Abstract
Many unilateral amputations are followed by a contralateral amputation within three years, sometimes presenting as bilateral transfemoral amputations. Bilateral transfemoral amputees that successfully use prostheses are an understudied patient population. This study establishes reference values for this population in users of short non-articulating (stubby) or full-length articulating prostheses. Anthropometric and demographic information was collected from participants. Additionally, participants completed a self-reported Prosthesis Evaluation Questionnaire–Mobility Subscale 12/5 (PEQ-MS) and performed multiple physical mobility tests, including walking tests and the multi-directional Four Square Step Test (FSST). Full-length users rated their abilities to complete the PEQ-MS tasks as less difficult than stubby users in eight of the 12 items. Gait analysis revealed a greater amount of time is spent in stance phase with a greater portion in double limb support for both user groups, and a greater percentage in stance phase for the subject-reported dominant limb. Stubby users’ gait velocity had a significant reduction from that of their full-length peers; however, cadence was similar between groups. Both user groups completed the FSST at comparable times. These outcomes may be of benefit for identifying tasks bilateral transfemoral prosthetic users may find to be most difficult as well as for identifying normal ambulation patterns within this population. Future studies with a greater number of subjects would enable these results to be further generalized.
Keywords: Above knee, Amputation, Amputee, Bilateral, Double, Four square step test, Gait, Prostheses, Prosthesis evaluation questionnaire, Prosthetic, Rehabilitation, Stubbies, Temperospatial, Transfemoral
INTRODUCTION
Multiple studies have shown that a unilateral lower limb amputation will result in a second contralateral amputation within three years of the initial amputation (1–3). Some of these unilateral amputees have the opportunity to use a prosthesis prior to the second amputation. Evans et al. report successfully ambulating as a unilateral amputee serves as a good precursor to using bilateral prostheses 50% of the time, as unilateral amputees who did not ambulate with a prosthesis prior to a second amputation are only successful users of bilateral prostheses 6.8% of the time (2). Of the study group, 74% were not prosthetic users, largely because of comorbidities endured by this patient population (2). In addition to these comorbidities, the significant energy requirements for ambulation with bilateral transfemoral prostheses, 280% of that of the general able-bodied population, can further adversely impact function and research participation (4,5).
While a majority of amputations are caused by vascular disease (90%) (6), the remaining traumatic amputees are more likely to be younger and require less energy when walking at self-selected speeds (7). The majority of studies of persons with bilateral transfemoral amputations (BTFA) report case studies, case series, or small samples. Further, few studies report widely used clinical outcome measures. This creates a considerable knowledge gap regarding the function of persons with BTFA, particularly relative to common clinical outcome measures. Therefore, the purpose of this study was to observationally report the function of persons with BTFA in a relatively larger sample, including users of short non-articulating (stubby) or full-length articulating prostheses.
METHODS
Procedures were administered in accordance with the Declaration of Helsinki. All subjects provided written informed consent prior to their participation.
During a clinic held for bilateral transfemoral prosthetic users at a prosthetics and orthotics facility in Oklahoma City, OK, community ambulating individuals post BTFAs were provided training on how to better use their respective prostheses and to improve upon their life skills. Inclusion requirements for clinic attendance and subsequent study involvement were 1) to be able to ambulate independently without assistance, 2) to be healthy enough to travel to the clinic, and 3) to utilize prostheses. The clinic was led by experienced prosthetic users well adapted to using prostheses in everyday life and to serving in peer-to-peer support activities. During the clinic, information was collected from attendees to improve upon the level of understanding of post BTFA rehabilitation. This information provided insight to attending clinicians on the gait patterns of this patient population as well as which tasks were perceived to be more or less difficult by participants. Data collected were reviewed following the conclusion of the clinic (Retrospective Cohort Design).
Anthropometric data were collected from the subjects. Participants then rated the difficulty of performing various tasks on the Prosthesis Evaluation Questionnaire – Mobility Section 12/5 (PEQ-MS) (8). Subjects traversed a GaitRite walkway (CIR Systems, Inc., Franklin, NJ) at a self-selected walking speed (SSWS) five times. Finally, participants completed three trials of the Four Square Step Test (FSST) (9).
Most of the subjects (n = 18) had stubby (short-length non-articulating) prostheses. Stubby prostheses are initially provided to new users in this clinic, as it has been shown that using shortened prostheses that are gradually lengthened improves the long-term success of bilateral transfemoral prosthetic users (BTFPU) (10). Though most subjects had both types of prostheses, they were only evaluated using the prostheses most often utilized. Generally, this led to the more advanced ambulators being evaluated with their full-length prostheses and newer ambulators being evaluated with their stubby prostheses. Participants were categorized solely by the type of prosthesis primarily used: full-length or short-length prostheses. Further, prosthetic socket/ interface, suspension method, knee components, and feet components varied from patient to patient and were not explicitly included in the data collection. However, all full-length articulated prosthesis users ambulated with some type of microprocessor prosthetic knee.
OUTCOME MEASURES
Anthropometry and Etiology
Anthropometric data were also collected by either taking measurements of the patient or by self-report. Measurements were taken to determine patient height (calculated by arm span), weight, and residuum length (11). Patients were asked which foot they would use to kick a ball to determine their dominant lower extremity (12,13). Patients were also asked what caused their amputations.
PEQ-MS
The PEQ-MS, which is a condensed questionnaire from the initial Prosthesis Evaluation Questionnaire, was administered (8,14,15). The condensed questionnaire asks about the difficulty of twelve tasks and allows respondents to score the difficulty using five points on the ordinal scale. A higher score indicates a higher ability to complete a given task. This simplifies data collection while maintaining validity (accuracy) and reliability (consistency) (8,16).
Gait
Subjects traversed a 4.9 m GaitRite portable walkway at a self-selected walking speed five times. The GaitRite is a valid and reliable instrument for recording spatiotemporal parameters of gait, including swing, stance, single and double limb support percentages, gait velocity, and cadence (17).
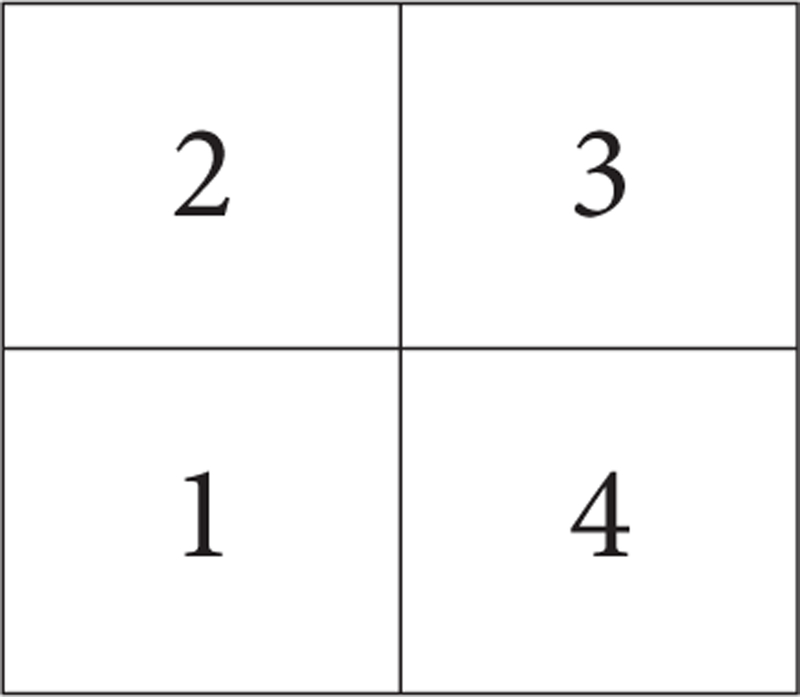
FSST
Finally, subjects also participated in four hand-timed trials of the FSST. This test is a valid and reliable measure used to determine balance and mobility as well as the risk of falls (9). As an amputee patient’s rehabilitation progresses, it is reasonable to expect that their balance and mobility would improve while risk of falls would decrease. It was also of interest to determine which user group moved faster in multi-directional stepping. In the FSST, a cross is formed using four single-point canes laid down with the inferior tips aligned in the center, thus creating four separate square quadrants. The subject starts the sequence with both feet in square 1 looking toward square 2. Participants then step straight into square 2. When both feet are in square 2, the subject side-steps into square 3, then backwards to square 4, and then sideways back to square 1. They then immediately reverse the pattern by side stepping into square 4, forward stepping into square 3, side stepping into square 2, and then backwards to return to square 4. The stopwatch starts when the first foot steps into square 2 and ends when the last foot returns to square 1 after completing the entire sequence. Prior to beginning the FSST, each participant was individually given the following directions from the initial study by Dite et al.: “Try to complete the sequence as fast as possible without touching the sticks. Both feet must make contact with the floor in each square. If possible, face forward during the entire sequence.” The subjects were also shown the entire sequence before the test commenced (9).
Statistical Analyses
Normally distributed data were analyzed using independent samples t-tests. Otherwise, the Wilcoxon rank-sum test for median differences was used. NCSS PASS statistical software was used for analyses (Kaysville, UT). Statistical significance was set at p ≤ 0.05.
RESULTS
Subjects: Sociodemography, Etiology, and Anthropometry
Twenty-two (n = 22) community ambulating BTFPUs participated in the data collection (Table 1). Twenty of the participants were male, and the remaining two were female. The mean age of the group was 27.7 (± 8.84) years. The mean Body Mass Index (BMI) for the group was 24.3 (± 3.35). The self-reported limb dominance resulted in right-limb dominance for 17 (77.3%) participants and left-limb dominance with the resultant five (22.7%). Measured residual limb lengths indicated longer right-limb lengths in eight (36.4%) of the participants, longer left-limb lengths in seven (31.8%) of the participants, and even limb lengths in seven (31.8%) of the participants. The amputation etiology was predominantly traumatic, with 17 (77.3%) of the participants having lost limbs from either military conflict, industrial or occupational accidents, or motor vehicle accidents. Four (18.2%) of the participants went through an amputation for treatment of systemic infections. The remaining participant (4.5%) had a congenital birth defect requiring amputation.
Table 1.
Participant Information
| Entire Group (n = 22) | Full-Length Users (n = 17) | Stubby-Length Users (n = 5) | |
|---|---|---|---|
| Sex: | Male = 20 (90.9%) | Male = 16 (94.1%) | Male = 4 (80.0%) |
| Female = 2 (9.1%) | Female = 1 (5.8%) | Female = 1 (20.0%) | |
| Age: (SD) | 27.7 (± 8.84) years | 27 (± 9) years | 32 (± 7) years |
| BMI: (SD) | 24.3 (± 3.35) years | 23.8 (± 2.5) years | 28 (± 7) years |
| Dominant Limb: | Right = 17 (77.3%) | Right = 13 (76.5%) | Right = 4 (80.0%) |
| Left = 5 (22.7%) | Left = 4 (23.5%) | Left = 1 (20.0%) | |
| Longer Limb: | Right = 8 (36.4%) | Right = 6 (35.5%) | Right = 2 (40.0%) |
| Left = 7 (31.8%) | Left = 6 (35.5%) | Left = 1 (20.0%) | |
| Equal = 7 (31.8%) | Equal = 5 (29.4% | Equal = 2 (40.0%) | |
| Amputation Etiology | Traumatic = 17 (77.3%) | Traumatic = 13 (76.5%) | Traumatic = 4 (80.0%) |
| Infection = 4 (18.2%) | Infection = 3 (17.6%) | Infection = 1 (20.0%) | |
| Congenital = 1 (4.5%) | Congenital = 1 (5.9%) | Congenital = 0 (0%) |
The seventeen-member full-length user subset had a mean age of 27 (± 9) years. One participant (5.9%) was female and the remaining 16 (94.1%) male. The mean BMI for the subgroup was 23.8 (± 2.5). Reported limb dominance was right for 13 (76.5%) participants and left for four (23.5%) participants. Longer residuum lengths were right for six (35.3%) participants, left for six (35.3%) participants, and with equal lengths for five (29.4%) participants. Amputation etiology for the full-length subgroup was trauma for 13 (76.5%) members, infection for three (17.6%) members, and congenital for one (5.9%) member.
In the smaller five-member stubby-length subset, the mean age was slightly older at 32 (± 7) years. One participant (20%) was female and the remaining four (80%) male. The mean BMI was 28 (± 7). Self-reported limb dominance was right in four (80%) participants and left in the remaining (20%) participant. Residual limb length was longer in the right for two (40%) participants, left in one (20%) participant, and equal in two (40%) participants. The amputation etiology for this group was trauma for four (80%) members and infection for the remaining member (20%).
PEQ-MS
The PEQ-MS provided insights on which tasks both the stubby and full-length user groups perceived to be more or less difficult. In eleven of the twelve items, the median score among the stubby user group was two (moderate difficulty) on a 5-point ordinal scale (0 to 4), and item 8 (walking on slippery surfaces) was rated the lowest, with a median score of 1 (high difficulty). Conversely, the full-length user group tended to rate each item higher (easier), such that the median score of 2 only appeared once on item 2 (confined spaces). The median score of 3 appeared in seven of 12 items. In four items, the median score was 4. Items 1 (walking), 4 (walking downstairs), 11 (sit & stand from low chairs), and 12 (sit & stand-toilet) were the four items that were not statistically significant between the groups.
Gait and FSST
Using the GaitRite portable walkway, gait was assessed and compared. Stance phase was identified at 64.2 ± 2.6% for the dominant side and 60.8 ± 2.2% for the non-dominant side. Both the dominant and non-dominant side stance phase presented greater than the normal 60% (18). The dominant side spent 35.8 ± 2.6% of the time in the swing phase of gait. For the non-dominant side, 33.7 ± 2.2% of time was spent in swing phase. As opposed to double limb support, a lesser percentage of time was spent in swing phase than the normally found 40%. For single limb support (SLS), the dominant side spent 36.3 ± 2.3% of the time in that phase of gait. The non-dominant side spent 34.2 ± 2.5 of the gait cycle in SLS. Both sides spent less time in SLS than the normal 40% (18). Conversely, a greater percent of the cycle was spent in double support (28.0 ± 4.4% dominant vs. 27.0 ± 4.5% non-dominant) than is classically reported (20%).
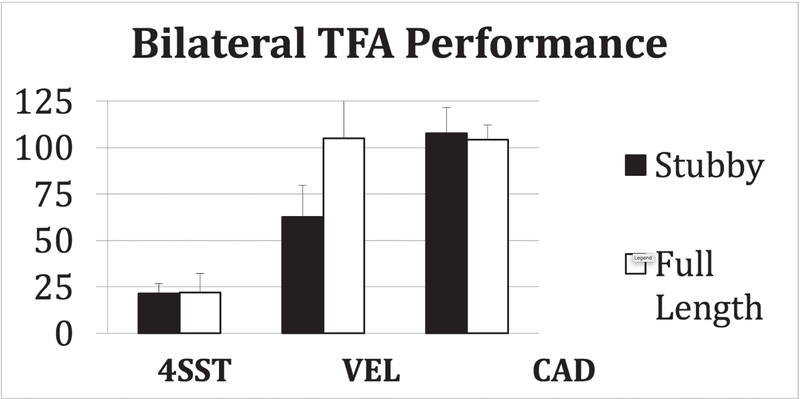
Comfortable gait velocity for the stubby users was 40% slower than in the full-length user group. The mean stubby user group velocity was 62.7 cm/s, and the full-length user group velocity was 105.1 cm/s. The mean velocity for a “normal” sample of similar age is 122.7 ± 11.1 cm/s (19).
Unlike the significant differentiation between the groups observed for gait velocity (VEL), cadence (CAD) and the four square step test (FSST) were similar (p > 0.05) for both groups, with both measures only yielding differences of 3%. The stubby users completed the FSST with a mean time of 21.4 ± 5.3 seconds, and full-length users had a mean time of 22.0 ± 10.2 seconds. Cadence was measured at 107.7 ± 14.0 for the stubby users and 104.4 ± 8.0 for the full-length users.
DISCUSSION
Full-length users rated their abilities to complete the PEQ-MS tasks significantly higher (less difficult) than that of stubby users in eight of the 12 items, including stair descent (item 4), ramp descent (item 6), sit and stand from low chairs (item 11), and sit and stand from the toilet (item 12). These tasks represent activities where a high degree of knee control is necessary. These functional areas have been emphasized as strengths for microprocessor controlled prosthetic knee systems (20). While full-length users were more confident in their abilities as related to the PEQ-MS, the responses do not present an obvious ceiling effect. This leaves room for quantification of improvement in locomotor tasks throughout the rehabilitation process.
Full-length users of bilateral transfemoral prostheses vary the percentage of their gait cycles spent in stance versus swing and single versus double limb support. A greater amount of time is spent in stance phase with a greater portion in double limb support. This is relatively common in diagnostic populations with gait patterns known to be less stable (21). It was also discovered that the self-reported dominant limb had a greater percentage in stance phase than the non-dominant limb. This finding suggests that this patient population favors stance phase stability and highlights the importance of weight-bearing socket comfort for the patient. This finding also suggests the criticality of prosthetic feet and knee components that can rapidly and predictably transition into and out of swing phase with a high degree of knee stability and reliability, features found in microprocessor controlled prosthetic knee systems (22–25).
The sidestepping within the FSST created a surprising challenge for the full-length user group. One high-activity prosthetic user had significant difficulty in this task despite being able to walk across significant slopes and terrains unaided. This may be due to the fact that microprocessor knees primarily evaluate forward and backward progression when determining which action to perform.
The stubby users rated their abilities to complete the tasks of the PEQ-MS significantly lower (more difficult) than the full-length group. Item 8 (walk on slippery surfaces) was identified in the BTFPUs using stubby prostheses as being the most difficult task, which corroborated the findings of Franchignoni et al. (8). Stubby users identified item 10 (sit & stand from a high seat) with a median score of 2, with a range of 2 to 3, suggesting that this group did not necessarily find this to be an easier task. Stubby users seemed to find it comparably difficult to most of the other items. It seems the obvious height restriction associated with stubby use is a factor in this task. Given that the full-length group have progressed out of the short stubby prostheses, the ease at which full-length users reported being able to complete most tasks should be attributed to a greater amount of experience rather than full-length prostheses making the tasks easier.
Stubby users’ gait velocity had a significant 40% reduction from that of their full-length peers. The diminished height of the stubby prostheses, as compared to the full-length legs, potentially limited the subjects’ linear walking.
The stubby users were able to complete the FSST at times comparable to the full-length user group. The stubby users positioned themselves closer to the cane intersections during testing, which limited the required travel distance when moving from square to square. While both user groups completed the FSST at comparable times, the task took longer to complete than in the non-amputee population by as much as 10 seconds in some instances (9).
The two user groups were quite comparable with cadence as well, with no significant difference between groups. Patients stepped at a comfortable rate, demonstrating consistent motor control regardless of condition. It is worth noting that subjects walked a gait mat alone, as opposed to socially walking beside someone, which may have altered the stepping rate and velocity. The consistent cadence is not surprising, as step length in stubbies will be decreased, a point which can be easily confirmed with future work. This finding has similarities to what might be expected when comparing the gait pattern of people with shorter limbs (i.e., shorter than average people, children, people with dwarfism) with those having longer limbs. That is, in order to walk at comparable speeds, those with shorter limbs must use higher cadence or use a similar cadence but walk slower as seen here.
CONCLUSION
There is a shortage of published data on BTFPUs, which has resulted in limited reference values for this patient population. This research provides valuable insights to clinical practice in the treatment of this unique user group as well as establishing reference values for subsets within this group. Additionally, this study highlights the importance for this patient population to have access to comfortable prosthetic interfaces with prosthetic technologies that provide reliable and responsive transitions between swing and stance phases of gait with high degrees of stability and reliability.
Further research should evaluate how BTFPU performance in outcome measures at each stage of the rehabilitation process predicts future success in subsequent stages. Additional research could also compare how using short non-articulating (stubby) and full-length articulating prostheses impacts the gait and performance on outcome measures for full-length users. This approach would allow for a more accurate comparison between the short and full-length prostheses, as the full-length user group is typically more capable and further along in the rehabilitation process as described by Irolla et. al (10). The field would benefit from longitudinal data collection of this limited patient population. Had the measures been performed at each stage of the rehabilitation process, greater insights could have been gleaned from this patient population. Lastly, a larger sample size with a greater number of subjects with non-traumatic amputations would provide valuable insights on how amputation etiology impacts the outcomes collected here.
Though the sample size in this study is valuable compared to the overall size of the population of bilateral transfemoral amputees who are successful users of prostheses, it is important for researchers to continue to study this patient population as more of them become successful prosthetic users. This information will be valuable to healthcare providers responsible for the treatment and rehabilitation of bilateral transfemoral amputees.
Figure 1.
The overhead layout of the four square step test (FSST).
Figure 2.
Performance differences between stubby and full-length prosthesis users in four square step test (FSST), velocity (VEL), and cadence (CAD).
Table 2.
PEQ-MS Performance
| PEQ-MS Performance | |||
|---|---|---|---|
| Item # | Sample Score: Median (Range) | p value⋆ | |
| Stubby (n = 5) | Full-Length (n = 17) | ||
| 1 | 2 (2–3) | 4 (2–4) | 0.004⋆⋆ |
| 2 | 2 (2) | 3 (2–4) | 0.0008⋆⋆ |
| 3 | 2 (0–2) | 2 (1–4) | 0.05⋆ |
| 4 | 2 (0–2) | 3 (0–4) | 0.06 |
| 5 | 2 (2–3) | 3 (2–4) | 0.02⋆⋆ |
| 6 | 2 (0–3) | 3 (0–4) | 0.18 |
| 7 | 2 (2) | 4 (1–4) | 0.003⋆⋆ |
| 8 | 1 (0–2) | 3 (1–4) | 0.008⋆⋆ |
| 9 | 2 (1–3) | 4 (3–4) | 0.0007⋆⋆ |
| 10 | 2 (2–3) | 4 (2–4) | 0.005⋆⋆ |
| 11 | 2 (1–4) | 3 (1–4) | 0.20 |
| 12 | 2 (1–4) | 3 (1–4) | 0.09 |
Wilcoxon Rank-Sum Test for Difference in Medians.
Significant at p ≤ 0.05
Table 3.
Gait Cycle
| Gait Cycle Percentages | |||
|---|---|---|---|
| Dominant | Non-Dominant | Normal | |
| Stance Phase | 64.2 ± 2.6% | 60.8 ± 2.2% | 60% |
| Swing Phase | 35.8 ± 2.6% | 33.7 ± 2.2% | 40% |
| Single Support | 36.3 ± 2.3% | 34.2 ± 2.5% | 40% |
| Double Support | 28.0 ± 4.4% | 27.0 ± 4.5% | 20% |
Table 4.
Gait Velocity
| Velocity | |
|---|---|
| Stubby User Group | 62.7 ± 17.0 cm/s |
| Full-Length User Group | 105.1 ± 21.1 cm/s |
ACKNOWLEDGMENTS
Contents of the manuscript represent the opinions of the authors and not necessarily those of the Department of Defense, Department of Veterans Affairs, Department of the Army, or any other government, academic, or clinical organization. Authors declare no conflict of interests. This project was partially funded by the National Institutes of Health, Scholars in Patient Oriented Research grant (1K30RR22270).
REFERENCES
- 1.Esquenazi A Geriatric amputee rehabilitation. Clin Geriatr Med 1993;9(4):731–743. [PubMed] [Google Scholar]
- 2.Evans WE, Hayes JP, Vermilion BD. Rehabilitation of the bilateral amputee. J Vasc Surg 1987;5(4):589–593. [DOI] [PubMed] [Google Scholar]
- 3.Dillingham TR, Pezzin LE, Shore AD. Reamputation, mortality, and health care costs among persons with dysvascular lower-limb amputations. Arch Phys Med Rehabil 2005;86(3):480–486. [DOI] [PubMed] [Google Scholar]
- 4.Huang C, Jackson J, Moore N, Fine P, Kuhlemeier K, Traugh G, Saunders P. Amputation: energy cost of ambulation. Arch Phys Med Rehabil 1979;60(1):18–24. [PubMed] [Google Scholar]
- 5.Wright D, Marks L, Payne R. A comparative study of the physiological costs of walking in ten bilateral amputees. Prosthet Orthot Int 2008;32(1):57–67. [DOI] [PubMed] [Google Scholar]
- 6.McCollum PT, Raza Z. Vascular disease: limb salvage versus amputation. In: Smith DG, Michael JW, Bowker JH, editors. Atlas of amputations and limb deficiencies Rosemont (IL): American Academy of Orthopaedic Surgeons; 2004. p. 31. [Google Scholar]
- 7.Barth DG, Schumacher L, Thomas SS. Gait analysis and energy cost of below-knee amputees wearing six different prosthetic feet. J Prosthet Orthot 1992;4(2):63–75. [Google Scholar]
- 8.Franchignoni F, Giordano A, Ferriero G, Orlandini D, Amoresano A, Perucca L. Measuring mobility in people with lower limb amputation: Rasch analysis of the Mobility Section of the Prosthesis Evaluation Questionnaire. J Rehabil Med 2007;39(2):138–144. [DOI] [PubMed] [Google Scholar]
- 9.Dite W, Temple VA. A clinical test of stepping and change of direction to identify multiple falling older adults. Arch Phys Med Rehabil 2002;83(11):1566–1571. [DOI] [PubMed] [Google Scholar]
- 10.Irolla C, Rheinstein J, Richardson R, Simpson C, Carroll K. Evaluation of a graduated length prosthetic protocol for bilateral transfemoral amputee prosthetic rehabilitation. J Prosthet Orthot 2013;25(2):84–88. [Google Scholar]
- 11.Reeves SL, Varakamin C, Henry CJ. The relationship between arm-span measurement and height with special reference to gender and ethnicity. Eur J Clin Nutr 1996;50(6):398–400. [PubMed] [Google Scholar]
- 12.Vanicek N, Sanderson DJ, Chua R, Kenyon D, Inclis JT. Kinematic adaptations to a novel walking task with a prosthetic simulator. J Prosthet Orthot 2007;19(1):29–35. [Google Scholar]
- 13.Howard C, Wallace C, Stokic DS. Lower limb preference on goal-oriented tasks in unilateral prosthesis users. Gait Posture, 2012;36(2):249–253. [DOI] [PubMed] [Google Scholar]
- 14.Prosthesis Evaluation Questionnaire. Kingston (WA): Prosthetics Research Study; 1998. [accessed 2018 Aug 17]. http://prs-research.org/files/PEQ.pdf. [Google Scholar]
- 15.Legro MW, Reiber GD, Smith DG, Aguila MD, Larsen J, Boone D. Prosthesis evaluation questionnaire for persons with lower limb amputations: assessing prosthesis-related quality of life. Arch Phys Med Rehabil 1998;79(8):931–938. [DOI] [PubMed] [Google Scholar]
- 16.Miller WC, Deathe AB, Speechley M. Lower extremity prosthetic mobility: a comparison of 3 self-report Scales. Arch Phys Med Rehabil 2001;82(10):1432–1440. [DOI] [PubMed] [Google Scholar]
- 17.Highsmith MJ, Kahle JT, Quillen WS, Mengelkoch LJ. Spatiotemporal parameters and step activity of a specialized stepping pattern used by a transtibial amputee during a denali mountaineering expedition. J Prosthet Orthot 2012;24(3):153–157. [Google Scholar]
- 18.Perry J Gait analysis: normal and pathological function Thorofare (NJ): SLACK Incorporated; 1992. [Google Scholar]
- 19.Öberg T, Karsznia A, Oberg K. Basic gait parameters: reference data for normal subjects, 10–79 years of age J Rehabil Res Dev 1993;30(2):210–223. [PubMed] [Google Scholar]
- 20.Hafner BJ, Willingham LL, Buell NC, Allyn KJ, Smith DG. Evaluation of function, performance, and preference as transfemoral amputees transition from mechanical to microprocessor control of the prosthetic knee. Arch Phys Med Rehabil 2007;88(2):207–217. [DOI] [PubMed] [Google Scholar]
- 21.von Schroeder HP, Coutts RD, Lyden PD, Billings E, Nickel VL. Gait parameters following stroke: a practical assessment. J Rehabil Res Dev 1995;32(1):25–31. [PubMed] [Google Scholar]
- 22.Berry D, Olson MD, Larntz K. Perceived stability, function, and satisfaction among transfemoral amputees using microprocessor and nonmicroprocessor controlled prosthetic knees: a multicenter survey. J Prosthet Orthot 2009;21(1):32–42. [Google Scholar]
- 23.Burnfield JM, Eberly VJ, Gronely JK, Perry J, Yule WJ, Mulroy SJ. Impact of stance phase microprocessor-controlled knee prosthesis on ramp negotiation and community walking function in K2 level transfemoral amputees. Prosthet Orthot Int 2012;36(1):95–104. [DOI] [PubMed] [Google Scholar]
- 24.Kahle JT, Highsmith MJ, Hubbard SL. Comparison of nonmicroprocessor knee mechanism versus C-Leg on Prosthesis Evaluation Questionnaire, stumbles, falls, walking tests, stair descent, and knee preference. J Rehabil Res Dev 2008;45(1):1–14. [DOI] [PubMed] [Google Scholar]
- 25.Kaufman KR, Levine JA, Brey RH, Iverson BK, McCrady SK, Padgett DJ, Joyner MJ. Gait and balance of transfemoral amputees using passive mechanical and microprocessor-controlled prosthetic knees. Gait Posture 2007;26(4):489–493. [DOI] [PubMed] [Google Scholar]