Abstract
Background
Repetitive peripheral magnetic stimulation (rPMS) is a non‐invasive treatment method that can penetrate to deeper structures with painless stimulation to improve motor function in people with physical impairment due to brain or nerve disorders. rPMS for people after stroke has proved to be a feasible approach to improving activities of daily living and functional ability. However, the effectiveness and safety of this intervention for people after stroke currently remain uncertain. This is an update of the review published in 2017.
Objectives
To assess the effects of rPMS in improving activities of daily living and functional ability in people after stroke.
Search methods
On 7 January 2019, we searched the Cochrane Stroke Group Trials Register; the Cochrane Central Register of Controlled Trials (CENTRAL), in the Cochrane Library; MEDLINE; Embase; the Cumulative Index to Nursing and Allied Health Literature (CINAHL); PsycINFO; the Allied and Complementary Medicine Database (AMED); Occupational Therapy Systematic Evaluation of Evidence (OTseeker); the Physiotherapy Evidence Database (PEDro); ICHUSHI Web; and six ongoing trial registries. We screened reference lists, and we contacted experts in the field. We placed no restrictions on the language or date of publication when searching electronic databases.
Selection criteria
We included randomised controlled trials (RCTs) conducted to assess the therapeutic effect of rPMS for people after stroke. Comparisons eligible for inclusion were (1) active rPMS only compared with 'sham' rPMS (a very weak form of stimulation or a sound only); (2) active rPMS only compared with no intervention; (3) active rPMS plus rehabilitation compared with sham rPMS plus rehabilitation; and (4) active rPMS plus rehabilitation compared with rehabilitation only.
Data collection and analysis
Two review authors independently assessed studies for inclusion. The same review authors assessed methods and risk of bias, undertook data extraction, and used the GRADE approach to assess the quality of evidence. We contacted trial authors to request unpublished information if necessary. We resolved all disagreements through discussion.
Main results
We included four trials (three RCTs and one cross‐over trial) involving 139 participants. Blinding of participants and physicians was well reported within all trials. We judged the overall risk of bias across trials as low. Only two trials (with 63 and 18 participants, respectively) provided sufficient information to be included in the meta‐analysis. We found no clear effect of rPMS on activities of daily living at the end of treatment (mean difference (MD) ‐3.00, 95% confidence interval (CI) ‐16.35 to 10.35; P = 0.66; 1 trial; 63 participants; low‐quality evidence) and at the end of follow‐up (MD ‐2.00, 95% CI ‐14.86 to 10.86; P = 0.76; 1 trial; 63 participants; low‐quality evidence) when comparing rPMS plus rehabilitation versus sham plus rehabilitation. We found no statistical difference in improvement of upper limb function at the end of treatment (MD 2.00, 95% CI ‐4.91 to 8.91; P = 0.57; 1 trial; 63 participants; low‐quality evidence) and at the end of follow‐up (MD 4.00, 95% CI ‐2.92 to 10.92; P = 0.26; 1 trial; 63 participants; low‐quality evidence) when comparing rPMS plus rehabilitation versus sham plus rehabilitation. We observed a significant decrease in spasticity of the elbow at the end of follow‐up (MD ‐0.48, 95% CI ‐0.93 to ‐0.03; P = 0.03; 1 trial; 63 participants; low‐quality evidence) when comparing rPMS plus rehabilitation versus sham plus rehabilitation. In terms of muscle strength, rPMS treatment was not associated with improved muscle strength of the ankle dorsiflexors at the end of treatment (MD 3.00, 95% CI ‐2.44 to 8.44; P = 0.28; 1 trial; 18 participants; low‐quality evidence) when compared with sham rPMS. No studies provided information on lower limb function or adverse events, including death. Based on the GRADE approach, we judged the quality of evidence related to the primary outcome as low, owing to the small sample size of the studies.
Authors' conclusions
Available trials provided insufficient evidence to permit any conclusions about routine use of rPMS for people after stroke. Additional trials with large sample sizes are needed to provide robust evidence for rPMS after stroke.
Plain language summary
Repetitive peripheral magnetic stimulation for improving everyday activities in people after stroke
Review question Is repetitive peripheral magnetic stimulation (rPMS) effective for improving daily activities in people after stroke?
Background Stroke, the most common cause of disability, occurs when the blood supply to part of the brain is interrupted or reduced. Two types of stroke are known: ischaemic (due to lack of blood flow) and haemorrhagic (due to bleeding). Paralysis of the arm or leg after stroke causes problems with daily activities and functions, including eating, showering, dressing, and walking. People after stroke with hemiparesis require physical rehabilitation, that is, training of upper and lower limbs, exercise focused on activities of daily living, and fitting of appropriate walking aids (e.g. cane). However, effective treatments are currently limited. rPMS is a painless method of stimulation that has been used to try to improve movement in people with brain or nerve disorders.
Search date The search is current to 7 January 2019.
Study characteristics This is an update of the review published in 2017. We examined the evidence from four trials of rPMS (three individual RCTs and one cross‐over trial) involving a total of 139 participants. Two studies compared rPMS against 'sham' stimulation (a very weak stimulation or a sound only). Two studies compared rPMS plus rehabilitation versus sham plus rehabilitation.
Key results We found little evidence for the use of rPMS to improve activities of daily living, muscle strength, upper limb function, and spasticity (unusual stiffness of muscles) in people after stroke. Although one trial reported that rPMS reduced spasticity of the upper limb, the effect was small and remains unclear.
Quality of the evidence We classified the quality of the evidence as low for improving activities of daily living, mainly because one study had a small sample size.
Authors' conclusions It remains unclear whether use of rPMS is useful for improving activities of daily living and functional ability in people after stroke. More trials involving larger numbers of participants are needed to determine the effects of rPMS.
Summary of findings
Background
Description of the condition
Stroke is a serious healthcare problem that requires long‐term rehabilitation as a core component of recovery (Sacco 2013). Every year, around 16 million strokes occur throughout the world, causing 5.7 million deaths (Strong 2007). Approximately 88% of all strokes are of the ischaemic type; other types include haemorrhagic stroke and subarachnoid haemorrhage (Park 2012). The most common disability after stroke is motor impairment (Langhorne 2009), which adversely affects control of arm and leg movement and occurs in nearly 80% of people after stroke (De Vries 2007). At present, although post‐stroke functional recovery remains a high priority in health care, evidence on effective interventions for post‐stroke impairment is limited (McArthur 2011).
Description of the intervention
Repetitive peripheral magnetic stimulation (rPMS) is a unique non‐invasive treatment method that was developed for therapeutic neuromodulation in movement disorders (Beaulieu 2013). In rPMS, a stimulation coil (magnetic field generator) is placed over paralysed muscles of the arms, legs, or torso. The stimulation coil is attached to a stimulator (pulse generator), which provides an electrical current to the coil. The coil builds up a magnetic field as it passes through the skin, and it directs an electrical current into the neurons. Once the current achieves a certain value, an action potential is induced, which causes the neuron to depolarise and the muscles to eventually contract.
Treatment by rPMS allows painless stimulation of deep muscle structures that cannot be reached by neuromuscular electrical stimulation (NMES) (Barker 1991; Ito 2013). NMES recruits cutaneous receptors, whereas rPMS generates proprioceptive information during muscle contraction. Proprioceptive feedback during muscle contraction can influence brain plasticity and improve the sensorimotor system, while cutaneous receptors can generate noisy signals. These differences between NMES and rPMS are important. People receiving rPMS do not need to remove their clothes because the procedure does not require placement of electrodes on their skin. Implanted medical devices, such as pacemakers or deep brain simulators, are contraindications for rPMS as well as NMES. However, the technology has no known negative side effects. NMES is widely used to treat people with motor deficits resulting from brain or nerve disorders, and rPMS is also coming to be used for these conditions. rPMS devices are more bulky and expensive than NMES, which precludes wide use of the technology. Nevertheless, rPMS can be performed to safely stimulate deeper regions of muscle without pain, and can potentially improve functional recovery in people after stroke (Han 2006).
How the intervention might work
Applying rPMS to the muscle induces a proprioceptive input to the central nervous system in two ways (Struppler 2004).
Direct activation of sensorimotor nerve fibres with an orthodromic and antidromic conduction.
Indirect activation of mechanoreceptors during rhythmical contraction and relaxation, as well as vibration of the muscles.
This afferent input elicits sensations and reaches higher levels of the central nervous system.
Initial assessment of transcranial magnetic stimulation revealed an increase in corticomotor excitability after rPMS, and subsequent functional magnetic resonance imaging assessment showed focal activations within the sensorimotor cortex in healthy participants (Gallasch 2015). After stroke, rPMS increased motor‐evoked potential amplitude (Flamand 2014), as well as motor cortex excitability (Heldmann 2000; Krause 2008). One study showed that rPMS caused brain plastic change and increased ankle muscle strength on the paretic side in chronic patients after stroke, although NMES did not (Beaulieu 2017). Further, rPMS suppressed spasticity (Struppler 2003), and it had a modulatory effect on motor performance (Struppler 2004). This technique is also thought to increase neural excitability of the cortex and to balance interactions between hemispheres, thereby contributing to functional improvement in people after stroke (Kerkhoff 2001).
Why it is important to do this review
Several clinical trials have examined the use of rPMS for people with functional disability (Heldmann 2000; Nielsen 1996; Struppler 2004; Struppler 2007). However, the peer‐reviewed literature includes no systematic review that has assessed the findings of available trials. It remains unclear whether rPMS is useful for people with functional disability after stroke, what type of stimulation (high frequency, low frequency, or other) should be performed, and on which part of the body (upper limb, lower limb, or others). In addition, rPMS studies have tended to include small sample sizes. Therefore, a systematic review of trials is needed to evaluate the effectiveness of rPMS.
Objectives
To assess the effects of rPMS in improving activities of daily living and functional ability in people after stroke.
Methods
Criteria for considering studies for this review
Types of studies
We included individual randomised controlled trials (RCTs), cluster‐RCTs, and cross‐over trials. We excluded quasi‐RCTs (trials in which the method of allocating participants to a treatment is not strictly random, e.g. by date of birth, hospital record number, alternation).
Types of participants
We included people after stroke regardless of sex, age, and stroke severity and duration. Stroke is defined by the World Health Organization as a "neurological deficit of cerebrovascular cause that lasts more than 24 hours or leads to death within 24 hours" (World Health Organization 1989). We included mixed participant groups that consisted of people after stroke and other brain diseases, such as traumatic brain injury, if more than half of them had a diagnosis of stroke.
Types of interventions
We included trials comparing any type of active rPMS or rPMS plus rehabilitation for improving functional ability versus any type of control intervention (i.e. sham rPMS, sham rPMS plus rehabilitation for improving functional ability, or no intervention). Investigators conducted rPMS peripherally (not for the central nervous system such as brain or spinal cord) and non‐invasively (without use of puncture needle or implantation techniques).
We investigated the following comparisons.
Active rPMS only compared with sham rPMS.
Active rPMS only compared with no intervention.
Active rPMS plus rehabilitation compared with sham rPMS plus rehabilitation.
Active rPMS plus rehabilitation compared with rehabilitation only.
Types of outcome measures
Primary outcomes
Activities of daily living (ADLs) at the end of treatment and at the end of scheduled follow‐up. ADLs refer to basic tasks of everyday life, including self‐care activities such as eating, bathing, dressing, and toileting. We preferentially used the Barthel Index (BI) or the Functional Independence Measure (FIM) but allowed any related validated measuring tools such as:
Katz Index of Independence in Activities of Daily Living; and
Frenchay Activities Index (FAI).
Secondary outcomes
We included the following five secondary outcome measures. Any related validated measuring tools were allowed.
-
Upper limb function.
Fugl‐Meyer Assessment.
Action Research Arm Test.
Wolf Motor Function Test (seconds).
-
Lower limb function.
Gait velocity (cm/s).
Timed Up and Go Test (seconds).
Spasticity.
(Modified) Tardieu Scale.
Modified Ashworth Scale (MAS).
-
Muscle strength.
Grip strength (kg).
Medical Research Council (MRC) Scale.
Death (as adverse event).
We explored secondary outcomes at the end of treatment and at the end of scheduled follow‐up. We analysed these outcomes as continuous data.
Search methods for identification of studies
See the 'Specialized Register' information at the Cochrane Stroke Group's website. We searched for trials in all languages and arranged for translation of relevant articles published in languages other than English and Japanese. We did not impose any other restrictions for searches.
Electronic searches
We searched the Cochrane Stroke Group trials register and the following electronic databases.
Cochrane Central Register of Controlled Trials (CENTRAL; 2019, Issue 1), in the Cochrane Library (searched 7 January 2019) (Appendix 1).
MEDLINE in Ovid (1946 to 7 January 2019) (Appendix 2).
Embase in Ovid (1980 to 7 January 2019) (Appendix 3).
Cumulative Index to Nursing and Allied Health Literature (CINAHL), in EBSCO (1937 to 7 January 2019) (Appendix 4).
PsycINFO in Ovid (1806 to 7 January 2019) (Appendix 5).
Allied and Complementary Medicine Database (AMED), in Ovid (1985 to 7 January 2019) (Appendix 6).
Occupational Therapy Systematic Evaluation of Evidence (OTseeker; www.otseeker.com/) (searched 7 January 2019 ) (Appendix 7).
Physiotherapy Evidence Database (PEDro; www.pedro.fhs.usyd.edu.au/) (1929 to 7 January 2019) (Appendix 8).
Ichushi‐Web (Japan Medical Abstracts Society (JAMAS)) (www.jamas.or.jp/) (searched 7 January 2019) (Appendix 9).
We developed the MEDLINE search strategy (Appendix 2) with the help of the Cochrane Stroke Group Information Specialist and adapted it for use with the other databases.
We also searched the following ongoing trials registers.
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov; searched 7 January 2019) (Appendix 10).
ISRCTN Registry (www.isrctn.com/; searched 7 January 2019) (Appendix 11).
Stroke Trials Registry (www.strokecenter.org/trials/; searched 7 January 2019) (Appendix 12).
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp/search/en/; searched 7 January 2019) (Appendix 13).
Japanese University hospital Medical Information Network (UMIN) Clinical Trials Registry (UMIN‐CTR) (www.umin.ac.jp/ctr/; searched 7 January 2019 ) (Appendix 14).
Japan Registry of Clinical Trials (jRCT) (jrct.niph.go.jp/; searched 7 January 2019) (Appendix 15).
Searching other resources
To identify additional published and unpublished relevant studies for potential inclusion in the review, we:
contacted experts in the field;
screened reference lists of relevant articles; and
searched in Google Scholar (scholar.google.co.uk/).
Data collection and analysis
Selection of studies
Two review authors (YY, KT) independently screened titles and abstracts of references obtained as a result of our searching activities and excluded obviously irrelevant reports. We retrieved full‐text articles for the remaining references, and two review authors (YY, KT) independently screened these to identify studies for inclusion. We identified and recorded reasons for exclusion of ineligible studies. We resolved disagreements through discussion, or, if required, we consulted the third review author (RM). We collated multiple reports of the same study, so that each study ‐ not each reference ‐ was the unit of interest in the review. We recorded the selection process and completed a PRISMA flow diagram (Moher 2009). We included studies presented only as abstracts, if sufficient information was reported. We used Covidence software for reference handling (Covidence 2013).
Data extraction and management
Two review authors (YY, KT) independently extracted the following data from the included studies and entered those data into Covidence (Covidence 2013).
Methods: study design, randomisation method, allocation concealment method, blinding methods.
Participants: diagnosis (type, severity, and location of stroke), number in each group, age, sex, baseline comparability between two groups, time from onset, losses to follow‐up.
Interventions: details of rPMS (frequency, intensity, duration, treatment session), target of stimulation, co‐exercise.
Outcomes: types of outcomes, assessment time points.
Other: setting, publication year, sources of funding, intention‐to‐treat analysis (ITT).
All review authors resolved disagreements by discussion.
Assessment of risk of bias in included studies
Two review authors (YY, KT) independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) along with Covidence (Covidence 2013). We resolved disagreements between two authors by discussion or by consultation with the third review author (RM). Risk of bias includes the domains of random sequence, generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other bias. We assessed each domain as having low risk, high risk, or unclear risk of bias.
Overall risk of bias
We made explicit judgements about whether studies were at high risk of bias, according to the criteria given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). With reference to the above domains, we assessed the likely magnitude and direction of the bias and whether we considered it likely to impact study findings.
We graded the risk of bias for each domain and provided information from the study report together with a justification for our judgement in the 'Risk of bias' tables.
We used the GRADE approach to assess the quality of the body of evidence related to the following main outcomes at the end of treatment (Guyatt 2008).
ADLs.
Upper limb function.
Lower limb function.
Spasticity.
Muscle strength.
Death.
We used GRADEprofiler to import data from Review Manager 5.3 to create a 'Summary of findings' table (GRADE 2014; RevMan 2014). We produced a summary of the intervention effect and a measure of quality for each of the above outcomes using the GRADE approach (Ryan 2016). The GRADE approach is based on five considerations (study limitations, consistency of effect, imprecision, indirectness, and publication bias) and is used to assess the quality of the body of evidence for each outcome. Evidence can be downgraded from 'high quality' by one level for serious (or by two levels for very serious) limitations, depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates, or potential publication bias.
Measures of treatment effect
Dichotomous data
For dichotomous data, we presented results as risk ratios (RRs) with 95% confidence intervals (CIs).
Continuous data
For continuous data, we used the mean difference (MD) and 95% CI if outcomes were measured in the same way between trials. We used the standardised mean difference (SMD) and 95% CI to combine trials that measured the same outcome but used different scales.
Unit of analysis issues
Cluster‐randomised trials
We planned to include cluster‐randomised trials in the analyses, along with individually randomised trials. If we found such trials, we adjusted standard errors (SEs) using the methods described in the Cochrane Handbook for Systematic Reviews of Interventions, on the basis of an estimate of the intracluster correlation coefficient (ICC) derived from the trial if possible, from a similar trial, or from a study of a similar population. If we used ICCs from other sources, we reported this and conducted sensitivity analyses to investigate the effect of variation in the ICC. If we identified both cluster‐randomised trials and individually randomised trials, we planned to synthesise relevant information.
We also planned to assess heterogeneity in the randomisation unit and to perform a sensitivity analysis to investigate effects of the randomisation unit.
Cross‐over trials
We included cross‐over trials in the review and analysed only data from the first phase of these trials.
Multi‐armed trials
When we identified trials with multiple intervention arms, we planned to include only directly relevant arms. If the trial included several relevant intervention arms, we planned to combine all relevant experimental intervention groups of the study into a single group and to combine all relevant control intervention groups into a single control group.
Dealing with missing data
If necessary, we contacted trial authors to obtain missing data, as well as data collected but not reported. We recorded levels of attrition for included studies. We planned to perform sensitivity analysis to explore the impact of including studies with high levels of missing data in the overall assessment of treatment effect.
For all outcomes, we carried out analyses as far as possible on an ITT basis, that is, we attempted to include in the analyses all participants randomised to each group, and we analysed all participants in the group to which they were allocated, regardless of whether they received the allocated intervention. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis by using I². We regarded heterogeneity as substantial if I² was greater than 30%. We used Review Manager to assess heterogeneity (RevMan 2014).
Assessment of reporting biases
If we found 10 studies or more, we planned to use funnel plots to detect publication bias. If asymmetry was suggested by visual assessment, we planned to perform exploratory analyses to investigate this. We also investigated selective outcome reporting though comparison of the methods section of articles with results reported.
Data synthesis
Two review authors (YY, KT) independently extracted data from the included trials. One review author (KS) entered the data into RevMan, and the other review author (RM) checked the entries. We resolved disagreements through discussion, with reference to the original report.
We carried out statistical analysis using Review Manager (RevMan 2014). We used fixed‐effect meta‐analysis in combining data when it was reasonable to assume that studies were estimating the same underlying treatment effect, that is, when trials were examining the same intervention, and when trial populations and methods were judged sufficiently similar. If clinical heterogeneity was sufficient to expect that underlying treatment effects differ between trials, or if we detected substantial statistical heterogeneity, we used random‐effects meta‐analysis to produce an overall summary if an average treatment effect across trials was considered clinically meaningful. We treated the random‐effects summary as the average range of possible treatment effects, and we discussed the clinical implications of differing treatment effects between trials. If the average treatment effect was not clinically meaningful, we did not combine trials. If we used random‐effects analyses, we presented results as the average treatment effect with 95% CI, along with estimates of T² and I². If it was inappropriate or impossible to pool data quantitatively, we provided a narrative summary of study results.
Subgroup analysis and investigation of heterogeneity
When we identified substantial heterogeneity in the primary outcomes, we investigated this by conducting subgroup analyses. We considered whether an overall summary was meaningful, and if so, we used random‐effects analysis to produce it.
We planned to carry out the following subgroup analyses of primary outcomes if sufficient data were available.
Location of stimulation: upper limb versus lower limb or trunk.
Type of stroke: cerebral infarction versus cerebral haemorrhage.
Duration of illness: acute to subacute phase (to six months after stroke) versus chronic phase (more than six months after stroke).
We assessed subgroup differences by checking if a statistically significant subgroup difference was detected using Review Manager (RevMan 2014). We reported the results of subgroup analyses by quoting the Chi² statistic and the P value, and results by providing the I² value.
Sensitivity analysis
If we identified two or more studies for primary outcomes, we planned to perform sensitivity analyses to see how the results were affected by excluding:
studies with inadequate allocation concealment and random sequence generation;
studies in which outcome evaluation was not blinded;
studies in which loss to follow‐up was not reported or was greater than 10%; and
unpublished studies.
Results
Description of studies
Results of the search
See Figure 1.
1.
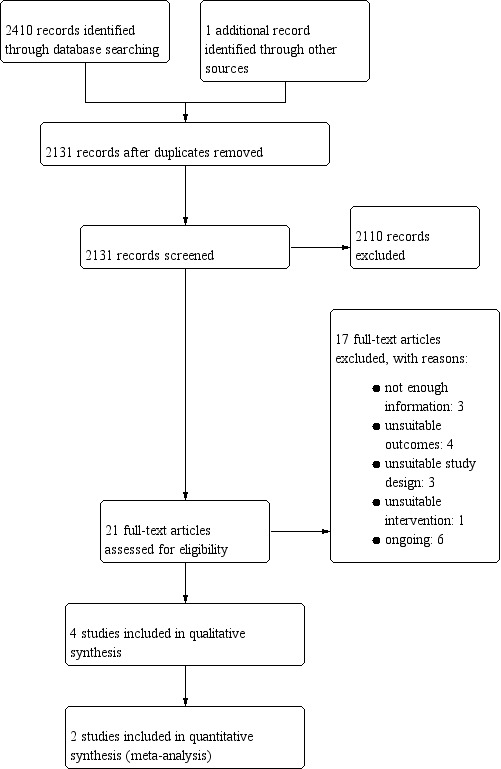
Study flow diagram.
The database searches for this update yielded 2411 records. After screening these through titles and abstracts, we identified 21 potentially relevant articles. After reviewing the full text of the articles, we included in the review four trials involving a total of 139 participants (Beaulieu 2015; Krewer 2014; Werner 2016; Zifko 2002).
Included studies
See Characteristics of included studies.
Study design and study location
We included three parallel‐group trials (Beaulieu 2015; Krewer 2014; Zifko 2002), as well as one cross‐over trial (Werner 2016), in the qualitative synthesis. Two trials were from Germany, one was from Canada, and the other was from Austria. In the previous version of this review, one trial was listed under 'Studies awaiting classification', as the trial had insufficient information (Zifko 2002). In this review, we decided to include this trial after discussion among review authors because the trial provided enough information on interventions and outcomes and lacked information only on assessment time point.
Sample characteristics
The four included trials involved 139 participants. Individual sample sizes of identified trials ranged from 18 in Beaulieu 2015 and Zifko 2002 to 63 in Krewer 2014. The mean age of participants was 55 years or younger (Beaulieu 2015; Krewer 2014; Werner 2016), and mean time from onset ranged from less than 26 weeks in Krewer 2014 to 83 months in Beaulieu 2015. Two studies included participants with stroke, and their elapsed time from onset was over 12 months (Beaulieu 2015; Werner 2016). Trials included more men (57%) than women (43%) participants. Two studies included traumatic brain injury (Krewer 2014; Werner 2016), and one study included tetraparesis (Werner 2016). We could not exclude study participants with traumatic brain injury. We decided to include trials of mixed groups if more than half had received a stroke diagnosis. We noted imbalances in time from onset in Beaulieu 2015 and Krewer 2014, and in mean age in Werner 2016, but we considered these unlikely to affect outcomes. Groups in all studies were comparable in terms of assessed baseline characteristics.
Intervention approaches
The included studies used varied protocols of rPMS. Frequency of rPMS ranged from 5 Hz in Werner 2016 to 25 Hz in Krewer 2014. One study adopted theta‐burst frequency rPMS (Beaulieu 2015). The duration of stimulation (per session) ranged from 190 seconds in Beaulieu 2015 to 20 minutes in Krewer 2014, and the number of stimulations (per session) ranged from 600 in Beaulieu 2015 to 5000 in Krewer 2014. Only one study conducted multiple stimulation sessions as part of the treatment regimen (two times a day, five times a week, for two weeks) (Krewer 2014). Targets of stimulation were the lower leg (Beaulieu 2015), the upper and lower arm (Krewer 2014), the upper arm (Zifko 2002), and the lower arm (Werner 2016). Co‐exercise included occupational therapy after each stimulation (Krewer 2014), as well as muscle stretching during stimulation (Werner 2016). Sham stimulation consisted of low‐intensity stimulation in Beaulieu 2015, or a clicking sound only in Krewer 2014Werner 2016 and Zifko 2002.
Outcomes
The included trials used several heterogeneous outcome measures. Only one study assessed our primary outcome (ADLs) as measured by the Barthel Index (Krewer 2014). As muscle strength evaluation, Beaulieu 2015 measured maximal isometric strength of the ankle dorsiflexors. Krewer 2014 assessed upper limb function using the Fugl‐Meyer Assessment, and Zifko 2002 used angle of motion for hand extension and hand flexion and the Bard and Hirschberg Score and Action Research Arm Test. Investigators measured spasticity by using the Modified Tardieu Scale (Krewer 2014), the Ashworth Score (Zifko 2002), the Modified Ashworth Score (Werner 2016), or the Gerstenbrand Spasticity Rating Scale (Zifko 2002). Two trials evaluated outcomes immediately after treatment (Beaulieu 2015; Werner 2016); one trial measured outcomes after two weeks of treatment and two weeks after the treatment phase (Krewer 2014). One trial had no information on the assessment time point (Zifko 2002). None of the included studies reported any adverse events including death.
Excluded studies
Among 21 potentially relevant studies, we excluded 17 trials because they did not meet the inclusion criteria. We have listed reasons for exclusion in the Characteristics of excluded studies table. Three studies were not RCTs (Bernhardt 2007; Struppler 2002; Struppler 2009), and four studies measured outcomes that were different from those provided in our protocol (Heldmann 2000; Kuznetsova 2016a; Kuznetsova 2016b; Momosaki 2014). One study provided an unsuitable intervention. Evidence was insufficient for review authors to determine inclusion eligibility for three trials (Kotchetkov 1999; Kuznetsova 2013; Samosiuk 2003), and we were unable to make contact with study authors.
Ongoing studies
We identified six ongoing trials that appeared to be relevant for inclusion (DRKS00007722; DRKS00007899; jRCTs042180014; UMIN000018750; UMIN000019106; UMIN000031957). See Characteristics of ongoing studies.
Risk of bias in included studies
2.
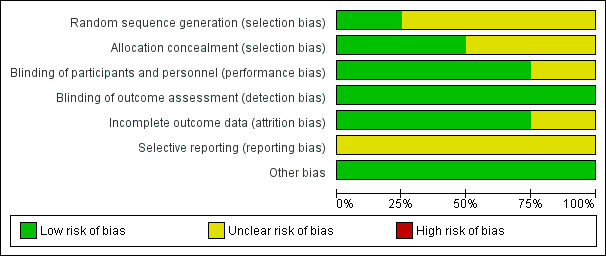
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
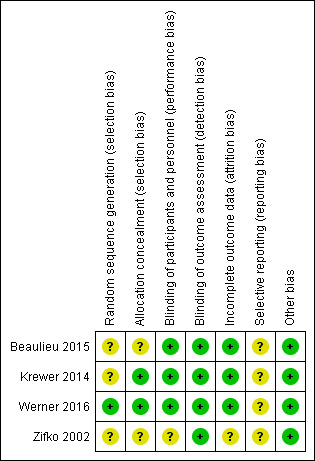
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Sequence generation
Werner 2016 conducted sequence generation with the help of a computer‐generated lot (www.randomizer.at), and so we judged this trial to be at low risk of bias. As the other studies did not report random sequence generation, we classified them as having unclear risk of bias.
Allocation concealment
We judged allocation concealment to be at low risk of bias in two trials (Krewer 2014; Werner 2016); however, two studies did not report on this (Beaulieu 2015; Zifko 2002), and so we judged them to be at unclear risk of bias.
Blinding
Participants and personnel
Three trials provided blinding with regard to participants and personnel, and one study provided no information on personnel. Investigators conducted sham stimulations adequately. We ranked three studies as having low risk of bias (Beaulieu 2015; Krewer 2014; Werner 2016), and one as having unclear risk of bias (Zifko 2002).
Outcome assessment
All trials provided blinding with regard to outcome assessors. We ranked these studies as having low risk of bias.
Incomplete outcome data
Beaulieu 2015 and Werner 2016 reported no withdrawals or dropouts, so we classified these studies as having low risk of bias. Krewer 2014 reported that only three participants were lost to follow‐up (5%) and described no differences in the reasons why outcome data were missing. In addition, Krewer 2014 performed ITT analysis, and we classified this study as having low risk of bias. Zifko 2002 reported that two participants (11%) did not complete the study. Information on the reason for this and on ITT analysis was unclear. We classified this study as having unclear risk of bias.
Selective reporting
Study protocols were not available for any of the included studies, and so we judged selective reporting bias as unclear.
Other potential sources of bias
We identified no other information associated with other potential sources of bias. We judged other potential sources of bias for all studies as low.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
Summary of findings for the main comparison. Active rPMS only compared with sham rPMS in stroke.
| Active rPMS only compared with sham rPMS in stroke | ||||||
|
Patient or population: people with stroke
Intervention: active rPMS
Comparison: sham rPMS Setting: not reported | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with sham rPMS | Risk with rPMS | |||||
| Activities of daily living (ADLs) assessed with Barthel Index Scale, from 0 to 100 | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| Upper limb function assessed with Fugl‐Meyer Assessment Scale, from 0 to 66 | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| Lower limb function | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| Spasticity (elbow) assessed with Modified Tardieu Scale, from 0 to 5 | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| Spasticity (wrist) assessed with Modified Tardieu Scale, from 0 to 5 | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| Muscle strength assessed with dorsiflexion strength | Mean muscle strength 10.44 kg | MD 3 kg higher (2.44 lower to 8.44 higher) | ‐ | 18 (1 RCT) | ⊕⊕⊝⊝ Lowa | |
| Death | ‐ | ‐ | See comments | ‐ | ‐ | No trials reported this outcome |
| *The risk in the intervention group (and its 95% confidence interval) is based on assumed risk in the comparison group and relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RCT: randomised controlled trial; rPMS: repetitive peripheral magnetic stimulation. | ||||||
| GRADE Working Group grades of evidence. High quality: we are very confident that the true effect lies close to the estimate of effect. Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of effect but may be substantially different. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of effect. Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aOne study with small sample size; 95% CI overlaps zero.
Summary of findings 2. Active rPMS only compared with no intervention in stroke.
| Active rPMS only compared with no intervention in stroke | ||||||
|
Patient or population: people with stroke Intervention: active rPMS Comparison: no intervention Setting: ‐ | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with no intervention | Risk with rPMS | |||||
| Activities of daily living (ADLs) assessed with Barthel Index Scale, from 0 to 100 | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| Upper limb function assessed with Fugl‐Meyer Assessment Scale, from 0 to 66 | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| Lower limb function | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| Spasticity (elbow) assessed with Modified Tardieu Scale, from 0 to 5 | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| Spasticity (wrist) assessed with Modified Tardieu Scale, from 0 to 5 | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| Muscle strength assessed with dorsiflexion strength | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| Death | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| *The risk in the intervention group (and its 95% confidence interval) is based on assumed risk in the comparison group and relative effect of the intervention (and its 95% CI). CI: confidence interval; rPMS: repetitive peripheral magnetic stimulation. | ||||||
| GRADE Working Group grades of evidence. High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
Summary of findings 3. Active rPMS plus rehabilitation compared with sham rPMS plus rehabilitation in stroke.
| Active rPMS plus rehabilitation compared with sham rPMS plus rehabilitation in stroke | ||||||
|
Patient or population: people with stroke Intervention: active rPMS plus rehabilitation Comparison: sham rPMS plus rehabilitation Settings: neurological rehabilitation hospital | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with sham rPMS plus rehabilitation | Risk with active rPMS plus rehabilitation | |||||
| Activities of daily living (ADLs) assessed with Barthel Index Scale, from 0 to 100 | Mean activities of daily living score 50 | MD 3 lower (16.35 lower to 10.35 higher) |
‐ | 63 (1 RCT) |
⊕⊕⊝⊝ Lowa | |
| Upper limb function assessed with Fugl‐Meyer Assessment Scale, from 0 to 66 | Mean upper limb function score 13 | MD 2 higher (4.91 lower to 8.91 higher) | ‐ | 63 (1 RCT) | ⊕⊕⊝⊝ Lowa | |
| Lower limb function | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| Spasticity (elbow) assessed with Modified Tardieu Scale, from 0 to 5 | Mean spasticity (elbow) score 1.41 | MD 0.41 lower (0.89 lower to 0.07 higher) | ‐ | 63 (1 RCT) | ⊕⊕⊝⊝ Lowa | |
| Spasticity (wrist) assessed with Modified Tardieu Scale, from 0 to 5 | Mean spasticity (wrist) score 2.13 | MD 0.2 lower (0.76 lower to 0.36 higher) | ‐ | 63 (1 RCT) | ⊕⊕⊝⊝ Lowa | |
| Muscle strength assessed with dorsiflexion strength | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| Death | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| *The risk in the intervention group (and its 95% confidence interval) is based on assumed risk in the comparison group and relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RCT: randomised controlled trial; rPMS: repetitive peripheral magnetic stimulation. | ||||||
| GRADE Working Group grades of evidence. High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
aOne study with small sample size; 95% CI overlaps zero.
Summary of findings 4. Active rPMS plus rehabilitation compared with rehabilitation only in stroke.
| Active rPMS plus rehabilitation compared with rehabilitation only in stroke | ||||||
|
Patient or population: people with stroke Intervention: active rPMS plus rehabilitation Comparison: rehabilitation only Settings: ‐ | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with rehabilitation only | Risk with active rPMS plus rehabilitation | |||||
| Activities of daily living (ADLs) assessed with Barthel Index Scale, from 0 to 100 | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| Upper limb function assessed with Fugl‐Meyer Assessment Scale, from 0 to 66 | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| Lower limb function | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| Spasticity (elbow) assessed with Modified Tardieu Scale, from 0 to 5 | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| Spasticity (wrist) assessed with Modified Tardieu Scale, from 0 to 5 | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| Muscle strength assessed with dorsiflexion strength | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| Death | ‐ | ‐ | See comments | ‐ | ‐ | No trials measured this outcome |
| *The risk in the intervention group (and its 95% confidence interval) is based on assumed risk in the comparison group and relative effect of the intervention (and its 95% CI). CI: confidence interval; rPMS: repetitive peripheral magnetic stimulation. | ||||||
| GRADE Working Group grades of evidence. High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
See Table 1Table 2Table 3 and Table 4.
We contacted the authors of included studies to request missing outcome data and data collected but not reported. However, we could not obtain data from the first phase of the cross‐over trial (Werner 2016). Zifko 2002 was reported as a conference abstract, and we could not obtain detailed study information nor the study author's contact address. Thus, we excluded these two studies from the quantitative synthesis (meta‐analysis). Finally, we included two studies in the quantitative analysis (Beaulieu 2015; Krewer 2014). As Krewer 2014 evaluated spasticity at both the elbow and the wrist, we analysed these data separately.
Comparison 1. Active rPMS versus sham rPMS
Primary outcome
Activities of daily living
We found no studies examining the effect of rPMS on ADLs as a primary outcome in people after stroke.
Secondary outcomes
Muscle strength
Only one small study assessed our secondary outcome of muscle strength using maximal isometric strength of the ankle dorsiflexors at the end of treatment (Beaulieu 2015). This trial included a total of 18 participants and showed that rPMS treatment was not associated with significant improvement in muscle strength at the end of treatment (after a single session) (mean difference (MD) 3.00, 95% confidence interval (CI) ‐2.44 to 8.44; Analysis 1.1). This study did not report muscle strength at the end of follow‐up.
1.1. Analysis.
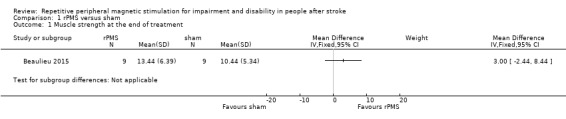
Comparison 1 rPMS versus sham, Outcome 1 Muscle strength at the end of treatment.
Upper limb function
One study reported significant improvement in upper limb function using the angle of motion for hand extension (from 151 to 157), the Action Research Arm Test (from 23.2 to 32.8), and the Bard and Hirschberg Score in regard to hand extension (from 1.4 to 1.7), finger extension (from 1.6 to 2.0), and pronation of the arm (2.2 to 2.7). The assessment time point of this outcome was unclear (Zifko 2002).
Spasticity
One study reported significant improvement in spasticity assessed via the Ashworth Scale (from 2.0 to 1.7) and Gerstenbrand Spasticity (from 2.3 to 1.8) (Zifko 2002). The assessment time point for this outcome was unclear (Zifko 2002).
Others
Included trials did not report adverse events including death associated with rPMS.
Comparison 2. Active rPMS only compared with no intervention
We found no studies that performed this comparison.
Comparison 3. rPMS plus rehabilitation versus sham rPMS plus rehabilitation
Primary outcome
Activities of daily living
Krewer 2014 provided data on activities of daily living as a Barthel Index score at the end of treatment (after two weeks' treatment) and at the end of follow‐up (two weeks after treatment phase). Data show no significant differences between the rPMS plus rehabilitation group and the sham plus rehabilitation group (end of treatment: MD ‐3.00, 95% CI ‐16.35 to 10.35: Analysis 2.1; end of follow‐up: MD ‐2.00, 95% CI ‐14.86 to 10.86: Analysis 2.2).
2.1. Analysis.
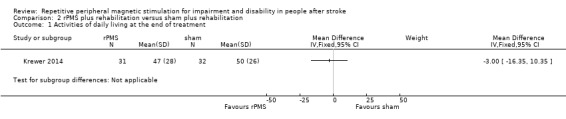
Comparison 2 rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 1 Activities of daily living at the end of treatment.
2.2. Analysis.
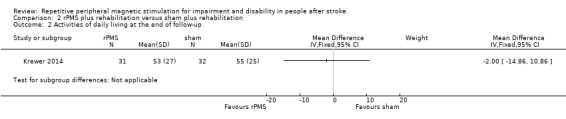
Comparison 2 rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 2 Activities of daily living at the end of follow‐up.
Secondary outcomes
Upper limb function
Krewer 2014 reported the Fugl‐Meyer Assessment as an outcome measure of upper limb function. Results of this study show that rPMS plus rehabilitation did not increase upper limb function compared with sham plus rehabilitation at the end of treatment (after two weeks' treatment) and at the end of follow‐up (two weeks after treatment phase) (end of treatment: MD 2.00, 95% CI ‐4.91 to 8.91: Analysis 2.3; end of follow‐up: MD 4.00, 95% CI ‐2.92 to 10.92: Analysis 2.4).
2.3. Analysis.
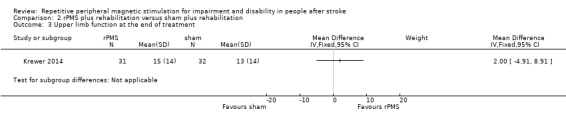
Comparison 2 rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 3 Upper limb function at the end of treatment.
2.4. Analysis.
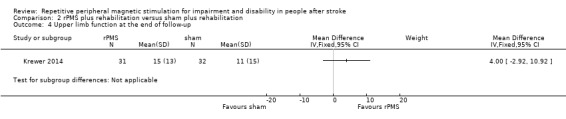
Comparison 2 rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 4 Upper limb function at the end of follow‐up.
Spasticity
Krewer 2014 evaluated spasticity at the elbow and the wrist using the Modified Tardieu Scale. We separately evaluated results related to the elbow and the wrist. We found no significant differences in spasticity between the rPMS plus rehabilitation group and the sham plus rehabilitation group at the end of treatment (after two weeks' treatment) (elbow: MD ‐0.41, 95% CI ‐0.89 to 0.07; wrist: MD ‐0.20, 95% CI ‐0.76 to 0.36: Analysis 2.5). rPMS plus rehabilitation slightly reduced spasticity of the elbow compared with sham plus rehabilitation at the end of follow‐up (two weeks after treatment phase) (MD ‐0.48, 95% CI ‐0.93 to ‐0.03). We found no differences between the rPMS plus rehabilitation group and the sham plus rehabilitation group in spasticity of the wrist at the end of follow‐up (two weeks after treatment phase) (MD ‐0.13, 95% CI ‐0.67 to 0.41; Analysis 2.6).
2.5. Analysis.
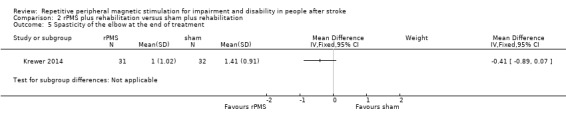
Comparison 2 rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 5 Spasticity of the elbow at the end of treatment.
2.6. Analysis.
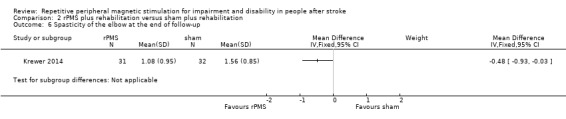
Comparison 2 rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 6 Spasticity of the elbow at the end of follow‐up.
Werner 2016 evaluated spasticity at the wrist and at the metatarsophalangeal (MCP) joints at 5, 30, 60, and 90 minutes following a single session of rPMS or sham plus stretch for five minutes. This study used a cross‐over design, and we could not obtain the spasticity score at the first phase in each group.
Others
No study reported lower limb function and muscle strength. None of the included trials reported adverse events including death associated with rPMS.
Comparison 4. rPMS plus rehabilitation versus rehabilitation only
We found no studies that performed this comparison.
Discussion
Summary of main results
We found four trials (139 participants) that were eligible for inclusion in the review. We did not find high risk of bias across these trials, and we determined that the overall risk of bias was low. Only one randomised controlled trial (RCT) (63 participants) reported the effects of repetitive peripheral magnetic stimulation (rPMS) on activities of daily living and showed that rPMS was not associated with a significant increase in the Barthel Index score (see Table 3). Two studies compared rPMS versus sham (Beaulieu 2015; Zifko 2002). Two studies compared rPMS plus rehabilitation versus sham plus rehabilitation (Krewer 2014; Werner 2016). Only one study conducted multiple stimulation sessions as part of treatment (Krewer 2014). Investigators reported spasticity, muscle strength, and upper limb function as secondary outcomes. Two studies reported significant reduction in spasticity (Krewer 2014; Zifko 2002). One of these studies reported the significant difference in spasticity of the elbow at the end of follow‐up (mean difference (MD) ‐0.48, 95% confidence interval (CI) ‐0.93 to ‐0.03) (Krewer 2014). No studies reported significant improvement in strength. Two studies reported upper limb function (Krewer 2014; Zifko 2002): one study did not find significant improvement (Krewer 2014), but the other study reported significant improvement (Zifko 2002). None of the included studies reported adverse events including death.
Overall completeness and applicability of evidence
The included trials did not provide sufficient information for review authors to address the aim of our review. Only four trials contributed data to our review, and three of these were individual RCTs. Additionally, we identified one cross‐over placebo‐controlled trial. We contacted the authors of this cross‐over trial, but as we received no response, we could not include this study in our analysis. Stimulation parameters (frequency, intensity, pulses) and mean time from onset also varied across studies. Two studies included not only participants after stroke, but also participants after traumatic brain injury. These differences might affect the accuracy of our results. Sample sizes of the studies were small, ranging from 18 to 63 participants, which may have led to insufficient statistical power to detect differences. Large‐scale RCTs are needed to verify the efficacy of rPMS. Most of the included trials assessed the outcome at the end of the treatment period or within several weeks after treatment. Whether rPMS had long‐term effects on functional recovery is unclear.
Quality of the evidence
Overall risk of bias was low. All studies reported blinding, so we were able to make a clear decision about performance bias. However, all included studies had relatively small sample sizes: 18 participants in Beaulieu 2015 and Zifko 2002, 63 in Krewer 2014, and 40 in Werner 2016. We downgraded the quality of evidence related to the primary outcome, mainly because one study had a small sample size with the 95% CI overlapping zero (Table 1).
Potential biases in the review process
Despite our extensive literature search, selection bias may have occurred. Although two review authors independently assessed eligibility of studies for inclusion, along with risks of bias to minimise potential bias in this review, we were required to make several subjective judgements during the review process. A different review team may judge risk of bias differently.
Agreements and disagreements with other studies or reviews
Two previous reviews have investigated the effectiveness of rPMS treatment (Beaulieu 2013; Beaulieu 2015b). Beaulieu 2013 summarised the results of 13 studies that used different types of outcomes (neurophysiological, biomechanical, clinical) in healthy individuals and in people with stroke or a spinal disorder. This review included quasi‐experimental studies and case studies and conducted no pooled analysis. The review authors reported that owing to limited evidence, they could reach no conclusion. Beaulieu 2015b dealt with stimulation parameters reported in any scientific research that applied rPMS as an intervention to improve somatosensory or motor disorders. The literature search yielded 24 studies on various pathological disorders. The review authors conducted no pooled analysis and concluded that future studies required a more structured design and larger samples. Similarly, our review assessed RCTs with small sample sizes that focused on clinical outcomes after stroke and found lack of sufficient evidence for effectiveness of rPMS.
An RCT that investigated the effects of low‐frequency repetitive transcranial magnetic stimulation on 112 participants after stroke showed significant improvement in ADLs after four‐week treatment (Zheng 2015). However, our review on rPMS for ADL with 63 participants did not show significant improvement in ADL. One reason for this might be the difference in targets of stimulation (transcranial or peripheral).
Authors' conclusions
Implications for practice.
To date, evidence is still insufficient to allow generalisable conclusions about the effects of rPMS for people with stroke. Routine use of rPMS for stroke cannot be supported even by the results of this updated review.
Implications for research.
We found more ongoing RCTs on this topic for this review than for the first review; these studies could involve larger numbers of participants and study findings could change known results on effects of rPMS and on quality of evidence in the future. Future studies with large sample sizes are needed to validate rPMS in people after stroke. In addition, the most optimal rPMS protocol (eligible participants, intensity, duration, and frequency) and long‐term effects of rPMS should be investigated for each outcome.
What's new
| Date | Event | Description |
|---|---|---|
| 7 January 2019 | New citation required but conclusions have not changed | Conclusions unchanged. Changes made to authorship |
| 7 January 2019 | New search has been performed | Three studies (121 participants) were included in the 2017 version of this review. We added 1 study (18 participants) to this updated review. The total number of included studies is 4 (139 participants). The study added to this update review was not included in the meta‐analysis |
Acknowledgements
We thank Hazel Fraser from the Cochrane Stroke Group for providing relevant information, and Joshua David Cheyne for helping to develop the search strategy and for conducting searches.
Appendices
Appendix 1. Cochrane Central Register of Controlled Trials (CENTRAL) search strategy
#1 [mh ^"cerebrovascular disorders"] or [mh "basal ganglia cerebrovascular disease"] or [mh "brain ischemia"] or [mh "carotid artery diseases"] or [mh "intracranial arterial diseases"] or [mh "intracranial arteriovenous malformations"] or [mh "intracranial embolism and thrombosis"] or [mh "intracranial hemorrhages"] or [mh ^stroke] or [mh "brain infarction"] or [mh ^"stroke, lacunar"] or [mh ^"vasospasm, intracranial"] or [mh ^"vertebral artery dissection"] or [mh ^"brain injuries"] or [mh ^"brain injury, chronic"] #2 (stroke or poststroke or post‐stroke or cerebrovasc* or brain next vasc* or cerebral next vasc* or cva* or apoplex* or SAH):ti,ab,kw (Word variations have been searched) #3 ((brain or cerebr* or cerebell* or vertebrobasil* or hemispher* or intracran* or intracerebral or infratentorial or supratentorial or middle cerebral artery or MCA* or anterior circulation or posterior circulation or basilar artery or vertebral artery or space‐occupying) near/5 (isch?emi* or infarct* or thrombo* or emboli* or occlus* or hypoxi*)):ti,ab,kw (Word variations have been searched) #4 ((brain* or cerebr* or cerebell* or intracerebral or intracran* or parenchymal or intraparenchymal or intraventricular or infratentorial or supratentorial or basal gangli* or putaminal or putamen or posterior fossa or hemispher* or subarachnoid) near/5 (h?emorrhag* or h?ematoma$ or bleed*)):ti,ab,kw (Word variations have been searched) #5 [mh ^hemiplegia] or [mh paresis] #6 (hempar* or hemipleg* or paresis or paraparesis or paretic):ti,ab,kw (Word variations have been searched) #7 {or #1‐#6} #8 [mh ^"magnetic field therapy"] #9 [mh ^magnetics] #10 [mh ^"electromagnetic fields"] or [mh ^"electromagnetic phenomena"] or [mh ^"magnetic fields"] #11 ((magnet* or electromagnet* or electro‐magnet*) near/5 (field* or coil* or induction)):ti,ab,kw (Word variations have been searched) #12 ((peripher* or nerv* or musc* or spine or spinal) near/5 (magnet* or electromagnet* or electro‐magnet*) near/5 (stimulat* or neurostimulat*)):ti,ab,kw (Word variations have been searched) #13 (PMS or rPMS or PrMS):ti,ab,kw (Word variations have been searched) #14 {or #8‐#13} #15 #7 and #14
Appendix 2. MEDLINE (Ovid) search strategy
1. cerebrovascular disorders/ or exp basal ganglia cerebrovascular disease/ or exp brain ischemia/ or exp carotid artery diseases/ or exp cerebral small vessel diseases/ or exp intracranial arterial diseases/ or exp "intracranial embolism and thrombosis"/ or exp intracranial hemorrhages/ or stroke/ or exp brain infarction/ or stroke, lacunar/ or vasospasm, intracranial/ or vertebral artery dissection/
2. (stroke$ or poststroke or apoplex$ or cerebral vasc$ or brain vasc$ or cerebrovasc$ or cva$ or SAH).tw.
3. ((brain or cerebr$ or cerebell$ or vertebrobasil$ or hemispher$ or intracran$ or intracerebral or infratentorial or supratentorial or middle cerebral artery or MCA$ or anterior circulation or posterior circulation or basilar artery or vertebral artery or space‐occupying) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$ or hypoxi$)).tw.
4. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracran$ or parenchymal or intraparenchymal or intraventricular or infratentorial or supratentorial or basal gangli$ or putaminal or putamen or posterior fossa or hemispher$ or subarachnoid) adj5 (h?emorrhag$ or h?ematoma$ or bleed$)).tw.
5. hemiplegia/ or exp paresis/ or exp Gait Disorders, Neurologic/
6. (hemipleg$ or hemipar$ or paresis or paraparesis or paretic).tw.
7. or/1‐6
8. magnetic field therapy/
9. magnetics/
10. electromagnetic fields/ or electromagnetic phenomena/ or magnetic fields/
11. ((magnet$ or electromagnet$ or electro‐magnet$) adj5 (field$ or coil$ or induction)).tw.
12. ((peripher$ or nerv$ or musc$ or spine or spinal) adj5 (magnet$ or electromagnet$ or electro‐magnet$) adj5 (stimulat$ or neurostimulat$)).tw.
13. (PMS or rPMS or PrMS).tw.
14. 8 or 9 or 10 or 11 or 12 or 13
15. 7 and 14
16. Randomized Controlled Trials as Topic/
17. random allocation/
18. Controlled Clinical Trials as Topic/
19. control groups/
20. clinical trials as topic/ or clinical trials, phase i as topic/ or clinical trials, phase ii as topic/ or clinical trials, phase iii as topic/ or clinical trials, phase iv as topic/
21. double‐blind method/
22. single‐blind method/
23. Placebos/
24. placebo effect/
25. cross‐over studies/
26. randomized controlled trial.pt.
27. controlled clinical trial.pt.
28. (clinical trial or clinical trial phase i or clinical trial phase ii or clinical trial phase iii or clinical trial phase iv).pt.
29. (random$ or RCT or RCTs).tw.
30. (controlled adj5 (trial$ or stud$)).tw.
31. (clinical$ adj5 trial$).tw.
32. ((control or treatment or experiment$ or intervention) adj5 (group$ or subject$ or patient$)).tw.
33. (quasi‐random$ or quasi random$ or pseudo‐random$ or pseudo random$).tw.
34. ((control or experiment$ or conservative) adj5 (treatment or therapy or procedure or manage$)).tw.
35. ((singl$ or doubl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).tw.
36. (cross‐over or cross over or crossover).tw.
37. (placebo$ or sham).tw.
38. trial.ti.
39. (assign$ or allocat$).tw.
40. controls.tw.
41. or/16‐40
42. 15 and 41
43. exp animals/ not humans.sh.
44. 42 not 43
Appendix 3. Embase (Ovid) search strategy
1. cerebrovascular disease/ or brain disease/ or exp basal ganglion hemorrhage/ or exp brain hemangioma/ or exp brain hematoma/ or exp brain hemorrhage/ or exp brain infarction/ or exp brain ischemia/ or exp carotid artery disease/ or exp cerebral artery disease/ or exp cerebrovascular accident/ or exp cerebrovascular malformation/ or exp intracranial aneurysm/ or exp occlusive cerebrovascular disease/ or exp vertebrobasilar insufficiency/
2. (stroke$ or poststroke or apoplex$ or cerebral vasc$ or brain vasc$ or cerebrovasc$ or cva$ or SAH).tw.
3. ((brain or cerebr$ or cerebell$ or vertebrobasil$ or hemispher$ or intracran$ or intracerebral or infratentorial or supratentorial or middle cerebral artery or MCA$ or anterior circulation or posterior circulation or basilar artery or vertebral artery or space‐occupying) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$ or hypoxi$)).tw.
4. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracran$ or parenchymal or intraparenchymal or intraventricular or infratentorial or supratentorial or basal gangli$ or putaminal or putamen or posterior fossa or hemispher$ or subarachnoid) adj5 (h?emorrhag$ or h?ematoma$ or bleed$)).tw.
5. exp hemiplegia/ or exp paresis/
6. (hemipleg$ or hemipar$ or paresis or paraparesis or paretic).tw.
7. or/1‐6
8. magnetotherapy/
9. exp magnetic field/ or exp magnetism/
10. ((magnet$ or electromagnet$ or electro‐magnet$) adj5 (field$ or coil$ or induction)).tw.
11. ((peripher$ or nerv$ or musc$ or spine or spinal) adj5 (magnet$ or electromagnet$ or electro‐magnet$) adj5 (stimulat$ or neurostimulat$)).tw.
12. (PMS or rPMS or PrMS).tw.
13. or/8‐12
14. Randomized Controlled Trial/ or "randomized controlled trial (topic)"/
15. Randomization/
16. Controlled clinical trial/ or "controlled clinical trial (topic)"/
17. control group/ or controlled study/
18. clinical trial/ or "clinical trial (topic)"/ or phase 1 clinical trial/ or phase 2 clinical trial/ or phase 3 clinical trial/ or phase 4 clinical trial/
19. Crossover Procedure/
20. Double Blind Procedure/
21. Single Blind Procedure/ or triple blind procedure/
22. placebo/ or placebo effect/
23. (random$ or RCT or RCTs).tw.
24. (controlled adj5 (trial$ or stud$)).tw.
25. (clinical$ adj5 trial$).tw.
26. ((control or treatment or experiment$ or intervention) adj5 (group$ or subject$ or patient$)).tw
27. ((control or experiment$ or conservative) adj5 (treatment or therapy or procedure or manage$)).tw.
28. ((singl$ or doubl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).tw.
29. (cross‐over or cross over or crossover).tw.
30. (placebo$ or sham).tw.
31. trial.ti.
32. (assign$ or allocat$).tw.
33. controls.tw.
34. or/14‐33
35. 7 and 13 and 34
36. (exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/) not (human/ or normal human/ or human cell/)
37. 35 not 36
Appendix 4. CINAHL (EBSCO) search strategy
S1 (MH "Cerebrovascular Disorders") OR (MH "Basal Ganglia Cerebrovascular Disease+") OR (MH "Carotid Artery Diseases+") OR (MH "Cerebral Ischemia+") OR (MH "Cerebral Vasospasm") OR (MH "Intracranial Arterial Diseases+") OR ( (MH "Intracranial Embolism and Thrombosis") ) OR (MH "Intracranial Hemorrhage+") OR (MH "Stroke") OR (MH "Vertebral Artery Dissections") OR (MH "Stroke Patients") OR (MH "Stroke Units")
S2 TI ( stroke or poststroke or post‐stroke or cerebrovasc* or brain vasc* or cerebral vasc or cva or apoplex or SAH ) or AB ( stroke or poststroke or post‐stroke or cerebrovasc* or brain vasc* or cerebral vasc or cva or apoplex or SAH)
S3 TI ( brain* or cerebr* or cerebell* or intracran* or intracerebral ) or AB ( brain* or cerebr* or cerebell* or intracran* or intracerebral)
S4 TI ( ischemi* or ischaemi* or infarct* or thrombo* or emboli* or occlus* ) or AB ( ischemi* or ischaemi* or infarct* or thrombo* or emboli* or occlus*)
S5 S3 AND S4
S6 TI ( brain* or cerebr* or cerebell* or intracerebral or intracranial or subarachnoid ) or AB ( brain* or cerebr* or cerebell* or intracerebral or intracranial or subarachnoid)
S7 TI ( haemorrhage* or hemorrhage* or haematoma* or hematoma* or bleed* ) or AB ( haemorrhage* or hemorrhage* or haematoma* or hematoma* or bleed*)
S8 S6 AND S7
S9 S1 OR S2 OR S5 OR S8
S10 (MH "Magnetics+") OR (MH "Magnet Therapy+") OR (MH "Magnets")
S11 TI ((magnet* or electromagnet* or electro‐magnet*) N5 (field* or coil* or induction)) OR AB ((magnet* or electromagnet* or electro‐magnet*) N5 (field* or coil* or induction))
S12 TI ((peripher* or nerv* or musc* or spine or spinal) N5 (magnet* or electromagnet* or electro‐magnet*) N5 (stimulat* or neurostimulat*)) or AB ((peripher* or nerv* or musc* or spine or spinal) N5 (magnet* or electromagnet* or electro‐magnet*) N5 (stimulat* or neurostimulat*))
S13 TI (PMS or rPMS or PrMS) or AB ( PMS or rPMS or PrMS)
S14 S10 OR S11 OR S12 OR S13
S15 (MH "Randomized Controlled Trials") or (MH "Random Assignment") or (MH "Random Sample+")
S16 (MH "Clinical Trials") or (MH "Intervention Trials") or (MH "Therapeutic Trials")
S17 (MH "Double‐Blind Studies") or (MH "Single‐Blind Studies") or (MH "Triple‐Blind Studies")
S18 (MH "Control (Research)") or (MH "Control Group") or (MH "Placebos") or (MH "Placebo Effect")
S19 (MH "Crossover Design") OR (MH "Quasi‐Experimental Studies")
S20 PT (clinical trial or randomized controlled trial)
S21 TI (random* or RCT or RCTs) or AB (random* or RCT or RCTs)
S22 TI (controlled N5 (trial* or stud*)) or AB (controlled N5 (trial* or stud*))
S23 TI (clinical* N5 trial*) or AB (clinical* N5 trial*)
S24 TI ((control or treatment or experiment* or intervention) N5 (group* or subject* or patient*)) or AB ((control or treatment or experiment* or intervention) N5 (group* or subject* or patient*))
S25 ((control or experiment* or conservative) N5 (treatment or therapy or procedure or manage*)) or AB ((control or experiment* or conservative) N5 (treatment or therapy or procedure or manage*))
S26 TI ((singl* or doubl* or tripl* or trebl*) N5 (blind* or mask*)) or AB ((singl* or doubl* or tripl* or trebl*) N5 (blind* or mask*))
S27 TI (cross‐over or cross over or crossover) or AB (cross‐over or cross over or crossover)
S28 TI (placebo* or sham) or AB (placebo* or sham)
S29 TI trial
S30 TI (assign* or allocat*) or AB (assign* or allocat*)
S31 TI controls or AB controls
S32 S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31
S34 S9 AND S14 AND S32
Appendix 5. PsycINFO (Ovid) search strategy
1. cerebrovascular disorders/ or cerebral hemorrhage/ or exp cerebral ischemia/ or cerebral small vessel disease/ or cerebrovascular accidents/ or subarachnoid hemorrhage/
2. (stroke$ or poststroke or apoplex$ or cerebral vasc$ or brain vasc$ or cerebrovasc$ or cva$ or SAH).tw.
3. ((brain or cerebr$ or cerebell$ or vertebrobasil$ or hemispher$ or intracran$ or intracerebral or infratentorial or supratentorial or middle cerebral artery or MCA$ or anterior circulation or posterior circulation or basilar artery or vertebral artery or space‐occupying) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$ or hypoxi$)).tw.
4. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracran$ or parenchymal or intraparenchymal or intraventricular or infratentorial or supratentorial or basal gangli$ or putaminal or putamen or posterior fossa or hemispher$ or subarachnoid) adj5 (h?emorrhag$ or h?ematoma$ or bleed$)).tw.
5. hemiparesis/ or hemiplegia/
6. (hemipleg$ or hemipar$ or paresis or paretic).tw.
7. or/1‐6
8. exp magnetism/
9. ((magnet$ or electromagnet$ or electro‐magnet$) adj5 (field$ or coil$ or induction)).tw.
10. ((peripher$ or nerv$ or musc$ or spine or spinal) adj5 (magnet$ or electromagnet$ or electro‐magnet$) adj5 (stimulat$ or neurostimulat$)).tw.
11. (PMS or rPMS or PrMS).tw.
12. or/8‐11
13. clinical trials/ or treatment effectiveness evaluation/ or placebo/
14. (random$ or RCT or RCTs).tw.
15. (controlled adj5 (trial$ or stud$)).tw.
16. (clinical$ adj5 trial$).tw.
17. ((control or treatment or experiment$ or intervention) adj5 (group$ or subject$ or patient$)).tw
18. ((control or experiment$ or conservative) adj5 (treatment or therapy or procedure or manage$)).tw.
19. ((singl$ or doubl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).tw.
20. (cross‐over or cross over or crossover).tw.
21. (placebo$ or sham).tw.
22. trial.ti.
23. (assign$ or allocat$).tw.
24. controls.tw.
25. or/13‐24
26. 7 and 12 and 25
Appendix 6. AMED (Ovid) search strategy
1. cerebrovascular disorders/ or cerebral hemorrhage/ or cerebral infarction/ or cerebral ischemia/ or cerebrovascular accident/ or stroke/ or brain injuries/
2. (stroke$ or poststroke or apoplex$ or cerebral vasc$ or brain vasc$ or cerebrovasc$ or cva$ or SAH).tw.
3. ((brain or cerebr$ or cerebell$ or vertebrobasil$ or hemispher$ or intracran$ or intracerebral or infratentorial or supratentorial or middle cerebral artery or MCA$ or anterior circulation or posterior circulation or basilar artery or vertebral artery or space‐occupying) adj5 (isch?emi$ or infarct$ or thrombo$ or emboli$ or occlus$ or hypoxi$)).tw.
4. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracran$ or parenchymal or intraparenchymal or intraventricular or infratentorial or supratentorial or basal gangli$ or putaminal or putamen or posterior fossa or hemispher$ or subarachnoid) adj5 (h?emorrhag$ or h?ematoma$ or bleed$)).tw.
5. hemiplegia/
6. (hemipleg$ or hemipar$ or paresis or paretic or brain injur$).tw.
7. or/1‐6
8. exp magnetics/
9. exp electromagnetics/ or exp electromagnetic fields/
10. ((magnet$ or electromagnet$ or electro‐magnet$) adj5 (field$ or coil$ or induction)).tw.
11. ((peripher$ or nerv$ or musc$ or spine or spinal) adj5 (magnet$ or electromagnet$ or electro‐magnet$) adj5 (stimulat$ or neurostimulat$)).tw.
12. (PMS or rPMS or PrMS).tw.
13. or/8‐12
14. clinical trials/ or randomized controlled trials/ or random allocation/
15. research design/ or comparative study/
16. double blind method/ or single blind method/
17. placebos/
18. (random$ or RCT or RCTs).tw.
19. (controlled adj5 (trial$ or stud$)).tw.
20. (clinical$ adj5 trial$).tw.
21. ((control or treatment or experiment$ or intervention) adj5 (group$ or subject$ or patient$)).tw.
22. ((control or experiment$ or conservative) adj5 (treatment or therapy or procedure or manage$)).tw.
23. ((singl$ or doubl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).tw.
24. (cross‐over or cross over or crossover).tw.
25. (placebo$ or sham).tw.
26. trial.ti.
27. (assign$ or allocat$).tw.
28. controls.tw.
29. or/14‐28
30. 7 and 13 and 29
Appendix 7. OTseeker (Occupational Therapy Systematic Evaluation of Evidence) search strategy
[Any Field] like 'stroke* or poststroke or apoplex* or cerebral vasc* or brain vasc* or cerebrovasc* or cva* or SAH' AND [Any Field] like 'magnet* or electromagnet* or electro‐magnet*' AND [Method] like 'Randomised controlled trial'
Appendix 8. PEDro (physiotherapy evidence database) search strategy
<electrotherapies, heat, cold> in “Therapy” field, <muscle weakness> in “Problem” field. <neurology> in "Subdiscipline" field, and <clinical trial> in "Method" field
Appendix 9. Ichushi‐Web (Japanese medical database) search strategy
(脳卒中/AL or 脳梗塞/AL or 脳出血/AL or クモ膜下出血/AL or 脳血管障害/AL) and (磁気/AL) and (臨床試験/AL or 比較試験/AL or ランダム化比較試験/AL or 準ランダム化比較試験/AL or 第I相試験/AL or 第II相試験/AL or 第III相試験/AL or 第IV相試験/AL or 盲検/AL or ランダム/AL or プラセボ/AL or 対照群/AL or コントロール群/AL)
(We used Japanese characters in the search.)
Appendix 10. US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov
(stroke* OR poststroke OR apoplex* OR "cerebral vascular" OR "brain vascular*" OR cerebrovascular* OR "transient ischemic" OR tia OR cva* OR SAH) AND (magnetic OR electromagnetic OR electro‐magnetic OR PMS OR rPMS OR PrMS) | Interventional Studies
Appendix 11. ISRCTN Registry
(cerebrovascular OR stroke OR TIA OR SAH OR "transient ischemic attack" OR (cerebral AND (ischemia OR ischemia OR embolism OR infarction OR haematoma OR hematoma OR haemorrhage OR hemorrhage))) AND magnet*
Appendix 12. Stroke Trials Registry
Intervention ; Clinical Trials:“Magnetic”
Appendix 13. World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP)
stroke or poststroke or apoplex or cerebral vasc or brain vasc or cerebrovasc or transient ischemic or tia or cva or SAH – Title AND magnetic OR electromagnetic OR electro‐magnetic OR PMS OR rPMS OR PrMS ‐ Intervention
Appendix 14. Japanese UMIN Clinical Trials Registry (UMIN‐CTR)
Study type: Intervention:“Magnetic”
Appendix 15. Japan Registry of Clinical Trials (jRCT)
Intervention: “Magnetic”
Data and analyses
Comparison 1. rPMS versus sham.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Muscle strength at the end of treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only |
Comparison 2. rPMS plus rehabilitation versus sham plus rehabilitation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Activities of daily living at the end of treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2 Activities of daily living at the end of follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3 Upper limb function at the end of treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4 Upper limb function at the end of follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5 Spasticity of the elbow at the end of treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6 Spasticity of the elbow at the end of follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7 Spasticity of the wrist at the end of treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8 Spasticity of the wrist at the end of follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only |
2.7. Analysis.
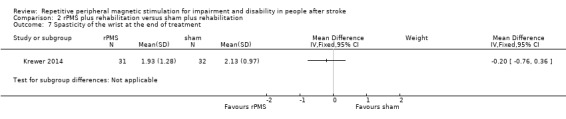
Comparison 2 rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 7 Spasticity of the wrist at the end of treatment.
2.8. Analysis.
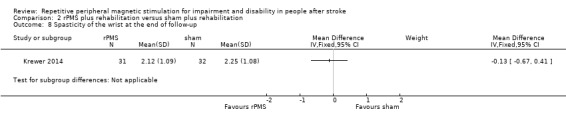
Comparison 2 rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 8 Spasticity of the wrist at the end of follow‐up.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Beaulieu 2015.
| Methods |
Study design: RCT Study grouping: parallel groups |
|
| Participants |
Inclusion criteria: chronic unilateral, first‐ever stroke more than 12 months before the start of the study. Participants with stroke presented with paretic ankle muscles with spasticity (medical records), had a CT or MRI scan taken within the previous 5 years, and were able to walk independently (i.e. with no physical assistance) more than 10 m with or without an assistive device Exclusion criteria: use of antispastic medication; past vertebral surgery; major circulatory, respiratory, or cardiac disease; neurological disease/deficit other than stroke; severe lower limb orthopaedic condition; or cognitive disorder Baseline characteristics Active rPMS (n = 9)
Sham rPMS (n = 9)
Baseline comparability between 2 groups: rPMS group was earlier from onset than sham group Loss to follow‐up: 0% |
|
| Interventions |
Intervention characteristics Active rPMS
Sham rPMS
Sham stimulation was applied using the same parameters but at a very low intensity |
|
| Outcomes | Muscle strength: dorsiflexion strength (kg)
|
|
| Identification |
Sponsorship source: Canadian Foundation for Innovation (CS) and studentships from the Fondsde la Recherche en Sante du Quebec (LDB, HMA) and the Canadian Institutes for Health Research (LDB, HMA) Country: Canada Setting: n/a Authors' names: Louis‐David Beaulieu, Hugo Masse‐Alarie, Brenda Brouwer, Cyril Schneider Institution: Laboratoire de Neurostimulation et Neurosciences Cliniques Email: cyril.schneider@rea.ulaval.ca Address: Centre de recherche du CHU de Quebec, Axe Neurosciences RC‐9800, 2705 Boulevard Laurier, Quebec, QC G1V 4G2, Canada |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | To ensure blinding, all participants were informed at enrolment that they could receive real rPMS or sham stimulation over the paretic lower limb, but they were not provided with information about the location of the coil nor sensations induced by stimulation |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Experimenters performing pre‐intervention and post‐intervention measures and analysis had to leave the room during the intervention and remained blind to group allocation during the experiments and to times of measurement during analysis (i.e. pre‐intervention or post‐intervention) until completion of analyses |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up 0% |
| Selective reporting (reporting bias) | Unclear risk | Protocol was not available |
| Other bias | Low risk | No other biases |
Krewer 2014.
| Methods |
Study design: RCT Study grouping: parallel groups |
|
| Participants |
Inclusion criteria: hemiparesis caused by stroke or traumatic brain injury; spasticity of an upper extremity, with a score of 1 to 3 on the Tardieu Scale; ages between 18 and 75 years Exclusion criteria: metal implant in the head or within the stimulation area; medically implanted device (cardiac pacemaker, cochlear implant, or medication pump); pregnancy; comorbidity with other neurodegenerative disorders or other neurological or orthopaedic disorders; increased intracranial pressure; unstable fracture of the paretic upper extremity Baseline characteristics Active rPMS plus rehabilitation (n = 31)
Sham rPMS plus rehabilitation (n = 32)
Baseline comparability between 2 groups: only rPMS groups included traumatic brain injury; rPMS group earlier from onset than sham group Loss to follow‐up: 0.05%; ITT analysis was performed |
|
| Interventions |
Intervention characteristics Active rPMS plus rehabilitation
Sham rPMS plus rehabilitation
|
|
| Outcomes | Activities of daily living: Barthel Index (scores range from 0 to 100)
Upper limb function: Fugl‐Meyer Assessment (scores range from 0 to 66)
Spasticity: Modified Tardieu Scale of elbow and wrist (scores range from 0 to 5)
|
|
| Identification |
Sponsorship source: n/a Country: Germany Setting: neurological rehabilitation hospital Authors' names: Carmen Krewer, Sandra Hartl, Friedemann Muller, Eberhard Koenig Institution: Schoen Klinik Bad Aibling, Motor Research Department, Bad Aibling, Germany Email: CKrewer@schoen‐kliniken.de Address: Schoen Klinik Bad Aibling, Kolbermoorer Strasse 72, D‐83043 Bad Aibling, Germany |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Low risk | Randomised allocation was done by an individual not involved in any other part of the study |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Active coil makes typical discharge noises. Blinding of participants and personnel was enough |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Trained therapists, blinded for treatment allocation, assessed each participant |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up 5%; no differences in reasons why outcome data were missing |
| Selective reporting (reporting bias) | Unclear risk | Protocol was not available |
| Other bias | Low risk | No other biases |
Werner 2016.
| Methods | Study design: cross‐over trial | |
| Participants |
Inclusion criteria: single history of CNS lesion due to stroke or traumatic brain injury; lesion interval > 12 months; increased muscle tone, i.e. 1, 2, 3, or 4 on the Modified Ashworth Score (0 to 5) in affected wrist or finger joints; no volitional distal motor function of the affected arm, except for mass flexion; no metal implants or open wounds in the stimulation area; no deep vein thrombosis; no relevant oedema; no pacemaker; no preceding botulinum toxin injection within previous 6 months; signed written informed consent (approved by local ethics committee) Exclusion criteria: n/a Baseline characteristics Group 1 (active rPMS plus rehabilitation‐sham rPMS plus rehabilitation) (n = 20)
Group 2 (sham rPMS plus rehabilitation‐active rPMS plus rehabilitation) (n = 20)
Baseline comparability between 2 groups: group 1 was younger than group 2 Loss to follow‐up: 0% |
|
| Interventions |
Intervention characteristics Active rPMS plus rehabilitation
Sham rPMS plus rehabilitation
|
|
| Outcomes | Spasticity: Modified Ashworth Score of wrist and finger (scores range from 0 to 4)
|
|
| Identification |
Sponsorship source: n/a Country: Germany Setting: n/a Comments: Verein zur Förderung der Hirnforschung und Rehabilitation, e.V., Berlin Authors' names: Werner C, Schrader M, Wernicke S, Bryl B, Hesse S Institution: Medical Park Berlin Humboldtmühle, Neurological Rehabilitation, Charité, University Medicine Berlin, Germany Email: c.werner@medicalpark.de Address: Medical Park Berlin Charité – University Medicine Berlin An der Mühle 2‐9, Berlin 13507, Germany |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was conducted with the help of a computer‐generated lot (www.randomizer.at) |
| Allocation concealment (selection bias) | Low risk | Before start of therapy, the subinvestigator of the study attached the rPMS or sham coil according to group assignment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | This study used a sham coil delivered with an atypical clicking sound. Therapists who applied stimulation and muscle stretch were not aware of whether the coil used was the one intended for rPMS or sham |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | A rater, blinded to treatment allocation, assessed participants |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up 0% |
| Selective reporting (reporting bias) | Unclear risk | Protocol was not available |
| Other bias | Low risk | No other biases |
Zifko 2002.
| Methods |
Study design: RCT Study grouping: parallel groups |
|
| Participants | 18 participants after stroke with spastic hemiparesis (mean age 60.8 years; 9 women, 9 men; 3 to 12 months after stroke) | |
| Interventions |
Intervention characteristics Active rPMS
Sham rPMS
|
|
| Outcomes | Upper limb function: angle of motion for hand extension and hand flexion (degree)
Upper limb function: Action Research Arm Test (scores range from 0 to 57 points)
Upper limb function: Bard and Hirschberg Score
Spasticity: Ashworth Score (scores range from 0 to 4)
Spasticity: Gerstenbrand Spasticity Rating Scale
|
|
| Identification |
Sponsorship source: n/a Country: Austria Setting: n/a Authors' names: Zifko UA, Morph M, Diem K, Havel PM, Struppler A Institution: Rehabilitationsklinik Pirawarth, Bad Pirawarth, Austria Email: n/a Address: n/a |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | The abstract states "double‐blind study". However, there was no information on blinding for personnel |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The abstract states "double‐blind study" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Loss to follow‐up 11% |
| Selective reporting (reporting bias) | Unclear risk | Protocol was not available |
| Other bias | Low risk | No other biases |
CNS: central nervous system. CT: computed tomography. ITT: intention‐to‐treat. MRI: magnetic resonance imaging. RCT: randomised controlled trial. rPMS: repetitive peripheral magnetic stimulation.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bernhardt 2007 | Unsuitable study design |
| Heldmann 2000 | Unsuitable outcomes |
| Kuznetsova 2016a | Unsuitable outcomes |
| Kuznetsova 2016b | Unsuitable outcomes |
| Momosaki 2014 | Unsuitable outcomes |
| Rossini 2005 | Unsuitable intervention |
| Struppler 2002 | Unsuitable study design |
| Struppler 2009 | Unsuitable study design |
Characteristics of studies awaiting assessment [ordered by study ID]
Kotchetkov 1999.
| Methods | Unknown |
| Participants | Participants with stroke |
| Interventions | Low‐frequency magnetic fields |
| Outcomes | Spasticity |
| Notes | — |
Kuznetsova 2013.
| Methods | Comparative study |
| Participants | 42 participants with stroke (mean age 64 ± 1.0 years) |
| Interventions | 10 daily sessions of 1 Hz repetitive transcranial magnetic stimulation and repetitive peripheral magnetic stimulation |
| Outcomes | Motor Club Assessment Scale |
| Notes | — |
Samosiuk 2003.
| Methods | Comparative study |
| Participants | 121 participants with ischaemic stroke in the acute period |
| Interventions | Technique of frequency‐modulated magnetolaser therapy |
| Outcomes | n/a |
| Notes | — |
Characteristics of ongoing studies [ordered by study ID]
DRKS00007722.
| Trial name or title | The effect of repetitive peripheral magnetic stimulation in stroke‐rehabilitation: a randomised controlled trial |
| Methods | RCT |
| Participants |
Inclusion criteria: subacute stroke (occurred no longer than 6 months previously); spastic hemiparesis of the upper limb (at least modified Ashworth Scale 1); slight function in the fingers or hand (at least 1 point on the Fugl‐Meyer Test in subscore C) Exclusion criteria: epilepsy, implanted metal in the stimulation area, implanted medical devices, dysfunctional speech comprehension, pregnancy |
| Interventions | Stimulation intensity is adjusted individually for each participant, so that a joint movement results from the muscle contraction. Muscles of the upper arm and forearm are stimulated with a butterfly coil; the participant takes a sitting position with raised feet in the wheelchair or on a chair with backrest; the arm is placed to be stimulated or maintained by the therapist |
| Outcomes | Primary outcome: group difference in the Fugl‐Meyer score 3 weeks post stimulation Secondary outcome: group difference in the Katz Index of Independence Activities of Daily Living Scale score after 6 months |
| Starting date | 23 September 2014 |
| Contact information | Kristin Pohl, Moritz Klinik Bad Klosterlausnitz, Hermann‐Sachse‐Straße 46 07639 Bad Klosterlausnitz Germany Email: kristin.pohl@moritz‐klinik.de |
| Notes | DRK00007722 |
DRKS00007899.
| Trial name or title | The effects of repetitive peripheral magnetic stimulation in patient with spastic hemiparesis after stroke: a randomised‐controlled study |
| Methods | RCT |
| Participants |
Inclusion criteria: subacute stroke (occurred no longer than 6 months previously); spastic hemiparesis of the upper limb (at least modified Ashworth Scale 1); slight function in the fingers or hand (at least 1 point on the Fugl‐Meyer Test in subscore C) Exclusion criteria: epilepsy, implanted metal in the stimulation area, implanted medical devices, dysfunctional speech comprehension, pregnancy |
| Interventions | Stimulation is 15 minutes daily for 3 weeks for a total of 15 sessions. Stimulation intensity is adjusted individually for each participant, so that a joint movement results from the muscle contraction. Muscles of the upper arm and forearm are stimulated with a butterfly coil. Participant takes a sitting position with raised feet in a wheelchair or on a chair with a backrest. The arm is then placed to be stimulated or maintained by the therapist |
| Outcomes | Primary outcome: Fugl‐Meyer Test of the upper extremity ‐ a test that evaluated the function of the affected upper extremity. This test will be performed directly after the end of the 3 weeks of intervention/control intervention Secondary outcome: Katz Index of Independence Activities of Daily Living questionnaire. This questionnaire aims to identify dependence on performance of activities of daily living and will be performed 6 months after the end of the intervention/control intervention |
| Starting date | 15 April 2015 |
| Contact information | Kristin Pohl, Moritz Klinik Bad Klosterlausnitz, Hermann‐Sachse‐Straße 46 07639 Bad Klosterlausnitz, Germany Email: kristin.pohl@moritz‐klinik.de |
| Notes | DRKS00007899 |
jRCTs042180014.
| Trial name or title | Immediate effect of simple magnetic stimulation for upper limb spasticity: a randomised‐controlled trial |
| Methods | RCT |
| Participants |
Inclusion criteria: adults after stroke with modified Ashworth Scale score of 1+ or more in the metacarpophalangeal joint (MP), wrist, or elbow flexor muscles Exclusion criteria: unstable condition and/or patients who used cardiac pacemaker |
| Interventions | 15 minutes of magnetic stimulation for spastic muscles |
| Outcomes |
Primary outcome: changes in spasticity evaluated by the modified Ashworth Scale Secondary outcomes: modified Ashworth Scale score and subjective symptoms of participants at 24 hours before, just before, just after, 1 hour after, 24 hours after stimulation |
| Starting date | 1 November 2018 |
| Contact information | Hitoshi Kagaya, Fujita Health University Hospital, 1‐98 Dengakugakubo, Kutsukake, Toyoake, Aichi, Japan email:hkagaya2@fujita‐hu.ac.jp |
| Notes | jRCTs042180014 |
UMIN000018750.
| Trial name or title | Repetitive peripheral magnetic stimulation for patients with hemiplegia |
| Methods | RCT |
| Participants | Inclusion criteria: cerebral hemisphere damage, people who could walk independently, modified Rankin Scale between 0 and 2 before onset Exclusion criteria: severe dementia, people with contraindications outlined in the guidelines for repetitive transcranial magnetic stimulation |
| Interventions | Repetitive peripheral magnetic stimulation + standard physical therapy Repetitive peripheral magnetic stimulation: while participants are participating in this study, they receive repetitive peripheral magnetic stimulation on the day they perform physical therapy. Repetitive peripheral magnetic stimulation is performed on the quadriceps femoris at 30 Hz for 10 minutes. Standard physical therapy is performed according to the standard schedule of the authors' hospital |
| Outcomes | Knee extension strength, evaluation time: at the time of starting physical therapy, 1 week later, 2 weeks later, 1 month later, 2 months later Stroke Impairment Assessment Set, 10‐meter walking speed, Functional Independence Measure, quadriceps muscle thickness, acceleration during walking, Berg Balance Scale, Timed Up and Go Test, biochemical blood test, number of days until gait reacquisition, hospitalisation |
| Starting date | 1 October 2015 |
| Contact information | Keita Suzuki, Kawasaki University of Medical Welfare, Department of Rehabilitation, 288 Matsushima, Kurashiki, Okayama, Japan Email: suzuki@mw.kawasaki‐m.ac.jp |
| Notes | UMIN000018750 |
UMIN000019106.
| Trial name or title | Effect of pairing peripheral and transcranial magnetic stimulations triggered by actual movement on motor plasticity |
| Methods | Cross‐over trial |
| Participants | Inclusion criteria: people with chronic stroke (more than 3 months after onset) who were inpatients and outpatients of Tohoku University Hospital Exclusion criteria: people with metal in cranium, trauma or operation of brain, intracardiac lines, increased intracranial pressure, pregnancy, childhood, heart disease, cardiac pacemaker, medication pump, tricyclic antidepressants, neuroleptics, febrile convulsion, epilepsy, family history of epilepsy |
| Interventions | Subthreshold peripheral and transcranial magnetic stimulations with actual movement |
| Outcomes | Direction of transcranial magnetic stimulation‐induced upper limb movement of the paretic side, excitability of corticospinal tract |
| Starting date | 1 October 2015 |
| Contact information | Akihiko Asao, Tohoku University Graduate School of Medicine, Department of Physical Medicine and Rehabilitation, 2‐1 Seiryo‐machi, Aoba‐ku, Sendai, Miyagi, Japan Email: a3omail@gmail.com |
| Notes | UMIN000019106 |
UMIN000031957.
| Trial name or title | Prevention of shoulder subluxation in stroke patients with magnetic stimulation: a randomised controlled trial |
| Methods | RCT |
| Participants |
Inclusion criteria: people with hemiplegia after stroke with stable general condition, aged 20 or older Exclusion criteria: history of epilepsy, cardiac pacemaker, difficulty in sitting position over 40 minutes, magnetic materials near the stimulation site, distance between acromion and humeral head more than 1/2 fingerbreadth, inpatients expected to discharge within 6 weeks, pregnant women |
| Interventions | 6 weeks of magnetic stimulation in addition to usual training: 20 minutes of stimulation per day, 5 days per week, plus physical therapy and occupational therapy |
| Outcomes |
Primary outcome: changes in humeral head position by X‐ray examination after 6‐week intervention Secondary outcomes: changes in motor function, joint range of motion, muscle strength, pain |
| Starting date | 1 April 2018 |
| Contact information | Kenta Fujimura, Fujita Health University, Faculty of Rehabilitation, School of Health Sciences, 1‐98 Dengakugakubo, Kutsukake, Toyoake, Aichi, Japan email: rehabmed@fujita‐hu.ac.jp |
| Notes | UMIN000031957 |
RCT: randomised controlled trial.
Differences between protocol and review
We divided our evaluation of spasticity into parts of the body (elbow and wrist), although this was not specified in the protocol. We used Covidence software for selection of studies, data extraction, and assessment of risk of bias (Covidence 2013). We included ADLs, upper limb function, lower limb function, muscle strength, spasticity, and death in the 'Summary of findings' tables.
Contributions of authors
Kotomi Sakai prepared the protocol and drafted the review with support from Ryo Momosaki. Yuichi Yasufuku and Tomohiko Kamo contributed to literature selection, data extraction, and analyses. Erika Ota provided critical revisions on this review . All review authors approved the final review.
Sources of support
Internal sources
No sources of support supplied
External sources
This research is supported by the Project for Baby and Infant in Research of Health and Development to Adolescent and Young Adult (BIRTHDAY), from the Japan Agency for Medical Research and Development, AMED, Japan.
Declarations of interest
Kotomi Sakai: none known.
Yuichi Yasufuku: none known.
Tomohiko Kamo: none known.
Erika Ota: none known.
Ryo Momosaki: none known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Beaulieu 2015 {published data only}
- Beaulieu L‐D, Masse‐Alarie H, Brouwer B, Schneider C. Noninvasive neurostimulation in chronic stroke: a double‐blind randomized sham‐controlled testing of clinical and corticomotor effects. Topics in Stroke Rehabilitation 2015;22(1):8‐17. [DOI] [PubMed] [Google Scholar]
Krewer 2014 {published data only}
- Krewer C, Hartl S, Muller F, Koenig E. Effects of repetitive peripheral magnetic stimulation on upper‐limb spasticity and impairment in patients with spastic hemiparesis: a randomized, double‐blind, sham‐controlled study. Archives of Physical Medicine and Rehabilitation 2014;95(6):1039‐47. [DOI] [PubMed] [Google Scholar]
Werner 2016 {published data only}
- Werner C, Schrader M. Repetitive peripheral magnetic stimulation (rpMS) in combination with muscle stretch decreased the wrist and finger flexor muscle spasticity in chronic patients after CNS lesion. International Journal of Physical Medicine and Rehabilitation 2016;4:4. [Google Scholar]
Zifko 2002 {published data only}
- Zifko U, Morph M, Diem K, Havel P, Struppler A. Repetitive peripheral magnetic stimulation is effective in the rehabilitation of the paretic arm. Neurorehabilitation and Neural Repair 2002;16(1):18‐9. [Google Scholar]
References to studies excluded from this review
Bernhardt 2007 {published data only}
- Bernhardt M, Angerer B, Buss M, Struppler A. Isometric muscle contraction induced by repetitive peripheral magnetic stimulation (RPMS)‐modeling and identification. Biomedical Signal Processing and Control 2007;2(3):180‐90. [Google Scholar]
Heldmann 2000 {published data only}
- Heldmann B, Kerkhoff G, Struppler A, Havel P, Jahn T. Repetitive peripheral magnetic stimulation alleviates tactile extinction. NeuroReport 2000;11(14):3193‐8. [DOI] [PubMed] [Google Scholar]
Kuznetsova 2016a {published data only}
- Kuznetsova S, Kuznetsov V, Skachkova N. Enhancement of cortical excitability and motor function in stroke patients after combined repetitive transcranial and peripheral magnetic stimulation. European Journal of Neurology 2016;23:223. [Google Scholar]
Kuznetsova 2016b {published data only}
- Kuznietsova S, Skachkova N, Semonova O. ID 243 – Enhancement of cortical excitability in stroke patients after combined repetitive transcranial and peripheral magnetic stimulation. Clinical Neurophysiology 2016;127(3):121. [Google Scholar]
Momosaki 2014 {published data only}
- Momosaki R, Abo M, Watanabe S, Kakuda W, Yamada N, Mochio K. Functional magnetic stimulation using a parabolic coil for dysphagia after stroke. Neuromodulation 2014;17(7):637‐641. [DOI] [PubMed] [Google Scholar]
Rossini 2005 {published data only}
- Rossini PM, Johnston CS. Facilitating acute stroke recovery with magnetic fields?. Neurology 2005;65(3):353‐4. [DOI] [PubMed] [Google Scholar]
Struppler 2002 {published data only}
- Struppler A, Havel P, Muller‐Barna P. Facilitation of skilled finger movements by repetitive peripheral magnetic stimulation (RPMS) ‐ a new approach in central paresis. NeuroRehabilitation 2002;18(1):69‐82. [PubMed] [Google Scholar]
Struppler 2009 {published data only}
- Struppler A, Angerer B, Gebhard B. Repetitive peripheral magnetic stimulation (RPMS) as a method for the rehabilitation of sensorimotor deficits of hand and arm following cerebral lesions. Neurologie und Rehabilitation 2009;15(1):28‐38. [Google Scholar]
References to studies awaiting assessment
Kotchetkov 1999 {published data only}
- Kotchetkov A Gorbunov F, Streltsova N, Fillina T. Spasticity modulation using low frequency magnetic fields (LFMF) in stroke patients. 2nd World Congress in Neurological Rehabilitation 1999;42:42. [Google Scholar]
Kuznetsova 2013 {published data only}
- Kuznetsova S, Kuznetsov V, Skachkova N. Combined central and peripheral magnetic stimulation to facilitate motor recovery after stroke. Cerebrovascular Diseases 2013;35 Suppl 3:548. [Google Scholar]
Samosiuk 2003 {published data only}
- Samosiuk NI. Magnetic and laser therapy of acute ischemic stroke. Voprosy Kurortologii, Fizioterapii, i Lechebnoi Fizicheskoi Kultury 2003;2:19‐20. [PubMed] [Google Scholar]
References to ongoing studies
DRKS00007722 {published data only}
- DRKS00007722. The effect of repetitive peripheral magnetic stimulation in stroke‐rehabilitation: a randomized controlled trial. https://www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00007722 (first reported 3 March 2015). [DRKS00007722]
DRKS00007899 {published data only}
- DRKS00007899. The effects of repetitive peripheral magnetic stimulation in patient with spastic hemiparesis after stroke: a randomized‐controlled study. https://www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00007899 (first reported 24 March 2015). [DRKS00007899]
jRCTs042180014 {published data only}
- jRCTs042180014. Immediate effect of simple magnetic stimulation for upper limb spasticity: a randomized‐controlled trial. https://rctportal.niph.go.jp/en/detail?trial_id=jRCTs042180014 (first reported 29 November 2018). [jRCTs042180014]
UMIN000018750 {published data only}
- UMIN000018750. Effect of repetitive peripheral magnetic stimulation for lower extremity of stroke patients with hemiplegia. https://upload.umin.ac.jp/cgi‐open‐bin/ctr/ctr.cgi?function=brows&action=brows&type=summary&recptno=R000021679&language=J (first reported 21 August 2015). [UMIN000018750]
UMIN000019106 {published data only}
- UMIN000019106. Effect of pairing peripheral and transcranial magnetic stimulations triggered by actual movement on motor plasticity. https://upload.umin.ac.jp/cgi‐open‐bin/ctr_e/ctr_view.cgi?recptno=R000022085 (first reported 1 October 2015). [UMIN000019106]
UMIN000031957 {published data only}
- UMIN000031957. Prevention of shoulder subluxation in stroke patients with magnetic stimulation: a randomized controlled trial. https://upload.umin.ac.jp/cgi‐open‐bin/ctr_e/ctr_view.cgi?recptno=R000036495 (first reported 29 March 2018). [UMIN000031957]
Additional references
Barker 1991
- Barker AT. An introduction to the basic principles of magnetic nerve stimulation. Journal of Clinical Neurophysiology 1991;8:26‐37. [DOI] [PubMed] [Google Scholar]
Beaulieu 2013
- Beaulieu LD, Schneider C. Effects of repetitive peripheral magnetic stimulation on normal or impaired motor control. A review. Clinical Neurophysiology 2013;43(4):251‐60. [DOI] [PubMed] [Google Scholar]
Beaulieu 2015b
- Beaulieu LD, Schneider C. Repetitive peripheral magnetic stimulation to reduce pain or improve sensorimotor impairments: a literature review on parameters of application and afferents recruitment. Neurophysiologie Clinique 2015;45(3):223‐37. [DOI] [PubMed] [Google Scholar]
Beaulieu 2017
- Beaulieu LD, Massé‐Alarie H, Camiré‐Bernier S, Ribot‐Ciscar É, Schneider C. After‐effects of peripheral neurostimulation on brain plasticity and ankle function in chronic stroke: the role of afferents recruited. Neurophysiologie Clinique 2017;47(4):275‐91. [DOI] [PubMed] [Google Scholar]
Covidence 2013 [Computer program]
- Melbourne, Australia: Veritas Health Innovation. Covidence systematic review software. Melbourne, Australia: Veritas Health Innovation, 2013.
De Vries 2007
- Vries S, Mulder T. Motor imagery and stroke rehabilitation: a critical discussion. Journal of Rehabilitation Medicine 2007;39(1):5‐13. [DOI] [PubMed] [Google Scholar]
Flamand 2014
- Flamand VH, Schneider C. Noninvasive and painless magnetic stimulation of nerves improved brain motor function and mobility in a cerebral palsy case. Archives of Physical Medicine and Rehabilitation 2014;95(10):1984‐90. [DOI] [PubMed] [Google Scholar]
Gallasch 2015
- Gallasch E, Christova M, Kunz A, Rafolt D, Golaszewski S. Modulation of sensorimotor cortex by repetitive peripheral magnetic stimulation. Frontiers in Human Neuroscience 2015;9:407. [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADE 2014 [Computer program]
- Hamilton (ON): McMaster University. GRADEpro. Hamilton (ON): McMaster University, 2014.
Guyatt 2008
- Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck‐Ytter Y, Schünemann HJ, et al. What is "quality of evidence" and why is it important to clinicians?. BMJ 2008;336(7651):995‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Han 2006
- Han TR, Shin HI, Kim IS. Magnetic stimulation of the quadriceps femoris muscle: comparison of pain with electrical stimulation. American Journal of Physical Medicine & Rehabilitation 2006;85(7):593‐9. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. www.cochrane‐handbook.org.
Ito 2013
- Ito T, Tsubahara A, Watanabe S. Use of electrical or magnetic stimulation for generating hip flexion torque. American Journal of Physical Medicine & Rehabilitation 2013;92:755‐61. [DOI] [PubMed] [Google Scholar]
Kerkhoff 2001
- Kerkhoff G, Heldmann B, Struppler A, Havel P, Jahn T. The effects of magnetic stimulation and attentional cueing on tactile extinction. Cortex 2001;37(5):719‐23. [DOI] [PubMed] [Google Scholar]
Krause 2008
- Krause P, Straube A. Peripheral repetitive magnetic stimulation induces intracortical inhibition in healthy subjects. Neurological Research 2008;30(7):690‐4. [DOI] [PubMed] [Google Scholar]
Langhorne 2009
- Langhorne P, Coupar F, Pollock A. Motor recovery after stroke: a systematic review. Lancet Neurology 2009;8(8):741‐54. [DOI] [PubMed] [Google Scholar]
McArthur 2011
- McArthur KS, Quinn TJ, Higgins P, Langhorne P. Post‐acute care and secondary prevention after ischaemic stroke. BMJ 2011;342:d2083. [DOI] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic reviews and Meta‐Analyses: the PRISMA statement. Annals of Internal Medicine 2009;151(4):264‐9. [DOI] [PubMed] [Google Scholar]
Nielsen 1996
- Nielsen JF, Sinkjaer T, Jakobsen J. Treatment of spasticity with repetitive magnetic stimulation: a double‐blind placebo‐controlled study. Multiple Sclerosis Journal 1996;2(5):227‐32. [DOI] [PubMed] [Google Scholar]
Park 2012
- Park JH, Razuk A, Saad PF, Telles GJ, Karakhanian WK, Fioranelli A, et al. Carotid stenosis: what is the high‐risk population?. Clinics (Sao Paulo) 2012;67(10):1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Ryan 2016
- Ryan R, Hill S. How to GRADE the quality of the evidence: Cochrane Consumers and Communication Group. https://cccrg.cochrane.org/author‐resources. December 2016.
Sacco 2013
- Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013;44(7):2064‐89. [DOI] [PMC free article] [PubMed] [Google Scholar]
Strong 2007
- Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurology 2007;6(2):182‐7. [DOI] [PubMed] [Google Scholar]
Struppler 2003
- Struppler A, Havel P, Müller‐Barna P. Facilitation of skilled finger movements by repetitive peripheral magnetic stimulation (RPMS) ‐ a new approach in central paresis. NeuroRehabilitation 2003;18:69‐82. [PubMed] [Google Scholar]
Struppler 2004
- Struppler A, Angerer B, Gündisch C, Havel P. Modulatory effect of repetitive peripheral magnetic stimulation on skeletal muscle tone in healthy subjects: stabilization of the elbow joint. Experimental Brain Research 2004;157:59‐66. [DOI] [PubMed] [Google Scholar]
Struppler 2007
- Struppler A, Binkofski F, Angerer B, Bernhardt M, Spiegel S, Drzezga A, et al. A fronto‐parietal network is mediating improvement of motor function related to repetitive peripheral magnetic stimulation: a PET‐H2O15 study. Neuroimage 2007;36(2):T174‐86. [DOI] [PubMed] [Google Scholar]
World Health Organization 1989
- World Health Organization. Stroke‐1989. Recommendations on stroke prevention, diagnosis, and therapy. Report of the WHO Task Force on Stroke and other Cerebrovascular Disorders. Stroke 1989;20(10):1407‐31. [DOI] [PubMed] [Google Scholar]
Zheng 2015
- Zheng C‐J, Liao W‐J, Xia W‐G. Effect of combined low‐frequency repetitive transcranial magnetic stimulation and virtual reality training on upper limb function in subacute stroke: a double‐blind randomized controlled trail. Journal of Huazhong University of Science and Technology 2015;35(2):248‐54. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Momosaki 2015
- Momosaki R, Yamada N, Ota E, Abo M. Repetitive peripheral magnetic stimulation for activities of daily living and functional ability in people after stroke. Cochrane Database of Systematic Reviews 2015, Issue 11. [DOI: 10.1002/14651858.CD011968] [DOI] [PMC free article] [PubMed] [Google Scholar]


