Abstract
We conducted a randomized control trial to evaluate the impact of a novel technology-based intervention on HIV risks and condom use behaviors among Thai men who have sex with men (MSM). Between April 2016 and August 2017, participants aged 18 years and above, and having engaged in unprotected sex in past six months were randomly assigned to control and intervention arm, and received HIV testing at baseline, month 6 and 12. Intervention arm participants engaged in 12-monthly HIV/STI prevention educational sessions delivered via Vialogues.com. Of 76 MSM enrolled, 37 were randomized to intervention and 39 to control arm. Median age was 28 (IQR 24-32) years. Thirty-three (89.2%) intervention arm participants completed all 12-monthly Vialogues sessions. At month 12, intervention arm had higher retention rate (p = 0.029) and higher median percentage of condom use for anal intercourse (p = 0.023) versus control arm. Over the 12-month period, intervention arm reported significant reduction in self-perceived HIV risk (p = 0.001), popper usage (p = 0.002), median number of sexual partners (p = 0.003), and increased median condom use percentage (p = 0.006). Our study highlights that “Vialogues” intervention significantly reduced number of sexual partners and condomless anal intercourse rates among Thai MSM, and has positive implications for reducing epidemic among key populations.
Keywords: Behavior change, condomless anal intercourse, HIV testing and counseling, men who have sex with men, Internet and communications technologies
Introduction
Condoms have long been considered a gold standard for HIV prevention. Consistent and correct condom use is a highly effective strategy to reduce the risk of HIV transmission among vulnerable populations (Smith DK, 2015). However, despite wide and prolonged public awareness efforts, condomless anal intercourse (CLAI) remains an inherent risk of HIV transmission for men who have sex with men (MSM) and transgender women (TGW), populations bearing the brunt of the global HIV epidemic (Fettig, Swaminathan, Murrill, & Kaplan, 2014; Hallett, Smit, Garnett, & de Wolf, 2011).
In Thailand, CLAI remains the primary driver of the HIV epidemic among MSM who account for approximately 41% of new HIV infections (Thai National AIDS Committee, 2014). Biomedical interventions such as pre-exposure prophylaxis (PrEP), post-exposure prophylaxis (PEP) and antiretroviral medications (ART) are increasingly accessible, and have demonstrated expanding evidence of effectiveness to prevent HIV transmission and reduce disease progression (Chomchey et al, 2017; Zablotska et al, 2016).
To reverse the pandemic, it is vital to determine how best to integrate all available prevention strategies - behavioural, biomedical and structural, with special focus on delivering risk reduction counseling in non-judgmental and non-stigmatizing settings to reinforce safe behaviors. To date, behavior change interventions such as offline motivational interviewing, peer-led education and outreach program together with condom distribution have commonly been deployed in Thailand, and to an extent proven effective means of reducing sexual risks among MSM and TGW (Pawa et al, 2013; Rongkavilit et al, 2013; Sherman, Sutcliffe, Srirojn, Latkin, Aramratanna, & Celentano, 2009). However, their in-person mode of service delivery limits the reach, engagement and impact, especially among stigmatized populations, and calls for more innovative modes of intervention delivery.
Thais, especially MSM spend highest time online, both on their personal computers (PCs) and smartphones, more than any other nation (Leesa-nguansuk, 2018). To date, novel interventions harnessing the potential of Internet and communications technologies have shown impact in engaging previously unreached Thai MSM, seamlessly linking them to offline HIV services and retaining them in HIV cascades (Phanuphak et al., 2018; Anand et al., 2017; Anand et al., 2017; Anand et al., 2015). However, unlike in the US (Hightow-Weidman, LeGrand, Simmons, Egger, Choi, & Muessig, 2017; Hightow-Weidman et al, 2012), technology-based HIV risk reduction interventions targeting Thai MSM remain scarce and research on their impact in encouraging behavior change is relatively unexplored (Nugroho, Erasmus, Zomer, Wu, & Richardus, 2017).
Asynchronous online discussion has become one of the major means of supporting learning in online environments, especially in health care education (Kleftodimos & Evangelidis, 2016; Gao, 2014). Given, surging technology adoption and utilization rates among Thai MSM, interventions such as asynchronous video discussions with demonstrated learning impact (Agarwala, Hsiao, Chae, & Natriello, 2012) could have immense potential in engaging online MSM in sexual health and behavior change discussions, enable enriched experiences and longer consultation periods, primary challenges faced in offline interventions.
We leveraged a randomized control trial of technology-based HIV risk reduction intervention using ‘Vialogues’ (www.vialogues.com) asynchronous video discussion tool and tested empirical evidence of intervention impact for supporting retention in HIV testing and behavior change among Thai MSM. Evidence of the impact of the intervention in reducing HIV risk behaviors and factors associated with CLAI are reported.
Methods
Overall study design
We conducted a 12-monthly randomized controlled two arm trial, with six-monthly visits to compare retention rates in HIV testing (primary outcome), and changes in HIV/AIDS knowledge, behavioral intentions, attitudes and extent of motivation for engaging in safer sexual behaviors, condom use self-efficacy (person’s ability to negotiate condom use), and sexual risk and substance use behaviors among participants receiving private clinic-based HIV counseling and testing and a monthly technology-based HIV risk reduction intervention (intervention arm) with those receiving clinic-based HIV counseling and testing alone (control arm). Outcome measures were assessed at month-6 and month-12 during the one-year follow-up period. The Institutional Review Board (IRB) of the Faculty of Medicine, Chulalongkorn University in Bangkok, Thailand approved the study protocol number IRB No.539/58. All participants were reimbursed $15 per study visit.
Recruitment and eligibility criteria
Between April 2016 to August 2017, Adam’s Love (www.adamslove.org) eCounseling and private clinic staffs approached via telephone HIV-negative MSM and TG participants who were existing clients of the Thai Red Cross Anonymous Clinic in Bangkok. Eligibility criteria included, 1) Thai national aged 18 and above, 2) being MSM and TG women, 3) not known to be HIV-positive at the time of enrollment and 4) ever engaged in unprotected anal sex or had three or more partners in the past 6 months. Participants interested in enrolling into the study scheduled their baseline clinic visit with the clinic staffs.
Randomization, informed consent process, and enrolment
Participants meeting preliminary criteria visited the private clinic and provided informed consent. Participants were randomized using simple randomization procedures (computerized random numbers) and randomly assigned, using concealed allocation to intervention arm (n=37) and control arm (n=39). Randomization occurred after informed consent and was revealed to participants by the clinic staff during a face-to-face session at the clinic.
The sample size calculation was estimated based on the primary objective of the study and assuming proportions of repeat HIV testing in every 6 months for the intervention group and control group are 90% and 65%, respectively, a sample size of 100 (intervention group =50, control group =50) will ensure that a two-sided test with alpha =0.05 has at least 80% power to detect this difference. Our final sample size (n=76) was lower than projected because of eligible participants declining to enroll in the study, primarily due to reasons including scheduling conflicts and greater time commitments needed to engage in the intensive 12-monthly Vialogues intervention sessions with the online counselors.
Data collection and study measures
Participants completed a baseline questionnaire at the clinic using Qualtrics software which solicited information on socio-demographic characteristics, risk behavior, technology use and time spent using internet/day, online sex seeking behavior, HIV/STI testing history, attitudes towards HIV prevention, substance use and condom use behavior. Follow-up questionnaires were conducted at six and 12 months after enrollment, at the clinic visit.
Study intervention delivery and follow-up
Intervention arm participants received once per month online intervention over the one year study period which included online video-based, monthly HIV/sexually transmitted infections (STI) prevention awareness and educational sessions integrated with behavioral change counseling, psychosocial support services and risk reduction strategies delivered via Vialogues video and discussion tool (www.vialogues.com) (EdLab, 2010) (Box 1).
Box 1. How to “Vialogues”.
Vialogues (vialogues.com), derived from “video dialogues”, is an asynchronous Video discussion and interaction platform which can be used for leveraging digital videos for learning by adding group interaction as part of the online video experience. Vialogues lets users upload videos (file formats supported are: .mov, .flv, .mp4, .mpeg, and .avi.) as well as use videos from sources such as YouTube. Video information component along with message transmission differentiates Vialogues from other video buffering software such as YouTube.
Questions can be posted at certain points of the video and the range of question types includes multi-choice (poll) as well as open-ended (text) questions. Private weblinks enable restricting questions/answers to a particular group. User created Vialogues appear in a list on the right side of the screen under My Vialogues upon initial log on, and clicking on the red Vialogues speech bubble takes one back to the home page with users listed Vialogues.
Four key steps:
Create: To get started, study counselor added YouTube links from existing Adam’s Love expert advise YouTube channel (https://www.youtube.com/user/AdamsLoveThailand/videos)
Invite: Counselor invite the participants to join the Vialogue session and added to the Vialogues main room
Watch: Participant and counselor start watching the selected video
Interact: Counselor encourage conversations over the video by adding timestamped comments, and surveys, to the discussion with participants. Time-code clicks helped reference to specific video fragment and the comment.
Implementation and essential components of the intervention
Two key features of Adam’s Love technology-based HIV risk reduction intervention included:
Online video-based 12-monthly educational sessions delivered using asynchronous ‘Vialogues’ video and discussion platform (Box 1). The videos focused on increasing participants’ HIV prevention and transmission awareness and reducing risk behaviors, and was developed based on critical analysis of the sexual health topics, commonly asked questions and inquiries by Thai MSM on Adam’s Love eCounseling and support platforms (Anand et al., 2015). Each session featured two Adam’s Love medical and community expert advise videos, with video topics selected from Adam’s Love educational video resources (youtube.com/adamslovethailand), and
eCounseling and asynchronous discussions with a health educator during the Vialogues sessions focused on deepening STI/HIV knowledge, improve correct and consistent condom use, reduce sexual risks, and set long-term goals to utilize knowledge and skills learned during the session.
How to “Vialogues”
At baseline clinic visit, the participants randomized to intervention arm were assisted by the study staffs to create a ‘Vialogues’ account using pseudoname to ensure privacy, added to the main study ‘Vialogues’ room and briefly trained on how to access and participate in 12-monthly video sessions. The staffs felt this step was necessary as none of the participants had prior experience with the ‘Vialogues’ tool. The intervention was designed to support risk reduction behaviors by increasing the client’s perception of personal risks. The counselor scheduled online appointment for Vialogues video and discussion session using phone call and instant messaging application (LINE, Line Corporation, Japan) at the beginning of each month and engaged in an interactive video discussion and conversation with the client to: 1) expose clients to a HIV awareness videos delivered by medical/community experts and encourage participants to inquire and determine what behaviors place the client at risk for HIV (or STIs); 2) use a “teachable moment” to engage in conversation, reduce myths and increase the client’s perception about HIV risk; and 3) reinforce safe behaviors and offer support when needed.
Statistical analysis
All statistical analysis was performed using Stata version 14 (Stata Corporation, College Station, Texas, USA). Descriptive statistics were performed to describe baseline characteristics among study groups of participants. Frequencies, percentages, mean (standard deviation, SD) and median (interquartile range, IQR) were provided according to nature of the variables. The differences in behavioral outcomes between the intervention and control groups were assessed using standard statistical comparison tests (the chi-square test or the Fisher’s exact test for categorical variables and two-sample t-tests or Wilcoxon Rank-Sum tests for continuous variables as appropriate). To assess the change in behavioral outcomes over time, we used a generalized estimation equation (GEE) approaches. Logistic regression was performed to investigate the relationship between selected predictors and having no CLAI. Odds ratios (OR) and 95% confidence intervals (CI) were calculated. The threshold for statistical significance was set at p < 0.05.
Results
Among 172 participants approached to participate in the study, 26 (15.1%) did not meet the study inclusion criteria, and 70 eligible MSM and TG (40.7%) declined to participate primarily due to reasons including scheduling conflicts and greater time commitments needed to engage in the intensive 12-monthly Vialogues intervention sessions with the online counselors. Of 76 participants, including 75 MSM and one TGW, successfully enrolled in the study, 37 were randomized to intervention and 39 to control arm, and received HIV testing at baseline. In the intervention arm, one participant changed phone number without informing study staffs and was lost to follow-up. In the control arm eight participants were lost to follow-up for reasons including being no longer interested, changed contact number or moved to another province (Figure 1).
Figure 1.
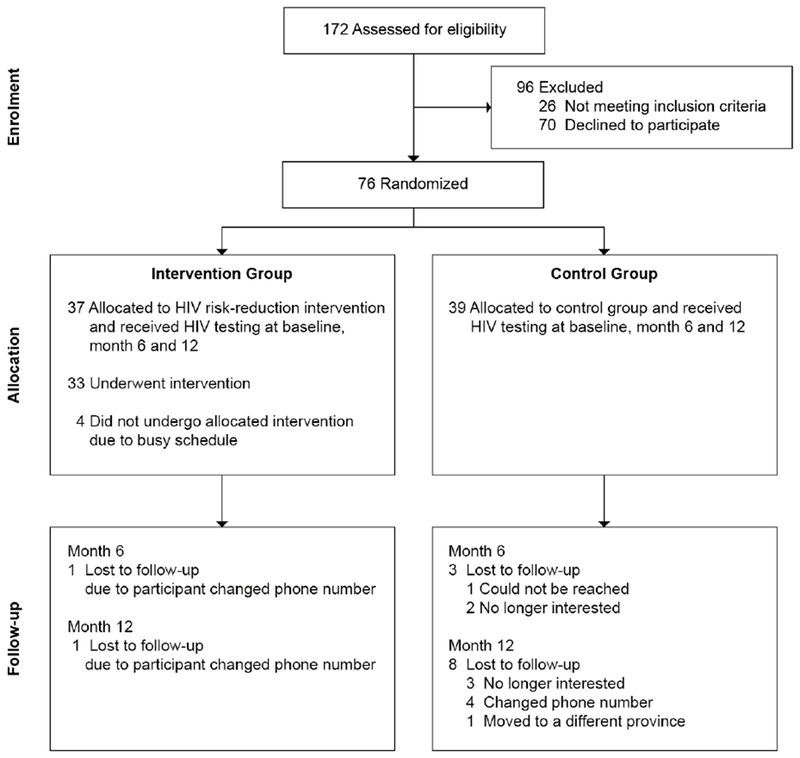
Study CONSORT flow diagram
Baseline socio-demographics and risk behaviors
Overall, the random allocation produced comparable intervention and control study groups (Table 1). Median (IQR) age was 28 (24-32) years and 89.5% had a bachelor degree or higher. Around half (46%) reported spending more than 7 h per day on the Internet, mainly through smartphones (89.5%). Majority (>60%) had ever sought sex online, mostly via applications. Almost half (42.5%) of the participants had been diagnosed with STI in the past reflecting a high-risk population.
Table 1.
Basic sociodemographic, technology use, HIV/STI testing of samples at baseline
| Baseline (N=76) | Total (N=76) | Control (N=39) | Intervention (N=37) | p-value |
|---|---|---|---|---|
| Socio-demographics | ||||
| Age | ||||
| Minimum, Maximum | 21, 49 | 22, 41 | 21, 49 | |
| Median (IQR) | 28 (24-32) | 27 (25-33) | 28 (24-32) | 0.44c |
| Education | 0.28b | |||
| High school | 5 (6.6) | 3 (7.7) | 2 (5.4) | |
| Diploma | 3 (3.9) | 3 (7.7) | 0 (0) | |
| Bachelor’s degree | 61 (80.3) | 31 (79.5) | 30 (81.1) | |
| Master’s degree or higher | 7 (9.2) | 2 (5.1) | 5 (13.5) | |
| Occupation | 0.022b | |||
| Unemployed | 2 (2.6) | 1 (2.6) | 1 (2.7) | |
| Student | 9 (11.8) | 2 (5.1) | 7 (18.9) | |
| Full-time worker | 39 (51.3) | 18 (46.2) | 21 (56.8) | |
| Part-time worker | 1 (1.3) | 0 (0) | 1 (2.7) | |
| Freelancer | 14 (18.4) | 12 (30.8) | 2 (5.4) | |
| Own business | 11 (14.5) | 6 (15.4) | 5 (13.5) | |
| Monthly income | 0.07b | |||
| No salary as studying | 9 (11.8) | 2 (5.1) | 7 (18.9) | |
| No salary as unemployed | 2 (2.6) | 1 (2.6) | 1 (2.7) | |
| ≤500 USD | 4 (5.3) | 1 (2.6) | 3 (8.1) | |
| 501-1,000 USD | 28 (36.8) | 20 (51.3) | 8 (21.6) | |
| 1,001-1,500 USD | 21 (27.6) | 10 (25.6) | 11 (29.7) | |
| ≥1,500 USD | 12 (15.8) | 5 (12.8) | 7 (18.9) | |
| Relationship status | 0.65b | |||
| Not in relationship | 42 (55.3) | 19 (48.7) | 23 (62.2) | |
| In serious relationship | 26 (34.2) | 15 (38.5) | 11 (29.7) | |
| Seeing someone | 1 (1.3) | 1 (2.6) | 0 (0) | |
| Multiple relationship | 7 (9.2) | 4 (10.3) | 3 (8.1) | |
| Technology use | 0.87b | |||
| Time spent using Internet/day | ||||
| 1-3 hours a day | 8 (10.5) | 4 (10.3) | 4 (10.8) | |
| 3-5 hours a day | 20 (26.3) | 11 (28.2) | 9 (24.3) | |
| 5-7 hours a day | 13 (17.1) | 6 (15.4) | 7 (18.9) | |
| More than 7 hours a day | 26 (34.2) | 12 (30.8) | 14 (37.8) | |
| Online on the mobile phone all the time | 9 (11.8) | 6 (15.4) | 3 (8.1) | |
| Technology devices used | 0.92b | |||
| Smartphone | 68 (89.5) | 35 (89.7) | 33 (89.2) | |
| Laptop | 3 (3.9) | 1 (2.6) | 2 (5.4) | |
| Personal computer | 4 (5.3) | 2 (5.1) | 2 (5.4) | |
| Tablet | 1 (1.3) | 1 (2.6) | 0 (0) | |
| Health seeking behaviors | ||||
| Don’t use internet for health in 3 months | 21 (27.6) | 13 (33.3) | 8 (21.6) | 0.25a |
| Search about HIV/STI information | 33 (43.4) | 16 (41) | 17 (45.9) | 0.67a |
| Search about general health information | 49 (64.5) | 24 (61.5) | 25 (67.6) | 0.58a |
| Online chat group about health | 18 (23.7) | 8 (20.5) | 10 (27) | 0.50a |
| Receive reminder or message about health | 4 (5.3) | 1 (2.6) | 3 (8.1) | 0.35b |
| Online sex seeking behaviors | ||||
| Have ever seek sex online | 46 (60.5) | 24 (61.5) | 22 (59.5) | 0.85a |
| Application used for seeking sex online (for those who have ever seek sex online only) | ||||
| Jack’d | 26 (56.5) | 11 (45.8) | 15 (68.2) | 0.13a |
| Grindr | 20 (43.5) | 6 (25) | 14 (63.6) | 0.008a |
| 18 (39.1) | 12 (50) | 6 (27.3) | 0.12a | |
| Blued | 11 (23.9) | 7 (29.2) | 4 (18.2) | 0.38a |
| Hornet | 9 (19.6) | 4 (16.7) | 5 (22.7) | 0.72b |
| Postjung | 5 (10.9) | 0 (0) | 5 (22.7) | 0.019b |
| GThai.net | 3 (6.5) | 0 (0) | 3 (13.6) | 0.10b |
| Palm Plaza | 3 (6.5) | 0 (0) | 3 (13.6) | 0.10b |
| Camfrog | 2 (4.3) | 0 (0) | 2 (9.1) | 0.22b |
| Beetalk | 2 (4.3) | 2 (8.3) | 0 (0) | 0.49b |
| 2 (4.3) | 1 (4.2) | 1 (4.5) | >0.99b | |
| 1 (2.2) | 0 (0) | 1 (4.5) | 0.48b | |
| Frequency in seeking sex online (for those who have ever seek sex online only) | 0.88b | |||
| Several times a day | 4 (8.7) | 3 (12.5) | 1 (4.5) | |
| About once a day | 6 (13) | 4 (16.7) | 2 (9.1) | |
| 3-5 days a week | 3 (6.5) | 1 (4.2) | 2 (9.1) | |
| 1-2 days a week | 13 (28.3) | 6 (25) | 7 (31.8) | |
| Once in few weeks | 9 (19.6) | 4 (16.7) | 5 (22.7) | |
| Once a month or less | 11 (23.9) | 6 (25) | 5 (22.7) | |
| HIV/STI testing history | ||||
| Last HIV test | 0.56b | |||
| Within 3 months | 24 (31.6) | 11 (28.2) | 13 (35.1) | |
| 3-6 months ago | 14 (18.4) | 7 (17.9) | 7 (18.9) | |
| 6-12 months ago | 30 (39.5) | 15 (38.5) | 15 (40.5) | |
| More than 12 months ago | 8 (10.5) | 6 (15.4) | 2 (5.4) | |
| Times of tested HIV in past year before joining Cascade study | ||||
| Minimum, Maximum | 0, 8 | 0, 8 | 1, 5 | |
| Median (IQR) | 2 (1-3) | 2 (1-3) | 2 (1-3) | 0.15c |
| Reason for previous HIV test | 0.22b | |||
| I test regularly | 34 (44.7) | 21 (53.8) | 13 (35.1) | |
| I got some risk exposure | 18 (23.7) | 6 (15.4) | 12 (32.4) | |
| I started new relationship | 10 (13.2) | 4 (10.3) | 6 (16.2) | |
| I had STI | 5 (6.6) | 4 (10.3) | 1 (2.7) | |
| My partner disclose his HIV-positive status to me | 4 (5.3) | 2 (5.1) | 2 (5.4) | |
| I had symptoms of HIV | 2 (2.6) | 1 (2.6) | 1 (2.7) | |
| I got some information about HIV testing | 2 (2.6) | 0 (0) | 2 (5.4) | |
| Because of work | 1 (1.3) | 1 (2.6) | 0 (0) | |
| Have ever tested for STI | 73 (96.1) | 36 (92.3) | 37 (100) | 0.24b |
| Last HIV test (for those who have ever tested for STI only) | 0.41b | |||
| Within 3 months | 19 (26) | 7 (19.4) | 12 (32.4) | |
| 3-6 months ago | 11 (15.1) | 6 (16.7) | 5 (13.5) | |
| 6-12 months ago | 33 (45.2) | 16 (44.4) | 17 (45.9) | |
| More than 12 months ago | 10 (13.7) | 7 (19.4) | 3 (8.1) | |
| Ever diagnosed with STI (for those who have ever tested for STI only) | 0.96b | |||
| None | 42 (57.5) | 20 (55.6) | 22 (59.5) | |
| Genital or anal warts | 10 (13.7) | 4 (11.1) | 6 (16.2) | |
| Chlamydia | 9 (12.3) | 5 (13.9) | 4 (10.8) | |
| Syphilis | 7 (9.6) | 4 (11.1) | 3 (8.1) | |
| Gonorrhea | 4 (5.5) | 2 (5.6) | 2 (5.4) | |
| Genital herpes | 1 (1.4) | 1 (2.8) | 0 (0) |
P-values are from Chi-square test
P-values are from Fisher’s Exact test
P-values are from Two-sample Wilcoxon rank-sum (Mann-Whitney) test
IQR, interquartile range; USD, United States dollar; STI, sexually transmitted infections.
Retention rates at month 6, and month 12 clinic visit
Almost all (97.3%) intervention arm participants completed month 6 clinic visit and received HIV testing as compared to 92.3% participants from the control arm (p=0.62). At month 12, intervention arm had significantly higher clinic visit retention rates versus control arm (97.3% vs. 79.5%, p=0.029) (Table 2). Among 37 intervention arm participants, 33 participants (89.2%) received all of the intervention components. Duration for Vialogues session varied between 20 and 180 min per participant (mean 37.45 minutes, SD 6.9). Almost one-third (30%) of participants preferred to do Vialogues between 18.00 – 21.00 h.
Table 2.
Visit attendance by study arm
| Follow up visit | Control group (N=39) | Intervention group (N=37) | P-values [1] |
|---|---|---|---|
| Month 6 | 0.62 | ||
| Visit shows | 36 (92.3) | 36 (97.3) | |
| Visit no-shows | 3 (7.7) | 1 (2.7) | |
| Month 12 | 0.029 | ||
| Visit shows | 31 (79.5) | 36 (97.3) | |
| Visit no-shows | 8 (20.5) | 1 (2.7) |
P-values are from Fisher’s exact test to compare proportions between two arms
Changes in behavioral outcomes among intervention and control arm subjects at baseline, month 6, and month 12 clinic visit
Both control and intervention arm participants exhibited high knowledge and awareness of HIV/AIDS at baseline, which remained unchanged during the study (Table 3).
Table 3.
Changes in behavioral outcomes among Participants at Baseline, and Six and 12-Months Post-Intervention
| Variable | Baseline | 6 month | 12 month | p-valuee | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Control (N=39) | Intervention (N=37) | p-value | Control (N=36) | Intervention (N=36) | p-value | Control (N=31) | Intervention (N=36) | p-value | Control | Intervention | |
|
HIV/AIDS Knowledge (total scores =16) |
|||||||||||
| Mean scores | 14.3 | 14.1 | 0.647c | 14.3 | 14.3 | 0.923c | 14.0 | 14.2 | 0.523c | 0.155 | 0.864 |
| % of items correctly answered | 89.1% | 88.3% | 0.647c | 89.2% | 89.1% | 0.923c | 87.3% | 88.5% | 0.523c | 0.155 | 0.864 |
|
Self-perceived risk for HIV/AIDS (low to high risk) |
2.98 | 3.08 | 0.551c | 2.75 | 2.74 | 0.966c | 2.74 | 2.60 | 0.459c | 0.055 | 0.001 |
|
Attitudes towards condom use (negative to positive attitude) |
3.87 | 4.01 | 0.398c | 4.11 | 3.97 | 0.362c | 3.90 | 4.07 | 0.286c | 0.025 | 0.707 |
|
Condom use self-efficacy (low to high efficacy) |
4.11 | 4.19 | 0.448c | 4.26 | 4.24 | 0.828c | 4.14 | 4.20 | 0.671c | 0.103 | 0.852 |
|
Behavioral intentions (not safe to safe) |
3.94 | 3.79 | 0.295c | 3.93 | 3.92 | 0.941c | 3.88 | 3.93 | 0.718c | 0.840 | 0.138 |
|
Sexual Risk Scale Norms (low to high strength) |
3.73 | 3.87 | 0.379c | 3.92 | 3.85 | 0.583c | 3.76 | 3.87 | 0.526c | 0.105 | 0.975 |
| Sexual risk behaviors | |||||||||||
| Have ever seek sex online | 61.5% | 59.5% | 0.853a | 58.3% | 44.4% | 0.238a | 61.3% | 44.4% | 0.169a | 0.875 | 0.017 |
| Median number of partners in the past 3 months | 2 | 2 | 0.548d | 2 | 1.5 | 0.161d | 2 | 1 | 0.124d | 0.046 | 0.003 |
|
Condom use percent/episodes (Receptive/Insertive/Both) |
|||||||||||
| Total | N=34 | N=33 | N=35 | N=33 | N=27 | N=33 | |||||
| Median percent | 100% | 88.9% | 0.428d | 93.3% | 100% | 0.520d | 93.3% | 100% | 0.023d | 0.676 | 0.006 |
| With unknown status partner | N=26 | N=25 | N=29 | N=23 | N=19 | N=21 | |||||
| Median percent | 100% | 100% | 0.377d | 100% | 100% | 0.389d | 100% | 100% | 0.039d | 0.630 | 0.107 |
| With Positive partner | N=2 | N=4 | N=3 | N=2 | N=1 | N=2 | |||||
| Median percent | 100% | 84.2% | N/A | 100% | 100% | N/A | 100% | 100% | N/A | 0.472 | 0.255 |
| With Negative partner | N=17 | N=19 | N=18 | N=15 | N=11 | N=16 | |||||
| Median percent | 93.3% | 94.4% | 0.828d | 67.5% | 66.7% | 0.808d | 55.6% | 100% | 0.080d | 0.416 | 0.236 |
| Drug use | |||||||||||
| Smoking | 15.4% | 16.2% | 0.921a | 11.1% | 16.7% | 0.496a | 6.5% | 16.7% | 0.270b | 0.475 | 0.969 |
| Alcohol | 56.4% | 70.3% | 0.211a | 50% | 61.1% | 0.343a | 54.8% | 61.1% | 0.604a | 0.739 | 0.525 |
| Any drug (not including smoking and alcohol) | 20.5% | 35.1% | 0.154a | 25% | 33.3% | 0.437a | 19.4% | 25.0% | 0.580a | 0.721 | 0.334 |
| Poppers | 15.4% | 29.7% | 0.134a | 19.4% | 11.1% | 0.326a | 12.9% | 13.9% | >0.999b | 0.204 | 0.002 |
| ATS | 0% | 13.5% | 0.024b | 2.8% | 11.1% | 0.357b | 0% | 13.9% | 0.057b | N/A | 0.825 |
Chi-square test was used to compare proportions between arms
Fisher’s exact test was used to compare proportions between arms
Two-sample t-test was used to compare means between arms
Wilcoxon rank-sum (Mann-Whitney) test was used to compare medians between arms
Generalized estimation equation (GEE) was used to investigate the longitudinal trends
At month 6, change in median percentage of condom use for anal intercourse did not differ between the control vs. intervention arms (p=0.52). At month 12, the median percentage of condom use for anal intercourse was higher in the intervention versus control arm (100% vs. 93.3%, p=0.023). Over the 12-month period, intervention arm reported significant reduction in self-perceived risk for HIV (3.08 on 5-point LIKERT scale to 2.6, p=0.001), popper usage (29.7% to 13.9%, p=0.002), seeking sex online (59.5% to 44.4%, p=0.017), median number of sexual partners in the past three months (2 to 1, p=0.003), and increased median percentage of condom use (88.9% to 100%, p=0.006). There were no significant changes in attitudes towards condom use, condom use self-efficacy, intentions to use condoms, sexual risk norms, and substance use behaviors among intervention arm participants. No significant behavioral changes were reported at month-12 among control arm participants.
Logistic regression for association between selected predictors and no CLAI in the past 3 month (reported at month 12 visit)
In a multivariate logistic regression model analysis (Table 4), having less than four episodes of sexual intercourse (aOR 4, 95%CI 1.1-13.8, p=0.031) and being randomized to intervention arm (aOR 3.8, 95%CI 1.1-12.7, p=0.032) were predictors independently associated with having no CLAI in the last three months. Sociodemographic characteristics, HIV/AIDS knowledge, attitudes (self-perceived risk for HIV/AIDS, attitudes towards condom use and condom use self-efficacy), and not using substance were not associated with having no CLAI.
Table 4.
Logistic regression for association between selected predictors and No CLAI in the past 3 month (reported at month 12 visit)
| Predictors | Bivariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | p-value | Adjusted Odds Ratio | 95% CI | p-value | |
| Socio-demographics (at baseline visit) | ||||||
| Age | ||||||
| ≤ 28 years old | Ref. | |||||
| > 28 years old | 1.7 | 0.5-5.3 | 0.37 | |||
| Education | ||||||
| Less than bachelor’s degree | 1.9 | 0.2-18.7 | 0.56 | |||
| Bachelor’s degree or higher | Ref. | |||||
| Occupation | ||||||
| Unemployed/Student | 1.1 | 0.2-6.6 | 0.93 | |||
| Full-time worker | Ref. | |||||
| Freelancer / Own business / Part-time worker | 0.8 | 0.2-2.6 | 0.72 | |||
| Monthly Income | ||||||
| ≤ 500 USD / No salary | 1.5 | 0.3-9.3 | 0.64 | |||
| 501-1,000 USD | Ref. | |||||
| > 1,000 USD | 0.8 | 0.2-2.6 | 0.69 | |||
| Relationship status | ||||||
| Not in relationship | 1.8 | 0.6-5.3 | 0.32 | |||
| In relationship | Ref. | |||||
| Risk Behaviors | ||||||
| Seek sex online | ||||||
| No | Ref. | |||||
| Yes | 1.2 | 0.4-3.4 | 0.80 | |||
| Number of partners | ||||||
| Single partner | Ref. | |||||
| Multiple partners | 0.8 | 0.3-2.3 | 0.63 | |||
| Number of episodes of sexual intercourse* | ||||||
| 1-4 episodes | 4.4 | 1.3-14.5 | 0.016 | 4.0 | 1.1-13.8 | 0.031 |
| >4 episodes | Ref. | Ref. | ||||
| Substance use (include alcohol) | ||||||
| No | Ref. | |||||
| Yes | 1.3 | 0.4-3.9 | 0.70 | |||
| Attitudes | ||||||
| Self-perceived risk for HIV/AIDS | ||||||
| Mean or below (low risk) | Ref. | |||||
| Above mean (high risk) | 1.3 | 0.4-3.9 | 0.67 | |||
| Attitudes towards condom use | ||||||
| Mean or below (negative attitude) | Ref. | |||||
| Above mean (positive attitude) | 1.3 | 0.4-3.9 | 0.67 | |||
| Condom use self-efficacy | ||||||
| Mean or below (low efficacy) | Ref. | |||||
| Above mean (high efficacy) | 1.7 | 0.5-5.3 | 0.37 | |||
| Behavioral intentions | ||||||
| Mean or below (not safe) | Ref. | |||||
| Above mean (safe) | 1.3 | 0.4-3.9 | 0.63 | |||
| HIV/AIDS Knowledge | ||||||
| Mean or below (poor knowledge) | Ref. | |||||
| Above mean (good knowledge) | 1 | 0.3-2.9 | 0.94 | |||
| Arm* | ||||||
| Control | Ref. | Ref. | ||||
| Intervention | 4.2 | 1.3-13.4 | 0.016 | 3.8 | 1.1-12.7 | 0.032 |
For indicated predictors that were selected into multivariate analysis (p-value ≤ 0.20)
Intervention feasibility, acceptability and satisfaction
Process measures yielded high participant satisfaction of Vialogues (mean 4.67 on a 5-point scale, SD 0.48). Study team also conducted exit interviews with intervention participants at month 12-clinic visit. Some of the participants’ feedbacks include:
“Joining Vialogues with online counselor is a fun activity, I gain new knowledge every month. Interestingly, each monthly video session has its own significance, and so when I participate and engage in Vialogues, I am very focused and concentrate on the video and related dialogue with counselor” N.M., 22 years old MSM.
“Joining Vialogues gives me awareness about HIV and STI prevention, and actually helps me reduce my risk behaviors” P.P., 21 years old MSM.
“Engaging in Vialogues every month doesn’t disturb my daily life, it rather provides information that I didn’t know before joining this study” W.S., 21 years old MSM.
“I like that this study uses technology and social networking to engage participants in HIV knowledge and risk reduction counseling, it suits my generation needs and it’s very convenient” J.P., 25 years old MSM.
Discussion
Clinic visit and intervention level retention rates were high in the intervention arm in our study implying that Vialogues has the potential to be an effective strategy to retain MSM in routine HIV counseling and testing. Higher retention rates reported among intervention arm participants are consistent with previously conducted randomized trial of online interventions among MSM (Liu et al., 2018). The study results highlight that a technology-based HIV risk reduction intervention integrated with online counseling, psychosocial support services and risk reduction strategies has the potential to change behaviors, lower CLAI rates and reduce number of sexual partners among MSM with high baseline use of Internet. Our results are consistent with previous findings supporting that effective interventions increasing condom use comprise educational information and discussions of the positive implication of using condoms (Long et al., 2016; Johnson, Michie, & Snyder, 2014; Abraham, Johnson, de Bruin, & Luszczynska, 2014; Albarracín, Gillette, Earl, Glasman, Durantini, & Ho, 2005).
Having no CLAI was independently associated with being randomized to the intervention arm and having lesser episodes of sexual intercourse in the past 3 months. Interestingly in the US, a randomized trial of an online risk reduction intervention for young black MSM reported similar results with lower self-reported CLAI among the intervention group at 3 months; however, unlike Thai MSM in our study, behavioral changes among US black MSM were not sustained over 12 month period (Hightow-Weidman et al., 2019). In addition, our results are broadly aligned with the findings from RCTs in the Cochrane review by Johnson and colleagues (Johnson et al., 2008), and behavioral outcome literature by Kalichman and colleagues, confirming positive effects of HIV risk-reduction interventions (Kalichman, Carey, & Johnson, 1996).
There is a controversy in the literature about the inter-relations between perceived risk, knowledge, and risk behavior. Increased knowledge of HIV doesn’t always translate into protective behaviors (Ferrer et al, 2007; Braithwaite & Thomas, 2001; Salgado de Snyder, Díaz Pérez, & Maldonado, 1996) and knowledge alone is not sufficient to change risky behavior (Bandura A, 1990). Although our sample of MSM reported high levels of HIV/AIDS knowledge at baseline yet this did not translate into actual reduced risk behaviors. Participants perceived themselves to be at risk for and engaged in high-risk behaviors. Furthermore, although HIV/AIDS awareness measured by the baseline questionnaires was high, MSM participants specifically noted during clinical visits and qualitative interviews that Vialogues intervention helped enhance and deepen their practical knowledge on HIV risk behaviors they were previously unaware of, and safe sex measures they could adopt to prevent transmission.
It is widely acknowledged that changes in attitudes towards condom use influences condom use behaviors and perceived safer sex self-efficacy is associated with decreases in CLAI (Arnold, Struthers, McIntyre, & Lane, 2013; Harvey & Henderson, 2006). Paradoxically, in our study, although the intervention did not yield any significant changes in attitudes towards condom use, condom use self-efficacy, and behavioral intentions, participants reported significant reductions in number of sexual partners and increase in condom use behaviors. Significant reduction in popper usage among participants engaged in Vialogues has important implications for future design and delivery of interventions targeting popper-using Thai MSM, a population with high reported educational level and multiple sexual partners (Anand et al, 2017).
Being randomized to Intervention arm reduced CLAI among the participants as shown in both bivariate and multivariate models. Interestingly, a recent study at a Bangkok based clinic observed a significant reduction in sexual partners and a significant increase in condom use among acutely infected HIV positive Thai MSM, but couldn’t establish whether this was impacted by the behavioral counseling at the clinic (Kroon et al, 2017). Given emerging evidence, we propose that behavioral counseling interventions should be tailored for both online and offline delivery and their potential to reduce risk behaviors should be further assessed among both HIV-negative and positive MSM.
The technology-based intervention was acceptable, feasible and demonstrated impact. Also, intervention arm participants attended majority of the sessions, implying that such interventions are feasible and acceptable to be widely scaled-up in Thailand and in settings with similar epidemic among MSM and technology use. The intervention not only enriched online learning experiences but also successfully retained participants and created knowledge enhancing opportunities. Similar acceptability and feasibility outcomes, high quality of online participation and engagement rates were reported in a recently conducted randomized control trial of an electronically directly observed therapy (e-DOT) for optimizing PrEP adherence among Thai MSM (Anand et al., 2019).
Overall, the findings support the acceptability and feasibility of delivering this prevention program to a group that has few interventions despite bearing a significant burden of the epidemic. Tailored online interventions for this target group are long overdue, making ours a very timely study.
Limitations
Substance use behaviors except popper usage remained unaffected in our study pointing to the need for refining our technology-based intervention with special attention to substance users. Furthermore, although the intervention proved effective in short-term among a relatively small sample, we are uncertain whether it would sustain long-term safe sex behaviors. On a positive note, the randomized control trial provides first evidence of a technology based intervention in reducing HIV risk behaviors and has implications for reducing epidemic among MSM. Furthermore, the intervention has high potential to be scaled up in settings with similar epidemic and Internet and technology use among key populations.
Acknowledgements
The authors are extremely grateful to all our sponsors, and thank all research participants and study staff for their significant contributions.
The randomized control trial was supported by Aidsfonds. Funding support was provided in part by ViiV Healthcare, MAC AIDS Fund, amfAR and through a grant from the National Institute of Health’s National Institute of Allergy and Infectious Diseases, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Cancer Institute, National Institute of Mental Health, and National Institute on Drug Abuse as part of the International Epidemiology Databases to Evaluate AIDS (IeDEA; U01AI069907).
Footnotes
Publisher's Disclaimer: Disclaimer: The content and views in this manuscript are solely the responsibility of the authors and do not necessarily represent the views or policies of the funders of the study.
Competing interests: None.
Ethics approval: The study was approved by the Ethics Research Committee/Institutional Review Board (IRB) at Chulalongkorn University, Department of Medicine, Bangkok, Thailand.
References
- Abraham C, Johnson BT, de Bruin M, & Luszczynska A (2014). Enhancing reporting of behavior change intervention evaluations. J Acquir Immune Defic Syndr, 66 Suppl3, S293–9. doi: 10.1097/QAI.0000000000000231 [DOI] [PubMed] [Google Scholar]
- Agarwala M, Hsiat I, Chae HS & Natriello G (2012). Vialogues: videos and dialogues based social learning environment. In Proceedings of the 12th IEEE International Conference on Advanced Learning Technologies, ICALT 2012, p. 629–633 [6268195]. doi.org: 10.1109/ICALT.2012.127 [Google Scholar]
- Albarracín D, Gillette JC, Earl AN, Glasman LR, Durantini MR, & Ho MH (2005). A test of major assumptions about behavior change: a comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychol Bull, 131(6), 856–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anand T, Nitpolprasert C, Ananworanich J, Pakam C, Nonenoy S, Jantarapakde J, Phanuphak N (2015). Innovative strategies using communications technologies to engage gay men and other men who have sex with men into early HIV testing and treatment in Thailand. J Virus Erad, 1(2), 111–115. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4946676/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anand T, Nitpolprasert C, Trachunthong D, Kerr SJ, Janyam S, Linjongrat D, Phanuphak N (2017). A novel Online-to-Offline (O2O) model for pre-exposure prophylaxis and HIV testing scale up. J Int AIDS Soc, 20(1), 21326. doi: 10.7448/IAS.20.1.21326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anand T, Nitpolprasert C, Kerr SJ, Apornpong T, Ananworanich J, Phanuphak P, Phanuphak N (2017). Implementation of an online HIV prevention and treatment cascade in Thai men who have sex with men and transgender women using Adam’s Love Electronic Health Record system. J Virus Erad, 3(1), 15–23. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5337417/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anand T, Nitpolprasert C, Jantarapakde J, Pengnonyang S, Sungsing T, Rodbamrung P, Phanuphak N (2017). Comparison of HIV risks and HIV prevalence between poppers, amphetamine-type substance (ATS) and polydrug using Thai men who have sex with men and transgender women [Abstract TUPEC0764]. The 9th IAS Conference on HIV Science, 23-26 July 2017, Paris, France Retrieved from http://programme.ias2017.org//PAGMaterial/eposters/3641.pdf [Google Scholar]
- Anand T, Nitpolprasert C, Kerr SJ, Apornpong T, Jantarapakde J, Phomthong S, Phanuphak N (2019). Electronic directly observed therapy (e-DOT) for PrEP adherence among Thai men who have sex with men: a feasibility randomized controlled trial [Abstract P02/04]. HepHIV 2019 Conference, 28-30 January 2019, Bucharest, Romania Retrieve from https://www.hiveurope.eu/Portals/0/PO2_04.pdf [Google Scholar]
- Arnold MP, Struthers H, McIntyre J, & Lane T (2013). Contextual correlates of per partner unprotected anal intercourse rates among MSM in Soweto, South Africa. AIDS Behav, 17(0 1), S4–11. doi: 10.1007/s10461-012-0324-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A (1990). Perceived self-efficacy in the exercise of control over AIDS infection. Evaluation and Program Planning, 13(1), 9–17. doi: 10.1016/0149-7189(90)90004-G [DOI] [Google Scholar]
- Braithwaite K, & Thomas VG (2001). HIV/AIDS knowledge, attitudes, and risk-behaviors among African-American and Caribbean college women. International Journal for the Advancement of Counselling, 23(2), 115–129. doi: 10.1023/A:1010611328452 [DOI] [Google Scholar]
- Chomchey N, Woratanarat T, Hiransuthikul N, Lertmaharit S, Lohsoonthorn V, Teeratakulpisarn N, … Phanuphak N (2017). Factors associated with intention to take non-occupational HIV post-exposure prophylaxis among Thai men who have sex with men. J Virus Erad, 3(3), 128–139. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5518241/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- EdLab. (2010). Vialogues. New York, NY, United States: Teachers College, Columbia University; Retrieved from https://vialogues.com/ [Google Scholar]
- Ferrer L, Cianelli R, Guzman E, Cabieses B, Irarrázabal L, Bernales M, Araya A (2007). Chilean university students: knowledge and concern about HIV/AIDS. J Assoc Nurses AIDS Care, 18(5), 51–56. doi: 10.1016/j.jana.2007.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fettig J, Swaminathan M, Murrill CS, & Kaplan JE (2014). Global Epidemiology of HIV. Infect Dis Clin North Am, 28(3), 323–337. doi: 10.1016/j.idc.2014.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao F (2014) Exploring the use of discussion strategies and labels in asynchronous online discussion. Online Learning, 18(3). Retrieved from https://eric.ed.gov/?id=EJ1043164 [Google Scholar]
- Hallett TB, Smit C, Garnett GP, & de Wolf F (2011). Estimating the risk of HIV transmission from homosexual men receiving treatment to their HIV-uninfected partners. Sex Transm Infect, 87(1), 17–21. doi: 10.1136/sti.2010.042622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey SM, & Henderson JT (2006). Correlates of condom use intentions and behaviors among a community-based sample of Latino men in Los Angeles. J Urban Health, 83(4), 558–574. doi: 10.1007/s11524-006-9064-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hightow-Weidman L, LeGrand S, Simmons R, Egger J, Choi SK, & Muessig K (2017). healthMpowerment: effects of a mobile phone-optimized, Internet-based intervention on condomless anal intercourse among young black men who have sex with men and transgender women (Abstract WEPEC2001) 9th International Conference on HIV Science (IAS 2017) Paris, France. [Google Scholar]
- Hightow-Weidman LB, Pike E, Fowler B, Matthews DM, Kibe J, McCoy R, Adimora AA (2012). HealthMpowerment.org: feasibility and acceptability of delivering an internet intervention to young Black men who have sex with men. AIDS Care, 24(7), 910–920. doi: 10.1080/09540121.2011.647677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hightow-Weidman LB, LeGrand S, Muessig KE, Simmons RA, Soni K, Choi SK, … Egger JR (2019). A randomized trial of an online risk reduction intervention for young black MSM. AIDS Behav, 23(5), 1166–1177. doi: 10.1007/s10461-018-2289-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson BT, Michie S, & Snyder LB (2014). Effects of behavioral intervention content on HIV prevention outcomes: a meta-review of meta-analyses. J Acquir Immune Defic Syndr, 66 Suppl3, S259–70. doi: 10.1097/QAI.0000000000000235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson WD, Diaz RM, Flanders WD, Goodman M, Hill AN, Holtgrave D, McClellan WM (2008). Bahavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane Database of Systematic Reviews 2008, 3, CD001230. doi: 10.1002/14651858.CD001230.pub2 [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Carey MP, & Johnson BT (1996). Prevention of sexually transmitted HIV infection: a meta-analytic review of the behavioral outcome literature. Ann Behav Med, 18(1), 6–15. doi: 10.1007/BF02903934 [DOI] [PubMed] [Google Scholar]
- Kleftodimos A & Evangelidis GD An interactive video-based learning environment that supports learning analytics for teaching ‘image editing’. (2016). SE@VBL Workshop at LAK’ 2016, 26–33. Retrieved from http://ceur-ws.org/Vol-1579/paper5.pdf [Google Scholar]
- Kroon EDMB, Phanuphak N, Shattock AJ, Fletcher JLK, Pinyakorn S, Chomchey N, Wilson DP (2017). Acute HIV infection detection and immediate treatment estimated to reduce transmission by 89% among men who have sex with men in Bangkok. J Int AIDS Soc, 20(1), 21708. doi: 10.7448/IAS.20.1.21708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leesa-nguansuk S (2018. February 21). Thais lead world in online time. Retrieved from https://www.bangkokpost.com/archive/thais-lead-world-in-online-time/1408094
- Liu AY, Vittinghoff E, von Felten P, Amico KR, Anderson PL, Lester R, Fuchs JD (2018). Randomized controlled trial of a mobile health intervention to promote retention and adherence to pre-exposure prophylaxis among young people at risk for immunodeficiency virus: the EPIC study. Clin Infect Dis, Epub ahead of print. doi: 10.1093/cid/ciy810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long L, Abraham C, Paquette R, Shahmanesh M, Llewellyn C, Townsend A, Gilson R (2016). Brief interventions to prevent sexually transmitted infections suitable for in-service use: a systematic review. Prev Med, 91, 364–382. doi: 10.1016/j.ypmed.2016.06.038 [DOI] [PubMed] [Google Scholar]
- Nugroho A, Erasmus V, Zomer TP, Wu Q, & Richardus JH (2017). Behavioral interventions to reduce HIV risk behavior for MSM and transwomen in Southeast Asia: a systematic review. AIDS Care, 29(1), 98–104. doi: 10.1080/09540121.2016.1200713 [DOI] [PubMed] [Google Scholar]
- Pawa D, Firestone R, Ratchasi S, Dowling O, Jittakoat Y, Duke A, Mundy G (2013). Reducing HIV risk among transgender women in Thailand: A quasi-experimental evaluation of the Sisters program. PLoS ONE, 8(10), e77113. doi: 10.1371/journal.pone.0077113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phanuphak N, Anand T, Jantarapakde J, Nitpolprasert C, Hummad K, Sungsing T, Phanuphak P (2018). What would you choose: Online or Offline or Mixed services? Feasibility of online HIV counselling and testing among Thai men who have sex with men and transgender women and factors associated with service uptake. J Int AIDS Soc, 21 Suppl5, e25118. doi: 10.1002/jia2.25118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rongkavilit C, Naar-King S, Wang B, Panthong A, Bunupuradah T, Parsons JT, Phanuphak P (2013). Motivational interviewing targeting risk behaviors for youth living with HIV in Thailand. AIDS Behav, 17(6), 2063–2074. doi: 10.1007/s10461-013-0407-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salgado de Snyder VN, Díaz Pérez M, & Maldonado M (1996). AIDS: risk behaviors among rural Mexican women married to migrant workers in the United States. AIDS Educ Prev, 8(2), 134–142. Retrieved from https://www.popline.org/node/297507 [PubMed] [Google Scholar]
- Sherman SG, Sutcliffe C, Srirojn B, Latkin CA, Aramratanna A, & Celentano DD (2009). Evaluation of a peer network intervention trial among young methamphetamine users in Chiang Mai, Thailand. Soc Sci Med, 68(1), 69–79. doi: 10.1016/j.socscimed.2008.09.061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DK, Herbst JH, Zhang X, & Rose CE (2015). Condom effectiveness for HIV prevention by consistency of use among men who have sex with men in the United States. J Acquir Immune Defic Syndr, 68(3), 337–344. doi: 10.1097/QAI.0000000000000461 [DOI] [PubMed] [Google Scholar]
- Thai National AIDS Committee. (2014). 2014 Thailand AIDS response progress report, reporting period: 2012-2013. Bangkok, Thailand: Retrieved from http://files.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2014countries/THA_narrative_report_2014.pdf. [Google Scholar]
- Zablotska I, Grulich AE, Phanuphak N, Anand T, Janyam S, Poonkasetwattana M, Lo YR (2016). PrEP implementation in the Asia-Pacific region: opportunities, implementation and barriers. J Int AIDS Soc, 19(7(Suppl 6)), 21119. doi: 10.7448/IAS.19.7.21119 [DOI] [PMC free article] [PubMed] [Google Scholar]


