Abstract
Perioperative shared decision-making can be improved through the development of novel patient-centered outcome measures made possible by digital phenotyping—“the moment-by moment quantification of individual-level human phenotype in situ using data from personal digital devices, in particular smartphones.” This Short Report presents data from a patient with breast cancer that illustrates the opportunities of digital phenotyping to better inform patient quality of life while also discussing the challenges to its adoption. With time, effort, and physician engagement, digital phenotyping can help surgeons better understand the patient experience in the postoperative period and in turn, help them provide care that maximizes patient quality of life.
Keywords: Shared decision-making, breast cancer, quality of life, digital health, smartphones
Patients have questions when surgeons offer them different treatments. We as surgeons have ccumulated data that can inform metrics like 30-day mortality and complication rates, from which we can make fairly accurate statements about the safety and short-term outcomes of procedures. But then, patients want to know more: “how will this procedure impact my quality of life (QoL)?”
It can be distressing for surgeons to navigate through conversations about the physical, emotional, cognitive, and social impact of surgery. A lack of training in having difficult discussions contributes to this, but perhaps even more important is the lack of reliable and nuanced data on the multifaceted components of postoperative QoL. Surgeons lack measure that help them understand when patients can “get back” to their lives again and thus we are at a disadvantage in helping our patients make treatment decisions. However, with the advent of martphone technology, there is an opportunity to develop new metrics for QoL. The availability of and insight provided by these metrics may allow surgeons to rethink the definition of a successful operation.
By 2020, it is anticipated that 70% of the world population (6.1 billion people) will own a smartphone capable of collecting vast amounts of data1, which if analyzed properly could transform our understanding of patient QoL and lead to interventions to improve it. Smartphone sensor and usage data can be processed with appropriate biostatistical techniques to understand behavioral patterns, social interactions, physical mobility, gross motor activity and cognitive function, which may inform QoL.
For example, GPS data can assess how patients divide their time between distinct locations, such as home and work. Similarly, accelerometer and gyroscope data can be used to estimate patient’s physical activity level. Phone call and text message logs can convey information about the size and reciprocity of a person’s social networks, potentially describing social support during recovery. When these data are combined with patient-reported data, an even more nuanced understanding of recovery outside of clinical settings can be developed.
The combination of smartphone sensor and usage data, surveys, audio samples, and simple on-screen cognitive tests gives rise to digital phenotyping, the “moment-by-moment quantification of individual-level human phenotype in situ using data from personal digital devices, in particular smartphones.2” Through digital phenotyping, trajectories of physical, social, and emotional functioning after surgery can be described and used in clinical practice to enhance shared decision-making. Our team at Ariadne Labs and the Harvard T.H. Chan School of Public Health is currently performing prospective digital phenotyping research in surgical patients. Our early findings suggest that this is not a pipe dream.
Consider the difficult decision that many women with breast cancer face: choosing between mastectomy and breast-conserving therapy, which are known to have equivalent survival outcomes, but suspected to have notable differences in QoL. Digital phenotyping may be able to inform this decision. Figure 1 shows the digital phenotype for a female patient throughout her treatment of a clinically suspicious breast mass. The bottom panel shows the dates of clinical events during the days of treatment: excisional breast biopsy (Day 0), pathology results available revealing cancer (Day 7), consultation with surgical oncologist (Day 28), bilateral mastectomy (Day 42) and postoperative follow up (Day 56). Throughout these events, three of the many data sources contributing to the patient’s digital phenotype are shown: self-reported emotional QoL, self-reported pain, and daily physical activity as quantified by passively103 collected smartphone accelerometer data.
Figure 1.
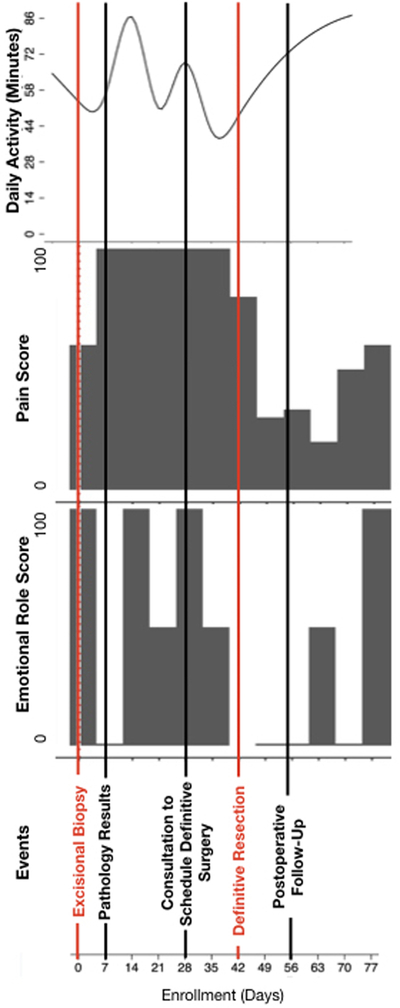
Postoperative experience for a single patient undergoing excisional breast biopsy followed by bilateral mastectomy for breast cancer. The top panel shows changes in the patient’s daily activity in minutes during multiple clinical events as measured by smartphone accelerometer data. Self-reported pain and emotional role quality of life scores are graphed below (higher scores indicate more favorable health states).
These data streams, individually and in combination, help define recovery by providing a measure of the impact of each clinical event in ways that are centered on the patient. As expected, the changes in self-reported physical pain occur both temporally (e.g., at the time of surgery) and in magnitude (e.g., bilateral mastectomy has greater impact than excisional breast biopsy). The changes seen in self-reported emotional QoL appear more sensitive. Specifically, there are greater magnitudes of change compared to self-reported physical pain around the non-operative events, such as the day the pathology results, which revealed cancer, were made available. Interestingly, daily physical activity as measured by smartphone accelerometers, like self-reported physical pain, has expected changes around the time of the operations. However, the day-to-day fluctuations mirror changes in self-reported emotional QoL during the non operative events. Each and all of these data streams could prove valuable to clinicians and patients to improve preoperative shared decision-making by providing metrics that better describe the journey through surgical recovery.
Although digital phenotyping has great potential, there are several significant challenges for its implementation. There are conceptual challenges: for example, of the many smartphone data streams, which ones will best capture QoL in the perioperative period and given the subjectivity of the patient experience, will distinct data types have different value to individual patients? There are technical challenges: how do we manage the vast volumes of data collected? There are regulatory challenges: who will control and have access to these data (e.g., patients, physicians, hospital systems, insurance companies, technology firms)? There are clinical challenges: how do we make these data actionable for physicians and patients? There are political challenges: how do you address privacy concerns and build trust among patients? here are collaborative challenges: how does the research community work with commercial industries that exist in this space? With so many considerations, there are many opportunitie for surgeons to lead this work in the right direction.
Traditional outcome measures will continue to be vitally important, but it is also time for surgeons to expand the ways we measure the impact of surgery on aspects of patients’ lives that matter most to them. With time, effort, and physician engagement, digital phenotyping will help us understand how patients define a successful operation and in turn will better inform the critical decisions around the time of surgery to ensure that patients’ choices maximize outcomes in the domains that they value most highly.
Acknowledgments
Conflicts of Interest and Source of Funding: NP is supported by NIH T32 DK007754-18 grant (Research Training in Alimentary Tract Surgery); NP, IS, and ABH are supported by an Ariadne Labs Spark Grant funded by the Paul G. Allen Family foundation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ericsson Mobility Report: 70 percent of world’s population using smartphones by 2020 https://www.ericsson.com/en/press-releases/2015/6/ericsson-mobility-report-70-percent-of-worlds-population-using-smartphones-by-2020 Accessed February 15, 2019.
- 2.Torous J, Kiang MV, Lorme J, Onnela J-P. New Tools for New Research in Psychiatry: A Scalable and Customizable Platform to Empower Data Driven Smartphone Research. JMIR Ment Heal 2016;3(2):e16. doi: 10.2196/mental.5165. [DOI] [PMC free article] [PubMed] [Google Scholar]


