Abstract
Objective:
To evaluate the percentage of children born extremely preterm who screen positive for ≥ one DSM-IV psychiatric disorder, the co-occurrence of and sex-related differences in these classifications, and the functional correlates of psychiatric symptoms.
Methods:
The Extremely Low Gestational Age Newborns (ELGAN) Study is a prospective cohort follow-up of children born < 28 weeks gestation. For 871 10-year-old children, parents completed the Child Symptom Inventory-4 (CSI-4), a child educational/medical history questionnaire, and the Pediatric Quality of Life Inventory (PedsQL).
Results:
At age 10 years, ELGANs were more likely to screen positive for a number of psychiatric disorders when compared to normative expectations on the CSI-4, with a few sex-related differences. Fifteen percent of participants screened positive for one disorder, 7% for two, 3% for three, and 4% for ≥ 4 psychiatric disorders. Compared to children who did not screen positive for psychiatric disorders, children who screened positive for ≥ 3 psychiatric disorders were approximately twice as likely to have repeated a grade, have an individualized educational program (IEP), have an individual school aide, and to require special remediation classes. Children who screened positive for any psychiatric disorder were four times more likely to use one or more psychotropic medication, and those who screened positive for ≥ 2 psychiatric disorder had lower PedsQL scores.
Conclusion:
Among 10-year-old children born extremely preterm, rates of psychiatric symptoms exceeded normative expectation, and children who screened positive for more than one psychiatric disorder were at increased risk for having multiple functional impairments.
Keywords: Preterm, School-Age, Psychiatric Disorders, Comorbidity, Impairment
INTRODUCTION:
Over the past 40 years, changes in perinatal care of extremely low gestational age newborns (ELGANs) have been accompanied by increasing survival rates and decreasing rates of morbidity.1 Nonetheless, preterm infants remain at risk for a variety of neurodevelopmental challenges, including elevated psychiatric symptomatology during school age.2 Prior studies indicate that premature infants followed into childhood have higher rates of both externalizing (attention deficit and hyperactivity disorder [ADHD], conduct disorder, delinquency)3-7 and internalizing disorders6-9 (emotional problems, depression, anxiety) than children born at term. In addition, a "preterm behavioral phenotype" has been described that includes difficulties in emotional, attention, and peer or social functioning.10
Children born prematurely are more likely than children term-born to be prescribed psychotropic medications in young adulthood.11 Additionally, they have higher rates of learning and school-related problems, autism spectrum disorders (ASD), somatic concerns and decreased social competence.5, 7, 10, 12, 13 The EPICure study assessed 219 extremely preterm children born < 26 weeks in the United Kingdom and Ireland at age 11 years and found them to be three times more likely than classmates to have psychiatric disorders, and to be at increased risk for ADHD, anxiety disorders, and ASD. Psychiatric disorders were associated with cognitive impairment, but no significant sex differences were found. In addition, functional correlates of these psychiatric disorders at age 11 years were not reported.7 A more recent study of children, ages 7-8 years, who were born extremely preterm (EP) or extremely low birth weight (ELBW) identified four behavioral profiles as determined by the Strengths and Difficulties Questionnaire Problem Scales (e.g emotional symptoms, conduct problems, hyperactivity/inattention and peer relationship problems), which assesses broad behavioral domains rather than specific psychiatric symptoms or disorders. These investigators found that more severe behavioral profiles were associated with poorer cognitive and academic performance.10
In some children born prematurely, psychiatric and developmental disorders of childhood continue into adolescence and adulthood.14 However, a systematic review of 15 studies that investigated risk factors for behavioral and psychiatric problems in children born prematurely concluded that further research is needed.15 Most studies of individuals born prematurely selected participants based on birthweight3, 4, 6 rather than gestational age, had a relatively small number of participants,2-4, 6, 7 or assessed the children before school age.6 Additionally, few studies have examined sex differences in the prevalence of psychiatric symptomatology in preterm born children, and to our knowledge, none (including the large EPICure study of similar age children) have reported on the burden and co-occurrence of elevated psychiatric symptoms.
In children and adolescents with psychiatric disorders, illness burden has been described as “functional impairment which substantially interferes with or limits the child’s role or functioning in family, school, or community activities”.16 Evaluating the prevalence of elevated psychiatric symptoms in ELGAN children in relation to measures of functional impairment (i.e. developmental and medical outcomes, and school, physical, social and emotional functioning) is an important step in understanding the psychiatric burden in this population. Moreover, co-occurrence of psychiatric conditions in childhood is an important public health issue. Children and adolescents who are born at term frequently present to mental health providers with a complex diagnostic picture. Remarkably, nearly half of children who presented to a general outpatient child psychiatry clinic were diagnosed with psychiatric co-occurrence,17 and this co-occurrence predicted functional and emotional impairment and persistence of psychiatric disorders.17-19 Children and adolescents with three or more co-occurring psychiatric disorders are more likely to have severe functional impairment,17, 19 while those who present with co-occurring internalizing and externalizing disorders suffer from higher levels of functional impairment than those with an isolated psychiatric disorder.18 However, to our knowledge, the burden of co-occuring psychiatric symptoms in children who were born preterm has not been investigated systematically. Studies conducted in general child outpatient practice underscore the compounding effects of co-occurring psychiatric illness on functional outcomes, highlighting the need for this type of assessment in the particularly vulnerable preterm population.17-19
While prior studies have indicated higher rates of psychiatric disorders in children born preterm, this study is novel in that it examines the frequency and correlates of isolated and co-occurring elevated psychiatric symptoms in the ELGAN population at age 10, thereby addressing the following goal: the identification of patterns of psychiatric phenotypes among ELGANs, specifically the number of positively screened psychiatric disorders, patterns of co-occurrence, and their functional correlates. These patterns have the potential to inform future studies that examine the predisposing environmental and neurobiological mechanisms of psychiatric symptoms in children born preterm.
In this study, we describe: (1) the prevalence of elevated psychiatric symptoms (positively screened psychiatric disorders); (2) sex differences in these prevalence rates; (3) the number and interrelationships of co-occurring psychiatric classifications, including co-occurrence across diagnostic groupings (internalizing, externalizing and autism spectrum [AS]); and (4) the functional impairment correlates (school function, social function, emotional function, physical health, and past and current use of psychotropic medications) and demographic correlates of co-occurring positive psychiatric screens.
METHODS
Participants
The ELGAN Study is a multi-center prospective, observational study of the risk of structural and functional neurologic disorders in EP infants.20 A total of 1506 infants born before the 28th week of gestation were enrolled during the years 2002-2004.21 Of these, 1200 survived to 2 years of age and 1102 participated in a developmental assessment at 2 years.21 At age 10 years, 889 (92%) of 966 children who were actively recruited for follow-up (because of the availability of data on inflammation-related proteins in blood samples from their first postnatal month) were enrolled, and 871 (98% of those enrolled) had a parent-completed Child Symptom Inventory-4 (CSI-4). These children are the participants of this report. Enrollment and consent procedures for this follow-up study were approved by the institutional review boards at all participating sites.
Procedures
All families who participated in the previous follow-up were contacted by mail and then by phone to invite them to participate in the 10-year follow up. Lost to follow-up families were searched for on state vaccination registries and through openly-available resources as approved by the local institution’s IRB.
During the 3-4 hour child assessment visit, the primary caregiver completed questionnaires regarding the child’s medical and neurological status and behavior, including the CSI-4.22, 23 The CSI-4 Parent Checklist is a 97-item screening tool for emotional and behavioral disorders as aligned with the DSM-IV. Specific DSM-IV disorders include: Disruptive Behavior Disorders (ADHD, Oppositional Defiant Disorder [ODD] and Conduct Disorder), Anxiety Disorders (Generalized Anxiety Disorder [GAD], Social Phobia, Separation Anxiety), Mood Disorders (including Major Depressive Disorder and Dysthymic Disorder), and other disorders (including ASD).22 We considered CSI-4 disorders as clinically valid and included them in our analyses only if the disorder screen included more than one symptom question to establish a positive classification for a diagnosis. The CSI-4 has satisfactory psychometric properties with respect to reliability and validity.22 The CSI-4 normative sample for the Parent Checklist (N=551) consisted of children between 5 and 12 years old (mean age 8.6 years) who attended public elementary schools. Children receiving special education services were not included in the normative sample.23
We examined CSI-4 parent ratings of our ELGAN sample relative to/in comparison to the CSI-4 normative data. Because the CSI-4 is a screening tool that does not provide a definitive diagnosis, we present CSI-4 classifications as indicators of elevated psychiatric symptomatology for the disorders described below. To aid in classification of psychiatric co-occurrence, in this study we used the CSI-Positive Screens (diagnostic construct based on symptom counts) rather than Symptom Severity scores (continuous quantitative construct).
During the assessment visit, parents also completed questionnaires which included educational and medical history, and the Pediatric Quality of Life Inventory (PedsQL) which addressed child physical, emotional, social, and school functioning. Scores under 70 on a scale of 0-100 are identified as indicating impaired health related quality of life.24 The demographic information about the children and their families that was used in this report was collected at birth, as there was little variation between demographic data at birth and the data collected at age 10 and there was no missingness in the data from birth. Verbal and nonverbal IQ were assessed at 10 years of age with the Differential Ability Scales-II (DAS-II).25
Data Analyses
First, we compared the prevalence of CSI-4 positive screens for psychiatric disorders in our cohort of EP children to the prevalence rates in the CSI-4 normative data as well as sex differences in prevalence rates of positively screened psychiatric disorders between EP and CSI-4 normative data with chi-square tests. Next, using positive screens as a proxy index for psychiatric disorders, we examined the number of co-occurring psychiatric classifications in children born EP, including co-occurrence across three diagnostic groupings. We defined the three diagnostic groups as follows: Internalizing Disorders: GAD, MDD, dysthymia, social phobia, and separation anxiety; Externalizing Disorders: ODD, CD, and ADHD; and ASD: Autistic Disorder, Asperger’s Disorder. Finally, using chi-square and F-tests, we examined demographic correlates and functional impairment correlates (school function, social function, emotional function, and physical health) of the number of co-occurring positive psychiatric screens while adjusting for maternal education at birth and child IQ at age 10 years. All analyses were conducted using SAS 9.4.
RESULTS
Sample Characteristics
Demographic characteristics of the sample were collected at time of birth and are presented in Table 1. Of 966 children who were eligible for participation in the 10-year follow-up visit (had newborn blood specimen available), 871 children had parent-completed CSI-4 questionnaires, 77 children were in attrition, and 18 children did not have parental report of CSI-4. The majority of participating children were born to women between 21 and 35 years of age (67%). Forty-one percent of mothers of participating children did not have a high school degree or its equivalent, while 36% of mothers had a college degree or higher. Chi-square tests were conducted to determine any systematic differences between participating and non-participating children and their families. We found no differences in maternal education, racial identity or ethnicity, child sex or birth weight. Participating children were lower in gestational age and were born to mothers who were somewhat older, to have mothers who were more likely to be married and more likely to have private (vs. public) insurance compared to non-participating children. These characteristics are presented in Table 1.
Table 1.
Demographic characteristics at time of birth of mothers and children in the sample and not in sample
| In Sample | Not in Sample | |||
|---|---|---|---|---|
| N=871 (%) | N=95 (%) | X2 | ||
| Maternal characteristics at birth | ||||
| Age, years | <21 | 113 (13%) | 15 (16%) | 8.57 (df=2)**, p = 0.014 |
| 21-35 | 580 (67%) | 68 (70%) | ||
| >35 | 178 (20%) | 12 (13%) | ||
| Education, years | ≤ 12 (high school) | 346 (41%) | 57 (60%) | 3.44 (df=2), n.s. p = 0.17 |
| < 12-16> | 198 (23%) | 26 (27%) | ||
| ≥ 16 (≥ college) | 301 (36%) | 12 (13%) | ||
| Single marital status | Yes | 343 (40%) | 54(57%) | 25.69 (df=1)*** p < 0.001 |
| Public insurance | Yes | 297 (35%) | 64 (67%) | 6.62 (df=1)** p = 0.01 |
| Racial identity | White | 544 (63%) | 50 (53%) | 1.70 (df=2), n.s. p = 0.43 |
| Black | 220 (26%) | 38 (40%) | ||
| Other | 97 (11%) | 7 (7%) | ||
| Hispanic | Yes | 84 (10%) | 12 (13%) | 3.50 (df=1), n.s p = 0.06 |
| Newborn characteristics at time of birth | ||||
| Sex | Male | 442 (51%) | 54 (57%) | 3.66 (df=1), n. s. p = 0.06 |
| Gestational age, weeks | 23-24 | 174 (20%) | 26 (27%) | 9.87 (df=2)**. p = 0.007 |
| 25-26 | 391 (46%) | 46 (49%) | ||
| 27 | 294 (34%) | 23 (24%) | ||
| Birth weight, grams | ≤ 750 | 321 (37%) | 42 (44%) | 7.26 (df=2), n.s. p = 0.06 |
| 751-1000 | 377 (43%) | 39(41%) | ||
| > 1000 | 173 (20%) | 14 (15%) | ||
Note:
p<.001
p<.01
p<.05
n.s.p ≥ .05.
Prevalence of Positively Screened Psychiatric Disorders in ELGANs at Age 10 Years
Overall, the ELGAN group was more likely to screen positive than CSI-4 normative expectations for the following internalizing disorders: Generalized Anxiety, Dysthymic disorder, and Social Phobia. Of the externalizing disorders, the ELGAN children were more likely to screen positive for Oppositional Defiant disorder, ADHD inattentive and ADHD combined subtypes, but not for ADHD hyperactive/impulsive subtype. Additionally, the ELGAN children were more likely to screen positive for Autistic Disorder, and Asperger’s Disorder. No statistically reliable differences were noted in positive screens for Major Depression, Separation Anxiety, or Conduct Disorder (for the exact chi-square statistics, see Table 2).
Table 2:
Comparisons (frequencies and %) of positive CSI-4 screens in girls, boys, and total sample from the ELGAN Study and from CSI-4 normative sample.
| Girls | Boys | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| CSI-4 disorders | ELGAN study N=429 |
CSI-4 normative sample N=279 |
X2 (df=1) |
ELGAN study N=442 |
CSI-4 normative sample N=272 |
X2 (df=1) |
ELGAN study n=871 |
CSI-4 normative sample n=551 |
X2 (df=1) |
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | ||||
| Internalizing | |||||||||
| General anxiety | 23 (5.4%) | 3 (1.1%) | 8.8** | 26 (5.9%) | 6 (2.2%) | 5.3* | 49 (5.3%) | 9 (1.6%) | 13.7 *** |
| Major depressive | 4 (1%) | 0 | 0.8, n.s. | 4 (1%) | 0 | 0.4, n.s. | 8 (1%) | 0 (0%) | 1.6, n.s. |
| Dysthymic disorder | 19 (4.4%) | 0 | 10.2 *** | 16 (3.6%) | 4 (1.5) | 2.8, n.s | 35 (4%) | 4 (.7%) | 11.9*** |
| Social phobia | 26 (6%) | 2 (.8%) | 12.7*** | 16 (3.6%) | 2 (.8%) | 5.7** | 42 (4.8%) | 4 (.8%) | 18.1*** |
| Separation anxiety | 14 (3.3%) | 6 (2.2%) | 0.8, n.s. | 12 (2.7%) | 6 (2.2%) | 0.2, n.s. | 26 (3%) | 12 (2.2%) | 0.8, n.s. |
| Externalizing | |||||||||
| Oppositional defiant | 31 (7.2%) | 13 (4.7%) | 1.9, n.s | 42 (9.5%) | 16 (6%) | 2.9, n.s. | 73 (8.4%) | 29 (5.3%) | 4.9 * |
| Conduct disorder | 9 (2.1%) | 6 (2.2%) | 0.0, n.s | 24 (5.4%) | 10 (3.7%) | 1.1, n.s. | 33 (3.8%) | 16 (2.9%) | 0.8, n.s. |
| ADHD inattentive | 43 (10%) | 6 (2.2%) | 16.3 *** | 57 (13%) | 14 (5.2%) | 10.9*** | 100 (11.5%) | 20 (3.6%) | 26.9 *** |
| ADHD hyperactive | 8 (1.9%) | 5 (1.8%) | 0.0, n.s | 25 (5.7%) | 6 (2.3%) | 4.8* | 33 (3.8%) | 11 (2%) | 3.6, n.s. |
| ADHD combined | 16 (3.7%) | 2 (.7%) | 6.2 ** | 32 (7%) | 7 (2.6%) | 7.1** | 48 (5.5%) | 9 (1.6%) | 13.2 *** |
| ASD | |||||||||
| Autistic disorder | 9 (2.1%) | 1 (.4%) | 3.6, n.s | 17 (3.9%) | 2 (.7%) | 6.3* | 26 (3%) | 3 (.5%) | 10.1** |
| Asperger’s disorder | 18 (4.2%) | 0 | 9.5 ** | 21 (4.8%) | 0 | 10.8*** | 39 (4.5%) | 0 (0%) | 20.4 *** |
Note: CSI-4: Child Symptom Inventory-4; ADHD: Attention Deficit Hyperactivity Disorder; ASD: Autism Spectrum Disorders;
p<.001;
p<.01;
p<.05; n.s.p ≥ .05.
Sex Differences in the Prevalence of Positively Screened Psychiatric Disorders.
Next, we examined differences in prevalence of positive screens separately for girls and boys. The results were largely in line with the comparisons of the total cohort, but with some exceptions (Table 2). On the one hand, the ELGAN girls, but not boys, were more likely than CSI-4 normative expectations to screen positive for Dysthymic Disorder. On the other hand, the ELGAN boys, but not the girls, were more likely than CSI-4 normative expectations to screen positive for ADHD hyperactive/impulsive subtype and for Autistic Disorder.
Number of Psychiatric Co-occurrences
Fifteen percent of participants were reported to have screened positive for one psychiatric disorder, 7% for two, 3% for three, and 4% screened positive for four or more psychiatric disorders (Supplemental Table 1). As such, about 30% of all ELGAN children had a positive screen for at least one psychiatric disorder. Twenty five percent of ELGAN girls and 34 % of ELGAN boys screened positive for ≥ 1 psychiatric disorder. Unfortunately, the normative data set did not include data on co-occurring positive screens for comparison.
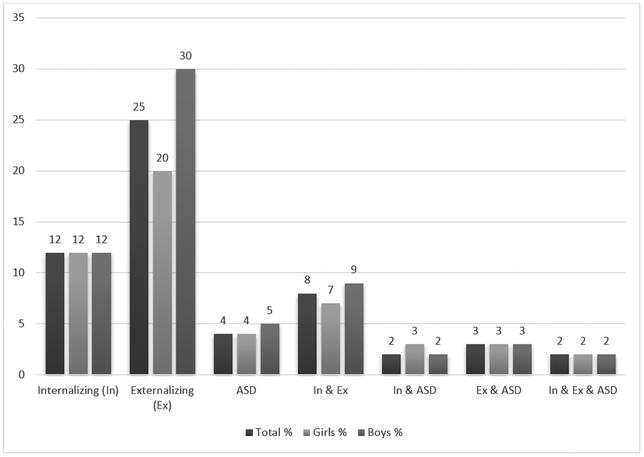
Regarding diagnostic groupings, externalizing and internalizing disorders were the most likely to co-occur (8% of all children in the ELGAN sample), followed by externalizing disorders and ASD (3% of all children in the ELGAN sample) (see Figure 1).
Figure 1:
Co-Occurring Positive Screens of Diagnostic Classification: The percent of ELGANS, boys and girls who were identified by parent to have internalizing, externalizing, comorbid internalizing and externalizing and ASD. Disorder groups: Internalizing: GAD, MDD, dysthymia, social phobia, and separation anxiety; Externalizing: ODD, CD, and ADHD; ASD: Autistic Disorder, Asperger’s Disorder.
Sex Differences in Psychiatric Co-Occurrences
Boys were more likely than girls to screen positive for one or two psychiatric disorders, but when three or more disorders were identified, no sex differences were found. Boys were more likely than girls to screen positive for externalizing disorders (30% vs 20%). However, the prevalence of positive screens for internalizing disorders (12% vs 12%) and ASD (5% vs 4%) were similar in boys and girls (Figure 1).
Correlates Between Co-Occurrence and Functional Impairment
Number of Positive Screens for Psychiatric Disorders and School Functioning.
School functioning was more likely to be impaired when a child screened positive for a higher number of psychiatric disorders. In children with no positive screens for psychiatric disorders,16% repeated a grade, 44% had an individualized educational program (IEP), 10% required an aide in school, and 15% were placed in a special remedial class (Table 3). In comparison, children with two or more positive screens for psychiatric disorders had significantly higher rates: 27-34% repeated a grade, 80% had an IEP, 16-23% required an aide in school, and 30-38% were placed in a special remedial class. Children who screened positive for only one psychiatric disorder were not different from children with no positive screens, except for having an IEP (44% vs 66%). As expected, children who screened positive for more psychiatric disorders were reported by their parents to have lower levels of school functioning as measured by the PedsQL School Functioning subscale. The ELGAN children with no positive screens had the highest level of school functioning (67% of children with 0 positive screens), whereas only 17% of children with three or more positive screens were identified as such. In general, compared to children with no positive psychiatric screens, children with three or more positive screens were rated by their parents as having the most impaired school functioning, followed by children with one or two positive screens. In addition, children with a positive screen for any psychiatric disorder scored reliably lower on verbal IQ compared to children with no positive screens. The number of co-occurring classifications was not significantly related to children’s verbal IQ.
Table 3.
Differences in child function by number of positive psychiatric disorder screens.
| Number of positive psychiatric disorder screens |
F (df=3); Significant group differences |
|||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | ≥ 3 | |||
| School functioning | ||||||
| Repeated a grade | Yes | 16% | 19% | 34% | 27% | 4.76** 0,1<2,3 |
| Has had an IEP | Yes | 44% | 66% | 81% | 80% | 26.79*** 0<1,2,3; 1<3 |
| Requires an aide in school | Yes | 10% | 16% | 16% | 23% | 4.51** 0,1,2<3 |
| In a special remedial class | Yes | 15% | 24% | 38% | 30% | 3.70* no group diff |
| Verbal IQ | <70 | 11% | 22% | 27% | 25% | 9.27***0>1,2,3 |
| 70-85 | 18% | 23% | 19% | 12% | ||
| 85+ | 71% | 55% | 54% | 63% | ||
| Nonverbal IQ | <70 | 9% | 19% | 24% | 14% | 9.45***0,3>1,2 |
| 70-85 | 22% | 26% | 32% | 22% | ||
| 85+ | 69% | 55% | 44% | 64% | ||
| PedsQL School Functioning | Low## | 28% | 60% | 69% | 90% | 69.63***0>1,2>3 |
| Medium | 26% | 23% | 23% | 5% | ||
| High | 46% | 16% | 8% | 5% | ||
| Medications | ||||||
| Number of psychotropic medications | 0 | 89% | 62% | 61% | 50% | 42.04***0<1,2,3 |
| 1 | 10% | 36% | 31% | 37% | ||
| ≥ 2 | 1% | 2% | 8% | 13% | ||
| Quality of Life | ||||||
| PedsQL Physical Functioning | Low | 13% | 24% | 33% | 40% | 38.10***0>1>2,3 |
| Medium | 12% | 13% | 26% | 27% | ||
| High | 75% | 63% | 41% | 33% | ||
| PedsQL Emotional Functioning | Low | 17% | 39% | 48% | 72% | 45.47***0>1>2>3 |
| Medium | 25% | 23% | 33% | 15% | ||
| High | 58% | 38% | 19% | 13% | ||
| PedsQL Social Functioning | Low | 16% | 36% | 56% | 66% | 60.73***0>1>2>3 |
| Medium | 17% | 24% | 19% | 17% | ||
| High | 67% | 40% | 25% | 17% | ||
| Maternal characteristics | ||||||
| Age, years | <21 | 11% | 13% | 30% | 15% | 9.33***0>2,3 |
| 21-35 | 66%% | 72% | 56% | 72% | ||
| >35 | 23% | 15% | 14% | 13% | ||
| Education, years | ≤ 12 | 37% | 48% | 51% | 54% | 59.97**0,1>2,3 |
| < 12-16> | 25% | 15% | 22% | 24% | ||
| ≥ 16 | 38% | 37% | 27% | 22% | ||
| Single marital status | Yes | 37% | 43% | 47% | 50% | 3.13*; no group diff |
| Public insurance | Yes | 30% | 43% | 42% | 57% | 11.52*** 0<1,3 |
Note: F statistics for group differences (reported as percentages) for the number of positive psychiatric disorders are adjusted for maternal education and child IQ at age 10. Maternal education and child verbal and nonverbal IQ models are unadjusted.
p<.001;
p<.01;
p<.05
Low <70, 70<Medium (Intermediate) <85, High >85. PedsQL subscales are scaled 0 to 100, with a score of 70 or less indicating impaired quality of life
Number of Positively Screened Psychiatric Disorders and Exposure to Psychotropic Medications.
Past and current exposure to psychotropic medications was more likely in participants who screened positive for any psychiatric disorders compared to those who had none. Among ELGAN Study children who did not screen positive for any psychiatric disorder, only 11% had any exposure to medication for ADHD, mood disorder, or anxiety, whereas between 38 and 50% of children who screened positive for one or more psychiatric disorders had exposure to psychotropic medications. (Table 3).
Number of Positively Screened Psychiatric Disorders and Functional Impairment.
ELGAN children were more likely to have lower parent-rated quality of life in physical, emotional, or social functioning, if they had a higher number of positive screens for psychiatric disorders. For example, low physical functioning was characteristic of 13% of children with no positive screens for psychiatric disorders, 24% of children with one, 33% of children with two, and 40% of children with three or more. Similar patterns were observed for low emotional functioning (17%, 39%, 48%, and 72% respectively) and low social functioning (16%, 36%, 56%, and 67%) (Table 3). In each case, the greater number of positive psychiatric disorder screens was reflected in lower physical, emotional, and social functioning, and having any co-occurrence (two or three or more positive screens) was related to significantly lower scores on PedsQL subscales. These findings were expected given that children with psychiatric disorders tend to show increased social and emotional dysfunction.
Number of Positively Screened Psychiatric Disorders and Social and Demographic Characteristics of the Mother.
Some maternal characteristics (e.g. younger maternal age, lower levels of education, and relying on public health insurance) were associated with one or more positively screened psychiatric disorders as reported by parents. Children with no positive screens for psychiatric disorders were more likely than others to have been born to women who had indicators of higher socio-economic status (e.g. higher levels of education, and not eligible for public health insurance) as well as with older maternal age. With the exception of maternal education, children who screened positive for one, two, or three or more psychiatric disorders were not significantly different from each other in terms of maternal characteristics. (Table 3).
DISCUSSION
The aim of this report was to describe the prevalence, sex differences in these prevalence rates, co-occurrence, and functional impact of positively screened psychiatric disorders among 10-year-old children born EP. We found higher rates of internalizing and externalizing symptoms as well as autism spectrum in children born EP, as compared to the normative expectations from the CSI-4. In addition, we found that psychiatric co-occurrence in children born EP is frequent, the most common being co-occurrence between internalizing and externalizing symptoms followed by externalizing symptoms and Asperger’s Disorder (now classified as ASD according to DSM-5 criteria). In general, co-occurrence rates in our ELGAN sample are higher than expected in the general population and similar to rates seen in other behavioral disorders. Epidemiological studies in the United States have found that of the 13% of the population that had at least one disorder, a fifth had two or more disorders.26 By contrast, co-occurrence is more frequent in youth with behavioral disorders. For example, in a multi-centered European study of co-occurrence prevalence and treatment outcome in a clinical sample of treatment naïve youth, of 1919 individuals who met diagnostic criteria for ADHD, a third had ADHD only, while two-thirds had at least one co-occurring psychiatric disorder, with those who had more severe impairment being more likely to present with co-occurring psychiatric disorders.26, 27 This is similar to our findings suggesting that 30% of the ELGAN population screened positive for at least one psychiatric disorder, and that children with positive screens for multiple co-occurring psychiatric disorders had more significant functional impairment.
Participants had higher rates of positive screens for externalizing disorders compared to the normative expectations from the CSI-4 which was comprised entirely of children born at term. Specifically, these comparisons included ODD (8% vs 5.3%), ADHD inattentive (11% vs 3.6%), ADHD hyperactive/impulsive (4% vs 2%), and ADHD combined (6% vs 1.6%). Our finding of more children with the inattentive type of ADHD is consistent with another study that used the CSI-4 to assess preterm children at a similar age6 and our findings regarding the rate of externalizing disorders is consistent with findings from prior studies of premature children.3-7
Compared to the CSI-4 normative data, children born EP had higher rates of positive screens for internalizing disorders including GAD (6% vs 3.3%), Dysthymic Disorder (4% vs 0.7%), and Social Phobia (5% vs 1.3%). Prior studies of children born preterm have found similar rates of internalizing disorders.6-9 Children born EP also had higher rates of positive screens for autistic disorder compared to the CSI-4 normative expectations (3% vs 0.5%). This is consistent with findings from prior studies of rates of ASD in extremely premature children.7, 13
Overall, our prevalence rates of positive psychiatric screens on the CSI-4 in our EP cohort are remarkably similar to the findings of Hack and colleagues who studied psychiatric outcomes at age 8 years using the CSI-4 in an extremely low birth weight (LBW) sample.6 However, compared to Hack and colleagues, we found lower rates of conduct disorder and social phobia symptoms and higher rates of Asperger’s Disorder in our EP sample. The prevalence rates of the psychiatric symptoms in the CSI-4 normative sample that we used for comparison to our sample are strikingly similar to the prevalence rates that Hack and colleagues reported in their normal birth weight contemporaneous controls, with the exception of conduct disorder and social phobia (with slightly lower rates in the CSI-4 normative sample). Therefore, with a few exceptions, we replicate the findings of Hack and colleagues in our EP cohort which has a much larger sample size and was enrolled based on gestational age rather than birth weight. In addition, we extend the findings of Hack and colleagues by assessing the impact of psychiatric burden on child functioning, controlling for child IQ and maternal education.
ELGAN girls, but not boys, were more likely relative to normative expectation to screen positive for Dysthymic Disorder; conversely, ELGAN boys, but not girls, were more likely to screen positive for ADHD hyperactive/impulsive subtype and for Autistic Disorder. Our sex difference findings were somewhat different from Hack and colleagues who found that the only significant sex difference was in the prevalence of Generalized Anxiety Disorder which was higher only in LBW girls.6 We also found that a quarter of our EP girls and a third of the EP boys had positive screens for one or more psychiatric disorders This difference in prevalence rates of positive screens by sex in our cohort is likely due to the higher male prevalence of ADHD hyperactive/impulsive subtype and of Autistic Disorder. Our finding that EP girls are less affected than boys by psychiatric symptoms is consistent with the findings of Burnett and colleagues who found girls tended to have minimal symptoms on the problem scales of the Strength and Difficulties Questionnaire.10
Past and current exposure to psychotropic medications was more likely in participants who had a higher number of positive screens for psychiatric disorders. However, 10% of EPs who had no positive screens for psychiatric disorders based on parent CSI-4 ratings, were reported to have been prescribed a psychotropic medication. A possible explanation is that parents did not report symptoms on the CSI-4 as those children were being adequately treated with medication and symptoms were less apparent at age 10 years. This also may partially explain the finding by other investigators that children born prematurely are more likely than children born at term to be prescribed psychotropic medications in young adulthood,11 and will be important to examine in our sample as the children move into their adolescent years. Taken together, these findings raise the issue of how medication is prescribed to children born EP in that prescribing practices may not be directly related to diagnosis but rather to symptom manifestation.
We found that psychiatric co-occurrence in EPs occurs frequently and has significant functional impact: greater co-occurrence (i.e., higher numbers of positive screens for psychiatric disorders) was associated with more impaired school function, higher likelihood of receiving psychotropic medication, and decreased physical, emotional and social function. Though a recent study reported on the association between behavioral domains on the Strengths and Difficulties Questionnaire and cognitive and academic performance,10 we extend these findings by examining the associations between psychiatric burden and multiple domains of daily functioning in EP born children. Importantly, though, others have reported similar functional correlates of psychiatric co-occurrence among children born at term.17-19 In addition, we found that certain maternal characteristics (older maternal age, higher levels of education, positive marital status, and non-public insurance) were associated with lower number of positive screens for psychiatric disorders (similar to the finding that socioeconomic state is an antecedent to ADHD in ELGANs at age 10).28
Clinical and Research Implications
The frequency of psychiatric co-occurrence and its significant functional impact is of great importance because clinicians managing behavioral health in children and adolescents frequently encounter co-occurring psychiatric presentations but have limited evidence-based information to guide diagnostic and treatment decisions. This is especially significant for EP children, who tend to have more complex medical and developmental presentations, and consequently are at greater risk for psychiatric manifestations over their life course. The implications of these findings are that clinicians should conduct early and structured screening for psychiatric conditions among the EP population. In addition, clinicians should carefully assess for and provide ongoing monitoring for psychiatric co-occurrence in a child with a history of prematurity and at least one existing psychiatric diagnosis, and carefully determine if any psychopharmacotherapies or other treatments may be needed to address the psychiatric diagnoses. The results of our study suggest that earlier identification of psychiatric symptoms could facilitate earlier initiation of intervention which may alleviate some of the associated functional impairment.
Study Strengths and Limitations
The primary strengths of this study are the relatively large sample, which enhances statistical power, and the selection of study participants based on gestational age and not birth weight, which limits bias from correlates of fetal growth restriction. In addition, the large number of participants available for follow-up assessment at age 10 years allows us to provide relatively reliable estimates of prevalence. Because follow-up data were collected prospectively, concern for recall bias is lessened. This study is unique in that it assesses positive psychiatric screens by sex and addresses psychiatric burden by assessing psychiatric co-occurring classifications and the functional impact of positively screened psychiatric disorders on individuals born extremely preterm.
Limitations of this study include the lack of direct evaluation of maternal psychiatric health and reliance on a parent-report screening tool, the CSI-4, to estimate rates of psychiatric symptoms.22 It is important to note that when this study was initiated, the DSM-IV provided the standard assessment of psychiatric disorders and served as a basis for the CSI-4. While the diagnostic criteria across most childhood disorders are largely similar between DSM-IV and DSM-5, there are some notable differences such as with ASD. The limitation of the CSI-4 is illustrated by our finding that when a rigorous diagnostic protocol was used, 7% of the ELGAN cohort was diagnosed with autism spectrum disorder.29 As teacher reports for the CSI-4 were unavailable for a large proportion of this cohort, we did not include information from different raters and settings. Importantly, a prior study of this sample suggested that only occasionally did agreement between parent and teacher provide more information than that provided by one reporter.30 Parents completed both the CSI-4 and PedsQL, thus likely introducing some level of responder bias into both measures. In addition, this cohort did not have an age-matched sample of children born at term or a contemporaneous peer group, requiring us to use the CSI-4 normative expectations, based on a sample of relatively healthy term born children in our rate comparisons. This normative sample of children did not include children in special education who may have higher rates of psychiatric symptoms. Therefore, it is possible that the differences in rates of psychiatric symptoms between the ELGAN cohort and the general term-born population is less than reported in this study. Moreover, given that the study design was observational, we were able to identify only non-causal associations between psychiatric symptoms and quality of life in our extremely preterm sample. Finally, with ongoing neurodevelopmental surveillance, we suspect that the prevalence of psychiatric disorders will be higher when assessed at post-pubertal ages. Given this limitation, and the limitations posed by our use of a screening instrument, the next important step will be to conduct comprehensive standardized psychiatric diagnostic interviews which we will do in our next wave of assessments.
Supplementary Material
Acknowledgements:
This study was supported by The National Institute of Neurological Disorders and Stroke (5U01NS040069-05; 2R01NS040069 - 06A2) and the National Institute of Child Health and Human Development (5R01HD092374-02 and 5P30HD018655-34) and the Office of the National Institutes of Health Director (1UG3OD023348-01). Dr. Frazier has the following disclosures: receiving research support from Takeda Pharmaceuticals, Fulcrum Therapeutics, Janssen Research and Development and Roche. No funds from these entities supported this project, and none of these entities reviewed/commented on this study. All other authors declare no financial or ethical conflicts of interest.
We are especially grateful to the participants and their families whose commitment to the ELGAN Study has made this work possible. We also acknowledge the inspiration, guidance and collaboration of Alan Leviton and Elizabeth Allred in conducting the ELGAN Study.
Contributor Information
Yael Dvir, Eunice Kennedy Shriver Center, University of Massachusetts Medical School, Worcester, MA.
Jean A. Frazier, Eunice Kennedy Shriver Center, University of Massachusetts Medical School, Worcester, MA.
Robert M. Joseph, Boston University School of Medicine, Boston, MA.
Irina Mokrova, University of North Carolina at Chapel Hill, Chapel Hill, NC.
Phoebe S. Moore, Eunice Kennedy Shriver Center, University of Massachusetts Medical School, Worcester, MA.
T. Michael O’Shea, University of North Carolina at Chapel Hill, Chapel Hill, NC.
Stephen R. Hooper, University of North Carolina at Chapel Hill, Chapel Hill, NC.
Hudson P Santos, Jr, University of North Carolina at Chapel Hill, Chapel Hill, NC.
Karl Kuban, Boston University School of Medicine, Boston, MA
REFERENCES
- 1.Stoll B, Hansen N, Bell E, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126(3): 443–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Treyvaud K, Ure A, Doyle LW, et al. Psychiatric outcomes at age seven for very preterm children: rates and predictors. Journal of Child Psychology and Psychiatry. 2013;54(7): 772–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taylor HG, Klein N, Minich NM, et al. Middle‐school‐age outcomes in children with very low birthweight. Child development. 2000;71(6): 1495–1511. [DOI] [PubMed] [Google Scholar]
- 4.Elgen I, Sommerfelt K, and Markestad T. Population based, controlled study of behavioural problems and psychiatric disorders in low birthweight children at 11 years of age. Archives of Disease in Childhood-Fetal and Neonatal Edition. 2002;87(2): F128–F132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Delobel-Ayoub M, Arnaud C, White-Koning M, et al. Behavioral problems and cognitive performance at 5 years of age after very preterm birth: the EPIPAGE Study. Pediatrics. 2009;123(6): 1485–1492. [DOI] [PubMed] [Google Scholar]
- 6.Hack M, Taylor HG, Schluchter M, et al. Behavioral outcomes of extremely low birth weight children at age 8 years. Journal of developmental and behavioral pediatrics. 2009;30(2): 122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson S, Hollis C, Kochhar P, et al. Psychiatric disorders in extremely preterm children: longitudinal finding at age 11 years in the EPICure study. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(5): 453–463. [PubMed] [Google Scholar]
- 8.Boyle M, Miskovic V, Van Lieshout R, et al. Psychopathology in young adults born at extremely low birth weight. Psychological medicine. 2011;41(8): 1763–1774. [DOI] [PubMed] [Google Scholar]
- 9.Conrad AL, Richman L, Lindgren S, et al. Biological and environmental predictors of behavioral sequelae in children born preterm. Pediatrics. 2010;125(1): e83–e89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burnett AC, Youssef G, Anderson PJ, et al. Exploring the "Preterm Behavioral Phenotype" in Children Born Extremely Preterm. J Dev Behav Pediatr. 2019;40(3): 200–207. [DOI] [PubMed] [Google Scholar]
- 11.Crump C, Winkleby MA, Sundquist K, et al. Preterm birth and psychiatric medication prescription in young adulthood: a Swedish national cohort study. International journal of epidemiology. 2010;39(6): 1522–1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gray RF, Indurkhya A, and McCormick MC. Prevalence, stability, and predictors of clinically significant behavior problems in low birth weight children at 3, 5, and 8 years of age. Pediatrics. 2004;114(3): 736–743. [DOI] [PubMed] [Google Scholar]
- 13.Pinto-Martin JA, Levy SE, Feldman JF, et al. Prevalence of autism spectrum disorder in adolescents born weighing< 2000 grams. Pediatrics. 2011;128(5): 883–891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lindström K, Lindblad F, and Hjern A. Psychiatric morbidity in adolescents and young adults born preterm: a Swedish national cohort study. Pediatrics. 2009;123(1): e47–e53. [DOI] [PubMed] [Google Scholar]
- 15.Linsell L, Malouf R, Morris J, et al. Prognostic factors for poor cognitive development in children born very preterm or with very low birth weight: a systematic review. JAMA pediatrics. 2015;169(12): 1162–1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kessler RC, Avenevoli S, Costello J, et al. Severity of 12-month DSM-IV disorders in the national comorbidity survey replication adolescent supplement. Archives of General psychiatry. 2012;69(4): 381–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Staller JA. Diagnostic profiles in outpatient child psychiatry. American Journal of Orthopsychiatry. 2006;76(1): 98–102. [DOI] [PubMed] [Google Scholar]
- 18.Basten MM, Althoff RR, Tiemeier H, et al. The dysregulation profile in young children: empirically defined classes in the Generation R study. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52(8): 841–850. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Biederman J, Petty CR, Clarke A, et al. Predictors of persistent ADHD: an 11-year follow-up study. Journal of psychiatric research. 2011;45(2): 150–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O’shea T, Allred E, Dammann O, et al. The ELGAN study of the brain and related disorders in extremely low gestational age newborns. Early human development. 2009;85(11): 719–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Helderman JB, O’Shea TM, Kuban KC, et al. Antenatal antecedents of cognitive impairment at 24 months in extremely low gestational age newborns. Pediatrics. 2012;129(3): 494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sprafkin J, Gadow KD, Salisbury H, et al. Further evidence of reliability and validity of the Child Symptom Inventory-4: Parent checklist in clinically referred boys. Journal of Clinical Child and Adolescent Psychology. 2002;31(4): 513–524. [DOI] [PubMed] [Google Scholar]
- 23.Gadow KD and Sprafkin JN. Child symptom inventory 4 : screening and norms manual. Stony Brook, N.Y.: Checkmate Plus; 2002 [Google Scholar]
- 24.Varni JW, Seid M, and Rode CA. The PedsQL™: measurement model for the pediatric quality of life inventory. Medical care. 1999: 126–139. [DOI] [PubMed] [Google Scholar]
- 25.Elliott C Differential Ability Scales - Second edition (DAS-II). San Antonio, TX: Harcourt Assessment; 2007 [Google Scholar]
- 26.Boyd JH, Burke JD, Gruenberg E, et al. Exclusion criteria of DSM-III. A study of co-occurrence of hierarchy-free syndromes. Arch Gen Psychiatry. 1984;41(10): 983–989. [DOI] [PubMed] [Google Scholar]
- 27.Reale L, Bartoli B, Cartabia M, et al. Comorbidity prevalence and treatment outcome in children and adolescents with ADHD. Eur Child Adolesc Psychiatry. 2017;26(12):1443–1457. [DOI] [PubMed] [Google Scholar]
- 28.Leviton A, Hoope SR, Hunter SJ, et al. Antecedents of Screening Positive for Attention Deficit Hyperactivity Disorder in Ten-Year-Old Children Born Extremely Preterm. Pediatr Neurol. 2018;81: 25–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Joseph RM, O’Shea TM, Allred EN, et al. Prevalence and associated features of autism spectrum disorder in extremely low gestational age newborns at age 10 years. Autism Res. 2017;10(2): 224–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leviton A, Hunter SJ, Scott MN, et al. Observer variability identifying attention deficit/hyperactivity disorder in 10-year-old children born extremely preterm. Acta Paediatr. 2017;106(8): 1317–1322. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.