10:204. doi: 10.1186/1471-2458-10-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Washington KT, Demiris G, Oliver DP, Day M. Telehospice acceptance among providers: A multidisciplinary comparison. Am J Hosp Palliat Care. 2008;25:452–7. doi: 10.1177/1049909108322289. [DOI] [PubMed] [Google Scholar]
- 29.Kunkler IH, Fielding RG, Brebner J, Prescott R, Maclean JR, Cairns J, et al. A comprehensive approach for evaluating telemedicine-delivered multidisciplinary breast cancer meetings in Southern Scotland. J Telemed Telecare. 2005;11(Suppl 1):71–3. doi: 10.1258/1357633054461804. [DOI] [PubMed] [Google Scholar]
- 30.Vodovnik A, Aghdam MR. Complete routine remote digital pathology services. J Pathol Inform. 2018;9:36. doi: 10.4103/jpi.jpi_34_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Delaney G, Jacob S, Iedema R, Winters M, Barton M. Comparison of face-to-face and videoconferenced multidisciplinary clinical meetings. Australas Radiol. 2004;48:487–92. doi: 10.1111/j.1440-1673.2004.01349.x. [DOI] [PubMed] [Google Scholar]
- 32.Simpson S, Knox J, Mitchell D, Ferguson J, Brebner J, Brebner E. A multidisciplinary approach to the treatment of eating disorders via videoconferencing in North-East Scotland. J Telemed Telecare. 2003;9(Suppl 1):S37–8. doi: 10.1258/135763303322196286. [DOI] [PubMed] [Google Scholar]
- 33.Axford AT, Askill C, Jones AJ. Virtual multidisciplinary teams for cancer care. J Telemed Telecare. 2002;8(Suppl 2):3–4. doi: 10.1177/1357633X020080S202. [DOI] [PubMed] [Google Scholar]


