Abstract
Purpose: This study was conducted to investigate the epidemiology behind the increased incidence of infant salmonella cases in Qatar during 2017 and identify the possible risk factors. Methods: This was a cross-sectional study using the notification reports of laboratory-confirmed infant salmonella cases received by the Ministry of Public Health during the year 2017. Furthermore, complementary phone interviews with the infants’ mothers using a validated questionnaire were conducted. Results: The infant salmonella attack rate was calculated at approximately 3.23 cases per 1000 infants. Among the 89 confirmed infant salmonella cases, there were more girls (53%) than boys (47%) with a median age of 8 months. The most common type of salmonella species isolated was group B (50.5%). Among the 59 infant cases whose mothers were interviewed, the majority (94.9%) were symptomatic and diarrhea was the main reported symptom (90%), particularly bloody diarrhoea (62%). Regarding their dietary consumption, the majority (69.5%) of the infected infants were formula-fed. Moreover, the majority reported having no pets at home (91.6%) and were not enrolled in a day care center (93.3%). Conclusion: This study revealed a high incidence of salmonella infection among infants in the State of Qatar, which poses a public health concern. Therefore, targeted interventions and health awareness programs are required for outbreak prevention, detection and control.
Keywords: salmonella, outbreak, infants
Introduction
Nontyphoidal salmonella has emerged as a public health priority as well as one of the four key global causes of diarrheal illnesses, which affect 550 million people annually, including 220 million children aged less than 5 years.1 Salmonella is primarily transmitted to humans through the consumption of contaminated animal-derived food products, contact with infected animals (natural reservoir), or person-to-person spread. Moreover, the World Health Organization (WHO) has called for ensuring food safety through the prevention, detection, and management of foodborne risks along the entire food system from production to consumption.2,3
Salmonella infection generally presents as a self-limiting gastroenteritis. However, the disease may become severe and lethal among certain subpopulations, especially infants. The symptoms typically appear 6–72 hours after the ingestion of salmonella and persist for 2–7 days.1,4 Subsequently, salmonella infection has been associated with several complications such as bacteremia, dehydration, and reactive arthritis.5 Moreover, infants are at a higher risk of contracting salmonella due to several factors such as consumption of contaminated powdered formula milk, attendance of a day care center, contact with a person having gastrointestinal illness, consumption of contaminated foods (egg/meat/poultry), contact with pets, and low maternal education level. In contrast, protective factors against infant salmonella include breastfeeding, increasing infant age (months), and consumption of home-prepared food.6–8
Several salmonella outbreaks have been recorded and investigated by public health authorities in Qatar. A review of all laboratory-confirmed salmonella cases between 2004 and 2012 revealed an increased incidence of the disease among children aged less than 3 years. In addition, the most frequently reported salmonella serotypes were type B (41.9%), type D (26.9%), and type C1 (12.2%).9
Furthermore, a case–control study (n = 423) was conducted at Hamad Medical Corporation's (HMC) hospitals, the country's major provider of secondary and tertiary health care services, between 2009 and 2012. Subsequently, salmonella infection was revealed to be one of the most common causes of food poisoning across the country. In addition, the annual incidence of salmonella cases fluctuated over the years between 2006 and 2012 from 12.3 up to 30.3 cases per 100,000 population. Similarly, the highest number of recorded salmonella cases was among children aged below 5 years.10,11
In Qatar, a national surveillance system has been established for the early detection and response to any potential foodborne disease outbreak. There are 78 notifiable communicable diseases in the country that should be reported by law to the Communicable Disease Control and Prevention section at the Ministry of Public Health (MoPH). In 2017, the rate of salmonella infection among infants increased to 89 cases, which indicated an obvious spike in the total number of cases from 45, 66, 75, and 73 cases in 2013, 2014, 2015, and 2016, respectively. Moreover, little was known about the possible sources of infection among this high-risk population, which prompted the country's public health officials to question the source, behavior, and practice associated with the outbreak. Such information can be used in the development and implementation of effective prevention and control strategies. Therefore, we aimed to investigate the epidemiology behind the increased incidence of infant salmonella cases in Qatar during 2017 and identify the possible associated factors.
Methodology
This cross-sectional study was conducted at the MoPH, which is the sole authority in the State of Qatar that receives notifications from all governmental and private healthcare facilities across the country as a part of its passive national surveillance efforts. The national surveillance system in Qatar categorizes notifiable infectious diseases into two classes based on national and international regulations. The diseases that are immediately notifiable (within 24 hours) by telephone or fax are designated as Class A, while those that may be notified as soon as possible (up to 1 week) are denoted as Class B. As of 2018, the list of notifiable diseases in the State of Qatar encompassed 78 diseases, including salmonella infection, which is classified as Class A.
Study population
The eligibility criteria included all infant (up to 12 months) with laboratory-confirmed salmonella infection, regardless of gender or nationality, and reported to the MoPH from January 1 to December 31, 2017. An infant salmonella case is defined based on positive stool analysis or blood test to any of the salmonella species in children aged less than one year.
Measures
The primary variables in this study were extracted from the relevant notification forms and included demographic information (age, gender, nationality) and illness-related data (date of diagnosis, date of reporting, reporting healthcare facility, type of sample taken, and salmonella group). Furthermore, contact details were extracted for a complementary phone interview (10–20 minutes) by one of three trained investigators. Upon contacting the infants’ mothers, adequate information was provided about the overall cross-sectional study and verbal consent was obtained before initiating any interview.
All procedures performed in this study were in accordance with the ethical standards and the 1964 Declaration of Helsinki and its later modifications. The MoPH ethics committee approved this study. Furthermore, no identifying information was gathered from the respondents and the collected data were maintained confidential through a password-protected computer with access restricted to the principal investigator.
The questionnaire
A questionnaire was developed based on a thorough literature review and expert opinion to include all the relevant factors associated with salmonella infection among infants, considering the local situation.2,7 The questionnaire was developed in a structured manner to elicit demographic characteristics (e.g., age, sex, nationality, and maternal education level) as well as other key epidemiological factors related to environmental exposure (e.g., day care attendance, contact with pets, and contact with sick people), dietary history (e.g., consumption of milk, meat, chicken, eggs, and infant feeding practices), and family kitchen practices (e.g., food storage and surface cleaning practices). The questionnaire included exposure variables relating to the 7-day period before the onset of disease. It encompassed 34 major questions of various formats (close-ended, open-ended, and multiple-choice).
Next, the face validity of the questionnaire was established through a comprehensive review by epidemiologists and public health specialists at the MoPH. The questionnaire was then pilot-tested among ten mothers of healthy infants through phone interviews. Subsequently, adequate modifications were introduced to the final version of the questionnaire.
Statistical analysis
The collected data were input into the Statistical Package of Social Sciences (SPSS, v.22), and adequate statistical analysis was conducted. Mean, standard deviation, and median values were calculated for continuous variables, while percentages were calculated for categorical variables.
Results
Overall, there were 89 infants that fitted the case definition for salmonella infection. Among the 89 mothers contacted, 59 responded (response rate = 66.3%) and all agreed to participate in the study, whereas 30 were inaccessible to the investigators’ calls. The investigators attempted to contact the potential participants three times before labeling them as inaccessible.
The infant salmonella attack rate was calculated at approximately 3.23 cases per 1000 infants (based on the 2017 population estimates for the infant age group during the first year of life). Regarding the incidence of infant salmonella cases, the number of notifications peaked twice as shown in Figure 1.
Figure 1.
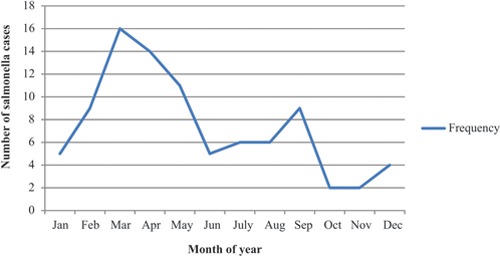
The epidemic curve of the infant salmonella outbreak during 2017 in Qatar.
Among the 89 recorded infant salmonella cases, the median age was 8 months and there were more girls (53%) than boys (47%). Moreover, almost one-sixth (17%) of the cases were Qatari; whereas the remaining cases were distributed among 23 nationalities such as Egyptians (11%), Indians (11%), and Pakistanis (9%). Approximately three-quarters (70.8%) of the reported cases were aged between 7 and 12 months. Moreover, the mean rank ( ± SD) of the sick infant among siblings was 2.14 ( ± 1.23). Among the 59 cases whose mothers were interviewed by phone, the majority (94.9%) were symptomatic. Moreover, diarrhea was the most commonly reported symptom (90%), especially bloody diarrhoea (62%) rather than that with mucous (15%) (Table 1).
Table 1.
General characteristics of infant salmonella cases in Qatar in 2017.
| Variable | Number (%) |
|
| |
| Infant age in months (n = 89) | |
|
| |
| 1-3 | 9 (10.1) |
|
| |
| 4-6 | 17 (19.1) |
|
| |
| 7-9 | 28 (31.5) |
|
| |
| 10-12 | 35 (39.3) |
|
| |
| Infant gender (n = 89) | |
|
| |
| Male | 42 (47.0) |
|
| |
| Female | 47 (53.0) |
|
| |
| Nationality (n = 89) | |
|
| |
| Qatari | 15 (17.0) |
|
| |
| Non-Qatari | 74 (83.0) |
|
| |
| Rank of sick child among siblings (n = 58) | |
|
| |
| 1 | 21 (36.2) |
|
| |
| 2 | 22 (37.9) |
|
| |
| ≥ 3 | 15 (25.9) |
|
| |
| Symptoms (n = 57) * | |
|
| |
| Diarrhoea | 54 (90.0) |
|
| |
| Vomiting | 17 (28.5) |
|
| |
| Abdominal colic | 11 (18.5) |
|
| |
*Some cases reported more than one symptom.
Regarding the characteristics of the mothers of infants with salmonella infection, the mean ( ± SD) age of the interviewed mothers was 30 years ( ± 5.07). The mean ( ± SD) number of children per mother was 2.24 ( ± 1.27) (Table 2).
Table 2.
General characteristics of the mothers of infant salmonella cases in Qatar in 2017.
| Variable | Number (%) |
|
| |
| Mothers’ age in years (n = 58) | |
|
| |
| Below 30 | 29 (50.0) |
|
| |
| 30 and above | 29 (50.0) |
|
| |
| Level of education (n = 59) | |
|
| |
| Primary and secondary | 18 (30.5) |
|
| |
| University and above | 41 (69.5) |
|
| |
| Employment (n = 59) | |
|
| |
| Employed | 20 (33.9) |
|
| |
| Unemployed | 39 (66.1) |
|
| |
| Number of children per mother (n = 59) | |
|
| |
| 1 | 20 (33.9) |
|
| |
| 2 | 21 (35.6) |
|
| |
| ≥ 3 | 18 (30.5) |
|
| |
Regarding the type of sample collected for identifying the cases of salmonella, the majority (97.75%) of notifications cited stool samples as a confirmatory test. Based on data retrieved from HMC's central laboratory, the most common type of salmonella species isolated from the collected samples was group B (50.5%) (Figure 2).
Figure 2.
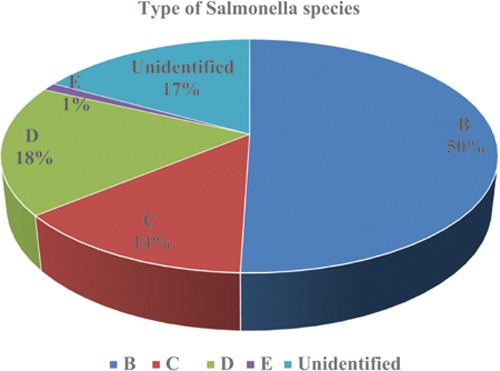
Type of Salmonella species isolated among the infant salmonella cases (n = 89).
Regarding the infants’ dietary habits, the mean age ( ± SD) of solid food introduction was 5.83 months ( ± 1.61) after which more than two-thirds (70.8%) of the cases occurred (Figure 3). During the week before the onset of symptoms, the majority (69.5%) of infants were formula-fed and the source of water used in preparing the formula was bottled water (85.2%) or boiled municipal tap water (14.8%). Almost one-third of the diseased infants were reported to have consumed food containing eggs (35.6%) or chicken (32.2%). In addition, more than one-fifth (22%) of the cases were given food from outside the household. The majority (91.7%) reported having no pets at home and were not previously exposed to any sick contact (67.8%) (Table 3). Mothers (81.7%) were the primary providers of food for their infants; whereas, almost a quarter (23.3%) of the infants with salmonella infection received food prepared by their nannies. Moreover, the majority (93.3%) of infants were not enrolled in a day care center. Finally, less than one-fifth (17.9%) of the respondents reported traveling abroad with their infants during the week before the onset of illness.
Figure 3.
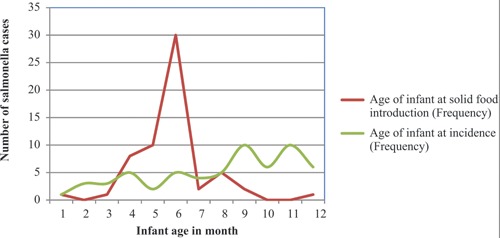
Variation in solid food introduction and infant salmonella incidence by age (months) in Qatar in 2017.
Table 3.
Possible associated factors among infant salmonella cases in Qatar in 2017 (n = 59).
| Variable | Number (%) |
|
| |
| Source of milk (n = 59) | |
|
| |
| Breastfeeding | 6 (10.2) |
|
| |
| Formula feeding | 41 (69.5) |
|
| |
| Mixed feeding | 12 (20.3) |
|
| |
| Egg consumption | |
|
| |
| Yes | 21 (35.6) |
|
| |
| No | 32 (54.2) |
|
| |
| Not sure | 6 (10.2) |
|
| |
| Chicken consumption | |
|
| |
| Yes | 19 (32.2) |
|
| |
| No | 35 (59.3) |
|
| |
| Not sure | 5 (8.5) |
|
| |
| Eat from outside | |
|
| |
| Yes | 13 (22.0) |
|
| |
| No | 40 (67.8) |
|
| |
| Not sure | 6 (10.2) |
|
| |
| History of contact with a sick person | |
|
| |
| Yes | 8 (13.6) |
|
| |
| No | 40 (67.8) |
|
| |
| I do not remember | 11 (18.6) |
|
| |
| Having a pet at home | |
|
| |
| Yes | 5 (8.4) |
|
| |
| No | 54 (91.6) |
|
| |
Regarding the family kitchen practices, the majority (98.3%) of the contacted mothers reported storing all eggs in the refrigerator. Furthermore, all mothers acknowledged the practice of cleaning the preparation surface of their infants’ meals through either soap and water (35%) or disinfectants (35%) or both techniques (30%). Similarly, they reported separating raw chicken, meat or eggs from vegetables during storage or preparation process.
Discussion
During 2017, Qatar's public health authorities documented an increase in infant salmonella cases. The incidence of salmonella infection among infants in Qatar peaked once during March (16 cases) and again during September (9 cases). Therefore, a continuous epidemic was suspected.
The attack rate of salmonella infection among infants was calculated at 3.23 cases per 1000 infants. Furthermore, an earlier study of the national salmonella surveillance data in 2016 reported that children aged less than three years comprised almost half of the reported cases.10 Globally, similar salmonella outbreaks have been reported among infants during 2017. In December of the same year, a salmonella outbreak was identified among infants in France.12 In addition, salmonella outbreaks were reported primarily by countries that import infant formula products from France, such as Qatar, Saudi Arabia, Switzerland, Taiwan, Turkey, United Arab Emirates, Kuwait, and others.13 This influenced our hypothesis given that the majority (69.5%) of the infected infants in Qatar were formula-fed. Therefore, it was suspected that exported milk formulas from France might be behind this outbreak. Moreover, laboratory serotyping of the collected samples identified that salmonella serotype B accounted for half of the reported cases, which is similar to the results reported by an earlier study on national salmonella surveillance data between 2004 and 2012.10 In addition, salmonella serotype B serovar Agona was identified as the primary culprit in the global outbreaks of formula-related salmonella during 2017.13 However, the specific serovar behind the outbreak in Qatar was not identified because no further serotyping was attempted at the time.
Regarding their dietary habits, it was found that solid food was introduced to three-quarters of the infants during the first 6 months of life, while more than two-thirds (72%) of the infants contracted salmonella at the age of 7 months and above. This reiterates earlier findings in the literature that contaminated food poses a major source of salmonella infection among infants. Moreover, almost a third of the sick infants consumed food containing eggs (35%) or chicken (31.7%) during the week before the onset of symptoms. Therefore, it is possible that such foods may have contributed to the infant salmonella outbreak.14 However, the exact source of salmonella infection in the current outbreak remains obscure. In addition, the role of breastfeeding as a protective factor was substantiated because the majority of the infant salmonella cases were not breastfed.
In the present study, it was observed that the majority (93.3%) of the infant salmonella cases were not enrolled in a day care center. On the other hand, the literature has described a two to three times increased risk of acquired infections among infants attending nurseries;15 however, only 7% of the infants attended day care centers in the current outbreak, which indicates that nursery attendance was poorly linked with infant salmonella infection. Furthermore, the lack of hygiene among caregivers in such settings has been identified as a risk factor for outbreaks.16 Nevertheless, subsequent investigations revealed the prevalence of good hygiene practice among the caregivers in the abovementioned nurseries.
Moreover, contact with pets has been associated with salmonella infection among infants throughout the literature. Similarly, contact with frogs has been linked to salmonella infection in Spain, while that with poultry was interrelated to salmonella cases in Washington.17,18 Furthermore, a case–control study conducted among children in Michigan revealed that exposure to cats makes children three times at risk of salmonella infection compared with controls (MOR = 2.53, 95% CI: 1.14–5.88). In addition, children who reported contact with reptiles had seven times more risk to become infected with salmonella.2,19 However, the majority (91.7%) of caregivers in Qatar denied possessing any pets, which in turn refutes the role of pets in the salmonella outbreak among infants.
This cross-sectional study provides an epidemiological description of the outbreak and will serve as a basis for future research as well as the implementation of control measures. This study has also reported an acceptable response rate to the phone interview (66.3%) compared to the typical low telephone response rate (27%) seen in 2017 among marketing industries.19 However, approximately 30% nonresponse bias could affect the reliability and validity of the results of a cross-sectional study. The primary limitation of this cross-sectional study is that its retrospective nature could not establish a definite temporal relationship and might introduce some recall bias. Furthermore, the numbers of cases associated with this outbreak are probably underestimated because patients with mild symptoms may not have consulted a healthcare professional nor had comprehensive diagnostic investigations (stool sample, culture, and identification of serotype). In addition, the current epidemiological investigation did not generate any strong hypothesis about the vehicle or the source of infection with regards to the infant salmonella outbreak of Qatar during 2017.
Conclusion
The high incidence of salmonella among infants in the State of Qatar poses a public health concern. Therefore, targeted interventions and health awareness programs are required for outbreak prevention, detection and control. Similarly, more public health efforts should be invested in the promotion of exclusive breastfeeding and proper hygiene practices among the caregivers of infants in the country. Moreover, there is a need to strengthen the salmonella surveillance system in Qatar, with a special emphasis on the laboratory aspect.
Funding
This research received no external funding.
Acknowledgements
None.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1. Center for Disease Control and Prevention (CDC). Surveillance [Internet]. [updated 2019 Feb 8; cited 2018 May 29]. Available from: https://www.cdc.gov/Salmonella/reportspubs/surveillance.html.
- 2.Younus M, Wilkins MJ, Davies HD, Rahbar MH, Funk J, Nguyen C et al. The role of exposures to animals and other risk factors in sporadic, non-typhoidal Salmonella infections in Michigan children. Zoonoses Public Health. 2010;57(7-8):e170–e176. doi: 10.1111/j.1863-2378.2010.01324.x. [DOI] [PubMed] [Google Scholar]
- 3. World Health Organization (WHO). Food safety [Internet]. [Updated 2019 Jun 04; cited 2018 Aug 14]. Available from: http://www.who.int/en/news-room/fact-sheets/detail/food-safety.
- 4.Baron S. Medical Microbiology. 4th ed. Galveston (TX): University of Texas Medical Branch at Galveston; 1996. [PubMed] [Google Scholar]
- 5.Kliegman R, Stanton B, St. Geme J, Schor N, Behrman R, Nelson W. Nelson textbook of pediatrics. 20th ed. Philadelphia: Elsevier; 2015. [Google Scholar]
- 6.Williams S, Markey P, Harlock M, Binns P, Gaggin J, Patel M. Individual and household-level risk factors for sporadic salmonellosis in children. J Infect. 2016;72(1):36–44. doi: 10.1016/j.jinf.2015.09.014. [DOI] [PubMed] [Google Scholar]
- 7.Younus M, Wilkins MJ, Davies HD, Rahbar MH, Funk J, Nguyen C et al. Case-control study of disease determinants for non-typhoidal Salmonella infections among Michigan children. BMC Res Notes. 2010;3(1):105. doi: 10.1186/1756-0500-3-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen CJ, Wu FT, Hsiung CA, Chang WC, Wu HS, Wu CY et al. Risk factors for salmonella gastroenteritis in children less than five years of age in Taiwan. Pediatr Infect Dis J. 2012;31(12):e239–e243. doi: 10.1097/INF.0b013e31826ff592. [DOI] [PubMed] [Google Scholar]
- 9.Nazzal Z, Said H, Al-Hajiri M, Tamim O. Salmonella food poisoning associated with macaroni salad in a labourers camp-state of Qatar, 2010. J Community Med Health Educ. 2012;2:1–4. [Google Scholar]
- 10.Farag E, Garcell HG, Ganesan N, Ahmed SN, Al-Hajri M, Al Thani SM et al. A retrospective epidemiological study on the incidence of salmonellosis in the State of Qatar during 2004-2012. Qatar Med J. 2016;2016(1):3. doi: 10.5339/qmj.2016.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weam B, Abraham M, Doiphode S, Peters K, Ibrahim E, Sultan A et al. Foodborne bacterial pathogens associated with the risk of gastroenteritis in the state of Qatar. Int J Health Sci (Qassim) 2016;10(2):197–207. [PMC free article] [PubMed] [Google Scholar]
- 12.Jourdan-da NS, Fabre L, Robinson E, Fournet N, Nisavanh A, Bruyand M et al. Ongoing nationwide outbreak of Salmonella Agona associated with internationally distributed infant milk products, France. Euro Surveill. 2018;23(2) doi: 10.2807/1560-7917.ES.2018.23.2.17-00852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. World Health Organization-Disease outbreak news. Outbreak of Salmonella Agona infections linked to internationally distributed infant formula-France [Internet]. [updated 2017 Dec 22; cited 2017 Dec 25]. Available from: https//wwwwhoint/csr/don/22-december-2017-salmonella-agona-infections-france/en/
- 14.World Health Organization. Rome: World Health Organization, Food and Agriculture Organization of the United Nations; 2002. Risk assessments of Salmonella in eggs and broiler chickens. [Google Scholar]
- 15.Gurgel RQ, Correia JD. Infectious diseases and daycare and preschool education. J Pediatr (Rio J) 2017;83(6):299–312. doi: 10.2223/JPED.1734. [DOI] [PubMed] [Google Scholar]
- 16.Thompson CN, Phan VT, Le TP, Pham TN, Hoang LP, Ha V et al. Epidemiological features and risk factors of Salmonella gastroenteritis in children resident in Ho Chi Minh City. Vietnam. Epidemiol Infect. 2013;141(8):1604–1613. doi: 10.1017/S0950268812002014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lafuente S, Bellido J, Moraga FA, Herrera S, Yagüe A, Montalvo T et al. Salmonella paratyphi B and Salmonella litchfield outbreaks associated with pet turtle exposure in Spain. Enferm Infecc Microbiol Clín. 2013;31(1):32–35. doi: 10.1016/j.eimc.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 18.Kauber K, Fowler H, Lipton B, Meschke JS, Rabinowitz P. Salmonella Knowledge, Attitudes and Practices: A Survey of Backyard Poultry Owners Residing in Seattle, Washington and the Surrounding Metropolitan Area. Zoonoses Public Health. 2016;64(1):21–28. doi: 10.1111/zph.12274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Telephone survey response rates have plunged, but may finally be stabilizing–marketing charts [Internet]. [Updated 2018 Jan 16; cited 2018 Sep 26]. Available from: https://www.marketingcharts.com/industries/market-research-81996.