Abstract
Background
HIV-related stigma among people living with HIV (PLHIV) is associated with worse health outcomes. We used longitudinal data from a multi-site cohort in South Africa to assess changes over time in stigma after HIV diagnosis and determine whether antiretroviral therapy (ART) initiation is associated with stigma reduction.
Methods
We administered the Internalized AIDS-Related Stigma Scale (IARSS, a six-item dichotomous scale questionnaire) at baseline, three months, and six months to newly diagnosed ART-eligible participants between 2014–2015. A confirmatory factor analysis indicated that the IARSS contained a four-item internalized stigma factor (α=0.80) and a two-item disclosure concerns factor (α=0.75). We fitted multiple logistic regression models specifying internalized stigma/disclosure concerns at six months as the outcome and ART initiation as the predictor of interest.
Results
Of the 500 participants (187 men and 313 women) enrolled, 308 (62%) initiated ART. Internalized stigma declined among people entering care (mean score, 1.0 to 0.7, p<0.01); however, disclosure concerns remained unchanged (percentage endorsing either disclosure concern item, 78% to 77%, p=0.23). These findings were similar between ART initiators and non-initiators. We estimated a statistically significant positive association between ART initiation and disclosure concerns at six months (OR=1.88; 95% CI, 1.20–2.94) but not between ART initiation and internalized stigma at six months (OR=1.15; 95% CI, 0.75–1.78).
Conclusions
Among ART-eligible South African PLHIV entering into HIV care, internalized stigma modestly declined over time but disclosure concerns persisted. PLHIV who initiated ART were more likely to have persistent disclosure concerns over time as compared with those who did not start ART.
Keywords: Stigma, internalized stigma, anticipated stigma, disclosure, South Africa
Introduction
HIV-related stigma has been recognized as a critical barrier to the success of HIV prevention and treatment efforts worldwide (Grossman & Stangl, 2013; UNAIDS, 2012). People living with HIV (PLHIV) may encounter multiple dimensions of HIV-related stigma, including internalized, enacted, and anticipated stigma (Earnshaw, Smith, Chaudoir, Amico, & Copenhaver, 2013). Internalized stigma results when PLHIV accept prevailing negative stereotypes and prejudice toward PLHIV as valid and apply these beliefs and feelings to themselves (Earnshaw et al., 2013; Link, Cullen, Struening, Shrout, & Dohrenwend, 1989). Enacted stigma involves experiences of negative treatment, including discrimination, stereotyping, and prejudice, at the hands of others in the past or the present (Earnshaw et al., 2013; Scambler & Hopkins, 1986). In addition to experiencing enactments of stigma, PLHIV may also expect negative treatment from others in the future, a phenomenon known as anticipated stigma (Link, Cullen, Frank, & Wozniak, 1987).
Among PLHIV, internalized stigma has been associated with worse mental health (Simbayi et al., 2007; Tsai et al., 2012), decreased adherence to antiretroviral therapy (ART) (Boyer et al., 2011; Katz et al., 2013), and reduced likelihood of serostatus disclosure (Norman, Chopra, & Kadiyala, 2007; Tsai, Bangsberg, Kegeles, et al., 2013c). Although there may be a bidirectional or cyclical relationship between internalized stigma and ART initiation (Earnshaw et al., 2018), the nature of this relationship is unclear. While internalized stigma has been associated with reduced likelihood of ART initiation (Logie et al., 2018), longitudinal studies conducted in low- and middle-income countries (LMICs) have yielded conflicting results about the extent to which taking ART is associated with changes over time in internalized stigma among PLHIV (Makoae et al., 2009; Tsai, Bangsberg, Bwana, et al., 2013b). It has been theorized that engagement in HIV care and ART initiation may attenuate stigma among PLHIV through ART-related counseling and improvements in physical health that reduce the extent to which PLHIV internalize stigmatizing beliefs (Castro & Farmer, 2005; Tsai, Bangsberg, Bwana, et al., 2013b) and restore or maintain their economic viability and social connectedness (Campbell et al., 2011; Venkataramani et al., 2014). Most of the evidence in support of this hypothesis comes from qualitative studies, including from Haiti (Castro & Farmer, 2005) and multiple countries in sub-Saharan Africa (Campbell et al., 2011; Tsai, Bangsberg, & Weiser, 2013a; Zuch & Lurie, 2012). Moreover, extensive pre-ART counseling has historically been the norm in LMICs, with countries such as South Africa often requiring up to six visits prior to ART initiation (Maughan-Brown et al., 2018). These ART preparation activities, aimed at improving long-term adherence (Myer, Zulliger, & Pienaar, 2012), could also plausibly counter internalized stigma among PLHIV. Conversely, others have suggested that ART may worsen internalized stigma because of the widespread belief that one only takes ART when one is very sick (Makoae et al., 2009; Roura et al., 2009). For PLHIV who harbor this belief, initiating ART may be perceived as an acknowledgement of poor health and potentially one’s own mortality (Katz et al., 2015).
Similarly, the impact of ART initiation on anticipated stigma among PLHIV remains unclear. The consistent behaviors required for successful ART initiation may make it more difficult for PLHIV to hide their serostatus, thus increasing their perceived risk of being subjected to stigma (Makoae et al., 2009). Conversely, PLHIV may be motivated to start ART to stay healthy and thus avoid involuntary serostatus disclosure resulting from visibly apparent HIV-related wasting and opportunistic infections (van Loggerenberg et al., 2015).
Whether the effect of ART initiation on these dimensions of stigma differs between men and women is also largely unknown. Previous studies have suggested differences in levels of stigma experienced by men and women in sub-Saharan Africa (Chan, Tsai, & Siedner, 2015; Mugoya & Ernst, 2014) and in South Africa particularly (Sorsdahl, Mall, Stein, & Joska, 2011). In a cross-country analysis of 18 countries in sub-Saharan Africa, women in the general population were more likely to hold stigmatizing attitudes compared to men (Chan et al., 2015). This finding suggests that women may be more likely than men to internalize stigma after HIV diagnosis, in light of recent studies indicating that prejudice before HIV/sexually transmitted infection (STI) diagnosis (Eaton et al., 2018) and perceived community stigma (Turan et al., 2017) are associated with internalized stigma after HIV/STI diagnosis. Women living with HIV may also be more likely to hold disclosure concerns, given the particularly dangerous consequences of disclosure faced by women, including violence, shaming, and abandonment at the hands of partners and family members (Evangeli & Wroe, 2017; Maman, Groves, McNaughton Reyes, & Moodley, 2016; Medley, Garcia-Moreno, McGill, & Maman, 2004; Monteiro, Villela, Soares, Pinho, & Fraga, 2018). Accordingly, women may be more likely to anticipate stigma, as disclosure concerns reflect the expectation of rejection or discrimination were one’s serostatus revealed to others (Gilbert & Walker, 2010; Olley, Ogunde, Oso, & Ishola, 2016).
Understanding the association of ART with multiple dimensions of stigma is important for policymakers, as a finding of persistent stigma among PLHIV in HIV care would provide an impetus for investment in anti-stigma interventions. To help answer this question, we used longitudinal data from a sample of PLHIV in South Africa, where a recent nationwide study revealed high levels of internalized, anticipated, and enacted stigma among PLHIV (Simbayi et al., 2016). We assessed changes over time in multiple dimensions of HIV-related stigma among a sample of predominantly Black, newly diagnosed, and ART-eligible South Africans. We also sought to understand the extent to which ART initiation is associated with changes in these dimensions of stigma and whether the association between ART initiation and change in stigma differs by sex.
Methods
Study design
Data for this analysis were drawn from a study that was conducted at three sites in two townships in South Africa, the Zazi Testing Center and a Ministry of Health (MOH) clinic in Soweto and an MOH testing center in Gugulethu (outside of Cape Town). Both townships are densely populated urban areas with an overall HIV prevalence of approximately 20%. People undergoing HIV testing and counseling were given their HIV results, and if positive, had blood drawn for a CD4+ count and asked to return in a week for CD4+ count results. Patients receiving CD4+ count results who were eligible for ART were referred to trained counselors or social workers to discuss ART initiation.
We sequentially recruited and enrolled 500 ART-eligible adults (≥ 18 years old) between July 2014 and July 2015, as they received their CD4+ count results. ART eligibility was based on South African guidelines, which changed over the duration of the study (CD4+ ≤350 cells/mm3 before Jan 1, 2015, and CD4+ ≤500 cells/mm3 after Jan 1, 2015). We excluded children and pregnant women, as they qualified for intensive adherence support under South African guidelines. Ethical approval for all study procedures was obtained from the Human Subjects Committees at Partners Healthcare, the University of Witwatersrand Ethics Committee, the Gauteng Department of Health, and the University of Cape Town Ethics Committee. All participants provided written informed consent. Study data were collected and managed using a secure, web-based, Research Electronic Data Capture (REDCap) tool hosted at Partners Healthcare (Harris et al., 2009).
Measures
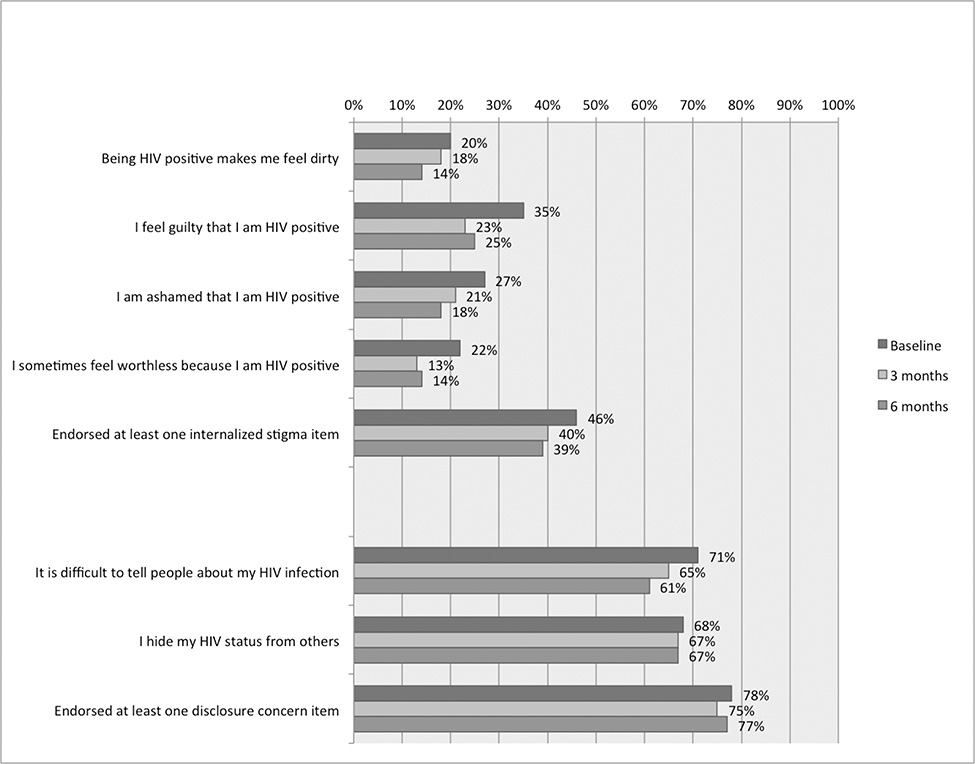
At baseline, month three, and month six, trained multilingual interviewers administered to study participants a questionnaire that measured clinical, structural and psychosocial factors, including the six-item Internalized AIDS-Related Stigma Scale (IARSS) (Kalichman et al., 2009). The IARSS collects responses on a binary scale (agree/disagree) and scores represent the sum of endorsed items. Four of the six items in the IARSS relate unequivocally to internalized stigma, including items on feelings of shame and/or self-hatred, whereas two items relate more closely to disclosure concerns (Figure 1). We regarded disclosure concerns as a correlate of anticipated stigma. There is recent evidence for a two-factor structure for the IARSS items, including a four-item internalized stigma factor and a two-item disclosure concerns factor, among PLHIV in India (Chan et al., 2018). Therefore, we conducted a confirmatory factor analysis on the IARSS items using a two-factor structure. The Chi-sq statistic had a p-value of <0.01 with a root mean square error of approximation of 0.06 and a Bentler’s comparative fit index of 0.98, indicating good model fit with the two-factor structure. At baseline, the estimated scale reliability coefficient for the internalized stigma and disclosure concerns sub-scales was 0.80 and 0.75, respectively.
Figure 1:
Internalized stigma and disclosure concerns among participants at baseline, 3 months, and 6 months in care
The primary exposure of interest was ART initiation within six months of HIV testing. This variable was ascertained by matching participants’ name and date of birth to routine laboratory data collected by the National Health Laboratory Service (NHLS), which provides services to all public-sector facilities in South Africa. ART initiation was imputed based on a measure of creatinine, which is performed prior to initiation of standard first-line ART in South Africa. ART workup blood testing as recorded in NHLS has been previously validated as an accurate measure of ART initiation among PLHIV who are in care in the South African public sector (Maskew et al., 2017). We also collected baseline socio-demographic variables (age, sex, educational attainment, marital status, and employment status) and CD4+ cell count.
Statistical analysis
We used descriptive statistics to characterize the sample and levels of stigma at baseline, three months, and six months, including McNemar’s tests for the binary stigma outcomes and paired t-tests for the stigma scales. To help understand to what extent changes over time in stigma were related to non-random attrition of study participants, we fitted a logistic regression model with attrition by six months as the outcome variable and baseline disclosure concerns score or internalized stigma score as the primary exposure of interest, adjusted for sociodemographic characteristics, CD4+ count, and study site (Soweto vs. Gugulethu). We then fitted logistic regression models to the data with ART initiation as the primary exposure of interest and disclosure concerns / internalized stigma (=1 if study participant endorsed either disclosure concerns item or any of the four internalized stigma items) at six months as the outcome variable, adjusted for sociodemographic characteristics, CD4+ count, study site, and disclosure concerns / internalized stigma at baseline. A statistically significant regression coefficient was considered evidence that an association existed between ART initiation and disclosure concerns/internalized stigma at six-month follow-up. As a sensitivity analysis, we fitted binomial regression models using the disclosure concerns score (0–2) or internalized stigma score (0–4) (expressed as R of N, where R is the participant’s score and N is the maximum possible score) as the outcome variable (adjusted for sociodemographic characteristics, CD4+ count, study site and disclosure concerns / internalized stigma score at baseline). Finally, we fitted all models with a product term to test for an interaction between sex and ART initiation. All analyses were performed using Stata software (Version 15.0, StataCorp, College Station, TX, USA).
Results
We enrolled 500 participants (200 in Soweto and 300 in Gugulethu) into the study (Table). A total of 308 (62%) participants initiated ART within six months; nine (2%) participants died before accessing treatment. We located and verified clinical data for 473 (95%) of the participants in this cohort through NHLS. Three hundred and eighty-three (81%) participants had complete follow-up survey data through six months. At baseline (i.e., one week after testing, at the determination of ART eligibility), disclosure concerns were particularly high, with 78% endorsing at least one disclosure concern item (Figure 1). Internalized stigma at baseline was also common, with 46% endorsing at least one internalized stigma item, including 35% who agreed with the statement “I feel guilty that I am HIV positive.”
Table:
Baseline characteristics of study participants (n=500)
| Median (interquartile range) or no. (%) | |
|---|---|
| Site | |
| Soweto | 200 (40%) |
| Gugulethu | 300 (60%) |
| Age, years | 35 (29–42) |
| Sex | |
| Male | 187 (37%) |
| Female | 313 (63%) |
| Race | |
| Black | 495 (99%) |
| White | 2 (0.4%) |
| Coloured | 3 (0.6%) |
| No high school education | 378 (76%) |
| Married or cohabiting | 112 (22%) |
| Currently employed | 239 (48%) |
| Current alcohol use | 262 (53%) |
| Current illicit drug use | 15 (3%) |
| CD4+ count, cells / mm3 | 242 (135–348) |
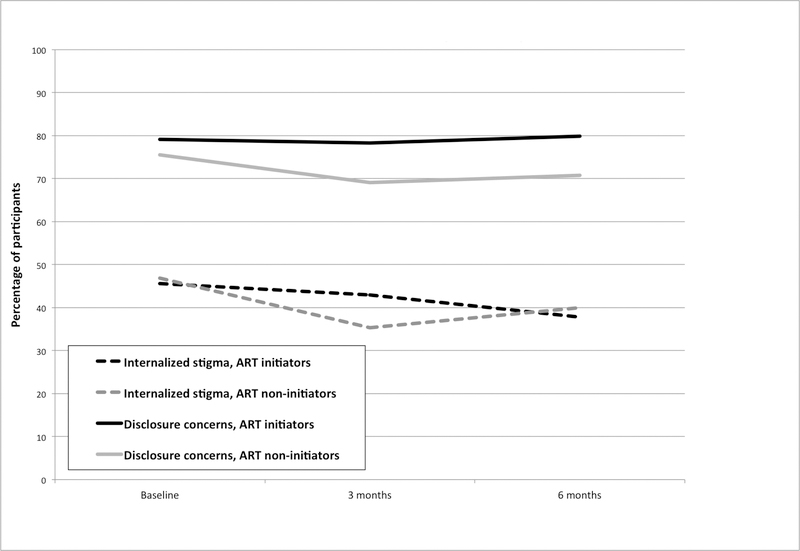
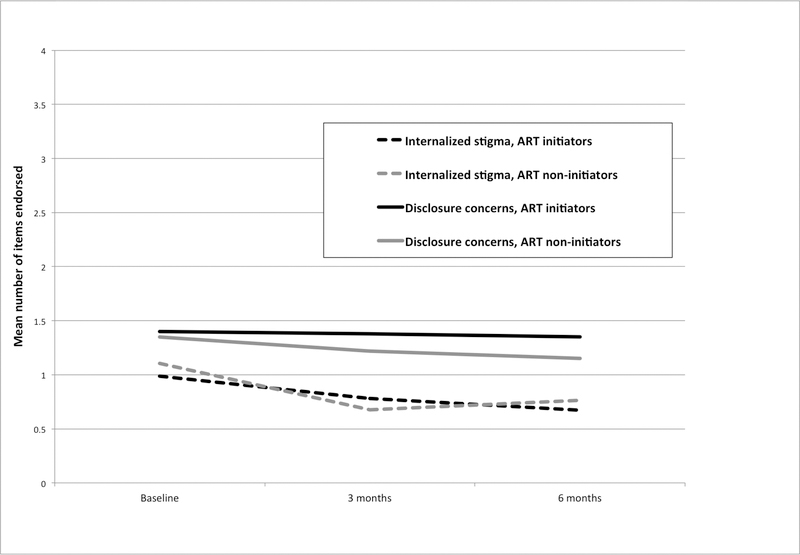
Internalized stigma declined over six months among participants (mean score, 1.0 to 0.7, p<0.01), including ART non-initiators (1.1 to 0.8, p<0.01) and ART initiators (1.0 to 0.7, p<0.01). There were declines in the percentages agreeing with each of the four internalized stigma items. Nevertheless, 39% of participants, including 40% of ART non-initiators and 38% of ART initiators, continued to endorse at least one internalized stigma item after six months (Figures 2 and 3). Disclosure concerns did not significantly decrease over six months among participants (percentage endorsing either disclosure concern item, 78% to 77%, p=0.23), including both ART non-initiators (76% to 71%, p=0.07) and ART initiators (79% to 80%, p=0.90). Findings appeared similar between men and women (results available in Supplementary Digital Content 1). Using a logistic regression model adjusted for sociodemographic characteristics, CD4+ count, and study site, we did not find a statistically significant association between baseline disclosure concerns (Odds Ratio [OR]=0.91, 95% Confidence Interval [CI], 0.71–1.18) or internalized stigma (OR=0.93; 95% CI, 0.79–1.10) with attrition of study participants by six months.
Figure 2:
Percentage endorsing internalized stigma and disclosure concerns among ART initiators and non-initiators in South Africa at baseline, 3 months, and 6 months in care
Figure 3:
Mean internalized stigma and disclosure concerns scores among ART initiators and non-initiators in South Africa at baseline, 3 months, and 6 months in care
Using logistic regression models adjusted for sociodemographic variables, baseline CD4+ count, study site, and baseline disclosure concerns / internalized stigma, we estimated a statistically significant positive association between ART initiation and disclosure concerns at six months (OR=1.88; 95% CI, 1.20–2.94) but not between ART initiation and internalized stigma at six months (OR=1.15; 95% CI, 0.75–1.78). In the models including a product term testing for an interaction between sex and ART initiation, the estimated regression coefficient for the product term was not statistically significant for either the association between ART initiation and disclosure concerns (p=0.40) or the association between ART initiation and internalized stigma (p=0.90).
The sensitivity analysis using binomial regression models for the disclosure concerns score (0–2) / internalized stigma score (0–4) as the outcome variable yielded similar results. We estimated a statistically significant positive association between ART initiation and disclosure concerns score at six months (adjusted b=0.44; 95% CI, 0.11–0.76) but not between ART initiation and internalized stigma score at six months (adjusted b= −0.05; 95% CI, −0.34 to 0.24). In the models including a product term testing for an interaction between gender and ART initiation, the estimated regression coefficient for the product term was again not statistically significant for either the association between ART initiation and disclosure concerns (p=0.50) or the association between ART initiation and internalized stigma (p=0.15). The regression estimates for all models used in this analysis are available in Supplementary Digital Content 2.
Discussion
In this analysis of prospective data collected from a multi-site cohort of predominantly Black South Africans eligible for ART, we found that internalized stigma was commonly endorsed at the time of ART eligibility determination and declined modestly over time among both ART non-initiators and initiators. Internalized stigma may naturally decrease over time as people have time to process, adjust to their diagnosis, and acquire social support. Further, the education, counseling, and support experienced by PLHIV accessing HIV care (regardless of ART initiation) may diminish internalized stigma, however slightly. It is worth noting that while internalized stigma declined among both ART initiators and non-initiators, it did so only modestly, with 39% of participants endorsing at least one internalized stigma item at six-month follow-up. This indicates that although engagement in HIV care may be mildly beneficial in countering internalized stigma, it is unlikely to be a panacea (Treves-Kagan et al., 2016).
Previous evidence suggests that ART may reduce internalized stigma over time as PLHIV experience improvements in HIV symptom burden and physical and psychosocial well-being (Tsai, Bangsberg, Bwana, et al., 2013b). Furthermore, at the time this study was conducted, PLHIV in South Africa frequently underwent multiple visits prior to ART initiation to enhance readiness for treatment (Maughan-Brown et al., 2018), a process that could also be expected to reduce internalized stigma. Unfortunately, our findings suggest that ART initiation is not associated with meaningful reductions in internalized stigma beyond usual HIV care, at least within the first six months after diagnosis. Given the striking rates of internalized stigma at the time of HIV diagnosis (46% of respondents endorsing at least one internalized stigma item) and the deleterious effects of internalized stigma on HIV-related outcomes (Boyer et al., 2011; Katz et al., 2013; Norman et al., 2007; Tsai, Bangsberg, Kegeles, et al., 2013c), further efforts to attenuate internalized stigma at the time of HIV diagnosis and during the first six months of care may be warranted. Such efforts could include initiatives to reduce stigmatizing attitudes in the general population such as educational campaigns or contact interventions (Chan & Tsai, 2017; Stangl, Lloyd, Brady, Holland, & Baral, 2013) or initiatives to help PLHIV build skills to cope with a stigmatizing environment such as support groups and patient empowerment interventions (Bogart et al., 2018; Roy et al., 2016). Another possible implication of our findings is that the practice of multiple counseling sessions prior to ART initiation may not necessarily lessen internalized stigma; thus, the current practice of fast-tracked ART initiation is unlikely to be disadvantageous in this regard.
While internalized stigma declined modestly among PLHIV in the first six months after HIV diagnosis, we found that disclosure concerns persisted. ART initiation may do little to counter disclosure concerns; indeed, the consistent behaviors required to successfully initiate ART may make it more difficult for PLHIV to hide their serostatus. Our findings of persistent disclosure concerns among PLHIV in care are important for policymakers, as non-disclosure has been associated with negative outcomes including poor mental health and reduced quality of life (Chandra, Deepthivarma, Jairam, & Thomas, 2003; Patel et al., 2012), loss to care (Akilimali et al., 2017), virological failure (Izudi, Alioni, Kerukadho, & Ndungutse, 2016; Ramadhani et al., 2007), and risky sexual behaviors (Booysen, Wouters, de Walque, & Over, 2017; Wong et al., 2009).
Previous studies have demonstrated differences in stigma experiences between men and women in LMICs; in particular, women living with HIV may face uniquely dangerous consequences of disclosure, including intimate partner violence and shaming and abandonment by partners or families (Evangeli & Wroe, 2017; Maman et al., 2016; Medley et al., 2004; Monteiro et al., 2018). However, the prevalence and trajectories of disclosure concerns and internalized stigma appeared similar between men and women in our cohort. Although women appear to be more likely than men in the general population of sub-Saharan Africa to hold stigmatizing attitudes (Chan et al., 2015), our findings indicate that this may not necessarily translate into women being more likely than men to internalize stigma after HIV diagnosis. Moreover, we did not find that the association between ART initiation and change in stigma differs significantly by sex. Our results suggest that interventions to counter stigma and to promote serostatus disclosure among PLHIV should target both women and men.
Our study has several limitations. First, our results may have been biased by the substantial rate of loss to follow-up, which affected about one-quarter of the enrolled participants. However, concern for non-random attrition of participants is mitigated by the lack of a statistically significant association between disclosure concerns or internalized stigma at baseline and attrition by six months. Moreover, any differential loss to follow-up would have likely biased our estimates of persisting stigma toward the null (because persistent stigma may have caused study participants to select out of the study, further enriching the sample for participants with lower levels of stigma)—buttressing our conclusion that stigma remains persistently high among PLHIV who access HIV care. Second, our primary exposure of interest, ART initiation, was obtained through a national database that relies upon clinician input into a registry. Despite the possibility of inaccuracies in this process, this method of imputing ART initiation has been previously validated among PLHIV in care in the public sector of South Africa (Maskew et al., 2017). Finally, the IARSS disclosure concerns items may not precisely capture the concept of fear of disclosure that may be deleterious to HIV-related outcomes. PLHIV who “hide [their] HIV status from others” or find it “difficult to tell people about [their] HIV infection” may have understandably decided against public disclosure, while garnering social support from select family and friends to whom they have disclosed. However, we feel that the use of the terms “hide” and “difficult” grants these items a negative connotation that likely reflects fears of rejection and exclusion that go beyond “normal” privacy concerns.
In conclusion, among a cohort of ART-eligible, predominantly Black South Africans recently diagnosed with HIV, internalized stigma modestly declined over time while disclosure concerns persisted, with ART initiators more likely to have persistent disclosure concerns over time compared with non-initiators. Policymakers should prioritize interventions to promote safe disclosure of serostatus among PLHIV, as well as consider redoubling efforts to counter internalized stigma among PLHIV.
Supplementary Material
Acknowledgements
This study would not have been possible with the dedication of the study participants in Soweto and Gugulethu.
Conflicts of Interest and Source of Funding: No authors have any conflicts of interest. The authors acknowledge the following sources of support: NIH K23MH110338 (Chan), P30MH058107 (Bogart), K01DA042881 (Earnshaw), K23MH097667 (Katz); National Research Foundation, South Africa, Research Career Advancement Fellowship (Maughan-Brown).
References
- Akilimali PZ, Musumari PM, Kashala-Abotnes E, Kayembe PK, Lepira FB, Mutombo PB, et al. (2017). Disclosure of HIV status and its impact on the loss in the follow-up of HIV-infected patients on potent anti-retroviral therapy programs in a (post-) conflict setting: A retrospective cohort study from Goma, Democratic Republic of Congo. PloS One, 12(2), e0171407 10.1371/journal.pone.0171407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogart LM, Dale SK, Daffin GK, Patel KN, Klein DJ, Mayer KH, & Pantalone DW (2018). Pilot intervention for discrimination-related coping among HIV-positive Black sexual minority men. Cultural Diversity & Ethnic Minority Psychology, 24(4), 541–551. 10.1037/cdp0000205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booysen FLR, Wouters E, de Walque D, & Over M (2017). Mutual HIV status disclosure is associated with consistent condom use in public sector ART clients in Free State province, South Africa: a short report. AIDS Care, 29(11), 1386–1390. 10.1080/09540121.2017.1290210 [DOI] [PubMed] [Google Scholar]
- Boyer S, Clerc I, Bonono C-R, Marcellin F, Bilé P-C, & Ventelou B (2011). Non-adherence to antiretroviral treatment and unplanned treatment interruption among people living with HIV/AIDS in Cameroon: Individual and healthcare supply-related factors. Social Science & Medicine, 72(8), 1383–1392. 10.1016/j.socscimed.2011.02.030 [DOI] [PubMed] [Google Scholar]
- Campbell C, Skovdal M, Madanhire C, Mugurungi O, Gregson S, & Nyamukapa C (2011). “We, the AIDS people. . .”: how antiretroviral therapy enables Zimbabweans living with HIV/AIDS to cope with stigma. American Journal of Public Health, 101(6), 1004–1010. 10.2105/AJPH.2010.202838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro A, & Farmer P (2005). Understanding and addressing AIDS-related stigma: from anthropological theory to clinical practice in Haiti. American Journal of Public Health, 95(1), 53–59. 10.2105/AJPH.2003.028563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan BT, & Tsai AC (2017). Personal contact with HIV-positive persons is associated with reduced HIV-related stigma: cross-sectional analysis of general population surveys from 26 countries in sub-Saharan Africa. Journal of the International AIDS Society, 19(1). 10.7448/IAS.20.1.00000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan BT, Pradeep A, Chandrasekaran E, Prasad L, Murugesan V, Kumarasamy N, et al. (2018). Reliability, validity, and factor structure of the Internalized AIDS-Related Stigma Scale in southern India. Journal of the International Association of Physicians in AIDS Care (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan BT, Tsai AC, & Siedner MJ (2015). HIV Treatment Scale-Up and HIV-Related Stigma in Sub-Saharan Africa: A Longitudinal Cross-Country Analysis. American Journal of Public Health, 105(8), 1581–1587. 10.2105/AJPH.2015.302716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandra PS, Deepthivarma S, Jairam KR, & Thomas T (2003). Relationship of psychological morbidity and quality of life to illness-related disclosure among HIV-infected persons. Journal of Psychosomatic Research, 54(3), 199–203. 10.1016/S0022-3999(02)00567-6 [DOI] [PubMed] [Google Scholar]
- Earnshaw VA, Bogart LM, Laurenceau J-P, Chan BT, Maughan-Brown B, Dietrich JJ, et al. (2018). Internalized HIV stigma, ART initiation and HIV-1 RNA suppression in South Africa: exploring avoidant coping as a longitudinal mediator. Journal of the International AIDS Society, 21, e25198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, & Copenhaver MM (2013). HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS and Behavior, 17(5), 1785–1795. 10.1007/s10461-013-0437-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton LA, Earnshaw VA, Maksut JL, Thorson KR, Watson RJ, & Bauermeister JA (2018). Experiences of stigma and health care engagement among Black MSM newly diagnosed with HIV/STI. Journal of Behavioral Medicine, 41(4), 458–466. 10.1007/s10865-018-9922-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evangeli M, & Wroe AL (2017). HIV Disclosure Anxiety: A Systematic Review and Theoretical Synthesis. AIDS and Behavior, 21(1), 1–11. 10.1007/s10461-016-1453-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert L, & Walker L (2010). “My biggest fear was that people would reject me once they knew my status...”: stigma as experienced by patients in an HIV/AIDS clinic in Johannesburg, South Africa. Health & Social Care in the Community, 18(2), 139–146. 10.1111/j.1365-2524.2009.00881.x [DOI] [PubMed] [Google Scholar]
- Grossman CI, & Stangl AL (2013). Editorial: Global action to reduce HIV stigma and discrimination. Journal of the International AIDS Society, 16(3 Suppl 2), 18881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izudi J, Alioni S, Kerukadho E, & Ndungutse D (2016). Virological failure reduced with HIV-serostatus disclosure, extra baseline weight and rising CD4 cells among HIV-positive adults in Northwestern Uganda. BMC Infect Dis, 16(1), 614 10.1186/s12879-016-1952-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Cloete A, Mthembu PP, Mkhonta RN, & Ginindza T (2009). Measuring AIDS stigmas in people living with HIV/AIDS: the Internalized AIDS-Related Stigma Scale. AIDS Care, 21(1), 87–93. 10.1080/09540120802032627 [DOI] [PubMed] [Google Scholar]
- Katz IT, Dietrich JJ, Tshabalala G, Essien T, Rough K, Wright AA, et al. (2015). Understanding treatment refusal among adults presenting for HIV-testing in Soweto, South Africa: a qualitative study. AIDS and Behavior, 19(4), 704–714. 10.1007/s10461-014-0920-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, & Tsai AC (2013). Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. Journal of the International AIDS Society, 16(3 Suppl 2), 18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Cullen FT, Frank J, & Wozniak JF (1987). The social rejection of former mental patients: understanding why labels matter. American Journal of Sociology, 92, 1461–1500. [Google Scholar]
- Link BG, Cullen FT, Struening E, Shrout PE, & Dohrenwend BP (1989). A Modified Labeling Theory Approach to Mental Disorders: An Empirical Assessment. American Sociological Review, 54(3), 400 10.2307/2095613 [DOI] [Google Scholar]
- Logie CH, Lacombe-Duncan A, Wang Y, Kaida A, Webster K, de Pokomandy A, et al. (2018). Pathways From HIV-Related Stigma to Antiretroviral Therapy Measures in the HIV Care Cascade for Women Living With HIV in Canada. Journal of Acquired Immune Deficiency Syndromes, 77(2), 144–153. 10.1097/QAI.0000000000001589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makoae LN, Portillo CJ, Uys LR, Dlamini PS, Greeff M, Chirwa M, et al. (2009). The impact of taking or not taking ARVs on HIV stigma as reported by persons living with HIV infection in five African countries. AIDS Care, 21(11), 1357–1362. 10.1080/09540120902862576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maman S, Groves AK, McNaughton Reyes HL, & Moodley D (2016). Diagnosis and disclosure of HIV status: Implications for women’s risk of physical partner violence in the postpartum period. Journal of Acquired Immune Deficiency Syndromes, 72(5), 546–551. 10.1097/QAI.0000000000001012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maskew M, Bor J, Hendrickson C, MacLeod W, Bärnighausen T, Pillay D, et al. (2017). Imputing HIV treatment start dates from routine laboratory data in South Africa: a validation study. BMC Health Services Research, 17(1), 41 10.1186/s12913-016-1940-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maughan-Brown B, Kuo C, Galárraga O, Smith P, Lurie MN, Bekker L-G, & Harrison A (2018). Stumbling Blocks at the Clinic: Experiences of Seeking HIV Treatment and Care in South Africa. AIDS and Behavior, 22(3), 765–773. 10.1007/s10461-017-1877-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medley A, Garcia-Moreno C, McGill S, & Maman S (2004). Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: implications for prevention of mother-to-child transmission programmes. Bulletin of the World Health Organization, 82(4), 299–307. [PMC free article] [PubMed] [Google Scholar]
- Monteiro S, Villela W, Soares P, Pinho A, & Fraga L (2018). “Protective” silence surrounding AIDS: Reasons and implications of non-disclosure among pregnant women living with HIV in Rio de Janeiro (Brazil). Global Public Health, 13(1), 51–64. 10.1080/17441692.2016.1211163 [DOI] [PubMed] [Google Scholar]
- Mugoya GCT, & Ernst K (2014). Gender differences in HIV-related stigma in Kenya. AIDS Care, 26(2), 206–213. 10.1080/09540121.2013.808733 [DOI] [PubMed] [Google Scholar]
- Myer L, Zulliger R, & Pienaar D (2012). Diversity of patient preparation activities before initiation of antiretroviral therapy in Cape Town, South Africa. Tropical Medicine & International Health, 17(8), 972–977. 10.1111/j.1365-3156.2012.03033.x [DOI] [PubMed] [Google Scholar]
- Norman A, Chopra M, & Kadiyala S (2007). Factors related to HIV disclosure in 2 South African communities. American Journal of Public Health, 97(10), 1775–1781. 10.2105/AJPH.2005.082511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olley BO, Ogunde MJ, Oso PO, & Ishola A (2016). HIV-related stigma and self-disclosure: the mediating and moderating role of anticipated discrimination among people living with HIV/AIDS in Akure Nigeria. AIDS Care, 28(6), 726–730. 10.1080/09540121.2016.1140894 [DOI] [PubMed] [Google Scholar]
- Patel R, Ratner J, Gore-Felton C, Kadzirange G, Woelk G, & Katzenstein D (2012). HIV disclosure patterns, predictors, and psychosocial correlates among HIV positive women in Zimbabwe. AIDS Care, 24(3), 358–368. 10.1080/09540121.2011.608786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramadhani HO, Thielman NM, Landman KZ, Ndosi EM, Gao F, Kirchherr JL, et al. (2007). Predictors of incomplete adherence, virologic failure, and antiviral drug resistance among HIV-infected adults receiving antiretroviral therapy in Tanzania. Clinical Infectious Diseases, 45(11), 1492–1498. 10.1086/522991 [DOI] [PubMed] [Google Scholar]
- Roura M, Urassa M, Busza J, Mbata D, Wringe A, & Zaba B (2009). Scaling up stigma? The effects of antiretroviral roll-out on stigma and HIV testing. Early evidence from rural Tanzania. Sexually Transmitted Infections, 85(4), 308–312. 10.1136/sti.2008.033183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy M, Czaicki N, Holmes C, Chavan S, Tsitsi A, Odeny T, et al. (2016). Understanding Sustained Retention in HIV/AIDS Care and Treatment: a Synthetic Review. Current HIV/AIDS Reports, 13(3), 177–185. 10.1007/s11904-016-0317-9 [DOI] [PubMed] [Google Scholar]
- Scambler G, & Hopkins A (1986). Being epileptic: coming to terms with stigma. Sociology of Health and Illness, 8(1), 26–43. [Google Scholar]
- Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, & Mqeketo A (2007). Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Social Science & Medicine, 64(9), 1823–1831. 10.1016/j.socscimed.2007.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simbayi LC, Zuma K, Cloete A, Jooste S, Zimela S, Blose S, et al. (2016). The People Living With HIV Stigma Index: South Africa 2014 Summary Report. Retrieved from http://www.stigmaindex.org/sites/default/files/reports/Summary-Booklet-on-Stigma-Index-Survey%20South%20Africa.pdf
- Sorsdahl KR, Mall S, Stein DJ, & Joska JA (2011). The prevalence and predictors of stigma amongst people living with HIV/AIDS in the Western Province. AIDS Care, 23(6), 680–685. 10.1080/09540121.2010.525621 [DOI] [PubMed] [Google Scholar]
- Stangl AL, Lloyd JK, Brady LM, Holland CE, & Baral S (2013). A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? Journal of the International AIDS Society, 16(3 Suppl 2), 18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treves-Kagan S, Steward WT, Ntswane L, Haller R, Gilvydis JM, Gulati H, et al. (2016). Why increasing availability of ART is not enough: a rapid, community-based study on how HIV-related stigma impacts engagement to care in rural South Africa. BMC Public Health, 16(1), 87 10.1186/s12889-016-2753-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Bangsberg DR, & Weiser SD (2013a). Harnessing poverty alleviation to reduce the stigma of HIV in Sub-Saharan Africa. PLoS Medicine, 10(11), e1001557 10.1371/journal.pmed.1001557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Bangsberg DR, Bwana M, Haberer JE, Frongillo EA, Muzoora C, et al. (2013b). How does antiretroviral treatment attenuate the stigma of HIV? Evidence from a cohort study in rural Uganda. AIDS and Behavior, 17(8), 2725–2731. 10.1007/s10461-013-0503-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Bangsberg DR, Frongillo EA, Hunt PW, Muzoora C, Martin JN, & Weiser SD (2012). Food insecurity, depression and the modifying role of social support among people living with HIV/AIDS in rural Uganda. Social Science & Medicine, 74(12), 2012–2019. 10.1016/j.socscimed.2012.02.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Bangsberg DR, Kegeles SM, Katz IT, Haberer JE, Muzoora C, et al. (2013c). Internalized stigma, social distance, and disclosure of HIV seropositivity in rural Uganda. Annals of Behavioral Medicine, 46(3), 285–294. 10.1007/s12160-013-9514-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan B, Budhwani H, Fazeli PL, Browning WR, Raper JL, Mugavero MJ, & Turan JM (2017). How Does Stigma Affect People Living with HIV? The Mediating Roles of Internalized and Anticipated HIV Stigma in the Effects of Perceived Community Stigma on Health and Psychosocial Outcomes. AIDS and Behavior, 21(1), 283–291. 10.1007/s10461-016-1451-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. (2012). Key programmes to reduce stigma and discrimination and increase access to justice in national HIV responses. Retrieved from http://www.unaids.org/en/media/unaids/contentassets/documents/document/2012/Key_Human_Rights_Programmes_en_May2012.pdf
- van Loggerenberg F, Gray D, Gengiah S, Kunene P, Gengiah TN, Naidoo K, et al. (2015). A qualitative study of patient motivation to adhere to combination antiretroviral therapy in South Africa. AIDS Patient Care and STDs, 29(5), 299–306. 10.1089/apc.2014.0293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venkataramani AS, Thirumurthy H, Haberer JE, Boum Y, Siedner MJ, Kembabazi A, et al. (2014). CD4+ cell count at antiretroviral therapy initiation and economic restoration in rural Uganda. AIDS, 28(8), 1221–1226. 10.1097/QAD.0000000000000188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong LH, Rooyen HV, Modiba P, Richter L, Gray G, McIntyre JA, et al. (2009). Test and tell: correlates and consequences of testing and disclosure of HIV status in South Africa (HPTN 043 Project Accept). Journal of Acquired Immune Deficiency Syndromes, 50(2), 215–222. 10.1097/QAI.0b013e3181900172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuch M, & Lurie M (2012). “A virus and nothing else”: the effect of ART on HIV-related stigma in rural South Africa. AIDS and Behavior, 16(3), 564–570. 10.1007/s10461-011-0089-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.