Abstract
Background:
Following spine surgery, different types of inhalational anesthetic agents can result in postoperative delirium (POD) that can increase perioperative/postoperative morbidity. Here, we compared the incidence of POD in adults undergoing spine surgery anesthetized with isoflurane versus desflurane.
Methods:
A prospective randomized double-blind clinical trial for patients undergoing spinal surgery was performed in 60 adults (aged 18–65 years); they were randomized to receive isoflurane or desflurane. On postoperative days 1 and 3, the diagnosis and severity of POD utilized 3D-Confusion Assessment Method (CAM) and CAM-severity delirium severity scores to assess patients’ status. Multiple other variables which may have influenced the frequency/severity of POD were also studied.
Results:
For the two groups, the incidence of POD utilizing isoflurane and desflurane was similar on postoperative days 1 (10% vs. 13.3%, P > 0.05) and 3 (6.6% vs. 0%, P > 0.05). The severity scores of POD for both anesthetic agents were also similar on postoperative days 1 (1.5 vs. 1) and 3 (0.5 vs. 0.5). In addition, there was no significant association of POD with other perioperative factors.
Conclusion:
A significant number of patients undergoing spine surgery experience POD. However, the incidence and severity of POD remained similar when utilizing either isoflurane or desflurane.
Keywords: Desflurane, Isoflurane, Postoperative delirium, Spine surgery

INTRODUCTION
Postoperative delirium (POD) occurs between 24 and 72 h after any surgery and can persist for months.[15,16] The reported incidence of POD specifically following spine surgery ranges from 3.3% to 3.8%.[4,8]
Desflurane and isoflurane are two commonly used inhalational anesthetic agents. While animal studies have shown prolonged exposure to isoflurane may be neurotoxic, clinical series have reported faster emergence and less postoperative cognitive dysfunction (POCD) utilizing desflurane.[2,11,12,14,17] Here, in a prospective, randomized double-blind clinical trial involving 60 patients undergoing spine surgery, we compared the incidence of POD at 24 (day 1) and 72 h (day 3) utilizing isoflurane versus desflurane. We also evaluated whether various other perioperative factors differentially influenced the incidence of POD utilizing these two anesthetics.
MATERIALS AND METHODS
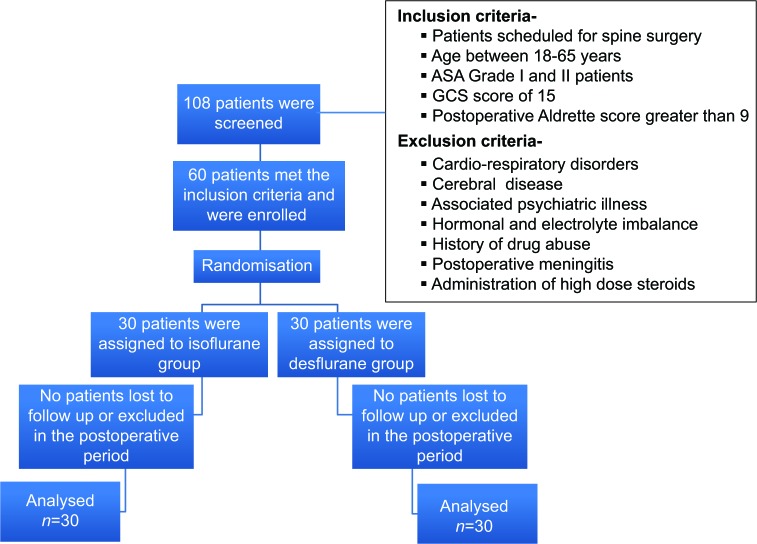
A prospective randomized double-blind clinical trial was conducted (2016–2017) in 60 patients, ages 18–65 years old, scheduled to undergo spine surgery; they provided written informed consent [Figure 1]. They were randomly divided into two equal groups; Group I (Isoflurane; n = 30) and Group D (Desflurane; n = 30) utilizing computer-generated random numbers. There were multiple exclusion criteria [Figure 1]. Further, both the patients and the investigators assessing for POD were blinded to the allocation groups.
Figure 1:
Patient recruitment.
Anesthetic technique
Patients were screened for cognitive dysfunction preoperatively using the Mini-Cog Test.[1] All patients were monitored intraoperatively with five lead electrocardiogram, pulse oximetry, and non-invasive blood pressure assessment. Anesthesia was induced with intravenous (IV) propofol (2–2.5 mg/kg) and fentanyl (2 µg/kg) followed by vecuronium (0.1 mg/kg) (e.g., for endotracheal intubation). Anesthesia was maintained with either isoflurane or desflurane. Fentanyl infusion (0.5–2 µg/kg/h) and intermittent doses of vecuronium (0.06 mg/kg) were administered intraoperatively. State entropy was maintained at 40–60 for adequate depth of anesthesia. After completion of surgery, neuromuscular blockade was reversed with IV neostigmine 0.05 mg/kg and glycopyrrolate 0.01 mg/kg.
Postoperative assessment of POD
The diagnosis and severity of POD utilized the 3D-Confusion Assessment Method (CAM) and CAM-severity (CAM-S) long-form delirium severity score, respectively, on postoperative days 1 and 3.[6,13]
Statistical analysis
The results of a previously conducted study on POCD comparing isoflurane and desflurane were used to calculate the sample size in our study to prove the superiority of desflurane over isoflurane with a margin of at least 5% using an alpha error of 0.05 and power of 85%.[17] The estimated sample size was 60 with 30 in each arm. All statistical analysis was done using SPSS version 22 (SPSS Inc., Chicago, IL, version 16.0 for Windows).
RESULTS
POD results
There were no statistically significant differences utilizing isoflurane versus desflurane on the incidence of POD between the two groups on postoperative days 1 (10% vs. 13.3%) and 3 (6.6% vs. 0%), respectively [Tables 1-3]. There were also similar CAM-S delirium severity scores for isoflurane versus desflurane groups on postoperative days 1 (1.5 vs. 1) and 3 (0.5 vs. 0.5), respectively. Further, the respective postoperative pain scores on day 1 and day 3 were comparable. The median ages of those who tested positive for delirium were also similar; 36 years for postoperative day 1 and 35.5 years for postoperative day 3. A univariable and multivariable analysis was performed to look for the association of the various perioperative factors with POD on day 1 and day 3; there were none (P > 0.05) [Tables 1 and 2].
Table 1:
Demographic and clinical characteristics.
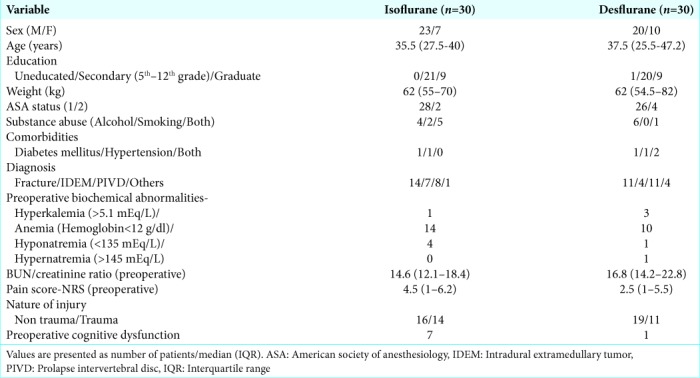
Table 3:
Outcome data: Postoperative delirium.
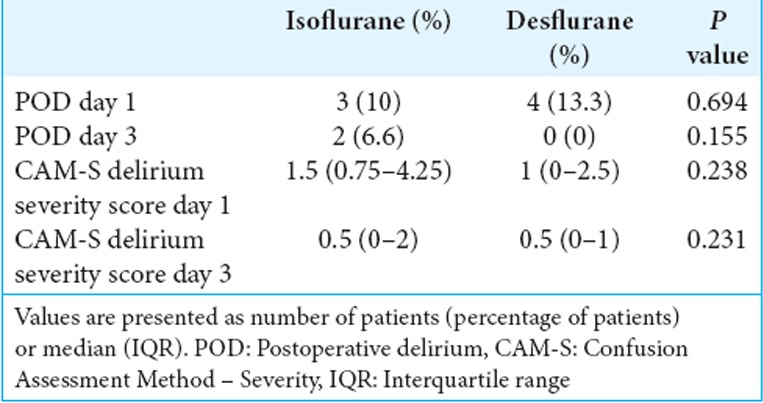
Table 2:
Intraoperative anesthetic and surgical variables.

DISCUSSION
Comparable outcomes for POD with isoflurane versus desflurane
Our original hypothesis was that isoflurane may be associated with an increased incidence of POD versus desflurane in patients undergoing spinal surgery. We found the incidence and severity of POD in middle-aged adults undergoing spine surgery were similar on postoperative days 1 and 3.
Animal studies
Animal studies have demonstrated different incidences of neurotoxicity utilizing isoflurane and desflurane as inhalational anesthetics; some studies showed isoflurane to be neurotoxic, while others demonstrated both isoflurane and desflurane were neuroprotective.[2,3,10-12] In neonatal mice, Kodama et al. demonstrated that desflurane was more neurotoxic than sevoflurane and isoflurane.[9] Alternatively, in newborn mice, Istaphanous et al. showed that equipotent doses of isoflurane, sevoflurane, and desflurane were equally neurotoxic.[7]
Prior incidence of POD in patients undergoing spine surgery
Previous studies on POD following spine surgery showed a higher incidence of delirium in patients older than 60 years.[4,8] In the studies by Gao et al. and Kawaguchi et al., the incidence of POD was 3.3% and 3.8%, respectively.[4,8] However, Kawaguchi et al. found that all patients who tested positive for delirium were older than 70 years of age (POD incidence of 12.5% in >70 years). A prior study in our hospital showed that delirium was diagnosed in 53% of patients 16–45 years of age, 24% who were between 46 and 60 years of age, but in only 19% of patients >60 years of age.[5] Here, we found a comparable overall incidence of POD utilizing isoflurane versus desflurane on postoperative days 1 (11.7%) and 3 (3.3%). Further, the median age of those who tested positive for delirium in our study was 36 years for postoperative day 1 and 35.5 years for postoperative day 3. We also found no significant relationship between POD and other perioperative factors studied.
Limitations
The study included only 60 patients randomized to two different anesthetic groups, and the study was only continued for 3 postoperative days. Further, the baseline incidence of preoperative cognitive dysfunction was higher in the isoflurane (n = 7) versus desflurane groups (n = 1).
CONCLUSION
The incidence and severity of POD in middle-aged patients receiving either isoflurane or desflurane for spine surgery were similar on postoperative days 1 and 3.
Acknowledgements and Disclaimer
Confusion Assessment Method. Copyright 2003, Hospital Elder Life Program, LLC. Not to be reproduced without permission.
No responsibility is assumed by the Hospital Elder Life Program, LLC for any injury and/or damage to persons or property arising out of the application of any of the content at hospitalelderlifeprogram.org.
Footnotes
How to cite this article: Joys S, Samra T, Kumar V, Mohanty M, Sodhi HB, Mahajan S, et al. Comparison of postoperative delirium in patients anesthetized with isoflurane versus desflurane during spinal surgery: A prospective randomized controlled trial. Surg Neurol Int 2019;10:226.
Contributor Information
Steve Joys, Email: stevejoys@gmail.com.
Tanvir Samra, Email: drtanvirsamra@yahoo.in.
Vishal Kumar, Email: drkumarvishal@gmail.com.
Manju Mohanty, Email: manjumohanty2011@gmail.com.
Harsimrat B. S. Sodhi, Email: sodhiharsimrat@gmail.com.
Shalvi Mahajan, Email: drshalvimahajan@gmail.com.
Hemant Bhagat, Email: bhagat.hemant@pgimer.edu.in.
Ethics approval
Clearance to conduct the study was obtained from the Institute Ethics Committee on April 4, 2016 (reference number 10313/PG-2Trg/2015/5408-9), in accordance with the Helsinki Declaration of 1975, as revised in 2000. The trial was registered with clinicaltrials.gov on October 6, 2016 (clinicaltrials.gov identifier NCT02925611).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Borson S, Scanlan J, Brush M, Vitaliano P, Dokmak A. The mini-cog: A cognitive ‘vital signs’ measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry. 2000;15:1021–7. doi: 10.1002/1099-1166(200011)15:11<1021::aid-gps234>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 2.Brambrink AM, Evers AS, Avidan MS, Farber NB, Smith DJ, Zhang X, et al. Isoflurane-induced neuroapoptosis in the neonatal rhesus macaque brain. Anesthesiology. 2010;112:834–41. doi: 10.1097/ALN.0b013e3181d049cd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Engelhard K, Werner C, Reeker W, Lu H, Möllenberg O, Mielke L, et al. Desflurane and isoflurane improve neurological outcome after incomplete cerebral ischaemia in rats. Br J Anaesth. 1999;83:415–21. doi: 10.1093/bja/83.3.415. [DOI] [PubMed] [Google Scholar]
- 4.Gao R, Yang ZZ, Li M, Shi ZC, Fu Q. Probable risk factors for postoperative delirium in patients undergoing spinal surgery. Eur Spine J. 2008;17:1531–7. doi: 10.1007/s00586-008-0771-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grover S, Subodh BN, Avasthi A, Chakrabarti S, Kumar S, Sharan P, et al. Prevalence and clinical profile of delirium: A study from a tertiary-care hospital in north India. Gen Hosp Psychiatry. 2009;31:25–9. doi: 10.1016/j.genhosppsych.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 6.Inouye SK, Kosar CM, Tommet D, Schmitt EM, Puelle MR, Saczynski JS, et al. The CAM-S: Development and validation of a new scoring system for delirium severity in 2 cohorts. Ann Intern Med. 2014;160:526–33. doi: 10.7326/M13-1927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Istaphanous GK, Howard J, Nan X, Hughes EA, McCann JC, McAuliffe JJ, et al. Comparison of the neuroapoptotic properties of equipotent anesthetic concentrations of desflurane, isoflurane, or sevoflurane in neonatal mice. Anesthesiology. 2011;114:578–87. doi: 10.1097/ALN.0b013e3182084a70. [DOI] [PubMed] [Google Scholar]
- 8.Kawaguchi Y, Kanamori M, Ishihara H, Abe Y, Nobukiyo M, Sigeta T, et al. Postoperative delirium in spine surgery. Spine J. 2006;6:164–9. doi: 10.1016/j.spinee.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 9.Kodama M, Satoh Y, Otsubo Y, Araki Y, Yonamine R, Masui K, et al. Neonatal desflurane exposure induces more robust neuroapoptosis than do isoflurane and sevoflurane and impairs working memory. Anesthesiology. 2011;115:979–91. doi: 10.1097/ALN.0b013e318234228b. [DOI] [PubMed] [Google Scholar]
- 10.Liu J, Wang P, Zhang X, Zhang W, Gu G. Effects of different concentration and duration time of isoflurane on acute and long-term neurocognitive function of young adult C57BL/6 mouse. Int J Clin Exp Pathol. 2014;7:5828–36. [PMC free article] [PubMed] [Google Scholar]
- 11.Loepke AW, Istaphanous GK, McAuliffe JJ, 3rd, Miles L, Hughes EA, McCann JC, et al. The effects of neonatal isoflurane exposure in mice on brain cell viability, adult behavior, learning, and memory. Anesth Analg. 2009;108:90–104. doi: 10.1213/ane.0b013e31818cdb29. [DOI] [PubMed] [Google Scholar]
- 12.Loepke AW, Soriano SG. An assessment of the effects of general anesthetics on developing brain structure and neurocognitive function. Anesth Analg. 2008;106:1681–707. doi: 10.1213/ane.0b013e318167ad77. [DOI] [PubMed] [Google Scholar]
- 13.Marcantonio ER, Ngo LH, O’Connor M, Jones RN, Crane PK, Metzger ED, et al. 3D-CAM: Derivation and validation of a 3-minute diagnostic interview for CAM-defined delirium: A cross-sectional diagnostic test study. Ann Intern Med. 2014;161:554–61. doi: 10.7326/M14-0865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pensado Castiñeiras A, Rama Maceiras P, Molins Gauna N, Fiqueira Moure A, Vásquez Fidalgo A. Immediate anesthesia recovery and psychomotor function of patient after prolonged anesthesia with desflurane, sevoflurane or isoflurane. Rev Esp Anestesiol Reanim. 2000;47:386–92. [PubMed] [Google Scholar]
- 15.Silverstein JH, Timberger M, Reich DL, Uysal S. Central nervous system dysfunction after noncardiac surgery and anesthesia in the elderly. Anesthesiology. 2007;106:622–8. doi: 10.1097/00000542-200703000-00026. [DOI] [PubMed] [Google Scholar]
- 16.Whitlock EL, Vannucci A, Avidan MS. Postoperative delirium. Minerva Anestesiol. 2011;77:448–56. [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang B, Tian M, Zhen Y, Yue Y, Sherman J, Zheng H, et al. The effects of isoflurane and desflurane on cognitive function in humans. Anesth Analg. 2012;114:410–5. doi: 10.1213/ANE.0b013e31823b2602. [DOI] [PMC free article] [PubMed] [Google Scholar]