Abstract
Background
Hypoxic ischemic encephalopathy (HIE) in the neonate is associated with high mortality and morbidity. Effective treatment options are limited and therefore alternative therapies such as acupuncture are increasingly used.
Objectives
We sought to determine the efficacy and safety of acupuncture on mortality and morbidity in neonates with HIE.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library), Cochrane Neonatal Specialized Register, MEDLINE, AMED, EMBASE, PubMed, CINAHL, PsycINFO, WHO International Clinical Trials Registry Platform, and various Chinese medical databases in November 2012.
Selection criteria
We planned to include randomized or quasi‐randomized controlled trials comparing needle acupuncture to a control group that used no treatment, placebo or sham treatment in neonates (less than 28 days old) with HIE. Co‐interventions were allowed as long as both the intervention and the control group received the same co‐interventions. We excluded trials that evaluated therapy that did not involve penetration of the skin with a needle or trials that compared different forms of acupuncture only.
Data collection and analysis
Two review authors independently reviewed trials for inclusion. If trials were identified, the review authors planned to assess trial quality and extract data independently. We planned to use the risk ratio (RR), risk difference (RD), and number needed to benefit (NNTB) or harm (NNTH) with 95% confidence intervals (CI) for dichotomous outcomes, and mean difference (MD) with 95% CI for continuous outcomes.
Main results
No trial satisfied our predefined inclusion criteria. Existing trials only evaluated acupuncture in older infants who survived HIE. There are currently no randomized controlled trials evaluating the efficacy of acupuncture for treatment of HIE in neonates. The safety of acupuncture for HIE in neonates is unknown.
Authors' conclusions
The rationale for acupuncture in neonates with HIE is unclear and the evidence from randomized controlled trial is lacking. Therefore, we do not recommend acupuncture for the treatment of HIE in neonates. High quality randomized controlled trials on acupuncture for HIE in neonates are needed.
Keywords: Humans; Infant, Newborn; Acupuncture Therapy; Hypoxia‐Ischemia, Brain; Hypoxia‐Ischemia, Brain/therapy
Plain language summary
Acupuncture for newborn babies with hypoxic ischemic encephalopathy (HIE)
Hypoxic ischemic encephalopathy (HIE) occurs in newborn infants when they lack oxygen in the peripartum period. HIE causes significant morbidity and mortality. Effective treatment options are limited. Acupuncture has been tried. We attempted to evaluate the efficacy and safety of acupuncture for HIE through a systematic review of randomized controlled trials (RCTs). However, no RCT was identified in a systematic and comprehensive search of the medical literature. Good evidence regarding the use of acupuncture for neonates with HIE is lacking currently. The safety of acupuncture for HIE in neonates is unknown. High quality RCTs are needed.
Background
Description of the condition
Peripartum asphyxia affects three to five per 1000 live births, with moderate or severe hypoxic ischemic encephalopathy (HIE) in 0.5 to 1 per 1000 live births (Jacobs 2007). HIE is caused by the lack of oxygen and blood flow to the brain. At the reperfusion phase after initial injury, there is an accumulation of inflammatory cells and mediators that also contribute to ongoing brain injury (Perlman 2006).
Newborns with HIE have a high incidence of mortality and morbidity; 10% to 60% of affected infants die and at least 25% of survivors have long‐term neurodevelopmental sequelae (Vannucci 1990). In most cases, the underlying cause and the timing of HIE remains unknown; however, it can be characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia (Gonzalez 2006).
The incidence of long‐term complications of HIE depends on the severity of the disease. Up to 80% of infants who survive severe HIE develop significant long‐term neurological disabilities (mental delay, intellectual disability, epilepsy, and cerebral palsy of varying degrees including hemiplegia, quadriplegia or dyskinetic type), 10% to 20% develop moderately serious disabilities and up to 10% are normal. Among the infants who survive moderately severe HIE, up to 50% may suffer from serious long‐term complications (Evan 2001).
Supportive treatment of the infant with HIE is the mainstay of care. Current recommendations to control the complications of HIE include careful management of fluids with avoidance of fluid overload in the hope of avoiding cerebral edema (Chalak 2007). With the possible exception of therapeutic mild hypothermia, no intervention has shown promising results in limiting mortality or brain damage in newborn infants with HIE (Edwards 2006; Jacobs 2007). The systematic review by Jacobs concluded that evidence from eight randomized controlled trials suggested that therapeutic hypothermia was beneficial to term newborns with HIE (Jacobs 2007). Cooling reduced mortality without increasing major disability in survivors. The benefits of cooling on survival and neurodevelopment outweighed the short‐term adverse effects. Therapeutic hypothermia resulted in a statistically significant and clinically important reduction in the combined outcome of mortality and major neurodevelopmental disability to 18 months of age, with a number needed to treat for benefit (NNTB) of seven (95% confidence interval (CI) 4 to 14). Cooling also resulted in statistically significant reductions in mortality, with a NNTB of 11 (95% CI 6 to 50), and in neurodevelopmental disability in survivors. Adverse effects of hypothermia included an increase in the need for inotrope support and an increase in thrombocytopenia.
In China, cerebrolysin is sometimes used in neonates with HIE (Liu 1994; Zhang 2010). Cerebrolysin is a peptide mixture isolated from pig brain with standardized enzymatic breakdown of lipid‐free porcine brain proteins. It is composed of 25% low molecular weight peptides and 75% free amino acids. It has antioxidant property (Gonzalez 1998) and exerts neurotrophic as well as neuroprotective effects both in vitro (Satou 2000; Hartbauer 2001) and in vivo (Veinbergs 2000; Tatebayashi 2003). Clinical trials suggested that cerebrolysin might be effective in dementia (Alvarez 2011; Guekht 2011), ischemic stroke (Skvortsova 2004; Ladurner 2005), and intracranial hemorrhage (Maksimova 2009). Cerebrolysin appears safe as adverse events are rare and equally frequent in the cerebrolysin‐treated and control groups.
In China, Citicoline is also sometimes used in neonates with HIE (Tian 2007; Wang 2011). Citicoline is a compound normally present in all cells and is an intermediate in the biosynthesis of phosphatidylcholine. It has been shown to have neuroprotective effects in many brain injury models, including cerebral ischemia (Hurtado 2011). Meta‐analysis suggested beneficial effects on patients with ischemic stroke (Davalos 2002). Adverse effects of citicoline include nausea, vomiting, diarrhea, liver dysfunction, hypotension, and bradycardia or tachycardia (Fernandez 1983; Tazaki 1988).
Hyperbaric oxygen has also been used for neonatal HIE (Liu 2001; Wang 1999). This treatment has been shown to decrease cerebral edema, normalize water content in the brain, decrease the severity of brain infarction, and maintain blood‐brain barrier integrity (Al‐Waili 2005). In studies that investigated the effects of this therapy on the damaged brain, hyperbaric oxygen was found to inhibit neuronal death, arrest the progression of radiation‐induced neurologic necrosis, improve blood flow in regions affected by chronic neurologic disease as well as aerobic metabolism in brain injury, and accelerate the resolution of clinical symptoms (Al‐Waili 2005). In some studies of cerebral palsy, hyperbaric oxygen therapy improved the function of damaged cells, attenuated the effects of hypoxia on the neonatal brain, enhanced gross motor function and fine motor control, and alleviated spasticity (Al‐Waili 2005). Adverse effects associated with hyperbaric oxygen include damage to the ears, sinuses and lungs from the effects of pressure (Shupak 2008), claustrophobia and oxygen poisoning (Leach 1998).
Description of the intervention
Acupuncture has been an integral part of Traditional Chinese Medicine (TCM) for 2000 years and has become more established in Western medicine as a complement or alternative to conventional therapies. The increased use of acupuncture is, in part, due to the low risk of complications and side effects (Vickers 1999; MacPherson 2001; White 2001).
Traditional Chinese Medicine postulates that the body has a constant energy force running through it, known as Qi. This is the essential life activating force that includes the spiritual, emotional, mental and the physical aspects of life. It flows up and down in the body by special pathways called meridians. It is believed that interruptions or imbalances in the flow of Qi lead to illness. A series of specific points along the meridians can be used to alter the flow of Qi, by needle insertion or other manipulations termed acupuncture. The proponents of TCM believe that acupuncture treatment can regulate the flow of Qi, promoting the balance and flow of energy throughout the body. In the study of the biological basis of medical acupuncture, investigators try to identify anatomical correlates and physiological and biochemical mechanisms that may explain the ancient idea of the flow of Qi and the meridian points. Electrical impedance of connective tissues can be measured around meridian points (Wong 2010) and connective tissues associated with meridians may have lower electrical impedance than non‐meridian tissues (Ahn 2005). There is currently no strong evidence to show that acupoints correspond to any specific anatomical feature. Proponents believe that acupoints lie in close proximity to the nervous system (Fu 2000). One study (Dung 1984) investigated the anatomical features of acupoints and found that structures around acupoints exclusively involved nerves. Therefore, it is hypothesized that a sequence of neurological responses might be elicited by needle acupuncture at these innervated acupoints. Acupuncture is a treatment procedure in which steel, silver or gold needles are inserted into specific meridian points in order to influence physiological functioning of the body for therapeutic purposes (Cabyoglu 2006). Apart from the traditional needle acupuncture, various other forms of acupuncture have been developed including electro‐acupuncture (electric stimulation of the needle following insertion), laser acupuncture (a variant of acupuncture in which needling is replaced by laser irradiation on the points) and acupoints injection (injection of liquid medicine into the acupuncture points). Acupoint injection is a relatively new method of acupuncture that is increasingly used. Acupoint injection combines the use of modern medicine with traditional needle acupuncture. Administration of small amount of medications into acupoints may reduce the adverse effects of the medications as well as increase their therapeutic effects (Ni 2003). Several medications have been used in injection acupuncture therapy, including steroid, local anesthetic, growth factors, atropine, vitamin B1, vitamin B12 and herbal extracts (Lu 2008).
A survey of acupuncture that was released by a US National Institutes of Health (NIH) Consensus Development Panel suggested that promising data existed for the use of acupuncture in treating postoperative or chemotherapy induced nausea and vomiting as well as postoperative dental pain in adults, although there were inherent problems of study design, sample size and appropriate controls in the acupuncture literature (NIH Consensus 1998).
The effect of acupuncture may vary with the number of needles inserted, needle diameter, duration of stimulation, the frequency, and environmental and psychological factors. With this in mind, standardization of study protocols, where all patients receive the same treatment, will improve the validity of acupuncture studies. The most commonly reported adverse effects of acupuncture are needle site bleeding, needle pain, bruising and aggravation of symptoms which are caused by needle penetration (Vickers 1999; MacPherson 2001; White 2001). No special adverse effects have been reported in neonates who received acupuncture.
How the intervention might work
Acupuncture has been used for thousands of years to treat a variety of diseases and symptoms. The mechanisms of action for acupuncture are not completely understood. Some researchers report that levels of neurotransmitters such as endomorphin‐1, beta endorphin, encephalin and serotonin increase in plasma and brain tissue through acupuncture (Cabyoglu 2006). A variety of Cochrane reviews have addressed the application of acupuncture in neurological conditions. These include idiopathic headache (Melchart 2009), insomnia (Cheuk 2012), Bell's palsy (He 2010), epilepsy (Cheuk 2006), stroke rehabilitation (Wu 2008) and acute stroke (Zhang 2008a). The results of these reviews are generally equivocal or contradictory.
Why it is important to do this review
Anecdotal reports (Meng 2003; Liu 2006; Liu 2003) have suggested that acupuncture may reduce the occurrence or severity of complications of neonates suffering from HIE. Recently, a number of clinical trials were performed to study the efficacy of acupuncture for HIE. It remains uncertain whether the existing evidence is rigorous enough to support the use of acupuncture in HIE. For this reason, we decided to undertake a systemic review of all the randomized controlled trials of acupuncture therapy for HIE in neonates to summarize the currently available evidence and to provide the best available evidence to inform both clinical practice and further research planning on the treatment of HIE.
Objectives
To determine the effect of acupuncture on mortality and morbidity in neonates with HIE and the safety of acupuncture in these patients.
We investigated the following hypotheses:
acupuncture is effective in either short term (seizures, death) or long term (developmental delay, intellectual impairments, visual or auditory impairments) outcomes or both;
acupuncture can improve the speed of rehabilitation;
acupuncture can reduce the extent of disability (as a result of HIE complications) in neonates with HIE;
acupuncture can improve the quality of life of neonates with HIE;
acupuncture is safe.
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials and quasi‐randomized trials. Cross‐over and cluster trials were excluded.
Types of participants
Inclusion criteria
Newborn infants: term neonates with postnatal age of 28 days or less would be included.
-
Evidence of peripartum asphyxia with each enrolled infant satisfying at least one of the following criteria:
Apgar score of 5 or less at 10 minutes;
mechanical ventilation or resuscitation at 10 minutes;
cord blood pH < 7.1, or an arterial blood pH < 7.1 or base deficit of 12 or more within 60 minutes of birth.
-
Evidence of encephalopathy according to Sarnat staging (Sarnat 1976):
stage 1 (mild): hyperalertness, hyperreflexia, dilated pupils, tachycardia, absence of seizures;
stage 2 (moderate): lethargy, hyperreflexia, miosis, bradycardia, seizures, hypotonia with weak suck and Moro;
stage 3 (severe): stupor, flaccidity, small to mid position pupils which react poorly to light, decreased stretch reflexes, hypothermia and absent Moro.
Exclusion criteria
Major congenital abnormalities or syndromes recognizable at birth.
Types of interventions
Trials evaluating all forms of acupuncture therapy which involve the penetration of the skin with needles, including scalp acupuncture, body acupuncture, auricular acupuncture, tongue acupuncture, injection acupuncture or electro‐acupuncture, or any combination of the above, regardless of frequency of treatment, duration of the treatment period and location(s) of stimulation (for example scalp, body, tongue, or ear) would be included.
We excluded other forms of acupuncture therapy that do not involve penetration of the skin with a needle, such as acupressure, laser acupuncture and percutaneous neuromodulation.
Acupuncture could be given alone or in combination with conventional medical treatment for HIE. The control intervention might be no treatment, placebo acupuncture, sham acupuncture, or conventional medical treatment (which may be baseline treatment) for HIE. We planned to analyse these separately. Placebo acupuncture refers to a needle attached to the skin surface (not penetrating the skin but at the same acupoints) (White 2001). Sham acupuncture refers to a needle placed in an area close to, but not in, acupuncture points (Streitberger 1998; White 2001; Lund 2006) or subliminal skin electro‐stimulation via electrodes attached to the skin (SCSSS 1999).
The treatment comparisons investigated in this review were:
acupuncture alone versus no treatment;
acupuncture alone versus placebo or sham treatment;
acupuncture in combination with conventional medical intervention versus same conventional medical intervention alone;
acupuncture in combination with conventional medical intervention versus placebo or sham acupuncture in combination with same conventional medical intervention.
The frequency and duration of treatment were not restricted for inclusion in the current review. We excluded studies comparing different forms of acupuncture only (different manipulation methods or different acupoints) since these studies could not deduce the net effect of acupuncture and hence were unable to demonstrate the efficacy of acupuncture per se.
Types of outcome measures
Primary outcomes
Infant mortality (death during the first year of life).
Long‐term (> 12 months) major neurodevelopmental disability such as cerebral palsy, developmental delay (Bayley or Griffith assessment more than 2 SD below the mean) or intellectual impairment (IQ more than 2 SD below mean), blindness (vision < 6/60 in both eyes), sensorineural deafness requiring amplification, or any combination of these disabilities.
Secondary outcomes
Frequency of seizures, either apparent clinically or detected by electro‐encephalographic recordings.
Frequency of cortical, white matter, or basal ganglia abnormalities on brain imaging (computed tomography (CT), magnetic resonance imaging (MRI) or ultrasound) in the first month of life and at 12 months of age or more.
Quality of life scores if assessed by validated and reliable scales.
Frequency of adverse events of acupuncture during treatment period and after treatment period, including needle site bleeding, needle pain, bruising, aggravation of symptoms and other adverse events.
Search methods for identification of studies
We planned to identify all relevant trials regardless of date, language, or publication status.
Electronic searches
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2012, Issue 2) on 7 May 2011. We also searched the Cochrane Neonatal Specialized Register on 23 May 2011. This register contains reports of trials identified from regular searches of CENTRAL and MEDLINE. Relevant reports are also identified by handsearching selected journals and conference proceedings. In addition, we searched MEDLINE (1948 to week 4 April 2011, searched on 6 May 2011); MEDLINE® In‐Process & Other Non‐Indexed Citations (searched on 5 May 2011); OLDMEDLINE® (1946 to 1965, searched on 6 May 2011); AMED (Allied and Complementary Medicine Database) (1985 to May 2011, searched on 6 May 2011); EMBASE (1947 to 2011 Week 17, searched on 6 May 2011); PubMed, MedlinePlus and PubMed Ahead of Print (searched on 6 May 2011) via Ovid; CINAHL Plus (1982 to 2010, searched on 6 May 2011) via EBSCOhost; PsycINFO (1872 to 2011, searched on 6 May 2011) via CSA Internet Database Service; and WHO International Clinical Trials Registry Platform (ICTRP) at www.who.int/ictrp (searched on 7 May 2011).
Major mainland Chinese academic literature databases were also searched on 6 May 2011 using keywords in both traditional and simplified Chinese: China Journal Full‐text Database (1915 to 2011), China Master Theses Full‐text Database (1999 to 2011), China Doctor Dissertation Full‐text Database (1999 to 2011), China Proceedings of Conference Database (2000 to 2011) via China National Knowledge Infrastructure (CNKI), Wei Pu Information (VPI) (1989 to 2011), Wang Fang Data (1980 to 2010) and Index to Taiwan Periodical Literature System (1970 to 2011).
We updated these searches on November 5, 2012.
All electronic search strategies are reported in full in the Appendices (Appendix 1; Appendix 2; Appendix 3; Appendix 4; Appendix 5; Appendix 6).
Searching other resources
We searched the reference lists of all relevant papers and trials registries for further studies. In addition, we contacted colleagues and experts in the field to ascertain any unpublished or ongoing studies. Multiple publications reporting the same groups of patients or subsets were considered as one single study.
Data collection and analysis
Two review authors (VW and VC) ran the searches and collated the search results.
Selection of studies
Two review authors (VW and VC) independently reviewed titles and abstracts of references retrieved from the searches and selected all potentially relevant studies. Copies of these articles were obtained and reviewed independently by the same review authors against the inclusion criteria of the review. Review authors were not blinded to the names of the trials' authors, institutions or journals of publication. The review authors then extracted data from included trials and assessed trial quality independently. Where disagreements occurred, the third review author (DKLC) considered the article and decided the outcome.
Data extraction and management
The following data were extracted, if available.
(1) Study methods:
design;
randomization method (including list generation);
method of allocation concealment;
blinding method;
stratification factors.
(2) Participants:
inclusion and exclusion criteria;
number of patients entering the trial, number of patients randomized, number of excluded patients (with reasons), and number of evaluable patients;
age and sex distribution;
clinical stage of perinatal hypoxic ischemic brain injury.
(3) Intervention and control:
type of acupuncture;
details of treatment regime including duration of treatment;
type of control;
details of control treatment including drug dosage and schedules;
details of co‐interventions.
(4) Follow‐up data:
duration of follow‐up;
loss to follow‐up;
dates of treatment withdrawal and reasons for treatment withdrawal;
withdrawal rates.
(5) Outcome data:
as described above.
(6) Analysis data:
methods of analysis (intention‐to‐treat and per protocol analysis);
comparability of groups at baseline (yes or no);
statistical techniques.
Two review authors independently extracted data from included studies. All differences were resolved by discussion among the review authors.
Assessment of risk of bias in included studies
Two review authors (VW and VC) independently assessed the methodological quality of each eligible trial using the Cochrane Collaboration's tool for assessing risk of bias (Higgins 2011). The third review author (DKLC) resolved any discrepancies regarding the methodological quality.
We examined the risk of bias derived from the methods used to generate the concealment of randomization, blinding of intervention, completeness of outcome data, selective reporting and other risk of bias according to Cochrane Neonatal Review Group (CNRG) Guidelines.
There has been concern that trials conducted in China and published as RCTs might not have assigned subjects by random allocation. If studies were identified, we planned to contact authors to clarify the randomization method.
Measures of treatment effect
We planned to use risk ratio (RR) and risk difference (RD) with 95% confidence intervals (CI) for binary outcomes. We also planned to calculate number needed to treat to benefit (NNTB) and to harm (NNTH). We planned to use mean difference (MD) with 95% CI for continuous outcomes. All analyses included all participants in the treatment groups to which they were allocated (intention‐to‐treat analyses). We planned to perform per protocol analyses if information for intention‐to‐treat analyses was lacking.
Unit of analysis issues
The patient was the unit of analysis.
Dealing with missing data
We contacted the authors of included studies to supply missing data. Missing data and drop‐outs or attrition were to be assessed for each included study, and the extent to which the results or conclusions of the review could be altered by the missing data were to be assessed and discussed. If, for a particular outcome, less than 80% of patients allocated to the treatments were reported on at the end of the trial, those data were not used as they were considered to be too prone to bias.
Assessment of heterogeneity
Clinical heterogeneity would be assessed by comparing the distribution of important participant factors between trials (age, sex, specific diagnosis or diagnostic subtypes, severity of HIE), and trial factors (randomization concealment, blinding of outcome assessment, losses to follow‐up, treatment regimens, co‐interventions). We planned to assess statistical heterogeneity by examining the I2 statistic (Higgins 2002), which describes the proportion of variation in point estimates that is due to heterogeneity rather than sampling error. If significant heterogeneity was present (that is, I2 ≥ 50% (Higgins 2011), we planned to investigate trials for possible explanations.
A rough guide to interpretation of I2 is as follows:
0% to 40%, might not be important;
30% to 60%, may represent moderate heterogeneity;
50% to 90%, may represent substantial heterogeneity;
75% to 100%, considerable heterogeneity.
Assessment of reporting biases
We planned to draw funnel plots (estimated differences in treatment effects against their standard error) if sufficient studies (more than five) were found. Asymmetry could be due to publication bias but could also be due to a relationship between trial size and effect size. In the event that a relationship was found, we intended to examine the clinical diversity of the studies (Egger 1997). However, we did not draw a funnel plot because no study was included.
Data synthesis
Where the interventions were the same or similar enough, we intended to synthesize results in a meta‐analysis where there was no important clinical heterogeneity. If no significant statistical heterogeneity was present, we planned to synthesize the data using a fixed‐effect model. However, no trial was included and therefore no meta‐analysis was possible.
Subgroup analysis and investigation of heterogeneity
If data permitted, we planned to conduct subgroup analyses for the different age groups, type of acupuncture and severity of HIE, to assess whether the treatment effects varied between subgroups. However, since no trial was included we could not perform any subgroup analysis.
Sensitivity analysis
We planned to perform sensitivity analyses to assess the impact of study quality, assessing:
all studies;
only those with adequate methods of allocation concealment.
However, no study was included and therefore sensitivity analysis was not performed.
Results
Description of studies
Results of the search
The electronic searches yielded a total of 119 records. We did not find any additional records from other sources. After we removed duplicates, 111 records remained. We screened all these records and excluded 94 records based on information in the title or abstract. We obtained full texts of the remaining 17 records reporting 16 trials (one trial was reported in two papers). We excluded 16 records (reporting 15 trials). One record (Liu 2003) awaited classification because we were uncertain whether the intervention involved needle acupuncture and we waited for a reply from the study authors for clarification. None of the trials fulfilled the prespecified inclusion criteria. The flow of studies is shown in Figure 1.
1.
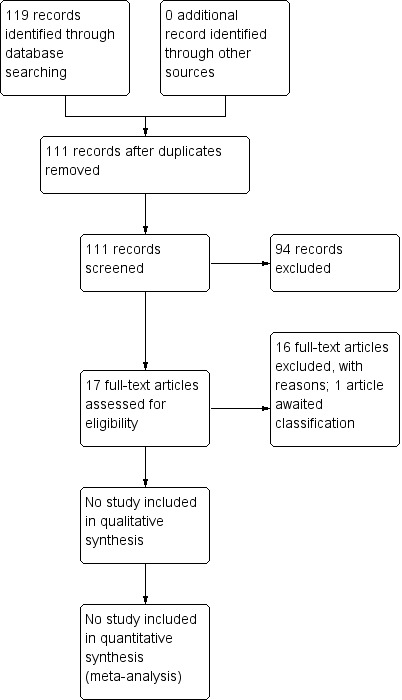
Study flow diagram.
Included studies
No study was included as none of the identified studies fulfilled the inclusion criteria.
Excluded studies
We summarized the reasons for exclusion in the table 'Characteristics of excluded studies'. Eight trials actually evaluated acupoint massage that did not involve needle acupuncture (Li 2003; Chen 2006; Guo 2007; Liu 2007; Zhang 2008; Li 2008; Cai 2008; Wu 2010). One trial evaluated body massage and not needle acupuncture (Zhou 2006). One trial evaluated the effect of acupuncture combined with hyperbaric oxygen (Cao 2006). Since the control group received routine care only, without hyperbaric oxygen, we could not ascertain whether any treatment effect was due to acupuncture or hyperbaric oxygen. One trial did not assign treatment groups by randomization (Qian 2001). Three trials did not involve neonates (Meng 2003; Peng 2005; Guo 2009), and we were uncertain whether the participants were neonates in one trial (Liu 2006).
Risk of bias in included studies
Since no study was included, risk of bias was not assessed.
Effects of interventions
Since no trial was included in the current review, we could not assess the effects of intervention. We have summarized the findings from five relevant excluded studies (Meng 2003; Peng 2005; Cao 2006; Liu 2006; Guo 2009):
Liu 2006 performed a randomized controlled trial compared needle acupuncture plus hyperbaric oxygen with hyperbaric oxygen alone in 59 children with HIE (33 participants in the intervention group and 26 participants in the control group). The age of the participants at the start of treatment was not reported. This trial reported the number of patients with clinical improvement after treatment and found that there were more patients in the intervention group who showed some clinical improvement compared to the control group. However, there was no significant difference in the frequency of clinically significant improvement between the treatment and the control groups. Adverse effects were not mentioned in the report.
Peng 2005 performed a randomized controlled trial compared injection acupuncture (vitamin B1 and mouse neurotrophic factor) plus intravenous medication (cerebrolysin and citicoline) with intravenous medication alone in 114 infants aged one to two months with HIE (65 participants in the intervention group and 49 participants in the control group). This trial reported the number of patients with cerebral palsy at three, six and 12 months. The frequency of cerebral palsy at three months was not significantly different between the intervention and the control groups. However, participants in the intervention group were less likely to develop cerebral palsy at six months and 12 months. There was no significant difference in the frequency of abnormal posture at three months between the intervention and the control groups. Again adverse effects were not mentioned in the report.
Guo 2009 performed a randomized controlled trial compared injection acupuncture (vitamin B1, B6, B12, citicoline and ganglioside) plus intravenous medication (cerebrolysin and Chinese herb complex (Fu Feng Dan Xin)) with intravenous medication alone in 120 infants aged one to twp months with HIE (64 participants in the intervention group and 52 participants in the control group). This trial reported no significant difference in the frequency of cerebral palsy between the intervention and the control groups at three months. However, participants in the intervention group were less likely to develop cerebral palsy at six months and 12 months. Adverse effects were not mentioned in the report.
Meng 2003 performed a randomized controlled trial compared needle acupuncture plus injection acupuncture (vitamin B1, B12 and citicoline) plus intravenous medication (cerebrolysin and Chinese herb complex (Fu Feng Dan Xin)) with intravenous medication alone in 116 infants aged above one month with HIE (58 participants in the intervention group and 58 participants in the control group). This trial reported the number of patients with cerebral palsy at six and 12 months. The risk of cerebral palsy at six months was not significantly different between the intervention and the control groups. However, participants in the intervention group were less likely to develop cerebral palsy at 12 months. This trial also did not report adverse effects of acupuncture treatment.
Cao 2006 The fifth randomized controlled trial compared acupuncture plus hyperbaric oxygen with supportive care alone in 148 newborns with HIE (83 participants in the intervention group and 65 participants in the control group). The age of the participants at the start of treatment was not reported. This trial reported that patients in the intervention group had significantly higher developmental quotient at three months, six months, 12 months and 18 months. There were significantly fewer children in the intervention group who had neurological disabilities compared to the control group.
Discussion
Summary of main results
No trial satisfied our predefined inclusion criteria. There is currently no randomized controlled trial evaluating the effectiveness of acupuncture for treatment of HIE in neonates. The safety of acupuncture for HIE in neonates is unknown as there is no adequate evidence to assess the safety of acupuncture for HIE in neonates. Acupuncture as an adjunct to other treatments may reduce the risk of cerebral palsy in older infants who survive after HIE but further critical examination of evidence is needed before any conclusion can be made.
Potential biases in the review process
We searched extensively in the international and Chinese literature. Studies that were not published in English or Chinese might have been missed.
Agreements and disagreements with other studies or reviews
As far as we are aware, this is the only systematic review on acupuncture for hypoxic ischemic encephalopathy in neonates.
Authors' conclusions
Implications for practice.
The rationale for acupuncture in neonates with HIE is unclear and the evidence from randomized controlled trial is lacking. Therefore, we do not recommend acupuncture for the treatment of HIE in neonates.
Implications for research.
There are no randomized controlled trial assessing acupuncture for neonatal HIE. The existing trials were performed on older infants with neonatal HIE, or the age of participants was not described or acupuncture was combined with other therapy. Therefore, the effectiveness of acupuncture for HIE in neonates is uncertain. Further high quality randomized controlled trials on acupuncture for HIE in neonates aged below 28 days are needed. The age of the patients at the start of acupuncture therapy should be fully described. Placebo acupuncture should be used in the control group to minimize placebo effect. If acupuncture is to be combined with other therapies, both the intervention and the control arms should receive exactly the same co‐interventions to minimize performance bias. Although co‐interventions included in both the intervention and the control groups would not affect the validity of the trial, it would be best if co‐interventions also have high quality evidence to support their effectiveness on their own. Since there is high quality evidence from randomized controlled trials and a systematic review supporting hypothermia for treatment of neonatal HIE, it is worthwhile to consider comparing acupuncture with hypothermia against placebo or sham acupuncture with hypothermia to assess whether acupuncture as an adjunctive therapy would further enhance the effectiveness of hypothermia. Since sham acupuncture involves penetration of the skin, it is not usually inert. Therefore, trials comparing acupuncture with sham acupuncture might be comparing two active treatments and might not be appropriate for investigation of efficacy of acupuncture.
Although blinding of the therapist applying acupuncture is difficult, blinding of the patients, the other care providers and outcome assessors should be attempted in order to minimize performance and detection biases. Infant mortality should be included as one of the major outcomes. Since HIE is a highly heterogeneous disease with different etiologies and severity, acupuncture may have different effects on different subgroups of patients. Therefore, future clinical trials should focus on a particular subgroup or include a very large sample size to delineate the effect of acupuncture on different types of patients.
Acknowledgements
We thank Ms Yolanda Montagne for searching relevant databases and the Cochrane Neonatal Review Group for their editorial support.
Appendices
Appendix 1. Search strategy for CENTRAL and Cochrane Neonatal Specialized Register
(hypoxic ischemic encephalopathy OR hypoxia ischemia encephalopathy OR hypoxic isch* OR cerebral hypoxic isch* OR encephalopathy ischemic hypoxic OR hypoxia brain OR encephalopathy OR cerebral ischemia OR cerebral hypoxia OR perinatal asphyxia OR perinatal hypoxic ischemic encephalopathy OR perinatal hypoxic ischemia encephalopathy) and (infant OR infan* OR newborn OR newborn* OR new‐born* OR baby OR baby* OR babies OR neonat* OR child OR child* OR boy* OR girl*) and (acupuncture OR acupuncture* OR acupoints OR acupoints* OR electro‐acupuncture OR electro acupuncture OR neuro‐electric therapy OR neuroelectric therapy OR electrostimulation OR laser therapy OR acupressure OR meridian OR meridian* OR alternative medicine)
Appendix 2. Search Strategy for MEDLINE, MEDLINE(R) In‐Process & Other Non‐Indexed Citations, OLDMEDLINE(R), AMED, EMBASE, PubMed, MedlinePlus, PubMed Ahead of Print via Ovid
Brain Ischemia/ or Hypoxia, Brain/ or Hypoxia‐Ischemia, Brain/ or hypoxia ischemia encephalopathy.mp.
encephalopathy ischemic hypoxic.mp.
hypoxia brain.mp.
encephalopathy.mp.
cerebral ischemia.mp.
cerebral hypoxia.mp.
perinatal asphyxia.mp.
perinatal hypoxic ischemic encephalopathy.mp.
perinatal hypoxic ischemia encephalopathy.mp.
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9
(infant or infan*).mp.
(newborn or newborn* or new‐born*).mp.
(baby or baby* or babies).mp.
Infant, Newborn/ or neonat*.mp.
(child or child*).mp.
(boy* or girl*).mp.
11 or 12 or 13 or 14 or 15 or 16
(acupuncture or acupuncture*).mp.
(acupoints or acupoints*).mp.
(electro‐acupuncture or electro acupuncture).mp.
(neuro‐electric therapy or neuroelectric therapy).mp.
Electric Stimulation/ or Electric Stimulation Therapy/ or electrostimulation.mp.
laser therapy.mp. or Laser Therapy/
acupressure.mp. or Acupressure/
(meridian or meridian*).mp.
alternative medicine.mp. or Complementary Therapies/
18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26
10 and 17 and 27
Randomized Controlled Trials as Topic/ or randomi?ed.mp.
randomised controlled trial.mp. or Randomized Controlled Trial/
controlled clinical trial.mp. or Controlled Clinical Trial/
placebo.mp. or Placebos/ or Placebo Effect/
clinical trials.mp. or Clinical Trial/
randomly.mp.
trial.mp. or Randomized Controlled Trial/ or Clinical Trial/
29 or 30 or 31 or 32 or 33 or 34 or 35
28 and 36
Appendix 3. Search Strategy for CINAHL Plus via EBSCO
hypoxic ischemic encephalopathy OR hypoxia ischemia encephalopathy OR hypoxic isch* OR cerebral hypoxic isch* OR encephalopathy ischemic hypoxic OR hypoxia brain OR encephalopathy OR cerebral ischemia OR cerebral hypoxia OR perinatal asphyxia OR perinatal hypoxic ischemic encephalopathy OR perinatal hypoxic ischemia encephalopathy
infant OR infan* OR newborn OR newborn* OR new‐born* OR baby OR baby* OR babies OR neonat* OR child OR child* OR boy* OR girl*
acupuncture OR acupuncture* OR acupoints OR acupoints* OR electro‐acupuncture OR electro acupuncture OR neuro‐electric therapy OR neuroelectric therapy OR electrostimulation OR laser therapy OR acupressure OR meridian OR meridian* OR alternative medicine
randomised Controlled Trial OR randomi?ed OR controlled clinical trial OR placebos OR clinical trials OR randomly OR trial
(1) AND (2) AND (3) and (4)
Appendix 4. Search Strategy for PsycINFO
(hypoxic ischemic encephalopathy OR hypoxia ischemia encephalopathy OR hypoxic isch* OR cerebral hypoxic isch* OR encephalopathy ischemic hypoxic OR hypoxia brain OR encephalopathy OR cerebral ischemia OR cerebral hypoxia OR perinatal asphyxia OR perinatal hypoxic ischemic encephalopathy OR perinatal hypoxic ischemia encephalopathy) and (infant OR infan* OR newborn OR newborn* OR new‐born* OR baby OR baby* OR babies OR neonat* OR child OR child* OR boy* OR girl*) and (acupuncture OR acupuncture* OR acupoints OR acupoints* OR electro‐acupuncture OR electro acupuncture OR neuro‐electric therapy OR neuroelectric therapy OR electrostimulation OR laser therapy OR acupressure OR meridian OR meridian* OR alternative medicine) and (randomised Controlled Trial OR randomi?ed OR controlled clinical trial OR placebos OR clinical trials OR randomly OR trial) NOT (Animal* OR rat* or rabbit*)
Appendix 5. Search strategy for WHO International Clinical Trials Registry Platform (ICTRP)
(hypoxia OR asphyxia OR ischemia OR encephalopathy ) AND (acupuncture OR electroacupuncture OR electro acupuncture OR electro‐acupuncture OR electric stimulation OR electrostimulation OR acupressure OR laser OR neuroelectric OR neuro‐electric OR acupoints OR meridian)
Appendix 6. Search strategy for China Journal Full‐text Database, China Master Theses Full‐text Database, China Doctor Dissertation Full‐text Database, China Proceedings of Conference Database, Wei Pu Information, Wang Fang Data, and Index to Taiwan Periodical Literature System
1. "QueYang"(Anoxia) and "QueXie" (ishemia)
2. "QueYangQueXue" (Hypoxic ischemia) or "QueYangQueXueXingNao Bing" (Hypoxic ischemic encephalopathy)
3. 1 or2
4. "ZhenJiu" (Acupuncture) or "ZhenCi" (Acupuncture) or "DianZhen" (Electro‐acupuncture) or "ZhenYa" (Acupressure) or "ErZhen" (Ear Acupuncture) or "TiZhen" (Body acupuncture) or "SheZhen" (Tongue acupuncture) or "TouPiZhen" (Scalp acupuncture) or "XueWei" (acupoints)
5. "DongWu" (animals) or "Shu" (rat) or "Tu" (rabbit)
6. 3 and 4 not 5
Characteristics of studies
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Cai 2008 | Acupoint massage compared to simple touch. Needle acupuncture was not investigated |
| Cao 2006 | Acupuncture plus hyperbaric oxygen compared to routine care. Cannot evaluate effectiveness of needle acupuncture |
| Chen 2006 | Acupoint massage plus routine care compared to routine care. Needle acupuncture was not investigated |
| Guo 2007 | Acupoint massage plus medications compared to medications. Needle acupuncture was not investigated |
| Guo 2009 | Participants were aged above 1 month and not neonates |
| Li 2003 | Acupoint massage plus routine care compared to routine care. Needle acupuncture was not investigated |
| Li 2008 | Acupoint massage plus routine care compared to routine care. Needle acupuncture was not investigated |
| Liu 2006 | Age of the participants were not reported. It was uncertain whether the participants were neonates |
| Liu 2007 | Acupoint massage plus routine care compared to routine care. Needle acupuncture was not investigated |
| Meng 2003 | Participants were aged above 1 month and not neonates |
| Peng 2005 | Participants were aged 1‐2 months and not neonates |
| Qian 2001 | Non‐randomized trial comparing repeated acupoints massage with single acupoints massage. Needle acupuncture was not investigated |
| Wu 2010 | Acupoint massage plus routine care compared to routine care. Needle acupuncture was not investigated |
| Zhang 2008 | Acupoint massage plus medications compared to medications. Needle acupuncture was not investigated |
| Zhou 2006 | Body massage plus routine care compared to routine care. Needle acupuncture was not investigated |
Characteristics of studies awaiting assessment [ordered by study ID]
Liu 2003.
| Methods | Design: RCT Randomization method: not reported Method of allocation concealment: not reported Blinding method: not reported Stratification: not used |
| Participants | Inclusion: neonates with HIE Exclusion: Nil Number of patients randomized (Treatment: Control): 36: 36 Dropouts (Treatment: Control): 2: 6 Age (Treatment: Control): not reported Number of boys (Treatment: Control): 20: 17 Stage of HIE: Treatment group: moderate (26), severe (10); Control group: moderate (23), severe (9) |
| Interventions | Treatment group: acupuncture + acupressure + conventional supportive care and rehabilitation Acupuncture started at 6 months to 2 years old. Treatment was applied 10‐15 times per month. Use of needles, selection of acupoints and stimulation method were not reported Acupressure to 10 acupoints: Bai‐hui (GV20), Sishencong (EX‐HN1), Yintang (EX‐HN3), Yamen (GV15), Dazhu (BL11), Zusanli (ST36), Yanlingquan (GB34), Xuanzhong (GB39), Quchi (LI11), and Tongli (HT5) Selection of acupoints might be modified according to syndrome differentiation by Traditional Chinese Medicine. Further details were not provided. Treatment was applied daily for 10 days then rest for 7‐10 days (1 course). Total number of courses was not reported Control: conventional supportive care and rehabilitation alone as in treatment group Duration of treatment: not reported |
| Outcomes | Bayley Scales of infant development at 2 years old Frequency of motor developmental delay at 2 years old Frequency of mental retardation at 2 years old Frequency of epilepsy at 2 years old |
| Notes | Await clarification of whether needle acupuncture was used |
Differences between protocol and review
Electronic searches of databases were amended.
We did not search the Trials Register of the Cochrane Complementary Medicine Field as this was incorporated into CENTRAL. We did not search TCMLARS as we lost access to this database. We replaced the search of the Chinese Acupuncture Trials Register, the NCCAM (National Center for Complementary and Alternative Medicine), and NIH (National Institute of Health) Clinical Trials Database by the WHO International Clinical Trials Registry Platform (ICTRP) as the latter would include the former three databases. We added the search of the Index to Taiwan Periodical Literature System, which is the major Chinese Medical database in Taiwan.
Contributions of authors
V Wong: conceiving the review, designing the review; coordinating the review; undertaking searches; screening search results; screening retrieved papers against eligibility criteria; appraising risk of bias in papers; interpretation of data; providing a clinical perspective; writing the protocol; providing general advice on the review; writing the protocol and final review.
DKL Cheuk: designing the review; co‐ordinating the review; designing search strategies; screening retrieved papers against eligibility criteria; appraising risk of bias in papers; extracting data from papers; data management for the review; entering data into Review Manager 5; analysis of data; interpretation of data; providing a methodological perspective; providing a clinical perspective; writing the protocol and final review.
V Chu: co‐ordinating the review; data collection for the review; designing search strategies; undertaking searches; screening search results; organizing retrieval of papers; screening retrieved papers against eligibility criteria; appraising risk of bias in papers; extracting data from papers; data management for the review; entering data into Review Manager 5; writing to authors of papers for additional information; analysis of data; interpretation of data; writing the protocol and final review.
Sources of support
Internal sources
-
Hospital Authority, Hong Kong, Hong Kong.
Funding for development of 'Integration of Chinese Medicine and Western Medicine in Acute Rehabilitation of Traumatic Brain Injury and Other Neurological Disorders'.
The University of Hong Kong, Hong Kong.
External sources
-
Eunice Kennedy Shriver National Institute of Child Health and Human Development National Institutes of Health, Department of Health and Human Services, USA.
Editorial support of the Cochrane Neonatal Review Group has been funded with Federal funds from the Eunice Kennedy Shriver National Institute of Child Health and Human Development National Institutes of Health, Department of Health and Human Services, USA, under Contract No. HHSN275201100016C.
Declarations of interest
No conflict of interest was known.
New
References
References to studies excluded from this review
Cai 2008 {published data only}
- Cai W, Li H, Lu J, Chen X. Effect of touch and acupoint massage on growth and development of children with hypoxic‐ischemic encephalopathy. Journal of Nursing Science 2008;23(9):34‐5. [Google Scholar]
Cao 2006 {published data only}
- Cao W. Effect of acupuncture at early stage on prognosis of the infantile of anoxic and ischemic cerebral injury. Chinese Acupuncture and Moxibustion 2006;26(1):18‐20. [PubMed] [Google Scholar]
Chen 2006 {published data only}
- Chen J, Ping X, Wang H, Jiang S, Lu X. Effects of early touch intervention on neurobehavioral rehabilitation of newborns with hypoxic ischemic encephalopathy. Chinese Journal of Clinical Rehabilitation 2006;10(12):27‐9. [Google Scholar]
- Chen J, Ping X, Wang H, Jiang S, Lu X. Effects of therapeutic touch on the neurobehavioral rehabilitation of newborns with hypoxic‐ischemic encephalopathy. Practical Clinical Medicine 2005;6(9):96‐8. [Google Scholar]
Guo 2007 {published data only}
- Guo X. Observation on effect of touching to treat newborns with neonatal hypoxic ischemic encephalopathy. Chinese Nursing Research 2007;21(6):1635‐6. [Google Scholar]
Guo 2009 {published data only}
- Guo P. Injection of acupoint to reduce incidence of cerebral palsy in neonates with hypoxic ischemic encephalopathy. The Sichuan Journal of Traditional Chinese Medicine 2009;27(1):112‐4. [Google Scholar]
Li 2003 {published data only}
- Li Y, Wang X, Liu Y. Effect of touching and acupoint massage on growth and development of children with hypoxic ischemic encephalopathy. Journal of Nursing Science 2003;18(4):246‐8. [Google Scholar]
Li 2008 {published data only}
- Li J, Feng L, Yan L. Observation on acupoint massage and exercise therapy for neonatal hypoxic ischemic encephalopathy. Chinese Journal of Practical Nervous System Diseases 2008;11(6):139‐40. [Google Scholar]
Liu 2006 {published data only}
- Liu J. Observations on the treatment of hypoxemic infantile encephalopathy with acupuncture plus hyperbaric oxygen. Shanghai Journal of Acupuncture and Moxibustion 2006;25(5):18‐9. [Google Scholar]
Liu 2007 {published data only}
- Liu SM, Shang XM. Research on Jingling Koufuye acupoint massage for neonate with hypoxic ischemic encephalopathy. Chinese Community Doctor 2007;14:73. [Google Scholar]
Meng 2003 {published data only}
- Meng E. Early prevention of cerebral palsy from hypoxic ischemic encephalopathy by scalp acupuncture and acupoint injection. Sichuan Journal of Traditional Chinese Medicine 2003;21(11):92‐3. [Google Scholar]
Peng 2005 {published data only}
- Peng GL, Chen T, Huang ZQ, Zhang JY. Effect of acupoint injection and massage on neonates with hypoxic ischemic encephalopathy. Sichuan Journal of Traditional Chinese Medicine 2005;23(12):103‐4. [Google Scholar]
Qian 2001 {published data only}
- Qian J, Zhou X, Hsu Z, Cheng Y, Li Y. Touching and acupoint massage therapy for neonatal brain injury: observation of 30 cases. Jiangsu Medical Journal 2001;27(8):603‐4. [Google Scholar]
Wu 2010 {published data only}
- Wu Y. Effect of early intervention with acupoint massage on gross motor development of neonatal hypoxic ischemic encephalopathy. Journal of Xinxiang Medical College 2010;27(6):612‐4. [Google Scholar]
Zhang 2008 {published data only}
- Zhang Y, Xu S, Zhang L, Lu J, Xie H. Effects of early massage and touching on intellectual development of children with brain injury. Shandong Medical Journal 2008;48(28):99‐100. [Google Scholar]
Zhou 2006 {published data only}
- Zhou Q. The rehabilitative effects medical massage techniques to promote the recovery of hypoxic‐ischemic brain damage due to perinatal period. Chinese Journal of Obstetrics & Gynecology and Pediatrics 2006;2(4):195‐7. [Google Scholar]
References to studies awaiting assessment
Liu 2003 {published data only}
- Liu XH. Improvement of prognosis of newborn hypoxia‐ischemia encephalopathy by early acupoint stimulation. Journal of New Chinese Medicine 2003;35(9):37‐8. [Google Scholar]
Additional references
Ahn 2005
- Ahn AC, Wu J, Badger GJ, Hammerschlag R, Langevin HM. Electrical impedance along connective tissue planes associated with acupuncture meridians. BMC Complementary and Alternative Medicine 2005;5:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Al‐Waili 2005
- Al‐Waili NS, Butler GJ, Beale J, Abdullah MS, Hamilton RW, Lee BY, et al. Hyperbaric oxygen in the treatment of patients with cerebral stroke, brain trauma, and neurologic disease. Advances in Therapy 2005;22(6):659‐78. [DOI] [PubMed] [Google Scholar]
Alvarez 2011
- Alvarez XA, Cacabelos R, Sampedro C, Couceiro V, Aleixandre M, Vargas M, et al. Combination treatment in Alzheimer's disease: results of a randomized, controlled trial with cerebrolysin and donepezil. Current Alzheimer Research 2011;8(5):583‐91. [DOI] [PubMed] [Google Scholar]
Cabyoglu 2006
- Cabyoglu MT, Ergene N, Tan U. The mechanism of acupuncture and clinical applications. International Journal of Neuroscience 2006;116(2):115‐25. [DOI] [PubMed] [Google Scholar]
Chalak 2007
- Chalak L, Kaiser J. Neonatal guideline hypoxic‐ischemic encephalopathy (HIE). Journal of the Arkansas Medical Society 2007;104(4):87‐9. [PubMed] [Google Scholar]
Cheuk 2006
- Cheuk DK, Wong V. Acupuncture for epilepsy. Cochrane Database of Systematic Reviews 2006, Issue 2. [DOI: 10.1002/14651858.CD005062.pub3] [DOI] [PubMed] [Google Scholar]
Cheuk 2012
- Cheuk DK, Yeung WF, Chung KF, Wong V. Acupuncture for insomnia. Cochrane Database of Systematic Reviews 2012, Issue 9. [DOI: 10.1002/14651858.CD005472.pub3] [DOI] [PubMed] [Google Scholar]
Davalos 2002
- Davalos A, Castillo J, Alvarez‐Sabin J, Secades JJ, Mercadal J, Lopez S, et al. Oral citicoline in acute ischemic stroke: an individual patient data pooling analysis of clinical trials. Stroke 2002;33(12):2850‐7. [DOI] [PubMed] [Google Scholar]
Dung 1984
- Dung HC. Anatomical features which contribute to the formation of acupuncture points. American Journal of Acupuncture 1984;12(2):139‐44. [Google Scholar]
Edwards 2006
- Edwards AD, Azzopardi DV. Therapeutic hypothermia following perinatal asphyxia. Archives of Disease in Childhood. Fetal and Neonatal Edition 2006;91(2):F127‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey‐Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Evan 2001
- Evans DJ, Levene MI. Anticonvulsants for preventing mortality and morbidity in full term newborns with perinatal asphyxia. Cochrane Database of Systematic Reviews 2001, Issue 3. [DOI: 10.1002/14651858.CD001240.pub2] [DOI] [PubMed] [Google Scholar]
Fernandez 1983
- Fernandez RL. Efficacy and safety of oral CDP‐choline. Arzneimittelforschung 1983;33:1073‐80. [PubMed] [Google Scholar]
Fu 2000
- Fu H. What is the material base of acupuncture? The nerves!. Medical Hypotheses 2000;54(3):358‐9. [DOI] [PubMed] [Google Scholar]
Gonzalez 1998
- González ME, Francis L, Castellano O. Antioxidant systemic effect of short‐term cerebrolysin administration. Journal of Neural Transmission 1998;53:333‐41. [DOI] [PubMed] [Google Scholar]
Gonzalez 2006
- Gonzalez FF, Miller SP. Does perinatal asphyxia impair cognitive function without cerebral palsy?. Archives of Disease in Childhood. Fetal and Neonatal Edition 2006;91(6):F454‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guekht 2011
- Guekht AB, Moessler H, Novak PH, Gusev EI. Cerebrolysin in vascular dementia: improvement of clinical outcome in a randomized, double‐blind, placebo‐controlled multicenter trial. Journal of Stroke and Cerebrovascular Disease 2011;20(4):310‐8. [DOI] [PubMed] [Google Scholar]
Hartbauer 2001
- Hartbauer M, Hutter‐Paier B, Skofitsch G, Windisch M. Antiapoptotic effects of the peptidergic drug cerebrolysin on primary cultures of embryonic chick cortical neurons. Journal of Neural Transmission 2001;108(4):459‐73. [DOI] [PubMed] [Google Scholar]
He 2010
- He L, Zhou MK, Zhou D, Wu B, Li N, Kong SY. Acupuncture for Bell's palsy. Cochrane Database of Systematic Reviews 2010, Issue 8. [DOI: 10.1002/14651858.CD002914.pub5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2002
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine 2002;21(11):1539‐58. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. [Google Scholar]
Hurtado 2011
- Hurtado O, Lizasoain I, Moro MÁ. Neuroprotection and recovery: recent data at the bench on citicoline. Stroke 2011;42 Suppl 1:33‐5. [DOI] [PubMed] [Google Scholar]
Jacobs 2007
- Jacobs S, Hunt R, Tarnow‐Mordi W, Inder T, Davis P. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database of Systematic Reviews 2007, Issue 4. [DOI: 10.1002/14651858.CD003311.pub2] [DOI] [PubMed] [Google Scholar]
Ladurner 2005
- Ladurner G, Kalvach P, Moessler H, Cerebrolysin Study Group. Neuroprotective treatment with cerebrolysin in patients with acute stroke: a randomised controlled trial. Journal of Neural Transmission 2005;112(3):415‐28. [DOI] [PubMed] [Google Scholar]
Leach 1998
- Leach RM, Rees PJ, Wilmshurst P. Hyperbaric oxygen therapy. BMJ 1998;317(7166):1140‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 1994
- Liu N. Cerebrolysin treatment of 30 cases of neonatal hypoxic ischemic encephalopathy. Hebei Medical Journal 1994;16(3):148‐9. [Google Scholar]
Liu 2001
- Liu T, Li S, Yao G. Clinical observation on hyperbaric oxygen for treatment of neonatal hypoxic ischemic encephalopathy. Taishan Health Journal 2001;6:19‐20. [Google Scholar]
Lu 2008
- Lu J. Overview of clinical application of acupoint injection. Modern Journal of Integrated Traditional Chinese and Western Medicine 2008;3:345‐7. [Google Scholar]
Lund 2006
- Lund I, Lundeberg T. Are minimal, superficial or sham acupuncture procedures acceptable as inert placebo controls?. Acupuncture Medicine 2006;24(1):13‐5. [DOI] [PubMed] [Google Scholar]
MacPherson 2001
- MacPherson H, Thomas K, Walters S, Fitter M. The York acupuncture safety study: prospective survey of 34 000 treatments by traditional acupuncturists. BMJ 2001;323:486‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maksimova 2009
- Maksimova MIu, Briukhov VV, Timerbaeva SL, Kistenev BA, Rebrova OIu, Suslina ZA. Effectiveness of cerebrolysin in hypertensive supratentorial intracranial hemorrhages: results of a randomized triple blind placebo‐controlled study. Zhurnal Nevrologii I Psikhiatrii Imeni S.S. Korsakova 2009;109(1):20‐6. [PubMed] [Google Scholar]
Melchart 2009
- Melchart D, Linde K, Fischer P, Berman B, White A, Vickers A, et al. Acupuncture for idiopathic headache. Cochrane Database of Systematic Reviews 2009, Issue 1. [DOI: 10.1002/14651858.CD001218] [DOI] [PubMed] [Google Scholar]
Ni 2003
- Ni F, Lin J, Zhou C, Yao X, Wu X. Study on mechanisms of acupoint injection therapy. Chinese Acupuncture & Moxibustion 2003;23(10):609‐11. [Google Scholar]
NIH Consensus 1998
- NIH Concensus Development Panel of Acupuncture. Acupuncture. JAMA 1998;280(17):1518‐24. [PubMed] [Google Scholar]
Perlman 2006
- Perlman JM. Intervention strategies for neonatal hypoxic‐ischemic cerebral injury. Clinical Therapeutics 2006;28(9):1353‐65. [DOI] [PubMed] [Google Scholar]
Sarnat 1976
- Sarnat HB, Sarnat MS. Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Archives of Neurology 1976;33(10):696‐705. [DOI] [PubMed] [Google Scholar]
Satou 2000
- Satou T, Itoh T, Tamai Y, Ohde H, Anderson AJ, Hashimoto S. Neurotrophic effects of FPF‐1070 (cerebrolysin) on cultured neurons from chicken embryo dorsal root ganglia, ciliary ganglia, and sympathetic trunks. Journal of Neural Transmission 2000;107(11):1253‐62. [DOI] [PubMed] [Google Scholar]
SCSSS 1999
- Swedish Collaboration on Sensory Stimulation in Stroke (SCSSS). Sensory stimulation after stroke: a randomized controlled trial. Cerebrovascular Disease 1999;9 Suppl 1:28. [Google Scholar]
Shupak 2008
- Shupak A, Gilbey P. Effects of pressure. In: Neuman T, Thom S editor(s). Physiology and medicine of hyperbaric oxygen therapy. 1st Edition. Philadelphia: Saunders Elsevier, 2008:513‐26. [Google Scholar]
Skvortsova 2004
- Skvortsova VI, Stakhovskaia LV, Gubskiĭ LV, Shamalov NA, Tikhonova IV, Smychkov AS. A randomized, double‐blind, placebo‐controlled study of Cerebrolysin safety and efficacy in the treatment of acute ischemic stroke. Zhurnal Nevrologii I Psikhiatrii Imeni S.S. Korsakova 2004;Suppl 11:51‐5. [PubMed] [Google Scholar]
Streitberger 1998
- Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet 1998;352(9125):364‐5. [DOI] [PubMed] [Google Scholar]
Tatebayashi 2003
- Tatebayashi Y, Lee MH, Li L, Iqbal K, Grundke‐Iqbal I. The dentate gyrus neurogenesis. A therapeutic target for Alzheimer's disease. Acta Neuropathologica 2003;105(3):225‐32. [DOI] [PubMed] [Google Scholar]
Tazaki 1988
- Tazaki Y, Sakai F, Otomo E, Kutsuzawa T, Kameyama M, Omae T, et al. Treatment of acute cerebral infarction with a choline precursor in a multicenter double‐blind placebo‐controlled study. Stroke 1988;19(2):211‐6. [DOI] [PubMed] [Google Scholar]
Tian 2007
- Tian X, Gao H. Citicoline for treatment of neonatal hypoxic ischemic encephalopathy. Journal of Yanan University (Medical Sciences) 2007;5(4):62. [Google Scholar]
Vannucci 1990
- Vannucci RC. Current and potentially new management strategies for perinatal hypoxic‐ischemic encephalopathy. Pediatrics 1990;85(6):961‐8. [PubMed] [Google Scholar]
Veinbergs 2000
- Veinbergs I, Mante M, Mallory M, Masliah E. Neurotrophic effects of cerebrolysin in animal models of excitotoxicity. Journal of Neural Transmission 2000;59:273‐80. [DOI] [PubMed] [Google Scholar]
Vickers 1999
- Vickers A, Zollman C. ABC of complementary medicine. Acupuncture. BMJ 1999;319(7215):973‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 1999
- Wang M, Zhang S, Yang S. Hyperbaric oxygen for treatment of neonatal hypoxic ischemic encephalopathy: report of 23 cases. Ningxia Medical Journal 1999;2:52‐3. [Google Scholar]
Wang 2011
- Wang J. The neurobehavioral effect of citicoline on hypoxic ischemic encephalopathy in neonate. China Medical Herald 2011;8(18):51‐2. [Google Scholar]
White 2001
- White A, Hayhoe S, Hart A, Ernst E. Adverse events following acupuncture: prospective survey of 32 000 consultations with doctors and physiotherapists. BMJ 2001;323(7311):485‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wong 2010
- Wong FW, Lim CE, Smith W. A new bioimpedance research device (BIRD) for measuring the electrical impedance of acupuncture meridians. Journal of Alternative and Complementary Medicine 2010;16(3):257‐64. [DOI] [PubMed] [Google Scholar]
Wu 2008
- Wu HM, Tang JL, Lin XP, Lau J, Leung PC, Woo J, Li YP. Acupuncture for stroke rehabilitation. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD004131.pub2] [DOI] [PubMed] [Google Scholar]
Zhang 2008a
- Zhang SH, Liu M, Asplund K, Li L. Acupuncture for acute stroke. Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD003317.pub2] [DOI] [PubMed] [Google Scholar]
Zhang 2010
- Zhang H. Combined naloxone and cerebrolysin for treatment of 60 cases of neonatal hypoxic ischemic encephalopathy. Journal of Zhengzhou University (Medical Sciences) 2010;45(4):686‐7. [Google Scholar]


