Abstract
Tibial plateau subchondral bone geometry has been associated with the risk of sustaining a non-contact ACL injury; however, little is known regarding the influence of the meniscus and articular cartilage interface geometry on risk. We hypothesized that geometries of the tibial plateau articular cartilage surface and meniscus were individually associated with the risk of non-contact ACL injury. In addition, we hypothesized that the associations were independent of the underlying subchondral bone geometry. MRI scans were acquired on 88 subjects that suffered non-contact ACL injuries (27 males, 61 females) and 88 matched control subjects that were selected from the injured subject’s teammates and were thus matched on sex, sport, level of play, and exposure to risk of injury. Multivariate analysis of the female data revealed that increased posterior-inferior directed slope of the middle articular cartilage region and decreased height of the posterior horn of the meniscus in the lateral compartment were associated with increased risk of sustaining a first time, non-contact ACL injury, independent of each other and of the slope of the tibial plateau subchondral bone. No measures were independently related to risk of non-contact ACL injury among males.
Injuries to the anterior cruciate ligament (ACL) of the knee are often immediately debilitating and can lead to post-traumatic osteoarthritis (PTOA) regardless of whether the ACL injuries are treated with surgical intervention or rehabilitation alone.1 Since current treatment options are ineffective in preventing PTOA, recent research has focused on reducing the incidence of ACL injuries. To achieve this it is necessary to thoroughly understand the risk factors for ACL injury, so that appropriate interventions can be developed and targeted at those most at risk. Risk factors for ACL injury are multifactorial and may be different for males and females.2 A few identified risk factors, such as neuromuscular control, are modifiable and may be intervened upon. Others risk factors, such as knee geometry, are not modifiable but may play a critical role in identifying individuals at increased risk for ACL injury who may benefit from alternative preventive strategies.
Tibial plateau subchondral bone geometry has been associated with knee biomechanics and ACL strain values, which influence ACL injury risk. Research has shown that increased posterior-inferior directed slope of the tibial plateau subchondral bone is associated with increased anterior translation of the tibia relative to the femur3 and increased ACL strain values4,5 in response to compressive loading of the knee. In addition, this increased posterior-inferior directed slope of the subchondral bone, primarily in the lateral compartment and in females, is associated with an increased risk of suffering an ACL injury.6–10
While previous reports have focused on analyses of subchondral bone geometry, these analyses are insufficient at depicting articular surface contact mechanics of the tibiofemoral joint11 and do not consider the importance of the meniscus on ACL loading.12 Consequently, it is unclear how the geometries of these complex interfaces affect knee biomechanics, ACL strain biomechanics, and the risk of suffering severe knee injury such as an ACL disruption. Since the subchondral bone geometry alone does not accurately depict articular surface contact mechanics of the tibiofemoral joint,11 investigation of the articular cartilage surface and meniscus geometries could provide an improved understanding of the mechanisms and risk of ACL trauma.
While meniscal resection has been shown to significantly increase ACL strain values in humans,12 little in known regarding the effects of meniscal and articular cartilage geometries. Geometric features of cartilage and menisci that have been associated with an increased ACL injury risk include: greater posterior-inferior orientation of sagittal plane profiles of the medial and lateral compartments of the tibial articular cartilage surfaces,13 decreased lateral compartment articular cartilage radius of curvature,14 and increased posterior-inferior directed slope of a line connecting the superior prominences of the anterior and posterior meniscal horns.15 The mechanism that these geometric features were related to ACL injury risk was considered to be biomechanically based and produced by a change in restraint of anterior translation and internal rotation of the tibia relative to the femur. The current study aimed to build on previous work and identify the influence of all tibial plateau contact interfaces on the risk of sustaining an ACL injury.
We hypothesized that the tibial plateau articular cartilage surface and menisci geometries are associated with the risk of suffering a non-contact ACL injury. Further, we hypothesized that these associations are independent of the slope of the underlying subchondral bone of the tibial plateau, are independent of each other, and differ between males and females.
METHODS
Our committee on human research in medical sciences at the University of Vermont approved this study and all participants provided written consent in advance of participation. This report is based on additional analysis of MRI data obtained from a subset of subjects that participated in a larger prospective cohort study with a nested, matched case-control analysis.16,17 In this investigation, athletes were followed prospectively throughout their season and those suffering a non-contact ACL injury were identified and participated in the study. Controls were selected from the injured subject’s teammates and were thus matched on sex, sport, level of play, and exposure to risk of injury. With this design, the type and amount of exposure to injury risk was controlled for between ACL-injured and uninjured control subjects. Bilateral MRI data were obtained on 88 first-time, non-contact, grade-III ACL injured subjects, and 88 matched controls (61 female and 27 male case-control pairs). Using a Phillips Achievea 3.0T MRI system (Phillips Medical Systems, Best, The Netherlands) with an 8-channel SENSE knee coil, sagittal T1-weighted MRIs (voxel size: 0.3 mm × 0.3 mm × 1.2 mm) were acquired on injured subjects after injury but prior to surgery and matched control subjects. The recruitment protocol and demographic information for this study population were described in our initial report.8
MRI segmentation of the tibial plateau subchondral bone, articular cartilage surface and posterior aspect of the meniscus was completed using a Cintiq 21UX digitizing tablet (Wacom Technology Corporation, Vancouver, WA) with OsiriX software (Pixmeo, Geneva, Switzerland, version 5.5.1) (Supplemental Text and Supplemental Fig. S1). The digitizing tablets have an LCD display resolution of 1600 by 1200 UXGA and a digitizing tablet resolution of 5080 lpi. Segmented data were post-processed using custom MATLAB code. First, data for each structure (initially acquired relative to the MRI scanners coordinate system) were transformed to a coordinate system that was fixed in the tibia. This approach allowed us to corrected for variable limb orientation in the MRI scanner during data acquisition so consistent measurements could be made between and within subjects (Supplemental Fig. S2).8 Next, two dimensional linear inter-polation was used to produce data in the para-sagittal, anteroposterior plane of the tibial coordinate system. Interpolated subchondral bone and articular cartilage surface slices were generated at 1.0 mm intervals in the medial-lateral direction and points were spaced by 1.0 mm in the anterior-posterior direction for each para-sagittal slice. Inter-polated meniscus slices were generated at 1.0 mm intervals in the medial-lateral direction, but points were spaced by 0.3 mm in the anterior-posterior direction for each parasagittal slice. The articular cartilage profiles of both the medial and lateral compartments of the tibial plateau displayed a region of concavity where the femoral cartilage and tibial cartilage surfaces were in contact. The depth of concavity was calculated in each sagittal slice of the tibia. Geometric measurements were made on the slice of maximum depth of concavity of the cartilage profile. Identification and characterization of this location has been described previously.13
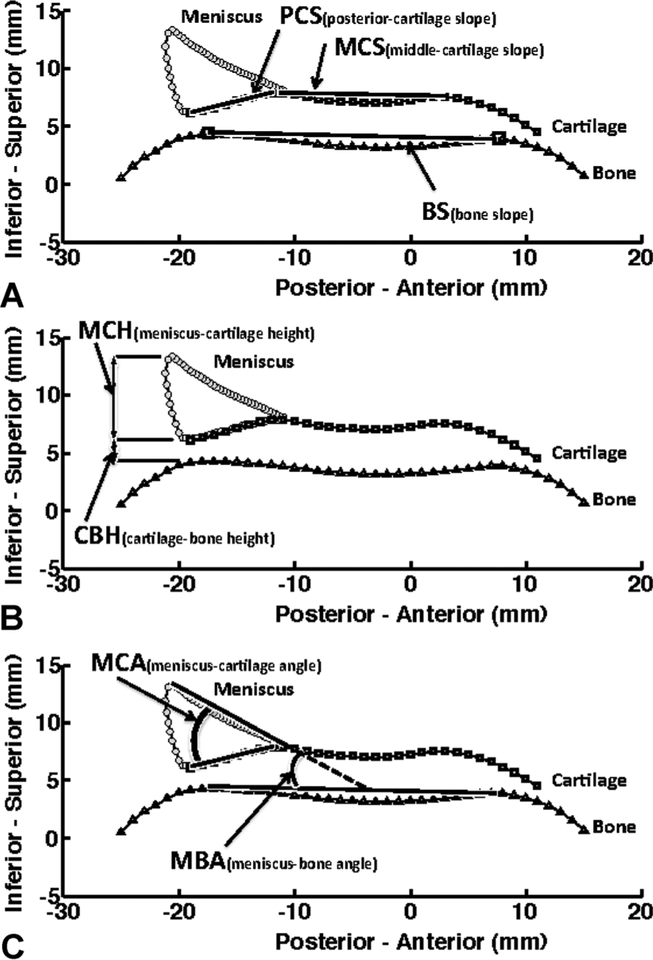
The middle cartilage slope was defined as the angle between a line that joined the most superior, anterior, and posterior located prominences of the middle articular cartilage surface region of the tibial plateau (where contact with the femur occurs with the knee in extension) and the anterior-posterior directed axis of the tibia. The posterior-inferior cartilage slope was defined as the angle between a best-fit line to the posterior articular cartilage surface region of the tibial plateau (underlying the posterior meniscal horn) and the anterior-posterior directed axis of the tibia (Fig. 1A). The meniscus-cartilage height was measured from the superior most point of the posterior meniscal horn to the surface of the underlying articular cartilage. The articular cartilage-bone height was measured from the posterior most point of the articular cartilage surface profile down to the underlying subchondral bone (Fig. 1B). The posterior meniscus-subchondral bone angles and posterior meniscus-articular cartilage angles were measured as the angle of the wedge shaped profile formed between of the superior surface of the posteri- or meniscus and the subchondral bone surface and the articular cartilage surface, respectively (Fig. 1C). Using the approach that has been previously described,8 medial and lateral compartment measurements of subchondral bone slope were also made at this slice location (Supplemental Text and Supplemental Fig. S3).
Figure 1.
Segmented data for meniscus (dots), articular cartilage (squares), and underlying subchondral bone (triangles) in the lateral (Lat) compartment and tibial coordinate system inferior-superior axis (vertical) and posterior-anterior axis (horizontal). All measures also replicated in the medial (Med) compartment. (A) Middle and posterior cartilage slopes (MCS and PCS) and subchondral bone slope (BS) measured relative to the posterior-anterior axis. (B) Height of the posterior meniscus measured relative to cartilage (MCH) and height of the posterior cartilage measured relative to bone (CBH). (C) Posterior meniscus wedge angle measured relative to cartilage (MCA) and relative to subchondral bone (MBA).
Articular cartilage and menisci are viscoelastic structures that deform in response to contact stress in a time dependent manner.18 Due to differences in orientation between knees of ACL-injured and control subjects in this study,19 it was important to consider the orientation of the tibia relative to the femur, and subsequently the location of the contact stress across the tibiofemoral joint during MRI data acquisition. Consequently, the location and orientation of the tibial coordinate system relative to that of the femur were measured and used in the statistical analysis to determine if they had an influence on the risk associated with tibial plateau articular cartilage surface and meniscus geometry. These included the internal-external rotation angle, flexion-extension angle, anterior-posterior position and medial-lateral position of the tibia relative to the femur.
Intra- and inter-observer reliability of the measurement techniques were investigated using data collected from measurements made at two time-points on a random subset of 25 knees. These measurements were made by two investigators; the first collected data at both time-points to asses intra-observer reliability, and the second collected data at the first time point to asses inter-observer reliability. Reliability of each outcome was established using variance component analysis to estimate the variability between examiners, within examiners and between subjects, and Intraclass Correlation Coefficients (ICCs) were calculated (Supplemental Table S1). ICCs for intra-observer reliability ranged between 0.75 and 0.96, indicating good repeatability. Inter-observer ICCs were lower, ranging between 0.55 and 0.91, but all measurements reported in this investigation were made by the same individual (Supplemental Table S1).
Statistical Methods
The geometries of the articular cartilage surface and subchondral bone have been shown to change soon after an ACL injury,13,20 likely accounting for differences in articular cartilage and subchondral bone geometry that were found between the injured and uninjured knees of the ACL injured subjects in the current study. No differences existed between both uninjured knees within control subjects (Supplemental Text and Supplemental Tables S2–S4). Consequently, analyses of risk were completed using data obtained from the uninjured leg of ACL-injured subjects and the corresponding leg, left or right, of matched control subjects.
To test our hypothesis that the geometries of the tibial plateau articular cartilage surface and meniscus are individually associated with the risk of non-contact ACL injury, univariate conditional logistic regression was used to test the associations between articular cartilage and meniscus geometry, and the risk of suffering a non-contact ACL injury. Pearson correlation coefficients were computed to examine linear correlations between variables. Multivariate conditional logistic regression was used to test whether the effects of the cartilage and meniscus variables that were associated with risk of injury were independent of each other and of the slope of the tibial plateau subchondral bone. Odds ratios (ORs) and 95% confidence intervals (CI) were used to quantify the associations with risk. Analyses were performed separately for females and males, and had 80% power to detect relative risks of 1.81 in females and 2.65 in males, per each standard deviation of increase or decrease in the variable being analyzed. Secondary analyses examined the position of the tibia relative to the femur during MRI data acquisition, body weight, and BMI as covariates to assess their influence on the relationship between the geometric measures and ACL injury risk.
RESULTS
Summary statistics for each measurement made on the uninjured side are presented in Table 1. Univariate analysis of data obtained from females demonstrated that the lateral compartment middle and posterior cartilage slopes were directly associated with ACL injury risk (ORs = 1.303 and 1.155 per degree increase, p = 0.0001 and 0.0003, respectively) while the lateral compartment meniscus-bone angle (OR = 0.863 per degree increase, p = 0.004), and the lateral and medial compartment meniscus-cartilage height (OR = 0.438 and 0.629 per millimeter increase, p = 0.01 and 0.048, respectively), were inversely related to risk of suffering an ACL injury (Table 2). Univariate analysis of the males as a separate group revealed that only the lateral compartment cartilage-bone height was significantly inversely associated with risk of suffering an ACL injury (OR = 0.243 per millimeter increase, p = 0.04) (Table 2). Subsequent analyses that included the position of the tibia relative to the femur during the MRI acquisition, body weight or BMI as covariates produced similar results.
Table 1.
Mean ± Standard Deviation (SD) Data for Each Outcome Using the Contralateral Uninjured Limb of ACL Injured Subjects and Corresponding Limb of Control Subjects
| Female | Male | |||
|---|---|---|---|---|
| Variable | ACL-Injured (Mean ± SD) |
Control (Mean ± SD) |
ACL-Injured (Mean ± SD) |
Control (Mean ± SD) |
| LatMCS (degrees) | 0.6 ± 3.8 | −3.7 ± 4.2 | −1.3 ± 3.5 | −1.8 ± 3.8 |
| LatPCS (degrees) | 13.3 ± 6.4 | 8.5 ± 5.6 | 9.5 ± 5.7 | 9.3 ± 6.1 |
| LatMCA (degrees) | 40.3 ± 5.3 | 40.5 ± 6.3 | 38.5 ± 5.6 | 40.3 ± 5.5 |
| LatMBA (degrees) | 27.9 ± 4.2 | 30.6 ± 4.7 | 26.8 ± 3.9 | 28.5 ± 4.0 |
| LatMCH (mm) | 6.3 ± 0.7 | 6.6 ± 0.8 | 6.8 ± 0.9 | 7.1 ± 0.7 |
| LatCBH (mm) | 2.7 ± 0.6 | 2.7 ± 0.5 | 2.8 ± 0.4 | 3.1 ± 0.6 |
| MedMCS (degrees) | −0.6 ± 2.8 | −0.5 ± 3.5 | −1.6 ± 2.5 | −0.8 ± 3.5 |
| MedPCS (degrees) | −6.0 ± 3.3 | −6.6 ± 3.4 | −6.5 ± 3.4 | −6.6 ± 3.1 |
| MedMCA (degrees) | 21.7 ± 3.3 | 21.9 ± 3.6 | 22.4 ± 3.5 | 21.7 ± 4.1 |
| MedMBA (degrees) | 24.1 ± 2.8 | 24.6 ± 2.8 | 24.3 ± 2.8 | 24 ± 3.7 |
| MedMCH (mm) | 5.2 ± 0.8 | 5.5 ± 1.0 | 5.9 ± 1.1 | 6.0 ± 1.2 |
| MedCBH (mm) | 1.6 ± 0.4 | 1.6 ± 0.5 | 1.7 ± 0.6 | 1.9 ± 0.4 |
Data are presented for female subjects and male subjects as separate groups.
Table 2.
Univariate Associations Between Measurements of Meniscus and Articular Cartilage Geometry and Risk of Suffering a Non-Contact ACL Injury
| Female Subjects | Male Subjects | |||
|---|---|---|---|---|
| Variable | Odds Ratio (95% CI) | p-value | Odds Ratio (95% CI) | p-value |
| LatMCS (degrees) | 1.303 (1.142–1.486) | 0.0001 | 1.054 (0.895–1.241) | 0.53 |
| LatPCS (degrees) | 1.155 (1.068–1.25) | 0.0003 | 1.005 (0.918–1.099) | 0.92 |
| LatMCA (degrees) | 0.993 (0.93–1.061) | 0.84 | 0.939 (0.844–1.044) | 0.25 |
| LatMBA (degrees) | 0.863 (0.781–0.953) | 0.004 | 0.900 (0.782–1.036) | 0.14 |
| LatMCH (mm) | 0.438 (0.235–0.818) | 0.01 | 0.546 (0.23–1.298) | 0.17 |
| LatCBH (mm) | 1.015 (0.526–1.96) | 0.96 | 0.243 (0.061–0.968) | 0.04 |
| MedMCS (degrees) | 0.985 (0.879–1.104) | 0.80 | 0.925 (0.778–1.099) | 0.37 |
| MedPCS (degrees) | 1.049 (0.941–1.169) | 0.39 | 1.012 (0.85–1.204) | 0.89 |
| MedMCA (degrees) | 0.982 (0.88–1.096) | 0.74 | 1.085 (0.905–1.302) | 0.38 |
| MedMBA (degrees) | 0.914 (0.788–1.059) | 0.23 | 1.041 (0.853–1.27) | 0.69 |
| MedMCH (mm) | 0.629 (0.397–0.996) | 0.048 | 0.929 (0.547–1.577) | 0.78 |
| MedCBH (mm) | 0.874 (0.362–2.112) | 0.76 | 0.635 (0.233–1.725) | 0.37 |
The results are from conditional logistic regression analysis of data using the uninjured knees of the ACL injured subjects and the corresponding side of the matched control subjects. Results presented for females and males as separate groups.
Univariate analysis also revealed that the lateral compartment slope of the subchondral bone of the tibial plateau was significantly associated with ACL injury risk when considering the females as a group (OR = 1.203, 95% CI = 1.065−1.359, p = 0.003), but not in the males (OR = 1.023, 95% CI = 0.862−1.213, p = 0.79) (Supplemental Text and Supplemental Table S5) .The medial compartment slope of the subchondral bone was not associated with risk for either sex (Supplemental Table S4). When the cartilage and meniscus measurements were adjusted for the slope of the subchondral bone, most of the associations with ACL injury risk that were observed in the univariate analyses remained significant and many were strengthened (Table 3).
Table 3.
Associations Between Measurements of Meniscus and Articular Cartilage Geometry and Risk of Suffering a Non-Contact ACL Injury After Adjustment for the Slope of the Underlying Subchondral Bone
| Female Subjects | Male Subjects | |||
|---|---|---|---|---|
| Variable | Adjusted Odds Ratio (95% CI) | p-value | Adjusted Odds Ratio (95% CI) | p-value |
| LatMCS (degrees) | 1.271 (1.105–1.462) | 0.001 | 1.061 (0.871–1.293) | 0.55 |
| LatPCS (degrees) | 1.141 (1.024–1.272) | 0.02 | 0.995 (0.888–1.116) | 0.94 |
| LatMCA (degrees) | 0.938 (0.865–1.018) | 0.12 | 0.925 (0.824–1.037) | 0.18 |
| LatMBA (degrees) | 0.800 (0.707–0.906) | 0.0004 | 0.880 (0.755–1.025) | 0.10 |
| LatMCH (mm) | 0.357 (0.167–0.763) | 0.008 | 0.546 (0.230–1.295) | 0.17 |
| LatCBH (mm) | 0.602 (0.270–1.345) | 0.22 | 0.105 (0.014–0.767) | 0.03 |
| MedMCS (degrees) | 0.872 (0.683–1.113) | 0.27 | 0.866 (0.633–1.184) | 0.37 |
| MedPCS (degrees) | 1.099 (0.913–1.321) | 0.32 | 1.141 (0.844–1.542) | 0.39 |
| MedMCA (degrees) | 0.982 (0.879–1.096) | 0.74 | 1.090 (0.908–1.310) | 0.36 |
| MedMBA (degrees) | 0.912 (0.787–1.058) | 0.22 | 1.048 (0.856–1.282) | 0.65 |
| MedMCH (mm) | 0.601 (0.373–0.967) | 0.04 | 0.985 (0.537–1.807) | 0.96 |
| MedCBH (mm) | 0.853 (0.350–2.082) | 0.73 | 0.652 (0.237–1.791) | 0.41 |
The results are from conditional logistic regression analysis of data using the uninjured knees of the ACL injured subjects and the corresponding side of the matched control subjects.
There were statistically significant relationships between many of the cartilage and meniscus measurements made within the lateral and medial compartments. Although the magnitude of the correlation was generally moderate or small, there was substantial correlation (r > .50) between several of the lateral compartment measurements made in females. The meniscus-bone angle was correlated with the meniscus cartilage angle (r = 0.62) and both were correlated with meniscus-cartilage height and cartilage-bone height (r’s ranging from 0.51 to 0.52). In addition, the meniscus-cartilage angle was correlated with posterior cartilage slope (r = .82), which was also related to middle cartilage slope (r = 0.59). Medial compartment meniscus-bone angle and meniscus-cartilage angle were also substantially correlated in females (r = 0.82) and both were correlated with meniscus-cartilage height (r = .55 and r = .60, for meniscus-bone angle and meniscus-cartilage angle, respectively) but not with cartilage-bone height. Correlations between measurements were lower in males, but meniscus-cartilage angle and posterior-cartilage slope were substantially correlated in the lateral compartment (r = 0.71), while bone-meniscus angle and meniscus-cartilage angle were substantially correlated in the medial compartment (r = 0.82).
Multivariate analysis that included both the cartilage and meniscus measurements was performed to identify which factors were independently associated with ACL injury risk. In females, lateral compartment middle cartilage slope and meniscus-cartilage height were found to be independently associated (p = 0.003 and 0.044, respectively) with risk of ACL injury after adjustment for the subchondral bone slope (Table 4). As in the univariate analyses, the lateral compartment middle cartilage slope was directly associated with risk while the meniscus-cartilage height was inversely associated with risk. A millimeter decrease in the height of the posterior meniscus and a degree increase in the posterior-inferior directed slope of the middle articular cartilage surface were associated with a 144% and 25% increase in risk, respectively. Additional analysis demonstrated that the effects of the lateral compartment middle cartilage slope and meniscus-cartilage height on the risk of ACL injury were not influenced by body weight, BMI, or the position of the tibia relative to the femur during acquisition of the MRI data. Multivariate analysis of the data obtained from the males found no combination of measures that were independently associated with the risk of suffering an ACL injury (Table 4).
Table 4.
Multivariate Associations Between Measurements of Meniscus and Articular Cartilage Geometry and Risk of Suffering a Non-Contact ACL Injury Unadjusted and Adjusted for the Slope of the Underlying Subchondral Bone (LatBS)
| Unadjusted Model | Model Adjusted for LatBS | |||
|---|---|---|---|---|
| Variable | Odds Ratio (95% CI) | p-value | Odds Ratio (95% CI) | p-value |
| Female subjects only | ||||
| LatMCS (degrees) | 1.30 (1.13–1.49) | 0.0002 | 1.25 (1.08–1.45) | 0.003 |
| LatMCH (mm) | 0.46 (0.21–1.04) | 0.06 | 0.41 (0.17–0.98) | 0.04 |
| LatBS (degrees) | 1.12 (0.94–1.32) | 0.21 | ||
| Male subjects only | ||||
| LatMCS (degrees) | 1.04 (0.88–1.24) | 0.61 | 1.05 (0.85–1.28) | 0.67 |
| LatMCH (mm) | 0.56 (0.23–1.33) | 0.19 | 0.56 (0.23–1.33) | 0.19 |
| LatBS (degrees) | 1.00 (0.81–1.23) | 0.98 | ||
The results are from conditional logistic regression analysis of data using the uninjured knees of the ACL injured subjects and the corresponding side of the matched control subjects. Variables in the models are independently predictive of risk. Results are presented for females and males as separate groups.
DISCUSSION
Previous reports and meta-analyses have concluded that an increased posterior-inferior directed slope of the subchondral bone portion of the tibial plateau is associated with an increased risk of ACL injury,9,10 primarily in the lateral compartment of the tibial plateau7,21,22 and often for females but not in males.6–8 The findings from the current study build on this prior work by revealing that measurements of the tibial plateau articular cartilage surface and menisci geometry also influence risk of injury. Both were stronger independent predictors of injury than the subchondral bone slope, and their relationships with ACL injury risk were different for males and females.
In univariate analyses of the data obtained from females, an increased posterior-directed slope of the middle- and posterior-articular cartilage regions, decreased meniscus-subchondral bone angle in the lateral compartment and decreased meniscus-articular cartilage height in both the lateral and medial compartments were associated with an increase in the risk of suffering an ACL injury. In univariate analyses of data obtained from the males, only the lateral compartment articular cartilage-subchondral bone height was found to have a significant association with risk of ACL injury.
Multivariate analysis of female data revealed that the lateral compartment middle articular cartilage slope and the meniscus-cartilage height were independently associated with risk of suffering an ACL injury after adjustment for subchondral bone slope. These measures of meniscus and articular cartilage were associated with risk of injury independent of tibial position relative to the femur during MRI acquisition. Multivariate analysis of the male data revealed that none of the measurements of articular cartilage or meniscus geometry were independently associated with risk.
In our prior work,13 the sagittal-plane profile of the tibial articular cartilage surface was characterized by fitting polynomials equations, whose coefficients were related to the risk of suffering ACL injury. The polynomial equation that was fit to the lateral compartment articular cartilage surface described a posterior-inferior orientation in the ACL-injured group (characterized by a positive first-order linear term) and a posterior-superior orientation in the control group (characterized by a negative first-order linear term).13 The current study confirmed that the sagittal-plane orientation, or slope, of the lateral compartment articular cartilage surface was associated with the risk of suffering an ACL injury in females. During transmission of compressive loads from the distal femur to the tibial plateau, such as landing from a jump, a greater posterior-inferior oriented slope of the articular cartilage would provide less resistance to anterior translation of the tibia relative to the femur and result in greater ACL strain values.4,5 While this observation suggest a direct link between the biomechanics of contact stress transmission across the knee and risk of ACL injury, it remains unclear whether this mechanism influences risk of injury through a single loading event, through repetitive loading events over time that produce fatigue failure of the ACL, or some combination of both.
Hudek et al.15 identified a relationship between meniscus geometry and ACL injury risk by defining a posterior directed slope of the line that passed through the peaks of the anterior and posterior meniscal horns. We focused on measurement of the posterior meniscal horn. The rationale for this was based on observations that the posterior meniscal horns transmit higher contact stresses throughout flexion,21 and consequently would provide resistance to anterior translation of the tibia relative to the femur. Our findings suggest that the geometry of the posterior meniscal horn could have been the primary mechanism for the previously described association between the slope of the line that passed though the peaks of the anterior and posterior meniscal horns and risk of suffering an ACL injury. Future research should investigate the relationships between articular cartilage and meniscus geometry and the biomechanics of the ACL and knee.
Findings from this study add to the growing body of literature that suggests the factors associated with the risk of suffering a non-contact ACL injury are different between males and females.6–8,13 Statistical analysis that was performed with adjustment for subject body weight and BMI did not alter the risk associated with tibial plateau geometry in females, suggesting that the difference in results for males and females is not due to their differing size. Sex specific associations could instead reflect inherent differences in characteristics of tibial plateau articular cartilage and meniscus geometry between males and females. Previous studies have reported similar male-female differences in tibiofemoral geometry,15,22–25 as well as knee laxity26 and lower extremity alignment.27,28
A potential limitation of the study is that it was not possible to acquire MRI’s of the involved knee prior to the injury, and thus determine the extent to which the injury modified the measurements of meniscus, cartilage, and bone geometry. Side-to-side differences were found in ACL-injured subjects but not the control subjects. Consequently, the contralateral healthy knee was used as a surrogate for the condition of the injured knee prior to injury. Our finding of no differences in measurements of meniscus, cartilage, and bone geometry between knees of the control subjects provides convincing evidence in support of the approach of using the corresponding measurements obtained from the contralateral healthy knee of the ACL injured subjects as an accurate measure of the ACL injured knee prior to injury. Another potential limitation is that MRI’s were obtained with the knee unloaded. However, only very small deformations of cartilage from the non-weight bearing scenario of MRI acquisition would be expected when the injury occurs. This is supported by observations of minimal deformations in articular cartilage after repeated high impact loads (a 7% decrease in overall cartilage volume)29 or after various exercises (a 7.2% decrease in lateral tibial cartilage volume after jumping exercises).29 Further, the primary mechanisms in which the articular cartilage and menisci support the large magnitudes of compressive stress that are developed across the tibiofemoral joint at the time of ACL trauma are through pressurization of the interstitial fluid in cartilage and the development of drag force of interstitial fluid flow through the cartilage matrix. The ACL injuries that we studied occurred over very short time intervals during which the pressure and drag forces were very high, and therefore, we expect there was very little fluid flow through cartilage and as a result, very little deformation of this structure. From these perspectives, the geometry of cartilage measured with the knee unloaded in the MRI scanner may be an accurate representation of the geometry of the knee at the time of injury. Strengths and limitations of the overall study have been previously discussed.8,13,16
Studies of modifiable and non-modifiable risk factors for ACL injury are both important. Changing a modifiable risk factor has the immediate satisfaction of lowering the risk of injury. However, identifying all risk factors including those that are not modifiable can decrease injury rates as well. Non-modifiable risk factors can be used to identify those at greatest risk for injury and for the development of new approaches that can mitigate risk.2,30 For example, individuals that are identified as having a large number of non-modifiable risk factors (increased slope of the articular cartilage surface combined with decreased meniscus wedge angle, and a positive family history of ACL injury etc.) could decrease ACL injury risk by decreasing injury exposure (decreasing scrimmage/game time and changing off season workouts to emphasize skill development over game participation), by targeting individuals for monitored neuromuscular training programs, or the use of equipment that can help attenuate the impulsive loads transmitted across the knee and ACL. Consequently, understanding who is at highest risk for injury provides an opportunity to decrease injury exposure and target athletes who need extra monitored training.2,30–32
The study findings suggest that the geometries of the articular cartilage and meniscus are associated with the risk of sustaining an ACL injury in females. The influence of the overlying articular cartilage surface and meniscus geometries on risk is a stronger independent predictor and not simply a reflection of the underlying subchondral bone. Consequently, such measures should be considered in future studies that assess the role of knee joint geometry on its biomechanical behavior and subsequent influence on an individual’s risk of sustaining an ACL injury.
Supplementary Material
ACKNOWLEDGMENTS
Each author certifies that he or she has no commercial associations that might pose a conflict of interest in connection with the submitted article. The research was performed at the McClure Musculoskeletal Research Center of the University of Vermont College of Medicine Department of Orthopaedics and Rehabilitation. Financial support includes research funding through NIH R01-AR050421 and MRI equipment funding through DOE SC 0001753.
Grant sponsor: NIH; Grant number: R01-AR050421; Grant sponsor: MRI; Grant number: DOE SC 0001753.
Footnotes
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article at the publisher’s web-site.
REFERENCES
- 1.Lohmander LS, Englund PM, Dahl LL, et al. 2007. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J sports Med 35: 1756–1769. [DOI] [PubMed] [Google Scholar]
- 2.Smith HC, Vacek P, Johnson RJ, et al. 2012. Risk factors for anterior cruciate ligament injury: a review of the literature - part 1: neuromuscular and anatomic risk. Sports health 4:69–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dejour H, Bonnin M. 1994. Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg Br 76:745–749. [PubMed] [Google Scholar]
- 4.Lipps DB, Oh YK, Ashton-Miller JA, et al. 2012. Morphologic characteristics help explain the gender difference in peak anterior cruciate ligament strain during a simulated pivot landing. Am J Sports Med 40:32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McLean SG, Oh YK, Palmer ML, et al. 2011. The relationship between anterior tibial acceleration, tibial slope, and ACL strain during a simulated jump landing task. J Bone Joint Surg Am 93:1310–1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hohmann E, Bryant A, Reaburn P, et al. 2011. Is there a correlation between posterior tibial slope and non-contact anterior cruciate ligament injuries? Knee Surg Sports Traumatol Arthrosc 19:S109–114. [DOI] [PubMed] [Google Scholar]
- 7.Todd MS, Lalliss S, Garcia E, et al. 2010. The relationship between posterior tibial slope and anterior cruciate ligament injuries. Am J Sports Med 38:63–67. [DOI] [PubMed] [Google Scholar]
- 8.Beynnon BD, Hall JS, Sturnick DR, et al. 2014. Increased Slope of the Lateral Tibial Plateau Subchondral Bone Is Associated With Greater Risk of Noncontact ACL Injury in Females but Not in Males: A Prospective Cohort Study With a Nested, Matched Case-Control Analysis. Am J Sports Med 42:1039–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wordeman SC, Quatman CE, Kaeding CC, et al. 2012. In vivo evidence for tibial plateau slope as a risk factor for anterior cruciate ligament injury: a systematic review and meta-analysis. Am J Sports Med 40:1673–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zeng C, Cheng L, Wei J, et al. 2014. The influence of the tibial plateau slopes on injury of the anterior cruciate ligament: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 22:53–65. [DOI] [PubMed] [Google Scholar]
- 11.DeFrate LE, Sun H, Gill TJ, et al. 2004. In vivo tibiofemoral contact analysis using 3D MRI-based knee models. J Biomech 37:1499–1504. [DOI] [PubMed] [Google Scholar]
- 12.Spang JT, Dang AB, Mazzocca A, et al. 2010. The effect of medial meniscectomy and meniscal allograft transplantation on knee and anterior cruciate ligament biomechanics. Arthroscopy 26:192–201. [DOI] [PubMed] [Google Scholar]
- 13.Beynnon BD, Vacek PM, Sturnick DR, et al. 2014. Geometric profile of the tibial plateau cartilage surface is associated with the risk of non-contact anterior cruciate ligament injury. J Orthop Res 32:61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wahl CJ, Westermann RW, Blaisdell GY, et al. 2012. An association of lateral knee sagittal anatomic factors with non-contact ACL injury: sex or geometry? J Bone Joint Surg Am 94:217–226. [DOI] [PubMed] [Google Scholar]
- 15.Hudek R, Fuchs B, Regenfelder F, et al. 2011. Is noncontact ACL injury associated with the posterior tibial and meniscal slope? Clin Orthop Relat Res 469:2377–2384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith HC, Johnson RJ, Shultz SJ, et al. 2012. A prospective evaluation of the Landing Error Scoring System (LESS) as a screening tool for anterior cruciate ligament injury risk. Am J Sports Med 40:521–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goetschius J, Smith HC, Vacek PM, et al. 2012. Application of a clinic-based algorithm as a tool to identify female athletes at risk for anterior cruciate ligament injury: a prospective cohort study with a nested, matched case-control analysis. Am J Sports Med 40:1978–1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mow VCGW Chen FH., 2005. Structure and function of articular cartilage and meniscus In: Van C. Mow RH, editor Basic orthopaedic biomechanics and mechano-biology, 3 ed Philadelphia, PA: Lippincott Williams & Wilkins; pp. 181–258. [Google Scholar]
- 19.Carter J, Sturnick DR, Vacek PM, et al. 2014. Geometry of the distal femur and patellar tendon orientation in association with the risk of suffering an ACL injury. To be submitted to Am J Sports Med [Google Scholar]
- 20.Tourville TW, Johnson RJ, Slauterbeck JR, et al. 2013. Assessment of early tibiofemoral joint space width changes after anterior cruciate ligament injury and reconstruction: a matched case-control study. Am J Sports Med 41:769–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Walker PS, Erkman MJ., 1975. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res 109:184–192. [DOI] [PubMed] [Google Scholar]
- 22.Hashemi J, Chandrashekar N, Gill B, et al. 2008. The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Surg Am 90:2724–2734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murshed KA, Cicekcibasi AE, Karabacakoglu A, et al. 2005. Distal femur morphometry: a gender and bilateral comparative study using magnetic resonance imaging. Surg Radiol Anat 27:108–112. [DOI] [PubMed] [Google Scholar]
- 24.van Diek FM, Wolf MR, Murawski CD, et al. 2013. Knee morphology and risk factors for developing an anterior cruciate ligament rupture: an MRI comparison between ACL-ruptured and non-injured knees. Knee Surg Sports Traumatol Arthrosc [DOI] [PubMed] [Google Scholar]
- 25.Anderson AF, Dome DC, Gautam S, et al. 2001. Correlation of anthropometric measurements, strength, anterior cruciate ligament size, and intercondylar notch characteristics to sex differences in anterior cruciate ligament tear rates. Am J Sports Med 29:58–66. [DOI] [PubMed] [Google Scholar]
- 26.Uhorchak JM, Scoville CR, Williams GN, et al. 2003. Risk factors associated with noncontact injury of the anteri- or cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med 31:831–842. [DOI] [PubMed] [Google Scholar]
- 27.Nguyen AD, Shultz SJ., 2007. Sex differences in clinical measures of lower extremity alignment. J Orthop Sports Phys Ther 37:389–398. [DOI] [PubMed] [Google Scholar]
- 28.Shultz SJ, Nguyen AD, Schmitz RJ., 2008. Differences in lower extremity anatomical and postural characteristics in males and females between maturation groups. J Orthop Sports Phys Ther 38:137–149. [DOI] [PubMed] [Google Scholar]
- 29.Eckstein F, Lemberger B, Gratzke C, et al. 2005. In vivo cartilage deformation after different types of activity and its dependence on physical training status. Ann Rheum Dis 64:291–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shultz SJ, Schmitz RJ, Benjaminse A, et al. 2012. ACL Research Retreat VI: an update on ACL injury risk and prevention. J Athl Train 47:591–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Griffin LY, Agel J, Albohm MJ, et al. 2000. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg 8:141–150. [DOI] [PubMed] [Google Scholar]
- 32.Gilchrist J, Mandelbaum BR, Melancon H, et al. 2008. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am J Sports Med 36:1476–1483. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.