Abstract
As the opioid epidemic continues to worsen throughout the United States, researchers and practitioners require additional tools to help in efforts to address use and prevent overdose. Although opioids are increasingly of concern to all racial and socioeconomic groups, specific geographic regions and sub-populations remain more burdened by overdoses than others. The example of Flint, Michigan, is used to contextualize the landscape of opioid overdose death and understand geographic and demographic variation in risk. Kernel density analysis and spatial joins in ArcGIS were used to map opioid overdose death clusters, treatment availability, and neighborhood-level conditions to uncover factors related to overdose death.
Spatial analysis revealed three geographic clusters in opioid overdose death in Flint. These neighborhoods tended to be somewhat poorer but also significantly Whiter than the average Flint neighborhood. Alternatively, opioid overdose death clusters did not occur in predominately African-American neighborhoods. As well, treatment sites were not coincident with the location of overdose death clusters, suggesting a potential need for geographically-targeted interventions. Of the 47 treatment sites, only 29 offered medication-assisted treatment, and expansion of these programs may therefore be warranted. This work is of great importance to ongoing prevention and treatment efforts in Flint, but also to other communities with a need for better tools to monitor and intervene in the opioid epidemic.
Keywords: Geographic Information Systems (GIS), Opioids, Overdose, Prevention
1. Background
Abuse of heroin and prescription opioids remains a critical public health problem across the United States (Arria and Compton, 2017; Kolodny et al., 2015). The problem is exacerbated in low-income communities and in regions where people lack access to healthcare services and other basic amenities, including the shrinking cities of the Rust Belt (Williams and Latkin, 2007; Weiss et al., 2004). A deprivation amplification effect can occur in these regions, by which marginalized populations incur further negative health outcomes as a function of the built environments where they live (Macintyre, 2007; Mennis et al., 2012).
Researchers are increasingly incorporating the built environment into their models for predicting salutogenic and pathogenic behaviors such as healthy eating or physical activity, but consideration of how the built environment can affect risk for substance use disorder (SUD) or how SUD may cluster in certain neighborhoods has been understudied (see for example: McLafferty, 2008; Généreux et al., 2010; Mennis et al., 2011).
The phenomenon of clustering itself is tied to the Tobler’s First Law of Geography, which offers that—while all objects are related in space—objects nearer to one another are more related (Tobler, 2004). Examples of this phenomenon include how businesses and innovation cluster in key areas (Schiele, 2008; Baptista, 2001) (e.g. Silicon Valley), and how disease and health risk tends to cluster in disadvantaged areas and places where environmental exposure is concentrated (Margolis et al., 2011; Chakraborty, 2011).
In the case of heroin/opioid overdose death (OOD), specific built environmental characteristics cause OOD to cluster by way of the deprivation amplification effect noted above. Studies have found that neighborhoods with more overdoses and overdose reversal sites had higher income inequality, more white residents, more drug arrests, and higher population density (Bohnert et al., 2011; DiMaggio et al., 2011; Rowe et al., 2008).
Using what is known about environmental determinants of the risk of OOD and building on the literature about activity spaces, geographic information systems (GIS) can provide a lens through which to uncover a deeper understanding of the effect of the built environment. Such mapping is of great value to urban planners and policymakers in their pursuit of healthier cities.
What is currently known about drug use and the built environment comes primarily from large urban contexts (e.g., Furr-Holden et al., 2016; Deering et al., 2014; Hembree et al., 2005) or nationwide studies (Stewart et al., 2017); little work has been conducted on individual mid-sized urban regions. In terms of large urban regions, Cerda et al. (2013) examined opioid overdose fatalities in relation to built environment factors across New York City. They observed the connection between deterioration of the built environment and increased risk of overdose fatality (Cerda et al., 2013).
Stewart et al.’s (2017) county-level study of the United States showed the diffusion of the opioid epidemic across the country and used Moran’s I to determine if significant clusters existed. This is of great importance to regional strategies, but local level analysis is equally important for prioritizing service provision.
Such local analysis is important because, at the regional level and especially across the Rust Belt, the historical context and built environment likely have a differential effect on the risk for drug use and overdose (Teixiera, 2016; Kruger et al., 2007). Such cities have high vacancy rates and levels of socioeconomic distress, which correlate to opportunity spaces for drug use (Draus et al., 2012). McLean (2016) likewise noted deindustrialization—a key shared characteristic of cities across the Rust Belt—as a risk factor for overdose. As well, a recent report identified emerging trends in heroin overdose and found that younger, White males in the Mid-Atlantic and Great Lakes regions had the highest rates of overdose (Stewart et al., 2017). Our goal in this report is to map the geographic and socioeconomic variations in OOD in the Rust Belt city of Flint, Michigan, to inform future prevention and treatment efforts locally and create a template other mid-sized cities may follow.
Flint offers an interesting case study because of its concentrated poverty and racial bifurcation. The African-American population has experienced a long history of discrimination in housing, employment, and education, and remains segregated primarily in the northwest and southeast parts of the city (Sadler and Lafreniere, 2016; Sadler and Highsmith, 2016; Highsmith and Erickson, 2015). Even so, white flight has meant that both the predominately African-American (57%) and the White (37%) populations have poverty rates of around 40% (Minnesota Population Center, 2011). This similar socioeconomic trajectory but different structural past raises questions about how and why OOD may vary in the area.
2. Methods
2.1. Data
The data for this study included every treatment site (n=47) and OOD from 2013 to 2015 in Genesee County, Michigan (n=543), as well as socioeconomic data from the 2010 United States Census. Data on treatment sites were obtained from the Michigan Department of Licensing and Regulatory Affairs Bureau of Health Systems' License Listing Report (2017) and included all behavioral health organizations licensed to provide direct drug treatment services including inpatient and outpatient services. Twenty-nine of the 47 treatment locations were licensed to provide medication-assisted services (SAMHSA, 2019). The analytic data also include a distress index signifying an unweighted sum of the z-scores for community-level rates of low educational attainment, poverty, unemployment, and lone parenthood (as used in Sadler et al., 2017). Overdose deaths1 were obtained from the Genesee County 911 Consortium (2015) and treated as discrete point data. The OOD data included some details beyond location, but were not linked with individual identifiers such as age, sex, or race (thus our rationale for an ecological study by cross-referencing community-level data to infer some such relationships).
2.2. Analytic Techniques
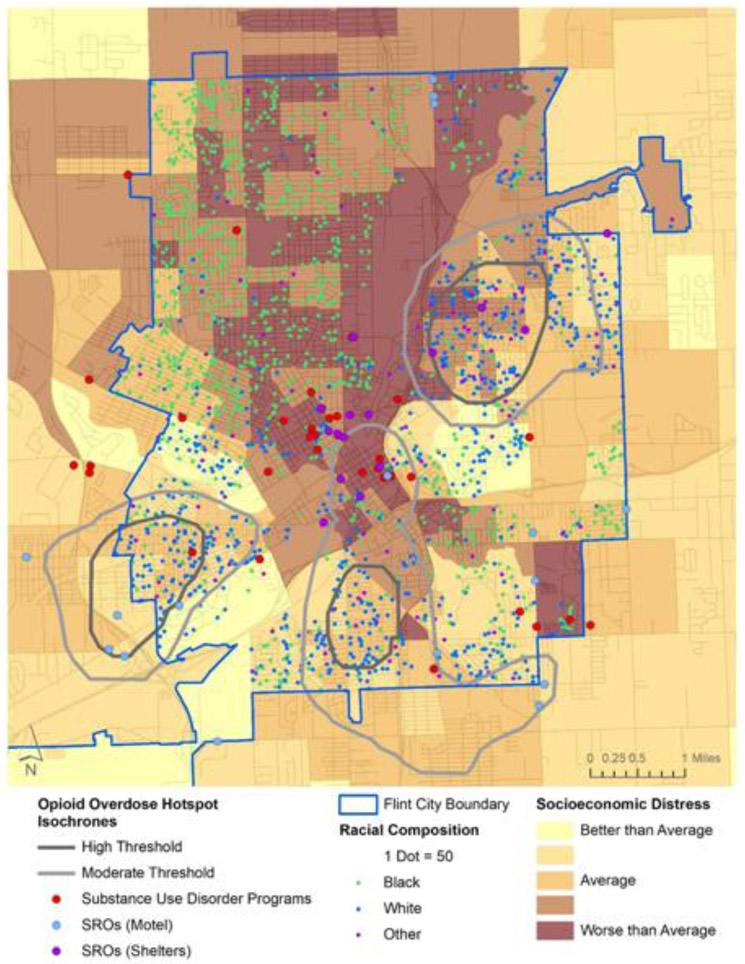
Every treatment site (shown in red circles in Figure 1) and OOD was geocoded to its exact location using a custom address locator for Genesee County using ArcGIS (ESRI, 2018). We then conducted a series of joins between OODs and census block group (CBG)-level data to contextualize the places where OOD occured. This included linking CBG-level characteristics such as race and socioeconomic status to each OOD. We also ran kernel density analysis—with an optimized bandwith estimating number of OODs per square mile2 (ArcGIS, 2019)—to highlight clusters in OOD and determine how many treatment sites fell within existing clusters. We simplified their representation into ‘high’ (>20 OODs per square mile) and ‘moderate’ (10-20 OODs per square mile) threshold isochrones3 for visualization and confidentiality purposes (shown as black and grey lines in Figure 1). Figure 1 also shows neighborhood socioeconomic distress (in shades of yellow to brown) and racial composition (with Black residents in green, White residents in blue, and residents of other races in purple), which are irrespective of the clusters of OODs. We also mapped annual and seasonal variation as an additional tool to use in resource planning and allocation (figures discussed but not shown in results).
Figure 1.
Clustering of Opioid Overdose Deaths, Substance Use Disorder Programs, SROs, Racial Composition, and Socioeconomic Distress in Flint, MI.
3. Results
3.1. Clustering of OOD Deaths
After running kernel density analysis, we highlighted the OODs that occurred within these clusters (signifying the intensity of the clustering). Three clusters emerged from this analysis, including one in northeast Flint (Eastside), one in south Flint (Lincoln Park), and one in southwest Flint (Westside). Observing the racial and socioeconomic composition of the areas within these clusters on Figure 1 revealed that these tended to be poorer White neighborhoods.
A total of 543 opioid overdose deaths were recorded during the study period. The average population during this study period was 98,919, yielding an average annual rate of 18 deaths per 10,000 population. Of these, 241 OODs (or 44%) occurred in these three clusters, despite the fact that those clusters comprised only 11 square miles and encompassed approximately 41,000 people (or approximately 2% of the land area and 10% of the population of Genesee County). This means the probability of OOD in these clusters is 26 times higher as a function of geography and 5 times higher as a function of population density.
3.2. Seasonal Variations
Though not shown in a figure, we also ran individual kernel density analyses by season and year. Seasonally, summer saw the fewest OODs, with 143 in winter, 151 in spring, 110 in summer, and 139 in fall. In contrast to the overall number of OODs during the summer, the northeast cluster and the northern part of the southern cluster (in Flint’s downtown) are worst in the summer. The southernmost part of the southern cluster, in contrast, disappears in the summer. The absence of more intense clusters in the fall, winter, and spring suggests these may be more geographically dispersed than summer OODs.
3.3. Temporal Variations
Annually, the incidence of OOD increases by nearly a third throughout the time period, with 155 incidents in 2013, 185 in 2014, and 203 in 2015 (a change from 15.5 to 20.7 deaths per 10,000 population). The cluster pattern annually disperses away from the 3 primary clusters, encapsulating a larger area, but no new clusters emerge. Thus in general, existing clusters are getting worse while relatively unaffected areas continue to be spared from OOD.
3.4. Co-occurrence with other Socioeconomic Factors
The locations of OODs were cross-referenced with local housing and demographic data at the CBG level to determine general neighborhood-level characteristics associated with OOD. The rate of OOD was most strongly correlated with density of White residents (R = 0.41, p < 0.01), followed by percent of vacant properties (R = 0.28, p < 0.01), vacancies per square mile (R = 0.25, p < 0.01), and population density (R = 0.23). It was weakly, but not significantly, correlated with density of Black residents (R = −0.06, p = 0.23).
CBG characteristics normalized to z-scores were also appended to each OOD, and mean values were derived for a series of socioeconomic variables. Because OODs occurred in a wide range of neighborhoods, the mean values for each variable fell very close to 0. Low educational attainment had the highest score (z = 0.24, range = −1.61 to 2.92), followed by poverty rate (z = 0.09, range = −1.01 to 4.04), unemployment (z = 0.07, range = −1.21 to 5.43), and lone parenthood (z = −0.03, range = −1.21 to 3.50). As well, on average, the neighborhoods where overdose deaths occurred were nearly 80% White (contrasting with the fact that Flint is only 37% White).
3.5. Treatment Sites
Because one of the long-term goals of this research is to use this information to help inform treatment services, the location of treatment sites were incorporated into the analysis. Genesee County has 47 treatment sites in total, but only 1 falls within the ‘high threshold’ cluster (in west Flint on Figure 1), and only 7 fall within even a moderate intensity cluster (mostly in the center of Flint on Figure 1)—these sites combined thus only account for 17% of the total. A cluster of sites exist around a hospital north of the center of Flint, and others are scattered near some clusters, but otherwise they are not coincident with the most intense clusters for OOD.
4. Discussion
From this brief analysis, we have geographically situated the nature of the problem of OODs in Flint and Genesee County in terms of neighborhood racial and socioeconomic composition, including with respect to existing support services. OODs increased from 2013 to 2015 by approximately 31%. This trends very closely with the Michigan average during a similar period, which increased from 14 to 20 deaths/100,000 population from 2010 to 2015 (Rudd et al., 2016). Given similarities to state- and national-level trends, similar inquiries elsewhere could aid regional and national efforts to reverse the opioid epidemic.
OOD incidence was lowest but more geographically clustered in the summer. This trend aligns with two Italian studies that found overdoses to be more common in winter months (Rocchi et al., 2003; Rocchi et al., 2004). Conversely, it runs counter to one Ohio-based study indicating opioid prescribing is more common in the summer (Weiner et al., 2017), and an Australian study suggesting that people (some of whom were suspected of having overdosed on opioids) were more likely to leave emergency departments prior to treatment in the summer (Lee et al., 2004). The reasons for clustering more in the summer could be due to a social network effect whereby people may spend more time together in the summer (Schroeder et al., 2001), but remained unexplained.
We discovered that all 3 OOD clusters in Flint occurred in areas that were poorer, had a higher proportion of White residents, and had relatively higher vacancy rates. While the northeast cluster and the northern part of the southern cluster are most intense in the summer, the southernmost part of the cluster in south Flint disappeared during the summer. The causes for this are not clear from the data, but may be attributable to lower population density in this area. Further investigation is necessary to uncover potential reasons for geographic clustering of OODs overall or seasonally.
CBG-level analysis also revealed that the socioeconomic factors community-level low educational attainment, poverty, unemployment, and lone parenthood were not strongly correlated to the location of OOD. The lack of a relationship between predominately Black neighborhoods and OODs does not mean efforts should not be made across the community to limit the spread of OOD; rather, only that existing clusters occur in neighborhoods with more White residents. Continued monitoring is necessary to ensure these clusters do not wind up spreading to more neighborhoods, particularly given the closing gap in opioid use among African-Americans (Chen et al., 2005; New York Times, 2017).
The specific location of the clusters may also be considered in the context of other built environmental features such as those that have been discussed in prior work, including single-room occupancy housing, extended stay motels, and section 8 housing (Davidson et al., 2003; Bardwell et al., 2017). No authoritative list of such housing exists for Genesee County, but an examination of business and shelter listings revealed a distinction among our three primary clusters. The center of the south cluster has no motels or shelters. In contrast, the northeast cluster has three shelters within the core, and the southwest cluster is coincident with four motels and a shelter, including one motel that was closed in 2015 due to excessive drug activity and prostitution (25News, 2015). The difference in the relationship between SROs and these clusters warrants further examination. Additionally, the co-location of many services and shelters in the downtown (center) of the city may have a protective effect.
We discovered a lack of overlap between existing treatment sites and OOD clusters. There were only twenty-nine medication-assisted treatment programs among the 47 treatment sites, and the strongest evidence for preventing OOD is associated with medicated assisted treatment programs (e.g., Leshner et al., 2019; Kolody et al. 2015; Schartz et al., 2013). This lack of association between treatment sites and OOD is also troubling from the perspective that opioid users may also have mobility restrictions (Draus et al., 2017), thus many of the people who would conceivably suffer from opioid misuse are not geographically proximate to the resources they need to recover. This presents a direct opportunity for service providers in Flint to consider specific sites for future expansion or relocation of medication assisted program in these clusters. Likewise, because the methods are general and novel, this exercise can easily be replicated by service providers and support services in other communities (with access to GIS expertise) to help those places optimize their service provision. Evaluation of effectiveness of service delivery could be conducted by tracking clusters or hot spots before and after service provision to such neighborhoods. Such an approach has been suggested previously. In one study, authors discovered no relationship between opioid prescribing practices and overdose clusters at the ZIP code level, and suggested that increasing access to prevention and treatment services may have a better chance of reducing those clusters (Stopka et al., 2019).
Limitations of the utility of this work include the challenges often faced in retrieving recent OOD data and the validity of that data, which has to be verified and updated on the medical record. This can take serval months, if it happens at all. Also, there are great disconnects in many states between first responder data, hospital data, and medical examiner data and antiquated data collection and data sharing systems.
This study has both direct and future implications for work on opioid overdose prevention in Flint and elsewhere. Our team comprises part of the Flint Center for Health Equity Solutions (an NIMHD-funded Transdisciplinary Collaborative Center), of which one public health intervention is a deployment of the evidence-based strengthening families program and peer recovery support services. We intend to use these results to partner with the health department and other service providers to prioritize sites for Narcan/Naloxone distribution and unused medication collection. Given the community integrated nature of that center, we recommend community participatory approaches that elicit feedback and information from community members to better inform researchers, service providers, and policy makers on the needs of and possible preventive intervention strategies for this population (Palombi et al., 2018).
Our findings also build on the long history of integrating concepts of place and health into the study of drug use (Cooper and Tempalski, 2014). Both of relevance to the Flint community and more broadly, given our findings on the relationship between vacant properties and OODs, we suggest that environmental strategies to combat the opioid epidemic should dovetail with strategies to reduce blight and improve economic opportunity in declining communities both urban and rural (Eisenberg, 2019). We likewise offer that, although this study presents data from only one community, the method employed is useful for identifying any community’s spatial clusters of opioid overdose deaths and understanding the neighborhood context behind this challenge.
We also acknowledge the advances made in activity space tracking of drug use and drug markets, which provide for greater specificity in understanding the types of neighborhoods where drug use and overdose are more common (Curtis and Curtis, 2017; Kirchner and Shiffman, 2016). We therefore situate our work in that context, recommending that future research projects partner with agencies on work of this nature to understand individual drug use/market behavior. Through building on such advances, we can more fully uncover the connections between the built environment and drug use and plan community-level intervention strategies.
Highlights.
Treatment sites were not coincident with the location of overdose death hotspots
Kernel density analysis and spatial join in ArcGIS were used
Environmental strategies need to be used to combat the opioid epidemic
Acknowledgments
Role of Funding Source
None.
Footnotes
Overdose deaths were defined as those reported by the 911 Consortium via toxicology reports.
The optimized bandwidth is calculated from a formula including the mean center of all points in the set, the distance from the center to all points, and a generated standard distance.
Lines representing identical values, similar to elevation lines on a topographic map.
Conflict of Interest
The authors declare they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 25News, 2015. Court ruling closes Hometown Inn, and evictions start. Retrieved from: https://nbc25news.com/news/local/court-ruling-closes-hometown-inn-and-evictions-start.
- ArcGIS Pro (2019). How Kernel Density Works. Retrieved from: https://pro.arcgis.com/en/pro-app/tool-reference/spatial-analyst/how-kernel-density-works.htm.
- Arria AM, & Compton WM, 2017. Complexities in understanding and addressing the serious public health issues related to the nonmedical use of prescription drugs. Addic Behav, 65, 215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baptista R (2001). Geographical clusters and innovation diffusion. Tech Fore Soc Change, 66(1), 31–46. [Google Scholar]
- Bardwell G, Collins AB, McNeil R, Boyd J, 2017. Housing and overdose: an opportunity for the scale-up of overdose prevention interventions? Harm Reduction J, 14(1), 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohnert AS, Nandi A, Tracy M, Cerdá M, Tardiff KJ, Vlahov D, & Galea S (2011). Policing and risk of overdose mortality in urban neighborhoods. Drug Alc Depend, 113(1), 62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerdá M, Ransome Y, Keyes KM, Koenen KC, Tardiff K, Vlahov D, Galea S, 2013. Revisiting the role of the urban environment in substance use: the case of analgesic overdose fatalities. Am J Pub Health, 103(12), 2252–2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakraborty J (2011). Revisiting Tobler’s first law of geography: Spatial regression models for assessing environmental justice and health risk disparities In Geospatial Analysis of Environmental Health (pp. 337–356). Springer, Dordrecht. [Google Scholar]
- Chen I, Kurz J, Pasanen M, Faselis C, Panda M, Staton LJ,… Mechaber AJ, 2005. Racial differences in opioid use for chronic nonmalignant pain. J Gen Inter Med, 20(7), 593–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HL, Tempalski B, 2014. Integrating place into research on drug use, drug users’ health, and drug policy. Int J Drug Pol, 25(3), 503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis JW, Curtis A, 2017. Using GIS for Substance Abuse Research and Intervention In Research Methods in the Study of Substance Abuse (pp. 161–178). Springer, Cham. [Google Scholar]
- Davidson PJ, McLean RL, Kral AH, Gleghorn AA, Edlin BR, Moss AR, 2003. Fatal heroin-related overdose in San Francisco, 1997–2000: a case for targeted intervention. J Urb Health, 80(2), 261–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deering KN, Rusch M, Amram O, Chettiar J, Nguyen P, Feng CX, Shannon K, 2014. Piloting a ‘spatial isolation’index: The built environment and sexual and drug use risks to sex workers. Int J Drug Pol, 25(3), 533–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMaggio C, Bucciarelli A, Tardiff KJ, Vlahov D, & Galea S (2008). Spatial analytic approaches to explaining the trends and patterns of drug overdose deaths In Geography and Drug Addiction (pp. 447–464). Springer, Dordrecht. [Google Scholar]
- Draus P, Roddy J, Greenwald M, 2012. Heroin mismatch in the Motor City: Addiction, segregation, and the geography of opportunity. J Ethn Sub Abuse, 11(2), 149–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg A, 2019. Distributive Justice and Rural America Forthcoming, Boston College Law Review, 2020. [Google Scholar]
- Environmental Systems Research Institute, 2018. ArcGIS 10.3. Redlands, CA. [Google Scholar]
- Furr-Holden CDM, Milam AJ, Nesoff ED, Johnson RM, Fakunle DO, Jennings JM, Thorpe RJ Jr, 2016. Not in my back yard: a comparative analysis of crime around publicly funded drug treatment centers, liquor stores, convenience stores, and corner stores in one mid-Atlantic city. J Stud Alc Drugs, 77(1), 17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Généreux M, Bruneau J, Daniel M, 2010. Association between neighbourhood socioeconomic characteristics and high-risk injection behaviour amongst injection drug users living in inner and other city areas in Montréal, Canada. Int J Drug Pol, 21(1), 49–55. [DOI] [PubMed] [Google Scholar]
- Hembree C, Galea S, Ahern J, Tracy M, Piper TM, Miller J, … Tardiff KJ, 2005. The urban built environment and overdose mortality in New York City neighborhoods. Health Place, 11(2), 147–156. [DOI] [PubMed] [Google Scholar]
- Highsmith AR, & Erickson AT (2015). Segregation as splitting, segregation as joining: Schools, housing, and the many modes of Jim Crow. Am J Educ, 121(4), 563–595. [Google Scholar]
- Kirchner TR, Shiffman S, 2016. Spatio-temporal determinants of mental health and well-being: advances in geographically-explicit ecological momentary assessment (GEMA). Soc Psych Psychiat Epi, 51(9), 1211–1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolodny A, Courtwright DT, Hwang CS, Kreiner P, Eadie JL, Clark TW, Alexander GC, 2015. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Ann Rev Pub Health, 36, 559–574. [DOI] [PubMed] [Google Scholar]
- Kruger DJ, Reischl TM, Gee GC, 2007. Neighborhood social conditions mediate the association between physical deterioration and mental health. Am J Comm Psych, 40(3-4), 261–271. [DOI] [PubMed] [Google Scholar]
- Lee G, Endacott R, Flett K, & Bushnell R. (2006). Characteristics of patients who did not wait for treatment in the emergency department: a follow up survey. Accid Emerg Nurs, 14(1), 56–62. [DOI] [PubMed] [Google Scholar]
- Leshner AI, Mancher M, 2019. Committee on Medication-Assisted Treatment for Opioid Use Disorder; Board on Health Sciences Policy; Health and Medicine Division; National Academies of Sciences, Engineering, and Medicine Medications for Opioid Use Disorder Save Lives. Washington (DC): National Academies Press (US) Available from: https://www.ncbi.nlm.nih.gov/books/NBK538936/pdf/Bookshelf_NBK538936.pdf [PubMed] [Google Scholar]
- Macintyre S, 2007. Deprivation amplification revisited; or, is it always true that poorer places have poorer access to resources for healthy diets and physical activity? Int J Behav Nut Phys Act, 4(1), 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolis DJ, Hoffstad O, Nafash J, Leonard CE, Freeman CP, Hennessy S, & Wiebe DJ (2011). Location, location, location: geographic clustering of lower-extremity amputation among Medicare beneficiaries with diabetes. Diab Care, 34(11), 2363–2367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLafferty S, 2008. Placing substance abuse In Geography and Drug Addiction (pp. 1–16). Springer, Dordrecht. [Google Scholar]
- McLean K, 2016. “There's nothing here”: Deindustrialization as risk environment for overdose. Int J Drug Pol, 29, 19–26. [DOI] [PubMed] [Google Scholar]
- Mennis J, Harris PW, Obradovic Z, Izenman AJ, Grunwald HE, Lockwood B, 2011. The effect of neighborhood characteristics and spatial spillover on urban juvenile delinquency and recidivism. Prof Geog, 63(2), 174–192. [Google Scholar]
- Mennis J, Stahler GJ, Baron DA, 2012. Geographic barriers to community-based psychiatric treatment for drug-dependent patients. Annals Assoc Am Geog, 102(5), 1093–1103. [Google Scholar]
- Michigan Department of Licensing and Regulatory Affairs, 2017. Bureau of Health Systems License Listing Report for Behavioral Health Sites. Lansing, MI. [Google Scholar]
- Minnesota Population Center (2011) National Historical Geographic Information System: Version 2.0. Minneapolis, MN: University of Minnesota. [Google Scholar]
- New York Times, 2017. The Opioid Crisis is Getting Worse, Particularly for Black Americans. Retrieved from: https://www.nytimes.com/interactive/2017/12/22/upshot/opioid-deaths-are-spreading-rapidly-into-black-america.html.
- Palombi LC, LaRue A, Fierke KK, 2018. Facilitating community partnerships to reduce opioid overdose: An Engaged Department initiative. Res Soc Admin Pharm, doi: 10.1016/j.sapharm.2018.07.002. [DOI] [PubMed] [Google Scholar]
- Rocchi MB, Miotto P, & Preti A (2003). Distribution of deaths by unintentional illicit drug overdose in Italy based on periodicity over time, 1984–2000. Drug Alc Depend, 72(1), 23–31. [DOI] [PubMed] [Google Scholar]
- Rocchi M, Miotto P, & Preti A (2004). Seasonal variation in suicides and in deaths by unintentional illicit acute drug intoxications. Addic Bio, 9(3- 4), 255–263. [DOI] [PubMed] [Google Scholar]
- Rowe C, Santos GM, Vittinghoff E, Wheeler E, Davidson P, & Coffin PO (2016). Neighborhood-level and spatial characteristics associated with lay naloxone reversal events and opioid overdose deaths. J Urb Health, 93(1), 117–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd RA (2016). Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. MMWR. Morb Mort Week Rep, 65. [DOI] [PubMed] [Google Scholar]
- Sadler RC, & Highsmith AR (2016). Rethinking Tiebout: the contribution of political fragmentation and racial/economic segregation to the Flint water crisis. Environ Just, 9(5), 143–151. [Google Scholar]
- Sadler RC, LaChance J, Hanna-Attisha M, 2017. Social and Built Environmental Correlates of Predicted Blood Lead Levels in the Flint Water Crisis. Am J Pub Health, 107(5), 763–769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadler RC, & Lafreniere DJ (2017). Racist housing practices as a precursor to uneven neighborhood change in a post-industrial city. Hous Stud, 32(2), 186–208. [Google Scholar]
- Schiele H (2008). Location, location: the geography of industry clusters. J Bus Strat, 29(3), 29–36. [Google Scholar]
- Schroeder JR, Latkin CA, Hoover DR, Curry AD, Knowlton AR, & Celentano DD (2001). Illicit drug use in one's social network and in one's neighborhood predicts individual heroin and cocaine use. Annals Epi, 11(6), 389–394. [DOI] [PubMed] [Google Scholar]
- Schwartz RP, Gryczynski J, O'Grady KE, Sharfstein JM, Warren G, Olsen Y, Mitchell SG, Jaffe JH, 2013. Opioid agonist treatments and heroin overdose deaths in Baltimore, Maryland, 1995–2009. Am J Pub Health, 103(5):917–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stopka TJ, Amaravadi H, Kaplan AR, Hoh R, Bernson D, Chui KK, … Rose AJ, 2019. Opioid overdose deaths and potentially inappropriate opioid prescribing practices (PIP): a spatial epidemiological study. Int J Drug Pol, 68, 37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teixeira S, 2016. Beyond broken windows: Youth perspectives on housing abandonment and its impact on individual and community well-being. Child Indic Res, 9(3), 581–607. [Google Scholar]
- Tobler W (2004). On the first law of geography: A reply. Annals Assoc Am Geog, 94(2), 304–310. [Google Scholar]
- Weiner SG, Baker O, Poon SJ, Rodgers AF, Garner C, Nelson LS, & Schuur JD (2017). The effect of opioid prescribing guidelines on prescriptions by emergency physicians in Ohio. Annals Emerg Med, 70(6), 799–808. [DOI] [PubMed] [Google Scholar]
- Weiss L, McCoy K, Kluger M, Finkelstein R, 2004. Access to and use of health care: perceptions and experiences among people who use heroin and cocaine. Addic Res Theo, 12(2), 155–165. [Google Scholar]
- Williams CT, Latkin CA, 2007. Neighborhood socioeconomic status, personal network attributes, and use of heroin and cocaine. Am J Prev Med, 32(6), S203–S210. [DOI] [PMC free article] [PubMed] [Google Scholar]