Abstract
BACKGROUND:
Developments in information technology (IT) have driven a push in healthcare innovation in the emergency department (ED). Many of these applications rely on mobile technology (MT) such as smartphones but not everyone is comfortable with MT usage. Our study aims to characterize the technology usage behavior of users in the ED so as to guide the implementation of IT interventions in the ED.
METHODS:
A cross-sectional survey was conducted in the emergency department of a tertiary hospital. Patients and their caregivers aged 21 and above were recruited. The survey collected demographic information, technology usage patterns, and participant reported comfort level in the usage of MT. We performed descriptive statistics and multivariate logistic regression to identify factors differentially associated with comfort in usage of MT.
RESULTS:
A total of 498 participants were recruited, and 299 (60%) were patients. English was the most commonly written and read language (66.9%) and 64.2% reported a comfort level of 3/5 or more in using MT. Factors that were associated with being comfortable in using MT include having a tertiary education, being able to read and write English, as well as being a frequent user of IT. Caregivers were more likely to display these characteristics.
CONCLUSION:
A large proportion of ED patients are not comfortable in the usage of MT. Factors that predicted comfort level in the usage of MT were common amongst caregivers. Future interventions should take this into consideration in the design of MT interventions.
KEY WORDS: Mobile health technology, Information technology, Emergency department
INTRODUCTION
Developments in information technology (IT) have driven a push in healthcare innovation, with IT being used in multiple areas of healthcare delivery including documentation, appointment reminders and tele- consultation. The usage of IT in healthcare delivery has the potential to facilitate cost savings, improved access and increased efficiency of utilization of healthcare resources.[1,2]
The existing literature have reported a potential utility of IT in the follow-up of patients with chronic diseases such as asthma, diabetic foot ulcers, and several other medical problems.[3-5] In the emergency department (ED), researchers have also utilized IT to assist in history taking while patients are waiting to see their providers.[6,7] In Singapore, telemedicine applications for acute care that have been described include telephone-based toxicology consultation services[8] as well as a maritime radio-medical consultation service.[9]
Possible uses of IT in the ED include using tele- consultation for follow-up of post discharge patients, using IT to facilitate patient triage, and also using tele-consultation for low acuity patients.[10-12] Many of these interventions may rely on mobile technology (MT) such as smartphones and tablets. However, IT has barriers to participation. For instance, language support for most IT systems are in English, and certain groups of patients might not be comfortable with the language nor able to utilize mobile devices or computers. This includes elderly patients who can form a large proportion of patients. This is particularly relevant in countries with ageing populations and a cosmopolitan makeup where populations speak multiple languages or dialects. However, to our knowledge, most published investigations often excluded patients who were unable to read or speak English.[13,14]
The ED is also a unique healthcare environment that sees a whole spectrum of users from all age groups, varying severity of illnesses and a wide range of socio-demographic backgrounds. Unlike in the clinic setting or inpatient setting where there might be more time for patient selection for MT interventions, healthcare providers who wish to develop such innovations in the ED might find it more challenging to identify the users who can participate in technological interventions.
This study aims to address these knowledge gaps to guide the implementation of IT in acute healthcare delivery by identifying the profiles of patients most amenable to IT-based interventions. The primary aim of this study is to characterize the technology usage behavior of patients and their caregivers from a multi-racial and multi-cultural population recruited in the ED of a tertiary hospital in Singapore. This is to answer the core question “can users of the ED participate in technology related interventions?”.
Secondary aims of this study are to describe the relationship between sociodemographic factors and patient-reported willingness to utilize MT, as well as to evaluate whether caregivers can form a potential target audience for MT. This will serve as a guide to physicians, researchers and innovators seeking to increase the uptake of such technologies in the ED.
METHODS
Study design and setting
A cross-sectional paper survey was conducted among patients and their caregivers presenting to the emergency department of a tertiary hospital in Singapore. This department sees approximately 120,000 patients yearly and serves a multi-racial population approximately 75% ethnic Chinese, 15% Malay, 7% Indian and others (3%). The study was approved by the institutional review board with a waiver of written consent (Singhealth CIRB Ref: 2018/2151) and all study procedures were performed in accordance with the declaration of Helsinki.
Study subjects
ED patients and caregivers aged 21 and above were eligible to participate. We excluded patients and caregivers if they were too ill as determined by the treating physician or if they were triaged to the critical care area of our department.
Study procedures
We enrolled a convenience sample of patients based on study team member availability. Enrollment spanned any time of the day on any day of the week. Consecutive patients and their caregivers were screened immediately after triage and were provided with information regarding the survey in the language of their choice. No patient data was collected on those who declined participation in the study. Willing participants were given a survey form in English to fill up.
Participants comfortable with the English language proceeded with the study as a self-administered survey. Participants not comfortable with the English language proceeded with the study as an interviewer-administered survey administered by the recruiting study team member with the assistance of a translator (where the study team member was not comfortable with the requested language). To mitigate problems of translation errors, team members were briefed on the survey and the questions.
Questionnaire
The survey was developed based on existing validated survey questions[15] and anecdotal evidence from consultation with senior consultant emergency department specialists. Data collected include patient demographics as well as participant-reported comfort level in the usage of the English language, current use of technology as well as comfort level in the usage of MT.
The survey was piloted on a random sample of 10 adults to seek input on clarity, formatting and phrasing, with changes made accordingly before recruitment was initiated.
Data analysis
Statistical analysis was conducted using SPSS version 23. Participant responses were analyzed and presented using descriptive statistics. Chi-square test was used to investigate for associations between participant-reported comfort level in the usage of MT and their socio- demographic factors. Stratified analysis was conducted based on age and identity of the individual surveyed (patient versus caregiver). To adjust for multiple testing with 9 independent variables, we set the significance at a P value of 0.005 using the Bonferroni correction.
Multivariate logistic regression analysis was conducted to identify factors associated with participant-reported comfort level in using MT. This was defined as a participant response of 3/5 and above for the statement, “I am comfortable using English to send and receive information via my mobile device/ computer”. Our hypothesis was that age would be the single socio-demographic factor that will have a significant association with participant-reported willingness to utilize MT.
For the purpose of analysis, age was converted into a categorical variable with ages 21–40, 41–60 and 60 and above. “Frequent IT user” was defined as someone who reported using the Internet, checking their emails, and using social media an average of at least once a day.
Further subgroup analysis was also conducted on the subgroup of patients who read/ write English and own a mobile phone to identify factors associated with reported comfort level in using MT.
RESULTS
From March 2018 to December 2018, 498 participants completed the survey. Table 1 shows the demographics of our study population, with further categorization by age and role. Totally 299 (60%) of participants were patients and 199 (40%) were caregivers. Amongst the patients, roughly half came to the ED alone (49.8%, 149/498). Amongst those who came to the ED with a caregiver, a majority stayed with their caregiver (76%, 114/150).
Table 1.
Characteristics and language usage of survey participants, n (%)
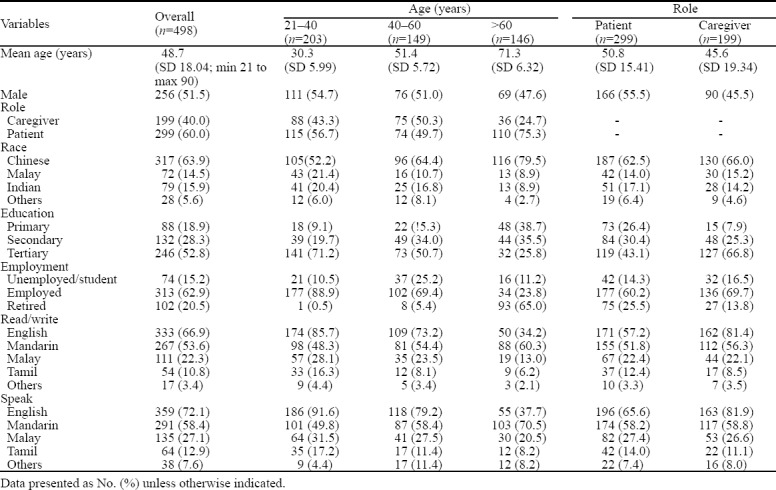
Overall, English was the most commonly written and read language (66.9%, 333/498). However, amongst participants older than 60 years old, Mandarin was more commonly written and read (Mandarin 60.3%, 88/146 vs. English 34.2%, 50/146).
Mobile phone ownership was high at 94.4% (n=470) while smartphone ownership was lower at 76.1% (n=378). About 72.6% (n=361) participants reported being able to access and use the Internet at all times. Older participants reported lower baseline technology use, especially those above 60 (Table 2).
Table 2.
Baseline technology use and comfort level in technology use, n (%)
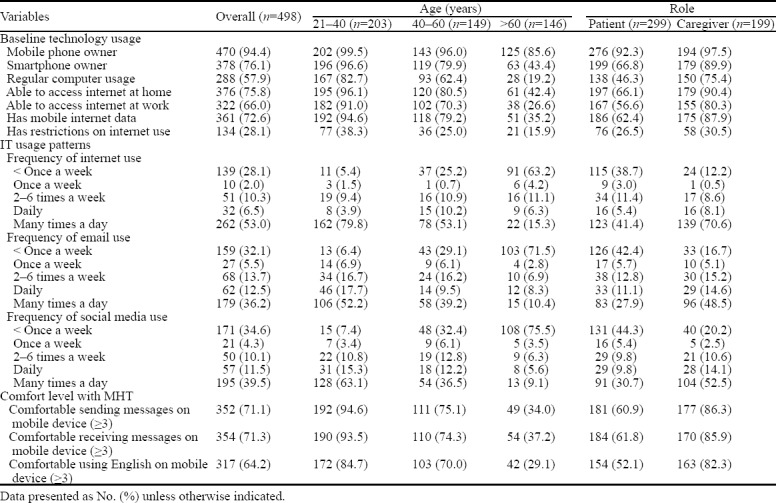
About 71.1% (n=352) of participants were comfortable with sending information via mobile technology, while 71.3% (n=354) were comfortable with receiving information (Table 2). However, fewer participants (64.2%, n=317) were comfortable doing the above in English.
Compared with patients, caregivers were more likely to have a tertiary education (patients 43.1% 119/299 vs. caregivers 66.8% 127/199), read and write English (patients 57.2% 171/299 vs. caregivers 81.4% 162/199), as well as to own a smartphone (patients 66.8% 199/299 vs. caregiver 89.9% 179/199). Patients also reported lower baseline technology use (Table 2).
On univariate analysis (Table 3), several demographic factors were significantly associated with being comfortable in using MT, including being a caregiver (P=0.001), age <60 (P=0.001) and having a tertiary education (P=0.001). Being able to read and write English (P=0.001), owning a mobile phone (P=0.001) and being able to access the internet at all times (P=0.001) were also significantly associated with being comfortable in using MT.
Table 3.
Comfort level in MT usage, based on demographic characteristics (n=498), n (%)
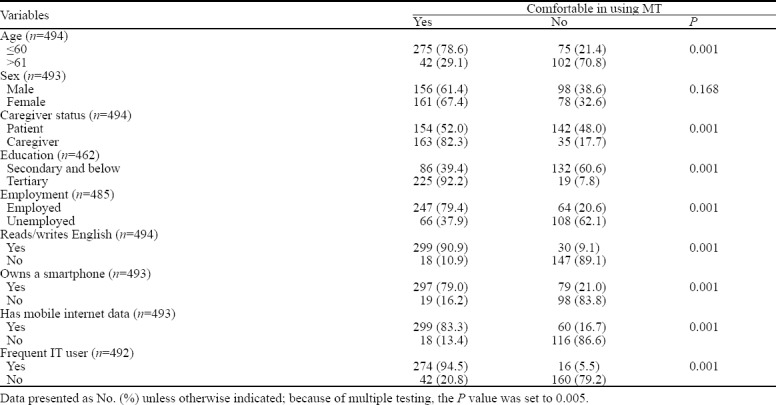
On multivariate analysis (adjusting for demographic variables, language use as well as IT usage), having a tertiary education, being able to read and write English, having mobile internet data as well as being a frequent user of IT remained significant for comfort in using MT.
On subgroup analysis of participants who read/ write English and own a smartphone, having mobile internet data as well as being a frequent user of IT were identified as significant predictors of comfort in using MT.
DISCUSSION
The aim of this study was to gain greater insight into the ability of ED patients and caregivers in using MT as well as their usage and preferences with regard to MT.
In our survey, we found that 35% of participants were not comfortable in the usage of MT. If we look amongst the subgroup of patients (as opposed to caregivers) alone, about 50% would not be comfortable. This would greatly impact uptake of any MT intervention. Other studies that report success at MT interventions had higher baseline technology comfort rates.
In a study by Do et al[16] that used MT to monitor tuberculosis medication adherence, their study group at baseline had a high comfort level in MT use, with 80.8% of their participants preferring to communicate with their health care provider via MT. Another study that used MT to improve post rape service delivery reported that 72% reported high comfort levels.[17] With a baseline lower comfort level in the ED, providers can expect a lower uptake of any MT intervention in the ED.
Our study identified certain factors that were associated with participant-reported comfort level in using MT- being able to read and write in English, frequency of IT usage, as well as having a tertiary education. This finding corroborates with other studies, which have reported an association between user-reported technology use and demographic factors such as race and education level.[18]
In a clinical setting, it will be difficult to identify these characteristics in patients and to target MT interventions accordingly. Taking that into consideration, we note that the demographic of caregivers can form a potential target group to increase the pool of participants who are able to use the technology. Compared to patients, a higher percentage of caregivers had a tertiary education, was comfortable reading/ writing in English and were frequent IT users. This gives us a clear demographic that can assist in increasing patient’s participation in MT.
Contrary to our hypothesis, our results reveal that age does not have a significant association with reported comfort level in using MT. This is in agreement with previous studies by Ranney et al.[13] Instead, it is educational levels, usage of English and existing usage of MT that had a stronger association. In Singapore, English was only introduced as a compulsory subject in 1966. As a result, a good proportion of the elderly may not be comfortable with communicating in English especially in written form.[19]
The authors believe that with time, the educational levels, usage of IT and English literacy will increase globally. However, such demographic shifts may take years. In order to increase the participation in such innovations, we believe the participation of caregivers needs to be incorporated into the design and implementation of MT so that caregivers can assist patients in using such technology.
Possible useful features based on these findings include options for secure access by selected caregivers, features that maintain the patient’s privacy, and assistive modules to allow caregivers to help the patients navigate the MT. With this approach, we can allow more patients to participate in mobile healthcare technology. The initial assistance with the technology by their caregivers will allow greater exposure, possibly increasing the patient’s comfort with using MT in future.[16] Other aspects that can be explored would be to include animation or pictorial presentations that could overcome language barriers.
While age itself is not necessarily a factor that determines comfort level with MT, it must not be assumed that the elderly interact with MT the same was as the younger generation. The elderly might in general be comfortable with MT, but developers must consider making their interventions elderly-friendly. This can include features accommodating visual impairments (e.g larger display), cognitive impairments (e.g limited menu options) and motor impairments (e.g allowing for slower response times), as described by Kuerbis et al.[20,21]
To our knowledge, this is the first investigation of the association between demographics of patients and their caregivers with their comfort level in using MT. Our findings give us a snapshot of the current demographic of users of the ED and offer some insight into their technology usage. Developers of MT targeting the ED should take these findings into consideration.
Limitations
Firstly, although survey consisted of many questions that were adapted from other validated surveys, the study survey itself was not formally validated. There are no validated questionnaires or scales on the acceptability of IT in healthcare. Secondly, data was not collected on participants who refused participation, and it was not possible to investigate for inherent differences in participants who chose not to participate. For example, those who opted not to participate might at baseline be less comfortable with the English language. To mitigate against this effect, we ensured that translation services were available where required for willing participants who were uncomfortable with filling in the survey form in English. Thirdly, the usage of a few different translators in multiple languages could have resulted in biases during the process of administration of the survey. Fourthly, sampling bias may be present due to recruitment of patients that presented consecutively during a non-random, convenience sample of shifts. Finally, the study survey required participants to recall past behaviors, which may result in recall bias.
CONCLUSIONS
A large proportion of ED patients are not comfortable in the usage of MT. Factors associated with being comfortable with MT use include being able to read and write in English, frequency of IT usage as well as a tertiary education. Caregivers display these attributes more often than patients, and can potentially form a demographic that can assist in the usage of MT. Future interventions should take this into consideration in the design of MT interventions.
Footnotes
Funding: None.
Ethical approval: The study was approved by the institutional review board with a waiver of written consent (Singhealth CIRB Ref: 2018/2151) and all study procedures were performed in accordance with the declaration of Helsinki.
Conflicts of interests: ZL, RP, KP, LHH and MN report no conflict of interest. DVG has received grant funding through the Commonwealth Fellowship in Innovation award. DVG reports stock ownership in DoctorBell and VISRE that produce products relevant to the subject material. DVG reports advisory as Head of Web/Big data protocol to the Collaborative Ocular Tuberculosis Study (COTS) group, an international initiative utilising cloud computing to investigate ocular tuberculosis (TB) as an early opportunity to address asymptomatic carriage of pulmonary TB.
Contributors: ZL, DVG and RP researched the literature and conceived the study concept and design; ZL and MN were involved in acquisition of data; ZL, LHH, KP, DVG and RP were involved in analysis and interpretation of the data; All authors were involved in drafting the manuscript as well as critical revision of the manuscript.
REFERENCES
- 1.Jaffray DA, Alleyne G. Research and innovation in global cancer control. Lancet Glob Health. 2018;6:S1–2. [Google Scholar]
- 2.Ullman TA, Atreja A. Building evidence for care beyond the medical centre. The Lancet. 2017;390(10098):919–20. doi: 10.1016/S0140-6736(17)31857-3. [DOI] [PubMed] [Google Scholar]
- 3.Smith-Strøm H, Igland J, Østbye T, Tell GS, Hausken MF, Graue M, et al. The effect of telemedicine follow-up care on diabetes-related foot ulcers:A cluster-randomized controlled noninferiority trial. Diabetes Care. 2018;41(1):96–103. doi: 10.2337/dc17-1025. [DOI] [PubMed] [Google Scholar]
- 4.Chongmelaxme B, Lee S, Dhippayom T, Saokaew S, Chaiyakunapruk N, Dilokthornsakul P. The effects of telemedicine on asthma control and patients'quality of life in adults:A systematic review and meta-analysis. J Allergy Clin Immunol Pract. 2019;7(1):199–216. e11. doi: 10.1016/j.jaip.2018.07.015. [DOI] [PubMed] [Google Scholar]
- 5.van der Kop ML, Muhula S, Nagide PI, Thabane L, Gelmon L, Awiti PO, et al. Effect of an interactive text-messaging service on patient retention during the first year of HIV care in Kenya (WelTel Retain):an open-label, randomised parallel-group study. Lancet Public Health. 2018;3(3):e143–52. doi: 10.1016/S2468-2667(17)30239-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arora S, Goldberg A, Menchine M. Patient impression and satisfaction of a self-administered, automated medical history taking device in the emergency department. West J Emerg Med. 2014;15(1):35–40. doi: 10.5811/westjem.2013.2.11498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benaroia M, Elinson R, Zarnke K. Patient-directed intelligent and interactive computer medical history-gathering systems:A utility and feasibility study in the emergency department. Int J Med Inform. 2007;76(4):283–8. doi: 10.1016/j.ijmedinf.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 8.Ponampalam R, Loh C. Cost benefits of the drug and poison information centre in preventing unnecessary hospitalisation:The Singapore experience. Hong Kong J Emerg Med. 2010;17(1):45–53. [Google Scholar]
- 9.Lateef F, Anantharaman V. Maritime radio-medical services:the Singapore General Hospital experience. Am J Emerg Med. 2002;20(4):349–51. doi: 10.1053/ajem.2002.33782. [DOI] [PubMed] [Google Scholar]
- 10.Jury SC, Walker AM, Kornberg AJ. The introduction of web-based video-consultation in a paediatric acute care setting. J Telemed Telecare. 2013;19(7):383–7. doi: 10.1177/1357633X13506530. [DOI] [PubMed] [Google Scholar]
- 11.Weinstein RS, Lopez AM, Joseph BA, Erps KA, Holcomb M, Barker GP, et al. Telemedicine, telehealth, and mobile health applications that work:opportunities and barriers. Am J Emerg Med. 2014;127(3):183–7. doi: 10.1016/j.amjmed.2013.09.032. [DOI] [PubMed] [Google Scholar]
- 12.Aeimchanbanjong K, Pandee U. Validation of different pediatric triage systems in the emergency department. World J Emerg Med. 2017;8(3):223–7. doi: 10.5847/wjem.j.1920-8642.2017.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ranney ML, Choo EK, Wang Y, Baum A, Clark MA, Mello MJ. Emergency department patients'p for technology-based behavioral interventions. Ann Emerg Med. 2012;60(2):218–227. e48. doi: 10.1016/j.annemergmed.2012.02.026. [DOI] [PubMed] [Google Scholar]
- 14.Semple JL, Sharpe S, Murnaghan ML, Theodoropoulos J, Metcalfe KA. Using a mobile app for monitoring post-operative quality of recovery of patients at home:A feasibility study. JMIR Mhealth Uhealth. 2015;3(1):e18. doi: 10.2196/mhealth.3929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ray M, Dayan PS, Pahalyants V, Chernick LS. Mobile health technology to communicate discharge and follow-up information to adolescents from the emergency department. Pediatr Emerg Care. 2016;32(12):900–5. doi: 10.1097/PEC.0000000000000970. [DOI] [PubMed] [Google Scholar]
- 16.Do D, Garfein RS, Cuevas-Mota J, Collins K, Liu L. Change in patient comfort using mobile phones following the use of an app to monitor tuberculosis treatment adherence:longitudinal study. JMIR Mhealth Uhealth. 2019;7(2):e11638. doi: 10.2196/11638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mahlalela NB, Johnson S, Mills E. Feasibility and acceptability of a mobile phone intervention to improve post-rape service delivery in South Africa. https://opendocs.ids.ac.uk/opendocs/handle/123456789/12771 .
- 18.Czaja SJ, Charness N, Fisk AD, Hertzog C, Nair SN, Rogers WA, et al. Factors predicting the use of technology:Findings from the center for research and education on aging and technology enhancement (create) Psychol Aging. 2006;21(2):333–52. doi: 10.1037/0882-7974.21.2.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Afendras EA, Kuo ECY, editors. Language and society in Singapore. Singapore: Univ. Pr; 1980. [Google Scholar]
- 20.Kuerbis A, Mulliken A, Muench F, Moore AA, Gardner D. Older adults and mobile technology:Factors that enhance and inhibit utilization in the context of behavioral health. Ment Health Addict Res. 2017;2(2):1–11. [Google Scholar]
- 21.Parker SJ, Jessel S, Richardson JE, Reid MC. Older adults are mobile too!Identifying the barriers and facilitators to older adults'use of mHealth for pain management. BMC Geriatr. 2013;13(1):43. doi: 10.1186/1471-2318-13-43. [DOI] [PMC free article] [PubMed] [Google Scholar]


