Dear Editor,
Epstein-Barr virus (EBV)-associated lymphoproliferative disorders (LPD) involved in the gastrointestinal tract are rarely encountered, especially in an immunocompetent patient (1). A review of the English literature revealed only 9 published cases. Here, we report the case of EBV-associated NK/T-cell LPD with colonic involvement that eventually developed into hemophagocytic syndrome in a patient from China.
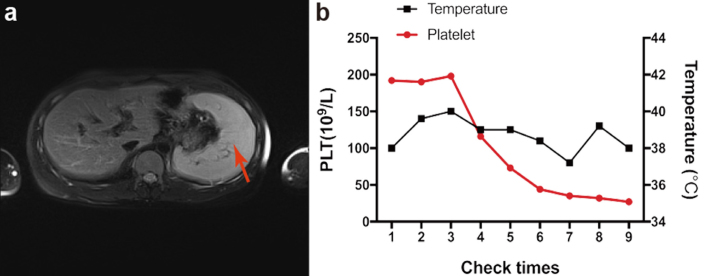
A 22-year-old young man was admitted to our department for left next abdominal pain and fever since 1 month. He had no significant medical background or family history. Physical examination revealed no abnormal findings. Tomography-computed tomography (PET-CT) revealed a thickened sigmoid colon and multiple enlargements of mesentery lymph nodes with advanced metabolism. Initially, his lower gastrointestinal endoscopy revealed multiple jumping ulcers on the entire colon, and biopsy samples from the ulcer site revealed NK/T-cell lymphoma (Figure 1a, b). Repeat colonoscopy revealed multiple ulcers on the ileocecal and descending colon, and the biopsy suggested Crohn’s disease (Figure 1c, d). Immunohistochemical staining revealed that these cells were positive for CD3, CD20, CD43, CD56, granzyme, TIA-1, and EBV-encoded RNAs in situ hybridization. Bone marrow biopsy identified only 2% of suspected lymphoma cells. Flow cytometry assay of bone marrow indicated no change in the rate of lymphocytes or their abnormal phenotypes. Gene sequencing of peripheral blood revealed negative results for the monoclonal rearrangement of TCR. Splenomegaly was identified on abdominal MRI (Figure 2a). HIV and T-SPOT tests were negative. The load of EBV DNA was 1.02×106 copies/mL. Liver and kidney function were severely impaired, and blood cells, especially platelets, decreased markedly (Figure 2b). The patient refused any further aggressive treatment due to high cost and died 2 days after discharge from the hospital.
Figure 1. a–d.

Colonoscopic and histologic findings for the ileocecal junction showing well-demarcated deep ulcers with clean bases (a) and diffuse lymphoid infiltration and lymphoid hyperplasia of the lamina propria (H&E stain, ×100) (b). (c, d) Repeat colonoscopy revealed multiple ulcers in the descending colon (c), and the corresponding histopathology revealed chronic inflammation with multiple erosion and shallow ulcers (×40) (d).
Figure 2. a, b.
Abdominal MRI revealed splenomegaly. (b) Platelet counts and body temperatures during the hospitalization period.
EBV-associated LPD should be considered as a differential diagnosis of intestinal ulcers in addition to inflammatory bowel disease (IBD), intestinal tuberculosis (TB), and lymphoma (2–4). The colon is an unusual site for EBV-associated NK/T-cell LPD, especially in patients without immunodeficiency. Although endoscopic biopsy findings may suggest EBV-associated NK/T-cell LPD, the results are sometimes inconclusive, and a diagnosis may not be made without immunohistochemical staining, similar to the case in our study. It is important to make a proper differential diagnosis because the treatment strategy and prognosis of patients with EBV-associated LPD differ markedly from those of patients with IBD, intestinal TB, and lymphoma (5). This report highlights that intestinal ulcers should be diagnosed with caution because it can sometimes be a precancerous lesion.
Footnotes
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and its accompanying images.
Author Contributions: Concept - L.J., W.H.Z., G.C.; Design - W.H.Z., L.J., Z.Q.; Supervision - Z.Q., Z.R., L.J.; Materials: L.J., S.X.Y.; Data Collection and/or Processing - W.H.Z., G.C., Y.M.X.; Analysis and/or Interpretation - G.C., Z.R., Y.M.X., L.J.; Literature Search - S.X.Y., Z.R., L.J.; Writing Manuscript - W.Z., G.C., Y.M.X.; Critical Review - L.J., S.X.Y., Z.Q.
Peer-review: Externally peer-reviewed.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Support: This study was supported by National Natural Science Foundation of China (Jing Liu, no. 81472735), Wuhan Science and Technology Bureau (Jing Liu), Wuhan City Health and Family Planning Commission (Jing Liu) and Wuhan University (Jing Liu).
REFERENCES
- 1.Chen H, Yu Z, Jiang Z, et al. A case report of NK-cell lymphoproliferative disease with a wide involvement of digestive tract develop into Epstein-Barr Virus associated NK/T cell lymphoma in an immunocompetent patient. Medicine. 2016;95:e3176. doi: 10.1097/MD.0000000000003176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Na HK, Ye BD, Yang SK, et al. EBV-associated lymphoproliferative disorders misdiagnosed as Crohn’s disease. J Crohns Colitis. 2013;7:649–52. doi: 10.1016/j.crohns.2012.09.018. [DOI] [PubMed] [Google Scholar]
- 3.Chen H, Yu Z, Jiang Z, et al. A case report of NK-cell lymphoproliferative disease with a wide involvement of digestive tract develop into Epstein-Barr Virus associated NK/T cell lymphoma in an immunocompetent patient. Medicine. 2016;95:e3176. doi: 10.1097/MD.0000000000003176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zheng X, Xie J, Zhou X. Epstein-Barr virus associated T-cell lymphoproliferative disease misdiagnosed as ulcerative colitis: a case report. Int J Clin Exp Pathol. 2015;8:8598–602. [PMC free article] [PubMed] [Google Scholar]
- 5.Kato S, Miyata T, Takata K, et al. Epstein-Barr virus-positive cytotoxic T-cell lymphoma followed by chronic active Epstein-Barr virus infection-associated T/NK-cell lymphoproliferative disorder: a case report. Human Pathology. 2013;44:2849–52. doi: 10.1016/j.humpath.2013.05.025. [DOI] [PubMed] [Google Scholar]