Abstract
Few studies have examined the intersection of race/ethnicity and socioeconomic status on experiences of minority stressors among lesbian, gay, and bisexual adults. We examined whether there are differences in reports of minority stressors (i.e., enacted, anticipated, and internalised stigma) by race/ethnicity and socioeconomic status, and whether socioeconomic status moderates the associations between race/ethnicity and minority stressors. We analysed data from Project Stride, a community-based sample of 396 self-identified lesbian, gay, and bisexual adults in New York City. We conducted a hierarchical multiple regression analysis to examine the associations between race/ethnicity and socioeconomic status on minority stressors. In adjusted models, African American and Latinos sexual minority adults experienced greater anticipated stigma relative to their White-counterparts. Socioeconomic status significantly moderated the association of race/ethnicity and enacted stigma. For African Americans, higher socioeconomic status was associated with more enacted stigma, whereas higher socioeconomic status was associated with reduced enacted stigma among Whites. Minority stress processes are likely to operate differently for sexual minority people of colour compared with White sexual minority people, and for higher socioeconomic status versus lower socioeconomic status sexual minority people. Future research should consider intersectional axes of identity that contribute to enacted stigma and disparities in mental and physical health, especially for African American sexual minority adults.
Keywords: sexual minority, minority stress, homophobia, socioeconomic status, race, stigma
Introduction
Sexual minority individuals (i.e. lesbian, gay, and bisexual) in the USA continue to face violence and experiences of stigma based on their sexual identities, attractions, and behaviours (Lick, Durso and Johnson 2013; Burton et al. 2013). Sexual minority-specific stigma has been linked to poor health outcomes among sexual minority populations (Lehavot and Simoni 2011; Whitehead, Shaver and Stephenson 2016). Herek, Gillis, and Cogan (2009) described three domains of stigma commonly experienced among sexual minority individuals: anticipated stigma (i.e., concern for possible future instance of discrimination), internalised stigma (i.e., devaluation of self, based on sexual orientation), and enacted stigma (i.e., actual instances of experienced discrimination) (Herek, Gillis and Cogan 2009). Each of these types of stigma have been documented across sexual minority populations (Gamarel et al. 2012; Whitehead, Shaver and Stephenson 2016; Frost, Lehavot and Meyer 2015; Lehavot and Simoni 2011; Pachankis et al. 2018).
The minority stress model posits that stigma and the resulting social stress experienced by sexual minority individuals contribute to adverse health outcomes (Meyer 1995). According to this model, people of disadvantaged social status or with marginalised identities – e.g., due to their race, gender or sexual orientation – are frequently exposed to excess social stress related to prejudice and stigma, which in turn can affect health processes at biological and behavioural levels (Meyer 1995; King et al. 2003; Conron, Mimiaga and Landers 2010; Frost, Lehavot and Meyer 2015). Stigma experienced by sexual minority individuals contributes to a higher incidence of poor mental and physical health outcomes among sexual minority people compared to their heterosexual counterparts (Meyer 2013; Institute of Medicine 2011). However, few studies have examined if minority stress experiences vary by race and socio-economic status within sexual minority populations.
In addition to the persisting racial and ethnic health disparities in the general US population (Dressler 2005), evidence suggests that there may be further risk for increased health problems among sexual minority people of colour compared to White sexual minority people (Meyer 2003; Whitehead, Shaver and Stephenson 2016; Molina et al. 2014). Such patterns of health disparities point to the importance of investigating health outcomes at the intersection of multiple social identities, such as sexual orientation and race/ethnicity. An intersectionality framework (Bowleg 2012) proposes that sexual minority people of colour may be at unique risk for exposure to enacted, anticipated, and internalised stigma based on the multiple axes of stigmatised identities that they inhabit. For example, Calabrese et al. (2015) found that Black sexual minority women experienced poorer mental health outcomes as well as poorer psychological and social wellbeing relative to White sexual minority women. The same authors observed that Black sexual minority women experienced greater enacted stigma than White sexual minority women (Calabrese et al. 2015). It is possible that different mechanisms, such as exposure to more complex forms of institutionalised prejudice and social macroaggressions, contribute to these mental health outcomes disparities among Black compared with White sexual minority women.
Sexual minority people of colour are faced with the impact of living in a racist and heterosexist society, influencing their experiences in managing heterosexist stigma within racial minority communities or racism within sexual minority communities (Moradi et al. 2010). Research that has been conducted with sexual minority people of colour has shown that African American and Latino gay and bisexual men have higher levels of internalised stigma than White gay and bisexual men (O’Leary et al. 2007). The impact of multiple marginalised identities on mental health was further demonstrated in a study by Szymanski and Gupta (2009) who found that internalised racism and internalised stigma had an additive effect in predicting levels of psychological distress among African American and Asian American sexual minority men and women (Szymanski and Gupta 2009). Also, anticipated stigma has been shown to affect health-seeking behaviours especially among sexual minority individuals of colour. Brenick et al. 2017 examined psychosocial barriers to routine engagement in care among Black women who have sex with women and found that anticipated stigma was associated with significantly lower engagement in care (Brenick et al. 2017). Findings from a nationally representative survey revealed that African American and Latino sexual minority individuals had increased risk of poor health outcomes such as heavy drinking, poor sleep, and stroke (Trinh et al. 2017). In another study using a nationally representative survey, African American sexual minority men had higher risk for sexually transmitted infections including HIV and poor mental health compared with White sexual minority men; in contrast, African American sexual minority women had higher risk for Hepatitis C, poor mental health, and substance use compared with White sexual minority women (Perez et al. 2018). These studies provide evidence that race/ethnicity plays a major role in the health of sexual minority populations in the USA.
Studies suggest that higher socioeconomic status confers health advantages at the population level (Adler and Newman 2002), and thus may be protective against health problems associated with being a racial or sexual minority (McGarrity and Huebner 2014; Williams et al. 1997). However, research investigating socioeconomic status, experiences of enacted stigma, and their impacts on health outcomes report mixed results. Ríos-Salas and Larson (2015) reported that being of higher SES was associated with reduced detrimental effects of enacted stigma on young Latinos’ mental health (Ríos-Salas 2015), whereas Kwate and Goodman (2015) showed that among African Americans, enacted stigma increased with higher education but decreased with higher subjective social status (Kwate and Goodman 2015). In the context of health care, enacted stigma among African American patients was higher among those with higher levels of education and income, whereas White patients reported the opposite pattern (Stepanikova and Oates 2017). A recent study (Pachankis et al. 2018) showed that gay and bisexual men of higher socioeconomic status reported significantly lower levels of anticipated stigma compared to those of lower socioeconomic status; however, this study did not assess differences in the association between socioeconomic status and stigma by race. Recent findings have also shown that increased levels of income and education do not protect African Americans against cardiovascular disease as they do for White Americans (Bell et al. 2018). Other reports have noted that young African American men who grew up wealthy are more likely than their White counterparts to have lower SES as adults (Badger 2018, March 19). These findings suggest that higher socioeconomic status does not always confer the same benefits to African Americans as it does to White Americans and does not necessarily protect against the detrimental effects of enacted stigma.
In the light of the growing literature on minority stress as a determinant of health among sexual minority populations, there is need for an improved understanding about the intersections of sexual orientation, race and socioeconomic status with regard to exposure to sexual minority-specific anticipated, internalised and enacted stigma. Research has documented higher levels of these three domains of stigma among sexual minority individuals and racial/ethnic minority individuals (Frost, Lehavot and Meyer 2015; Gamarel et al. 2012; Whitehead, Shaver and Stephenson 2016), and a nascent literature points to higher enacted, internalised and anticipated stigma among sexual minority people of colour (Bowleg 2012; Bostwick et al. 2014; Calabrese et al. 2015). However, little is known about whether and how socioeconomic status affects this patterning of sexual minority-specific enacted, anticipated and internalised stigma. To our knowledge, only one study examined association between perceived enacted stigma and mental health and showed enacted stigma attributed to SES was the most robust predictor of mental health among gay and bisexual men (Gamarel et al. 2012) but this study did not examine differences by race/ethnicity. Thus, the aims of the current study were to investigate (a) whether sexual minority individuals demonstrated race-based differences in exposure to sexual minority-specific internalised sexual stigma, enacted stigma, and anticipated stigma and (b) whether socioeconomic status plays a moderating role in the relationship between race/ethnicity and each of these indicators of minority stress. We hypothesised that sexual minority individuals of colour would report higher levels of enacted, anticipated, and internalised stigma compared to their White counterparts. We also hypothesised that high socioeconomic status would be associated with lower levels of the three forms of sexual minority-specific stigma (internalised stigma, enacted stigma, and anticipated stigma). As an exploratory hypothesis, we examined whether these forms of stigma would be higher among high- socioeconomic status participants of colour compared with high- socioeconomic status White participants.
Methods
Data for the study were collected as part of Project STRIDE, a large-scale US National Institute of Mental Health-funded research project conducted in the New York City area among diverse populations of sexual minority adults (Meyer, Schwartz and Frost 2008). Three hundred and ninety-six respondents completed a face-to-face interview that included interviewer- and self-administered measures using computer assisted interview and paper and pencil methods. Data was collected between 2004 and 2005.
Further details on recruitment strategies and methods used in Project STRIDE are available elsewhere (Meyer, Schwartz, and Frost 2008)). Briefly, respondents were sampled from a range of venues in New York City in order to maximise diversity within the sample. Recruitment venues included alcohol-serving establishments, other commercial/social establishments, outdoor venues, organised community and social groups, and sexual minority-themed events. To meet eligibility criteria, respondents were 18–59 years-old, resided in New York City for two years or more and self-identified as: (a) lesbian, gay, or bisexual; (b) male or female (and their gender identity matched sex at birth); and (c) white, African-American or Latino. The response rate was 60% and did not differ by race/ethnicity. Sample demographics are presented in Table 1.
Table 1:
Overall characteristics of the study sample (N=396)
| n (%) or Mean (SD), Median (IQR) | |
|---|---|
| Gender | |
| Male | 198 (50.0) |
| Female | 198 (50.0) |
| Age | |
| <30 | 196 (49.5) |
| 31-40 | 121 (30.6) |
| >40 | 79 (19.9) |
| Race | |
| White | 134 (33.8) |
| African American | 131 (33.1) |
| Latino/Hispanic | 131 (33.1) |
| Immigration status | |
| Born in USA | 328 (82.8) |
| Born outside USA | 68 (17.2) |
| Grew up in NYC | |
| Yes | 202 (51.0) |
| No | 194 (49.0) |
| Income Mean (SD) | 21.4 (7.5) |
| Education Mean (SD) | 6.8 (2.1) |
| SES (SD) | 0 (1) |
| Relationship status | |
| In a relationship | 184 (46.5) |
| Not in a relationship | 212 (53.5) |
| Parental status | |
| Has children | 69 (17.4) |
| No children | 327 (82.6) |
| Employment status | |
| Employed | 233 (58.8) |
| Not employed | 163 (41.2) |
| General stress | 1.54 (1.1) |
| Yes | 307 (77.5) |
| No | 89 (22.5) |
| Minority stressors | |
| Internalised stigma M (SD) | 1.4 (0.5) |
| Anticipated stigma M (SD) | 2.1 (0.8) |
| Enacted stigma (SD) | 2.4 (0.6) |
Notes: SES; composite socio-economic status variable created by averaging the standardised scores of education and income. M=Mean. SD= standard deviation. NYC=New York City
Measures
Enacted Stigma.
Enacted stigma was assessed with the Everyday Discrimination scale (Williams et al. 1997), which has been used extensively in studies with sexual minority adults (Gamarel et al. 2012; Frost, Lehavot and Meyer 2015; Calabrese et al. 2015; Ghabrial 2017). The 8-item scale assessed the frequency of discriminatory experiences, such as: being treated with less courtesy, being treated with less respect, receiving poorer services, being treated as not smart, people acting like they are afraid of you, people acting like you are dishonest, people acting like they are better than you, and being called names or insulted (Cronbach’s alpha = 0.84). Frequency of occurrence was reported on a 4-point scale (1 ‘‘often’’ through 4 ‘‘never’’), with higher scores reflecting greater everyday enacted stigma. Summed scores were divided by the number of items to obtain mean total scores for each participant, thereby maintaining the 1–4 response metric.
Anticipated Stigma.
A measure of anticipated stigma assessed the degree to which a participant anticipates being rejected or discriminated against based on his or her sexual orientation. Participants rated their degree of agreement with six statements (e.g. “Most people would willingly accept someone like me as a close friend”) on a 4-point scale ranging from “strongly agree” to “strongly disagree” (Cronbach’s alpha=0.88). Summed scores were divided by the number of items in the scale to obtain mean total scores for each participant, and higher scores reflected greater reports of anticipated stigma.
Internalised Stigma.
Participants completed a 9-item internalised homophobia scale to assess the extent to which individuals have internalised negative beliefs and attitudes about sexual minority individuals (Martin and Dean 1987). Items were rated on a 4-point scale from 1 “often” to 4 “never” (sample item, “How often have you wished you weren’t gay/lesbian/bisexual?” Cronbach’s alpha= 0.84). Summed scores were divided by the number of items in the scale to obtain a mean total score for each participant, and higher scores reflected greater levels of internalised sexual stigma.
Race/ethnicity.
Race/ethnicity was our main exposure variable and was assessed using measures developed and used by the US Census Bureau in US Population Survey of 2000. Participants were categorised as White (non-Hispanic), African American (non-Hispanic), and Latino/Hispanic.
Socioeconomic status.
Education was assessed using a single item indicating the participant’s highest level in school. Participants responded on a scale ranging from 1 (“never attended school”) to 11 (“doctoral degree; PhD, L.L.D, M.D, etc”). Income was assessed using a single item indicating the participant’s total yearly personal income. Participants responded on a scale ranging from 1 (less than $ 1000) to 34 (more than $1,000,000). Education and income were used to compute a composite socioeconomic status measure. Although the use of multiple indicators is ideal to measures socioeconomic status, use of a single indicator is common in the literature (Matthews and Gallo 2011). To compute this variable, first, education and income were standardised by transformation into z -scores so that the mean of these variables was 0 and the standard deviation was 1. Second, the composite socioeconomic status variable was created by averaging the standardised scores.
Covariates.
Sociodemographic variables included in the analysis were age in years (continuous), self-reported sex (dichotomous), employment, immigration status, parental status, relationship status, and experience of general stressful life events over one year measured by the narrative life event interview (Dohrenwend 1993). We adjusted for general stressful life events to show examine differences in minority stressors by race/ethnicity over and above general life stress. General life stress assessed any stressful event that was not related to physical health or involve stigma. Lastly, we included drug use, alcohol use, and tobacco dependence as co-variates given evidence that sexual minority individuals report high prevalence of substance use compared to non-sexual minority individuals (Mimiaga et al. 2010; King et al. 2008; Santos et al. 2014). Substance and alcohol use are considered a coping mechanism for dealing with a biased and discriminatory social environment (Meyer 2003), and thus could confound the association between key variables in this analysis.
Data analysis
We conducted descriptive statistics by race (White, African American, and Latino) for all the study variables for this analysis. To identify any significant differences between these three racial/ethnic groups, we conducted one-way ANOVA tests for continuous variables and Chi square tests for categorical variables. All continuous outcome measures (enacted stigma, anticipated stigma, and internal stigma) were normally distributed (±2 values for skewness and kurtosis) except for age which we categorised into three categories as presented in Table 1. Tukey’s post hoc test was employed to further assess for group differences. Significance was accepted at p-value=0.05.
To test the study hypotheses that minority stressors vary by race, and more specifically that SES moderates the relationship between race and minority stressors (internalised, anticipated, and enacted), we did a hierarchical multiple regression analysis. In the first step, we assessed our main independent variables (race) and each of the three indicators of minority stress (model a). Next, the interaction term between socioeconomic status and race was added to the regression model (Model b). To examine the moderating role of SES, we conducted moderation analysis using PROCESS Macro (Hayes 2013). To avoid potentially problematic high multicollinearity with the interaction term, the variables were centred and an interaction term between socioeconomic status and enacted stigma was created. White race was used as the reference category in all analyses. Significant interaction was probed following steps outlined by Aiken and West (Aiken, West and Reno 1991).
Results
Table 1 presents characteristics of the sample (N=396). The sample consisted of an approximately equal number of African-American (n=131), Latino (n=131), and White (n=134) participants. Half of the participants were aged 30 years or below, and the mean annual income reported was $21,400 (SD=7.5). Most participants were born in the US (82.8%) and half were men. With regard to minority stressors, the mean scores of enacted stigma, anticipated stigma, and internalised stigma for the entire sample were 2.4 (SD=0.6), 2.1 (SD=0.8), and 1.4 (SD=0.5) respectively.
Key sociodemographic characteristics differed by race as shown in Table 2. Latino and African-American participants earned a lower annual income (p<0.01) and had lower education than White participants (p<0.01). With regard to parental status, a higher percentage of African-Americans had children than White and Latino participants (p<0.01). No significant differences were found for the remaining variables. There were significant differences in minority stress by race/ethnicity (see Table 2). African-American and Latino participants reported greater enacted stigma (p=0.01) and higher mean scores of anticipated and internalised stigma compared with White participants (p<0.01). Additionally, a greater proportion of African-American and Latino participants reported experiencing general stressful life events in the past 12 months compared to White participants (p<0.01). A Tukey post-hoc test revealed that all forms of stigma and general stress values were statistically significantly higher among African American and Latino participants.
Table 2:
Descriptive summary of study variables by race (N= 396)
| Variables |
White (n=134) M (SD) or N (%) |
African American (n=131) M (SD) or N (%) |
Latino (n=131) M (SD) or N (%) |
Statistical test valuea |
P-value |
|---|---|---|---|---|---|
| Dependent variables | |||||
| Internalised sexual stigma | 1.3 (0.4) | 1.5 (0.5)* | 1.5 (0.6)* | 5.9 | 0.003 |
| Anticipated stigma | 1.7 (0.6) | 2.3 (0.8)* | 2.2 (0.8)* | 23.2 | <0.001 |
| Enacted stigma | 2.3 (0.5) | 2.5 (0.6)* | 2.5 (0.7)* | 4.3 | 0.014 |
| Covariates | |||||
| General stress (yes) | 85 (63.4) | 106 (80.9)* | 116 (88.6)* | 25.3 | <0.001 |
| Drug/alcohol abuse | |||||
| Alcohol abuse (yes) | 23 (17.4) | 15 (11.7) | 20 (15.6) | 1.7 | 0.42 |
| Drug abuse (yes) | 19 (14.4) | 19 (14.8) | 24 (18.7) | 1.1 | 0.57 |
| Nicotine dependence (yes) | 20 (15.2) | 9 (7.0) | 26 (20.3)† | 9.4 | 0.009 |
| Socio-demographic | |||||
| Gender | 0.13 | 0.93 | |||
| Male | 67 (50.0) | 67 (51.2) | 64 (48.8) | ||
| Female | 67 (50.0) | 64 (48.8) | 67 (51.2) | ||
| Age | 2.2 | 0.70 | |||
| <30 | 67 (50.0) | 66 (50.4) | 63 (48.1) | ||
| 31-40 | 38 (28.4) | 44 (33.6) | 39 (29.8) | ||
| >40 | 29 (21.6) | 21 (16.0) | 29 (22.1) | ||
| Immigration status | 10.7 | 0.005 | |||
| Born in USA | 116 (86.6) | 115 (87.8) | 97 (74.1)** | ||
| Born outside USA | 18 (13.4) | 16 (12.2) | 34 (25.6) | ||
| Grew up in NYC | 74.1 | <0.001 | |||
| Yes | 28 (20.9) | 90 (68.7)* | 84 (64.1)* | ||
| No (Moved to NYC) | 106 (79.1) | 41 (31.3) | 47 (35.9) | ||
| Education | 8 (2) | 6 (2)* | 6 (2)* | <0.001 | |
| Income (K$) | 30 (5.2) | 20 (8.5)* | 19 (7.7)* | <0.001 | |
| Socioeconomic status (SES) | 0.48 (0.6) | −0.23 (1) | −0.26 (1) | <0.001 | |
| Relationship status | 1.9 | 0.39 | |||
| In a relationship | 63 (47.0) | 66 (50.4) | 55 (42.0) | ||
| Not in a relationship | 71 (53.0) | 65 (49.6) | 76 (58.0) | ||
| Parental status | 31.5 | <0.001 | |||
| Has children | 4 (3.0) | 37 (28.2)* | 28 (21.4)* | ||
| No children | 130 (97.0) | 94 (71.8) | 103 (78.6) | ||
| Employment status | 0.9 | 0.65 | |||
| Employed | 83 (61.9) | 76 (58.0) | 74 (56.5) | ||
| Not Employed | 51 (38.1) | 55 (42.0) | 57 (43.5) |
Note. Statistical test value
: one-way ANOVA were conducted for continuous variables and Chi Square tests were conducted for categorical variables.
Post hoc tests revealed significant differences on these values between all the races with African American and Latino reporting high values of stigma and general stress and low education and income compared to White, significance p<0.05.
Post hoc tests revealed significant differences on immigration status between Latino/African American and White.
Post hoc tests revealed significant differences only between African American/Latino with Latinos reporting high nicotine dependence, significance p<0.05
Table 3 presents final fitted multivariable regression models showing the main effects of race/ethnicity and each of the indicators of minority stress (internalised, anticipated, and enacted stigma). We adjusted all models for age, gender, immigration status, nicotine dependence, and general stressful life events over the past 12 months.
Table 3:
Multivariate linear regression for the association between race, socio-economic status, and enacted, anticipated and internalised stigma (N=396)
| Variables | Enacted stigma (n=210) | Anticipated stigma (n=207) | Internalised stigma (n=210) | |||
|---|---|---|---|---|---|---|
| Model 1a | Model 1b | Model 2a | Model 2b | Model 3a | Model 3b | |
| B (SE) | B (SE) | B (SE) | B (SE) | B (SE) | B (SE) | |
| Racea | ||||||
| African American | 0.10 (0.07) | 0.01 (0.08) | 0.44 (0.08)*** | 0.45 (0.10)*** | 0.10 (0.10) | 0.14 (0.07)* |
| Latino | 0.03 (0.07) | −0.07 (0.08) | 0.27 (0.08)*** | 0.26 (0.10)** | 0.13 (0.10)* | 0.16 (0.07)* |
| SES | 0.02 (0.03) | −0.19 (0.08)** | −0.03 (0.04) | −0.04 (0.08) | −0.06 (0.02)* | 0.03 (0.06) |
| SES*African American | 0.29 (0.08)*** | 0.05 (0.10) | −0.09 (0.07) | |||
| SES*Latino | 0.22 (0.08)** | −0.02 (0.10) | −0.12 (0.08) | |||
| R-Squared | 0.26 | 0.29 | 0.37 | 0.38 | 0.07 | 0.073 |
| Adjusted R-Squared | 0.24 | 0.26 | 0.36 | 0.36 | 0.05 | 0.05 |
| F-value | F 10, 367=13.02 | F 12, 365=12.13 | F 10 363=21.71 | F 12, 361=18.10 | F 10, 367=2.79 | F 11,365 =2.52 |
Note. Model a: without interaction. Model b: with interaction. All models were adjusted for age, gender, immigration status, parental status, nicotine dependence, and general stressful life events over the past 12 months.
Reference category = White
p<0.001,
p<0.01,
p<0.05
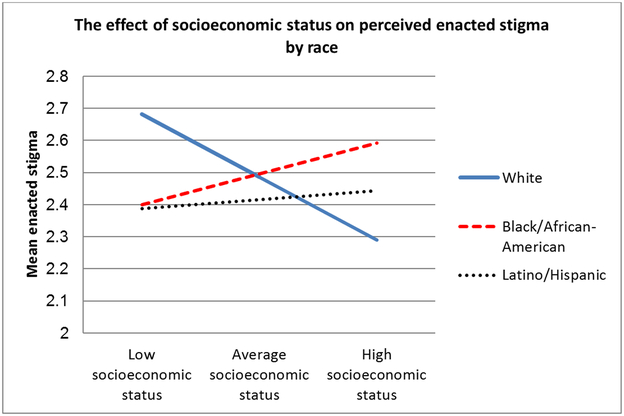
Enacted Stigma
In model 1a, socioeconomic status was significantly and negatively associated with enacted stigma scores (B = −0.19, SE = 0.08, p < .01). In this model, we did not find significant differences in levels of enacted stigma based on race/ethnicity. In model 1b, socioeconomic status significantly moderated the association between identifying as African American and enacted stigma, (B = 0.29, SE = 0.08, p < .01), as well as the association between identifying as Latino and enacted stigma (B = 0.22, SE = 0.08, p < .01). Examination of the interaction plot in Figure 1 showed an enhancing effect such that for White Americans, higher socioeconomic status was associated with lower levels of enacted stigma, whereas for African-Americans higher socioeconomic status was associated with increased levels of enacted stigma. For Latino participants in this study, the slope between socioeconomic status and enacted stigma appeared stable.
Figure 1:
The effect of socioeconomic status on enacted stigma by race. Low socioeconomic status graphed at 1 standard deviation below the mean and high SES graphed at 1 standard deviation above the mean
Internalised stigma
In model 2a, Latinos had significantly higher levels of internalised stigma compared with White participants (B = 0.13, SE = 0.30, p < .05). However, internalised stigma scores did not differ between African-American and White participants. Socioeconomic status was negatively associated with internalised stigma scores (B = −0.06, SE = 0.02, p < .05). In model 2b, none of the interaction terms achieved statistical significance.
Anticipated Stigma
In model 3a, African-Americans (B = 0.44, SE = 0.08, p < .001) and Latinos (B = 0.27, SE = 0.08, p < .001) had significantly higher levels of anticipated stigma compared with White participants. Socioeconomic status was not associated with anticipated stigma. In model 3b, none of the interaction terms achieved statistical significance.
Discussion
These findings reveal complex patterns that demonstrate the importance of considering intersecting marginalised identities (e.g. race/ethnicity, sexual orientation, socioeconomic status) when understanding minority stress processes. African American and Latino sexual minority individuals reported greater reports of anticipated and internalised stigma than their White counterparts. Unexpectedly, there were no differences in enacted stigma by race/ethnicity. However, interaction effects between socioeconomic status and race/ethnicity revealed that higher levels of socioeconomic status were associated with lower levels of enacted stigma for Whites but not for African American and Latino participants. This finding suggests that socioeconomic status does not necessarily equally confer protective effects against enacted stigma for all subgroups within disadvantaged populations. Consistent with an intersectionality writings on sexual minority individuals (Bowleg 2012), our findings highlight the importance of examining differences by race/ethnicity in the experience of these minority stressors among sexual minority adults.
Indeed, in examining the moderating effect of socioeconomic status and those who identified as African American, we found greater levels of enacted stigma among African Americans with higher socioeconomic status indicators, suggesting that increasing levels of income and education can contribute to greater exposure to, or recognition of, enacted stigma. By contrast, a strong protective effect of higher socioeconomic status against enacted stigma was observed for White participants. These findings are consistent with research by Stepanikova and Oates (2017) who demonstrated that African Americans with higher income and education levels report greater enacted stigma compared to their lower socioeconomic status counterparts, whereas the pattern was reversed for White patients. For Latino participants in our study, the slope between socioeconomic status and enacted stigma appeared constant. However, compared with the negative slope for White participants, a consistent pattern emerges – that increasing socioeconomic status does not confer protective benefits for sexual minority individuals of colour as it does for White individuals with regard to enacted stigmaHowever, more research is needed to clarify whether these associations reflect actual exposure to enacted stigma, sensitivity to enacted stigma, or awareness/recognition of enacted stigma.
We did not observe an interaction between race/ethnicity and socioeconomic status for anticipated and internalised stigma. Reasons for these distinctions are unclear but may reveal nuanced patterns and social contexts by which different minority stress processes might operate. Conceptually, anticipated and internalised stigma represent factors that are more proximal to the self – i.e., the psychological expectation or internalisation of stigma – whereas enacted stigma represents interpersonal processes that occur in social interactions. The latter type of stigma might be particularly potent for higher socioeconomic status African American and Latino sexual minority people who inhabit heterogeneous social, work, or other environments where direct intergroup contact is more likely. However, anticipated and internalised stigma are also responsive to social context and may fluctuate over time. Longitudinal designs that assess momentary perceptions of stigma (anticipated, internalised, enacted) would be useful in examining intersectional patterns of minority stress across multiple situations.
Findings from this research have implications for our understanding of minority stress as a determinant of health in sexual minority populations (Meyer 1995; Frost, Lehavot and Meyer 2015), and urge for the consideration of intersectional axes of identity that can influence minority stress processes. For example, research about health processes or outcomes in sexual minority populations might mask important within-group differences that differentiate sexual minority subpopulations – including differences associated with race/ethnicity or socioeconomic status, as well as other key groups that fall within the sexual minority spectrum (e.g., individuals who identify as pansexual, asexual, and queer). Findings from this research also have implications for the broader body of literature on socioeconomic status gradients in population health, which have been well characterised (Adler and Newman 2002; Marmot 2005). Specifically, the current findings challenge a unified view of socioeconomic status as a health protective factor. In the findings presented here, higher levels of socioeconomic status were associated with greater enacted stigma among African American and Latino sexual minority compared with their White counterparts. Due to repeated exposures to enacted stigma over time, high-socioeconomic status African American and Latino sexual minority adults may have unique physical health vulnerabilities. Additional research is needed to clarify whether higher levels of exposure to enacted stigma based on sexual identity or race/ethnicity among high-socioeconomic status African American and Latino sexual minority are associated with poor physical health outcomes.
Limitations
There are limitations to this study. Due to the cross-sectional design, we cannot derive inferences about causation or temporality among variables. As noted, the cross-sectional survey did not capture distinctions in self-reports of anticipated, internalised, and enacted stigma across varying social contexts (e.g., racially/ethnically homogenous versus heterogeneous contexts). The study involved a non-representative sample of targeted venues in New York City; thus, findings might not be generalisable to other geographic settings in the USA or in international contexts. Self-report measures of stigma might have been prone to recall or response biases. Further, the internalised stigma scale may not capture experiences of bisexual individuals; therefore, future research with more culturally-specific measures on internalised stigma related to bisexuality is warranted. Data used in this analysis were collected between 2004 and 2005, and further research is needed to examine whether the findings reported persist in the context of current historical and political trends. Further analyses are also necessary to examine intersectional associations between race/ethnicity, SES, minority stress, and physical health outcomes in sexual minority populations.
Conclusion
In conclusion, findings from this research support the need for an intersectional view of minority stress processes in understanding the health for sexual minority adults. Specific consideration should be given to the roles of race/ethnicity and socioeconomic status as population variables contributing important complexity to the minority stress framework. Findings from this research also prompt a nuanced view in which higher socioeconomic status can potentially confer unique forms of minority stress for sexual minority individuals of colour –Future research will be important to corroborate findings reported here and to examine longitudinal effects of intersectional minority stress processes on sexual minority population health outcomes. Qualitative research can be particularly useful in examining the lived experiences of intersectional sexual minority individuals, particularly sexual minority people of colour across different levels of the socioeconomic status continuum.
References
- Adler NE, and Newman K. 2002. “Socioeconomic Disparities in Health: Pathways and Policies.” Health Affairs (Millwood) 21 (2): 60–76. [DOI] [PubMed] [Google Scholar]
- Aiken Leona S., West Stephen G., and Reno Raymond R.. 1991. Multiple Regression: Testing and Interpreting Interactions. Thousand Oaks: SAGE. [Google Scholar]
- Badger E 2018. “Extensive data shows punishing reach of racism for black boys.” The New York Times, March 2019 https://www.nytimes.com/interactive/2018/03/19/upshot/race-class-white-and-black-men.html. [Google Scholar]
- Bell CN, Thorpe RJ Jr., Bowie JV, and LaVeist TA. 2018. “Race Disparities in Cardiovascular Disease Risk Factors Within Socioeconomic Status Strata.” Annals of Epidemiololgy 28 (3):147–152. [DOI] [PubMed] [Google Scholar]
- Bostwick WB, Boyd CJ, Hughes TL, West BT, and McCabe SE. 2014. “Discrimination and Mental Health Among Lesbian, Gay, and Bisexual Adults in the United States.” American Journal of Orthopsychiatry 84 (1):35–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L 2012. “The Problem With the Phrase Women and Minorities: Intersectionality-an Important Theoretical Framework for Public Health.” American Journal of Public Health 102 (7):1267–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenick A, Romano K, Kegler C, and Eaton Lisa A.. 2017. “Understanding the influence of stigma and medical mistrust on engagement in routine healthcare among black women who have sex with women.” LGBT health 4 (1):4–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton CM, Marshal MP, Chisolm DJ, Sucato GS, and Friedman MS. 2013. “Sexual Minority-related Victimization as A Mediator of Mental Health Disparities in Sexual Minority Youth: A Longitudinal Analysis.” Journal of Youth and Adolescence 42 (3): 394–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calabrese SK, Meyer IH, Overstreet NM, Haile R, and Hansen NB. 2015. “Exploring Discrimination and Mental Health Disparities Faced by Black Sexual Minority Women Using a Minority Stress Framework.” Psychololgy of Women Quarterly 39 (3): 287–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conron KJ, Mimiaga MJ, and Landers SJ. 2010. “A Population-based Study of Sexual Orientation Identity and Gender Differences in Adult Health.” American Journal of Public Health 100 (10):1953–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dohrenwend BP, Raphael K, Schwartz S, Stueve A, & Skodol A. 1993. “The Structured Event Probe and Narrative Rating Method for Measuring Stressful Life Events” In Handbook of Stress: Theoretical and Clinical Aspects, edited by Goldberger L and Bresnitz S, 174–199. New York: Free Press; 2nd edition. [Google Scholar]
- Dressler WW, Oths KS, & Gravlee CC. 2005. “Race and Ethnicity in Public Health Research: Models to Explain Health Disparities.” Annual review of Anthropology 34: 231–252. [Google Scholar]
- Frost DM, Lehavot K, and Meyer IH. 2015. “Minority Stress and Physical Health Among Sexual Minority Individuals.” Journal of Behavioral Medicine 38 (1): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamarel KE, Reisner SL, Parsons JT, and Golub SA. 2012. “Association between Socioeconomic Position Discrimination and Psychological Distress: Findings from A Community-based Sample of Gay and Bisexual Men in New York City.” American Journal of Public Health 102 (11): 2094–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC 2008. “A multilevel Analysis of the Relationship Between Institutional and Individual Racial Discrimination and Health Status.” American Journal of Public Health 98 (9 Suppl): S48–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghabrial Monica A. 2017. ““Trying to Figure Out Where We Belong”: Narratives of Racialized Sexual Minorities on Community, Identity, Discrimination, and Health.” Sexuality Research and Social Policy 14 (1): 42–55. [Google Scholar]
- Hayes Andrew F. 2013. “Introduction to mediation, moderation, and conditional process analysis: A regression-based approach”A Regression-Based Approach, edited by Little TD, 77–82. Guilford Press; 2nd edition. [Google Scholar]
- Herek GM, Gillis JR, and Cogan JC. 2009. “Internalized Stigma Among Sexual Minority Adults: Insights from A Social Psychological Perspective.” Journal of Counseling Psychology 56 (1): 32. [Google Scholar]
- Hudson DL, Bullard KM, Neighbors HW, Geronimus AT, Yang J, and Jackson JS. 2012. “Are Benefits Conferred With Greater Socioeconomic Position Undermined by Racial Discrimination Among African American Men?” Journal of Mens Health 9 (2): 127–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. 2011. “The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding.” Washington, DC: Institute of Medicine. [PubMed] [Google Scholar]
- King M, McKeown E, Warner J, Ramsay A, Johnson K, Cort C, Wright L, Blizard R, and Davidson O. 2003. “Mental Health and Quality of Life of Gay Men and Lesbians in England and Wales: Controlled, Cross-sectional Study.” The British Journal of Psychiatry 183:552–8. [DOI] [PubMed] [Google Scholar]
- King M, Semlyen J, Tai SS, Killaspy H, Osborn D, Popelyuk D, and Nazareth I. 2008. “A Systematic Review of Mental Disorder, Suicide, and Deliberate Self Harm in Lesbian, Gay and Bisexual People.” BMC Psychiatry 8(1): 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwate NO, and Goodman MS. 2015. “Racism at the Intersections: Gender and Socioeconomic Differences in the Experience of Racism Among African Americans.” American Journal of Orthopsychiatry 85 (5): 397–408. [DOI] [PubMed] [Google Scholar]
- Lehavot K, and Simoni JM. 2011. “The Impact of Minority Stress on Mental Health and Substance Use Among Sexual Minority Women.” Journal of Consulting and Clinical Psychology 79 (2): 159–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lick DJ, Durso LE, and Johnson KL. 2013. “Minority Stress and Physical Health Among Sexual Minorities.” Perspectives on Psychological Science 8 (5): 521–48. [DOI] [PubMed] [Google Scholar]
- Marmot M 2005. “Social Determinants of Health Inequalities.” The Lancet 365 (9464): 1099–104. [DOI] [PubMed] [Google Scholar]
- Matthews KA, and Gallo LC. 2011. “Psychological Perspectives on Pathways Linking Socioeconomic Status and Physical Health.” Annual Review of psychology 62:501–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGarrity LA, and Huebner DM. 2014. “Is being Out About Sexual Orientation Uniformly Healthy? The Moderating Role of Socioeconomic Status in a Prospective Study of Gay and Bisexual men.” Annals of Behavioral Medicine 47 (1): 28–38. [DOI] [PubMed] [Google Scholar]
- Meyer IH 2003. “Prejudice as Stress: Conceptual and Measurement Problems.” American Journal of Public Health 93 (2): 262–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, Schwartz S, and Frost DM. 2008. “Social Patterning of Stress and Coping: Does Disadvantaged Social Statuses Confer More Stress and Fewer Coping Resources?” Social Science & Medicine 67 (3): 368–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH 1995. “Minority Stress and Mental Health in Gay Men.” Journal of Health and Social Behavior 36 (1): 38–56. [PubMed] [Google Scholar]
- Meyer Ilan H. 2013. “Prejudice, Social Stress, and Mental Health in Lesbian, Gay, and Bisexual Populations: Conceptual Issues and Research Evidence.” Psychological Bulletin 129 (5): 674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mimiaga MJ, Reisner SL, Fontaine Y-M, Bland SE, Driscoll MA, Isenberg D, Cranston K, Skeer MR, and Mayer KH. 2010. “Walking the Line: Stimulant Use During Sex and HIV risk Behavior Among Black Urban MSM.” Drug & Alcohol Dependence 110 (1): 30–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina Y, Lehavot K, Beadnell B, and Simoni J. 2014. “Racial Disparities in Health Behaviors and Conditions Among Lesbian and Bisexual Women: The Role of Internalized Stigma.” LGBT Health 1 (2): 131–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moradi B,, Wiseman MC, DeBlaere C,, Goodman MB, Sarkees A, Brewster ME, and Huang Y. 2010. “LGB of Color and White Individuals’ Perceptions of Heterosexist Stigma, Internalized Homophobia, and Outness: Comparisons of levels and links.” The Counseling Psychologist 38 (3): 397–424. [Google Scholar]
- O’Leary A, Fisher HH, Purcell DW, Spikes PS, and Gomez CA. 2007. “Correlates of Risk Patterns and Race/Ethnicity Among HIV-positive Men Who Have Sex With Men.” AIDS and Behavior 11 (5): 706–715. [DOI] [PubMed] [Google Scholar]
- Pachankis JE, Sullivan TJ, Feinstein BA, and Newcomb ME. 2018. “Young Adult Gay and Bisexual Men’s Stigma Experiences and Mental Health: An 8-year Longitudinal Study.” Developmental Psychology 54 (7): 1381. [DOI] [PubMed] [Google Scholar]
- Perez AE, Gamarel KE, van den Berg JJ, and Operario D. 2018. “Sexual and Behavioral Health Disparities Among African American Sexual Minority Men and Women.” Ethnicity & Health 3: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ríos-Salas V, & Larson A. 2015. “Perceived Discrimination, Socioeconomic Status, and Mental Health Among Latino Adolescents in US immigrant families.” Children and Youth Services Review 56: 116–125. [Google Scholar]
- Santos GM, Rapues J, Wilson EC, Macias O, Packer T, Colfax G, and Raymond HF. 2014. “Alcohol and Substance Use Among Transgender Women in San Francisco: Prevalence and Association With Human Immunodeficiency Virus Infection.” Drug and Alcohol Review 33 (3): 287–295. [DOI] [PubMed] [Google Scholar]
- Stepanikova I, and Oates GR. 2017. “Perceived Discrimination and Privilege in Health Care: The Role of Socioeconomic Status and Race.” American Journal of Preventive Medicine 52 (1s1): S86–s94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szymanski DM, and Gupta A. 2009. “Examining the Relationship Between Multiple Internalized Oppressions and African American Lesbian, Gay, Bisexual, and Questioning Persons’ Self-esteem and Psychological Distress.” Journal of Counseling Psychology 56 (1): 110. [Google Scholar]
- Trinh MH, Agenor M, Austin SB, and Jackson CL. 2017. “Health and Healthcare Disparities Among U.S. Women and Men at the Intersection of Sexual Orientation and Race/Ethnicity: A Nationally Representative Cross-sectional Study.” BMC Public Health 17 (1): 964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehead J, Shaver J, and Stephenson R. 2016. “Outness, Stigma, and Primary Health Care Utilization among Rural LGBT Populations.” PLoS One 11 (1): e0146139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, and Anderson NB. 1997. “Racial Differences in Physical and Mental Health: Socio-economic Status, Stress and Discrimination.” Journal of health psychology 2 (3): 335–351. [DOI] [PubMed] [Google Scholar]