Abstract
This study examined whether employment category was associated with insomnia-related symptoms (IRS). We analyzed the 2010 Comprehensive Survey of Living Conditions in Japan. The anonymous data of 43,865 people ranging from 20–59 yr of age were analyzed. We defined six employment categories: regularly employed, non-regularly employed, self-employed, others, unemployed and not in the labor force. Sex-specific odds ratios (ORs) and 95% confidence intervals (CIs) of IRS were calculated using multivariable logistic regression analysis, adjusted for confounding factors. We further conducted stratified analyses by mental illness, smoking status, and age. For men, the multivariable ORs (95% CI) of IRS for the unemployed and those who were not in the labor force were 2.5 (1.8–3.4) and 2.1 (1.2–3.7). For women, the multivariable ORs (95% CI) for the unemployed was 1.9 (1.5–2.5). After being stratified by mental illness, we found that the associations were not significant in persons with mental illness, and were more evident in persons without mental illness. Smoking and age did not modify the associations. In conclusion, we found a significantly higher OR of IRS for the unemployed, and men who were not in the labor force. These associations were particularly more evident for individuals without mental illness.
Keywords: Insomnia-related symptoms, Employment category, Sleep guidelines, Comprehensive survey of living conditions, Ministry of Health, Labor, and Welfare of Japan
Introduction
Insomnia is related to a wide variety of health problems, including depression and metabolic syndrome, as well as socio-economic problems, such as workplace accidents1,2,3). The overall prevalence of insomnia among Japanese people during the preceding month in February or March 1997 was 21.4%, and included difficulty initiating sleep (DIS) (8.3%), difficulty maintaining sleep (DMS) (15.0%) and early morning awakening (EMA) (8.0%)4).
An independent, not-for-profit policy research organization showed that in Japan, insufficient sleep reduced the size of the working population by making workers miss work due to sickness. Together with reduced work performance, this resulted in large economic losses (between 88 and 138 billion dollars)5).
Previous studies in Western countries suggest that insomnia is associated with socioeconomic status, including income and employment status6,7,8,9). Most of these studies showed that lower income groups had a higher prevalence of respondents who were bothered by insomnia-related symptoms (IRS) (i.e., DIS, DMS, EMA, poor sleep quality) than higher income groups. Other studies have shown that employment status is the strongest determinant of income, and the unemployed have a higher risk of sleep disturbance6,7,8,9,10,11,12) due to their poorer mental and/or physical health9) and strained domestic circumstances (e.g., difficulty in job seeking, financial threats)12).
In Japan, the Sleep Guidelines for Health Promotion were devised in 2003, and revised in 2014, by the Ministry of Health, Labor, and Welfare (MHLW)13). The guidelines comprise twelve messages on how sleep can improve health (e.g., how sleep can reduce the risk of non-communicable diseases and accidents); they also include messages for three different age groups: the young, the middle-aged, and the elderly. However, the guidelines do not mention anything regarding the relationship between insomnia and employment category.
Given that the Japanese economy is gradually recovering and the real and nominal GDP growth rates rose for 5 consecutive years, the employment situation is also steadily improving: the average unemployment rate decreased between 2009 and 2016, with that of 2016 being the lowest rate since 1994. However, the proportion of non-regularly employed individuals has been gradually increasing14).
To date, several studies have examined the association between employment category and IRS in Japan4, 15,16,17,18). A previous study of local government employees showed that low-grade male employees had poor sleep quality compared to high-grade male employees15). However, a cross-sectional study of employees of a telecommunications company showed that daytime white-collar workers had poorer sleep quality than the general population of Japanese adults16). Another cross-sectional study of a representative sample of Japanese people (n=3,030) showed that the unemployed had a higher prevalence of insomnia than the employed4). As of yet, no study using a representative sample of Japanese individuals has examined the association between IRS and employment category, specifically for the unemployed and those not in the labor force.
Given that the lower productivity levels and higher mortality risks related to insufficient sleep could cause substantial economic losses to modern economies, it is important to investigate the background factors that cause insomnia. Specifically, the relationship between insomnia and socioeconomic status in Japan must be investigated so that effective measures to reduce economic losses due to insufficient sleep5) can be implemented. The purpose of the present study was to use the 2010 Comprehensive Survey of Living Conditions (CSLC)—which is a representative sample of the Japanese population—to examine whether employment category was associated with IRS and to assess effect modification by potential confounding factors.
Subjects and Methods
The outline of the Comprehensive Survey of Living Conditions (CSLC)
The Comprehensive Survey of Living Conditions (CSLC) is a comprehensive survey carried out by the MHLW using a self-reported questionnaire. The purpose of the CSLC is to investigate living conditions—such as health, medical care, welfare, pension, and income—and to obtain the basic data required by the MHLW for planning and management. The CSLC covers households and household members nationwide. For the 2010 survey, which is used in the present study, 5,510 districts were randomly sampled from the 2005 National Census. Further details on the CSLC can be found on the MHLW website19).
Basic materials
The data source for the present study is the anonymous data in the 2010 CSLC. We obtained approval from the MHLW to use this data in accordance with Article 36 of the Statistics Law of Japan on November 20th, 2015 (No. 1120-6).
Subjects
The anonymous data from 44,031 people (21,716 men and 22,315 women) between 20–59 yr of age were obtained from the MHLW. Of these, 127 people did not provide an answer for employment status, 14 people did not provide an answer for employment category, and 25 unemployed people did not answer whether or not they have an intention to find work. We excluded these non-respondents from the present study and analyzed the data of the remaining 43,865 people (21,649 men and 22,216 women).
Assessment of employment category
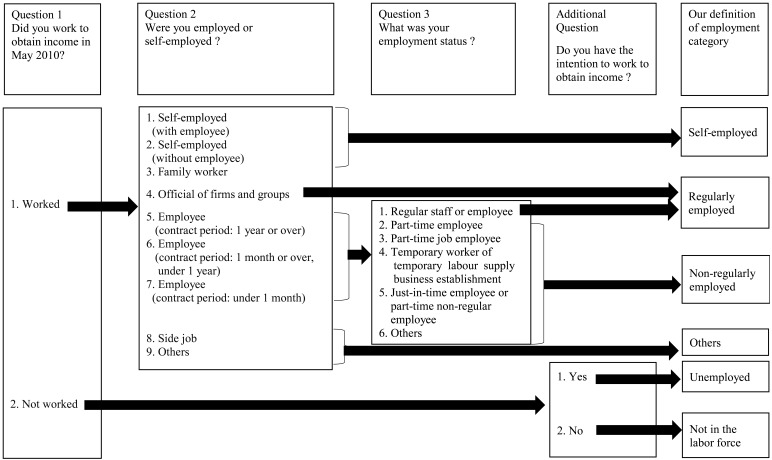
In the 2010 CSLC, participants were asked three questions: “Did you work to obtain income in May 2010?”, “Were you employed or self-employed?”, and “What was your employment category?” When the participant answered “Not worked”, he or she was also asked whether or not he or she had the intention to find work to obtain income. We defined six employment categories according to International Labor Organization standards: regularly employed, non-regularly employed, self-employed, others, unemployed, and not in the labor force, as shown in Fig. 1.
Fig. 1.
Assessment of employment category.
Assessment of insomnia-related symptoms (IRS)
We assessed IRS using the CSLC self-administered questionnaire responses. Participants answered the following question: “Over the past several days, did you experience any symptoms of sickness or injury?” Those respondents who selected “I could not sleep” from 42 symptom choices were defined as having IRS.
Assessment of confounding factors
We also assessed participants’ recent history of mental illness, insomnia related chronic diseases, smoking status and household expenditure using the self-administered questionnaire. For recent history of mental illness, participants who selected “depression or other mental illness with outpatient visit” from a list of 41 diseases and injuries were defined as being with mental illness. For insomnia related chronic diseases, participants who selected “hyperlipidemia”, “Parkinsonism”, “hypertension”, “Asthma”, “disease of stomach or duodenum” or “rheumatoid arthritis” from a list of 41 diseases and injuries were defined as being related to IRS by side effect of treating these illnesses20).
For smoking status, participants could select from four answers: participants who chose “Never” or “Past (have not smoked for more than 1 month)” were defined as non-smokers, while participants who chose “Smoking everyday” or “Smoking sometimes” were defined as smokers. Smokers were divided into two subgroups based on the number of cigarettes they reported smoking: “Smoking ≤20 cigarettes per day” and “Smoking ≥21 cigarettes per day”. For household expenditure, participants answered their household expenditure in May 2010. We divided under 25 percentile (men; under 150,000 yen, women; under 170,000 yen), 25 to 50 percentile (men; 150,000 to 250,000 yen, women; 170,000 to 250,000 yen), 50 to 75 percentile (men; 250,000 to 335,000 yen, women; 250,000 to 350,000 yen) and 75 percentile (men; 335,000 yen, women; 350,000 yen) or over.
We also assessed the following confounding factors using the self-administered questionnaire: marital status (single, married, and divorced or widowed), education level (junior high school, high school, junior college or technical upper secondary school, and university or graduate school) and parental status (in need of long-term care or not in need of long-term care).
Statistical analysis
Sex- and age-specific proportions of participants, percentages of respondents with age, marital status, education level, mental illness, smoking status, parental status, household expenditure and insomnia related chronic diseases were calculated according to the six employment categories. These differences were then tested using χ2 tests. The sex-specific proportion of participants with IRS was calculated according to the six employment categories. Sex-specific odds ratios (ORs) and 95% confidence intervals (CIs) of IRS for each employment category were compared to those for the regularly employed using multivariable logistic regression analysis, adjusting for the potentially confounding factors of age, mental illness, marital status, education level, smoking status, parental status, household expenditure and insomnia related chronic diseases.
The same analyses were also performed stratified by mental illness, smoking status, and age subgroups (20–39 and 40–59 yr). The effect modification of these factors was tested using an interaction term generated by multiplying each employment category by each of the factors above.
All statistical analyses were performed using SAS ver. 9.4 software (SAS Institute Inc., Cary, USA). All probability values for statistical tests were two-tailed, and values of p<0.05 were regarded as statistically significant.
No protocol approval was needed for this study because the survey data are publicly available.
Results
The proportion of participants with IRS was 2.1% (452/21,649) in men and 2.6% (581/22,216) in women. Table 1 shows respondents’ demographic characteristics according to the six employment categories. For both sexes, participants aged 50–59 had the highest proportion of self-employment (39.5% in men and 43.3% in women). In men, the unemployed had the highest proportion of people with mental illness (7.3%). In women, those who were not in the labor force had the highest proportion of mental illness (4.1%). For both men and women, those who were not in the labor force had the highest percentage of non-smokers (63.3% and 80.8%, respectively). Participants aged 30–39 made up the largest group of the regularly employed in men (28.8%) and the largest group of the unemployed in women (36.0%).
Table 1. Demographic characteristics according to employment category of 43,865 people (21,649 men and 22,216 women).
| Men | Women | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unemployed | Not in the labor force | Regularly employed | Non-regularly employed | Self-employed | Others | p | Unemployed | Not in the labor force | Regularly employed | Non-regularly employed | Self-employed | Others | p | ||
| N | 1,075 | 341 | 15,056 | 2,083 | 2,808 | 286 | 3,483 | 2,581 | 6,853 | 7,087 | 1,729 | 483 | |||
| Age of persons | |||||||||||||||
| 20–29 | 34.8 | 47.5 | 16.0 | 39.8 | 7.1 | 20.6 | <0.0001 | 16.9 | 8.8 | 27.5 | 16.4 | 7.0 | 12.8 | <0.0001 | |
| 30–39 | 16.3 | 7.9 | 28.8 | 23.7 | 23.0 | 22.4 | 36.0 | 21.2 | 27.4 | 25.0 | 20.5 | 23.4 | |||
| 40–49 | 19.1 | 10.0 | 28.3 | 14.8 | 30.4 | 24.1 | 26.0 | 21.3 | 23.8 | 30.6 | 29.2 | 30.2 | |||
| 50–59 | 29.9 | 34.6 | 26.9 | 21.7 | 39.5 | 32.9 | 21.1 | 48.7 | 21.4 | 28.0 | 43.3 | 33.5 | |||
| Marital status | |||||||||||||||
| Married | 27.4 | 17.6 | 69.8 | 30.1 | 74.5 | 52.8 | <0.0001 | 83.6 | 89.2 | 46.5 | 68.3 | 77.2 | 72.3 | <0.0001 | |
| Single | 65.8 | 76.0 | 27.2 | 64.5 | 21.3 | 42.3 | 11.0 | 7.4 | 43.9 | 22.4 | 14.3 | 22.0 | |||
| Divorced or widowed | 6.9 | 6.5 | 3.0 | 5.5 | 4.2 | 4.9 | 5.5 | 3.5 | 9.5 | 9.3 | 8.5 | 5.8 | |||
| Education level | |||||||||||||||
| Junior high school | 12.7 | 10.9 | 4.2 | 8.8 | 10.2 | 11.2 | <0.0001 | 5.6 | 6.6 | 2.3 | 4.9 | 5.3 | 7.3 | <0.0001 | |
| High school | 36.2 | 26.7 | 37.9 | 39.9 | 41.1 | 43.0 | 39.3 | 40.9 | 32.2 | 43.8 | 41.6 | 42.7 | |||
| Junior college or technical upper secondary school | 11.1 | 6.2 | 12.9 | 14.7 | 15.3 | 12.2 | 31.5 | 29.5 | 33.9 | 30.6 | 29.6 | 26.9 | |||
| University or graduate school | 34.1 | 49.9 | 37.1 | 29.4 | 23.2 | 25.9 | 16.9 | 16.9 | 23.5 | 13.0 | 13.0 | 14.5 | |||
| Mental illness | |||||||||||||||
| Yes | 7.3 | 6.5 | 1.2 | 1.3 | 0.7 | 2.4 | <0.0001 | 3.9 | 4.1 | 1.4 | 1.7 | 1.2 | 2.1 | <0.0001 | |
| No | 92.7 | 93.5 | 98.8 | 98.7 | 99.3 | 97.6 | 96.1 | 95.9 | 98.6 | 98.3 | 98.8 | 97.9 | |||
| Smoking status | |||||||||||||||
| Smoking 21 or more cigarettes per day | 8.7 | 2.4 | 9.2 | 7.1 | 13.6 | 7.0 | <0.0001 | 1.4 | 1.0 | 0.8 | 1.5 | 1.7 | 1.0 | <0.0001 | |
| Smoking 20 or less cigarettes per day | 27.8 | 18.2 | 30.4 | 32.3 | 27.0 | 30.3 | 12.9 | 7.9 | 12.3 | 13.9 | 12.3 | 12.0 | |||
| Non-smokers | 49.6 | 63.3 | 50.1 | 47.7 | 45.9 | 48.2 | 78.2 | 80.8 | 78.8 | 75.5 | 73.1 | 73.9 | |||
| Parental status | |||||||||||||||
| In need of long-term care | 5.4 | 9.7 | 0.3 | 1.1 | 0.4 | 4.5 | <0.0001 | 1.0 | 2.6 | 0.3 | 0.3 | 0.2 | 2.3 | <0.0001 | |
| Not in need of long-term care | 94.6 | 90.3 | 99.7 | 98.9 | 99.6 | 95.5 | 99.0 | 97.4 | 99.7 | 99.7 | 99.8 | 97.7 | |||
| Household expenditure* | |||||||||||||||
| Under 25 percentile | 40.7 | 37.5 | 13.8 | 25.9 | 17.1 | 23.1 | <0.0001 | 27.0 | 20.2 | 24.7 | 23.7 | 25.9 | 22.6 | <0.0001 | |
| 25 to 50 percentile | 26.6 | 23.5 | 32.9 | 31.6 | 30.9 | 33.6 | 27.2 | 22.4 | 21.7 | 23.2 | 21.8 | 22.2 | |||
| 50 to 75 percentile | 14.8 | 17.0 | 27.5 | 21.0 | 24.4 | 21.7 | 26.6 | 29.3 | 26.4 | 27.3 | 23.4 | 27.3 | |||
| 75 percentile or over | 11.3 | 15.3 | 20.8 | 16.0 | 21.4 | 16.4 | 14.9 | 23.0 | 21.9 | 20.3 | 22.7 | 21.5 | |||
| Insomnia related chronic diseases | |||||||||||||||
| With diseases | 9.5 | 10.6 | 8.7 | 5.4 | 8.5 | 7.0 | <0.0001 | 6.9 | 11.6 | 6.2 | 7.5 | 9.1 | 8.9 | <0.0001 | |
| Without diseases | 90.5 | 89.4 | 91.3 | 94.6 | 91.5 | 93.0 | 93.1 | 88.4 | 93.8 | 92.5 | 90.9 | 91.1 | |||
p values: χ2 test. *25 percentile (men; under 150,000 yen, women; under 170,000 yen), 25 to 50 percentile (men; 150,000 to 250,000 yen, women; 170,000 to 250,000 yen), 50 to 75 percentile (men; 250,000 to 335,000 yen, women; 250,000 to 350,000 yen) and 75 percentile (men; 335,000 yen, women; 350,000 yen) or over.
Table 2 shows age- and multivariable-adjusted ORs (95% CI) according to the six employment categories. The age-adjusted ORs (95% CI) of IRS for unemployed men and men who were not in the labor force were 4.3 (3.2–5.6) and 4.0 (2.5–6.5) compared to the regularly employed. For unemployed women, the ORs of IRS was 2.1 (1.7–2.6). After adjusting for confounding factors, the associations were attenuated, but remained statistically significant. The multivariable ORs (95% CI) of IRS for unemployed men and men who were not in the labor force were 2.5 (1.8–3.4) and 2.1 (1.2–3.7) compared with the regularly employed. The multivariable OR of IRS for unemployed women was 1.9 (1.5–2.5).
Table 2. Multivariable adjusted Odds Ratios (ORs) and 95% Confidence Intervals (CIs) for insomnia-related symptoms.
| Men | Women | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unemployed | Not in the labor force | Regularly employed | Non-regularly employed | Self-employed | Others | Unemployed | Not in the labor force | Regularly employed | Non-regularly employed | Self-employed | Others | |
| N | 1,075 | 341 | 15,056 | 2,083 | 2,808 | 286 | 3,483 | 2,581 | 6,853 | 7,087 | 1,729 | 483 |
| No. of persons with insomnia-related symptoms (%)* | 71 (6.6) | 20 (5.9) | 273 (1.8) | 38 (1.8) | 44 (1.6) | 6 (2.1) | 148 (4.3) | 73 (2.8) | 144 (2.1) | 171 (2.4) | 32 (1.9) | 13 (2.7) |
| Age-adjusted OR (95% CI) | 4.3 (3.2–5.6) | 4.0 (2.5–6.5) | 1.0 | 1.2 (0.8–1.7) | 0.8 (0.6–1.1) | 1.2 (0.5–2.7) | 2.1 (1.7–2.6) | 1.2 (0.9–1.6) | 1.0 | 1.1 (0.9–1.4) | 0.8 (0.5–1.2) | 1.2 (0.7–2.2) |
| Multivariable OR# (95% CI) | 2.5 (1.8–3.4) | 2.1 (1.2–3.7) | 1.0 | 1.1 (0.8–1.6) | 0.9 (0.6–1.2) | 1.0 (0.4–2.3) | 1.9 (1.5–2.5) | 1.1 (0.8–1.5) | 1.0 | 1.1 (0.9–1.4) | 0.9 (0.6–1.3) | 1.3 (0.7–2.3) |
*Proportion of persons with insomnia-related symptoms among persons by employment category. #Adjusted for age, marital status, education level, mental illness, smoking status, parental status, household expenditure and insomnia related chronic diseases.
Table 3 shows the multivariable ORs (95% CI) of IRS, stratified by mental illness, smoking status, and age group (20–39 and 40–59 yr). After adjusting for age, marital status, education level, smoking status, parental status, household expenditure and insomnia related chronic diseases, three groups without mental illness—unemployed men, men who were not in the labor force, and unemployed women—had a higher prevalence of IRS compared to the regularly employed population.
Table 3. Multivariable odds ratios (ORs) and 95% Confidence Intervals (CIs) for insomnia-related symptoms, stratified by mental illness, smoking status and age subgroups.
| Men | Women | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unemployed | Not in the labor force | Regularly employed | Non-regularly employed | Self-employed | Others | Unemployed | Not in the labor force | Regularly employed | Non-regularly employed | Self-employed | Others | |||
| N | 1,075 | 341 | 15,056 | 2,083 | 2,808 | 286 | 3,483 | 2,581 | 6,853 | 7,087 | 1,729 | 483 | ||
| Mental ilness | ||||||||||||||
| Yes | ||||||||||||||
| No. of persons with insomnia-related symptoms (%)* | 25 (31.6) | 7 (31.8) | 46 (24.5) | 7 (25.0) | 4 (19.0) | 1 (14.3) | 45 (33.3) | 20 (19.0) | 28 (29.8) | 28 (23.0) | 7 (35.0) | 1 (10.0) | ||
| Multivariable adjusted ORs (#1) (95% CI) | 1.4 (0.7–2.9) | 1.3 (0.4–3.9) | 1.0 | 1.0 (0.3–2.8) | 0.7 (0.2–2.2) | 0.4 (0.0–4.2) | 1.3 (0.7–2.4) | 0.7 (0.3–1.4) | 1.0 | 0.7 (0.4–1.3) | 1.4 (0.5–3.9) | 0.4 (0.0–3.2) | ||
| No | ||||||||||||||
| No. of persons with insomnia-related symptoms (%)* | 46 (4.6) | 13 (4.1) | 227 (1.5) | 31 (1.5) | 40 (1.4) | 5 (1.8) | 103 (3.1) | 53 (2.1) | 116 (1.7) | 143 (2.1) | 25 (1.5) | 12 (2.5) | ||
| Multivariable adjusted ORs (#1) (95% CI) | 3.0 (2.1–4.3) | 2.7 (1.4–4.9) | 1.0 | 1.1 (0.7–1.6) | 0.9 (0.6–1.3) | 1.2 (0.5–2.9) | 2.1 (1.6–2.8) | 1.2 (0.9–1.7) | 1.0 | 1.2 (1.0–1.6) | 0.9 (0.5–1.3) | 1.5 (0.8–2.7) | ||
| Smoking status | ||||||||||||||
| Smokers | ||||||||||||||
| No. of persons with insomnia-related symptoms (%)* | 34 (8.7) | 7 (10.0) | 101 (1.7) | 17 (2.1) | 19 (1.7) | 5 (4.6) | 37 (7.4) | 13 (5.7) | 25 (2.8) | 42 (3.9) | 5 (2.1) | 1 (1.6) | ||
| Multivariable adjusted ORs (#2) (95% CI) | 3.5 (2.2–5.7) | 3.6 (1.4–9.2) | 1.0 | 1.3 (0.8–2.3) | 1.0 (0.6–1.6) | 2.5 (0.9–6.6) | 2.2 (1.2–3.9) | 1.7 (0.8–3.8) | 1.0 | 1.3 (0.8–2.3) | 0.9 (0.3–2.3) | 0.6 (0.1–4.7) | ||
| Non-smokers | ||||||||||||||
| No. of persons with insomnia-related symptoms (%)* | 35 (6.6) | 11 (5.1) | 155 (2.1) | 19 (1.9) | 22 (1.7) | 1 (0.7) | 104 (3.8) | 53 (2.5) | 109 (2.1) | 115 (2.2) | 24 (1.9) | 12 (3.4) | ||
| Multivariable adjusted ORs (#2) (95% CI) | 2.0 (1.3–3.3) | 1.4 (0.7–3.0) | 1.0 | 1.0 (0.6–1.6) | 0.8 (0.5–1.2) | 0.3 (0.0–1.9) | 2.0 (1.5–2.6) | 1.0 (0.7–1.5) | 1.0 | 1.1 (0.8–1.4) | 0.9 (0.6–1.4) | 1.6 (0.8–3.0) | ||
| Age subgroup | ||||||||||||||
| 20–39 yr of age | ||||||||||||||
| No. of persons with insomnia-related symptoms (%)* | 24 (4.4) | 5 (2.6) | 101 (1.5) | 17 (1.3) | 7 (0.8) | 4 (3.3) | 62 (3.4) | 11 (1.4) | 70 (1.9) | 72 (2.5) | 9 (1.9) | 4 (2.3) | ||
| Multivariable adjusted ORs (#3) (95% CI) | 1.7 (1.0–2.8) | 1.6 (0.6–4.1) | 1.0 | 0.8 (0.5–1.4) | 0.6 (0.3–1.2) | 2.1 (0.7–6.1) | 1.7 (1.2–2.6) | 0.7 (0.4–1.4) | 1.0 | 1.2 (0.8–1.7) | 1.0 (0.5–2.1) | 1.3 (0.5–3.8) | ||
| 40–59 yr of age | ||||||||||||||
| No. of persons with insomnia-related symptoms (%)* | 47 (8.9) | 15 (9.9) | 172 (2.1) | 21 (2.8) | 37 (1.9) | 2 (1.2) | 86 (5.2) | 62 (3.4) | 74 (2.4) | 99 (2.4) | 23 (1.8) | 9 (2.9) | ||
| Multivariable adjusted ORs (#3) (95% CI) | 3.0 (2.0–4.6) | 2.5 (1.3–4.9) | 1.0 | 1.4 (0.9–2.2) | 1.0 (0.7–1.5) | 0.5 (0.1–2.0) | 2.0 (1.4–2.8) | 1.3 (0.9–1.9) | 1.0 | 1.1 (0.8–1.5) | 0.9 (0.5–1.4) | 1.3 (0.6–2.7) | ||
*Proportion of persons with insomnia-related symptoms among persons by employment category. #1: Adjusted for age, marital status, education level, smoking status, parental status, household expenditure and insomnia related chronic diseases. #2: Adjusted for age, marital status, education level, and mental illness, parental status, household expenditure and insomnia related chronic diseases. #3: Adjusted for marital status, education level, mental illness, and smoking status, parental status, household expenditure and insomnia related chronic diseases.
Discussion
Summary of the results
The proportion of individuals with IRS was 2.1% of men and 2.6% of women in the present study, whereas previous studies showed higher insomnia prevalence rates4). We defined individuals with IRS as those who chose “I could not sleep” among 42 possible responses to the question: “Over the past several days, did you experience any symptoms due to sickness or injury?” However, insomnia is characterized as a hypnagogic disorder, deep sleep disorder, middle wakening, or early wakening21). Thus, the discrepancy of the proportion of IRS between that of the present study and that of previous studies may be due to underestimating the symptoms of insomnia; however, the characteristics of persons with IRS identified in the present study were similar to those found in previous studies, e.g., age and smoking behavior.
The prevalence of IRS in the present study was extremely low compared to a previous study, which focused on insomnia and employment status4). This is because in the present study the targeted duration of IRS was shorter and the causes of IRS were confined.
For both men and women, being unemployed had a higher ORs of IRS, and the association seemed to be more derived by those without mental illness. Talala et al. showed that the unemployed had a higher proportion of self-reported insomnia than the employed for both men (OR: 2.48, 95% CI: 2.22–2.76; p<0.05) and women (OR: 1.80, 95% CI: 1.60–2.02; p<0.05) in their age-adjusted model. After further adjustment for all socioeconomic status variables (educational level, employment category, and household income) and depression, the multivariable ORs (95% CI) were attenuated to 1.76 (1.55–2.00; p<0.05) for men and 1.39 (1.22–1.58; p<0.05) for women, but the multivariable ORs remained statistically significant10). According to the results of previous studies, sleep complaints, sleep disturbance, and the prevalence of insomnia were higher among the unemployed than among the regularly employed4, 7, 12). Chen et al. showed that unemployed individuals who were actively seeking work had the highest levels of sleep disturbance compared to those with other employment categories12).
The results of the present study exhibited a similar trend with those from previous studies. Indeed, the ORs of IRS for unemployed men, men who were not in the labor force, and unemployed women were higher (as compared with the regularly employed) in both the age-adjusted and multivariable models than the ORs of IRS previously reported in the literature.
We were able to assess mental illness as a confounding factor using the self-administered questionnaire because a previous longitudinal study revealed a statistically significant relationship between insomnia subtype (e.g., difficulty initiating sleep) and having depression when looking at data from a period of three years1). We were able to assess smoking status as a confounding factor because previous cross-sectional studies strongly suggested that cigarette smoking is associated with poor sleep habits, poor sleep quality, delayed sleep onset, and diminished sleep duration22, 23).
Mechanisms
Although the biological mechanisms linking unemployment and insomnia are not clear, our data suggested an association between unemployment and IRS based on a large and representative sample of Japanese individuals. Previous studies have suggested that unemployment causes depressive symptoms24), and these symptoms could induce insomnia25, 26).
The key findings in the present study are that unemployed men, men who were not in the labor force, and unemployed women are significantly associated with IRS, especially among men without mental illness. Riemann et al. developed a neurocognitive model of insomnia in which acute insomnia (1–90 d) is associated with predisposing and precipitating factors (e.g., psychosocial stressors), and chronic insomnia (over 6 months) is associated with perpetuating factors (e.g., extension of time in bed). In this study, cognitive-behavioral and neuro-biologic domains are depicted in a parallel way. The authors assume that both domains are strongly interconnected and not independent of each other27). Therefore, the higher OR of IRS for unemployed individuals was due to the interaction of both domains.
Strengths
In the present study, we used anonymous data derived from the 2010 CSLC Household and Health questionnaire, which collected randomly sampled data at the household (approximately 290,000 households) and household member (approximately 750,000 persons) levels. The strength of the present study is its large sample size of those aged between 20 and 59, representing national samples. To date, there are very few large-scale studies investigating the association between employment category and IRS that are without sampling bias. Therefore, this is the first study with high statistical power that has investigated the impact of mental illness-, smoking status-, and age-stratified employment category on IRS in an Asian population.
Limitations
There are several limitations to the present study. First, because this study was cross-sectional, we could not determine any causal relationship between unemployment and IRS. Second, because only self-reported information was available regarding participants’ IRS, we could not clarify whether participants had physical illnesses or injury in relation to IRS. Though the causes of IRS are various and not always clearly identified, in the present study the definition of IRS was confined by duration and cause. Thus, the self-report-defined non-insomnia category likely contained a substantial undiagnosed population. This suggests that the ORs of IRS associated with employment category observed in our analyses may have been underestimated. Third, because there was no information on participants’ exercise and drinking habits in the 2010 CSLC, it was not possible to evaluate how IRS relates to habitual exercise or alcohol consumption. These factors have been reported to have an impact on insomnia4, 28). Fourth, while we adjusted for confounding factors, i.e., history of mental illness, marital status, education level, smoking behavior, parental status, household expenditure and insomnia related chronic diseases, there are potential residual confounding factors, i.e., income. Because we did not receive infromation of income from Ministry of Health, Labour and Welfare, we used household expenditure on behalf of income. Finally, in this study, there may be several persons classified in the “Not in the labor force”, because they suffered from child-rearing stress. However, we could not support that because the questionnaires were not enough to search the details of respondents who chose “Not in the labor force”. We consider that the misclassification could be low, as compared to the age composition of unemployed women, among women not in the labor force, there were comparatively more women aged 40–59 and fewer aged 20–39.
Implications
Measures should be taken to ensure that there are medical checkup opportunities and the utilization of the 2014 Sleep Guidelines for Health Promotion13) for unemployed individuals with the aim of preventing unemployment-induced insomnia. This will reduce the economic losses due to insufficient sleep, as the unemployed have a significant association with IRS. Additionally, the Guidelines should be revised from the viewpoint of employment category, with a specific focus on the unemployed.
Conclusions
We found a significant association between insomnia-related symptoms and the following groups: unemployed men, men who were not in the labor force, and unemployed women. This association was particularly strong for men without mental illness. Measures should be implemented to ensure medical checkup opportunities and the utilization of the 2014 Sleep Guidelines for Health Promotion.
Authors’ Contributions
MM and TS participated in the study concept and design, and interpretation of data, and drafting the manuscript. YK and RF participated in the interpretation and analysis of data. TT, HI, HW, AI and KM participated in the study concept and design, interpretation of data, and critically revised the manuscript. The authors have no competing interests. As the authors have independently created or processed the anonymous data, the results were not the statistics developed and issued by the Ministry of Health, Labour and Welfare of Japan.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare that there are no conflicts of interest.
References
- 1.Yokoyama E, Kaneita Y, Saito Y, Uchiyama M, Matsuzaki Y, Tamaki T, Munezawa T, Ohida T. (2010) Association between depression and insomnia subtypes: a longitudinal study on the elderly in Japan. Sleep 33, 1693–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ikeda M, Kaneita Y, Uchiyama M, Mishima K, Uchimura N, Nakaji S, Akashiba T, Itani O, Aono H, Ohida T. (2014) Epidemiological study of the associations between sleep complaints and metabolic syndrome in Japan. Sleep Biol Rhythms 12, 269–78. [Google Scholar]
- 3.Shahly V, Berglund PA, Coulouvrat C, Fitzgerald T, Hajak G, Roth T, Shillington AC, Stephenson JJ, Walsh JK, Kessler RC. (2012) The associations of insomnia with costly workplace accidents and errors: results from the America Insomnia Survey. Arch Gen Psychiatry 69, 1054–63. [DOI] [PubMed] [Google Scholar]
- 4.Kim K, Uchiyama M, Okawa M, Liu X, Ogihara R. (2000) An epidemiological study of insomnia among the Japanese general population. Sleep 23, 41–7. [PubMed] [Google Scholar]
- 5.Hafner M, Stepanek M, Taylor J, Troxel WM, Stolk C .(2016) Why sleep matters—the economic costs of insufficient sleep. RAND Europe. p.50. [PMC free article] [PubMed] [Google Scholar]
- 6.Grandner MA, Patel NP, Gehrman PR, Xie D, Sha D, Weaver T, Gooneratne N. (2010) Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med 11, 470–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lallukka T, Sares-Jäske L, Kronholm E, Sääksjärvi K, Lundqvist A, Partonen T, Rahkonen O, Knekt P. (2012) Sociodemographic and socioeconomic differences in sleep duration and insomnia-related symptoms in Finnish adults. BMC Public Health 12, 565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel NP, Grandner MA, Xie D, Branas CC, Gooneratne N. (2010) “Sleep disparity” in the population: poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health 10, 475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Soltani M, Haytabakhsh MR, Najman JM, Williams GM, O’Callaghan MJ, Bor W, Dingle K, Clavarino A. (2012) Sleepless nights: the effect of socioeconomic status, physical activity, and lifestyle factors on sleep quality in a large cohort of Australian women. Arch Women Ment Health 15, 237–47. [DOI] [PubMed] [Google Scholar]
- 10.Talala KM, Martelin TP, Haukkala AH, Härkänen TT, Prättälä RS. (2012) Socio-economic differences in self-reported insomnia and stress in Finland from 1979 to 2002: a population-based repeated cross-sectional survey. BMC Public Health 12, 650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hirotsu C, Bittencourt L, Garbuio S, Andersen ML, Tufik S. (2014) Sleep complaints in the Brazilian population: impact of socioeconomic factors. Sleep Sci 7, 135–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen YY, Kawachi I, Subramanian SV, Acevedo-Garcia D, Lee YJ. (2005) Can social factors explain sex differences in insomnia? Findings from a national survey in Taiwan. J Epidemiol Community Health 59, 488–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Noda H. (2015) The Japanese government’s “good sleep” challenge: Sleep Guidelines for Health Promotion 2014. J Epidemiol 25, 339–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ministry of Health, Labour and Welfare. Analysis of the Labour Economy. http://www.mhlw.go.jp/english/wp/l-economy/index.html. Accessed August 5, 2018.
- 15.Sekine M, Chandola T, Martikainen P, Marmot M, Kagamimori S. (2006) Work and family characteristics as determinants of socioeconomic and sex inequalities in sleep: the Japanese Civil Servants Study. Sleep 29, 206–16. [DOI] [PubMed] [Google Scholar]
- 16.Doi Y, Minowa M, Tango T. (2003) Impact and correlates of poor sleep quality in Japanese white-collar employees. Sleep 26, 467–71. [DOI] [PubMed] [Google Scholar]
- 17.Sakurai K, Nakata A, Ikeda T, Otsuka Y, Kawahito J. (2014) Employment type, workplace interpersonal conflict, and insomnia: a cross-sectional study of 37,646 employees in Japan. Arch Environ Occup Health 69, 23–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yoshioka E, Saijo Y, Kita T, Satoh H, Kawaharada M, Kishi R. (2013) Effect of the interaction between employment level and psychosocial work environment on insomnia in male Japanese public service workers. Int J Behav Med 20, 355–64. [DOI] [PubMed] [Google Scholar]
- 19.Ministry of Health, Labour and Welfare. Comprehensive Survey of Living Conditions. http://www.mhlw.go.jp/english/database/db-hss/cslc.html. Accessed August 5, 2018.
- 20.Van Gastel A. (2018) Drug-induced insomnia and excessive sleepiness. Sleep Med Clin 13, 147–59. [DOI] [PubMed] [Google Scholar]
- 21.Ohayon MM, Partinen M. (2002) Insomnia and global sleep dissatisfaction in Finland. J Sleep Res 11, 339–46. [DOI] [PubMed] [Google Scholar]
- 22.Lexcen FJ, Hicks RA. (1993) Does cigarette smoking increase sleep problems. Percept Mot Skills 77, 16–8. [DOI] [PubMed] [Google Scholar]
- 23.Phillips BA, Danner FJ. (1995) Cigarette smoking and sleep disturbance. Arch Intern Med 155, 734–7. [PubMed] [Google Scholar]
- 24.McGee RE, Thompson NJ. (2015) unemployment and depression among emerging adults in 12 states, behavioral risk factor surveillance system, 2010. Prev Chronic Dis, 12, E38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rowshan Ravan A, Bengtsson C, Lissner L, Lapidus L, Björkelund C. (2010) Thirty-six-year secular trends in sleep duration and sleep satisfaction, and associations with mental stress and socioeconomic factors—results of the Population Study of Women in Gothenburg, Sweden. J Sleep Res 19, 496–503. [DOI] [PubMed] [Google Scholar]
- 26.Xiang YT, Ma X, Cai ZJ, Li SR, Xiang YQ, Guo HL, Hou YZ, Li ZB, Li ZJ, Tao YF, Dang WM, Wu XM, Deng J, Lai KYC, Ungvari GS. (2008) The prevalence of insomnia, its sociodemographic and clinical correlates, and treatment in rural and urban regions of Beijing, China: a general population-based survey. Sleep 31, 1655–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Riemann D, Spiegelhalder K, Feige B, Voderholzer U, Berger M, Perlis M, Nissen C. (2010) The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev 14, 19–31. [DOI] [PubMed] [Google Scholar]
- 28.Fabsitz RR, Sholinsky P, Goldberg J. (1997) Correlates of sleep problems among men: the Vietnam Era Twin Registry. J Sleep Res 6, 50–6. [DOI] [PubMed] [Google Scholar]