Abstract
Introduction
Recurrent spontaneous abortion is a multifactorial disorder and till date, various factors have been attributed in its pathogenesis. Still, approximately 50% of RSA cases remain unexplained. Premutation (PM) expanded allele of fragile-X mental retardation 1 (FMR1) gene is known to contribute to ovarian dysfunction in 20% of the cases. Recently, the link between expanded FMR1 allele and recurrent miscarriages has been reported.
Method
In the present prospective case–control study, we have investigated the status of CGG repeat size at 5′UTR of the FMR1 gene in women with unexplained RSA in comparison to age-matched healthy control women (n = 100 each). The genomic DNA from these samples was subjected to molecular analysis for characterization of CGG repeat size and composition at FMR1 gene
Results
As compared to the control women, the RSA women cohort had a higher frequency of carriers with alleles in gray zone (GZ) and expanded PM range, i.e., 2% (2/100) versus 5% (5/100), respectively. Also, the RSA cohort had a significantly higher number of normal alleles with ≥ 35 CGG repeats (24 out of 200 alleles) as compared to control cohort (8 out of 200 alleles). The number of larger FMR1 alleles with pure CGG repeat tract was found to be significantly higher (P = 0.0063) in the RSA cohort (15 out of 200 alleles) as compared to that in control cohort (3 out of 200 alleles).
Conclusion
Henceforth, the CGG expanded uninterrupted FMR1 allele might be associated with recurrent abortions and may help to explain many of these unexplained cases.
Keywords: Fragile X syndrome, CGG repeats, Unexplained recurrent miscarriages, Molecular diagnosis
Introduction
Recurrent spontaneous abortion (RSA) is characterized by ≥ 2 successive pregnancy losses before 20–22 gestational weeks. Approximately 1–5% of reproductive age women are affected by RSA [1–3]. It is multifactorial in nature and the known factors include uterine anomalies [4], immunological blood clotting disorder [5], genitourinary infection [6], endocrine dysfunction [7, 8], and chromosomal abnormalities [9–11]. Despite the number of proposed etiologies, the cause of RSA still remains unexplained in ∼ 45–50% of the patients [12–14]. In patients with idiopathic RSA, genetic factors have been proposed to be a major underlying cause [15, 16].
The role of X-linked FMR1 gene in ovarian dysfunction had been already defined. The dynamic nature of CGG repeat expansion in the FMR1 gene has a variable trait. The full-mutation FMR1 allele (> 200 CGG repeats at 5′UTR) is associated with an inherited form of mental retardation, and the permutation allele (55 to 200 CGG) with FXPOI, a form of ovarian dysfunction [17]. Furthermore, few studies have reported that high normal alleles (35 to 44 CGG repeats) and gray zone alleles (45 to 54 CGG repeats) are also at an elevated risk of POI [18–21]. It has been anticipated recently that POI should be considered as a continuum of ovarian dysfunction and not as a dichotomous state having normal ovarian functionality followed by menopause [22, 23]. This is evident from the finding that PM carrier females, who are cycling normally, have a significant level of ovarian reserve depletion [24, 25]. Continuous effect of increasing repeat size on disease onset and severity has been documented previously in other triplet repeat disorder like Huntington diseases [26]. Thus, probably increasing the size of CGG repeats beyond the normal range at the FMR1 gene may have pathogenic consequences ranging from recurrent miscarriages to infertility. Also, recently connecting links between oocyte-specific genes involved in ovarian reserve depletion and RSA is highlighted and the possibility of interrogating these genes in cases of unexplained RSA was suggested [27]. As the PM allele of the FMR1 gene is already known to be associated with POI, it is also reasonable enough to cross-examine the FMR1 gene for its putative role in RSA. The pattern of AGG interruption in PM and GZ alleles had also been previously linked to POI phenotype [28, 29]. Hence, the possible correlation between the CGG repeat composition and RSA manifestation needs to be inspected. We hypothesized that presence of pure CGG tract in FMR1 allele is prone to get expanded in the next generation, and these expanded allele may have pathogenic consequences leading to recurrent abortions. Thus, we investigated the impact of both CGG repeat size and composition at the FMR1 gene in women with unexplained RSA.
Materials and methods
Subjects
We have enrolled 100 women of unexplained RSA (cases) (age ± standard deviation: 29.2 ± 3.8 years) and 100 age-matched healthy women (controls) (age ± standard deviation: 29.4 ± 4.1 years) in this study.
The RSA cohort consists of women who had at least two successive pregnancy losses up to the completion of 20 weeks of pregnancy. Clinical examination and laboratory investigations were performed for the study subjects to exclude other causes of abortion. Women with the known causes for RSA like parental chromosomal abnormalities, untreated hypothyroidism, uncontrolled diabetes mellitus, uterine anatomic abnormalities antiphospholipid antibody syndrome (APS), other endocrine disorders, thrombophilias, immunologic abnormalities, infections, and environmental factors have been excluded from this study. The control cohort consists of reproductively active women with documented fertility and no history of recurrent pregnancy loss.
The cases were referred from the outpatient department of Genetics, SGPGI, Lucknow. The control women were those who were visiting the General Hospital, SGPGIMS, Lucknow, for a routine checkup.
Study duration and setting
This study was carried out from September 2014 to July 2018 in the department of medical genetics, Sanjay Gandhi Postgraduate Institute Of Medical Sciences, Lucknow. The study was approved by the institutional ethical committee (IEC: 2016-28-PHD-90) and informed consent was obtained from the cases and controls.
Sample collection and DNA isolation
Two milliliters of peripheral blood was collected in EDTA-coated vials from the cases and the controls. Genomic DNA was extracted by the standard phenol-chloroform method. The DNA concentration was measured using Nanodrop.
Methodology
Genomic DNA samples from cases and control were tested for the presence of CGG expansion in the FMR1 gene using a two-step PCR protocol. Briefly, fluorescent SP-PCR was carried out for all the samples. The samples that yielded single amplification band were then subjected to TP-PCR reaction. The amplified product (4 μl) was diluted in 8 μl of Hi-Di formamide and 0.5 μl of LIZ 500, denatured, and subjected to fragment analysis (capillary electrophoresis (ABI 310) with the following parameters: injection time 5 s, injection voltage 15 kW, run time 28 min, running voltage 12.5 kW, polymer POP4 [30].
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics v21. Continuous data were described as mean ± S.D. and frequencies as n (%). Comparison between the two cohorts to test the level of significance was performed using Fisher exact test.
Results
Out of 100 RSA women enrolled for the study, 59% had a minimum of two pregnancy losses (average age ± standard deviation 29.2 ± 3.8 years), while 41% had three or more pregnancy losses (average age ± standard deviation 29.2 ± 3.8 years) (28% with three, 10% with four, and 3% with five pregnancy losses). Eighty-six percent losses were in the first trimester and 14% were reported in the second trimester.
Molecular analysis of the CGG repeat region at FMR1 gene identified polymorphic nature of the repeat region in both size (number of repeats) and composition (presence of AGG interruptions and its location).
A total of 19 different sized alleles were obtained in the control cohort (comprising of normal and GZ alleles). The CGG repeats in normal alleles ranged from 18 to 44 repeats within the normal range, the most common repeat is 29 (33%), followed by 28 (19%). Combining the results of fluorescent SP-PCR and TP-PCR, 79% were found to be heterozygous and 21% were homozygous for the repeat size at FMR1 gene. GZ allele was observed in two (2%) control subjects, while no PM alleles were identified among the control subjects. Among the RSA women, a total of 28 different sized alleles were obtained including the normal, GZ, and PM alleles. The CGG repeats in normal alleles ranged from 18 to 43 repeats. Here also, the most commonly found repeat size is 29 repeats (31%), followed by 28 (15.5%). Seventy-eight percent were found to be heterozygous and 22% were homozygous for the repeat size at FMR1 gene. GZ allele and PM allele were observed in five (5%) and two (2%) cases respectively.
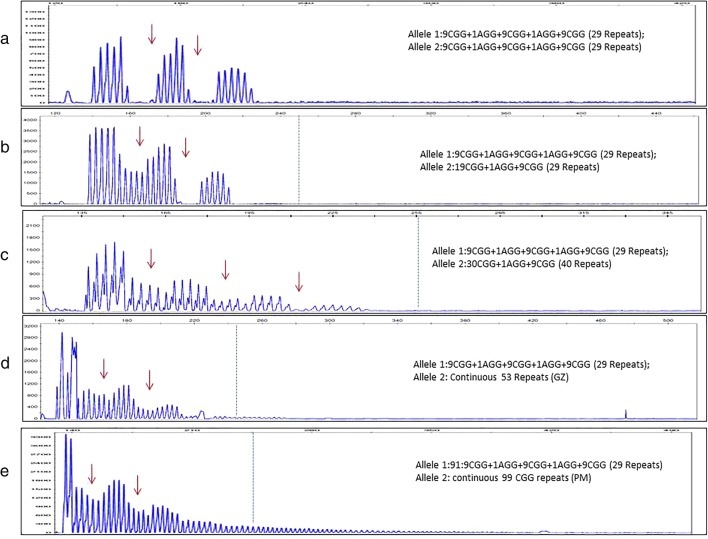
The comparative FMR1 gene allelic frequency within the normal range among the control and the RSA women is depicted in Fig. 1.
Fig. 1.
Comparative FMR1 allelic frequency of RSA and control cohort (n = 100 each)
As compared to the control women, the RSA women cohort had a higher frequency of carriers with alleles in GZ and PM range, i.e., 2% (2/100) versus 5% (5/100), respectively. Also, the RSA cohort had a significantly higher number of normal alleles with ≥ 35 CGG repeats (24 out of 200 alleles) as compared to the control cohort (eight out 200 alleles) (P = 0.005)
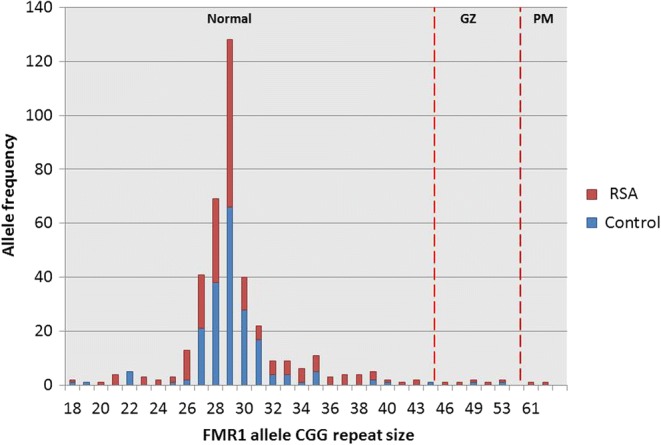
The pattern of AGG interruption at the FMR1 repeat gene was also studied in both the cohorts. Mostly, FMR1 alleles with repeat size in a normal range were found to be interrupted with 1, 2, or 3 AGG interruptions in both cohorts. Furthermore, FMR1 allele with pure CGG repeat tract (comprising of normal, GZ, and PM alleles) was observed in nine (9%) control subjects and in 22 RSA cases (22%). Among the normal alleles, this continuous stretch of CGG repeats is found in either smaller-sized FMR1 alleles (with 18 to 25 CGG repeats) or with larger FMR1 alleles (with ≥ 35 CGG repeats but within the normal range). Upon statistical investigation of the data, it was found that the number of larger FMR1 alleles with pure CGG repeat tract was found to be significantly higher (P = 0.0063) in the RSA cohort (15 out of 200 alleles) as compared to that in the control cohort (3 out of 200 alleles). In the control cohort, one of the two identified expanded GZ allele was found to be interrupted while in RSA cohort all the GZ and PM alleles identified were uninterrupted. Table 1 shows the CGG repeat categories at the FMR1 gene in RSA and control cohort, Fig. 2 shows the representative TP-PCR peaks of normal, GZ, and PM alleles. The CGG repeat size obtained in RSA women cohort did not correlate with the number of miscarriages they had.
Table 1.
CGG repeat categories at FMR1 gene in RSA and control cohort
| FMR1 allele | RSA group | Control group |
|---|---|---|
| Normal alleles (6–44 CGG) | 193 | 198 |
| GZ alleles (45–54 CGG) | 5 | 2 |
| PM alleles (55–200 CGG) | 2 | 0 |
| FMR1 alleles (≥ 35 CGG repeats) | 24 | 8 |
| FMR1 alleles (uninterrupted ≥ 35 CGG repeats) | 17 | 4 |
Fig. 2.
TP-PCR DNA chromatogram for normal, GZ, and PM subject from control and RSA cohort. a Homozygous sample with interrupted normal FMR1 alleles (29 CGG repeats). b Homozygous sample with normal FMR1 alleles (29 CGG repeats). One allele is interrupted by two AGG while other by 1 AGG. c Heterozygous sample with interrupted normal FMR1 alleles 29 and 40 repeats. d Heterozygous sample with interrupted normal allele of 29 and continuous GZ allele of 53 repeats (Pure CGG tract on second allele). e Heterozygous sample with interrupted normal allele of 30 CGG repeats and continuous PM allele of 99 CGG repeats (pure CGG tract on second allele). Note: blue vertical line shows edge of repeats in normal range and red vertical arrows depicts the position of AGG interruptions
Discussion
FMR1 gene expansion mutation in the PM range has long been documented to be responsible for impaired ovarian response and decreased fertilization rate [31, 32]. While the reproductive consequences of GZ alleles, as well as larger normal alleles (35 to 44 CGG), are argumentative. Some of the previous studies have displayed augmented rates of larger normal repeats in POI and diminished ovarian reserve groups [33, 34]. Other studies had depicted expanded allele in GZ range to be associated with a higher frequency of subfertility, menstrual irregularities, earlier menopause, POI, higher rate of aneuploidies, miscarriage, and non-identical twinning as compared to normal [35, 36]. Previously, [37] it was reported that trisomy 21 births frequently occur in female fragile X carriers. While other studies could not find a positive relationship between the rate of unfavorable outcomes (including pregnancy loss) and premutation carrier status of women [38–40]. These findings suggest the involvement of the FMR1 gene in a spectrum of ovarian dysfunction.
In the current study, we inspected the incidence of expanded FMR1 alleles in women with unexplained RSA. Our study documented that these women had a higher number of expanded GZ and PM FMR1 allele in comparison to control women with documented normal fertility. The number of larger normal alleles was meaningfully different between the two cohorts. Also, a significantly higher abundance of uninterrupted larger FMR1 alleles was observed among the RSA cohort. The results of our study suggest a possible role of uninterrupted PM, GZ, and large normal FMR1 allele in unexplained RSA.
It is well known that the reproductive potential of a woman depends principally on the ovarian reserve, number, and quality of the oocytes. In line with this finding, a higher prevalence of decreased ovarian reserve has been found among the women with unexplained RSA [41, 42] and the expanded alleles of FMR1 gene, permutation allele [35, 43], a high normal allele [18, 19], and gray zone allele [20, 21], increase the risk of diminished ovarian reserve and/or premature ovarian insufficiency in women. Although in our study we have not obtained PM allele to be significantly different among the cases and control, we cannot directly link recurrent miscarriages with POI. However, we have obtained a significantly higher number of GZ and high normal alleles in the case-cohort. As it is already established, the diagnosis of POI represents the extreme spectrum of an impaired ovarian function. It is quite possible that FMR1 allele with CGG repeats in range of high normal and GZ results in diminished ovarian reserves (DOR). Compromised oocyte quality in this situation could ultimately lead to genetic defects (aneuploidies) that are not compatible with life, thus leading to abortion. This hypothesis is supported by the findings that women with repeats > 30 CGG have shown reduced ovarian reserve, as documented by measuring ovarian parameters like AMH and FSH levels [20, 44]. The diminished level of serum AMH and elevated level of serum FSH already has documented role in miscarriage, thus providing evidence of the link between CGG expansion in GZ and high normal FMR1 alleles with recurrent miscarriages. Furthermore, the study by Kline et al. in 2012 depicted that the proportion of FMR1 alleles with long CGG repeat length was quite higher in women who had trisomic spontaneous pregnancy loss in comparison to the controls [45].
The main limitation of our study is that we have not analyzed the AMH and FSH values of cases and control and the presence of potential confounding factors and genetic evaluation of the product of conceptus of the RSA women cohort. Therefore, further prospective studies in this direction are required to confirm the possible link between FMR1 CGG repeats and recurrent miscarriages and also to reveal the molecular pathophysiology involved.
In spite of extensive studies done so far, for approximately 50% of the RSA cases that are encountered by the treating physicians, the cause remains unknown. Our study suggests a possible role of uninterrupted CGG alleles in GZ and the high normal range in RSA. Interrogating the FMR1 gene in the future may provide an explanation for a number of miscarriages.
Acknowledgements
The authors are grateful to the SGPGI of Medical Sciences, Lucknow, Uttar Pradesh, India, for providing the infrastructure for the research work. DDD is thankful Council of Science and Industrial Research (CSIR)–New Delhi for providing her fellowship.
Funding information
This study was supported by the intramural project grant funded by the SGPGI of Medical Sciences, Lucknow, India (2015-36-IMP-83).
Compliance with ethical standards
The study was approved by the institutional ethical committee (IEC: 2016-28-PHD-90) and informed consent was obtained from the cases and controls.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Deepika Delsa Dean, Email: deepikadean.ddd@gmail.com.
Sarita Agarwal, Phone: 91-522-2494349 (0), Phone: +91-9415336601, Email: saritasgpgi@gmail.com.
Srinivasan Muthuswamy, Email: srinimbt@gmail.com.
References
- 1.Rai R, Regan L. Recurrent miscarriage. Lancet. 2006;368:601–611. doi: 10.1016/S0140-6736(06)69204-0. [DOI] [PubMed] [Google Scholar]
- 2.Royal College of Obstetricians and Gynaecologists (RCOG). The investigation and treatment of couples with recurrent first-trimester and second-trimester miscarriage. Green-top Guideline No. 17. Royal College of Obstetricians and Gynaecologists (RCOG), 2011.
- 3.Practice Committee of the American Society for Reproductive Medicine, 2012Practice Committee of the American Society for Reproductive Medicine. Evaluation and treatment of recurrent pregnancy loss: a committee opinion. Fertil Steril. 2012; 98: 1103–1111 [DOI] [PubMed]
- 4.Ali O, Hakimi I, Chanana A, et al. Grossesse sur utérus cloisonné menée à terme: à propos d’un cas avec revue de la literature. The Pan African Medical Journal. 2015;22:219. doi: 10.11604/pamj.2015.22.219.7790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cohn DM, Goddijn M, Middeldorp S, et al. Recurrent miscarriage and antiphospholipid antibodies: prognosis of subsequent pregnancy. J Thromb Haemost. 2010;8:2208–2213. doi: 10.1111/j.1538-7836.2010.04015.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Srinivas SK, Ma Y, Sammel MD, Chou D, et al. Placental inflammation and viral infection are implicated in second trimester pregnancy loss. Am J Obstet Gynecol. 2006;195:797–802. doi: 10.1016/j.ajog.2006.05.049. [DOI] [PubMed] [Google Scholar]
- 7.Arredondo F, Noble LS. Endocrinology of recurrent pregnancy loss. Semin Reprod Med. 2006;24:33–39. doi: 10.1055/s-2006-931799. [DOI] [PubMed] [Google Scholar]
- 8.Pluchino N, Drakopoulos P, Wenger JM, Petignat P, et al. Hormonal causes of recurrent pregnancy loss (RPL) Hormones (Athens) 2014;13(3):314–322. doi: 10.14310/horm.2002.1505. [DOI] [PubMed] [Google Scholar]
- 9.Niroumanesh S, Mehdipour P, Farajpour A, Darvish S. A cytogenetic study of couples with repeated spontaneous abortions. Ann Saudi Med. 2011;31:77–79. doi: 10.4103/0256-4947.75785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dubey S, Chowdhury MR, Prahlad B, Kumar V, Mathur R, et al. Cytogenetic causes for recurrent spontaneous abortions – an experience of 742 couples (1484 cases) Indian J Hum Genet. 2005;11:94–98. [Google Scholar]
- 11.Iravathy GK, Raina V, Verma S, Chadha G. Cytogenetics and genetic counselling of patients in North India. J K Science. 2006;8:28–30. [Google Scholar]
- 12.Stephenson MD. Frequency of factors associated with habitual abortion in 197 couples. Fertil Steril. 1996;66(1):24–29. [PubMed] [Google Scholar]
- 13.Stephenson M, Kutteh W. Evaluation and management of recurrent early pregnancy loss. Clin Obstet Gynecol. 2007;50(1):132–145. doi: 10.1097/GRF.0b013e31802f1c28. [DOI] [PubMed] [Google Scholar]
- 14.Toth B, Jeschke U, Rogenhofer N, Scholz C, Wurfel W, Thaler CJ, et al. Recurrent miscarriage: current concepts in diagnosis and treatment. J Reprod Immunol. 2010;85(1):25–32. doi: 10.1016/j.jri.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 15.Daher S, Mattar R, Gueuvoghlanian-Silva BY, Torloni MR. Genetic polymorphisms and recurrent spontaneous abortions: an overview of current knowledge. Am J Reprod Immunol. 2012;67(4):341–347. doi: 10.1111/j.1600-0897.2012.01123.x. [DOI] [PubMed] [Google Scholar]
- 16.Rull K, Nagirnaja L, Laan M. Genetics of recurrent miscarriage: challenges, current knowledge, future directions. Front Genet. 2012;3:34. doi: 10.3389/fgene.2012.00034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sullivan A.K., Marcus M., Epstein M.P., Allen E.G., Anido A.E., Paquin J.J., Yadav-Shah M., Sherman S.L. Association of FMR1 repeat size with ovarian dysfunction. Human Reproduction. 2005;20(2):402–412. doi: 10.1093/humrep/deh635. [DOI] [PubMed] [Google Scholar]
- 18.Pastore LM, Young SL, Baker VL, Karns LB, Williams CD. Silverman LM Elevated prevalence of 35-44 FMR1 trinucleotide repeats in women with diminished ovarian reserve. Reprod Sci. 2012;19(11):1226–1231. doi: 10.1177/1933719112446074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Streuli I, Fraisse T, Ibecheole V, Moix I, Morris MA, de Ziegler D. Intermediate and premutation FMR1 alleles in women with occult primary ovarian insufficiency. Fertil Steril. 2009;92(2):464–470. doi: 10.1016/j.fertnstert.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 20.Gleicher Norbert, Weghofer Andrea, Barad David H. A pilot study of premature ovarian senescence: I. Correlation of triple CGG repeats on the FMR1 gene to ovarian reserve parameters FSH and anti-Müllerian hormone. Fertility and Sterility. 2009;91(5):1700–1706. doi: 10.1016/j.fertnstert.2008.01.098. [DOI] [PubMed] [Google Scholar]
- 21.Karimov CB, Moragianni VA, Cronister A, Srouji S, Petrozza J, Racowsky C, et al. Increased frequency of occult fragile X-associated primary ovarian insufficiency in infertile women with evidence of impaired ovarian function. Hum Reprod. 2011;26(8):2077–2083. doi: 10.1093/humrep/der168. [DOI] [PubMed] [Google Scholar]
- 22.Sullivan SD, Welt C, Sherman S. FMR1 and the continuum of primary ovarian insufficiency. Semin Reprod Med. 2011;29:299–307. doi: 10.1055/s-0031-1280915. [DOI] [PubMed] [Google Scholar]
- 23.Man L, Lekovich J, Rosenwaks Z, Gerhardt J. Fragile X-associated diminished ovarian reserve and primary ovarian insufficiency from molecular mechanisms to clinical manifestations. Front Mol Neurosci. 2017;10:290. doi: 10.3389/fnmol.2017.00290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Murray A, Webb J, MacSwiney F, Shipley EL, Morton NE, Conway GS. Serum concentrations of follicle stimulating hormone may predict premature ovarian failure in FRAXA premutation women. Hum Reprod. 1999;14:1217–1218. doi: 10.1093/humrep/14.5.1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rohr J, Allen EG, Charen K, Giles J, He W, Dominguez C, et al. Anti-Mullerian hormone indicates early ovarian decline in fragile X mental retardation (FMR1) premutation carriers: a preliminary study. Hum Reprod. 2008;23:1220–1225. doi: 10.1093/humrep/den050. [DOI] [PubMed] [Google Scholar]
- 26.Harper PS, Jones L. Huntington's disease: genetic and molecular studies. In: Harper PS, Jones L, editors. Huntington’s disease, edited by Bates GP. Oxford, UK: Oxford University Press; 2002. pp. 113–158. [Google Scholar]
- 27.Dean DD, Agarwal S, Tripathi P. Connecting links between genetic factors defining ovarian reserve and recurrent miscarriages. J Assist Reprod Genet. 2018;35(12):2121–2128. doi: 10.1007/s10815-018-1305-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bodega B, Bione S, Dalprà L, Toniolo D, Ornaghi F, et al. Influence of intermediate and uninterrupted FMR1 CGG expansions in premature ovarian failure manifestation. Hum Reprod. 2005;21(4):952–957. doi: 10.1093/humrep/dei432. [DOI] [PubMed] [Google Scholar]
- 29.Lekovich J, Man L, Xu K, Canon C, Lilienthal D, et al. CGG repeat length and AGG interruptions as indicators of fragile X-associated diminished ovarian reserve. Genet Med. 2018;20(9):957–964. doi: 10.1038/gim.2017.220. [DOI] [PubMed] [Google Scholar]
- 30.Srinivasan M, Dean DD, Agarwal S. Molecular screening of intellectually disabled and premature ovarian failure cases for CGG repeat expansion at FMR1 locus: implication of combined triplet repeat primed polymerase chain reaction and methylation-specific polymerase chain reaction analysis. Neurol India. 2016;64(6):1175–1179. doi: 10.4103/0028-3886.193786. [DOI] [PubMed] [Google Scholar]
- 31.Bibi G, Malcov M, Yuval Y, Reches A, Ben-Yosef D, et al. The effect of CGG repeat number on ovarian response among fragile X premutation carriers undergoing preimplantation genetic diagnosis. Fertil Steril. 2010;94(3):869–874. doi: 10.1016/j.fertnstert.2009.04.047. [DOI] [PubMed] [Google Scholar]
- 32.Pastore LM, Christianson MS, McGuinness B, Vaught KC, et al. Does theFMR1 gene affect IVF success? Reprod BioMed Online. 2019;38(4):560–569. doi: 10.1016/j.rbmo.2018.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bretherick KL, Fluker MR, Robinson WP. FMR1 repeat sizes in the gray zone and high end of the normal range are associated with premature ovarian failure. Hum Genet. 2005;117:376–382. doi: 10.1007/s00439-005-1326-8. [DOI] [PubMed] [Google Scholar]
- 34.Bodega B, Bione S, Dalpr’a L, Toniolo D, Ornaghi F, Vegetti W, et al. Influence of intermediate and uninterrupted FMR1 CGG expansions in premature ovarian failure manifestation. Hum Reprod. 2006;21:952–957. doi: 10.1093/humrep/dei432. [DOI] [PubMed] [Google Scholar]
- 35.Sherman SL. Premature ovarian failure in the fragile X syndrome. Am J Med Genet. 2000;97:189–194. doi: 10.1002/1096-8628(200023)97:3<189::AID-AJMG1036>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 36.Te Velde ER, Pearson PL. The variability of female reproductive ageing. Hum Reprod Update. 2002;8:141–154. doi: 10.1093/humupd/8.2.141. [DOI] [PubMed] [Google Scholar]
- 37.Watson Michael S., Breg W. Roy, Pauls David, Brown W. Ted, Carroll Andrew J., Howard-Peebles Patricia N., Meryash David, Shapiro Lawrence R. Aneuploidy and the fragile X syndrome. American Journal of Medical Genetics. 1988;30(1-2):115–121. doi: 10.1002/ajmg.1320300110. [DOI] [PubMed] [Google Scholar]
- 38.Murray A, Ennis S, MacSwiney F, Webb J, Morton NE. Reproductive and menstrual history of females with fragile X expansions. Eur J Hum Genet. 2000;8:247–252. doi: 10.1038/sj.ejhg.5200451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hundscheid RD, Smits AP, Thomas CM, Kiemeney LA, Braat DD. Female carriers of fragile X premutations have no increased risk for additional diseases other than premature ovarian failure. Am J Med Genet A. 2003;117A:6–9. doi: 10.1002/ajmg.a.10862. [DOI] [PubMed] [Google Scholar]
- 40.Allen E.G., Sullivan A.K., Marcus M., Small C., Dominguez C., Epstein M.P., Charen K., He W., Taylor K.C., Sherman S.L. Examination of reproductive aging milestones among women who carry the FMR1premutation. Human Reproduction. 2007;22(8):2142–2152. doi: 10.1093/humrep/dem148. [DOI] [PubMed] [Google Scholar]
- 41.Trout Susan W, Seifer David B. Do women with unexplained recurrent pregnancy loss have higher day 3 serum FSH and estradiol values? Fertility and Sterility. 2000;74(2):335–337. doi: 10.1016/s0015-0282(00)00625-7. [DOI] [PubMed] [Google Scholar]
- 42.Gurbuz B, Yalti S, Ozden S, Ficicioglu C. High basal estradiol level and FSH/LH ratio in unexplained recurrent pregnancy loss. Arch Gynecol Obstet. 2004;270:37–39. doi: 10.1007/s00404-003-0490-0. [DOI] [PubMed] [Google Scholar]
- 43.Dean DD, Agarwal S, Kapoor D, Vati C. Molecular characterization of FMR1 gene in reproductive age women and premature ovarian insufficiency cases by TP-PCR. J mol Diagn Ther. 2017;22:91–100. doi: 10.1007/s40291-017-0305-9. [DOI] [PubMed] [Google Scholar]
- 44.Chatterjee S, Maitra A, Kadam S, et al. CGG repeat sizing in the FMR1 gene in Indian women with premature ovarian failure. Reprod BioMed Online. 2009;19(2):281–286. doi: 10.1016/s1472-6483(10)60086-7. [DOI] [PubMed] [Google Scholar]
- 45.Kline J., Kinney A., Brown S., Levin B., Oppenheimer K., Warburton D. Trisomic pregnancy and intermediate CGG repeat length at the FMR1 locus. Human Reproduction. 2012;27(7):2224–2232. doi: 10.1093/humrep/des098. [DOI] [PMC free article] [PubMed] [Google Scholar]