Abstract
Male partner involvement is an important factor in prevention of mother-to-child transmission (PMTCT). Yet, poor conceptualization has hindered optimal assessment of male involvement. We created and evaluated a brief 10-item male partner involvement scale using principal components analysis and scree plots, Cronbach’s alpha, and linear regression with survey data from postpartum women with HIV (n = 200) in Kenya. The scale had a two-factor structure: male encouragement/reminders and active participation. The overall scale and the encouragement/reminders sub-scale displayed strong internal reliability. In the multivariable models, the scales were positively associated with constructive relationship dynamics, HIV status disclosure, and couple HIV testing and counseling, and negatively associated with internalized HIV stigma. The encouragements/reminders sub-scale was also negatively associated with a new HIV diagnosis during pregnancy. This work furthers the conceptualization of male partner involvement in PMTCT and provides a valid measure to assess male involvement as a pathway to better PMTCT outcomes.
Keywords: PMTCT, Pregnant and postpartum women with HIV, Peripartum women with HIV, Male partner involvement, Sub-Saharan Africa, Scale development
Introduction
Male partner involvement in prevention of mother-to-child transmission (PMTCT) is increasingly recognized as a critical aspect of adherence and engagement across the continuum of HIV care for mother-baby pairs. For optimal health outcomes in low-resource settings, numerous steps in the PMTCT continuum need to occur [1], beginning with all pregnant women attending antenatal care (ANC) and testing for HIV. Pregnant women testing HIV-positive should then be linked to HIV care and immediately initiate lifelong antiretroviral therapy (ART). Further, postpartum women with HIV should practice safe infant feeding (i.e. exclusive breastfeeding to 6 months and continued breastfeeding to at least 12 months), as well as stay engaged in HIV care and adhere to ART long-term. Finally, detection of an infant’s HIV status is also a critical step through HIV testing across the postpartum/breastfeeding period. A meta-analysis of PMTCT uptake in sub-Saharan Africa (SSA) recently indicated that ART use during pregnancy improved if male partners were involved [2]. Similarly, Aluisio et al. found that infant HIV acquisition and mortality were lower when male partners were invited by their pregnant female partners with HIV to attend ANC visits [3]. Relatedly, studies have found that low levels of male partner involvement deter pregnant women from engaging in PMTCT-related activities [4, 5]. Additional research further indicates that pregnant women who lack support from their male partners are less likely to accept HIV testing [6], initiate ART [7, 8], deliver in a health facility [9], or adhere to recommended HIV care [10].
Despite increasing appreciation for the role of male partners, there is currently no accepted standard definition of male partner involvement in PMTCT. A recent systematic review by Takah et al. revealed that individual studies use a wide range of definitions to measure male partner involvement in various PMTCT-related activities; the most common definition, however, is male attendance at ANC and/or male participation in HIV counseling and testing [11]. Prior studies have recognized the inadequacy of such single indicators as ANC attendance as a measure of male partner involvement, given that it may be interpreted, for example, as the male partner simply escorting the woman to the clinic and waiting outside, without any meaningful participation in PMTCT [12]. Studies have also attempted to define male partner involvement as status disclosure within the couple [13, 14] or financial support [15]. Male partner involvement in reality likely includes many more nuanced elements that are neglected in existing quantitative research—possibly due to the difficulty in measuring these behaviors.
Two research groups have previously used ad hoc indices to gauge the level of male partner involvement in PMTCT in sub-Saharan African settings. However, these indices have several notable limitations [16]. In 2010, Byamugisha et al. developed a 6-item male involvement index, which has been used in Uganda [17] and South Africa [18] with male participants. This index includes aspects about numerous male partner behaviors (e.g., ANC attendance and support), but is exclusively focused on the antenatal/pregnancy time period, which is only the beginning of critical PMTCT interventions for mother-baby pairs. Byamugisha also do not provide details on the reliability or validity of their index. Peltzer et al. have additionally used a 6-item index to measure male involvement in PMTCT with pregnant and postpartum women in South Africa [19]. Unfortunately, they also do not detail the rationale for item selection or the reliability or validity of the index.
Poor conceptualization and measurement of male partner involvement has hindered meaningful assessment of the influence of male partners across the PMTCT continuum of care [11, 16, 20]. Further study into the complexities of male partner involvement in PMTCT is required in order to successfully leverage male partners to help achieve the elimination of mother-to-child transmission and reduce HIV-related maternal and infant morbidity and mortality [20]. Consequently, the aim of this study was to develop and validate a novel scale measuring male partner involvement in the PMTCT continuum of care in a high HIV-prevalence setting (> 15% adult rate) of Kenya [21]. Using self-reported data from a cross-sectional survey with postpartum women living with HIV in southwestern Kenya, we established the internal reliability and construct validity of a brief 10-item male partner involvement scale and two sub-scales capturing distinct aspects of male partner involvement in PMTCT.
Methods
Study Design
This study was a sub-study within the Mother-Infant Visit Adherence and Treatment Engagement (MOTIVATE!) parent study (R01HD0808477; Clinicaltrials.gov#; PIs: Abuogi and Turan). Details of the parent study have been published elsewhere [22]. In brief, MOTIVATE! is a two-by-two factorial design cluster randomized trial, testing the individual and combined effects of two interventions to promote PMTCT adherence and retention in care: community mentor mothers and mobile phone text messages. Over 1000 pregnant women were enrolled in MOTIVATE! from 24 clinical sites within Kisumu, Migori, and Homabay counties in southwestern Kenya. The present sub-study used a convergent parallel mixed methods design [23]. Here, we report on data collected through the quantitative cross-sectional survey portion of the sub-study, which was administered to 200 women with HIV who were enrolled in the parent study, on ART, and at least 12 months postpartum. Data were collected from May to September 2017. The rationale for surveying women at 12 months postpartum was to prevent potential influence on the parent study outcomes. In this paper we describe the preliminary validation of a novel male partner involvement scale, including conceptualization and item development; survey implementation; scale validation; and regression analysis. We used Stata 14 for all statistical analysis [24].
Conceptualization and Item Development
Questions regarding male partner involvement on the survey, which constitute the male partner involvement scale, were developed by the research team through a multi-phase process. First, we conducted a review of key literature on male partner involvement in PMTCT. Based on this review, we developed a pool of potential questions on this concept based on previous measures of male partner involvement in the literature [11, 13, 25, 26]. These measures were also informed by themes from our team’s qualitative work with postpartum women living with HIV and their perceptions and experiences of male partner involvement [27]. After consultation with experts in the field, who established the face validity of scale items, we narrowed the pool of items to 10 questions, and pilot tested the entire survey with 10 participants in western Kenya. Pilot testing included consultation with local researchers regarding the cultural appropriateness of the scale, correctness of translations, and participant comprehension. We subsequently revised the scale and implemented the final version of the survey with 200 participants.
The final 10-item male partner involvement scale asks female participants (postpartum women living with HIV) how frequently in the last year/during their last pregnancy their male partner engaged in 10 specific behaviors related to the PMTCT continuum of care: (1) attendance at health care visits during pregnancy or postpartum; (2) encouraging a facility delivery; (3) reminders to take HIV medication; (4) reminders to go for HIV or PMTCT care; (5) giving transport money to go to the clinic/dispensary; (6) reminders to give infant prophylaxis; (7) help giving infant prophylaxis; (8) collecting HIV medication for the woman or infant; (9) encouraging specific infant feeding behaviors; and (10) encouraging infant HIV testing (specific questions are listed in Table 1). A 6-point unidirectional Likert scale captured participant responses (5 = all of the time, 4 = most of the time, 3 = more often than not, 2 = occasionally, 1 = rarely, 0 = never) for each item on the scale.
Table 1.
Results of principal components factor analysis
| Items | Factor loadingsa |
|---|---|
| In the past year, how often has your main romantic partner…b | |
| Encouragement/reminders | |
| Encouraged you to delivery/give birth at a clinic? | 0.77 |
| Reminded you to take your HIV medication? | 0.86 |
| Reminded you to go for HIV or PMTCT care? | 0.85 |
| Reminded you to give HIV prophylaxis medication to the baby? | 0.85 |
| Encouraged you to feed the baby in a certain way? | 0.74 |
| Encouraged you take the baby for HIV testing? | 0.66 |
| Gave you transport money to go to the clinic or dispensary? | 0.47 |
| Active participation | |
| Come with you to health care visits (ANC, PMTCT, or postnatal/well-child care)? | 0.76 |
| Helped give HIV prophylaxis medication to the baby? | 0.59 |
| Collected medication for you or the baby from the clinic/dispensary? | 0.80 |
After orthogonal rotation
Response choices: 5 = all of the time, 4 = most of the time, 3 = more often than not, 2 = occasionally, 1 = rarely, 0 = never
Survey Implementation
We recruited postpartum women living with HIV to participant in the survey from each of the four MOTIVATE! intervention trial arms (community mentor mothers only, text messages only, both interventions, and control) from the 24 clinic locations. Study coordinators determined eligibility for the sub-study (i.e., 12 months postpartum and currently enrolled in MOTIVATE!) and contacted eligible women via cell phone or during routine care visits. Eligible women were invited to participate in the survey at one of the clinics at a convenient time of their choosing. The survey was verbally administered in-person by gender-matched research assistants in the participant’s preferred language (Luo, Swahili, or English) on tablets using the REDCap mobile application [28]. The survey modules included male partner involvement in PMTCT activities (scale items); measures of sociodemographic characteristics for the woman and her male partner; depression; stigma; self-reported PMTCT adherence; couple relationship dynamics with male partners; and MOTIVATE! intervention experiences and perceptions. The questions on the survey represented a combination of validated scales, as well as measures created by the research team based on their prior research experience in this setting and expertise. Completed survey data were stored on a secure REDCap server at the University of Colorado and exported into Stata 14 for analysis. Participants were paid a small travel reimbursement.
Scale Validation
First, we created an overall scale score for each participant on the 10-item male partner involvement scale. This was done by averaging the frequency of each male partner involvement item into an overall score, with each item given equal weight. The higher the score on the male partner involvement scale, the more involved male partners were in PMTCT activities. Next, we explored the internal reliability and the construct validity of the newly developed male partner involvement scale.
Through principal components factor analysis, we explored the variance in our sample and underlying latent factors in the scale. We used two approaches to evaluate the number of latent factors: Kaiser-Guttman criterion and Catell’s scree plot [29, 30]. First, we applied Kaiser-Guttman criterion of retaining eigenvalues of greater than one [29], which resulted in two latent factors. Catell’s scree plot provided a visual analysis of the number of latent factors contributing to variance in our sample [30], which also indicated two factors prior to an elbow. On the basis of these analyses, we concluded that our scale had a two-factor structure. We subsequently applied orthogonal rotation to produce distinct and uncorrelated factors. We examined another scree plot after orthogonal rotation, which confirmed the two-factor structure, with all 10-items loading greater than 0.40 on the first two factors. Lastly, we conducted a post-factor estimation to measure sampling adequacy using Kaiser–Mayer Olkin test, which resulted in a robust score of 0.90 [31].
We labeled the first factor “encouragement/reminders” because it includes seven items related to encouragement of PMTCT (e.g., facility delivery, specific infant feeding, and infant HIV testing), reminders regarding maternal ART, HIV care, and infant prophylaxis, and providing transport money to go to the clinic. We labeled the second factor “active participation” because it includes three male active behaviors, including attending health care appointments (ANC/PMTCT), collecting medication for the woman or infant, and giving the infant HIV prophylaxis. We followed Comrey and Lee’s guidelines for selecting items for factor loadings and omitting those with factor loadings of less than 0.40 [32]—which, in this instance, did not apply to any of the items (see Table 1).
We subsequently conducted internal reliability testing of the scale, seeking the highest Cronbach’s alpha possible [30]. All of the original 10 items either contributed substantially to the Cronbach’s alpha for the overall scale or to one of the sub-scales and were thus retained. The alpha (0.90) for the overall male partner involvement scale indicates strong internal reliability. We additionally found evidence of strong internal reliability for the 7-item encouragement/reminders sub-scale (alpha = 0.90) and modest reliability for the 3-item active participation sub-scale (alpha = 0.70). Next, we examined pairwise correlations between the overall male partner involvement scale, the encouragement/reminders sub-scale, and the active participation sub-scale (Table 2). Pairwise correlation indicates low-moderate correlation between the two sub-scales, suggesting that these are likely unique dimensions of male partner involvement.
Table 2.
Pairwise correlation coefficients between the overall male partner involvement scale and two sub-scales
| Dimension | Overall scale | Encouragement/remind- ers sub-scale |
Active participation sub-scale |
|---|---|---|---|
| Overall scale | 1.00 | ||
| Encouragement/reminders sub-scale | 0.95* | 1.00 | |
| Active participation sub-scale | 0.80* | 0.56* | 1.00 |
p < 0.05
Finally, we explored the construct validity of the overall male partner involvement scale and two sub-scales by examining associations with key measures of couple relationship dynamics and health behaviors that would theoretically be associated with male partner involvement based on extant literature [16, 17, 33-35]. This included constructive relationship dynamics, such as more positive interactions with the male partner and relationship satisfaction, as well as couple-level HIV-related health behaviors (discussed in detail below).
Simple and Multivariable Regression Analysis
Simple and multivariable linear regression analysis using ordinary least-squares (OLS) was used to establish construct validity of the overall scale and sub-scales. We examined specific individual and relationship-level characteristics potentially associated with the overall male partner involvement scale and two sub-scales. We used listwise deletion (complete-case analysis) for any missing data (< 10% on all key variables). Independent variables significantly associated with the male partner involvement scales in the simple analysis (p < 0.05) were included in the multivariable analysis. Beta coefficients represent the mean difference in scale scores between the various individual and couple-level predictor variables.
Individual demographic measures included: age, highest education level, parity, age of the index child (i.e., the child born approximately 1 year ago), and when the woman was diagnosed with HIV (either before or after enrollment in the parent study). Socioeconomic status was captured on the survey through two individual questions asking about (1) electricity in the home and (2) food insecurity within the past 4 weeks. Participants who reported a current relationship with a male partner (N = 180; 92%) also answered a series of questions about their male partners, including his age, education, employment status, HIV status (positive, negative, or unknown), whether he is the father of the index child, length of the relationship, and cohabitation and marital status. Participants also provided information on important couple-level HIV-related health behaviors, including women’s HIV status disclosure to the male partner and participation in couple HIV testing and counseling (CHTC). Lastly, participants completed several additional modules using established scales, including internalized HIV stigma (Cronbach’s alpha = 0.80 in this sample) and depression (Cronbach’s alpha = 0.72), as well as relationship dynamics with their current male partner, including relationship satisfaction (Cronbach’s alpha = 0.95) and positive/negative interactions (Cronbach’s alpha = 0.82), which are described in Table 3.
Table 3.
Details of key independent measures
| Scale/measure | Source |
|---|---|
| Internalized/self-stigma (six-items) | Modified version of the people living with HIV Stigma Index [46] |
| Major depression (binary—a score of > 10 indicates major depression) | Patient Health Questionnaire Depression Scale (PHQ-8) [47, 48] |
| Relationship satisfaction scale (five-items) | Investment Model Scale (satisfaction level facet) [49] |
| Positive and negative interactions with the male partner scale (11-items)— negative items reverse codeda | Adapted from previous measures of affective support [50, 51] |
A higher score indicates more positive interactions
Results
Sample Characteristics
Table 4 displays the descriptive findings from the 180 female survey participants who reported having a current male partner at the time of the survey. The mean age of these participants was 28 years (sd 5.1) with 101 (56%) reporting completion of primary education. Participants reported 4 pregnancies on average (sd 1.7) with the index child being, on average, 13 months of age (sd 1.7). Forty-six participants (26%) met the criteria for major depression. Levels of internalized stigma were also high (mean scale score of 9.1; sd 3.8). For example, 46 participants (26%) reported having low self-esteem sometimes or often because of their HIV status. The sample was also of relatively low socioeconomic status, as evidenced by only 36 participants (20%) reporting electricity in their home and 31 participants (17%) experiencing food insecurity (i.e., having no food to eat because the household could not afford to buy food) often or sometimes in the past month.
Table 4.
Descriptive findings from survey participants
| Variable | Na | Descriptive statistic |
|---|---|---|
| Total sample size (female participants with a male partner) | 180 | 100% |
| Individual characteristics | ||
| Woman’s age (years): mean (standard deviation (sd)) | 180 | 28.4 (5.1) |
| Completed primary school (yes): % (n) | 180 | 56.1% (101) |
| No. times pregnant: mean (sd) | 180 | 3.9 (1.7) |
| Age of index child (months): mean (sd) | 180 | 12.7 (1.7) |
| Major depression (yes): % (n) | 180 | 25.6% (46) |
| Newly diagnosed HIV positive (yes): % (n)b | 178 | 43.8% (78) |
| Internalized HIV stigma scale score: mean (sd)c | 171 | 9.1 (3.8) |
| Household economics | ||
| Electricity in the home (yes): % (n) | 179 | 20.1% (36) |
| Food insecurity past 4 weeks (often/sometimes)d | 180 | 17.2% (31) |
| Male partner characteristics | ||
| Age of male partner: mean (sd) | 173 | 36.3 (9.1) |
| Male partner completed primary school (yes): % (n) | 175 | 68.6% (120) |
| Male partner unemployed (yes): % (n) | 180 | 6.0% (12) |
| Male partner HIV status | 180 | |
| Positive (yes): % (n) | 58.9% (106) | |
| Negative (yes): % (n) | 27.2% (49) | |
| Unknown (yes): % (n) | 13.9% (25) | |
| Father of index child (yes): % (n) | 179 | 97.8% (175) |
| Relationship dynamics | ||
| Relationship length with male partner | 175 | |
| < 6 years: % (n) | 38.3% (67) | |
| 6–10 years: % (n) | 33.7% (59) | |
| > 10 years: % (n) | 28.0% (49) | |
| Cohabitating with male partner (yes): % (n) | 179 | 82.7% (148) |
| Married (yes): % (n) | 178 | 91.0% (162) |
| Polygamous relationship (yes): % (n) | 158 | 41.8% (66) |
| Relationship satisfaction scale score: mean (sd)e | 162 | 13.1 (5.8) |
| Interactions with male partner scale score: mean (sd)f | 178 | 19.8 (9.3) |
| Couple HIV-related behaviors | ||
| Disclosed HIV status to male partner (yes): % (n) | 179 | 95.5% (171) |
| Ever tested for HIV as a couple (yes): % (n) | 179 | 51.4% (92) |
Denominator used
Reference group: women known to be living with HIV at the time of parent study recruitment
Range 6–24
Reference group: never/rarely
Range 0–25
Range 0–55 (negative items, reverse coded)
Male partners were, on average, older than the female respondents, with a mean age of 36 years (sd 9.1). Male partners also had higher educational achievement with 120 partners (69%) completing primary education. Male employment was high with only 12 women (6%) reporting their male partner was unemployed. The most common relationship duration with male partners reported by 67 participants (38%) was a duration of less than 6 years. The vast majority of participants reported cohabitating with the male partner and being married: 148 reported cohabiting (83%) and 162 reported being married (91%). Sixty-six participants (42%) also reported being in a polygamous marriage where the husband had other wives. Levels of relationship satisfaction were relatively high with the majority of participants reporting they agree completely/almost completely/mostly with all five measures on the relationship satisfaction scale (mean score of 13.1; sd 5.8). For instance, 106 participants (59%) agreed completely/almost completely/mostly that they “feel satisfied with the relationship.” Similarly, participants reported high levels of positive interactions with the male partner. For example, 121 participants (67%) reported their male partner makes them feel valued/important all the time/most of the time/more often than not. Simultaneously, however, twenty-one participants (12%) reported that their partner physically hurts them more often than not/most of the time/all of the time during disagreements; and 25 participants (14%) reported their partner says cruel/angry things all the time/most of the time/more often than not during disagreements (compared to occasionally/rarely/never).
The majority, 106 couples (59%), were HIV sero-concordant (according to the female partner’s self-report) with the male partner also living with HIV, while 49 women (27%) reported their male partner is HIV-negative, and 25 (14%) did not know their male partner’s HIV status. The vast majority, 171 participants (96%), reported disclosing their positive HIV status to the male partner. Finally, 92 participants (51%) reported participating in CHTC with the male partner.
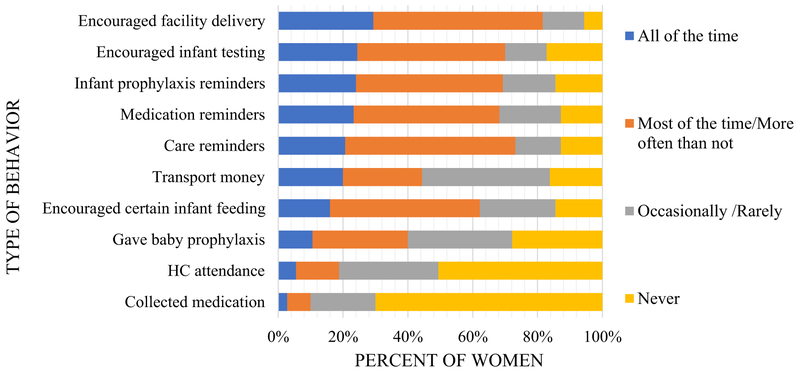
Frequency of Specific Forms of Male Partner Involvement
Figure 1 presents the frequency of the 10 specific male partner behaviors assessed for inclusion in the male partner involvement scale, as reported by female participants on the survey. The most commonly reported form of male partner involvement was encouraging a facility delivery: 53 participants (29%) reported that their male partner engaged in this behavior all of the time, and 95 participants (52%) reported that their male partner engaged in this behavior most of the time/more often than not. The majority of women also reported that their male partner engaged in the following behaviors all of the time/most of the time/more often than not (compared to occasionally/rarely/never): 126 (70%) encouraged infant HIV testing; 124 (69%) reminded women to give the infant HIV prophylaxis; 123 (68%) reminded women to take their HIV medication; 131 (73%) reminded women to go for HIV or PMTCT care; and 112 (62%) encouraged specific infant feeding practices. Nearly half (49%; n = 91) of male partners attended a healthcare visit with the woman in the past year and 34 (19%) attended healthcare visits with the female partner all of the time/most of the time/more often than. The least reported male partner involvement behavior was collecting medication from the clinic/dispensary: 126 (70%) of women reported their male partner never engaged in this behavior.
Fig. 1.
Frequency of male partner involvement in PMTCT as reported by postpartum women living with HIV
Other Forms of Male Partner Involvement
In addition to the 10 closed-ended pre-defined questions from the survey, discussed above, some female participants provided additional information through an open-ended question about other types of supportive male partner behaviors. The most commonly mentioned other types of involvement were: 10 participants (5%) reported the male partner provided food/nutrition; 6 (3%) reported the male partner gave the woman her medication; 3 (2%) reported the male partner reminded women when to take ART or how to “take medicine in the right way.” Three participants (2%) also stated that the male partner helped by “giving food and medicine.” These responses highlight the perceived connection between male partner support, nutrition, and taking ART among peripartum women with HIV.
Scale Scoring
Scores on the overall male partner involvement scale were concentrated in the middle to high range and averaged 2.9 (see Table 5). Scores on the encouragement/reminders sub-scale were even higher with an average of 3.2. For the active participation sub-scale, however, scores were concentrated on the low end of the scale with a mean of only 1.4. The most variability was also seen in the active participation sub-scale.
Table 5.
Overall scale and sub-scale scores
| Scale/items | N | Range | Mean (SD) |
|---|---|---|---|
| Overall male partner involvement scale (9 items) | 178 | 0.78–4.78 | 2.90 (0.96) |
| Encouragement/reminders sub-scale (6 items) | 178 | 1.00–5.00 | 3.17 (0.95) |
| Active participation sub-scale (3 items) | 180 | 0.00–4.66 | 1.40 (1.21) |
Construct Validity
In the simple linear regression models (see Table 6), the following participant characteristics were significantly associated with a lower score on the overall male partner involvement scale: number of pregnancies (B = − 0.10; p < 0.01); major depression (B = − 0.51; p < 0.01); and internalized stigma (B = − 0.08; p < 0.001). Conversely, higher economic status (i.e., having electricity in the home) was associated with a higher score on the overall male partner involvement scale (B = 0.42; p < 0.05). The following factors were associated with a lower score on the encouragement/reminders sub-scale in the simple models: number of pregnancies (B = − 0.09; p < 0.05); major depression (B = − 0.54; p < 0.01); internalized stigma (B = − 0.07; p < 0.01); and being newly diagnosed with HIV (B = − 0.38; p < 0.05). Having electricity in the home was also associated with a higher score on the encouragement/reminders sub-scale (B = 0.55; p < 0.01). For the active participation sub-scale, three individual characteristics were associated with a lower score in the simple models: number of pregnancies (B = − 0.12; p < 0.05); major depression (B = − 0.46; p < 0.05); and internalized stigma (B = − 0.09; p < 0.001).
Table 6.
Simple and multivariable regression results
| Overall male partner involvement scale |
Encouragement/reminders Sub-scale |
Active participation sub-scale |
||||
|---|---|---|---|---|---|---|
| Variable | Simple model: beta coef- ficient (95% CI) (N = 178) |
Multivariable model: beta coefficient (95% CI) (N = 124) |
Simple model: beta coef- ficient (95% CI) (N = 178) |
Multivariable model: beta coefficient (95% CI) (N = 124) |
Simple model: beta coef- ficient (95% CI) (N = 178) |
Multivariable model: beta coefficient (95% CI) (N = 141) |
| Female participant demographics | ||||||
| Woman’s age | −0.03 (−0.06 to 0.00) | – | −0.02 (−0.05 to 0.01) | – | −0.03 (−0.07 to 0.00) | – |
| Completed primary school (yes) | 0.12 (−0.16 to 0.39) | – | 0.12 (−0.17 to 0.40) | – | 0.11 (−0.25 to 0.47) | – |
| No. times pregnant | −0.10** (−0.18 to −0.02) | −0.03 (−0.09 to 0.03) | −0.09* (−0.17 to 0.01) | −0.04 (−0.10 to 0.03) | −0.12* (−0.22 to −0.02) | −0.06 (−0.17 to 0.05) |
| Major depression (yes) | −0.51** (−0.82 to −0.21) | −0.15 (−0.42 to 0.13) | −0.54** (−0.85 to −0.22) | −0.21 (−0.48 to 0.05) | −0.46* −0.86 to −0.06 | −0.16 (−0.62 to 0.29) |
| Newly diagnosed HIV positive (yes) | −0.26 (−0.61 to 0.10) | – | −0.38* (−0.75 to −0.01) | −0.27* (−0.53 to −0.01) | 0.00 (−0.46 to 0.46) | – |
| Internalized stigma score | −0.08*** (−0.11 to −0.04) | −0.03* (−0.07 to −0.00) | −0.07** (−0.10 to −0.03) | −0.02 (−0.05 to 0.01) | −0.09*** (−0.14 to −0.04) | −0.04 (−0.10 to 0.01) |
| Household economics | ||||||
| Electricity in the home (yes) | 0.42* (0.08 to 0.76) | 0.08 (−0.20 to 0.35) | 0.55** (0.20 to 0.90) | 0.23 (−0.03 to 0.49) | 0.08 (−0.37 to 0.53) | – |
| Food insecurity past month (yes) | 0.05 (−0.31 to 0.41 | – | 0.13 (−0.24 to 0.51) | – | −0.14 (−0.61 to 0.33) | – |
| Male partner demographics | ||||||
| Age of male partner (mean) | −0.01 (−0.03 to 0.01) | – | −0.01 (−0.03 to 0.01) | – | −0.01 (−0.03 to 0.01) | – |
| Male partner completed primary school (yes) | 0.08 (−0.22 to 0.39) | – | 0.21 (−0.10 to 0.53) | – | −0.21 (−0.60 to 0.18) | – |
| Male partner unemployed (yes) | −0.40 (−0.97 to 0.17) | – | −0.40 (−0.96 to 0.22) | – | −0.55 (−1.26 to 0.16) | – |
| Male partner HIV status | ||||||
| Positive (yes) | Ref | – | Ref | – | Ref | – |
| Negative (yes) | 0.00 (−0.30 to 0.30) | – | −0.06 (−0.37 to 0.24) | – | 0.12 (−0.28 to 0.53) | – |
| Unknown (yes) | −0.98*** (−1.36 to −0.60) | −0.03 (−0.41 to 0.34) | −1.12*** (−1.51 to −0.74) | −0.08 (−0.44 to 0.29) | −0.64* (−1.16 to 0.11) | 0.03 (−0.67 to 0.72) |
| Father of index child (yes) | 0.18 (−0.90 to 1.25) | – | 0.14 (−0.97 to 1.24) | – | 0.55 (−0.66 to 1.75) | |
| Relationship dynamics | ||||||
| Relationship length with male partner (years) | ||||||
| > 6 | Ref | – | Ref | – | Ref | – |
| 6–10 | 0.07 (−0.26 to 0.39) | – | 0.03 (−0.30 to 0.36) | – | 0.14 (−0.29 to 0.57) | – |
| > 10 | −0.06 (−0.40 to 0.28) | – | −0.15 (−0.50 to 0.19) | – | 0.15 (−0.30 to 0.60) | – |
| Cohabitating with male partner (yes) | 0.51** (0.15 to 0.87) | 0.12 (−0.20 to 0.43) | 0.43* (0.06 to 0.81) | 0.04 (−0.26 to 0.34) | 0.70** (0.24 to 1.16) | 0.07 (−0.50 to 0.64) |
| Married (yes) | 0.63* (0.15 to 1.10) | 0.03 (−0.41 to 0.47) | 0.53* (−0.04 to 1.02) | −0.06 (−0.48 to 0.36) | 0.84** (0.22 to 1.45) | 0.20 (−0.54 to 0.94) |
| Polygamous (yes) | −0.33* (−0.62 to −0.04) | 0.03 (−0.19 to 0.26) | −0.30* (−0.60 to −0.01) | 0.06 (−0.15 to 0.27) | −0.36 (−0.75 to 0.03) | – |
| Relationship satisfaction scale score (mean) | 0.10*** (0.08 to 0.12) | 0.07*** (0.04 to 0.09) | 0.10*** (0.08 to 0.12) | 0.08*** (0.05 to 0.10) | 0.10*** (0.07 to 0.13) | 0.06** (0.02 to 0.09) |
| Interactions with male partner scale score (mean) | 0.05*** (0.03 to 0.07) | 0.05***(0.03 to 0.07) | 0.05*** (0.03 to 0.07) | 0.04*** (0.02 to 0.06) | 0.06*** (0.03 to 0.09) | 0.05** (0.02 to 0.08) |
| Couple-level HIV-related behaviors | ||||||
| Disclosed HIV status to male partner (yes) | 1.50*** (0.84 to 2.16) | 1.15***(0.59 to 1.72) | 1.60*** (0.93 to 2.28) | 1.21*** (0.67 to 1.76) | 1.25** (0.45 to 2.15) | 1.07* (0.00 to 2.14) |
| Ever tested for HIV as a couple (yes) | 0.55*** (0.29 to 0.82) | 0.30** (0.09 to 0.51) | 0.52*** (0.25 to 0.80) | 0.26* (0.05 to 0.46) | 0.58** (0.23 to 0.93) | 0.51** (0.14 to 0.87) |
p < 0.05;
p < 0.01;
p < 0.001
At the relationship-level, numerous male partner characteristics and couple relationship dynamics were associated with a higher score across the scales in simple regression (see Table 6). The following characteristics were associated with a higher score on all three scales (i.e., the overall scale, the encouragement/reminders sub-scale, and the active participation sub-scale): living with the male partner (B = 0.43–0.70; p < 0.01—p < 0.05); being married (B = 0.53–0.84 p < 0.01—p < 0.05); relationship satisfaction scale score (B = 0.10; p < 0.001), and interactions with male partner scale score (B = 0.05–0.06; p < 0.001). Conversely, having a male partner with an unknown HIV status was associated with a lower score on all the male partner involvement scales in simple regression (B = − 0.64–1.12; p < 0.001—p < 0.05). Being in a polygamous marriage was additionally associated with a lower score on the overall scale and the encouragement/reminders sub-scale (B = − 0.30–0.33; p < 0.05), but not the active participation sub-scale (B = − 0.36; p = 0.07). Finally, HIV status disclosure to the male partner and CHTC were associated with a higher score on all of the scales in the simple regression models (B = 1.25–1.60; p < 0.001—p < 0.01, and B = 0.52–0.58; p < 0.001—p < 0.01, respectively).
In the multivariable models, internalized stigma remained negatively associated with the overall male partner involvement scale, but not with the sub-scales. For each decrease in one’s internalized stigma score, participants had a 0.03 increase in the male partner involvement scale score (p < 0.05), after adjusting for covariates. An additional factor associated only with the encouragement/reminders subscale in the multivariable models was being newly diagnosed with HIV. After adjusting for covariates, participants who reported being newly diagnosed with HIV during pregnancy had, on average, a 0.27 decrease in their encouragement/reminders sub-scale score, compared to women who knew their HIV-positive status prior to enrollment (p < 0.05). This association was not seen, however, with the overall male involvement scale or the active participation sub-scale.
Relationship dynamics and couples-level HIV behaviors were consistently associated with a higher score across the three scales in the multivariable models. First, for each increase in the relationship satisfaction scale score, participants had, on average, a 0.07 increase in the overall male partner involvement scale score (p < 0.001), as well as a 0.08 increase in the encouragement/reminders sub-scale score (p < 0.001), and a 0.06 increase in the active participation sub-scale score (p < 0.01). Similarly, for each increase in the interactions with male partners scale score (i.e., more positive interactions), participants had, on average, a 0.05 increase in both the overall male partner involvement scale score and active participation sub-scale score (p < 0.001 and p < 0.01, respectively), as well as a 0.04 increase in the encouragement/reminders sub-scale score (p < 0.001). In addition, in the multivariable models, women who disclosed their HIV status to the male partner had, on average, a 1.15 increase in the overall male partner involvement score (p < 0.001), a 1.21 increase in the encouragement/reminders sub-scale score (p < 0.001), and a 1.07 increase in the active participation sub-scale score (p < 0.05), compared to women who did not disclose their HIV status to their male partner. Lastly, couples who tested for HIV together through CHTC had a 0.30 increase in mean overall male partner involvement score (p < 0.01), a 0.26 increase in mean encouragement/reminders sub-scale score (p < 0.05), and a 0.51 increase in mean active participation sub-scale score (p < 0.01), compared to couples who had not tested together through CHTC, after adjusting for covariates.
Discussion
Although various measures have been developed to capture male involvement in HIV care during pregnancy and after the birth in different contexts globally [17, 35], this is the first study to our knowledge to develop and validate a scale measuring male behaviors across the PMTCT continuum of care in a sub-Saharan African country in the context of a high HIV prevalence. Our novel male partner involvement scale builds on the work of Byamugisha and colleagues, who developed an index measuring male partner involvement in PMTCT during the antenatal time period [17]. Our scale, however, measures a range of specific behaviors that males can engage into enhance PMTCT efforts across the continuum of care from pregnancy into postpartum. This significantly contributes to the field by establishing a valid tool to measure male partner involvement in PMTCT—including behaviors both inside and outside of the home—instead of focusing on a vague concept of male engagement [13, 14] or on one isolated behavior, such as male accompaniment to ANC [25, 36]. Our scale also moves the conceptualization of male partner involvement beyond the narrow focus of the antenatal time period [17, 37], which is increasingly important with countries moving towards lifelong ART for all women, often initiated through PMTCT [38].
The psychometric properties, including construct validity, of the present male partner involvement scale and sub-scales are promising. Not only does the overall scale provide strong internal reliability, but it also is associated with theoretically-relevant measures of positive couple relationship dynamics and positive couple-level HIV-related health behaviors, thus indicating preliminary validity. Our findings indicate that women who report better functioning relationships with male partners, measured through relationship satisfaction and positive interactions, score higher, on average, on the overall male partner involvement scale and sub-scales in both simple and multivariable regression models. These findings are in-line with other studies that indicate the importance of the marital relationship for men’s involvement in PMTCT [16, 17, 33, 37, 39] and the couple adopting healthy HIV-related behaviors [40, 41].
Due to the cross-sectional nature of the study, we are, unfortunately, not able to determine the direction of the relationships. For instance, it is unclear whether positive HIV-related health behaviors (e.g., CHTC) lead to higher male partner involvement, or if couples with more male partner involvement are subsequently more likely to practice positive HIV-related health behaviors like seeking testing together. It is clear, however, that positive couple-level HIV-related behaviors, including status disclosure and CHTC, in this study are consistently associated with higher scores on the overall male partner involvement scale, as well as the sub-scales of encouragement/reminders and active participation. This finding provides additional support for the preliminary validity of the scale to measure an important construct related to HIV care and treatment among members in families affected by HIV.
HIV-related stigma among the participants in this study appears to be an important factor negatively associated with the overall male partner involvement scale, and potentially the encouragement/reminders and active participation subscales. Women’s greater internalized HIV-related stigma was associated with lower score on the sub-scales in the simple models; however, it was not longer significant in the multivariable models. Yet, for the overall male partner involvement scale, the negative relationship with women’s internalized HIV stigma persisted even in the context of controlling for HIV status disclosure and other covariates in the multivariable model. It is plausible that women who received little support from their male partners, even after disclosure, may feel more internalized stigma around their HIV status than women who have partners involved in PMTCT. Or, it may be that women who have low self-worth related to their HIV status feel unable to solicit the support they need from their male partners. Although not significant in the multivariable models, depression is another important variable that was associated with lower scores on the male partner involvement scales in the simple models. Indeed, depression is often noted in prior work as being associated with sub-optimal HIV care and treatment [41-44]. This finding warrants more exploration into the interaction between male partner involvement, relationship dynamics, and women’s mental health and stigma.
Although our study reports compelling associations, there is a need for future longitudinal research that could help to elucidate the direction of these relationships and provide further evidence in terms of temporality. Studies using this version of the male partner involvement scale or an adapted version that allow for testing of pathways using structural equation modeling or other types of path analyses would be especially relevant. Future research can also build on our findings by improving the reliability of the active participation sub-scale and testing the overall scale in larger samples to determine its reliability, validity, and stability over time and in different settings. Given the importance cited by women in this study, future versions of the male partner involvement scale may also want to include the provision of food/nutrition as an additional item. Lastly, the scale provides an opportunity for future studies to use a valid measure to test whether interventions are able to increase male involvement as a pathway to better HIV-related health outcomes among peripartum women, their children, and male partners themselves.
The findings of this study should be considered in the light of limitations. First, the data collected was crosssectional, making it difficult to assess the directionality of relationships. The sample also consisted of postpartum women with HIV who were enrolled in a trial testing different approaches for enhancing PMTCT, and thus, may not be representative of the experiences of all peripartum women with HIV in such low-resource high HIV-prevalence settings. However, we observed considerable variation in predictor variables and male partner involvement in this sample, and were able to uncover significant associations using rigorous statistical methods. Our outcome, however, may have been influenced by other variables that were not captured in this study. Finally, the portion of the study reported here did not elicit men’s perspectives on male partner involvement in PMTCT, although a subsequent set of in-depth interviews with male partners that has been reported elsewhere provides insights and allows for triangulation [45].
Conclusions
This study developed a novel scale to measure male partner involvement in the PMTCT continuum of care from pregnancy to postpartum in a high HIV-prevalence setting of Kenya. The internal reliability of the overall male partner involvement scale and two sub-scales were promising. Positive relationship dynamics and couples-level HIV-related behaviors were associated with higher scores on the overall male partner involvement scale and two sub-scales (encouragement/reminders and active participation), which indicate strong construct validity. The scale would benefit from further testing in larger samples with longitudinal data. This work advances the conceptualization of male partner involvement in PMTCT and provides a valid measure to assess male behaviors across the PMTCT continuum of care.
Acknowledgments
Funding This work was supported by the National Institute of Mental Health under Grant K99MH116735; the National Institute of Child Health and Human Development under Grant R01HD080477; and the National Institute of Allergy and Infectious Disease-funded Colorado HIV Research Training Program under Grant 4T32AI007447. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
Ethical Approval All procedures performed involving human participants were in accordance with the ethical standards of the institutional and/or national research committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Relevant institutional review boards at the University of Colorado Denver, University of Alabama Birmingham, and Kenya Medical Research Institute (KEMRI) provided ethical approval for the study. Individual consent was obtained by trained Kenyan research assistants who conducted an informed consent process, including a signed consent (or thumbprint) form and an information sheet read aloud in the participant’s preferred language.
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hamilton E, Bossiky B, Ditekemena J, Esiru G, Fwamba F, Goga AE, et al. Using the PMTCT cascade to accelerate achievement of the global plan goals. J Acquir Immune Defic Syndr. 2017;75(Suppl 1):S27–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wettstein C, Mugglin C, Egger M, Blaser N, Vizcaya LS, Estill J, et al. Missed opportunities to prevent mother-to-child-transmission: systematic review and meta-analysis. AIDS. 2012;26(18):2361–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aluisio A, Bosire R, Bourke B, Gatuguta A, Kiarie JN, Nduati R, et al. Male partner participation in antenatal clinic services is associated with improved hiv-free survival among infants in Nairobi, Kenya: a prospective cohort study. J Acquir Immune Defic Syndr. 2016;73(2):169–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baiden F, Remes P, Baiden R, Williams J, Hodgson A, Boelaert M, et al. Voluntary counseling and HIV testing for pregnant women in the Kassena-Nankana district of northern Ghana: is couple counseling the way forward? AIDS Care. 2005;17(5):648–57. [DOI] [PubMed] [Google Scholar]
- 5.Chinkonde JR, Sundby J, Martinson F. The prevention of mother-to-child HIV transmission programme in Lilongwe, Malawi: why do so many women drop out. Reprod Health Matters. 2009;17(33):143–51. [DOI] [PubMed] [Google Scholar]
- 6.Turan JM, Bukusi EA, Onono M, Holzemer WL, Miller S, Cohen CR. HIV/AIDS stigma and refusal of HIV testing among pregnant women in rural Kenya: results from the MAMAS study. AIDS Behav. 2011;15(6):1111–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Farquhar C, Kiarie JN, Richardson BA, Kabura MN, John FN, Nduati RW, et al. Antenatal couple counseling increases uptake of interventions to prevent HIV-1 transmission. J Acquir Immune Defic Syndr. 2004;37(5):1620–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kiarie JN, Kreiss JK, Richardson BA, John-Stewart GC. Compliance with antiretroviral regimens to prevent perinatal HIV-1 transmission in Kenya. AIDS. 2003;17(1):65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turan JM, Hatcher AH, Medema-Wijnveen J, Onono M, Miller S, Bukusi EA, et al. The role of HIV-related stigma in utilization of skilled childbirth services in rural Kenya: a prospective mixed-methods study. PLoS Med. 2012;9(8):e1001295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jefferys LF, Nchimbi P, Mbezi P, Sewangi J, Theuring S. Official invitation letters to promote male partner attendance and couple voluntary HIV counselling and testing in antenatal care: an implementation study in Mbeya Region, Tanzania. Reprod Health. 2015;12:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Takah NF, Kennedy ITR, Johnman C. The impact of approaches in improving male partner involvement in the prevention of mother-to-child transmission of HIV on the uptake of maternal antiretroviral therapy among HIV-seropositive pregnant women in sub-Saharan Africa: a systematic review and meta-analysis. BMJ Open. 2017;7(11):e018207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nyondo-Mipando AL, Chimwaza AF, Muula AS. “He does not have to wait under a tree”: perceptions of men, women and health care workers on male partner involvement in prevention of mother to child transmission of human immunodeficiency virus services in Malawi. BMC Health Serv Res. 2018;18(1):187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kalembo FW, Zgambo M, Mulaga AN, Yukai D, Ahmed NI. Association between male partner involvement and the uptake of prevention of mother-to-child transmission of HIV (PMTCT) interventions in Mwanza district, Malawi: a retrospective cohort study. PLoS ONE. 2013;8(6):e66517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spangler SA, Onono M, Bukusi EA, Cohen CR, Turan JM. HIV-positive status disclosure and use of essential PMTCT and maternal health services in rural Kenya. J Acquir Immune Defic Syndr. 2014;67(Suppl 4):S235–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mabachi NM, Brown M, Sandbulte M, Wexler C, Goggin K, Maloba M, et al. Using a social support framework to understand how HIV positive kenyan men engage in PMTCT/EID care: qualitative insights from male partners. AIDS Behav. 2019;1:1 10.1007/s10461-019-02451-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.WHO. Male involvement in the prevention of mother-to-child transmission of HIV. Geneva: World Health Organization; 2012. [Google Scholar]
- 17.Byamugisha R, Tumwine JK, Semiyaga N, Tylleskar T. Determinants of male involvement in the prevention of mother-to-child transmission of HIV programme in Eastern Uganda: a cross-sectional survey. Reprod Health. 2010;7:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Matseke MG, Ruiter RAC, Rodriguez VJ, Peltzer K, Setswe G, Sifunda S. Factors associated with male partner involvement in programs for the prevention of mother-to-child transmission of HIV in rural South Africa. Int J Environ Res Public Health. 2017;14(11):1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peltzer K, Jones D, Weiss SM, Shikwane E. Promoting male involvement to improve PMTCT uptake and reduce antenatal HIV infection: a cluster randomized controlled trial protocol. BMC Public Health. 2011;11:778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tokhi M, Comrie-Thomson L, Davis J, Portela A, Chersich M, Luchters S. Involving men to improve maternal and newborn health: a systematic review of the effectiveness of interventions. PLoS ONE. 2018;13(1):e0191620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.NACC. Kenya HIV estimates: report 2018. National AIDS Control Council. Kenya Ministry of Health; 2018. [Google Scholar]
- 22.Odeny TA, Onono M, Owuor K, Helova A, Wanga I, Bukusi EA, et al. Maximizing adherence and retention for women living with HIV and their infants in Kenya (MOTIVATE! study): study protocol for a randomized controlled trial. Trials. 2018;19(1):77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. Thousand Oaks: SAGE; 2007. p. 275. [Google Scholar]
- 24.StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 25.Aluisio AR, Bosire R, Betz B, Gatuguta A, Kiarie JN, Nduati R, et al. Male partner participation in antenatal clinic services is associated with improved HIV-free survival among infants in Nairobi, Kenya: a prospective cohort study. J Acquir Immune Defic Syndr. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sherr L, Croome N. Involving fathers in prevention of mother to child transmission initiatives–what the evidence suggests. J Int AIDS Soc. 2012;15(Suppl 2):17378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hampanda K. “It was from this encouragement I got used to taking the medication:”A Qualitative Study on Male Partner Support after Status Disclosure among Pregnant and Postpartum Women Living with HIV in Zambia. Alabama: Inter-CFAR Collaborative Symposium on HIV Research in Women; Birmingham; 2016. [Google Scholar]
- 28.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Netemeyer RG, Bearden WO, Sharma S. Scaling procedures: issues and applications. Thousand Oaks: Sage; 2003. p. 203. [Google Scholar]
- 30.DeVellis RF. Scale development: theory and applications, 4th edn. Los Angeles: SAGE; 2017. p. 262. [Google Scholar]
- 31.Kaiser HF. An index of factor simplicity. Psychometrika. 1974;39:31–6. [Google Scholar]
- 32.Comrey AL, Lee HB. A first course in factor analysis. 2nd ed. Hillsdale: L. Erlbaum Associates; 1992. p. 430. [Google Scholar]
- 33.Orne-Gliemann J, Tchendjou PT, Miric M, Gadgil M, Butsashvili M, Eboko F, et al. Couple-oriented prenatal HIV counseling for HIV primary prevention: an acceptability study. BMC Public Health. 2010;10:197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Betancourt TS, Abrams EJ, McBain R, Fawzi MC. Family-centred approaches to the prevention of mother to child transmission of HIV. J Int AIDS Soc. 2010;13(Suppl 2):S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Turan JM, Nalbant H, Bulut A, Sahip Y. Including expectant fathers in antenatal education programmes in Istanbul, Turkey. Reprod Health Matters. 2001;9(18):114–25. [DOI] [PubMed] [Google Scholar]
- 36.Nyondo AL, Choko AT, Chimwaza AF, Muula AS. Invitation cards during pregnancy enhance male partner involvement in prevention of mother to child transmission (PMTCT) of human immunodeficiency virus (HIV) in Blantyre, Malawi: a randomized controlled open label trial. PLoS ONE. 2015;10(3):e0119273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Katz DA, Kiarie JN, John-Stewart GC, Richardson BA, John FN, Farquhar C. Male perspectives on incorporating men into antenatal HIV counseling and testing. PLoS ONE. 2009;4(11):e7602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.World Health Organization. Progress Report 2016: Prevent HIV, Test and Treat All: WHO Support For Country Impact. Geneva: World Health Organization; 2016. [Google Scholar]
- 39.Rogers AJ, Achiro L, Bukusi EA, Hatcher AM, Kwena Z, Musoke PL, Turan JM, Weke E, Darbes LA. Couple interdependence impacts HIV-related health behaviours among pregnant couples in southwestern Kenya: a qualitative analysis. J Int AIDS Soc. 2016;19(1):21224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Turan JM, Darbes LA, Musoke PL, Kwena Z, Rogers AJ, Hatcher AM, et al. Development and piloting of a home-based couples intervention during pregnancy and postpartum in Southwestern Kenya. AIDS Patient Care STDS. 2018;32(3):92–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Darbes LA, van Rooyen H, Hosegood V, Ngubane T, Johnson MO, Fritz K, et al. Uthando Lwethu (‘our love’): a protocol for a couples-based intervention to increase testing for HIV: a randomized controlled trial in rural KwaZulu-Natal, South Africa. Trials. 2014;15:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hatcher AM, Stöckl H, Christofides N, Woollett N, Pallitto CC, Garcia-Moreno C, et al. Mechanisms linking intimate partner violence and prevention of mother-to-child transmission of HIV: a qualitative study in South Africa. Soc Sci Med. 2016;168:130–9. [DOI] [PubMed] [Google Scholar]
- 43.Letta S, Demissie A, Oljira L, Dessie Y. Factors associated with adherence to Antiretroviral Therapy (ART) among adult people living with HIV and attending their clinical care, Eastern Ethiopia. BMC Int Health Hum Rights. 2015;15:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mellins CA, Kang E, Leu CS, Havens JF, Chesney MA. Longitudinal study of mental health and psychosocial predictors of medical treatment adherence in mothers living with HIV disease. AIDS Patient Care STDS. 2003;17(8):407–16. [DOI] [PubMed] [Google Scholar]
- 45.Hampanda KM, Turan JM, Helova A, Onono M, Odwar T, Hoople K, Bukusi E, Abuogi LL. “When we come together, we leave with a common goal:” men’s perspectives on male partner involvement in the prevention of mother-to-child transmission. AIDS Impact 14th International Conference; 2019; London. [Google Scholar]
- 46.International Parenthood Federation (IPF), Global Network of People Living with HIV (GNP+), International Community of Women Living with HIV (ICW), UNAIDS. The People Living with HIV Stigma Index: an index to measure the stigma and discrimination experienced by people living with HIV London: International Parenthood Federation; 2008. [Google Scholar]
- 47.Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1–3):163–73. [DOI] [PubMed] [Google Scholar]
- 48.Kroenke K, Spitzer RL, Williams JB, Lowe B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. 2010;32(4):345–59. [DOI] [PubMed] [Google Scholar]
- 49.Rusbult C, Martz J, Agnew C. The Investment Model Scale: measuring commitment level, satisfaction level, quality of alternatives, and investment size. Pers Relationsh. 1998;5(4):357–91. [Google Scholar]
- 50.Schuster TL, Kessler RC, Aseltine RH. Supportive interactions, negative interactions, and depressed mood. Am J Community Psychol. 1990;18(3):423–38. [DOI] [PubMed] [Google Scholar]
- 51.Turner RJ, Frankel BG, Levin DM. Social support: conceptualization, measurement, and implications for mental health. Res Community Ment Health. 1983;3:67–111. [Google Scholar]