Abstract
The macroenzyme form of aspartate aminotransferase (macro-AST) is formed by the binding of AST with immunoglobulins. Macro-AST excretion from serum is prolonged because of its high molecular weight, leading to increased AST activities. Because of the difficulty in detecting macro-AST through routine laboratory tests, affected patients often undergo repeated examinations, with associated anxiety. We report a case in which macro-AST was detected by assaying the patient’s serum after refrigeration at 4ºC for 3 days. The sample showed progressive loss of AST activity compared with that frozen in the refrigerator, indicating the presence of macro-AST, which was confirmed as a complex with IgG-κ. The cold storage method was validated using many samples obtained from several patients. Use of this simple method to detect macro-AST may avoid unnecessary examinations and patient anxiety even at primary care facilities.
Keywords: isolated elevation of aspartate aminotransferase, macroenzyme, macro-AST, cold storage method
Introduction
Increased enzyme activity in serum is usually considered representative of the existence of disease. However, enzyme levels can also be elevated in the presence of benign high-molecular-mass complexes known as macroenzymes. Macroenzymes are formed by the binding of enzymes with immunoglobulins (Ig) or other plasma components.1 Because of the large molecular size of macroenzymes, their excretion from serum is prolonged and enzyme activities remain higher. Although macroenzymes are usually benign, they frequently interfere with routine laboratory examinations; thus, distinguishing between enzyme activity and a corresponding macroenzyme species is difficult.2,3 The presence of macroenzymes may lead to diagnostic confusion and expensive and time-consuming retesting, or invasive investigations, as well as anxiety to the patient. Therefore, an accurate diagnosis of macroenzyme is important to avoid unnecessary tests and relieve patient anxiety.
We had an adult patient with chronic and isolated increased aspartate aminotransferase (AST) caused by the macroenzyme, macro-AST. This report illustrates the importance of diagnosing macro-AST to avoid frequent examinations and patient anxiety. We got a written informed consent from this patient to have the case details published.
Case Presentation
A 22-year-old woman presented to the general medicine department at the Nara Medical University Hospital in good physical condition, with a 2-year history of persistent AST elevation almost 10 times the upper limit of normal, which was detected repeatedly at several clinics, without clarification of its cause. The AST elevation had been noted initially when she had visited a clinic for a common cold. She had no family history of liver or muscle diseases, and no recent history of taking medicine.
During the 2 years before presenting to us, the patient frequently searched the internet for diseases related to AST elevation. The possibility of serious disease made her anxious and depressed.
At first presentation to our hospital, she looked well and had no physical complaints. She had no abdominal symptoms and no tenderness in response to palpation of the abdomen. Systemic review and physical examination were unremarkable.
Laboratory findings showed elevated AST level of 232 U/L (normal level <12 U/L), normal mitochondrial AST level of 2 U/L, normal level of alanine aminotransferase (ALT; 12 U/L), normal level of lactate dehydrogenase (152 IU/L), normal level of creatine kinase (48 U/L), and no other abnormal findings. Screening tests for hepatitis B, hepatitis C, cytomegalovirus, and Epstein-Barr virus were all negative. Additionally, she had no signs of connective tissue diseases or metabolic diseases, or drug abuse. A liver ultrasound did not reveal any abnormal findings.
None of these laboratory results clarified the reason for the independently increased serum AST level. Further workup was not conducted because of her overall positive health.
Based on the patient’s history of good health without remarkable findings, benign causes for the increased AST level including macro-AST were suspected. To relieve the patient’s anxiety, we decided to assess her for macro-AST to confirm a benign etiology for the elevated AST.
Methods And Results
According to the method described by Davidson and Watson,4 cold storage method was applied to detect macro-AST. In brief, serum samples were divided into 4 aliquots and frozen in a −20 ºC freezer (such as the part of the home refrigerator) until cold storage test started. As long as serum samples were placed at lower than −20 ºC, the enzymes activity of serum will not change. The three aliquots were thawed and placed into a 4 °C refrigerator for 1, 2, and 3 days, respectively. The activities of AST of the aliquots that had been placed at 4 °C were compared with that placed at −20 ºC. One normal healthy serum (AST; 31 U/L), and 16 pathological control serums (AST ranged from 181 to 382 U/L) obtained from other patients with liver dysfunction including hepatocellular carcinoma, nonalcoholic steatohepatitis, autoimmune hepatitis, lymphoid myocarditis, acute obstructive cholangitis, or liver cirrhosis were also investigated using cold storage method. As it is reported previously,5 the AST level of the patient decreased (decrease rate; around 80%, from 210 to 43 U/L in our case), while the AST levels of the pathological and healthy controls were stable (decrease rate; mean±2SD, 0.61% ±2.5%) in Table 1, suggesting that the AST of our patient was macro-AST.
Table 1.
Serum AST Activity (IU/L) Changes After Cold Storage
| Period At 4°C (Days) | Day0 | Day1 | Day2 | Day3 | Decrease Rate(%): 100X(Day0-Day3)/Day0 |
|---|---|---|---|---|---|
| Maro-AST (present case) | 210 | 111 | 65 | 43 | 79.5 |
| Pathological control samples (n=16) |
224.1±62.1 | 223.1±62.3 | 223.4±63.0 | 223.0±62.6 | 0.61±1.23 |
| Normal (n=1) | 31 | 29 | 30 | 30 | 3.2 |
Note: Expressed as mean ± standard deviation.
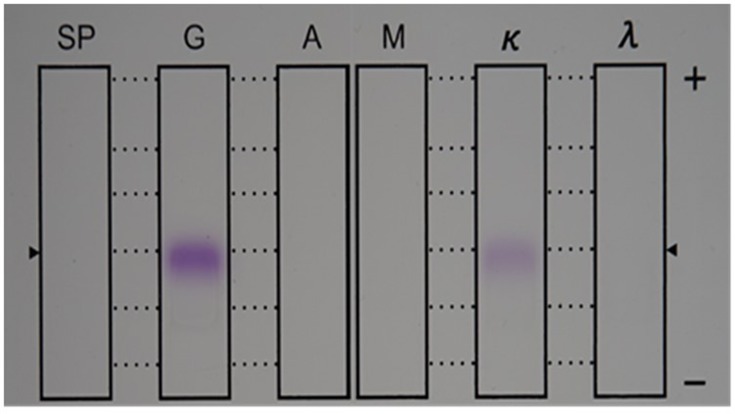
Next, we conducted 2 experiments to confirm the existence of macro-AST as described previously.6 First, AST activity was examined after Ig absorption. As shown in Table 2, AST activity was decreased after IgG absorption, but not after IgA or IgM absorption, indicating AST was bound with IgG. Plasma immunofixation electrophoresis with AST staining (Kainos, Tokyo, Japan) was performed. These results confirmed that the AST molecule of the patient was an anomaly of AST formed by binding with IgG-κ (Figure 1). Thus, we made the diagnosis of benign macro-AST as the cause of our patient’s elevation of AST, much to her relief.
Table 2.
AST And ALT Activity After IgG, IgA, Or IgM Absorption
| AST (U/L) | ALT (U/L) | IgG (mg/dL) | IgA (mg/dL) | IgM (mg/dL) | |
|---|---|---|---|---|---|
| No absorption | 201 | 9 | 1227 | 141 | 153 |
| IgG absorption | 9 | 6 | 42 | 147 | 207 |
| IgA absorption | 201 | 12 | 1338 | 12 | 189 |
| IgM absorption | 183 | 9 | 1314 | 138 | 0 |
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; Ig, immunoglobulin.
Figure 1.
Immunofixation electrophoresis with AST staining. The serum protein (SP) lane represents routine electrophoresis of this patient’s serum. On the next 3 protein separations, antiserum against IgG, IgA, and IgM were applied to the G, A, and M lanes, respectively. Antiserum to κ light chain was added to the next protein separation, and antiserum to λ light chain was added to the last protein separation. Positive bands (purple) were detected on the anti-IgG antibody lane and anti-IgG-κ antibody lane, which proved the existence of IgG-κ binding with AST.
Abbreviations: AST, aspartate aminotransferase; Ig, immunoglobulin.
Discussion
AST is distributed in several organs or cells, such as the liver, kidney, brain, muscle, and erythrocytes, among others. When these organs or cells are injured, AST is released into the blood circulation, and consequently the serum level of AST will increase. Thus, an elevated level of serum AST can be a sign of injury or dysfunction of various organs or cells, in which case, serum AST levels will usually increase with some other enzymes depending on the pathological situation, for example, with ALT in the liver disease, or with lactate dehydrogenase in heart disease or hemolysis. Therefore, when a patient has an isolated elevation of serum AST, an accurate diagnosis is usually difficult to obtain. In such a case, further investigations will be conducted, including expensive image diagnostics and sometimes interventional procedures or biopsy. Meanwhile, an undetermined diagnosis usually brings anxiety to the patient, as happened in this case.
If the patient has chronic and isolated AST elevation, no symptoms, and a negative physical examination, existence of macro-AST should be considered. Several reports have indicated that the cause of isolated AST elevation was macro-AST in 40% to 100% of healthy individuals.7,8 Unfortunately, however, routine laboratory examination cannot differentiate between normal AST and the macro-AST molecule. Several methods have been recommended for diagnosing macro-AST, including protein electrophoresis, precipitation with polyethylene glycol or protein-A or G-Sepharose, measurements of heat stability, and size exclusion chromatography.2,6 Polyethylene glycol precipitation, as described by Davidson and Watson,4 seems to be an easy method, but is sometimes difficult for primary care facilities to perform.
This case report has demonstrated a simpler way to detect macro-AST,4 which is based on the decrease of serum level of AST after storage for several days at 4°C in the refrigerator. Our case showed a decrease in AST level of 80% after 3 days at 4°C, comparable to decreases reported in other studies (>90% or a 50% decrease of AST level after 6 days of refrigerated storage4,9). The decrease in AST activity in the sample was possibly due to the precipitation of the enzyme-Ig complex during refrigerated storage.4
Notably, no other samples with elevated AST levels obtained from patients with various diseases (including alcoholic hepatitis, nonalcoholic steatohepatitis, hepatocellular carcinoma, liver cirrhosis, etc.) yielded any significant AST decrease (decrease rate, average±2SD, 0.61%±2.5%), suggesting that this method is useful to differentiate between AST and macro-AST. As far as we investigated in the literature, all patients whose activity in AST decreased by 50% or more within 7 days of cooling at 4°C compared with frozen at −20 °C sample can be considered as macro-AST.10 This method is simple enough to incorporate at primary care facilities, thus enabling the diagnosis of macro-AST at more facilities. Therefore, this method could be used whenever any patient has chronic and an isolated elevation of AST.
Contradictory to our findings, Chtioui et al11 reported that a serum sample from their patient with macro-AST did not show any decrease in AST activity after storage at 4°C for 1 week. This discrepancy may be due to the heterogeneity of the macro-AST molecule implicated by the different types of immunoglobulins or other plasma components. In our report, the macro-AST of the patient was confirmed based on the binding of AST with IgG-κ. Accumulation of information about the components of macro-AST from more studies like our case report will help to confirm that the decrease in AST level after storage at 4°C is indeed diagnostic for macro-AST.
When the cause of chronic and isolated elevation of AST remains unknown, several problems can ensue, such as those observed in the present case. Unnecessary medical expenses from repeated time-consuming and invasive tests can adversely affect patients. In addition, people can access a lot of medical information of dubious quality through the internet that can lead to anxiety about the possibility of having a disease, which can then induce depression. These problems could have been avoided in our patient if a diagnosis had been made earlier. Thus, a rapid accurate diagnosis of macro-AST can relieve the anxiety of patients who have chronic and isolated elevation of AST, because macro-AST does not appear to be pathologic and does not require specific treatment.
Conclusion
Physicians should be aware of benign macro-AST as a cause of chronic and isolated elevation of AST after screening tests for liver dysfunction and detect it using cold storage method to avoid unnecessary examinations and help allay patient’s fears.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Remaley AT, Wilding P. Macroenzymes: biochemical characterization, clinical significance, and laboratory detection. Clin Chem. 1989;35:2261–2270. [PubMed] [Google Scholar]
- 2.Patteet L, Simoens M, Piqueur M, Wauters A. Laboratory detection of macro-aspartate aminotransferase: case report and evaluation of the PEG-precipitation method. Clin Biochem. 2012;45:691–693. doi: 10.1016/j.clinbiochem.2012.03.004 [DOI] [PubMed] [Google Scholar]
- 3.Wener RR, Loupatty FJ, Schouten WE. Isolated elevated aspartate aminotransferase: a surprising outcome for clinicians. Neth J Med. 2012;70:136–138. [PubMed] [Google Scholar]
- 4.Davidson DF, Watson DJ. Macroenzyme detection by polyethylene glycol precipitation. Ann Clin Biochem. 2003;40:514–520. doi: 10.1258/000456303322326425 [DOI] [PubMed] [Google Scholar]
- 5.Castiella A, Aguayo FJ, Rueda M, Fernandez J, Zapata E. Macroaspartate aminotransferase (Macro-AST) a rare cause of hypertransaminasemia: another way to diagnosis? J Clin Gastroenterol. 2006;40:655. doi: 10.1097/00004836-200608000-00024 [DOI] [PubMed] [Google Scholar]
- 6.Krishnamurthy S, Korenblat KM, Scott MG. Persistent increase in aspartate aminotransferase in an asymptomatic patient. Clin Chem. 2009;55:1573–1575. doi: 10.1373/clinchem.2008.120782 [DOI] [PubMed] [Google Scholar]
- 7.Caropreso M, Fortunato G, Lenta S, et al. Prevalence and long-term course of macro-aspartate aminotransferase in children. J Pediatr. 2009;154:744–748. doi: 10.1016/j.jpeds.2008.11.010 [DOI] [PubMed] [Google Scholar]
- 8.Briani C, Zaninotto M, Forni M, Burra P. Macroenzymes: too often overlooked. J Hepatol. 2003;38:119. doi: 10.1016/S0168-8278(02)00333-1 [DOI] [PubMed] [Google Scholar]
- 9.Beşer OF, Laçinel S, Gülcü D, Kutlu T, Cullu Çokuğraş F, Erkan T. An easy method for diagnosing macro-aspartate aminotransferase: a case series. Turk J Gastroenterol. 2014;25:568–570. doi: 10.5152/tjg [DOI] [PubMed] [Google Scholar]
- 10.González RA, Coca ZR, Martín SE. Isolated elevation of aspartate aminotransferase (AST) in an asymptomatic patient due to macro‐AST. J Clin Lab Anal. 2019;33:e22690. doi: 10.1002/jcla.2019.33.issue-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chtioui H, Mauerhofer O, Gunther B, Dufour JF. Macro-AST in an asymptomatic young patient. Ann Hepatol. 2010;9:93–95. doi: 10.1016/S1665-2681(19)31687-4 [DOI] [PubMed] [Google Scholar]