Abstract
Body mass index (BMI) has been used for years by clinicians to approximate total body fat. However, the body adiposity index (BAI), body adiposity index from the FELS longitudinal study (BAIFELS), and an equation developed by Deurenberg et al. (BFD) were created recently to offset BMI’s limitations and accurately estimate percent body fat (%BF). The prevalence of overweight and obese Caucasian men is increasing in the United States; currently, there is no established way to quickly and accurately predict their %BF. Purpose: To compare the existing %BF equations (BAI, BAIFELS, and BFD) to measured %BF via air displacement plethysmography (ADP) in order to determine the most accurate way to predict %BF in overweight and obese Caucasian men. Methods: Four hundred and fifty-two Caucasian men aged from 18 to 76, with a BMI of 25.0 to 42.4 kg/m2, participated in this study. Height, weight, waist circumference, hip circumference, and body composition using ADP were measured on each participant. These measurements were inserted into the three equations to determine any differences between the equations and the actual %BF measured by ADP. Results: Differences in %BF between ADP and the BAI (p < 0.001) and ADP and the BAIFELS (p < 0.001) were discovered. While no differences (p = 1.00) between ADP and BFD existed. Conclusion: In a population of overweight and obese Caucasian adults from the United States, the BAI and BAIFELS are not appropriate to predict %BF while the BFD prediction equation proved worthy of consideration.
Keywords: Anthropometrics, Fat Distribution, Bod Pod
INTRODUCTION
The prevalence of obesity began increasing during the 1970s in the United States, and currently continues to show no signs of improvement (9). Obesity is becoming more common among adults, especially men, in the United States, and can be measured and diagnosed in multiple ways (9). There are many different techniques to assess body composition, total body mass, or total body fat such as: skinfolds, densitometry, hydrostatic weighing, dual-energy X-ray absorptiometry (DEXA), bioelectrical impedance, and body mass index (BMI). BMI is most commonly used in clinical settings and large groups due to administering ease for health care providers and simplicity when calculating total body mass (10, 19, 28). It has previously been reported that physician face-to-face time with patients averages about 19.7 minutes (27). Therefore, to estimate body fat using anything other than BMI (mass to height ratio) in clinical settings is not ideal.
BMI can be calculated after obtaining height and weight on an individual. It is calculated by dividing weight (kg) by height (m2). Once BMI is calculated, it can be assigned a classification. Those with a BMI between 25.0–29.9 kg/m2 are considered overweight, while those with a BMI greater than or equal to 30.0 kg/m2 are obese. Although BMI is commonly studied and used, it has significant limitations. While relying on height and weight allow for an easy measurement, it also creates the main source of error. BMI does not compartmentalize body weight, which means it cannot differentiate between lean and fat mass (11). This can lead to overestimations in a muscular athlete’s total body fat as well as the inability to properly assess an obese individual’s total body fat (11, 31, 32, 34, 39). BMI also does not take into account sex. Females tend to store more fat mass while males often have more lean mass, but both can have the same estimated body fatness when using BMI (13, 21, 36). Additionally, older individuals tend to carry more fat mass than younger individuals, but they can also both have the same estimated body fatness using BMI (34). There have been attempts to reduce these limitations in BMI by creating BMI equations which consider physical activity and ethnicity to predict %BF. However, other techniques, like skinfolds and the DEXA, have been found to predict %BF more accurately than the BMI equations can predict total body fatness (8, 30).
Therefore, to combat all of the BMI limitations, the Body Adiposity Index (BAI) was developed in 2012 (2). We previously found overestimations in percent body fat (%BF) when using the original BAI equation and a variation equation taken from the FELS longitudinal study (BAIFELS) (3). Alternative equations have been developed in attempts to accurately determine %BF. One such equation was developed by Deurenberg et al. (BFD). Although slightly overestimating %BF, the BFD equation considers age and sex, giving it the potential to be a more accurate way of predicting %BF (5).
Research has shown the BAI has demonstrated significant disagreements between predicted %BF and measured %BF via the DEXA and air displacement plethysmography (ADP) (3, 4, 15, 29, 33). BMI has even occasionally been shown to predict total body adiposity better than the BAI (20). However, many studies have concluded the BAI to be superior to BMI as a predictor of adiposity (18, 22, 37).
Therefore, the purpose of this study was to use ADP to determine which existing %BF equation (BAI, BAIFELS, and BFD) is the most suitable for a population of overweight and obese Caucasian men. By limiting the participants according to sex and a specific %BF range, we were able to accurately accomplish this. Based on our previous findings, we predicted all measures, from each prediction equation, would be significantly different from ADP (3).
METHODS
Participants
Four hundred and fifty-two (452) overweight and obese Caucasian males participated in this study. Participants included males aged 18 – 76 with a BMI that ranged between 25.0 to 42.4 kg/m2. Prior to testing, participants were asked to refrain from caffeine and alcohol for 24 hours. Participants were also asked to fast for two hours and only permitted to drink water ad libitum during this time. Mean participant characteristics are presented in Table 1. The exclusion criteria included being female, BMI less than 25 and greater than 50 kg/m2, being under the age of 18 yrs, clinically detectable edema, physical amputations, and refusal to give informed consent. The study was approved for completion by the local Institutional Review Board at The University of Utah. A minimum of 161 participant, determined by conducting a power analyses using G*power (Version 3.1.9.3), were required to identify a small effect (power = 0.80, alpha = 0.05).
Table 1.
Descriptive statistics.
| Mean | SD | |
|---|---|---|
| Age (yrs) | 37.15 | 9.91 |
| Height (m) | 1.79 | 0.09 |
| Weight (kg) | 93.47 | 14.20 |
| WC (cm) | 94.99 | 10.52 |
| HC (cm) | 100.24 | 8.95 |
| BF (%) | 27.20 | 7.70 |
| BAI | 23.92 | 4.85 |
| BAIFELS | 23.12 | 6.28 |
| BMI (kg/m2) | 28.99 | 3.36 |
| BFD | 27.13 | 4.85 |
yrs = years; m = meters; kg = kilograms; WC = waist circumference; HC = hip circumference; cm = centimeters; BF = body fat; % = percent; BAI = body adiposity index; BAIFELS = body adiposity index FELS longitudinal study; BMI = body mass index; kg/m2 = kilogram per meter squared; BFD = percent body fat calculated from Deurenberg et al.
Protocol
This study used a repeated measures design to assess the difference in %BF using ADP, two prediction equations for BAI, and Deurenberg et al.’s BMI conversion equation (5). All participants underwent body composition analysis using ADP via the Bod Pod. Before entering the Bod Pod, waist circumference (WC) and hip circumference (HC) were measured. Visual inspection of Bland-Altman plots allowed for the determination of agreement between measurements.
Anthropometry
WC and HC were measured to the nearest mm using an anthropometric measuring tape (Creative Health Products, Ann Arbor, MI, USA). WC was measured at the smallest portion of the midsection, between the xiphoid process and iliac crest, while having feet shoulder width apart (6). HC was measured at the maximum circumference of the buttocks while having both feet together (6). BMI (14), BAI (2), BAIFELS (22), and BFD (5) were calculated using the following equations:
Note: For sex, male = 1 and female = 0
Air Displacement Plethysmography
Body composition was determined using the Bod Pod (Life Measurement Inc., Concord, CA, USA). The Bod Pod has demonstrated to be a valid and reliable tool for assessing body composition in overweight and obese individuals (16, 17, 24). For appropriate %BF measurements, prior to entering the chamber, participants were instructed to change into form-fitting clothing including spandex shorts, a sports bra for females, and a swim cap in following the manufacturer’s directions. Height was measured without shoes to the nearest mm using a stadiometer (Novel Products Inc., IL, USA). Weight was measured using an electronic scale which was calibrated according to manufacturer’s directions (Life Measurement Inc., Concord, CA, USA). Body volume was measured a minimum of two times. However, a third measurement was taken if the first two measurements were not within 150 ml or 0.3% as instructed by the Bod Pod. Thoracic gas volume was estimated using the prediction equation provided by the Bod Pod software (26). Body density was converted to %BF using the two-compartment Siri equation (35). All calculations were performed by the Bod Pod’s software (version 1.91).
Statistical Analysis
Data are reported as means ± standard error. All data were screened for outliers, multivariate normality, and sphericity before proceeding with Repeated Measures ANOVA. Differences in %BF between methods were compared using repeated measures ANOVA with Bonferroni post hoc analysis. Pearson correlation coefficients examined relationships between ADP and the BAI, BAIFELS, and BFD. Agreement of estimating %BF was assessed between the BAI equations and the Bod Pod using a Bland-Altman plot with 95% limits of agreement. Constant error (CE) was calculated as CE=gold standard – new measure. Standard error of measure (SEM) was calculated as the standard deviation divided by the square root of N. Data were exported from the Bod Pod software to Excel (Microsoft Office, USA), and analyzed using SPSS version 20 (IBM Corp., Armock, NY, USA) with alpha set a priori at p < 0.05.
RESULTS
A significant value for Mauchly’s Test of Sphericity was found indicating the assumption of sphericity had been violated. Because the assumption of sphericity was violated, a repeated measures ANOVA with a Greenhouse-Geisser correction was utilized and determined the mean %BF were statistically different among the methods used to predict %BF (F(1.884, 849.717) = 107.769, (p < 0.001). Post hoc tests using the Bonferroni correction revealed a statistically significant difference in %BF between ADP and the BAI (p < 0.001) as well as ADP and the BAIFELS (p < 0.001). However, there was no significant difference (p = 1.00) between ADP and BFD. Pearson correlation coefficients were all statistically significant and are listed in Table 2. BFD (r = 0.51) had the strongest correlation with ADP, followed by BMI (r = 0.49) and WC (r = 0.48). Additionally, CE and SEM can be seen in Table 3. Tables 4, 5, and 6 show %BF for each equation (BAI, BAIFELS, and BFD) based on the participants’ BMI.
Table 2.
Pearson’s correlation coefficients between %BF determined by ADP and different variable.
| Measure | r | Level of Significance |
|---|---|---|
| BAI | 0.43 | p < 0.000 |
| BAIFELS | 0.43 | p < 0.000 |
| BFD | 0.52 | p < 0.000 |
| BMI | 0.49 | p < 0.000 |
| HC | 0.33 | p < 0.000 |
| WC | 0.49 | p < 0.000 |
| WHR | 0.21 | p < 0.000 |
BAI = body adiposity index; BAIFELS = body adiposity index FELS longitudinal study; BFD = percent body fat calculated from Deurenberg et al.; BMI = body mass index; HC = hip circumference; WC = waist circumference; WHR = waist to hip ratio.
Table 3.
Constant error and standard error of measure for the different measures of %BF.
| BAI | BAIFELS | BFD | |
|---|---|---|---|
| CE | −3.28 | −4.08 | −0.07 |
| SEM | 0.23 | 0.30 | 0.229 |
BAI = body adiposity index; BAIFELS = body adiposity index FELS longitudinal study; BFD = percent body fat calculated from Deurenberg et al.; CE = constant error; SEM = standard error of measure.
Table 4.
Mean and SD body composition measures according to BMI of 25–29.99.
| BMI 25–29.99 | %BF | BAI | BAIFELS | BFD | |
|---|---|---|---|---|---|
| Average | 27.10 | 24.91 | 23.12 | 22.05 | 24.69 |
| SD | 1.36 | 7.16 | 4.55 | 5.88 | 2.97 |
BMI = body mass index; %BF = percent body fat; BAI = body adiposity index; BAIFELS = body adiposity index FELS longitudinal study; BFD = percent body fat calculated from Deurenberg et al.; SD = standard deviation.
Table 5.
Mean and SD body composition measures according to BMI of 30–39.99.
| BMI 30–39.99 | %BF | BAI | BAIFELS | BFD | |
|---|---|---|---|---|---|
| Average | 32.96 | 32.14 | 25.63 | 25.40 | 32.34 |
| SD | 2.38 | 6.32 | 5.04 | 6.52 | 3.56 |
BMI = body mass index; %BF = percent body fat; BAI = body adiposity index; BAIFELS = body adiposity index FELS longitudinal study; BFD = percent body fat calculated from Deurenberg et al.; SD = standard deviation.
Table 6.
Mean and SD body composition measures according to BMI of 40–50.
| BMI 40–49.99 | %BF | BAI | BAIFELS | BFD | |
|---|---|---|---|---|---|
| Average | 41.48 | 37.17 | 27.96 | 28.73 | 40.63 |
| SD | 0.80 | 4.21 | 3.59 | 4.79 | 1.22 |
BMI = body mass index; %BF = percent body fat; BAI = body adiposity index; BAIFELS = body adiposity index FELS longitudinal study; BFD = percent body fat calculated from Deurenberg et al.; SD = standard deviation.
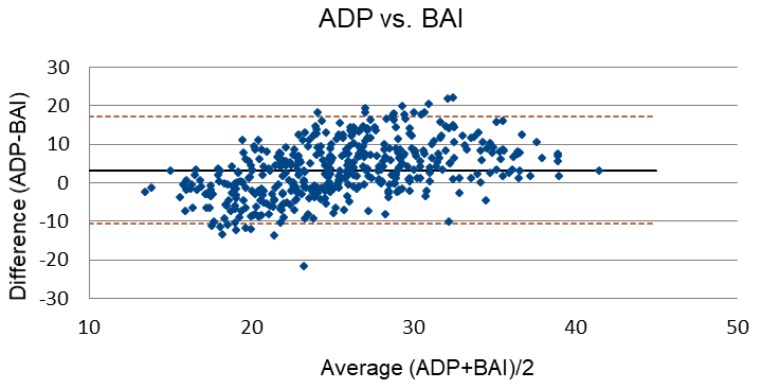
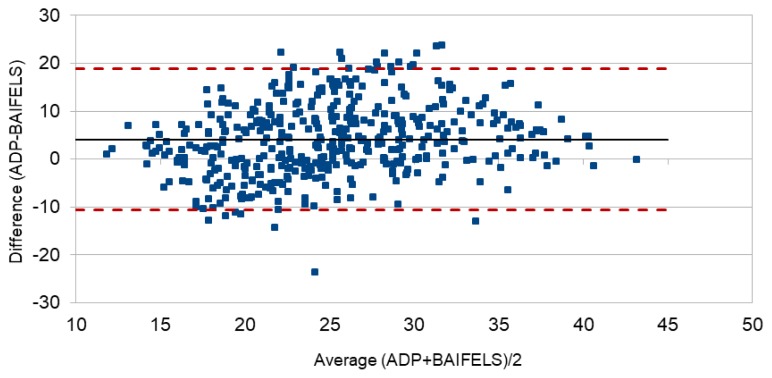
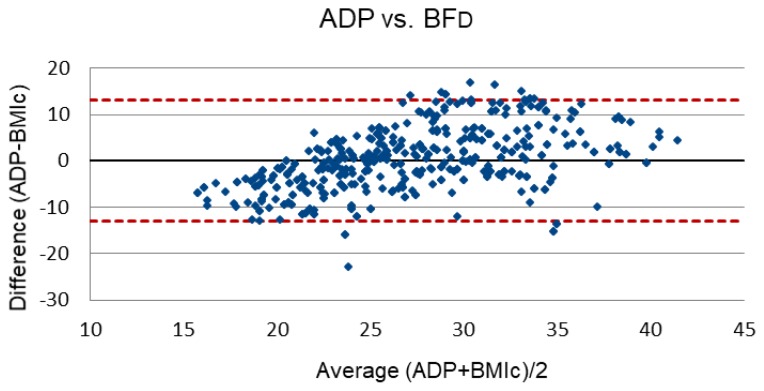
Bland-Altman plots were also created to show the differences between ADP and each of the three equations. ADP versus BAI is depicted in Figure 1, ADP verses BAIFELS is depicted in Figure 2, and ADP verses BFD is depicted in Figure 3.
Figure 1.
Bland-Altman plot depicting the difference and average between air displacement plethysmography (ADP) and the body adiposity index (BAI).
Figure 2.
Bland-Altman plot depicting the difference and average between air displacement plethysmography (ADP) and the body adiposity index FELS longitudinal study (BAIFELS).
Figure 3.
Bland-Altman plot depicting the difference and average between air displacement plethysmography (ADP) and the percent body fat as calculated from Deurenberg et al. (BFD).
DISCUSSION
The purpose of this study was to compare predicted %BF from two different BAI prediction equations and BFD equation to the measured %BF via ADP in a sample of overweight and obese Caucasian men. The results from our study found all measures, except for the BFD equation, to be significantly different from the measured %BF via ADP. This was unexpected as Deurenberg et al. found their equation slightly overestimated %BF in obese participants (5). These findings may be the result of using a population of both overweight and obese participants, with BMIs ranging from 13.9 to 40.9 kg/m2. In addition, Deurenberg et al. used a sample with both sexes while our sample consisted of only male participants (5).
When formulating our prediction in this study, the measurements in each %BF equation were considered. When Bergman et al. originally developed the BAI, they looked at Mexican and African Americans of both genders and found HC to be a better predictor of %BF than WC (2). Therefore, HC was included in the original BAI equation (2). However, this is problematic because men store fat around the trunk whereas women store fat around the hips (23). This means, using HC in the BAI prediction equation may not be suitable for both genders. Therefore, we predicted the original BAI equation would be significantly different than the %BF measured via ADP, which did occur and is supported by one of our previous studies conducted with a mixed sex sample (3).
The inaccuracy in predicting %BF with the BAI can be seen further in other studies. In a study conducted with severely obese adults, the BAI exhibited to be a poor predictor of %BF (1). Likewise, in a sample of overweight and obese postmenopausal Caucasian women the BAI underestimated %BF by 7.56% (23). In a sample of collegiate female athletes, BAI was found to be an inaccurate measurement of %BF when compared to the DEXA, by overestimating %BF levels (7). Additionally, in a group of middle aged and elderly participants from Norway, the BAI underestimated %BF at higher BMI levels (38).
Our next prediction that the BAIFELS equation would also produce significantly different results for %BF than the measure taken by ADP did occur in our Caucasian male participants. This finding was also seen in our previous research with a mixed sex sample (3). The BAIFELS equation was originally created using European-American adults from the FELS longitudinal study (22). In this study, it was determined that both BAI equations, the original BAI and BAIFELS, differed significantly from the DXA; however, they did note the BAIFELS performed better at high levels of adiposity (22). This study along with another that found the BAI to be an inaccurate choice for assessing severely obese Caucasian women (15), helped develop our sample and prediction. We elected to limit our sample to adult Caucasian men with a BMI of 25 to 39.9 kg/m2 to attempt to get the most accurate results. Additionally, we elected to use an equation previously developed by Deurenberg et al. to consider sex and discard HC (5) because the BAI equation has been found to be a less accurate measure of %BF when compared to BMI, HC, and WC (12).
When assessing the Bland Altman plots and CE for this study, the BFD equation is suggested to be the best for predicting %BF when compared with the BAI and BAIFELS equations. The limited agreement on the Bland Altman plots suggest large individual differences from %BF measure by ADP. Based upon our findings, we believe the BFD is the best equation out of the three to predict %BF. We conclude that both the BAI and BAIFELS are not suitable for predicting %BF in overweight and obese Caucasian men. Clinicians should utilize other existing methods to assess body fat in order to avoid large errors associated with either BAI equation.
This study does have limitations. This study had few (n = 29) participants with a BMI above 35.0 kg/m2. Additionally, the results from this study can only be applied to overweight and obese Caucasian men from the United States. However, with the large sample size and use of ADP, we feel that this limitation is acceptable.
In conclusion, the BAI and BAIFELS are not appropriate to predict %BF in a population of overweight and obese Caucasian adults from the United States, while the BFD prediction equation is appropriate. Future studies should evaluate the differences in body fat using the BFD equation in multiple ethnic groups.
ACKNOWLEDGEMENTS
The authors would like to thank all of the volunteers for their time and efforts. No funding or contributions were received for this study.
REFERENCES
- 1.Belarmino G, Torrinhas RS, Sala P, Horie LM, Damiani L, Lopes NC, Heymsfield SB, Waitzberg DL. A new anthropometric index for body fat estimation in patients with severe obesity. BMC Obes. 2018;5:25. doi: 10.1186/s40608-018-0202-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bergman RN. A better index of body adiposity. Obesity (Silver Spring) 2012;20(6):1135. doi: 10.1038/oby.2012.99. [DOI] [PubMed] [Google Scholar]
- 3.Brown JR, Young LM, Ball TJ, Del Pozzi AT. Accuracy of the body adiposity index and body adiposity index fels compared with air displacement plethysmography. J Fit Res. 2016;5(3):28–37. [Google Scholar]
- 4.Cerqueira M, Amorim P, Magalhaes F, Castro E, Franco F, Franceschini S, Cerqueira L, Marins J, Doimo L. Validity of body adiposity index in predicting body fat in a sample of brazilian women. Obesity (Silver Spring) 2013;21(12):E696–699. doi: 10.1002/oby.20543. [DOI] [PubMed] [Google Scholar]
- 5.Deurenberg P, Weststrate JA, Seidell JC. Body mass index as a measure of body fatness: Age- and sex-specific prediction formulas. Br J Nutr. 1991;65(2):105–114. doi: 10.1079/bjn19910073. [DOI] [PubMed] [Google Scholar]
- 6.Dobbelsteyn CJ, Joffres MR, MacLean DR, Flowerdew G. A comparative evaluation of waist circumference, waist-to-hip ratio and body mass index as indicators of cardiovascular risk factors. The canadian heart health surveys. Int J Obes Relat Metab Disord. 2001;25(5):652–661. doi: 10.1038/sj.ijo.0801582. [DOI] [PubMed] [Google Scholar]
- 7.Esco MR. The accuracy of the body adiposity index for predicting body fat percentage in collegiate female athletes. J Strength Cond Res. 2013;27(6):1679–1683. doi: 10.1519/JSC.0b013e3182712714. [DOI] [PubMed] [Google Scholar]
- 8.Esco MR, Nickerson BS, Bicard SC, Russell AR, Bishop PA. Agreement of bmi-based equations and dxa in determining body-fat percentage in adults with down syndrome. Adapt Phys Activ Q. 2016;33(1):89–96. doi: 10.1123/APAQ.2014-0240. [DOI] [PubMed] [Google Scholar]
- 9.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among us adults, 1999–2010. JAMA. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 10.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293(15):1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 11.Frankenfield DC, Rowe WA, Cooney RN, Smith JS, Becker D. Limits of body mass index to detect obesity and predict body composition. Nutrition. 2001;17(1):26–30. doi: 10.1016/s0899-9007(00)00471-8. [DOI] [PubMed] [Google Scholar]
- 12.Freedman DS, Thornton JC, Pi-Sunyer FX, Heymsfield SB, Wang J, Pierson RN, Jr, Blanck HM, Gallagher D. The body adiposity index (hip circumference / height(15)) is not a more accurate measure of adiposity than is bmi, waist circumference, or hip circumference. Obesity (Silver Spring) 2012;20(12):2438–2444. doi: 10.1038/oby.2012.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gallagher D, Visser M, Sepulveda D, Pierson RN, Harris T, Heymsfield SB. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am J Epidemiol. 1996;143(3):228–239. doi: 10.1093/oxfordjournals.aje.a008733. [DOI] [PubMed] [Google Scholar]
- 14.Garn SM, Leonard WR, Hawthorne VM. Three limitations of the body mass index. Am J Clin Nutr. 1986;44(6):996–997. doi: 10.1093/ajcn/44.6.996. [DOI] [PubMed] [Google Scholar]
- 15.Geliebter A, Atalayer D, Flancbaum L, Gibson CD. Comparison of body adiposity index (bai) and bmi with estimations of % body fat in clinically severe obese women. Obesity (Silver Spring) 2013;21(3):493–498. doi: 10.1038/oby.2012.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gibson CD, Atalayer D, Flancbaum L, Geliebter A. Body adiposity index (bai) correlates with bmi and body fat pre- and post-bariatric surgery but is not an adequate substitute for bmi in severely obese women. Int J Body Compos Res. 2012;10(1):9–14. [PMC free article] [PubMed] [Google Scholar]
- 17.Ginde SR, Geliebter A, Rubiano F, Silva AM, Wang J, Heshka S, Heymsfield SB. Air displacement plethysmography: Validation in overweight and obese subjects. Obes Res. 2005;13(7):1232–1237. doi: 10.1038/oby.2005.146. [DOI] [PubMed] [Google Scholar]
- 18.Godoy-Matos AF, Moreira RO, Valerio CM, Mory PB, Moises RS. A new method for body fat evaluation, body adiposity index, is useful in women with familial partial lipodystrophy. Obesity (Silver Spring) 2012;20(2):440–443. doi: 10.1038/oby.2011.343. [DOI] [PubMed] [Google Scholar]
- 19.Gregg EW, Cheng YJ, Cadwell BL, Imperatore G, Williams DE, Flegal KM, Narayan KM, Williamson DF. Secular trends in cardiovascular disease risk factors according to body mass index in us adults. JAMA. 2005;293(15):1868–1874. doi: 10.1001/jama.293.15.1868. [DOI] [PubMed] [Google Scholar]
- 20.Gupta S, Kapoor S. Body adiposity index: Its relevance and validity in assessing body fatness of adults. ISRN Obes. 2014;2014:243294. doi: 10.1155/2014/243294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jackson AS, Stanforth PR, Gagnon J, Rankinen T, Leon AS, Rao DC, Skinner JS, Bouchard C, Wilmore JH. The effect of sex, age and race on estimating percentage body fat from body mass index: The heritage family study. Int J Obes Relat Metab Disord. 2002;26(6):789–796. doi: 10.1038/sj.ijo.0802006. [DOI] [PubMed] [Google Scholar]
- 22.Johnson W, Chumlea WC, Czerwinski SA, Demerath EW. Concordance of the recently published body adiposity index with measured body fat percent in european-american adults. Obesity (Silver Spring) 2012;20(4):900–903. doi: 10.1038/oby.2011.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krotkiewski M, Bjorntorp P, Sjostrom L, Smith U. Impact of obesity on metabolism in men and women. Importance of regional adipose tissue distribution. J Clin Invest. 1983;72(3):1150–1162. doi: 10.1172/JCI111040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Le Carvennec M, Fagour C, Adenis-Lamarre E, Perlemoine C, Gin H, Rigalleau V. Body composition of obese subjects by air displacement plethysmography: The influence of hydration. Obesity (Silver Spring) 2007;15(1):78–84. doi: 10.1038/oby.2007.533. [DOI] [PubMed] [Google Scholar]
- 25.Lemacks JL, Liu PY, Shin H, Ralston PA, Ilich JZ. Validation of body adiposity index as a measure of obesity in overweight and obese postmenopausal white women and its comparison with body mass index. Menopause. 2012;19(11):1277–1279. doi: 10.1097/gme.0b013e31825408e5. [DOI] [PubMed] [Google Scholar]
- 26.McCrory MA, Mole PA, Gomez TD, Dewey KG, Bernauer EM. Body composition by air-displacement plethysmography by using predicted and measured thoracic gas volumes. J Appl Physiol (1985) 1998;84(4):1475–1479. doi: 10.1152/jappl.1998.84.4.1475. [DOI] [PubMed] [Google Scholar]
- 27.Middleton K, Hing E. National hospital ambulatory medical care survey: 2003 outpatient department summary. Adv Data. 2005;366:1–36. [PubMed] [Google Scholar]
- 28.Mooney SJ, Baecker A, Rundle AG. Comparison of anthropometric and body composition measures as predictors of components of the metabolic syndrome in a clinical setting. Obes Res Clin Pract. 2013;7(1):e55–66. doi: 10.1016/j.orcp.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 29.Nickerson BS, Esco MR, Bicard SC, Russell AR, Williford HN, Schaefer G. Validity of the body adiposity index in adults with down syndrome. Res Dev Disabil. 2015;38:92–96. doi: 10.1016/j.ridd.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 30.Nickerson BS, Esco MR, Bishop PA, Fedewa MV, Snarr RL, Kliszczewicz BM, Park KS. Validity of bmi-based body fat equations in men and women: A 4-compartment model comparison. J Strength Cond Res. 2018;32(1):121–129. doi: 10.1519/JSC.0000000000001774. [DOI] [PubMed] [Google Scholar]
- 31.Ode JJ, Pivarnik JM, Reeves MJ, Knous JL. Body mass index as a predictor of percent fat in college athletes and nonathletes. Med Sci Sports Exerc. 2007;39(3):403–409. doi: 10.1249/01.mss.0000247008.19127.3e. [DOI] [PubMed] [Google Scholar]
- 32.Piers LS, Soares MJ, Frandsen SL, O’Dea K. Indirect estimates of body composition are useful for groups but unreliable in individuals. Int J Obes Relat Metab Disord. 2000;24(9):1145–1152. doi: 10.1038/sj.ijo.0801387. [DOI] [PubMed] [Google Scholar]
- 33.Ramirez-Velez R, Correa-Bautista JE, Gonzalez-Ruiz K, Vivas A, Garcia-Hermoso A, Triana-Reina HR. Predictive validity of the body adiposity index in overweight and obese adults using dual-energy x-ray absorptiometry. Nutrients. 2016;8(12) doi: 10.3390/nu8120737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, Allison TG, Batsis JA, Sert-Kuniyoshi FH, Lopez-Jimenez F. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond) 2008;32(6):959–966. doi: 10.1038/ijo.2008.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Siri WE. Body composition from fluid spaces and density: Analysis of methods. 1961. Nutrition. 1993;9(5):480–491. discussion 480, 492. [PubMed] [Google Scholar]
- 36.Sjostrom L, Smith U, Krotkiewski M, Bjorntorp P. Cellularity in different regions of adipose tissue in young men and women. Metabolism. 1972;21(12):1143–1153. doi: 10.1016/0026-0495(72)90109-6. [DOI] [PubMed] [Google Scholar]
- 37.Sun G, Cahill F, Gulliver W, Yi Y, Xie Y, Bridger T, Pace D, Zhang H. Concordance of bai and bmi with dxa in the newfoundland population. Obesity (Silver Spring) 2013;21(3):499–503. doi: 10.1002/oby.20009. [DOI] [PubMed] [Google Scholar]
- 38.Vinknes KJ, Elshorbagy AK, Drevon CA, Gjesdal CG, Tell GS, Nygard O, Vollset SE, Refsum H. Evaluation of the body adiposity index in a caucasian population: The hordaland health study. Am J Epidemiol. 2013;177(6):586–592. doi: 10.1093/aje/kws271. [DOI] [PubMed] [Google Scholar]
- 39.Wellens RI, Roche AF, Khamis HJ, Jackson AS, Pollock ML, Siervogel RM. Relationships between the body mass index and body composition. Obes Res. 1996;4(1):35–44. doi: 10.1002/j.1550-8528.1996.tb00510.x. [DOI] [PubMed] [Google Scholar]