Abstract
Vision loss, dementia, and motor and speech declines all impact the educational experience of individuals with Batten disease and can adversely impact effective learning. There are as yet limited data to support evidence-based approaches to meeting the educational needs of affected individuals. This paper provides an overview of recent work to evaluate and address educational issues with a life-long perspective relevant to individuals with juvenile-onset neuronal ceroid lipofuscinosis (JNCL) and the professionals that provide them with educational support. In particular, several main activities of the recently completed ‘JNCL and Education’ project are summarised, including a survey of parents, educational professionals and social/health workers, development of a formative assessment tool to identify and respond to an individual student’s strengths and needs in the learning environment, and proposed strategies for prolonging literacy and language skills. A key concept that should be emphasised in the educational plan for students with JNCL is that of of ‘proactive’ and ‘hastened’ learning, that is, providing an early emphasis on adaptive skills that will be required in the later stages of disease progression when new learning will be more difficult to achieve. An additional key concept is participation in real-life activities to maintain skills and quality of life, particularly in the later stages of disease progression.
Keywords: Batten disease; JNCL; CLN3 disease; paediatric dementia, education
1. Introduction
Among children with NCL disorders, the myriad symptoms including vision loss, seizures, cognitive, communication and motor decline, and changes in mood and behaviour impact daily function, including participation in school and social engagement with peers and the community.1–4 Early publications on the educational needs for individuals with NCL disorders focused upon school-age children with juvenile-onset phenotypes of Batten disease.2,5–9 Though preceding genetic discovery of NCL disorders, many of the individuals described therein might likely be diagnosed today with CLN3 disease. These early papers, largely case descriptions, illustrated the progressive declines in vision, motor abilities, cognition and behaviour requiring increased educational support. It was also noted that there were limited data to promote evidence-based practices in the school environment or to inform school personnel. Nonetheless, these early papers recognised that such children belonged in the school setting, could have a meaningful educational experience, and were entitled to receive support to enable participation in school and in the local community to the fullest extent possible.
More recently several projects have been completed or are in progress to evaluate and address the educational and social support needs of individuals with juvenile-onset NCL disorders. In this article, we will review selected findings from these projects (each of which involved certain of the authors of the current paper), and discuss key concepts relevant to individuals with JNCL. Because much of this work did not seek confirmation of the genetic diagnosis we will use the inclusive term, juvenile neuronal ceroid lipofuscinosis (JNCL) unless genetic status was specifically considered in the research. This paper will focus in particular on several key outcomes from the ‘JNCL and Education Project’: 1) Development of a new educational assessment tool for individuals with JNCL, the “Educational Development Observation” (EDO) tool (HRA, BC, BE, AGT); 2) Selected results from a survey and interviews of parents and educational professionals (BE, AGT); and 3) Development of a framework for supporting the transition to young adulthood for affected individuals (SR, BE). This paper will also summarise ongoing work of a separate (though complementary to the JNCL and Education Project), therapeutic music intervention programme for persons with JNCL (RA, AO). First, however, we present a brief overview of the concept of paediatric dementia, illustrated with recent data from another separate, prospective longitudinal study of cognitive changes in affected children (HRA).
2. Childhood Dementia
Dementia is a pathological loss of previously attained cognitive skills impacting memory, judgment and reasoning skills, language, and other abilities, and can also involve changes in behaviour and personality. Individuals with dementia experience declines in their ability to perform age-expected activities of daily living resulting in loss of independence and personal autonomy.10 Though rare, childhood-onset dementia exhibits the same overall features as dementia in the elderly population. Additionally, paediatric dementia may also be characterised by an intermediate phase of deceleration in cognitive growth and/or a plateau in skill attainment, prior to cognitive decline.11
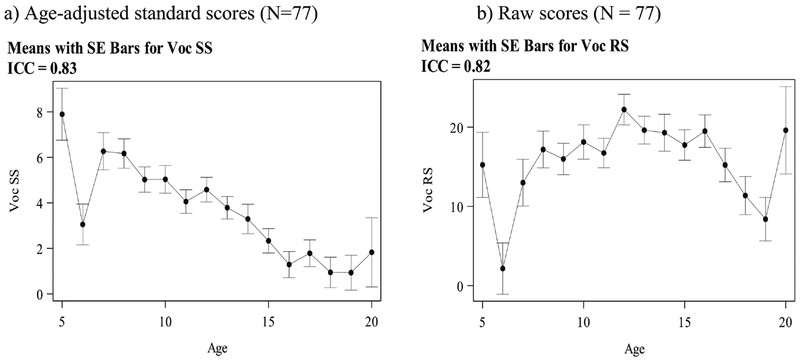
In JNCL, paediatric dementia is a core feature of the overall neurodegenerative disease process.1,12–16 Recent work by the University of Rochester Batten Center (Adams et al., unpublished) shows that children with JNCL demonstrate an initial slowing in cognitive attainment followed by an eventual loss of cognitive skills. In a 15-year, prospective longitudinal study, symptomatic children (i.e., at least vision loss) with genetically confirmed CLN3 disease completed a brief evaluation of attention, memory, language, and verbal reasoning on an approximately annual basis. Full details of the study methods have been described previously.13 The longitudinal analysis included N=77 individuals (n= 42 males) with CLN3 disease; at least n=40 had completed at least one assessment and n=21 completed ≥ 3 evaluations. Figures 1a and 1b present plots (adjusted for multiple assessments within subjects over time) of the change in age-adjusted ‘scaled scores’ (SS) and raw scores on the Vocabulary subtest of the Wechsler Intelligence Scale for Children – Fourth edition (WISC-IV), a proxy for general verbal reasoning skills. Age-adjusted scaled scores are normalized so that the mean score for any age = 10 (standard deviation = 3), and scores between 6 – 14 fall within the average range. Thus, at any chronological age, a child with an age-adjusted scaled score = 10 is considered as performing in the average range compared to same age peers, and in typically developing children the majority of age-adjusted scores will continue to fall within the average range band over increasing years of age. By contrast, raw scores describe non-adjusted performance on a test, i.e., how many test items were passed. For example, if a child (of any age) passes 7 of 10 possible items on a test, their raw score = 7. Raw scores may or may not change in a linear fashion over time, and the pattern of change in raw scores will vary for different tasks and domains of skill.
Figure 1.
Declines in age-expected verbal reasoning abilities (Figure 1a); Within-subject growth and subsequent declines in verbal reasoning (Figure 1b)
Figure 1a illustrates that even in the early years after diagnosis, children with CLN3 disease obtain low-average to below-average scaled scores on the WISC-IV Vocabulary task compared to healthy children (for which the normative sample mean = 10, s.d. = 3), and that task performance declines markedly over time (Fig 1a., y axis) as children grow older (Fig 1a., x axis) in relation to healthy, same-age peers. However, Figure 1b which presents ‘raw’ (non-age-adjusted) data offers a more nuanced understanding of cognitive change in young persons with CLN3 disease. Raw scores reflect subjects’ performance without regard for age-based comparisons and permit construction of a ‘growth curve’ of cognitive change over time. In essence, the raw score curve shows the number of test items correctly passed (Fig 1b., y axis) by children in this sample, plotted as a function of chronological age (Fig 1b., x axis). The raw score curve for the WISC-IV Vocabulary test (Voc RS) shows that children with CLN3 disease do experience initial modest gains in verbal reasoning skills (albeit to a lesser extent than to healthy peers) prior to an eventual slowing and then decline in previously attained skills.
An understanding of the anticipated course of paediatric dementia in JNCL/CLN3 disease makes it possible to tailor educational interventions to prepare and support the affected child or young person with this disease.1 Specifically, instruction should consider the window of opportunity for learning (i.e., prior to significant cognitive decline) and the concept of ‘hastened learning’ or an intensification of early learning of complex skills and interests. Additionally, precautionary or proactive learning should be emphasized; this is a focus upon learning of skills not needed at the moment but that will be required in the future. In particular, for children with JNCL, proactive learning should include the development of daily independence skills such as orientation & mobility and activities of daily living, braille and computer skills (or other tactile systems for literacy and numeracy) to anticipate vision loss and eventual blindness, and introduction of augmentative/alternative communication (AAC) systems in anticipation of the eventual loss of oral communication abilities. The work of the JNCL and Education Project, though conducted separately from the research presented above, considers the evolving cognitive support needs of children with JNCL. Below the paper presents the background and methods for the JNCL and Education Project, and summarise several key outcomes.
3. The JNCL and Education Project
3.1. Project Background.
The JNCL and Education Project (henceforth, the ‘Project’) was a multinational collaboration among NCL education and advocacy specialists representing 6 nations and 18 different organisations (comprising family support organisations, advocacy groups and educational consultation services), schools and academic and medical institutions focusing on the educational and social care needs of individuals with the juvenile neuronal ceroid lipofuscinosis disorder (JNCL).17 The Project was supported through funding by Erasmus+, the European Union’s programme to support educational and other youth initiatives. Outcomes and ongoing Project activities were presented at a special satellite session at the16th International Conference on Neuronal Ceroid Lipofuscinoses (London, UK 12–16 Sept 2018) and subsequently at a meeting to launch a JNCL and Education textbook1 (Snekkersten, Denmark 16–18 Nov 2018).
3.2. Project Survey – Methods.
The Project’s elements included parent- and school-based surveys and semi-structured interviews, and development of an evaluation tool, the ‘Educational Development Observation’ (EDO) to aid schools in identifying areas of strength and support needs for children with juvenile-onset NCL specifically (JNCL). Full details of the survey methods and results, EDO implementation, and recommendations for educational supports are published in a recent textbook (“Juvenile Neuronal Ceroid Lipofuscinosis, Childhood Dementia and Education”1); production of the textbook was itself a component of the Project. Surveys were disseminated to parents, school-based professionals, and social workers/health professionals to describe existing educational services and needs, and evaluate the well-being and quality of life of children and young persons with JNCL. The initial intent of the project was to have each individual with JNCL (who was rated in the surveys) evaluated by both a parent and a school professional or other daily caregiver. Ultimately this was not possible; some school personnel or other caregivers did not participate in the survey because remuneration was unavailable to support their time. This resulted in a total of 111 surveys completed by parents of individuals with JNCL (including n=33 bereaved parents), and 81 surveys completed by professionals. In addition, due to missing responses to some survey items, sample sizes vary across different sections of the survey. Among the survey respondents, themes identified via the surveys were explored in greater depth through semi-structured interviews with 25 parents and 30 professionals. Identifying information regarding affected individuals was not provided in the surveys, hence it is not possible to determine how many unique affected individuals were rated, only the number of surveys that were returned, i.e., some, but not all affected individuals were rated by a parent and by a professional. Surveys could be completed electronically or on paper. They were disseminated to parents and professionals in Norway, Finland, Denmark, Germany, the United Kingdom, and the United States of America. In Norway, Finland, and Denmark, surveys were provided to all individuals known in those countries to be parents of affected children or professionals working with JNCL-affected students. In the other three nations, surveys were disseminated only to those who had made contact with the Batten disease support organization of their respective country and expressed interest in participation.
3.2. JNCL and Education Project Survey: Important Survey Outcomes
Onset of educational problems:
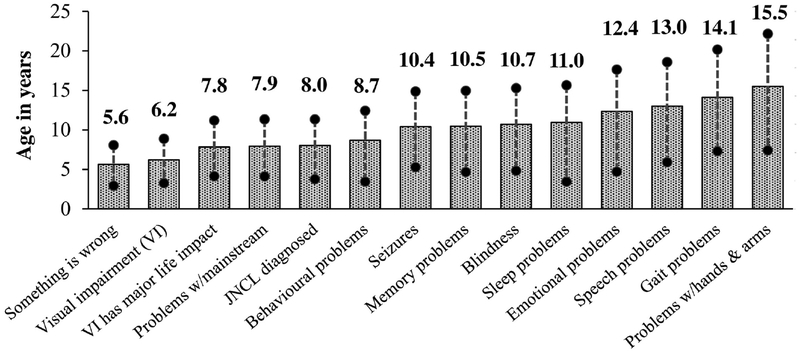
Parents of children with JNCL were asked to retrospectively estimate the age of onset for various symptoms such as vision loss, challenging behaviours, and difficulties in learning (N = 111 parents; Figure 2). Preceding diagnosis by approximately 2 ½ years, parents already had a sense that ‘something was wrong’ with their child (average age =5.6 years), and at the time of diagnosis (average age = 8.0 years), children were already viewed as having difficulty obtaining goals defined in the mainstream educational curriculum.
Figure 2.
Average age at which parents reported selected JNCL symptoms (N = 111)
Educational service provision:
The JNCL and Education Project also surveyed 81 and interviewed 30 (some but not all interviewees were a subset of the survey group) non-medical professional staff (e.g., teachers, classroom aides, visual impairment specialists, etc.) working with JNCL-affected children and young persons. Many expressed difficulties with tasks such as defining educational goals, completing educational plans, and implementing appropriate interventions for their student with JNCL due to the unpredictable nature of the disease. Survey results also indicated that personnel lacked adequate resources and information to build sufficient local competence to support affected individuals.1
Communication and Language:
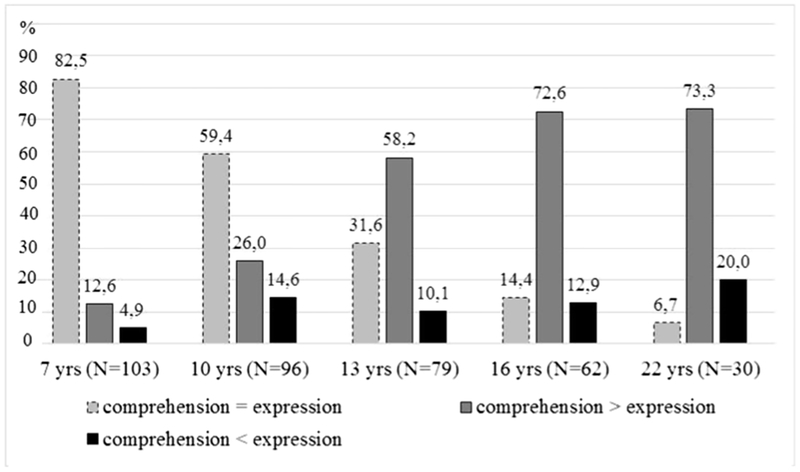
Language use involves both receptive comprehension and expression of ideas. Parents completing the JNCL and Education Project survey were asked to compare their child’s comprehension in relation to expressive language abilities. Figure 3 shows the changes in comprehension and expressive language skills across affected individuals of different ages. During the early primary school years, a time that typically coincides with symptom onset and diagnosis, receptive and expressive language skills were rated as comparable for the majority of affected children. With increasing age (considered a reasonable proxy for disease progression in this condition), children’s expressive language abilities declined1. However, it was thought by parents that comprehension was retained better than oral expression.
Figure 3.
Proportion of individuals with JNCL at different ages whose comprehension is rated as better, worse, or the same as oral expression
Most individuals with JNCL in the Project survey were described by parents as having more than one specific speech problem. Speech problems became noticeable in early teens for most individuals. In the total sample of parent surveys (N=111), word finding problems (n=83, 75%) and speech dysfluency (i.e., cluttering or stuttering) (n=47, 42%) were the two most high-frequent specific speech problems. Limited vocabulary with repetition of the same words became prominent during the late teen years. The mean age for those that developed unintelligible speech was 20.3 years (n=32).
For children with JNCL, who lose their vision, speech is a particularly important mode of communication. Parents of affected individuals were asked to evaluate the extent of social consequences based on speech problems (1 = no negative effect; 5 = very high negative effect). 43% (46/106) reported that speech problems had a ‘high’ or a ‘very high’ negative effect on social life; none reported there to be ‘no negative effect’. Within the sample, 14% (15/106) had not yet developed any problems with speech or language probably because of their young age at the time the survey was completed by their parents.
Communication and language interventions should be an obvious goal in the curriculum of individuals with the JNCL to prepare and compensate for the inevitable speech decline (i.e., precautionary or proactive learning). However, there are few studies on language and communication interventions for this group. In the Project survey, parents were asked if their child had ever received speech and language therapy. Forty percent of parents (43/108) reported that their child had received such services, and that speech and language therapy was first provided at an average age of 9.9 years (SD = 5.6, range = 5 – 25 years). Parents were also asked to evaluate the effect of the therapy (1 = ‘no impact’; 5 = ‘very high impact’). The average evaluation score was = 3.2 (SD = 1.2, range 1–5). Forty-three individuals received speech and language therapy; of these, parents of 18 (42%) reported that this intervention had a ‘high impact’ or ‘very high’ impact while 14 respondents (33%) stated that it had “low impact” or “no impact”. The results suggested that speech and language therapy is useful for some children with JNCL.
Augmentative and alternative communication (AAC) can supplement or substitute for oral speech and may help to close the possible gap between comprehension and expression of language. Unaided forms of AAC are produced by the user without any device but will require some degree of motor ability, such as use of vocalizations, facial expressions, signed language systems, or gestures.18–20 Aided forms of AAC are selected by the user and utilise a device such as a board, book, or electronic device with synthetic speech. In the Project survey, only 11 out of 105 parents (approximately 10%) reported that their child with JNCL received communication training other than speech and language therapy according to parents. Training started at an average age of 12 years (SD = 6.1, range = 3 to 25 years). The low number of individuals receiving this type of training was too small to make any conclusive remarks. While AAC can be considered for children with JNCL due to progressive loss of speech production and expressive language skills over time, more study is needed to assess outcomes in response to AAC interventions.
Manual signing is a form of unaided AAC. For persons with JNCL this should involve keyword signing or sign-supported speech, rather than acquisition of a formal signed language system.21–23 The Project implemented a small, four-month pilot intervention study on manual signs for four Norwegian individuals with JNCL aged 8, 14, 17, and 19 years old, respectively. The objectives were to gather experience with teaching manual signs to children and adolescents with JNCL. The youngest individual (8 years old) learned more than 200 manual signs He continued to learn signs and to sign frequently and spontaneously for several years after the pilot study was concluded. The three older participants learned few signs (no more than 15) and could produce the signs upon request; in a few instances, signs were also used spontaneously for communication. Though this study engaged only a small sample over short time, results are consistent with the progressive declines in cognition, memory, and new learning that are experienced by children with JNCL. That is, the younger participant demonstrated greater learning and more benefit from the intervention than did the older participants with more advanced disease. This may support the importance of an early emphasis upon hastened and precautionary learning. The project also identified several key environmental factors to support learning, including everyday practice, use by as many dialogue partners as possible, and use in multiple settings within and outside the school environment. Learning manual signs may also be possible for some individuals who are older and at more advanced disease stages, but this could not be thoroughly assessed in the current project due to environmental factors that limited participants’ ongoing exposure and practice with manual signing across multiple settings. Overall, Tetzchner et al.1 concluded that manual signing may be a useful communication form for some individuals with JNCL. The authors further noted that training should start early and if possible before speech starts to decline or has become severely impaired, and that it is critical to identify and remove any barriers to learning (e.g., insufficient opportunities for practice), so that learning can be optimized.
Literacy - Reading and Writing:
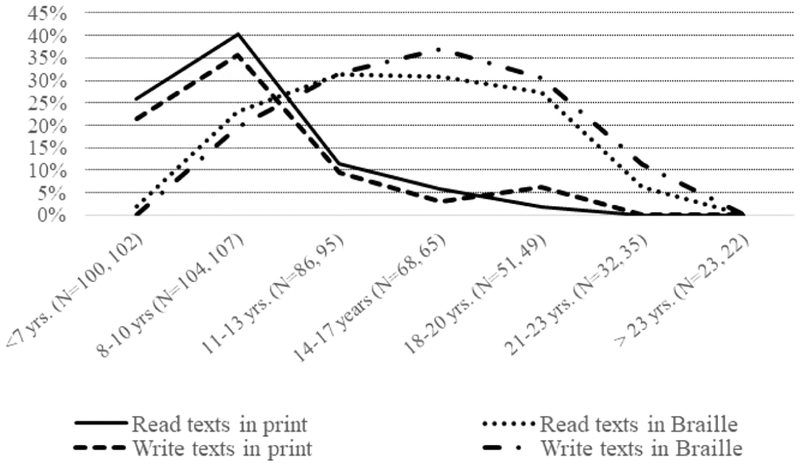
At the time of diagnosis, which often occurs in the early primary school years, many children with JNCL have already begun learning to read and write using vision. In the Project survey, parents were asked to indicate their child’s best level of reading and writing competence at different ages. They were asked if their child was able to read and write letters, words, short texts (up to 10 sentences) or longer texts and books. The survey also asked about the use of print writing versus braille. Braille is currently the most common tactile reading and writing system in use today around the world. Each braille ‘cell’ consists of a rectangular area with the potential to hold up to 6 or 8 embossed tactile perceptible dots arranged in various patterns to represent letters, numbers, punctuation, and words. Results indicated that the students who learned braille early in life became the best braille readers. Figure 4 shows the percentage of participants within different age groups who were able to read and write a text in print or braille, respectively.
Figure 4.
Proportion of individuals with JNCL at different ages who read or write texts in print or Braille
note: Within each age group, Ns are reported for reading and writing, respectively
As shown in Figure 4, print use was greatest at earlier ages and peaked between 8–10 years of age, when 40% of children read printed texts. Braille reading and writing peaked between 14–17 years of age and then declined; the figure also illustrates that for most students with JNCL, the total duration (in years) for Braille use is longer than for reading and writing in print. Nine children between 7–13 years of age were able to read both print and braille texts. Figure 4 also shows that as young persons with JNCL grow older, most do not retain the ability to use braille. Finally, many parents who completed the JNCL and Education Project survey expressed frustration that braille was introduced too late in the disease process to be effectively learned and used by their child.
An additional empirical question is whether students with JNCL can advance to learning the more advanced system of ‘contracted’ braille. Early braille learners first use un-contracted or ‘alphabetic’ (Grade 1) braille, in which each tactile form corresponds in one-to-one fashion to individual Latin letters. Students next advance to Grade 2 braille in which contractions provide substitutions for common whole words or parts of words. This provides greater efficiency when reading and writing and also reduces the physical size of braille-embossed texts. However, a concern for students with JNCL is that the additional cognitive demands upon working memory, long-term recall, and use of strategies required for contracted braille may be challenging, in light of progressive cognitive decline. The Project survey did not specifically ask how many students could use contracted braille, but several parents noted that their child’s memory problems interfered with effective learning of contracted braille.
Because individuals with JNCL may have difficulty mastering braille, alternate tactile reading/writing systems may be considered. The Moon System of Embossed Reading (Moon type) uses simplified versions of capital Latin letters.24,25 Moon type has been used in the UK by some children and adults with visual impairment in combination with learning difficulties, poor tactile discrimination, and/or who were previously visual readers. For these reasons, individuals with JNCL may find it easier to learn Moon rather than braille. In a review of tactile reading systems, the Royal National Institute of Blind People (RNIB) concluded that in comparison to braille, Moon can be learned more quickly among children including those with learning problems and multiple disabilities, and by those with poor fine motor discrimination.24,26 However, RNIB expressed concerns related to limited availability of Moon texts for young learners, the greater physical size of texts (compared to braille), and the lack of equipment and technology available for students to produce their own Moon writing. Nonetheless, Moon may be considered as an option for young students with JNCL. Though not surveyed formally, the Project identified several cases where students with JNCL who failed to learn braille succeeded in learning Moon.1
Finally, given that functional vision may be retained for an extensive period of time after diagnosis, affected children may have no immediate need to learn a tactile reading and writing system if this determination is based solely on their current visual ability.
In addition, as children’s vision declines, assistive devices such as magnifiers can support continued use of remaining functional vision. Nevertheless, once the diagnosis is made, it is recommended that children with JNCL begin learning braille and/or another tactile system in order to establish the best possible foundation for developing and maintaining literacy skills over time as vision loss and cognitive abilities decline.1,27
Musical Activities and Music Therapy for children with JNCL:
As symptoms of JNCL progress, affected individuals face increasing challenges in the production of language. Speech increases in speed with rapid stuttering, articulation is impaired, and words are mispronounced. Eventually, many young people’s verbal communication becomes incomprehensible. The Project survey included the first-ever systematic study of musical activities and music therapy for children and young persons with JNCL. Separately, the ongoing Music in Neurodegeneration (MIND) study is evaluating the use of therapeutic music activities to support communication and other skills in affected individuals; here we present findings from both activities, within selected themes.
a). Music and communication.
For the music portion of the Project survey, parents and professionals were asked about the role of music in their child’s life, their engagement with musical activities, and the role of music in facilitating social contact, communication, comfort, learning and understanding, and offering stimulation and relaxation. Altogether 129 respondents (n=65 parents, n=64 professionals) completed the music portion of the survey. As with other portions of the survey there was some overlap in ratings, as several affected individuals were rated both by parents and professionals in their respective surveys. Eighty-six percent of parents (n = 33/38) and 78% of professionals (n = 15/19) reported that music therapy had (or once had) a high impact, and around a third of children and young people (n = 36/102) with JNCL had access to music therapy. As the potential to take part in physical activity such as sport and dance declined, music, by contrast, gained in frequency. For young adults with JNCL (by the age of 22), just under 80% (n=29/37) of parents and professionals reported that music was the most important activity in the child’s life. Also, the practice of listening repeatedly to favourite songs was viewed by respondents as crucial to children and young people’s positive emotional state and wellbeing.
Consistent with a prior report5, parents completing the Project survey noted that familiar songs helped their affected child to access his or her memories, and that music could aid communication when words alone no longer functioned. For example, one young girl was noted by a professional to speak more clearly when singing what she wanted to say, and for another child, her ‘lyrics came out clearly, even though her speech was so little, stuttering and slow’.
The ongoing MIND study is trialling music and speech activities codified in Neurologic Music Therapy with ‘micro-songs’.28,29 In micro-songs, short bursts of functional language are combined with simple melodies and songs to help children maintain verbal communication. The project has been facilitating work around encouragement of language in song, particularly introducing familiar topics such as days of the week and everyday activities, as well as more abstract themes such as feelings. Individuals are also being encouraged to sing warm up vocal activities each day in an attempt to encourage lasting articulation and pacing of speech. The next step is to seek to embed these songs and exercises with carers and parents beyond the music sessions.
b). Music and movement.
Parents and staff completing the Project survey reported that physical activity could be uniquely facilitated by the use of music. For example, one parent noted that, ‘walking … succeeds when she is listening to her favourite music and singing along’ and it was noted that music helped another child to be more coordinated and aware of his body. Although formal research into the capacity of music to function in this way for young people with JNCL has yet to be undertaken, the specialist techniques that have evolved as part of the emerging discipline of Neurologic Music Therapy might be of benefit.29 For example, the MIND project is exploring the benefits of rhythmic auditory stimulation (RAS) for individuals with JNCL, applying the technique of entraining a patient to a musical beat, and matching and facilitating their movements accordingly.
c). Participation and Inclusive Technology.
Producing music and sound with conventional instruments is a task that requires co-ordination, strength, dexterity, and control, and encouragingly, around half of the children and young people who were rated by parents or professionals in the Project survey were able to play an average of 2 instruments (n = 44/87). However, as the disease progresses and individuals’ physical capabilities deteriorate, the challenge is to find other ways to help children remain engaged and able to actively participate in producing music. The MIND project is exploring the use of Musical Instrument Digital Interface (MIDI) -based technology and Apps that allow individuals to operate switches and beams with very small movements to control computer generated music and sounds. This might enable individuals with JNCL to continue participating in shared music activities at home or with peers at school.
d). Music and memory.
In the Project survey, parents indicated that music fulfilled a special function in helping to revive memories for their children with dementia. For example, one parent noted that listening to music helped their daughter to remember special events:
‘…If she went to that particular concert and what the group were wearing or doing during a particular song. She will also remember what we did before the concert or any funny things that happened. This is really important for us as parents, as it helps not only with her communication but also her long-term memory.’
In the ongoing MIND project, music memory books are being evaluated to help maintain memories. A memory book may include sound bites, physical objects, materials, and braille that represent songs, favourite musicians, holidays, outings, or special occasions. These music memory books are being introduced as a classroom or home activity; as one parent put it, this allows music to serve as a ‘bridge’ to a past reality in the final stages of the disease.
For individuals with severe visual impairment, sounds of the environment become vital in making sense of everyday life. Although most children and young people listen to music in many situations, the lack of vision may make music even more important for individuals with JNCL. The Project survey demonstrated the importance that parents and professionals attribute to music activities for children and young people with this disease. By systematically introducing a music education framework for individuals with JNCL, it is hoped that the MIND project will identify strategies by which music can support functional improvements in speech articulation and fluency, awareness, comprehension and memory.
3.3. Educational Development Observation (EDO) Tool:
In addition to the Project survey, a major aim of the JNCL and Education Project was to develop a tool that could be used to assess the educational, social, and community support needs and strengths of children and young persons with JNCL, and to guide implementation of relevant services and interventions. The Educational Development Observation (EDO) tool is the product of that work. The EDO working group consisted of three Project members with a professional background in education of students with disabilities, including vision loss (BC, BE, AGT) and one paediatric neuropsychologist (HRA). All four had expertise in JNCL. Through a series of meetings (videoconference & phone calls) over the course of a year, the group developed EDO content and structure. Eleven core areas were identified that each address particular aspects of an affected child’s educational life, and each served as the basis of a ‘chapter’ in the EDO: Vision, Communication, Literacy, Social Life, Gross Motor function, Fine Motor function, Physical Activity, Behaviour and Mood, Attention and Memory, Independence and Autonomy, Interests and Equipment. An introductory section was added to gather demographic information (name, age, sex, family and school details, etc.). Within each of the 11 chapters, the authors identified key concerns based on the known symptoms of JNCL, which served as the basis for one or more items that can be ranked based on the child’s current optimal level of function on a ‘good day’, i.e., the context or setting where they are able to perform at their highest level. Box 1 provides a snapshot of one such item from the Communication Chapter.
Box 1. Sample Item from EDO Communication Chapter.
C. Communication
C.1. Speech intelligibility (mark one alternative):
Speech is understood by all, special attention from others is not required
Someone who knows the person well may not need to ask for repetition / clarification but someone who does not know the person well, may sometimes have to ask for clarification on a few words
Speech is unclear and not usually understandable to unfamiliar listeners out of context
Someone who knows the person well will understand simple, single words only (e.g., yes, no, etc.)
The person’s speech cannot be understood by anyone
After completing each respective chapter, the consequences of the child’s current function upon education and other non-medical service provision are considered, in order to guide selection and implementation of supports. In the final EDO chapter, ‘Interests and Equipment’, special attention is given to maintaining the child’s engagement in their areas of interest despite disease progression, with the use of any special equipment, assistive technology and an increasing need for sufficient individual support.
The EDO was designed to be completed by a multidisciplinary team consisting of parents/caregivers and the professionals who work with or know the affected person well in the school and community, under the guidance of an educational consultant with expertise in JNCL and training/experience in the use of the EDO. If possible, the EDO can be initially completed soon after diagnosis to establish and respond to the child’s baseline strengths and areas of needs in the classroom setting, but then be reviewed periodically as needed in response to the changing educational impact of JNCL symptom progression.
Finally, the EDO is a newly developed tool that is now undergoing pilot implementation in Norway and the United Kingdom (available in four languages: Norwegian, English, Finnish, German). The EDO authors are now in the process of engaging the first users to obtain feedback on the EDO’s utility and to inform future modifications and improvements. A future goal is to develop a web-based version of the tool and to conduct a systematic evaluation of its use. Further details of the EDO are provided within the final report for the Project and in the textbook1,17. In addition, sample copies are available upon request to the corresponding author (HRA) and can be used in collaboration with or after introduction from one of the EDO developers (BC, BE, AGT) or others who know the tool well.
3.4. Transition to Adulthood and Adult Living
Another component of the JNCL and Education Project was establishment of a framework to support young adults with JNCL, whose life path will differ from those of their typically developing peers. Typical development proceeds from interdependence, doing things together, to independence, doing things by oneself.30 From the perspective of participation in everyday life, independence means achieving personal goals without support, while interdependence means achieving personal goals with support. Additionally, there may be various degrees of independence and interdependence in different domains at any particular stage of development.1
As the individual with JNCL disease approaches adult years, he or she may experience a transition from independence back to interdependence due to disease progression, and in opposition to typical development. A model of interdependence for individuals with JNCL is one in which the supporting person (teacher, parent, more capable peer) actively enables the affected individual to be the driver of their own participation in activities, making their own choices, etc. Classically, this is achieved via ‘scaffolding’ which comprises the activities or involvement of an instructor and any supportive aids and technology to enable an individual to complete a desired activity and to facilitate their optimal participation.31 In the typically developing child, ‘scaffolding’ is removed over time as the child develops competence and takes on greater independence. By contrast for young adults with JNCL, an increase in scaffolding is required over time in order to sustain participation in the same activities and tasks.
Persons with severe disabilities such as young adults with JNCL are in most cases unable to meet the needs and challenges of the society as adults. These individuals need a person-centred approach in which the system is adapted to meet individual needs.32,33 Person-centred plans and interventions should be holistic, proactive and realistic in form and will require close collaboration among all relevant parties (i.e., affected individual, family and carers, and professionals from the various agencies serving the affected individual). The special challenge in supporting individuals with JNCL is to establish a system that is responsive to the individual’s changing needs caused by declines and losses. Important themes for adult living include supporting autonomy, interactive participation, interdependence and life flow.1 Autonomy is about self-government and self-determination but not necessarily self-reliance; maintenance of autonomy is a critical goal for persons with special needs and in particular those with dementia such as individuals with CNL3 disease.1,34,35 Interactive participation supported through interdependence in various kinds of desirable activities is critical for inclusion, quality of life and life flow (see below). In addition, participation in real-life activities, the most extensive arena for learning and development for all humans, facilitates implicit and incidental learning and maintenance of skills, and should thus be considered a core element when planning and implementing adult living for individuals with CLN3 disease.1
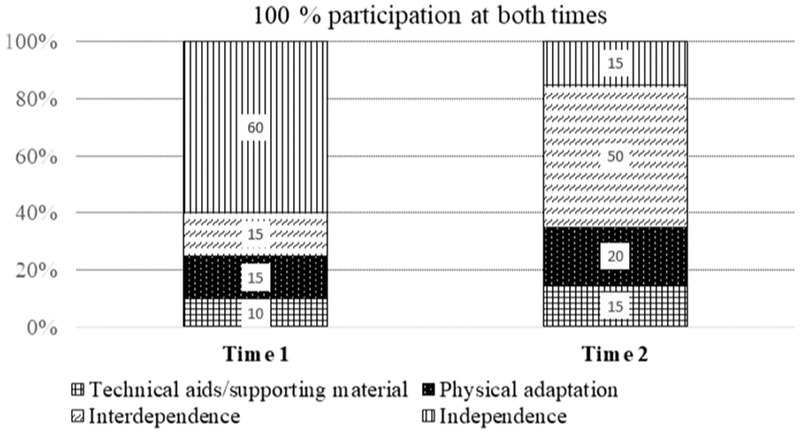
As described above, individuals with JNCL will experience a shift over time from independent to interdependent participation in activities. For the young adult with JNCL, the availability of individual support or interdependence will eventually mean the difference between participation and non-participation. Figure 5 presents the hypothetical example of a person with JNCL at two different ages.
Figure 5.
The Interdependence Model of participation for an individual with JNCL at two different ages (Time 1: 13 years old; Time 2: 20 years old).
At these two ages, the affected individual’s participation in an activity involves varying degrees of independent performance, physical adaptations of the environment, technical aids, and interdependence through the co-participation of other persons (e.g., parents, teachers). The critical point is that the affected individual experiences full participation at both times despite the declines.
Success factors for adult living for individuals with the JNCL disease include preparation for a vocational work setting within the affected person’s capabilities, and the establishment of a daily program based on participation in desired and specified activities that are supported by those who knows the affected person well. Finally, maintaining life flow means that life should have a certain degree of continuity. The concept of life flow acknowledges the person’s history and experiences, as well as skills, interests and social life. This principle is of special importance for planning of transitions, and in particular to adult life for individuals with JNCL.1
Conclusions
Individuals with JNCL experience many progressive symptoms that can impact learning and development, including vision loss, dementia, and motor and speech declines. Collectively, these symptoms have implications for educational interventions. The JNCL and Education Project survey highlighted the educational impacts on persons with JNCL, but the authors acknowledge several limitations of the survey methods and results. For parents whose children were deceased, or who were no longer in school, survey responses were based upon retrospective recall that may not have fully reflected their experience at the time when their child was still engaged in the school setting. As noted above, the survey was disseminated via different methods across the participating sites (countries). Among sites that engaged participants through parent support organisations, more respondents indicated a need for behavioural / mental health support, compared to sites that recruited broadly among all affected individuals in the respective country. We speculate that recruitment only via family organisations may yield a population that has greater needs for support. We did not explore whether differences in culture or educational systems may have been associated with behavioural health needs across the across the participating country sites. Finally, we note that the survey length and format may have contributed to some missing data. The survey was available on paper and an Internet-based form. For the latter, the online version could only be answered at one time; participants could not save a partially completed survey and resume work at another time. Some surveys were left incomplete and this may have been because participants were unable to finish the entire question set in one session. Also as noted earlier, some professionals who were invited to participate refused due to lack of remuneration for their time, resulting in less information overall from the perspective of school personnel.
A larger limitation of the JNCL and Education Project overall was its exclusive focus on juvenile-phenotype NCL, most commonly caused by CLN3 disease. It is hoped that the approach taken in this Project can be useful to considering educational and social support needs of individuals with other NCL diagnoses. Lacking from the current Project was a focus on early childhood years, which for children with JNCL is typically a time before diagnosis and before symptom onset. However, for earlier-onset and more rapidly progressing NCLs, including the classic CLN1 and other NCL diseases, it would be essential to investigate educational impacts and support needs prior to the start of formal schooling, e.g., addressing delay or failure to attain motor and language developmental milestones.36–38
Despite these limitations, the JNCL and Education Project survey identified a number of themes common to respondents from across multiple countries. Problems in school are noticed at or even before the time of diagnosis, and students need increasing support over their school years. Yet, school personnel may not be adequately equipped to anticipate and respond to student’s needs, due to a lack of knowledge about the disease and its progression, and in how to meet the challenges caused by the disease. It was felt by many parents that their child did not receive requisite training for establishing new and alternative skills in communication and literacy like AAC and braille. In addition, some parents communicated that such services were initiated too late, after childhood dementia had progressed too far. The Project as a whole has resulted in two outcomes that may help to address such concerns – the aforementioned textbook1, and the Educational Development Observation (EDO) tool to provide formative and continuing assessment of the educational and social needs of an individual with JNCL. Finally, the Project has provided a theoretical and practical framework for supporting young adults with JNCL as they age out of the school system and transition to other programmes and potentially other care settings within their communities.
Although educational interventions are not expected to modify disease progression, they can play a critical role in ameliorating the daily consequences of the disease. In particular, there should be an ongoing focus on implementing proactive measures to allow persons with JNCL to create meaning in their lives and to participate in and experience each day to the fullest extent possible. Proactive educational measures should also maintain a life-long perspective to support the affected individual over time, adapting to their situation from early childhood to adult living. Additionally, interventions should be person-centred rather than based upon standardized or systems-based methods, due to the fact that children and young persons with JNCL can show wide variations in their development and in the timing and rate of disease progression.
Working with individuals with JNCL is a challenging but also rewarding experience. Educational professionals have expressed a desire for additional support and information regarding the disease and its educational impacts. In particular, there has been little focus to date on the impacts of dementia on education – more research is needed in this area and more broadly to establish best practices for intervention. Many of the developmental and educational consequences of JNCL may be relevant for the other NCL disorders and more broadly for the many children impacted by paediatric neurodegenerative conditions. It is believed that further educational knowledge regarding JNCL may be valuable for these groups as well.
Highlights.
Children with juvenile-phenotype Batten disease (JNCL) experience paediatric-onset dementia, which results in a plateau in, and eventual loss of cognitive skills over time.
The educational model for children with JNCL should anticipate the progressive cognitive decline, through a model of proactive and hastened instruction.
Children with JNCL should learn skills, whilst still able to, that will enable them to maintain independence for as long as possible (e.g., alternative/augmentative communication; tactile learning systems, etc.).
Most learning takes places implicitly and incidentally through daily participation in real life activities, i.e. not based on predefined goals or curricula. Ensuring participation in real life activities is of special importance in adult life for individuals with JNCL.
Maintaining continuity of social life and participation in activities contributes to the ‘life flow’ of individuals with JNCL, and should be in particular considered during times of transitions to interdependence and adult living. Interests and activities can be sustained through scaffolding by collaboration/interaction with supporters, including physical adaptations to the environment, technical aids, and through activities involving music.
Funding:
Portions of this work were funded by:
Baily Thomas Charitable Fund (TRUST/VC/AC/SG/4015–6850) Batten Disease Support and Research Association, Columbus, OH, USA Biomarin Pharmaceutical Inc.
Erasmus+ (2014–1-NO01-KA200–000388)
National Institutes of Health (K23 NS058756; R01NS060022)
Statped, Norway
The Luke and Rachel Batten Foundation, Cypress, TX, USA
The Norwegian NCL Family Association (NSVF)
University of Rochester – Child Neurology Endowment Fund
Abbreviations:
- AAC:
Augmentative and alternative communication
- EDO
Educational Development Observation
- JNCL
Juvenile neuronal ceroid lipofuscinosis
- MIDI
Musical Instrument Digital Interface
- MIND
Music in Neurodegeneration
- RNIB
Royal National Institute of Blind People
- WISC-IV
Wechsler Intelligence Scale for Children – Fourth edition
- Voc-SS
WISC-IV Vocabulary scaled score
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Tetzchner S, Elmerskog B, Tøssebro A, Rokne S. Juvenile Neuronal Ceroid Lipofuscinosis, Childhood Dementia and Education. Melhus, Norway: Snøfugl forlag; 2019. [Google Scholar]
- 2.von Tetzchner S, Fosse P, Elmerskog B. Juvenile neuronal ceroid lipofuscinosis and education. Biochimica et biophysica acta. 2013;1832(11):1894–1905. [DOI] [PubMed] [Google Scholar]
- 3.Santavuori P, Linnankivi T, Jaeken J, Vanhanen SL, Telakivi T, Heiskala H. Psychological symptoms and sleep disturbances in neuronal ceroid-lipofuscinoses (NCL). Journal of inherited metabolic disease. 1993;16(2):245–248. [DOI] [PubMed] [Google Scholar]
- 4.Adams H, de Blieck E, JW M, et al. Standardized assessment of behavior and adaptive living skills in juvenile neuronal ceroid lipofuscinosis. Developmental medicine and child neurology. 2006;48(4):259–264. [DOI] [PubMed] [Google Scholar]
- 5.Bills W, Johnston L, Wilhelm R, Graham L. Teach and be taught: A guide to teaching students with Batten disease. Reynoldsburg, OH: Batten Disease Support and Research Association; 1998. [Google Scholar]
- 6.Gayton R The education and care problems of visually handicapped children suffering from juvenile neuronal ceroid lipofuscinosis, University of Birmingham; 1982. [Google Scholar]
- 7.Johnson B, Jochum J. Batten’s disease: Determining educational interventions. Interv Sch Clin. 1996;31(5):303–307. [Google Scholar]
- 8.van Delden G Education for children with Batten disease. ICEVI Europe Conference Accessed at www.icevi-europe.org/dublin2009/ICEVI2009_Paper_14.doc 04Mar2019; July 5–10, 2009; Dublin, Ireland. [Google Scholar]
- 9.Gayton R Juvenile Battens disease. Br J Vis Impair. 1987;5(2):55–57. [Google Scholar]
- 10.World Health Organization; International Classification of Diseases for Morbidity and Mortality Statistics: 11th Revision (ICD-11). Geneva, Switzerland: World Health Organization; 2018. [Google Scholar]
- 11.Shapiro E, Klein K. Dementia in childhood: Issues in neuropsychological assessment with application to the natural history and treatment of neurodgenerative storage diseases In: MG Tramontana SH, ed. Advances in child neuropsychology. Vol 2 New York, NY: Springer; 1994:119–171. [Google Scholar]
- 12.Adams HR, Kwon J, Marshall FJ, de Blieck EA, Pearce DA, Mink JW. Neuropsychological symptoms of juvenile-onset batten disease: experiences from 2 studies. Journal of child neurology. 2007;22(5):621–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adams HR, Mink JW. Neurobehavioral features and natural history of juvenile neuronal ceroid lipofuscinosis (Batten disease). Journal of child neurology. 2013;28(9):1128–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuper WFE, van Alfen C, Rigterink RH, Fuchs SA, van Genderen MM, van Hasselt PM. Timing of cognitive decline in CLN3 disease. Journal of inherited metabolic disease. 2018;41(2):257–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lamminranta S, Aberg LE, Autti T, et al. Neuropsychological test battery in the follow-up of patients with juvenile neuronal ceroid lipofuscinosis. J Intellect Disabil Res. 2001;45(Pt 1):8–17. [DOI] [PubMed] [Google Scholar]
- 16.Schoenberg M, Scott J. Cognitive decline in childhood or young adulthood In: Schoenberg M, Scott J, eds. The little black book of neuropsychology: A syndrome based approach. New York, NY: Springer; 2011:839–861. [Google Scholar]
- 17.Erasmus+. Juvenile Neuronal Ceroid Lipofuscinosis and Education. Accessed at: http://ec.europa.eu/programmes/erasmus-plus/projects/eplus-projectdetails/#project/2014-1-NO01-KA200-000388 04Mar2019. [DOI] [PubMed] [Google Scholar]
- 18.Clarke M, Wilkinson R. The collaborative construction of non-serious episodes of interaction by non-speaking children with cerebral palsy and their peers. Clinical linguistics & phonetics. 2009;23(8):583–597. [DOI] [PubMed] [Google Scholar]
- 19.Hormeyer I, Renner G. Confirming and denying in co-construction processes: a case study of an adult with cerebral palsy and two familiar partners. Augmentative and alternative communication (Baltimore, Md. : 1985). 2013;29(3):259–271. [DOI] [PubMed] [Google Scholar]
- 20.Solomon-Rice P, Soto G. Co-construction as a facilitative factor in supporting the personal narratives of children who use agmentative and alternative communication. Commun Disord Q. 2011;32:70–82. [Google Scholar]
- 21.Budiyanto K, Sheehy H, Khofidotur R. Developing Singalong Indonesia: Issues of happiness and pedagogy, training and stigmatization. International Journal of Inclusive Education. 2018;22:543–559. [Google Scholar]
- 22.Glacken M, Healy D, Gilrane U, et al. Key word signing: Parents′ experiences of an unaided form of augmentative and alternative communication (Lámh). Journal of intellectual disabilities : JOID. 2018:1744629518790825. [DOI] [PubMed] [Google Scholar]
- 23.Grove N, Woll B. Assessing language skills in adult key word signers with intellectual disabilities: Insights from sign linguistics. Research in developmental disabilities. 2017;62:174–183. [DOI] [PubMed] [Google Scholar]
- 24.Cryer H, Gunn D, Home S, Wilkins S. Identifying areas for research into an alternative tactile reading code. Birmingham, UK: RNIB Centre for Accessible Information;2008. [Google Scholar]
- 25.Steer M Moon code: a valuable supplement to your communications arsenal. Deaf-Blind Perspectives. 2000;7(3):8–10. [Google Scholar]
- 26.Cryer H, Home S, Wilkins S. User requirements for Moon: An informal investigation with experts. Birmingham, UK: RNIB Centre for Accesible Information;2011. [Google Scholar]
- 27.McCall S Accessing the curriculum In: Arter C, Mason H, McCall S, McLinden M, Stone J, eds. Children with visual impairments in mainstream settings. London, UK: David Fulton; 1999:29–40. [Google Scholar]
- 28.Ockelford A Tuning in Music Book: Sixty-four Songs for Children with Complex Needs and Visual Impairment to Promote Language, Social Interaction and Wider Development. London, UK: Jessica Kingsley Publishers; 2018. [Google Scholar]
- 29.Thaut M, Hoemberg V, eds. Handbook of neurologic music therapy. Oxford, UK: Oxford University Press; 2014. [Google Scholar]
- 30.Greenfield P. Independence and interdependence as developmental scripts In: Greenfield P, Cocking R, eds. Cross-cultural roots of minority child development. Hillsdale, NJ: Lawrence Erlbaum; 1994:1–40. [Google Scholar]
- 31.Wood D, Bruner JS, Ross G. The role of tutoring in problem solving. Journal of child psychology and psychiatry, and allied disciplines. 1976;17(2):89–100. [DOI] [PubMed] [Google Scholar]
- 32.Meadan H, Shelden D, Appel K, DeGrazia R. Developing a long-term vision: A road map for students’ futures. Teach Except Child. 2010;43:8–14. [Google Scholar]
- 33.O’Brien C, O’Brien J. The origins of person-centered planning: A community of practice perspective. Lithonia, GA: Responsive Systems Associates; 2000. [Google Scholar]
- 34.Entwistle VA, Carter SM, Cribb A, McCaffery K. Supporting patient autonomy: the importance of clinician-patient relationships. Journal of general internal medicine. 2010;25(7):741–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Agich G. Dependence and autonomy in old age: An ethical framework for long-term care. Cambridge, UK: Cambridge University Press; 2003. [Google Scholar]
- 36.Fietz M, AlSayed M, Burke D, et al. Diagnosis of neuronal ceroid lipofuscinosis type 2 (CLN2 disease): Expert recommendations for early detection and laboratory diagnosis. Molecular genetics and metabolism. 2016;119(1–2):160–167. [DOI] [PubMed] [Google Scholar]
- 37.Williams RE, Adams HR, Blohm M, et al. Management Strategies for CLN2 Disease. Pediatric neurology. 2017;69:102–112. [DOI] [PubMed] [Google Scholar]
- 38.Perez Poyato MS, Mila Recansens M, Ferrer Abizanda I, et al. Infantile neuronal ceroid lipofuscinosis: follow-up on a Spanish series. Gene. 2012;499(2):297–302. [DOI] [PubMed] [Google Scholar]