Abstract
Crystal-induced acute kidney injury (AKI) is caused by the intratubular precipitation of crystals, which results in obstruction and kidney injury. Levofloxacin is commonly used fluoroquinolone antibiotic especially for respiratory and urinary tract infections. It rarely causes any serious adverse events. Several cases of crystal nephropathy after ciprofloxacin use have been reported. Pre-existing renal dysfunction, high dose of the drug, and advanced age are considered as risk factors. To best of our knowledge, only two cases of crystal nephropathy due to levofloxacin use have been reported, we add a new one to it. The patient responded to conservative treatment with complete recovery on follow-up.
Keywords: Acute kidney injury, crystal nephropathy, levofloxacin
Introduction
Crystal induced acute kidney injury (AKI) is caused by the intratubular precipitation of crystals, which results in obstruction. Acute uric acid nephropathy and drugs or toxins are the two most common causes. Common drugs implicated in causing crystal induced AKI include acyclovir, sulphonamide antibiotics, methotrexate, and protease inhibitors. Other agents that have been described in case reports to cause crystal-induced AKI include orlistat, oral sodium phosphate purgatives, ciprofloxacin, and high-dose amoxicillin. Levofloxacin is another quinolone antibiotic commonly used for respiratory and urinary tract infections. Common side effects of levofloxacin are similar to other fluoroquinolones and include nausea (7%), headache (6%), diarrhea (5%), insomnia (4%), dizziness (3%), constipation (3%), abdominal pain (2%), dyspepsia (2%), and vomiting (2%). Although several cases have been reported of crystal nephropathy associated with ciprofloxacin,[1] levofloxacin crystal nephropathy, to the best of our knowledge, only two cases reported before.[2,3] We report a case of oliguric AKI secondary to levofloxacin-induced crystal nephropathy.
Case Report
A 37-year-old male came to our outpatient department with history of oliguria since 3 days. He had fever and cough with expectoration 5 days ago, for which at a local hospital he was started on injectable levofloxacin 500 mg once a day and oral paracetamol 500 mg thrice daily. He had reduced oral intake since onset of symptoms, which suggest that patient was dehydrated at start of treatment. Two days later, he started complaining of decreased urine output and investigations showed elevated serum creatinine of 4.1 mg/dL, for which he was referred to our center. He had pulmonary tuberculosis 1 year ago for which he received antitubercular therapy for 6 months. At admission routine investigations revealed serum creatinine 6.1 mg/dL, hemoglobin 10 g/dL, WBC 10400/mm3, neutrophils 80%, lymphocytes 15%, monocytes 3%, eosinophils 2%, platelet count 1.8 lakhs/mm3. Blood gas analysis revealed mild to moderate metabolic acidosis. No abnormality detected on peripheral blood smear. Urine examination showed trace proteins and no active sediments. Spot urine protein to creatinine ratio was 0.31 mg/mmol and 24 hour urine proteins was 100 mg/day. HIV, hepatitis C virus, and hepatitis B virus infections were ruled out. Ultrasound abdomen was unremarkable with bilateral normal size kidneys. His autoimmune workup was negative for anti-nuclear antibodies, anti-double stranded DNA antibodies, anti-neutrophil cytoplasmic antibodies, and complement levels were within normal limits. Serum creatinine increased to 7.5 mg/dL during the ward course. So renal biopsy was performed, and light microscopy showed normal glomeruli and circumferential, luminal refractive crystals in tubules [Figure 1]. Crystals were polygonal to needle shaped and showed reddish white polarization [Figure 2]. Electron microscopy showed electron lucent crystalline structures in tubules [Figure 3]. These features are consistent with crystal nephropathy. Immunofluorescence was negative for immunoglobulins, complements, and light chains. So, 24 hour urinary oxalate levels were done which were within normal limits; however, 24 hour urine excretion values might be fallacious in setting of renal failure. So, drug-induced crystal nephropathy was suspected and levofloxacin was stopped. Patient was observed and serum creatinine was monitored. Two days after stopping levofloxacin serum creatinine reduced to 3.5 mg/dL and urine output started improving. One week later serum creatinine was 1.8 mg/dL and patient was discharged in stable condition. After 1 week and 1 month post discharge his serum creatinine levels were 1.2 and 0.9 mg/dL, respectively.
Figure 1.
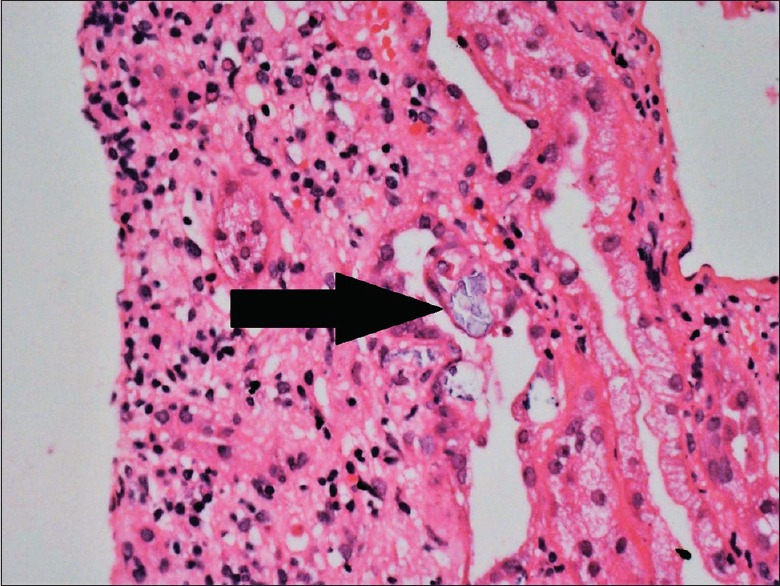
Circumferential, luminal refractive crystals in tubules
Figure 2.
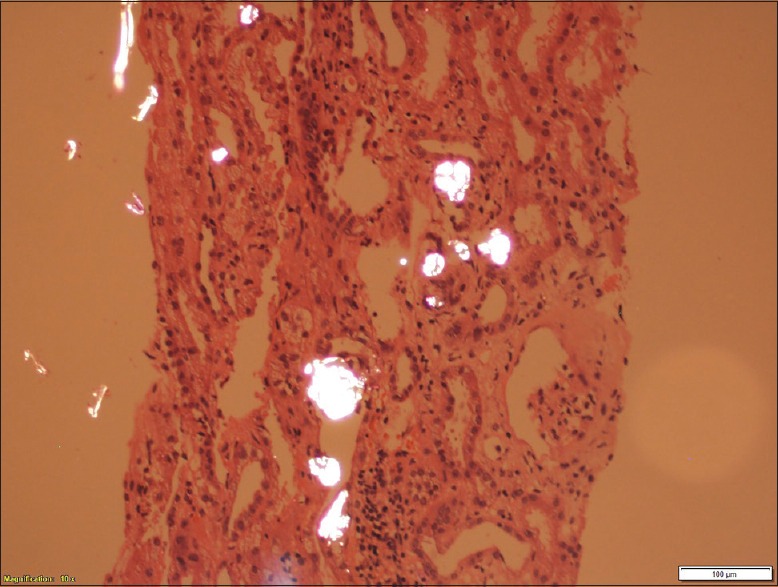
Reddish white polarized crystals
Figure 3.
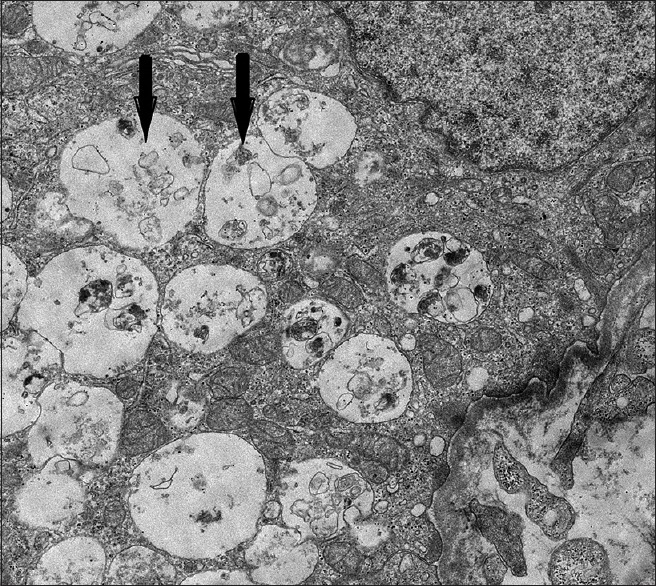
Electron lucent crystalline structures in tubules
Discussion
Levofloxacin is a commonly used antibiotic that can very rarely cause crystal nephropathy.[2] Crystal-induced AKI most commonly occurs as a result of acute uric acid nephropathy and following the administration of drugs or toxins that are poorly soluble or have metabolites that are poorly soluble in urine.[4,5] Common drugs implicated in causing crystal induced AKI include acyclovir, sulphonamide antibiotics, methotrexate, and protease inhibitors. Other agents that have been described in case reports to cause crystal-induced AKI include orlistat, oral sodium phosphate purgatives, ciprofloxacin, and high-dose amoxicillin. These crystals usually precipitate in distal tubules, obstruct urine flow, and elicit interstitial inflammation. Crystal precipitation depends on the concentration of the drug in urine and urinary pH.[6] Sulfadiazine and methotrexate tend to precipitate in tubule when urine pH is low.[7,8] Acyclovir intratubular precipitation is increased in alkaline urine.[9] Cases of AKI due to crystal nephropathy and rhabdomyolysis due to ciprofloxacin have been reported.[10,11] Renal injury due to levofloxacin is very rare. Our patient's urine analysis showed acidic urine without any crystals or casts, unlike alkaline urine pH in which such crystals form.[6] Urine pH in our case was measured by dipstick method, which is also an accurate and sensitive way of measuring urine pH. Acidic urine pH could be due to compensation for metabolic acidosis in our patient. Moreover, crystals due to fluoroquinolones can be formed either in acidic or alkaline urine pH as reported and discussed in article published by Baird et al.[3] He received intravenous fluids at admission leading to dilution of urine, which can cause difficulty in detection of crystals in screened urine sample. This can be a reason for absence of crystalluria in our patient. Previous cases have been described after receiving levofloxacin.[2,3] Pre-existing renal dysfunction, high-dose medication, volume depletion, and old age predispose to this complication.[12] Liu et al.[2] in 2015 described the first case of levofloxacin-induced crystal nephropathy in 64-year-old diabetic women. Baird et al.[3] reported crystal nephropathy secondary to pomalidomide and levofloxacin. History of levofloxacin intake, absence of evidence of other causes, and resemblance of crystal morphology in renal biopsy specimens with levofloxacin crystals in index cases have led to the diagnosis of levofloxacin-induced crystal nephropathy in our case. Our patient was managed conservatively and improved completely after stopping levofloxacin, without steroids or dialysis requirement which further confirms the diagnosis. We report and add to the list, a case of levofloxacin-induced crystal nephropathy. Thus, we conclude that patients on levofloxacin therapy should be monitored for renal function tests and if develops renal failure must be evaluated for crystal nephropathy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patient understands that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sedlacek M, Suriawinata AA, Schoolwerth A, Remillard BD. Ciprofloxacin crystal nephropathy – A 'new' cause of acute renal failure. Nephrol Dial Transplant. 2006;21:2339–40. doi: 10.1093/ndt/gfl160. [DOI] [PubMed] [Google Scholar]
- 2.Liu Y, He Q, Wu M. Levofloxacin-induced crystal. Nephrology. 2015;20:437–42. doi: 10.1111/nep.12405. [DOI] [PubMed] [Google Scholar]
- 3.Baird P, Leung S, Hoang H, Babalola O, Devoe CE, Wanchoo R, et al. A case of acute kidney injury from crystal nephropathy secondary to pomalidomide and levofloxacin use. J Oncol Pharm Pract. 2016;22:357–60. doi: 10.1177/1078155214568581. [DOI] [PubMed] [Google Scholar]
- 4.Perazella MA. Crystal-induced acute renal failure. Am J Med. 1999;106:459–65. doi: 10.1016/s0002-9343(99)00041-8. [DOI] [PubMed] [Google Scholar]
- 5.Teichman JM. Clinical practice. Acute renal colic from ureteral calculus. N Engl J Med. 2004;350:684–93. doi: 10.1056/NEJMcp030813. [DOI] [PubMed] [Google Scholar]
- 6.Thorsteinsson SB, Bergan T, Oddsdottir S, Rohwedder R, Holm R. Crystalluria and ciprofloxacin, influence of urinary pH and hydration. Chemotherapy. 1986;32:408–17. doi: 10.1159/000238444. [DOI] [PubMed] [Google Scholar]
- 7.Sasson JP, Dratch PL, Shortsleeve MJ. Renal US findings in sulfadiazine-induced crystalluria. Radiology. 1992;185:739–40. doi: 10.1148/radiology.185.3.1438755. [DOI] [PubMed] [Google Scholar]
- 8.Abelson HT, Fosburg MT, Beardsley GP, Goorin AM, Gorka C, Link M, et al. Methotrexate-induced renal impairment: Clinical studies and rescue from systemic toxicity with high-dose leucovorin and thymidine. J Clin Oncol. 1983;1:208–16. doi: 10.1200/JCO.1983.1.3.208. [DOI] [PubMed] [Google Scholar]
- 9.Obada EN, Level G, Mathieu P, Parent X, Gilson B, Bindi P. Acute renal failure following a treatment with acyclovir. Nephrol Ther. 2010;6:125–7. doi: 10.1016/j.nephro.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 10.Goli R, Mukku KK, Raju SB, Uppin MS. Acute ciprofloxacin-induced crystal nephropathy with granulomatous interstitial nephritis. Indian J Nephrol. 2017;27:231–3. doi: 10.4103/0971-4065.200522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khammassi N, Abdelhedi H, Mohsen D, Ben Sassi M, Cherif O. Rhabdomyolysis and acute renal failure secondary to ciprofloxacin therapy. Therapie. 2012;67:67–8. doi: 10.2515/therapie/2012005. [DOI] [PubMed] [Google Scholar]
- 12.Kammoun K, Jarraya F, Makni S, Ben Mahmoud L, Kharrat M, Ben Hmida M, et al. Ciprofloxacin-induced crystal nephropathy. Iran J Kidney Dis. 2014;8:240–2. [PubMed] [Google Scholar]


