Abstract
Previous research has found that insecure attachment is associated with depression. In the present study, we use an accelerated longitudinal cohort design to examine how the association between attachment and depression develops during childhood and adolescence. Specifically, 690 children from 3 distinct cohorts (grades 3, 6, and 9) completed self-report measures of attachment and depressive symptoms 3 times over 3 years. Growth curve analyses indicated that attachment anxiety and attachment avoidance were uniquely related to depressive symptoms. Higher levels of attachment anxiety and avoidance predicted higher levels of depressive symptoms over time. Additionally, changes in attachment security were associated with changes in depressive symptoms. The analyses suggest that insecure attachment and depressive symptoms co-vary and that these dynamics are evident in childhood and adolescence.
Keywords: Attachment, Depression, Longitudinal, Parent-Child Relationships, Development
Attachment theory is a prominent framework for understanding how close relationships shape social and emotional development (Cassidy & Shaver, 2016). One of the core assumptions of attachment theory is that early caregiving experiences influence the ways that people come to think about themselves and their interpersonal relationships. For example, children who have warm, supportive interactions with caregivers across early childhood develop secure attachments (i.e., a positive model of the self and a model of others as available and responsive during times of distress). Whereas, children who experience insensitive or disruptive interactions with caregivers tend to develop insecure attachments (i.e., a negative view of the self and belief that others will not be available when needed) (see Cassidy & Shaver, 2016, for a review).
Importantly, the quality of children’s attachments are not only relevant for understanding child-caregiver relationships, they also have implications for social and emotional development more broadly. In particular, a number of scholars have identified insecure attachment as a risk factor for the onset of depressive symptoms (e.g., Cummings & Cicchetti, 1990; Morley & Moran, 2011). Empirical studies also find that insecure attachment predicts depressive symptom severity in both adolescents (e.g., Abela et al., 2005; Lee & Hankin, 2009; Margolese, Markiewicz, & Doyle, 2005) and adults (e.g., Hammen et al., 1995; Liu, Nagata, Shono, & Kitamura, 2009).
From a developmental perspective, it is critical to examine associations between attachment patterns and depressive symptoms during childhood and adolescence. Rates of depression rise dramatically throughout adolescence, with an increase of about six-fold between the ages of 15 and 18 (e.g., see Hankin, 2006, for a review). Additionally, later childhood and adolescence are accompanied by a number of significant social changes, each of which has the potential to exacerbate risk for internalizing problems. For example, children transition from middle school to high school and tend to experience increased stress as they do so (Goldstein, Boxer, & Rudolph, 2015). Children also begin to focus increasingly on peer relationships, become subject to increased socialization pressures, and must learn to adapt to new peer norms and expectations (Allen, Porter, McFarland, Marsh, & McElhaney, 2005; Brown & Larson, 2009). Although some children navigate these challenges with relative ease, others face difficulties in doing so and are likely to experience depressive symptoms (Hankin et al., 2015).
Childhood through adolescence may also be a particularly important time-period for studying changes in attachment patterns. As children mature, they experience a number of developmental changes that alter the nature of the child-caregiver relationship and potentially the quality of the child’s attachment to that caregiver as well. For example, children begin spending more time either with peers or alone (Larson & Richards, 1991), negotiate a process of separation-individuation with their caregivers, and establish personal autonomy (Koepke & Denissen, 2012). Many children also form more egalitarian relationships with their caregivers as they develop (De Goede, Irene, Branje, Delsing, & Meeus, 2009). In line with these ideas, longitudinal studies on attachment show that attachment security is malleable (e.g., Cozzarelli, Karafa, Collins, & Tagler, 2003; Fraley, Vicary, Brumbaugh, & Roisman, 2011), and that attachment-related change is especially likely to occur during childhood and adolescence (Jones et al., 2017; Weinfeld, Sroufe, & Egeland, 2000).
Regardless of the specific conditions that might influence children’s experiences of attachment and depressive symptoms, existing work suggests that both constructs are dynamic in nature and may be particularly amenable to change during childhood and adolescence. It is therefore important to go beyond examining mean-level differences between children and look at relative shifts within children in attachment security and depressive symptoms. Doing so could enable us to answer a key developmental question: Are changes in attachment security associated with changes in depressive symptoms over time? In the present study, we examine associations between attachment and depressive symptoms longitudinally in a sample of 690 children and adolescents, ranging in age from 7 to 19 years. Our goal is to learn more about how changes in attachment and depressive symptomology may be associated by leveraging alternative models for analyzing change.
It should be noted that there are debates in the literature about how to best conceptualize and measure attachment in later childhood and adolescence (see Crowell, Fraley, & Roisman, 2016, for a review). Some researchers use interview-based approaches (Farnfield, 2016; Brown, Gustafsson, Mills-Koonce, & Cox, 2017), whereas other researchers use self-report methods (e.g., Kerns, Aspelmeier, Gentzler, & Grabill, 2001). Interview-based approaches assess individual differences in children’s attachments to their parents based on the coherence with which children describe their parental relationships. In contrast, self-report measures assess individual differences in attachment in terms of children’s subjective evaluations of the security of their parental relationships (i.e., the extent to which children feel that their parents are available and responsive when needed). Although interview and self-report measures of attachment have similar correlations with other relational variables, they tend to correlate weakly with one another (r = 0.09; see Crowell, Fraley, & Shaver, 2008, for a review). The weak correlation between the two measurement approaches suggests that they may be tapping into distinct aspects of attachment functioning.
We adopt the self-report approach to assessing the quality of children’s attachments to their parents in the present study. Self-report methods are used extensively in the adult attachment literature in social-personality psychology (e.g., Brennan, Clark, & Shaver, 1998; Fraley, Heffernan, Vicary, & Brumbaugh, 2011) and are increasingly being used to study attachment with children and adolescents as well (e.g., Buist, Deković, Meeus, & van Aken, 2002; Crawford et al., 2006; Muris, Mayer, & Meesters, 2000; Ruhl, Dolan, & Buhrmester, 2015). Specifically, we used the Relationship Structures (ECR-RS) questionnaire (Fraley et al., 2011) as a way to assess the extent to which children varied in how secure they were in their relationships with their primary caregivers.
Review of Previous Research
Many studies have investigated the interplay of attachment and depressive symptoms in children and adolescents. Overall, existing research indicates that insecure attachment is associated with depressive symptoms (Brumariu & Kerns, 2010; Groh, Roisman, van IJzendoorn, Bakermans-Kranenburg, & Fearon, 2012; Madigan, Brumariu, Villani, Atkinson, & Lyons-Ruth, 2016). It is difficult, however, to reach more nuanced conclusions based on the current literature. One reason is that the majority of research has assessed attachment as a unidimensional construct in which people are classified as either secure or insecure (see Brumariu & Kerns, 2010, for a discussion of this issue). Although there is some disagreement on the exact number of categories or dimensions that should be used, the general consensus is that attachment is a multidimensional construct that entails more than a single secure/insecure distinction (Fraley, Hudson, Heffernan, & Segal, 2015; Fraley & Spieker, 2003; Roisman, Fraley, & Belsky, 2007). One well-established framework conceptualizes individual differences in attachment as varying along two distinct dimensions, known as attachment anxiety and attachment avoidance (Bartholomew, 1990; Fraley & Shaver, 2000). Attachment anxiety captures the extent to which people worry that others will not be available when needed. It reflects a working model with negative beliefs about the self (e.g., that one is not worthy of care). Attachment avoidance represents the extent to which people are comfortable with emotional intimacy and reflects working models with negative beliefs about others (e.g., that others are unreliable). A prototypical secure person is low on both attachment anxiety and avoidance. But an insecure person may be high on either one or both of the attachment dimensions. Examining attachment as a unidimensional construct prevents scholars from understanding which aspects of insecurity are driving the association between attachment and depressive symptoms.
It is necessary to distinguish between the attachment dimensions for theoretical reasons. According to Bartholomew (1990), there are critical distinctions between people who are high on attachment anxiety and avoidance (sometimes referred to as fearfully avoidant) and those who are low on anxiety but high on attachment avoidance (sometimes referred to as dismissing avoidant). Fearfully avoidant individuals desire emotional intimacy but avoid it because they are afraid of being hurt by others. Dismissing avoidant individuals, in contrast, do not form close emotional ties with others because they do not desire emotional dependency and prefer being self-reliant. Given these distinctions, some researchers have suggested that attachment avoidance, on its own, may not be a risk factor for certain types of mental health problems, namely internalizing symptoms (Fraley & Bonnano, 2004; Fraley & Shaver, 2016). Instead, it is attachment anxiety that places people at risk for internalizing difficulties. There is some research to support this assertion: Dismissing avoidance has been found to predict lower depressive symptoms following bereavement (Fraley & Bonnano, 2004) and better adjustment to divorce (Yárnoz-Yaben, 2010) in adults than fearful avoidance. It is therefore plausible that only fearfully avoidant children, but not dismissingly avoidant children, will experience increased depressive symptoms as they move through adolescence. However, this possibility has yet to be addressed empirically.
Another feature of the existing literature is that there are inconsistent results across various studies. A meta-analytic review conducted by Madigan et al. (2016) found small-to-moderate associations between both attachment dimensions and internalizing problems, including depression. However, other reviews have found associations for attachment avoidance only (Groh et al., 2012; Madigan, Atkinson, Laurin, & Benoit, 2013). Part of the ambiguity may stem from measurement inconsistencies: Some reviews focus on behavioral measures of attachment (Groh et al., 2012; Madigan et al., 2013), whereas others examine representational and questionnaire measures only (Madigan et al., 2016). Furthermore, some meta-analyses collapse across childhood (Madigan et al., 2016), whereas others focus on particular time-periods such as early childhood (Groh et al., 2012) or middle childhood (Madigan et al., 2013). Another factor is that the majority of studies included in the reviews have small sample sizes. For example, in the Madigan et al. (2013) meta-analysis, the median study sample size was 52. The smaller the sample size of the study, the lower its ability to both detect true effects and to correctly reject false ones (see Fraley & Vazire, 2014). Without larger sample sizes, it will be difficult to carefully study the associations between attachment and depressive symptoms in childhood and adolescence.
Finally, the field has overwhelmingly focused on cross-sectional research that only examines associations between attachment styles and depressive symptoms at one time-point. As such, we know relatively little about whether changes in attachment are associated with changes in depression over time. Studies that examine longitudinal relationships between attachment and depression are few and far between, and the ones that do so tend to focus on unidirectional models in which attachment security at one time-point is used to predict depressive symptoms at another time-point (e.g., Kidd et al., 2016; Robakis et al., 2016). With only two time-points, the amount of change in attachment security can be estimated, but not the shape of the developmental trajectory or rate of individual change—which can only be estimated with at least three measurements (Duncan & Duncan, 2009).
In short, the majority of studies on attachment and depression are cross-sectional, and the question of whether changes in depressive symptoms are related to changes in attachment security has been largely unexplored. Given the dynamic nature of both constructs during childhood and adolescence, examining this question could expand our understanding of whether and how attachment security and depressive symptoms develop in conjunction with one another across an important maturational time-period.
Overview of the Present Research
The purpose of the present study was to examine how the quality of children’s attachments to their primary caregivers relates to their depressive symptoms across childhood and adolescence. To do so, we examined associations between self-reported child attachment insecurity and depressive symptoms over three years.
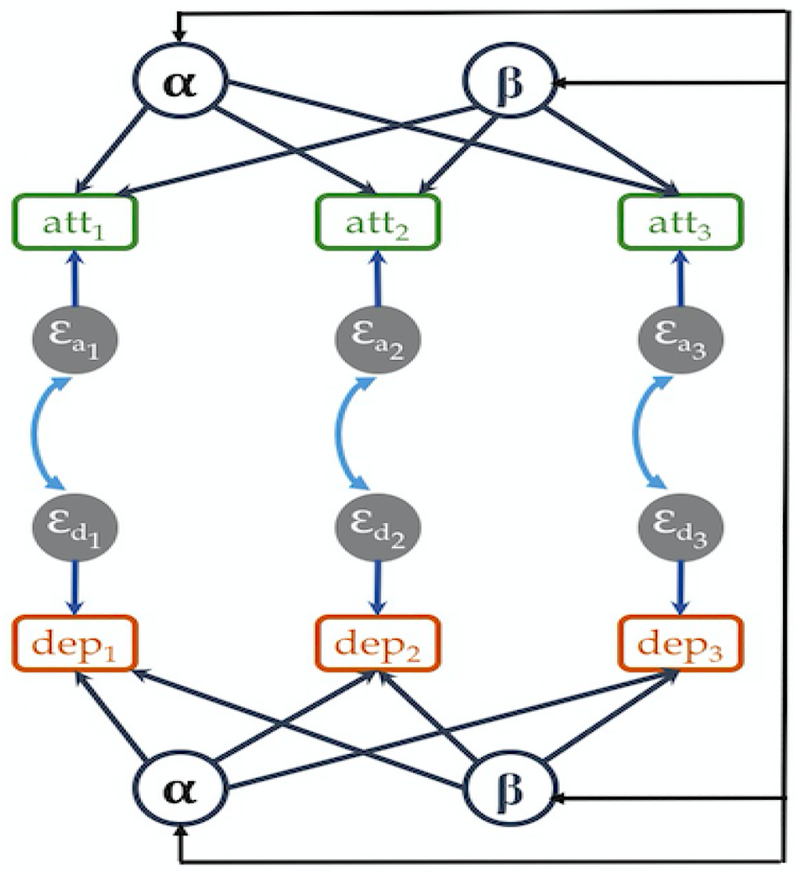
A number of different statistical methods exist that can be used to model the relationship between two or more latent constructs. We used the Latent Curve Model with Structured Residuals (LCM-SR) framework as originally proposed by Curran, Howard, Bainter, Lane, and McGinley (2014). The LCM-SR is similar to traditional multivariate latent curve models and requires at least three time-points for modeling the shape of change over time. Figure 1 illustrates the basic structure of our LCM-SR models.
Figure 1.
Example of an LCM-SR model with three measurement waves. α = average intercept; β = average slope; att = attachment anxiety or avoidance; dep = depressive symptoms.
The LCM-SR framework is valuable because it allows the admittedly vague question
“Do changes in X relate to changes in Y?” to be represented in two distinct and more precise ways. First, by modeling intercepts and slopes across people, the model allows the overall trajectory of attachment (or depressive symptoms) to be captured across time. This enables investigators to ask the traditional individual differences question: Are people with higher levels of attachment anxiety also reporting higher levels of depression (i.e., correlated intercepts)? However, in this case, the answer is not based on cross-sectional data alone, but on information obtained across multiple longitudinal assessments. In addition, it allows researchers to ask another developmentally valuable question: Is the rate of change in one variable related to the rate of change in another variable (i.e., correlated slopes)? In many respects, this is the kind of correlated change that is of greatest interest to scholars because it suggests that the trajectories of the variables in question are interdependent.
Second, by explicitly modeling residuals (i.e., deviations from individual trajectories), the LCM-SR allows processes related to longitudinal development (represented by the intercepts and slopes) to be separated from more state-like, contextual processes (represented by the residuals or error terms). In essence, the residuals reflect whether, at a given point in time, children are more or less depressed, for example, than their average. Estimating correlations between the residuals of two or more variable trajectories thus allows researchers to address whether fluctuations in attachment anxiety (or avoidance) beyond one’s average trajectory are associated with concurrent fluctuations in depressive symptoms. Importantly, correlations are thought to reflect within-person common causes—the existence of factors that lead people to change in similar directions with respect to both constructs of interest.
In short, the LCM-SR allows us to examine two kinds of psychological dynamics that are conflated in traditional research designs: (a) correlated trajectories (i.e., associations between intercepts and slopes), (b) correlated concurrent deviations from those trajectories (i.e., associations among time-specific residuals). We used this framework to address two research questions in particular.
Question 1: Are Trajectories of Attachment and Depression Correlated Across Time?
We investigated (a) whether children who were initially higher in attachment insecurity were also initially higher in depressive symptoms (correlated intercepts), and (b) whether changes in attachment insecurity predicted changes in depressive symptoms over time (correlated slopes). We did not have specific hypotheses regarding whether both forms of insecure attachment or only one (attachment anxiety or avoidance) would predict trajectories of depressive symptoms. But, based on previous research, we expected that at the very least attachment anxiety would be related to depressive symptoms over time.
Question 2: Are Concurrent Changes in Attachment and Depression Correlated Across Time?
What is the concurrent relationship between increases in attachment insecurity and increases in depressive symptoms beyond one’s average trajectory? That is, on occasions when children reported higher levels of attachment anxiety than usual, did they also report higher levels of depression than usual? These kinds of associations are typically thought to reflect within-person common-causes (e.g., failing an exam) that can lead to temporary changes in both variables of interest (see Hudson et al., 2013). By examining the concurrent correlations among the residuals, we aimed to determine whether there were correlated changes among the constructs. Given that attachment insecurity and depression are believed to have a similar set of causes (e.g., distress, unresponsive parenting, social isolation), we expected that, on occasions when people were more insecure than usual, they would also exhibit higher depressive symptoms than usual.
Methods
The sample comes from the Gene Environment Mood (GEM) study. As part of the GEM study, children and adolescents in the third, sixth, and ninth grades were recruited from participating school districts at two sites (Rutgers University and University of Denver) by letters sent to their homes. 690 youth aged 7–19 years (M = 11.84, SD = 2.41) took part in the study. Each cohort comprised approximately one-third of the sample, and about half of the total sample was female (55.2%, n = 381). Attachment and depression were assessed three times (18 months apart) over three years in the three distinct cohorts (grade 3, grade 6, and grade 9). Further demographic information on the overall sample can be found in Hankin et al. (2015).
Measures
Attachment.
Attachment patterns were assessed using the Relationship Structures (ECR-RS) Questionnaire (Fraley et al., 2011). The ECR-RS is a 9-item self-report measure of attachment patterns in close relationships. It can be administered with regard to a variety of relationships (e.g., with mothers, fathers, romantic partners), and was administered only with respect to the parent that accompanied the child in the present study (the mother in 85% of cases). The ECR-RS consists of two subscales, attachment anxiety and attachment avoidance. Children were asked to rate each item on a scale from 1 (strongly disagree) to 7 (strongly agree). Example items include “I’m afraid this person may abandon me” (attachment anxiety) and “I don’t feel comfortable opening up to this person” (attachment avoidance). Mean scores were calculated for each subscale and were used in all analyses. Reliability of the ECR-RS was good (Anxiety: αbaseline = 0.82, α18-months = 0.83, α36-months = 0.82; Avoidance: αbaseline = 0.81, α18-months = 0.80, α36-months = 0.82).
Depression.
Depressive symptoms were measured using the Children’s Depression Inventory (CDI; Kovacs, 1992). The CDI is a 27-item self-report measure designed to assess depressive symptoms in children and adolescents. Children were asked to respond to one of three statements for each item (e.g., 0 - “I am sad once in a while” to 2 - “I am sad all the time”), with higher scores indicating greater levels of depressive symptoms and scores varying between a theoretical minimum of 0 and maximum of 54. The CDI is reliable and valid (Klein, Dougherty, & Olino, 2005). Reliability in the present study was good (αbaseline = 0.83, α18-months = 0.83, α36-months = 0.86).
Preregistered Analyses
The preregistration for our analytic plan and research questions can be found at https://osf.io/4nnzy/. As outlined above, we chose to use the LCM-SR model to conduct our analyses. We followed Curran et al.’s (2014) recommendation and first established the optimally fitting sub-model for each construct (i.e., depression, attachment anxiety, and attachment avoidance)1. Then, we built two bivariate LCM-SR models including depression and attachment (i.e., anxiety and avoidance separately). We included cohort as a covariate in the models to account for potential age-related differences in the attachment dimensions (above and beyond temporal effects).
As we discuss below, some of our results prompted additional questions that we sought to address. Thus, we first report our results with respect to our pre-registered analytic plan and, in the Supplementary Analyses section, elaborate with some additional analyses that we did not register before analyzing the data.
Results
Descriptive statistics (means, standard deviations, and correlations between all variables) are provided in Table 1.
Table 1.
Descriptive Statistics
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1 T1 Anx. | 1 | ||||||||
| 2 T1 Avoid. | 0.33 | 1 | |||||||
| 3 T1 Depress. | 0.37 | 0.29 | 1 | ||||||
| 4 T2 Anx. | 0.25 | 0.23 | 0.25 | 1 | |||||
| 5 T2 Avoid. | 0.12 | 0.49 | 0.20 | 0.31 | 1 | ||||
| 6 T2 Depress. | 0.15 | 0.19 | 0.48 | 0.34 | 0.35 | 1 | |||
| 7 T3 Anx. | 0.20 | 0.15 | 0.17 | 0.44 | 0.27 | 0.22 | 1 | ||
| 8 T3 Avoid. | 0.09 | 0.39 | 0.17 | 0.33 | 0.63 | 0.28 | 0.39 | 1 | |
| 9 T3 Depress. | 0.11 | 0.15 | 0.37 | 0.24 | 0.24 | 0.54 | 0.31 | 0.37 | 1 |
| 10 Mean | 1.66 | 2.72 | 7.01 | 1.55 | 2.83 | 5.23 | 1.55 | 2.95 | 4.99 |
| 11 SD | 1.18 | 1.31 | 5.83 | 1.02 | 1.40 | 5.81 | 1.08 | 1.47 | 5.51 |
| 12 Alpha | 0.82 | 0.81 | 0.83 | 0.83 | 0.80 | 0.83 | 0.82 | 0.82 | 0.86 |
Note. Anx. = Attachment Anxiety; Avoid. = Attachment Avoidance; Depress. = Depressive Symptoms; SD = Standard Deviation.
We begin by reporting the fit of our two bivariate models (each of the attachment dimensions with depressive symptoms, respectively) and overall longitudinal trajectories of the included variables. We then report the analyses of interest for addressing our two research questions. The results are summarized in Table 2.
Table 2.
Parameter estimates for bivariate models
| Attachment Anxiety and Depression | Attachment Avoidance and Depression | |
|---|---|---|
| Intercepts Slopes Residuals Time 1 Time 2 Time 3 Combined |
1.629 [0.908, 2.350]* 0.320 [−.0.037, .677] 1.093 [.344, 1.842]* 0.688 [.316, 1.060]* 0.173 [−.521, .867] 0.648 [.372, .924]* |
1.443 [0.608, 2.278]* 0.473 [.071, .875]* 0.626 [−.170, 1.422] 0.955 [.510, 1.400]* 0.295 [−.520, 1.110] 0.779 [.485, 1.073]* |
indicates p < .05
Model 1: Attachment Anxiety and Depressive Symptoms
The first model examined attachment anxiety and depressive symptoms using the LCM-SR framework. Overall, this model fit the data reasonably well, χ2(6) = 19.428, p = .003, CFI = .982, RMSEA = .057, SRMR = .025. Children were relatively low in attachment anxiety on average (the average intercept, α, = 1.905, SE = .115) and tended to decrease in anxiety across time (the average slope, β, = −.222, SE = .081, p = .006). Children were also relatively low in depressive symptoms on average (α = 4.185, SE = .595) and tended to experience fewer depressive symptoms across time (β = −1.327, SE = .364, p < .001). For each of the growth terms, there were significant random effects (all p’s ≤ .017), suggesting that there was meaningful variability to be explained between children in both their intercepts and slopes.
Model 2: Attachment Avoidance and Depressive Symptoms
We next examined attachment avoidance and depressive symptoms using the LCM-SR framework. The model fit the data reasonably well, χ2(6) = 20.913, p = .002, CFI = .984, RMSEA = .060, SRMR = .024. On average, children were relatively low in attachment avoidance (α = 2.210, SE = .134) and did not significantly change in avoidance across time (β = .101, SE = .090, p = .259). As expected from the previous analyses, children were relatively low in depression on average (α = 4.209, SE = .595) and tended to report decreased depressive symptoms over time (β = −1.364, SE = .364, p < .001). There were also significant random effects (all p’s < .001) associated with each of the growth terms, indicating that children differed from one another in their intercepts and slopes. Thus, although children did not increase or decrease in avoidance on average, some children increased considerably over time whereas others decreased.
Question 1: Are Trajectories of Attachment and Depression Correlated Across Time?
Attachment Anxiety.
We examined the associations between the estimated intercepts and slopes across children to determine whether the longitudinal trajectories of attachment and depressive symptoms were correlated. Children who were initially more anxious with respect to attachment also tended to be more depressed initially (β = 1.629, SE = .368, p < .001, r = .638; correlated intercepts). In addition, there was a tendency for children who increased in anxiety across time to also increase in depressive symptoms across time (β = .320, SE = .182, p = .078, r = .432; correlated slopes).
Attachment Avoidance.
Children who were initially more avoidant with respect to attachment also tended to be initially more depressed (β = 1.443, SE = .426, p = .001, r = .327; correlated intercepts). Additionally, children who increased in avoidance over time also tended to increase in depressive symptoms over time (β = .473, SE = .205, p = .021, r = .404; correlated slopes).
Question 2: Are Concurrent Changes in Attachment and Depression Correlated Across Time?
Attachment Anxiety.
We examined the associations between the residuals at each assessment wave to assess whether concurrent changes in attachment and depressive symptoms were correlated across time. The residuals represent time-specific deviations from a person’s average trajectory. As such, correlations among the residuals imply that people who deviated from their expected values on one variable (e.g., attachment anxiety) also deviated from their expected values on the other variable (i.e., depression), net of any overall longitudinal effects. For all three waves, when children were more anxious than expected, they were also more likely to report more depressive symptoms than would be expected. Because all of the estimates were similar in magnitude, we decided to re-estimate the model while constraining the estimates to be identical. The common estimate indicated that there was a positive association between the residuals of attachment anxiety and depressive symptoms (β = .648, SE = .141, p < .001, r = .182-.289). Overall, it appears that when children experience time-specific deviations from their trajectories of attachment anxiety, they also deviate from their depression trajectories in the same direction.
Attachment Avoidance.
The associations between the avoidance and depression residuals were positive at each of the three waves. Because the estimates were all of similar magnitude, we re-estimated the parameters in a model in which these paths were constrained to be identical. The common estimate indicated that there was a positive association between the residuals of attachment avoidance and depressive symptoms (β = .779, SE = .150, p < .001, r = .211-.368). When children experienced time-specific deviations from their trajectories of avoidance, they also deviated from their depression trajectories in the same direction.
Supplementary Analyses
Attachment anxiety and avoidance tend to be correlated. In fact, the correlation between the two constructs in the present sample at the initial assessment wave was .328. We therefore thought it would be prudent to examine a model that includes both anxiety and avoidance simultaneously. Such a multivariate model would allow us to more accurately estimate the unique associations between each attachment dimension and depressive symptoms than the bivariate models. Moreover, such an analysis allows us to examine whether the linear combination of anxiety and avoidance is related to depressive symptoms, potentially informing debates about whether fearful- or dismissing-avoidance or both are associated with depression. We therefore ran a LCM-SR model including both attachment dimensions and depressive symptoms simultaneously. As before, cohort was included as a covariate and the magnitude of the correlated residuals was constrained to be equal across assessment waves. The results are summarized in Table 3.
Table 3.
Parameter estimates for multivariate model
| Attachment Anxiety and Depression | Attachment Avoidance and Depression | |
|---|---|---|
| Intercepts Slopes Residuals |
1.926 [1.375, 2.477]* 0.291 [.050, .532]* 0.661 [.385, .937]* |
1.333 [.718, 1.948]* 0.321 [.058, .584]* 0.770 [.478, 1.062]* |
indicates p < .05
Question 1.
The associations between the estimated intercepts and slopes of each attachment dimension with depressive symptoms were similar to those obtained previously. Children who were initially more anxious with respect to attachment tended to be initially more depressed as well (β = 1.926, SE = .281, p < .001, r = .691), and those who increased in anxiety over time also tended to increase in depressive symptoms over time (β = .291, SE = .123, p = .018, r = .408). Similarly, children who were initially more avoidant with respect to attachment also tended to be initially more depressed (β = 1.333, SE = .314, p < .001, r = .295), and those who increased in avoidance over time tended to increase in depressive symptoms over time (β = .321, SE = .134, p = .016, r = .280).
Question 2.
The common estimate for anxiety and depression was statistically significant (β = .661, SE = .141, p < .001, r = .184-.277), as was the common estimate for avoidance and depression (β = .770, SE = .149, p < .001, r = .206-.366). Children that experienced time-specific deviations from their trajectories of either attachment anxiety or avoidance also tended to deviate from their depression trajectories in the same direction. In short, the results from our analyses of a model that includes anxiety and avoidance simultaneously converged with those from models that treated them separately.
Discussion
We examined the association between attachment insecurity and depressive symptoms in a normative sample of children and adolescents. Our analyses indicate that, on average, children who are high in attachment insecurity also tend to be high in depressive symptoms (i.e., correlated intercepts). Additionally, those who increase in attachment insecurity over time also tend to increase in depressive symptoms over time (i.e., correlated slopes). We also found time-specific associations between attachment and depressive symptoms. Specifically, on occasions when children experienced more attachment insecurity than usual (i.e., when they deviated from their own trajectory), they also reported more depressive symptoms than usual (i.e., correlated residuals). Importantly, similar patterns were found for attachment anxiety and avoidance, and these remained even when the variance shared by the two dimensions was controlled.
These findings have multiple implications for attachment theory. First, although attachment researchers have emphasized the ways in which attachment patterns can change over time, there has been relatively little attention given to the concept of “correlated changes” in the attachment literature. Using the LCM-SR as a point of departure, we proposed that changes in attachment can correlate with changes in depressive symptoms in at least two separable ways. For example, increases in attachment anxiety over time can correlate with increases in depression across time (correlated slopes). Or within-person deviations in a person’s attachment trajectory can correlate with within-person deviations in a person’s trajectory of depressive symptoms (correlated residuals). Our results show that trajectories of change in attachment were associated with trajectories of change in depression. Moreover, we found that concurrent within-person deviations from those trajectories were correlated. Overall, these findings demonstrate that “correlated changes” can exist at multiple levels and, importantly, that they are relevant to understanding the developmental dynamics of attachment and depression.
Second, one of the major debates in the attachment literature involves the relative contribution of attachment anxiety and avoidance to psychological maladjustment. A number of studies have shown that attachment anxiety places individuals at risk for anxiety disorders, depression, and eating disorders (Eng, Heimberg, Hart, Schneier, & Liebowitz, 2001; Reis & Grenyer, 2004; Tasca & Balfour, 2014; Woodhouse, Ayers, & Field, 2015). What is less clear, however, is whether attachment avoidance—independent of its association with anxiety—is a risk factor for internalizing psychopathology. Fraley, Davis, and Shaver (1998) have suggested that attachment avoidance in the absence of anxiety (i.e., dismissing avoidance) may be protective against interpersonal stressors. Dismissing-avoidant individuals are compulsively self-reliant and tend to be less emotionally invested in others. Dismissing-avoidant individuals may therefore not be as vulnerable to the potentially negative impact of interpersonal stressors as less defensive individuals. This hypothesis may be especially relevant in the present context as interpersonal stressors have been found to predict depressive symptoms in youth (e.g., Hankin et al., 2015; Rudolph et al., 2000). The current findings contribute to the debate by showing that, at least in the case of childhood and adolescent depression, both forms of insecurity appear to be risk factors. Fearfully avoidant children (being high on anxiety and avoidance) are the most prone to depressive symptoms and dismissingly-avoidant children (being high on avoidance but low on anxiety), while not being as susceptible to depression as fearful children, are nonetheless at greater risk than relatively secure children (i.e., those who are low on both attachment dimensions).
Why might dismissing adults be relatively resilient even if dismissing children are not? The protective value of attachment avoidance against interpersonal stressors in adulthood may be contingent on the combined desire and ability to be self-reliant. Children who are dismissing-avoidant may desire self-reliance but are unlikely to be able to fully support themselves, emotionally and otherwise. The inability to be self-reliant during times of stress may result in dismissing-avoidant children having no choice but to depend on a parent or close other. The discomfort associated with dependence for dismissing-avoidant children may in turn increase the likelihood of them experiencing depressive symptoms. On the other hand, dismissing-avoidant adults are likely to desire self-reliance and be able to achieve it during times of stress because of more developed cognitive and emotional abilities, as well as increased access to resources. Dismissing-avoidant adults may therefore be less likely to experience depressive symptoms as a consequence of their attachment style. To the best of our knowledge, this idea has not yet been tested empirically.
Limitations and Future Directions
The current study makes a unique contribution to the literature on attachment security and depressive symptoms because it utilizes a longitudinal design with repeated measurements of both constructs with a large sample of children and adolescents. However, the present study has some limitations too. Foremost, our work only sheds light on the association between attachment insecurity and depressive symptoms; it does not hold any implications for other subtypes of internalizing symptoms. The degree to which attachment anxiety and avoidance predict different aspects of internalizing distress (e.g., anxiety) in childhood is still unclear. Future research could use a similar design as the present study and investigate the associations between other categories of childhood internalizing symptoms and each attachment dimension. Furthermore, the measures used in the present work were all child self-report, and it is possible that part of the strength of the associations reported here was due to shared measurement variance. Researchers should therefore seek to replicate the current findings using multiple measurement approaches (e.g., by using parent or clinician reports of child depressive symptoms).
Another limitation of the present study was that we were not able to address one of our pre-registered research questions: When people deviate from their trajectories of attachment at one time-point, do they also deviate from their trajectories of depressive symptoms at a later time-point (and vice versa)? Because the models would not converge appropriately when we included autoregressive paths among the residuals, we were not able to examine the prospective, cross-lagged associations among those residuals. It is unclear why the models failed to converge, but it is likely that the small number of assessment waves contributed to the problem. We believe one of the most obvious ways to improve this work in the future is to take more than three assessments of attachment and depressive symptoms over time. Doing so would allow us to provide additional information about how changes in attachment and depressive symptoms prospectively predict one another across time.
In conclusion, the present longitudinal analyses suggest that changes in attachment are related to changes in depressive symptoms among children and adolescents. Specifically, we identified two ways in which “change” plays out in this domain: (a) children who become more insecure over time tend to report greater depressive symptoms across time (i.e., correlated slopes or trajectories) and (b), on occasions when children report greater attachment insecurity than usual, they also report greater depressive symptoms than usual (i.e., correlated residuals). The results suggest that attachment and depression are bound across numerous developmental levels of analysis, and hopefully provide a stronger foundation for understanding the role of attachment in the development of depressive symptoms and vice versa.
Acknowledgments
We would like to thank all the parents and children that participated in the Gene-Environment-Mood (GEM) project. We would also like to thank the National Institute of Mental Health for providing funding for the GEM project and making our work possible.
Funding: This work was supported by National Institute of Mental Health (NIMH) under Grants R01-MH 077195, R01-MH 077178, R01 MH109662, 1R01MH105501, 2R01MH077195, and 1R21MH102210.
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
Our pre-registration includes another research question that we were unable to address. This question involves examining time-lagged associations between the residuals of interest. Modeling time-lagged associations requires the inclusion of autoregressive paths. However, inclusion of autoregressive paths prevented the univariate models from converging. Thus, we removed autoregressive paths from all analyses and, consequently, were unable to answer our third research question.
References
- Abela JRZ, Hankin BL, Haigh EAP, Adams P, Vinokuroff T, & Trayhern L(2005). Interpersonal vulnerability to depression in high-risk children: The role of insecure attachment and reassurance seeking. Journal of Clinical Child and Adolescent Psychology, 34(1), 182–192. doi: 10.1207/s15374424jccp3401_17 [DOI] [PubMed] [Google Scholar]
- Allen JP, Porter MR, McFarland FC, Marsh P, & McElhaney KB (2005). The two faces of adolescents’ success with peers: Adolescent popularity, social adaptation, and deviant behavior. Child Development, 76, 747–760. doi: 10.1111/j.1467-8624.2005.00875.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartholomew K (1990). Avoidance of intimacy: An attachment perspective. Journal of Social and Personal Relationships, 7(2), 147–178. doi: 10.1177/0265407590072001 [DOI] [Google Scholar]
- Brennan KA, Clark CL, & Shaver PR (1998). Self-report measurement of adult attachment: An integrative overview In Simpson JA & Rholes WS (Eds.), Attachment theory and close relationships (pp. 46–76). New York, NY, US: Guilford Press. [Google Scholar]
- Brown GL, Gustafsson HC, Mills-Koonce WR, & Cox MJ (2017) Associations between early caregiving and rural, low-SES, African-American children’s representations of attachment relationships. Attachment & Human Development, 19, 340–363. doi: 10.1080/14616734.2017.1318935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown BB, & Larson J (2009). Peer relationships in adolescence In Lerner RM & Steinberg L (Eds.), Handbook of adolescent psychology (pp. 74–103). New York, NY: Wiley. [Google Scholar]
- Brumariu LE, & Kerns KA (2010). Parent-child attachment and internalizing symptoms in childhood and adolescence: A review of empirical findings and future directions. Development and Psychopathology, 22(1), 177–203. doi: 10.1017/S0954579409990344 [DOI] [PubMed] [Google Scholar]
- Buist KL, Deković M, Meeus W, & van Aken MG (2002). Developmental patterns in adolescent attachment to mother, father and sibling. Journal of Youth and Adolescence, 31, 167–176. doi: 10.1023/A:1015074701280 [DOI] [Google Scholar]
- Cassidy J, & Shaver PR (2016). Handbook of attachment theory, research and clinical applications. New York, NY: The Guilford Press. [Google Scholar]
- Cook SH, Heinze JE, Miller AL, & Zimmerman MA (2016). Transitions in friendship attachment during adolescence are associated with developmental trajectories of depression through adulthood. Journal of Adolescent Health, 58(3), 260–266. doi: 10.1016/j.jadohealth.2015.10.252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cozzarelli C, Karafa JA, Collins NL, & Tagler MJ (2003). Stability and change in adult attachment styles: Associations with personal vulnerabilities, life events, and global construals of self and others. Journal of Social and Clinical Psychology, 22(3), 315–346. doi: 10.1521/jscp.22.3.315.22888 [DOI] [Google Scholar]
- Crawford TN, Shaver PR, Cohen P, Pilkonis PA, Gillath O, & Kasen S (2006). Self reported attachment, interpersonal aggression, and personality disorder in a prospective community sample of adolescents and adults. Journal of Personality Disorders, 20, 331–351. doi: 10.1521/pedi.2006.20.4.331 [DOI] [PubMed] [Google Scholar]
- Crowell JA, Fraley RC, & Roisman GI (2016). Measurement of individual differences in adult attachment In Cassidy J & Shaver PR (Eds.), Handbook of attachment: Theory, research, and clinical applications (3rd Edition)(pp. 598–635). New York: Guilford Press. [Google Scholar]
- Crowell JA, Fraley RC, & Shaver PR (2008). Measurement of individual differences in adolescent and adult attachment In Cassidy J, & Shaver PR (Eds.), 2nd ed.; handbook of attachment: Theory, research, and clinical applications (2nd ed.) (2nd ed. ed., pp. 599–634, Chapter xix, 1020 Pages) The Guilford Press, New York, NY. [Google Scholar]
- Cummings EM, & Cicchetti D (1990). Toward a transactional model of relations between attachment and depression In Greenberg MT, Cicchetti D & Cummings EM (Eds.), Attachment in the preschool years: Theory, research, and intervention; attachment in the preschool years: Theory, research, and intervention (pp. 339–372, Chapter xix, 507 Pages) University of Chicago Press, Chicago, IL. [Google Scholar]
- Curran PJ, Howard AL, Bainter SA, Lane ST, & McGinley JS (2014). The separation of between-person and within-person components of individual change over time: A latent curve model with structured residuals. Journal of Consulting and Clinical Psychology, 82(5), 879–894. doi: 10.1037/a0035297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goede De, Irene HA, Branje SJT, Delsing MJMH, & Meeus WHJ (2009). Linkages over time between adolescents’ relationships with parents and friends. Journal of Youth and Adolescence, 38(10), 1304–1315. doi: 10.1007/s10964-009-9403-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan TE, & Duncan SC (2009). The abc’s of LGM: An introductory guide to latent variable growth curve modeling. Social and Personality Psychology Compass, 3(6), 979–991. doi: 10.1111/j.1751-9004.2009.00224.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eng W, Heimberg RG, Hart TA, Schneier FR, & Liebowitz MR (2001). Attachment in individuals with social anxiety disorder: The relationship among adult attachment styles, social anxiety, and depression. Emotion, 1(4), 365–380. doi: 10.1037/1528-3542.1.4.365 [DOI] [PubMed] [Google Scholar]
- Farnfield S (2016). The Child Attachment and Play Assessment (CAPA): Validation of a new approach to coding narrative stems with children ages 3–11 years. International Journal of Play Therapy, 25, 217–229. doi: 10.1037/a0038726 [DOI] [Google Scholar]
- Fraley RC, & Bonanno GA (2004). Attachment and loss: A test of three competing models on the association between attachment-related avoidance and adaptation to bereavement. Personality and Social Psychology Bulletin, 30(7), 878–890. doi: 10.1177/0146167204264289 [DOI] [PubMed] [Google Scholar]
- Fraley RC, Davis KE, & Shaver PR (1998). Dismissing-avoidance and the defensive organization of emotion, cognition, and behavior In Simpson JA & Rholes WS (Eds.), Attachment theory and close relationships (pp. 249–279). New York: Guilford Press. [Google Scholar]
- Fraley RC, Heffernan ME, Vicary AM, & Brumbaugh CC (2011). The experiences in close relationships—Relationship structures questionnaire: A method for assessing attachment orientations across relationships. Psychological Assessment, 23, 615–625. doi: 10.1037/a0022898 [DOI] [PubMed] [Google Scholar]
- Fraley RC, Hudson NW, Heffernan ME, & Segal N (2015). Are adult attachment styles categorical or dimensional? A taxometric analysis of general and relationship specific attachment orientations. Journal of Personality and Social Psychology, 109, 354–368. doi: 10.1037/pspp0000027 [DOI] [PubMed] [Google Scholar]
- Fraley RC, & Shaver PR (2000). Adult romantic attachment: Theoretical developments, emerging controversies, and unanswered questions. Review of General Psychology, 4, 132–154. doi: 10.1037/1089-2680.4.2.132 [DOI] [Google Scholar]
- Fraley RC, & Shaver PR (2016). Attachment, loss, and grief: Bowlby’s views, new developments, and current controversies In Cassidy J & Shaver PR (Eds.), Handbook of attachment: Theory, research, and clinical applications (3rd Edition)(pp. 40–62). New York: Guilford Press. [Google Scholar]
- Fraley RC, & Spieker SJ (2003). Are infant attachment patterns continuously or categorically distributed? A taxometric analysis of strange situation behavior. Developmental Psychology, 39, 387–404. doi: 10.1037/0012-1649.39.3.387 [DOI] [PubMed] [Google Scholar]
- Fraley RC, & Vazire S (2014). The N-pact factor: Evaluating the quality of empirical journals with respect to sample size and statistical power. PLoS ONE, 9(10): e109019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraley RC, Vicary AM, Brumbaugh CC, & Roisman GI (2011). Patterns of stability in adult attachment: An empirical test of two models of continuity and change. Journal of Personality and Social Psychology, 101(5), 974–992. doi: 10.1037/a0024150 [DOI] [PubMed] [Google Scholar]
- Goldstein SE, Boxer P, & Rudolph E (2015). Middle school transition stress: Links with academic performance, motivation, and school experiences. Contemporary School Psychology, 19(1), 21–29. doi: 10.1007/s40688-014-0044-4 [DOI] [Google Scholar]
- Groh AM, Roisman GI, van IJzendoorn MH, Bakermans‐Kranenburg MJ, & Fearon RP (2012). The significance of insecure and disorganized attachment for children’s internalizing symptoms: A meta‐analytic study. Child Development, 83(2), 591–610. doi: 10.1111/j.1467-8624.2011.01711.x [DOI] [PubMed] [Google Scholar]
- Hammen CL, Burge D, Daley SE, Davila J, Paley B, & Rudolph KD (1995). Interpersonal attachment cognitions and prediction of symptomatic responses to interpersonal stress. Journal of Abnormal Psychology, 104(3), 436–443. doi: 10.1037/0021-843X.104.3.436 [DOI] [PubMed] [Google Scholar]
- Hankin BL (2006). Adolescent depression: Description, causes, and interventions. Epilepsy & Behavior, 8(1), 102–114. doi: 10.1016/j.yebeh.2005.10.012 [DOI] [PubMed] [Google Scholar]
- Hankin BL, Young JF, Abela JR, Smolen A, Jenness JL, Gulley LD, Technow JR, Gottlieb AB, Cohen JR, & Oppenheimer CW (2015). Depression from childhood into late adolescence: influence of gender, development, genetic susceptibility, and peer stress. Journal of Abnormal Psychology, 124, 803–816. doi: 10.1037/abn0000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones JD, Fraley RC, Ehrlich KB, Stern JA, Lejuez CW, Shaver PR, & Cassidy J (2017). Stability of attachment style in adolescence: An empirical test of alternative developmental processes. Child Development, doi: 10.1111/cdev.12775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerns KA, Aspelmeier JE, Gentzler AL, & Grabill CM (2001). Parent–child attachment and monitoring in middle childhood. Journal of Family Psychology, 15, 69–81. doi: 10.1037/0893-3200.15.1.69 [DOI] [PubMed] [Google Scholar]
- Kidd T, Poole L, Ronaldson A, Leigh E, Jahangiri M, & Steptoe A (2016). Attachment anxiety predicts depression and anxiety symptoms following coronary artery bypass graft surgery. British Journal of Health Psychology, 21(4), 796–811. doi: 10.1111/bjhp.12191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DN, Dougherty LR, & Olino TM (2005). Toward guidelines for evidence-based assessment of depression in children and adolescents. Journal of Clinical Child and Adolescent Psychology, 34(3), 412–432. doi: 10.1207/s15374424jccp3403_ [DOI] [PubMed] [Google Scholar]
- Koepke S, & Denissen JJA (2012). Dynamics of identity development and separation individuation in parent–child relationships during adolescence and emerging adulthood –- A conceptual integration. Developmental Review, 32(1), 67–88. doi: 10.1016/j.dr.2012.01.001 [DOI] [Google Scholar]
- Kovacs M Children’s Depression Inventory Manual. North Tonawanda, NY: Multi-Health Systems, Inc; 1992. [Google Scholar]
- Larson R, & Richards MH (1991). Daily companionship in late childhood and early adolescence: Changing developmental contexts. Child Development, 62(2), 284–300. doi: 10.2307/1131003 [DOI] [PubMed] [Google Scholar]
- Lee A & Hankin BL (2009). Insecure attachment, dysfunctional attitudes, and self-esteem predicting prospective symptoms of depression and anxiety during adolescence. Journal of Clinical Child and Adolescent Psychology, 38, 219–231. doi: 10.1080/15374410802698396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Licata M, Zietlow A, Träuble B, Sodian B, & Reck C (2016). Maternal emotional availability and its association with maternal psychopathology, attachment style insecurity and theory of mind. Psychopathology, 49(5), 334–340. doi: 10.1159/000447781 [DOI] [PubMed] [Google Scholar]
- Liu Q, Nagata T, Shono M, & Kitamura T (2009). The effects of adult attachment and life stress on daily depression: A sample of japanese university students. Journal of Clinical Psychology, 65(7), 639–652. doi: 10.1002/jclp.20572 [DOI] [PubMed] [Google Scholar]
- Madigan S, Atkinson L, Laurin K, & Benoit D (2013). Attachment and internalizing behavior in early childhood: A meta-analysis. Developmental Psychology, 49(4), 672–689. doi: 10.1037/a0028793 [DOI] [PubMed] [Google Scholar]
- Madigan S, Brumariu LE, Villani V, Atkinson L, & Lyons-Ruth K (2016). Representational and questionnaire measures of attachment: A meta-analysis of relations to child internalizing and externalizing problems. Psychological Bulletin, 142(4), 367–399. doi: 10.1037/bul0000029 [DOI] [PubMed] [Google Scholar]
- Margolese SK, Markiewicz D, & Doyle AB (2005). Attachment to parents, best friend, and romantic partner: Predicting different pathways to depression in adolescence. Journal of Youth and Adolescence, 34(6), 637–650. doi: 10.1007/s10964-005-8952-2 [DOI] [Google Scholar]
- Morley TE, & Moran G (2011). The origins of cognitive vulnerability in early childhood: Mechanisms linking early attachment to later depression. Clinical Psychology Review, 31(7), 1071–1082. doi: 10.1016/j.cpr.2011.06.006 [DOI] [PubMed] [Google Scholar]
- Muris P, Mayer B, & Meesters C (2000). Self-reported attachment style, anxiety, and depression in children. Social Behavior and Personality: An International Journal, 28, 157–162. doi: 10.2224/sbp.2000.28.2.157 [DOI] [Google Scholar]
- Reis S, & Grenyer BFS (2004). Fear of intimacy in women: Relationship between attachment styles and depressive symptoms. Psychopathology, 37(6), 299–303. doi: 10.1159/000082268 [DOI] [PubMed] [Google Scholar]
- Robakis TK, Williams KE, Crowe S, Lin KW, Gannon J, & Rasgon NL (2016). Maternal attachment insecurity is a potent predictor of depressive symptoms in the early postnatal period. Journal of Affective Disorders, 190, 623–631. doi: 10.1016/j.jad.2015.09.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roisman GI, Fraley RC, & Belsky J (2007). A taxometric study of the Adult Attachment Interview. Developmental Psychology, 43, 675–686. doi: 10.1037/0012-1649.43.3.675 [DOI] [PubMed] [Google Scholar]
- Rudolph KD, Hammen C, Burge D, Lindberg N, Herzberg D, & Daley SE (2000). Toward an interpersonal life-stress model of depression: The developmental context of stress generation. Development and Psychopathology, 12(2), 215–234. doi: 10.1017/S0954579400002066 [DOI] [PubMed] [Google Scholar]
- Ruhl H, Dolan EA, & Buhrmester D (2015). Adolescent attachment trajectories with mothers and fathers: The importance of parent-child relationship experiences and gender. Journal of Research on Adolescence, 25, 427–442. doi: 10.1111/jora.12144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tasca GA, & Balfour L (2014). Attachment and eating disorders: A review of currentearch. International Journal of Eating Disorders, 47(7), 710–717. doi: 10.1002/eat.22302 [DOI] [PubMed] [Google Scholar]
- Sweeney PD, Anderson K, & Bailey S (1986). Attributional style in depression: A meta analytic review. Journal of Personality and Social Psychology, 50(5), 974–991. doi: 10.1037/0022-3514.50.5.974 [DOI] [PubMed] [Google Scholar]
- Weinfield NS, Sroufe LA, & Egeland B (2000). Attachment from infancy to early adulthood in a high-risk sample: Continuity, discontinuity, and their correlates. Child Development, 71(3), 695–702. doi: 10.1111/1467-8624.00178 [DOI] [PubMed] [Google Scholar]
- Woodhouse S, Ayers S, & Field AP (2015). The relationship between adult attachment style and post-traumatic stress symptoms: A meta-analysis. Journal of Anxiety Disorders, 35, 103–117. doi: 10.1016/j.janxdis.2015.07.002 [DOI] [PubMed] [Google Scholar]
- Yárnoz-Yaben S (2010). Attachment style and adjustment to divorce. The Spanish Journal of Psychology, 13(1), 210–219. doi: 10.1017/S1138741600003796 [DOI] [PubMed] [Google Scholar]