Abstract
Despite the importance of empathic communication in cancer patient outcomes, the majority of opportunities to respond empathically to a patient’s concern within clinical consultations are “missed” (i.e., 70-90%), or not responded to by physicians. The present study examined the empathic opportunities and responses within clinical consultations of lung cancer patients and how these each are associated with patient-reported outcomes. Results indicate that lung cancer patients (n=56) most commonly presented empathic opportunities related to emotions, anxiety was significantly associated with empathic opportunity type (p=0.011), and physicians are most likely to respond with high empathy to statements around a patient making progress rather than bringing up a challenge or an emotion they felt (p = 0.031). The present study results highlight the need to train lung cancer physicians to respond with higher empathy to opportunities to respond to negative emotions, including mentions of challenges faced or emotions experienced, as these patients are at the highest risk of experiencing distress and the least likely to receive a high empathic response from physicians.
Keywords: empathic communication, lung cancer, stigma
Introduction
Physicians who treat patients with lung cancer face numerous patient-physician communication challenges including how to communicate effectively about prognosis, treatment, and the risks of persistent smoking in a nonjudgmental manner that empowers patients to quit smoking without exacerbating feelings of self-blame and guilt (Bayer & Stuber, 2006; Bell, Salmon, Bowers, Bell, & McCullough, 2010; Gritz, Sarna, Dresler, & Healton, 2007). Unique to patient-physician communication in the context of lung cancer is the commonly reported feeling of stigma (95%) lung cancer patients experience around the diagnosis being tied to a prior or current use of smoking or other tobacco use whether they are former, current, or never smokers (Hamann et al., 2013). As many as 48% of lung cancer patients have specifically reporting feeling stigmatized by medical care providers (Hamann et al., 2013). Lung cancer patients with a history of cigarette smoking experience blame and perceived stigma that may be triggered by health care providers’ routine probes about their smoking history (Chapple, Ziebland, & McPherson, 2004; Hamann et al., 2013; Morse, Edwardsen, & Gordon, 2008). Given the prevalence of these stigmatizing encounters with medical providers and the possibility for triggering stigma or other negative emotions within clinical encounters, lung cancer physicians often face the unique challenge of trying to create positive communication encounters with their patients in the context of real or perceived stigma of their patients.
Empathic physician communication may be critical to improving patient outcomes in the context of lung cancer because empathic communication has been associated with higher rates of patients’ satisfaction, treatment adherence, and enablement across a number of studies (Derksen, Bensing, & Lagro-Janssen, 2013; Kim, Kaplowitz, & Johnston, 2004) and lower levels of psychological distress (Lelorain, Brédart, Dolbeault, & Sultan, 2012). In the medical literature, empathic physician communication is defined as a physician’s recognition or elicitation and response to patients’ empathic opportunities in order to communicate understanding, alleviate distress, and provide support (Pehrson et al., 2016).
Clinical encounters with lung cancer patients provide many opportunities for physicians to respond empathically (Pollak et al., 2007). For instance, when patients express guilt or regret about the role of smoking in causing their lung cancer or about the stigma they experience when sharing their diagnosis with others, there is an opportunity for physicians to respond empathically to these concerns. Some examples of empathic responding may include a physician’s acknowledgment of patient emotions as well as an invitation for them to express their feelings in order to develop a shared understanding of patient emotion and experiences. Through the use of a variety of empathic communication skills, physicians may not only develop an understanding and sensitive appreciation of patient’s experiences or feelings, but also communicate that understanding back to the patient in a supportive way (Kurtz, Draper, & Silverman, 2016).
Prior research indicates that physicians working in oncology settings frequently (70-90%) “miss” empathic opportunities (Hsu et al., 2012), which occurs when an empathic opportunity is presented by a patient and not responded to by a physician. Missed empathic opportunities are even more frequent within the context of lung cancer care, with one study finding that 90% of empathic opportunities were missed during clinical encounters (Morse et al., 2008). Despite preliminary data indicating lung cancer patients are more likely to experience their physicians missing empathic opportunities, no study to date has examined rates and type of empathic communication within the context of lung cancer. As such, little is known about what type of empathic opportunities are presented within lung cancer patient-physician consultations or when and how physicians respond to them.
Additionally, it is unclear whether certain patient characteristics, such as demographic characteristics, stigma, or higher levels of distress, are associated with certain types of empathic opportunities or empathic responses in the context of lung cancer care. It is critical to understand the types of empathic opportunities and empathic responses within lung cancer contexts to determine how to improve lung cancer communication and patients’ corresponding outcomes by examining these encounters in real-world clinical settings. The goal of the present study was to provide a description of empathic discussions in the lung cancer setting, examining the frequencies and types of empathic opportunities and empathic responses using the Empathic Communication Coding System (ECCS) (Bylund & Makoul, 2005) and to examine associations between patient characteristics and type of patient empathic opportunities and physician empathic responses.
Methods
Analyses in the present study utilized data from 56 lung cancer patients and 11 treating lung cancer physicians. In the present analyses, audio recordings of actual clinical consultations between lung cancer patients and physicians (medical oncologists, thoracic surgeons, and radiation oncologists) were analyzed using the Empathic Communication Coding System (ECCS) (Bylund & Makoul, 2005). The ECCS was used to code the presence of empathic opportunities presented by patients and corresponding empathic responses by physicians. Additionally, patients completed a brief post-consultation questionnaire assessing their demographic and medical characteristics, lung cancer stigma (Janine K Cataldo, Slaughter, Jahan, Pongquan, & Hwang, 2011), and psychological distress (Zigmond & Snaith, 1983). Participants were recruited from an NCI-designated cancer center located in the northeast part of the United States. This study was approved by the participating institution’s Institutional Review Board.
Patient Recruitment and Study Procedures
Physicians and their patients were recruited as study participants. Physician eligibility criteria were (1) being a radiation oncologist, medical oncologist, or thoracic surgeon practicing within the thoracic disease management group at the participating institution and (2) currently treating lung cancer patients; and (3) willing and able to provide informed consent. Patient eligibility criteria included: (1) being a new patient (within 3 months) at the institution; (2) having lung cancer or a mass suspicious of lung cancer; (3) being a current or former smoker (smoked 100 packs or more in lifetime); (4) being fluent in English; (5) being able to provide informed consent; (6) being able and willing to complete all study procedures within three days of recorded clinical consultation; and (7) being be a patient of a consented physician participating in the study. Non-smokers were excluded from this study to focus on lung cancer patients most at risk of experiencing lung cancer stigma.
Physicians were informed at staff meetings about the purposes and procedures of the study. Interested physicians then met with research staff in one-on-one meetings to review study information in detail, review the consent form, answer any questions, and provide informed consent if interested and willing to participate. Participating physicians’ clinics were then monitored for potentially eligible patients. Once patients were identified as potentially eligible, they were approached in-person by a member of study staff during scheduled clinic appointments. Once eligibility was confirmed, patients were informed about the study and asked about their interest.
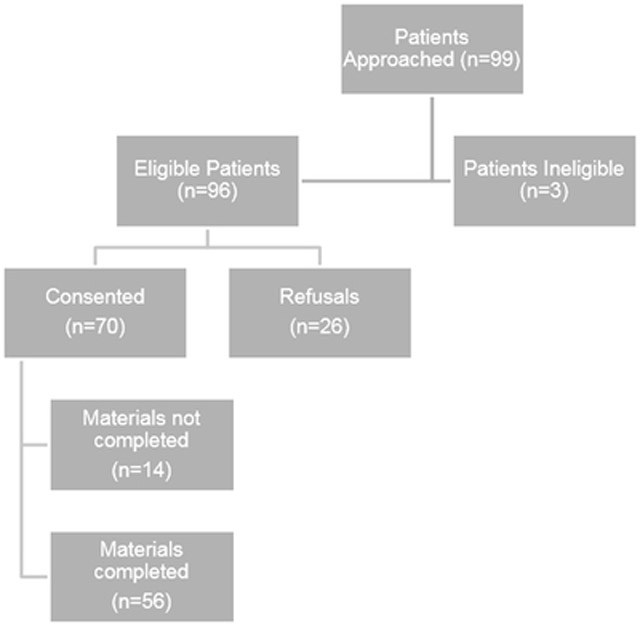
As indicated in Figure 1, a total of 70.7% of eligible patients who were approached consented to study procedures. Consented study participants were asked to have either their same day clinical consultation or their next upcoming appointment with the participating physician recorded. Additionally, patients were asked to complete the following assessments post-consultation (within three days): (1) a brief 15-minute survey battery and (2) 10 minute qualitative interview. The survey battery contained questionnaires to assess socio-demographics, medical characteristics, lung cancer stigma, and psychological distress. Participants completed the questionnaire in one of the following ways: (1) through a secure electronic (web-based) portal from their own computer, or (2) a paper-based version of the survey.
Figure 1.
Consort diagram of patient recruitment and enrollment.
Web-based study materials utilized REDCap (Research Electronic Data Capture),1 a data management software system. REDCap is a tool for the creation and collection of customized, secure data management systems including web-based data entry forms, reporting tools, and a full array of security features including user- and group-based privileges and an audit trail of data manipulation and export procedures. Data from participants who completed paper surveys were entered into REDCap by study staff.
Measures
Demographic and clinical information.
The majority of the demographic and clinical information was assessed via patient self-report (e.g., age, gender, marital status, race, education level, smoking status). Disease type and stage were assessed through self-report and confirmed via the electronic medical record (EMR), with preference given to EMR when information was inconsistent.
Smoking status.
Smoking status was evaluated with the following two questions: (1) “Have you smoked at least 100 cigarettes in your lifetime?” and (2) “Do you smoke cigarettes every day, some days, or not at all?” Those participants who reported smoking at least 100 cigarettes in their lifetime and that they were currently smoking (e.g., “Every day” or “Some days”) were categorized as “current” smokers; those who reported that they have smoked at least 100 cigarettes in their lifetime but were not currently smoking (e.g., “Not at all”) were categorized as “former” smokers.
Lung cancer stigma.
To measure lung cancer stigma, patients completed the Cataldo Lung Cancer Stigma Scale (CLCSS) (Janine K Cataldo et al., 2011), a 31-item validated instrument that assesses stigma and shame, social isolation, discrimination, and smoking related to lung cancer. Examples of items include: “I feel guilty because I have lung cancer” and “Some people have told me lung cancer is what I deserved for smoking” (1 = strongly disagree, 4 = strongly agree). Prior studies indicate the CLCSS is an internally reliable scale, with Cronbach’s α = .96 (Janine K Cataldo et al., 2011). This measure has been used across several studies assessing lung cancer stigma (Janine K Cataldo & Brodsky, 2013; J. K. Cataldo, Jahan, & Pongquan, 2012; Lee & Kim, 2011).
Psychological distress.
Psychological distress was measured by the 14-item Hospital Anxiety and Depression Scale (HADS) (Zigmond & Snaith, 1983), a self-report measure of distressed mood designed for use in medical populations. Each item on this scale is rated on a 4-point scale (0 to 3), and all items (anxiety and depressive symptoms) are summed to create a HADS total score as well as HADS anxiety and HADS depression subscale scores. HADS is widely used as a measure of psychological distress among medically ill patients and prior studies indicate the HADS is an internally reliable scale, with Cronbach’s α = 0.68 to 0.93 (Bjelland, Dahl, Haug, & Neckelmann, 2002).
Patients’ empathic opportunities and physician responses.
For analysis of the clinical consultation data, we used a modified version of the Empathic Communication Coding System (ECCS) (Bylund & Makoul, 2005). This interaction analysis system is designed to operationalize the phenomenon of empathic communication in physician-patient interactions by first identifying when patients create empathic opportunities of three types (progress, challenge, and emotion) and second categorizing physicians’ responses into hierarchical categories.
All audio-recorded clinical consultations were coded using the ECCS for the presence of empathic opportunities and physician responses to these empathic opportunities. Within the ECCS, the unit of analysis is a single empathic opportunity and corresponding response (or non-response from a physician) within the consultation. Thus, it is possible for multiple empathic opportunities to exist within a single consultation. The start point of all empathic opportunities were coded at the point at which a patient introduced the empathic opportunity and the end point was coded at the point at which a physician either responded or moved on to another topic. Allowances were made if the physician circled back to it later in the consultation to ensure that all physician responses were properly documented. Empathic opportunities and responses were coded as part of a single empathic opportunity encounter.
When an empathic opportunity was identified, it was further coded for which type of empathic opportunity it represented: (1) progress statement (something specific the patient does to improve his or her health such as cutting down on smoking, a physical ailment to improving, or a positive life event such as a child getting married), (2) challenge statement (any explicit statement that the patient makes about a negative effect of a physical or psychosocial problem or quality of life issue), or (3) emotion statement (any statement that includes an expressed and explicit emotion with words such as “happy” or “upset”). When an empathic opportunity was coded as being present, the physician’s response (or non-response) was coded according to level of empathic communication. The original coding system included seven categories (Bylund & Makoul, 2005). Recognizing the unique context of lung cancer communication, we added an additional category to capture any comment that was considered to be highly critical or judgmental.
With this modified coding system, physician responses were coded according to the following eight levels of empathic communication: (1) disconfirming; (2) denial; (3) perfunctory recognition; (4) implicit recognition; (5) acknowledgment; (6) pursuit; (7) validation/normalization; and (8) shared feeling or experience. Disconfirming refers to the physician making a critical, judgmental or harsh statement to the patient in response to the empathic opportunity. (“I can’t believe that you are still smoking”). Denial is characterized by the physician ignoring the patient’s empathic opportunity completely. This could be done by changing the subject (sometimes through interruption) or by not responding at all. Perfunctory recognition is characterized by a physician’s automatic, scripted-type response, often called back channeling cues. These are minimal responses that do not truly acknowledge that the patient has been heard. Examples are: “mmm-hmmm”, “ok”, “yeah,” etc. Implicit recognition responses do not explicitly recognize the central issue in the empathic opportunity, but focus instead on a peripheral aspect of the statement. These statements tend to be more content-based, or focused on the biomedical issue, while not dealing directly with the challenge, emotion or progress. This could include advice or questions (“The constant headaches are making it difficult for me to work” or “What kind of work do you do?”). Acknowledgment responses demonstrate explicitly that the physician heard what the patient said, but do not go any farther in terms of validating or pursuing this. Pursuit is characterized by the physician pursuing the topic with the patient by asking a question, asking the patient to clarify something about what he or she said, elaborating on a point the patient has raised, or trying to comfort the patient. Validation/ normalization responses convey to the patient that their emotion, challenge, progress, or experience with smoking history is valid (“I know it’s hard”). Finally, shared feeling or experience responses refer to when a physician tells of his or her own experience/feeling, using that to relate to the patient. Physician might share his/her struggles with other types of health behavior change.
Analytic Plan
Descriptive statistics were calculated for demographic and clinical variables. All coders were trained to use the ECCS by the developer of the original ECCS coding system and the first author/primary investigator. All coders (n=3) engaged in an initial set of coding n=5 consultations. Next, all coders met with the first and senior authors to discuss and reconcile differences and ensure consistency in coding across consultations and across coders. Once the coders had consistency and reliability in utilizing the ECCS, they then independently coded each consultation as pairs of coders. Each pair of coders met to discuss and reconcile their codes for each consultation. Any discrepancies were reconciled with the assistance of the senior author and original developer of the ECCS.
Using the ECCS, these trained pairs of independent coders first unitized the 56 audio-recorded clinical consultations into patient-created empathic opportunities and physician responses to these empathic opportunities. Each consultation was marked with time stamps for when empathic opportunities or responses were considered to be present. As noted, any disagreements between the pair of independent coders was reconciled by the senior author. Next, the type of empathic opportunity and level of physician response were coded.
Once the empathic opportunities and physician responses were coded using the ECCS coding system, descriptive statistics were calculated to indicate the number and type of empathic opportunities that fell into each of the three categories (progress, challenge, emotion) and the number and type of the eight physician responses (disconfirming, denial, perfunctory recognition, implicit recognition, acknowledgment, pursuit, validation/normalization, and shared feeling or experience). Additionally, we collapsed physician responses into two categories: low empathy (levels: disconfirming through implicit recognition) and high empathy (levels: acknowledgment through shared feeling or experience). This was done to power our analyses to examine between group differences in empathic response type by patient characteristics and patient empathic opportunity type.
Utilizing these newly collapsed physician response type categories, Pearson correlations (for continuous variables) and chi-square tests (for categorical variables) were conducted to examine if empathic opportunity and physician response types were each significantly associated with patient demographics, stigma, or distress. Finally, a chi-square test was conducted to examine if the proportion of physician responses (low empathy vs. high empathy) differed significantly across empathic opportunity types (progress, challenge, emotion).
Results
Demographic and Clinical Characteristics
Participants were 56 patients undergoing initial work-up and treatment for lung cancer, of which a small minority were later found to have a non-malignant lung mass (n=5). The mean age of participants was 67.95 years old (SD= 9.06). The majority of participants identified as White (76.8%), married (60.7%), and female (57.1%). Patients were fairly highly educated, with over half (60.7%) reporting having a college degree or higher. Patients were represented across all four disease stages: 25.0% Stage I, 1.8% Stage II, 14.3% Stage III, and 23.2% Stage IV. The remaining 35.7% were limited, extensive or other/unknown stage (see Table 1). Finally, the majority of participants were former smokers (83.9%), while 16.1% were current smokers. For more detailed demographic and clinical characteristics, see Table 1.
Table 1.
Demographic and clinical characteristics of the sample (N=56).
| Patient Characteristic | N | % |
|---|---|---|
| Age (in years) | M=67.95 | SD=9.06 |
| Gender | ||
| Female | 32 | 57.1% |
| Male | 24 | 42.9% |
| Marital status | ||
| Married/partnered | 34 | 60.7% |
| Race | ||
| White | 43 | 76.8% |
| Black | 7 | 12.5% |
| Other | 6 | 10.7% |
| Education | ||
| Less than college degree | 22 | 39.3% |
| College degree or higher | 34 | 60.7% |
| Type of Lung Cancer | ||
| Non-small cell lung cancer (NSCLC) | 30 | 53.6% |
| Small cell lung cancer (SCLC) | 13 | 23.2% |
| Suspicious mass | 13 | 23.2% |
| Pathological disease stage | ||
| Stage IA | 9 | 16.1% |
| Stage IB | 5 | 8.9% |
| Stage IIA | 1 | 1.8% |
| Stage IIIA | 5 | 8.9% |
| Stage IIIB | 3 | 5.4% |
| Stage IV | 13 | 23.2% |
| Limited stage | 7 | 12.5% |
| Extensive stage | 5 | 8.9% |
| Suspicious mass, later non-malignant | 5 | 8.9% |
| Other | 1 | 1.8% |
| Stage unknown | 2 | 3.6% |
| Smoking Status | ||
| Current smoker | 9 | 16.1% |
| Former smoker | 47 | 83.9% |
| Type of Lung Cancer Physician Seen | ||
| Medical oncologist | 21 | 37.5% |
| Thoracic oncology surgeon | 30 | 53.6% |
| Radiation oncologist | 5 | 8.9% |
Empathic Opportunities and Responses
Among the 56 recorded clinical consultations, 35 (62.5%) were coded as having at least one empathic opportunity for a total of n=67 empathic opportunities. The average number of empathic opportunities across all consultations (n=56) was M=1.21 and the average number across those consultations with at least one empathic opportunity present (n=35) was M=1.94.
The most commonly coded type of empathic opportunity was emotion statements (n=30, 44.7%), followed by challenge (n=20, 29.9%) and progress (n=17, 25.4%) statements. Of the emotion statements coded (n=30), only n=5 (16.7%) were positive emotions. The most commonly coded physician response types were implicit recognition (n=22, 33.0%) and validation/normalization (n=21, 31.0%), followed by acknowledgment (n=14, 21.0%), perfunctory recognition (n=5, 7.5%), and shared feeling or experience (n=3, 5.0%). There were no disconfirming or pursuit responses (n=0, 0.0%) and few (n=2, 3.0%) denied patients’ expressions of empathic opportunities. Examining the collapsed dichotomized variable of low empathy vs high empathy, physician responses highlighted a fairly even split between physicians giving a low empathy response (n=29, 43.3%) and a high empathy response (n=38, 56.7%). The frequency and level of physician response type by empathic opportunity is reported in Table 2, which highlights that implicit recognition was commonly a response to patients’ challenge statements (55.0%) whereas validation/normalization was most commonly a response to patients’ progress statements (47.1%).
Table 2.
Frequency and level of empathic response type by empathic opportunity (n=67 empathic opportunities).
| EO | Disconfirming | Denial | Perfunctory Recognition |
Implicit Recognition |
Acknowledgment | Pursuit | Validation/ Normalization |
Shared Feeling or Experience |
|---|---|---|---|---|---|---|---|---|
| 1. Progress (n=17) |
0.0% | 0.0% | 5.9% | 11.8% | 29.4% | 0.0% | 47.1% | 5.9% |
| 2. Challenge (n=20) |
0.0% | 0.0% | 5.0% | 55.0% | 10.0% | 0.0% | 30.0% | 0.0% |
| 3. Emotion (n=30) |
0.0% | 6.5% | 9.7% | 29.0% | 22.6% | 0.0% | 22.6% | 6.5% |
EO=Empathic opportunity
There were significant differences in physicians responding to each of the empathic opportunities (progress, challenge, and emotion statements) with a low or high empathy response [χ2 (df=2) = 6.40, p = 0.031]. Results indicate that progress statements were most commonly responded to with high empathy responses (82.4%) whereas challenge statements were most commonly responded to with low empathy responses (60.0%), and emotion statements were nearly evenly split between low empathy (46.7%) and high empathy (53.3%) responses (see Table 3).
Table 3.
Frequency and level of empathic response type by empathic opportunity (n=67 empathic opportunities).
| EO | Low empathy | High empathy |
|---|---|---|
| 1. Progress (n=17) |
17.6% | 82.4% |
| 2. Challenge (n=20) |
60.0% | 40.0% |
| 3. Emotion (n=30) |
46.7% | 53.3% |
EO=Empathic opportunity
Patient Characteristics’ Associations with Empathic Opportunities and Responses
There were no significant associations found between patient demographic characteristics (age, gender, race, stage, smoking status) and empathic opportunity type or empathic response type within clinical encounters. There were no significant associations found between patient-reported stigma and empathic opportunity type. Patient-reported anxiety (as measured by HADS anxiety) was significantly associated with empathic opportunity type [F(2) = 5.23, p = 0.011] such that those who presented empathic opportunities with emotion statements had significantly higher levels of anxiety (M=9.57) than those who presented progress (M=4.60) or challenge (M=4.91) statements (p < 0.001). Patient depression (HADS depression) and overall psychological distress (total HADS score) were not significantly associated with empathic opportunity type. Finally, there were no significant associations between patient characteristics (stigma and distress) and physician response type.
Discussion
The present study represents one of the first detailed investigations of empathic communication within the context of lung cancer care and highlights critical information about the number, type, and response to lung cancer patients’ empathic opportunities occurring within actual clinical encounters. This provides a more nuanced description than previous research in this setting. Specifically, the present study found that empathic opportunities are indeed common and that the most common type of empathic opportunities presented by lung cancer patients are emotion statements. Additionally, these findings build upon prior work (Morse et al., 2008), which found that the vast majority of empathic opportunities (90%) in lung cancer contexts are missed. In contrast, our current findings indicate physicians missed or responded with low empathic responses approximately half the time (46.7%). The discrepancies in these findings could be due to a number of factors. For instance, the present study examined communication between patients and lung cancer physicians working in a large cancer center whereas prior work (Morse et al., 2008) was conducted in the Veterans Affairs hospital. As such, the physicians in the present study may have more expertise in communicating specifically with lung cancer patients. Additionally, differences could be due to slight variations in how empathic opportunities were described in each study. For instance, Morse and colleague’s work focused specifically on empathic opportunities related to lung cancer care, diagnosis, treatment, and access to care whereas our study used a broader definition of empathic opportunity as defined by the ECCS coding system (Bylund & Makoul, 2005).
Another finding of the present study is that physicians were most likely to respond to progress statements with empathic statements compared to challenge and emotion statements. This finding is similar to prior work indicating that positively valenced empathic opportunities were more likely to receive higher empathic responses as well (Bylund & Makoul, 2005). This finding is concerning because patients who present challenge or emotion statements may be the most in need of empathic responses.
The present study also found that patients who presented emotion statements had the highest levels of anxiety, but empathic opportunity type had no association with depression or overall distress. However, these patients were not significantly more likely to be responded to with an empathic response. Given that prior work (Lelorain et al., 2012) has found that empathic communication has been shown to lower levels of psychological distress, this finding highlights a potential need for physicians who treat lung cancer patients to respond with greater empathic responses for patients who present emotion statements. Future research should examine the effects of empathic responses among physicians to patients’ emotion statements to determine if it lowers patients’ distress and perceived stigma.
Taken together, these findings illuminate what type of empathic opportunities are occurring in real world clinical settings between lung cancer patients and their physicians. Additionally, the present study findings highlight potential gaps in responding with empathic responses to patients who may be most in need of them – patients presenting challenge statements and those presenting emotion statements, who have statistically higher levels of distress and anxiety. Moreover, these findings highlight what type of empathic opportunities may be missed or responded to with low empathy responses. Furthermore, the present findings highlight potential gaps in responding to patients who present emotion statements, who are statistically more likely to be anxious and could benefit most from empathic communication (Lelorain et al., 2012).
Study Strengths and Limitations
This study had a number of strengths, including a rigorous and standardized analysis of actual clinical encounters between patients with lung cancer and their oncology care physicians, and details regarding the frequency and type of empathic opportunity types and physician responses. Moreover, these findings highlight which patient characteristics may be associated with varying physician response types, highlighting potential targeting of communication interventions. Despite these strengths, the present study does have limitations that should be considered when interpreting results. First, data and analysis in the present sample is limited to a single consultation at one institution. Thus, it is possible that physicians engage in empathic responses across many consultations not captured in the present study. Second, the consultations varied in terms of how long the patient had known the physician, leading to some variation and heterogeneity in communication. Efforts were made to recruit new patients and capture a first or early clinical consultation so as to control for quality of relationship with their treating physician. However, there may be varying quality of relationship already established that influences the number and type of empathic opportunities and responses. Third, because constructs were assessed post-consultation, it is possible that certain constructs (e.g., stigma) were influenced by the consultation itself and thus do not reflect baseline levels of these constructs. Fourth, the present study’s sample size was limited. Although it allowed for examination of actual clinical encounters, the generalizability of the results may be limited due to this sample size. Fifth, descriptive statistics and associations were examined between empathic opportunities, physician responses, and various patient characteristics, however, no causal inferences can be made as to how empathic opportunities or empathic responses predict or affect other patient-reported and medical outcomes. Finally, coded empathic responses were collapsed into high and low empathy categories due to a lack of adequate power to examine associations between patient characteristics and empathic opportunity type with each of the eight response types. Although this gives us insight into how patient characteristics and empathic opportunities may be associated with high and low levels of empathy, it lacks the nuance of understanding each of the eight response types. Future research should examine this in a large sample powered to detect such differences.
Clinical Implications
Use of a validated coding system (ECCS) (Bylund & Makoul, 2005) to examine empathic opportunities and empathic responses within the context of lung cancer care is novel and highlights both current clinical practice and important potential gaps in best communication practices experienced by the lung cancer patient population. Findings highlight the continued need to improve physician communication around responding effectively to empathic opportunities presented by patients, most notably to the patients sharing challenges and emotion-laded concerns during their routine clinic consultations. These findings support the need for the development and testing of communication skills interventions designed to improve empathic patient-physician communication ultimately improving patient care and improving patient outcomes.
Conclusions
By highlighting the type and frequency of empathic opportunities and responses, these data illuminate both current clinical practice in lung cancer patient populations as well as potentially fruitful areas for interventions to improve empathic communication between lung cancer patients and their physicians. The present study highlights the most frequently presented empathic opportunities (emotion statements) and physician responses (implicit recognition and validation/normalization). Additionally, the present study indicates that progress statements, in which patients express a positive progress, rather than challenge and emotion statements in which the patient expresses some form of challenge or struggle in most cases are most likely to receive empathic responses from their physicians. Furthermore, patients who presented emotion statements on average reported significantly higher levels of anxiety. Taken together, these findings indicate there may be a need to help train physicians on how to respond more empathically to patients who express facing a challenge or who express emotions, particularly negative emotions such as anxiety or fear. Future research could develop communication-based interventions designed to improve physicians’ communication with their patients, especially around discussion of challenges and emotions. This could be a critical next step to improving patient care among lung cancer patients.
Acknowledgments
Sources of funding: This work was supported by the following grants from the National Cancer Institute: R03CA154016 and K07CA207580.
Footnotes
Declaration of Interest Statement
The authors have no conflicts of interest to disclose.
References
- Bayer R, & Stuber J (2006). Tobacco control, stigma, and public health: rethinking the relations. American Journal of Public Health, 96(1), 47–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell K, Salmon A, Bowers M, Bell J, & McCullough L (2010). Smoking, stigma and tobacco ‘denormalization’: Further reflections on the use of stigma as a public health tool. A commentary on Social Science & Medicine's Stigma, Prejudice, Discrimination and Health Special Issue. Social science & medicine, 70(6), 795–799. [DOI] [PubMed] [Google Scholar]
- Bjelland I, Dahl AA, Haug TT, & Neckelmann D (2002). The validity of the Hospital Anxiety and Depression Scale: An updated literature review. Journal of psychosomatic research, 52(2), 69–77. [DOI] [PubMed] [Google Scholar]
- Bylund CL, & Makoul G (2005). Examining empathy in medical encounters: An observational study using the empathic communication coding system. Health communication, 18(2), 123–140. Retrieved from http://www.tandfonline.com/doi/pdf/10.1207/s15327027hc1802_2?needAccess=true. [DOI] [PubMed] [Google Scholar]
- Cataldo JK, & Brodsky JL (2013). Lung cancer stigma, anxiety, depression and symptom severity. Oncology, 85(1), 33–40. [DOI] [PubMed] [Google Scholar]
- Cataldo JK, Jahan TM, & Pongquan VL (2012). Lung cancer stigma, depression, and quality of life among ever and never smokers. Eur J Oncol Nurs, 16(3), 264–269. Retrieved from http://ac.els-cdn.com/S1462388911000974/1-s2.0-S1462388911000974-main.pdf?_tid=34ddd8ae-87e3-11e5-ba27-00000aab0f02&acdnat=1447184741_45bddaa259b38704e6e947dcfe04e6f0. doi: 10.1016/j.ejon.2011.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cataldo JK, Slaughter R, Jahan TM, Pongquan VL, & Hwang WJ (2011). Measuring stigma in people with lung cancer: Psychometric testing of the Cataldo Lung Cancer Stigma Scale. Oncol Nurs Forum, 38(1), E46–E54. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3182474/pdf/nihms316229.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapple A, Ziebland S, & McPherson A (2004). Stigma, shame, and blame experienced by patients with lung cancer: qualitative study. Bmj, 328(7454), 1470. doi: 10.1136/bmj.38111.639734.7C [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derksen F, Bensing J, & Lagro-Janssen A (2013). Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract, 63(606), e76–e84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gritz ER, Sarna L, Dresler C, & Healton CG (2007). Building a united front: aligning the agendas for tobacco control, lung cancer research, and policy. Cancer Epidemiol Biomarkers Prev, 16(5), 859–863. doi: 10.1158/1055-9965.epi-07-0342 [DOI] [PubMed] [Google Scholar]
- Hamann HA, Ostroff JS, Marks EG, Gerber DE, Schiller JH, & Lee SJC (2013). Stigma among patients with lung cancer: a patient reported measurement model. Psycho‐Oncology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu I, Saha S, Korthuis PT, Sharp V, Cohn J, Moore RD, & Beach MC (2012). Providing support to patients in emotional encounters: A new perspective on missed empathic opportunities. Patient education and counseling, 88(3), 436–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SS, Kaplowitz S, & Johnston MV (2004). The effects of physician empathy on patient satisfaction and compliance. Evaluation & the health professions, 27(3), 237–251. [DOI] [PubMed] [Google Scholar]
- Kurtz S, Draper J, & Silverman J (2016). Skills for communicating with patients: CRC Press. [Google Scholar]
- Lee JL, & Kim KS (2011). The relationships between stigma, distress, and quality of life in patients with lung cancer. Journal of Korean Oncology Nursing, 11(3), 237–246. [Google Scholar]
- Lelorain S, Brédart A, Dolbeault S, & Sultan S (2012). A systematic review of the associations between empathy measures and patient outcomes in cancer care. Psychooncology, 21(12), 1255–1264. [DOI] [PubMed] [Google Scholar]
- Morse DS, Edwardsen EA, & Gordon HS (2008). Missed opportunities for interval empathy in lung cancer communication. Arch Intern Med, 168(17), 1853–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pehrson C, Banerjee SC, Manna R, Shen MJ, Hammonds S, Coyle N, … Bylund CL (2016). Responding empathically to patients: Development, implementation, and evaluation of a communication skills training module for oncology nurses. Patient education and counseling, 99(4), 610–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollak KI, Arnold RM, Jeffreys AS, Alexander SC, Olsen MK, Abernethy AP,… Tulsky JA (2007). Oncologist communication about emotion during visits with patients with advanced cancer. Journal of Clinical Oncology, 25(36), 5748–5752. [DOI] [PubMed] [Google Scholar]
- Zigmond AS, & Snaith RP (1983). The hospital anxiety and depression scale. Acta psychiatrica scandinavica, 67(6), 361–370. [DOI] [PubMed] [Google Scholar]