SUMMARY
Zaire ebolavirus (EBOV) VP35 protein is a suppressor of type I interferon (IFN) production, an inhibitor of dendritic cell maturation, and a putative virulence determinant. Here, a recombinant EBOV encoding a mutant VP35 virus (VP35m) is demonstrated to activate RIG-I-like receptor signaling and innate antiviral pathways. When inoculated into cynomolgus macaques, VP35m exhibits dramatic attenuation as compared to wild-type EBOV (wtEBOV), with 20 or 300 times the standard 100% lethal challenge dose not causing EBOV disease (EVD). Further, VP35m infection, despite limited replication in vivo, activates antigen presentation and innate immunity pathways and elicits increased frequencies of proliferating memory T cells and B cells and production of anti-EBOV antibodies. Upon wtEBOV challenge, VP35m-immunized animals survive, exhibiting host responses consistent with an orderly immune response and the absence of excessive inflammation. These data demonstrate that VP35 is a critical EBOV immune evasion factor and provide insights into immune mechanisms of EBOV control.
Graphical Abstract

In Brief
Woolsey et al. demonstrate that immune evasion functions of the Ebola virus VP35 protein are critical for virulence in non-human primates. A VP35 mutant Ebola virus does not cause lethal disease and instead elicits adaptive immune responses that can protect animals from wild-type Ebola virus challenge.
INTRODUCTION
Zaire ebolavirus (EBOV), a member of the filovirus family of enveloped, non-segmented, negative-sense RNA viruses, is a zoonotic pathogen that causes outbreaks of severe, often lethal disease in humans (Feldmann et al., 2013). Fatal human cases of EBOV disease (EVD) are exemplified by high viral titers in blood, excessive inflammation, impaired adaptive immunity, severe coagulopathies, and shock (Cross et al., 2018; Feldmann et al., 2013). Until late 2013, EBOV caused sporadic and isolated outbreaks mostly in Central Africa. However, the 2013–2016 EBOV epidemic that affected over 28,000 individuals resulted in more than 11,000 deaths and export of cases from West Africa to Europe and the United States (Bausch, 2017). Subsequent outbreaks in 2017 and 2018 in the Democratic Republic of Congo further highlight the importance of understanding factors that contribute to EBOV virulence (WHO, 2019).
EBOV virulence is partially attributed to the ability of the virus to circumvent innate antiviral responses and suppress dendritic cell maturation, which may blunt development of effective adaptive immune responses (Messaoudi et al., 2015; Olejnik et al., 2017). Several in vitro studies demonstrate that the EBOV VP35 protein, a structural component of the nucleocapsid and essential cofactor for the viral RNA polymerase complex, inhibits both the production of type I interferon (IFN) and dendritic cell maturation by interfering with host retinoic-acid-inducible gene I-like receptor (RLR) signaling (Cárdenas et al., 2006; Hartman et al., 2006; Leung et al., 2010a; Lubaki et al., 2013; Prins et al., 2009, 2010; Yen et al., 2014). The RLRs are pattern recognition receptors that detect RNAs produced during virus infection and include retinoic-acid-inducible gene I (RIG-I), melanoma differentiation-associated protein 5 (MDA5), and laboratory of genetics and physiology protein 2 (LGP2) (Chow et al., 2018; Yoneyama et al., 2015). Activation of RIG-I and MDA5 leads to signaling that induces IFN production, and LGP2 regulates RLR signaling (Chow et al., 2018). Activating RLRs also promotes dendritic cell maturation (Kato et al., 2005; Reikine et al., 2014; Satoh et al., 2010). The VP35-mediated inhibition of RLR signaling correlates with its capacity to bind double-stranded RNA (dsRNA) and its interaction with the host protein PACT (Bale et al., 2013; Cárdenas et al., 2006; Edwards et al., 2016; Harcourt et al., 1998; Kimberlin et al., 2010; Leung et al., 2009; Leung et al., 2010a; Prins et al., 2010). Mutation of residues in a central basic patch located in the C-terminal IFN inhibitory domain (IID) of VP35, as well as residue F239, which facilitates positioning of VP35 over the blunt ends of dsRNA, largely abrogates RLR inhibitory activities. The same individual mutations have little impact on the function of VP35 in a minigenome system, which measures the function of the viral RNA polymerase complex (Leung et al., 2010a). Therefore, these residues are attractive targets for defining the direct contribution of VP35 to RLR-associated host immunosuppression, as any introduced mutations that result in virulence attenuation are not inextricably linked with defects in virus growth.
In this study, we investigated the importance of VP35-mediated immune evasion in EVD by performing in vitro and in vivo experiments with a recombinant EBOV bearing VP35 F239A, K319A, and R322A mutations (VP35m). The data demonstrate that the absence of VP35 leads to robust IFN responses in a MAVS-dependent manner. Despite this, attenuation in cell culture of VP35m relative to wild-type EBOV (wtEBOV) is modest. In contrast, VP35m in non-human primates (NHPs) replicates to low levels and is highly attenuated, triggering innate and adaptive immunity. The immune responses triggered are sufficiently robust that VP35m can immunize NHPs against wtEBOV challenge.
RESULTS
VP35 Regulates MAVS-Dependent Host Responses to EBOV Infection
Introduction of individual point mutations F239A, K319A, and R322A into VP35 impaired its capacity to suppress activation of the IFN-β promoter in response to Sendai virus (SeV) infection, consistent with prior reports (Cárdenas et al., 2006; Hartman et al., 2004; Leung et al., 2010a; Prins et al., 2010; Yen et al., 2014). Combinations of two or all three mutations resulted in a similar phenotype compared to each single point mutation (Figure 1A). When the same mutations were tested in a minigenome assay, which measures the function of the EBOV RNA synthesis complex, the individual VP35 point mutations led to a modest decrease in activity, but a double or triple mutant exhibited the same activity as the single point mutations, indicating there is not a cumulative impact of these mutations (Figure S1A). A recombinant EBOV was generated with all three mutations in VP35 (Luthra et al., 2013). wtEBOV and the VP35 mutant virus (VP35m) were then used to infect A549 cells or A549 cells in which the mitochondrial antiviral signaling protein (MAVS), critical for RLR signaling, was disrupted (MAVS knockout [KO]) (Li et al., 2016). Cells were infected at an MOI of 1. Although viral replication was delayed in MAVS KO cells, infectious titers of either VP35m or wtEBOV in either cell type were similar by 72 h (Figure 1B). Because macrophages are major targets of EBOV infection in vivo (Geisbert et al., 2003a, 2003b; Menicucci et al., 2017), we also examined virus growth and the host response in a THP-1 macrophage-like cell line. In THP-1 cells, the mutations did impair VP35m replication, as compared to wtEBOV (Figure S1B). These data are consistent with a model where the mutations do not substantially alter viral RNA synthesis in A549 cells. The attenuation of growth in THP-1 cells may reflect a more robust IFN response in these cells as compared to A549 cells.
Figure 1. VP35 Regulates MAVS-Dependent Host Responses to wtEBOV Infection.
(A) IFN-β promoter reporter assay to assess VP35 mutant IFN-inhibitory function. HEK293T cells were transfected with plasmids expressing wt VP35 or VP35 mutants (F239A, K319A, R322A, KRA-K319A/R322A, FKRA, and F239A/K319A/R322A at 10 or 100 ng) along with an IFN-β promoter-firefly reporter plasmid and Renilla reporter as a transfection control. SeV infection was used as an inducer of RIG-I activation and 20 h later luciferase activities were determined. Fold increase indicates Firefly luciferase normalized to Renilla luciferase values, with the empty vector (E) value set to 1. The error bars represent SD of three independent replicates. The p value was determined by a one-way ANOVA test followed by multiple comparisons using Tukey’s test. *p < 0.05, **p < 0.001, ***p <0.0005, ****p < 0.0001.
(B) Average viral titers of wtEBOV or VP35m in A549 wt or MAVS KO cells. Supernatants from infected cells were plated in duplicate and viral titers were determined at the indicated hours post-infection by plaque assay. PFU, plaque-forming units. The error bars represent SD of two independent replicates.
(C) Venn diagram comparing DEGs between VP35m- (n = 2) and wtEBOV-infected (n = 2) A549 cells at 72 h post-infection. Heatmap representing functional enrichment of DEGs common to either infection or exclusively only following VP35m or wtEBOV infection; color intensity represents the statistical significance (shown as −log10 of the q-value); range of colors is based on the lowest and highest −log10(q-value) for the entire set of GO processes. The number of DEGs enriching to each GO term is listed within each box; blank boxes represent lack of significant enrichment to a given GO term.
(D and E) Heatmap representing gene expression (shown as absolute normalized reads per kilobase per million mapped reads [RPKM] values) of DEGs that enriched to “defense response to virus” in A549 cells (D) or A549 MAVS KO cells (E) infected with wtEBOV or VP35m at 1 and 72 h. The range of colors is based on scaled and centered RPKM values of the entire set of genes (red represents increased expression, while blue represents decreased expression); each column represents one biological replicate.
(F) Venn diagram comparing DEGs between VP35m- (n = 2) and wtEBOV-infected (n = 2) A549 MAVS KO cells at 72 h post-infection. Heatmap representing functional enrichment of DEGs common to either infection or exclusively only following VP35m or wtEBOV infection.
(G) Heatmap representing gene expression of DEGs common to either infection that enriched to “cell division”; each column represents one biological replicate.
Disruption of VP35 IID activity upregulated expression of IFN-b and IFN-inducible genes RIG-I and IFIT1 in wild-type (wt) A549 cells. However, this response was absent in VP35m-infected MAVS KO cells, similar to what was found in wtEBOV-infected cells (Figure S1C). To fully assess differences in these cellular responses, we performed RNA sequencing (RNA-seq) analysis of A549 and A549 MAVS KO cells at 1 and 72 h post-infection (HPI) with wtEBOV or VP35m. Principal-component analysis (PCA) revealed distinct transcriptional profiles driven by disrupted MAVS (principal component 1 [PC1]) and/or viral infection (PC2) (Figure S1D). Overall, more substantial gene expression changes were detected in MAVS KO compared to wt cells (Figure S1E). Approximately 30% of the differentially expressed genes (DEGs) detected in A549 cells following infection with wtEBOV or VP35m were shared. Therefore, the majority of induced transcriptional changes were unique to each virus (Figure 1C). Common DEGs enriched to the Gene Ontology (GO) terms “regulation of defense response” and “response to wounding,” whereas DEGs detected exclusively during VP35m infection were involved in antiviral and cytokine signaling, as well as protein ubiquitination (Figure 1C). As expected, VP35m in wt A549 cells, but not A549 MAVS KO cells, stimulated increased expression of IFN-stimulated genes (ISGs) including IFIT1, IFITM1, OAS2, and the viral sensor DDX58 (Figures 1D and 1E). Additional genes important for innate immune signaling (e.g., IRAK2 and MYD88) and genes that play a role in antigen presentation (i.e., B2M and HLA-A) were also upregulated (Figure S1F). Interestingly, VP35m also induced HERC5 and TRIM56, E3 ubiquitin ligases that exhibit antiviral activity, and other transcripts important for degrading misfolded proteins like UBE2H and FBX06 (Figure S1G).
In congruence with the PCA, most transcriptional changes following infection with either EBOV or VP35m in A549 MAVS KO cells were shared and enriched to GO terms associated with cell-cycle progression, apoptosis, and metabolism, but not host defense (Figure 1F). Curiously, most of these DEGs were downregulated 72 HPI in both EBOV- and VP35m-infected MAVS KO cells (Figure 1G). Gene expression analyses in THP-1 cells revealed a suppression of innate immune genes in wtEBOV-infected cells and upregulation of innate immune genes in VP35m-infected cells (Figure S1H). Cumulatively, these findings indicate that VP35 blocks RLR signaling to suppress innate immune signaling and functions that stimulate adaptive immunity.
VP35m Substantially Curtails EVD and Induces Robust Gene Expression Changes
In the interest of establishing whether RLR-associated mutations in the VP35 protein alter EBOV pathogenesis in NHPs, we initially performed a small pilot study involving two cynomolgus macaques subjected to a 20,000 plaque-forming unit (PFU) target dose of the mutant virus. All subjects survived, and no viremia or signs of illness were detected in these animals (Table 1). Next, we speculated whether VP35m primed a memory response to protect NHPs from wtEBOV infection. To test this hypothesis, three macaques were infected at a target dose of VP35m (20,000 PFU) and back-challenged at 28 days post-infection (DPI) with a 1,000 PFU dose of the Kikwit variant of wtEBOV (Zaire ebolavirus; isolate 199510621). According to historical data, this virus stock was uniformly lethal in 34 of 34 cynomolgus macaques, with an average time to death of 6.4 days (Callendret et al., 2018; Matassov et al., 2018) (T.W.G., unpublished data). Blood samples following VP35m and wtEBOV infection were collected at 0, 3, 6, 10, 14, and 28 days (Figure 2A). Similar to the pilot study, all three macaques survived the initial VP35m challenge, with no evidence of viremia or disease (Figures S2A–S2C; Table 1). Following wtEBOV back-challenge, two of the three VP35m-vaccinated animals survived, with no indications of illness in the survivors. The fatal subject developed signs consistent with EVD, including fever, depression, anorexia, a petechial rash, and elevated serum levels of liver-associated enzymes (alanine aminotransferase [ALT], aspartate transaminase [AST], alkaline phosphatase [ALP], and gamma-glutamyltransferase [GGT]) and kidney-associated products (blood urea nitrogen [BUN] and creatinine [CRE]). This animal succumbed on day 9 after back-challenge, ~3 days later than the median time to death for control animals (Table 1).
Table 1.
Clinical Findings in VP35m-Challenged Cynomolgus Macaques
| VP35m Challenge | wtEBOV Back-Challenge | |||||||
|---|---|---|---|---|---|---|---|---|
| Animal ID | Study | Target Dose (PFU) | Viremia (log10 PFU/mL) | Clinical Signsa | Outcome | Viremia (log10 PFU/mL) | Clinical Signsa | Outcome |
| C07466b | pilot | 20,000 VP35m | none | none | survived | NA | NA | NA |
| C07492b | pilot | 20,000 VP35m | none | none | survived | NA | NA | NA |
| 141409 | lower dose | 20,000 VP35m 1,000 wtEBOV |
none | none | survived | none | none | survived |
| 141132 | lower dose | 20,000 VP35m 1,000 wtEBOV |
none | none | survived | 4.12 (6), 7.18(9) | fever (6), anorexia (8, 9), mild petechial rash (7), moderate petechial rash (8, 9), depression (7–9), leukopenia (6), thrombocytopenia (6), lymphopenia (6), BUN +++ (9), CRE +++ (9), ALT ++ (6) +++ (9), AST ++ (6) > (9), ALP +++ (9), GGT +++ (9), CRP increase (6, 9) | succumbed on day 9 |
| 141389 | lower dose | 20,000 VP35m 1,000 wtEBOV |
none | none | survived | none | none | survived |
| 12–1429C control | higher dose | 1,000 wtEBOV | NA | NA | NA | 6.89 (6) | diarrhea (0–6), anorexia (6), mild petechial rash (6), depression (6), dyspnea (6), leukopenia (6), thrombocytopenia (6), lymphopenia (3), BUN + (6), CRE ++ (6), ALT +++ (6), AST +++ (6), ALP +++ (6), GGT +++ (6), CRP increase (6) | succumbed on day 6 |
| 12–1609C | higher dose | 500,000 VP35m 1,000 wtEBOV |
none | none | survived | none | none | survived |
| 13–0478C | higher dose | 500,000 VP35m 1,000 wtEBOV |
2.44 (3), 2.54 (6) | fever (3, 6), leukopenia (28), thrombocytopenia (6), AST + (6)++(10), ALP + (10)++(6), GGT + (6), CRP increase (3, 6, 10) | survived | none | leukopenia (3, 6, 10, 14, 21, 28), thrombocytopenia (3), lymphopenia (14, 28) | survived |
| 12–0413C | higher dose | 500,000 VP35m 1,000 wtEBOV |
none | fever (6), lymphopenia (6), AST + (6), CRP increase (6, 10) | survived | none | leukopenia (14, 21) | survived |
| 13–0726C | higher dose | 500,000 VP35m 1,000 wtEBOV |
none | tremors (22), BUN + (22), ALT + (22), AST +++ (22) | euthanized on day 22 due to unrelated neurological issues | NA | NA | NA |
| 13–0676C | higher dose | 500,000 VP35m 1,000 wtEBOV |
none | diarrhea (13, 14, 16, 17, 20–26), weakness (20, 21) | survived | none | lymphopenia (3, 14, 21, 28) | survived |
Fever is defined as a temperature >2.5°F above baseline, ≥1.5°F above baseline, and R103.5°F, or 1.1 F above baseline and ≥104°F. Lymphopenia and thrombocytopenia are defined by a >40% drop in the number of lymphocytes and platelets, respectively. Leukocytosis and granulocytosis are defined as a R2-fold increase in leukocytes and granulocytes, respectively. Plus signs indicate increases in liver enzymes (ALT, AST, ALP, and GGT) or renal function test values (BUN and CRE): +, 2- to 3-fold increase; ++, >3- up to 5-fold increase; +++, >5-fold increase. BUN, blood urea nitrogen; CRE, creatinine; ALT, alanine aminotransferase; AST, aspartate aminotransferase; ALP, alkaline phosphatase; GGT, gamma-glutamyltransferase; CRP, c-reactive protein.
The day after challenge is in parentheses.
Note the pilot study animals were not back-challenged with wtEBOV. The study endpoint was day 21.
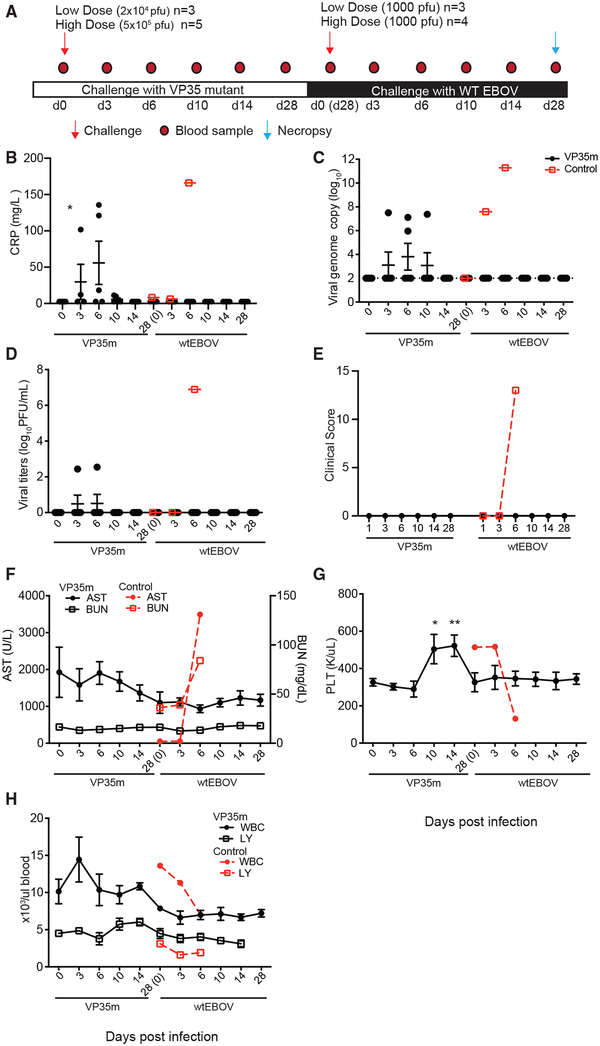
Figure 2. VP35m Infection Results in Mild Clinical Signs and Protects Animals against Subsequent wtEBOV Challenge.
(A) Study timeline.
(B) Plasma levels of C-reactive protein (CRP).
(C) Viral loads determined by qRT-PCR using probe targeting VP30.
(D) Infectious virus was quantified by plaque assay on Vero cells.
(E) Clinical score.
(F) Aspartate transaminase (AST) and blood urea nitrogen (BUN) levels.
(G) Platelet counts.
(H) White blood cells (WBCs) and lymphocyte (LY) counts.
Data in (B)–(H) are presented as mean ± SEM. *p % 0.05 and **p % 0.01 at the indicated time point compared to 0 DPI. The VP35m underlined time points correspond to the challenge with the VP35m portion of the study. The wtEBOV underlined time points correspond to the challenge with wtEBOV of animals previously infected with VP35m.
To further substantiate that VP35m is avirulent in NHPs and to evaluate whether a higher dose induces a more protective response against wtEBOV back-challenge, we inoculated five cynomolgus macaques with a 5 × 105 PFU VP35m dose and back-challenged these animals with 1,000 PFU of wtEBOV-Kikwit (Figure 2A). In addition, we included a single macaque (12–1429C) that was not vaccinated with VP35m to serve as a control for wtEBOV infection. Transient fever and raised levels of circulating C-reactive protein (CRP), a general inflammation marker, were evident in two of five animals following VP35m challenge (Figure 2B; Table 1). One of these animals at 6 DPI exhibited low-level viremia (102 PFU/mL), leukopenia, thrombocytopenia, and increased liver enzymes (Figures 2C and 2D; Table 1). Mild weakness and diarrhea were observed in a third animal, which exhibited low viral RNA titers but no detectable infectious titers (Figure 2C; Table 1). Overall, AST, BUN, platelet, total white blood cell, and lymphocyte concentrations remained relatively stable, and no viremia was detected in the other animals (Figures 2E–2H; Table 1). No subjects reached scorable criteria, and no animals succumbed to VP35m challenge. However, one animal (13–0726C) was euthanized at 22 DPI due to neurological issues that appeared to be unrelated to VP35m infection. This macaque did not display symptoms of EVD or exhibit notable hematological changes, and no infectious virus was observed in the blood or brain of this animal. No overt underlying disease process was found at gross examination or from the extensive histopathology examination.
Following wtEBOV back-challenge, all higher dose VP35m-challenged animals survived, with no detectable viremia or clinical signs (Figures 2B–2H), although some temporal hematological changes (i.e., leukopenia, thrombocytopenia, and lymphopenia) were noted in most of the monkeys (Table 1). In contrast, the control animal that did not receive VP35m showed distinct signs of EVD, including anorexia, petechial rash, increased CRP, high levels of viremia, decreased platelet and white blood cell levels, and evidence of liver and kidney damage as highlighted by elevated ALT, AST, ALP, GGT, and BUN levels (Figures 2B–2H; Table 1). By 6 DPI, this animal reached a clinical score that required euthanasia. The course of disease and time to death was consistent with previous historical macaque controls that received a similar preparation and dose of wtEBOV-Kikwit.
We next determined longitudinal gene expression changes in peripheral blood mononuclear cells (PBMCs) following VP35m infection using RNA-seq. In the lower dose group, more abundant transcriptional changes were detected after VP35m infection in the animals that survived back-challenge at 6 and 10 DPI compared to the animal that succumbed (Figure S2D). For the higher dose group, PCA of normalized reads showed that transcriptional profiles clustered by time point with the most variability observed at 3 DPI and the largest gene expression differences detected between 0 and 10 DPI (Figure S3A). Animals that exhibited fever (12–0413C and 13–0478C) or viremia (13–0478C) did not cluster together or away from the other non-viremic animals. Moreover, viremic and non-viremic animals had similar transcriptional profiles at 6 and 10 DPI.
We used short-time-series expression mining (STEM) to delineate distinct temporal expression profiles throughout infection in the higher dose group (Figures S3B–S3F). We identified five statistically significant gene clusters: cluster 1 contained 177 DEGs, the expression of which increased throughout infection (Figure S3B); cluster 2 is composed of 990 DEGs, which decreased in expression throughout infection (Figure S3C); cluster 3 contained 1,057 DEGs, the expression of which increased at 3 DPI, peaked at 6 DPI, and decreased at 10 DPI but remained higher than baseline (Figure S3D); cluster 4 contained 487 DEGs, the expression of which peaked at 6 DPI, and although it declined at 10 DPI, it remained higher than baseline (Figure S3E); and cluster 5 contained 643 DEGs, which increased in expression slightly at 3 and 6 DPI before increasing dramatically at 10 DPI (Figure S3F).
VP35m Activates Antigen Presentation and Innate Immune Responses
Genes in cluster 3 enriched to GO terms related to metabolism, gene expression, apoptosis, cell motility, and immunity (Figure 3A). Genes in this cluster included those associated with type I IFN response, such as IRF3 and ISGs (e.g., IFIH1, IFIT2, MX2, and RSAD2), immune signaling (e.g., RELA, TIRAP, and IFNGR1), and inflammation (e.g., IL17C, IL23A, CCL3L1m and TNF) (Figure 3B). Additional genes in this cluster play a role in natural killer (NK) cell cytotoxicity (e.g., NCR3), lymphocyte development (IL7), T cell differentiation (e.g., TCF7), and the differentiation of follicular B helper T cells (i.e., CXCR5 and CD40LG) (Figure 3B). Lastly, the most highly expressed DEGs that mapped to “cellular metabolic process” are involved in glucose metabolism (ISYNA1, PHKG2, GYS1, and GBA2), fatty acid metabolism (PPT2 and ACADVL), cell cycle (REC8 and AKAP8), mitogen-activated protein kinase (MAPK) signaling (MAP3K3 and MAPK81P1), and transcriptional regulation (MXD3, HMGXB3, and SMARCD3).
Figure 3. VP35m Induced Antigen Presentation and Regulated Innate Immunity.
(A and C) Bar graph depicting statistically significant GO processes to which cluster 3 (A) or cluster 4 (C) genes enriched; the line graph represents −log10(false discovery rate [FDR]) of the enriched term.
(B and D) Heatmaps representing gene expression (shown as absolute normalized RPKM values) of the DEGs in cluster 3 that enriched to “inflammatory response” and “response to cytokine” (B) and DEGs in cluster 4 that enriched to response to cytokine (D). The range of colors is based on scaled and centered RPKM values of the entire set of genes (red represents increased expression, while blue represents decreased expression); each column represents the median RPKM values for each DPI.
For gene expression data shown in (A)–(D), the number of biological replicates at each time point are as follows: day 0 (n = 5), day 3 (n = 5), day 6 (n = 4), day 10 (n = 5).
(E) Monocyte (CD14+HLA-DR+/−) and dendritic cell (DC; CD14−HLA-DR+) levels measured by flow cytometry (n = 4).
(F) Frequency of classical (CD16−) and CD16+ intermediate or nonclassical monocyte subsets (n = 4).
(G) Frequency of classical and CD16+ intermediate or nonclassical monocyte subsets expressing CD86 (n = 4).
(H) Frequencies of myeloid DCs (mDCs; CD123−CD11c+), plasmacytoid DCs (pDCs; CD123+CD11c−), and other DCs (CD123−CD11c+) (n = 4).
(I) Frequency of DC subsets expressing CD86 (n = 4).
Data are presented as mean ± SEM in (C)–(F). For changes in the frequencies within innate immune subsets, a nonparametric trend where each time point is modeled by its own mean was assumed for statistical analysis; *p % 0.05 compared to 0 DPI; *p % 0.05 for CD16−monocytes and mDCs and #p ≤ 0.05 for other DCs.
The 487 DEGs in cluster 4 enriched to GO terms cellular metabolic process, “regulation of cell proliferation,” “homeostatic process,” and “response to cytokine” (Figure 3C). DEGs mapping to response to cytokine play a role in apoptosis, including BAD, BCL2L1, and TNFRSF6B; chemotaxis, such as CCL11 and CCL14; antiviral defense (e.g., IRF7 and ISG20); antigen presentation, such as CCR7 and HLA-DQA1; and humoral immunity, including CD38 and TNRSF13B (Figure 3D). Similarly, animals in the lower dose group exhibited transcriptional changes associated with type I IFN signaling and antiviral defense at 3 DPI (Figures S2E and S2F). Notable DEGs that mapped to cellular metabolic process play a role in oxidative phosphorylation and cellular respiration (ATP5PF, COX6A1, NDUFA1, UQCRQ, and NDUFA13), mitochondrial translation (MRPL40, MRPS34, and MRRF), and response to oxidative stress (CYBA, NOS3, and NUDT1).
Flow cytometry analysis of PBMCs from the VP35m-infected animals correlated with innate immune gene expression signatures. In the higher dose group, although no changes in the frequency of monocytes (CD3−CD20−CD14+) (Figure 3E) or classical (CD16−) and CD16+ intermediate or nonclassical monocyte subsets (Figure 3F) were detected, we documented a significant increase in the frequency of monocytes expressing activation marker CD86 at 3–14 DPI (Figure 3G). For the lower dose group, sustained monocyte activation was also observed in the animals that went on to survive challenge, while the animal that succumbed to challenge exhibited sporadic and transient increases in CD86 expression (Figure S2G). Similarly, we observed no significant changes in the frequency of total dendritic cells (DCs) (Figure 3E) or their subsets (Figure 3H), but a significant increase in the expression of activation marker CD86 was detected at 3 and 6 DPI (Figure 3I). These results suggest that despite limited replication, VP35m activated innate immune responses.
Disruption of VP35 Function Triggers Adaptive Immunity
The 643 DEGs in cluster 5 mapped primarily to GO terms associated with host defense such as “immune effector process,” “antigen processing and presentation,” and “humoral immune response” (Figure 4A). Although some of the DEGs mapping to immune effector process play a role in innate antiviral immunity (e.g., IRF1, IFITM1, TRIM56, and MIF), the majority of the DEGs are important for adaptive immunity (Figure 4B). Several of these DEGs are critical for antigen presentation and/or recognition (B2M, CD74, HLA-B, and HLA-DMB), lymphocyte signaling (SYK, CD3E, and TRBC1), T cell activation (CD44 and LCP1), and effector responses (GZMB) (Figure 4B). Additionally, this cluster included genes that play a role in B cell responses such as LYN, PRKCB, IGHG2, IGLC1, and IGKC (Figure 4B). Similarly, animals in the lower dose group that survived back-challenge exhibited earlier and larger gene expression changes associated with host defense and adaptive immunity compared to the animal that succumbed where these changes were not evident until 14 DPI (Figures S2E and S2F).
Figure 4. Disruption of VP35 Function Resulted in Development of Adaptive Immunity.
(A) Bar graph depicting statistically significant GO processes to which cluster 5 genes enriched; the line graph represents −log10(FDR) of the enriched term.
(B) Heatmap representing gene expression (shown as absolute normalized RPKM values) of the DEGs in cluster 5 that enriched to “immune effector process”; range of colors is based on scaled and centered RPKM values of the entire set of genes (red represents increased expression while blue represents decreased expression); each column represents the median RPKM values for each DPI.
For gene expression data in (A) and (B), the number of biological replicates at each time point are as follows: day 0 (n = 5), day 3 (n = 5), day 6 (n = 4), and day 10 (n = 5).
(C) Frequency of CD4+ and CD8+ T cells and CD20+ B cells (n = 4).
(D and E) The magnitude of CD4 T cell (n = 4) (D) and CD8 T cell (n = 4) (E) proliferation was determined by measuring changes in the frequency of Ki67+ cells within naive, central (CM), and effector (EM) memory subsets.
(F) B cell proliferation was determined by measuring the frequency of Ki67+ within naive and memory subsets (n = 4).
(G) Average IgG antibody titers directed against EBOV GP as measured in duplicate by ELISA (n = 4). (H and I) Frequency of naive, CM, and EM T cells within CD4 (H) and CD8 (I) subsets.
(J) Frequency of naive and memory B cells (n = 4).
Data are presented as mean ± SEM in (C)–(J). For changes in proliferation frequencies within lymphocyte subsets, a nonparametric trend where each time point is modeled by its own mean was assumed for statistical analysis; *p ≤ 0.05 and #p ≤ 0.05 at the indicated time point compared to 0 DPI (*p ≤ 0.05 for Ki67+ CD4 CM T cells, Ki67+ CD8 CM T cells, CD8 EM T cells and memory B cells and #p % 0.05 for Ki67+ CD8 EM T cells).
Flow cytometry analysis also indicated the activation of lymphocytes following VP35m infection. Although no significant differences in the frequency of total CD4 T cells, CD8 T cells, and CD20+ B cells were evident following VP35m infection (Figure 4C), significant increases in the frequency of proliferating CD4 and CD8 T cell memory subsets were detected in the higher dose group (Figures 4D and 4E) and surviving animals in the lower dose group (Figures S2H and S2I). Specifically, in the higher dose group, a significant increase in proliferation of CD4 central memory (CM) T cells was detected at 6 DPI (Figure 4D), albeit with no significant changes in the frequency of CD4 CM T cells (Figure 4H). A significant increase in proliferation of CD8 effector memory (EM) T cells was noted 10 DPI (Figure 4E) and preceded an increase in the frequency of CD8 EM T cells at 14 DPI (Figure 4I). Additionally, the proliferation of CD8 CM T cells increased at 14 DPI (Figure 4E). Moreover, we observed an increase in the frequency of proliferating naive B cells 3–14 DPI in the higher dose group (Figure 4F), which was accompanied by a significant increase in memory B cells at 14 DPI (Figure 4J). Importantly, gene expression signatures of differentiation of follicular B helper T cells and B cell activation preceded detection of EBOV glycoprotein (GP)-specific immunoglobulin G (IgG) titers (1:1,600–3,200) in four out of five animals at 14 DPI and in all animals by 28 DPI, including the animal that developed neurological disease (Figure 4G). In contrast, the control never demonstrated an antibody titer >1:100. Congruent with this observation, surviving animals in the lower dose group showed increased proliferation of memory B cells, which correlated with increased antibody titers at 14 DPI and time of wtEBOV challenge. In comparison, the subject that succumbed to wtEBOV challenge had an antibody titer of 1:400 at this time point (Figures S2J and S2K).
Serum neutralizing antibody titers were quantified using a plaque reduction neutralization test (PRNT50) (Table S1). Titers were generally low following VP35m challenge at both doses, suggesting non-neutralizing mechanisms of viral clearance, such as antibody-dependent cell-mediated cytotoxicity. PRNT50 values at 21 or 28 DPI ranged from <1:10 to 1:20 for the pilot and lower dose studies and 1:10 to 1:40 for the higher dose cohort. Neutralizing titers in survivors generally increased (1:20 to 1:80) after back-challenge with wtEBOV. No detectable neutralizing antibodies were detected in subjects that succumbed to EVD.
VP35m Infection Induces Robust and Sustained Gene Expression Changes Associated with Cellular Metabolism and Cell Cycle within PBMCs
DEGs in cluster 1 enriched to GO terms associated with cellular metabolism, gene expression, cell cycle, and response to stress (Figure 5A). Genes mapping to “response to stress” play an essential role in promoting cell proliferation, differentiation, and growth (JUND, LGALS1, PIM1, and TGFB1); chromatin condensation and DNA repair (SMARCB1, YY1, CINP, and SLX1A); and host defense (PIK3CD, STAT6, SPI1, CD37, IGHA1, CD8A, and PRF1) (Figure 5B). DEGs in cluster 1 that enriched to GO term “cellular metabolic process” play a role in respiration (NDUFA13), innate immunity (CYBA, CSF1R, S100A9, and NFKBIA), translation (EIF3G, RPS11, CARM1), signal transduction (PPP1R1B), carbohydrate metabolism (PYGB and GPT), apoptosis (BAD), and protein degradation and autophagy (ATG12 and UBE2M).
Figure 5. Animals Exhibit Sustained Gene Expression Changes Associated with Cellular Metabolism and Cell Cycle following VP35m Infection and Limited Gene Expression Changes following Subsequent wtEBOV Challenge.
(A) Bar graph depicting GO processes to which cluster 1 genes (see Figure S3B) enriched; the line graph represents −log10(FDR) of the enriched term.
(B) Heatmap representing gene expression (shown as absolute normalized RPKM values) of the DEGs in cluster 1 that enriched to “response to stress.” The range of colors is based on scaled and centered RPKM values of the entire set of genes (red represents increased expression, while blue represents decreased expression); each column represents the median RPKM values for each DPI.
(C) Bar graph depicting statistically significant GO processes to which cluster 2 genes (see Figure S3C) enriched; the line graph represents −log10(FDR) of the enriched term.
(D) Network depicting direct interactions of DEGs in cluster 2 with an RPKM R25 that map to the GO process “cellular metabolic process.”
For gene expression data shown in (A)–(D), the number of biological replicates at each time point are as follows: day 0 (n = 5), day 3 (n = 5), day 6 (n = 4), and day 10 (n = 5).
(E) Bar graph depicts number of protein-coding differentially expressed genes (DEGs; defined as those R2-fold change compared to 0 DPI and FDR-corrected p value ≥ 0.05) that have human homologs in VP35m-infected animals following challenge with wtEBOV (VP35m-wtEBOV); day 0 (n = 3), day 3 (n = 4), day 6 (n = 4), day 10 (n = 4), and day 28 (n = 4).
(F) Bar graph depicting statistically significant GO processes to which DEGs at 10 and 28 days after back-challenge enriched; the line graph represents −log10(FDR) of the enriched term.
Transcripts in cluster 2 mapped to GO terms associated primarily with metabolism and cell cycle (Figure 5C). Several of the downregulated DEGs that enriched to the GO term cellular metabolic process are predicted to interact with one another (Figure 5D). This network includes several transcription factors (STAT1, NFE2L2, and CEBPZ), and genes that play a role in (1) the regulation of cell proliferation and growth (e.g., KRAS, RASGRP1, and PPP2R3A, and MAP2K1; (2) DNA repair and replication, such as ATAD5 and NME7; and (3) ubiquitination and protein degradation (i.e., USP16, RNF149, RFFL, and KIF11) (Figure 5D).
VP35m-Challenged Monkeys Exhibit a Distinct Transcriptional Response following wtEBOV Infection Compared to Naive Animals
To obtain further insight into the impact of VP35 on pathogenesis, we compared host transcriptional responses to VP35m versus those obtained following wtEBOV-Makona infection (Versteeg et al., 2017). We chose 6 DPI for this comparison, since viremia was highest in the wtEBOV-infected animals and two of five VP35m subjects exhibited viremia (Figures 2C and 2D; Table 1). While the VP35m backbone was derived from the Mayinga variant of EBOV, the transcriptional response to this virus in cynomolgus macaques has not been published to date. However, phylogenetic analyses indicate that the Makona variant has 97% nucleotide identity to Mayinga and Kikwit variants (Baize et al., 2014). Our analysis revealed limited overlap in the number of DEGs, indicating a substantial difference in the host response to wtEBOV versus VP35m (Figure S4A). Common DEGs enriched to GO terms were associated with inflammation, innate immunity, and apoptosis, with a higher magnitude in fold change in VP35m-infected animals compared to EBOV-infected animals (Figures S4B and S4C), despite the limited systemic replication of VP35m.
Following wtEBOV back-challenge of animals previously infected with a higher dose of VP35m (VP35m-wtEBOV), transcriptional changes were mostly detected at 10 DPI, with transcriptional profiles at 28 DPI clustering with samples collected following VP35m challenge and samples collected 3–6 days after back-challenge (Figures S4D and 5E). Most DEGs at 10 DPI were downregulated and enriched to cellular metabolic process, “cellular response to stress” and “cell cycle” (Figure 5F). DEGs at 28 DPI enriched to similar GO terms in addition to “viral process” and response to cytokine (Figure 5F). We compared these gene expression changes to the dataset we recently reported following wtEBOV-Makona infection (Versteeg et al., 2017) at time points associated with the largest transcriptional response (10 DPI for VP35m-wtEBOV animals and 6 DPI for wtEBOV animals). These host responses were distinct considering the limited number of common DEGs detected (Figure S4E). Shared transcripts enriched to GO terms related to innate immunity and metabolism but were differentially downregulated in VP35m-wtEBOV animals and upregulated in animals only infected with wtEBOV (Figures S4F and S4G).
DISCUSSION
The determinants of EBOV virulence are not fully defined. Here, we sought to elucidate the contribution of VP35 immune evasion functions to EBOV pathogenesis. To address this question, an EBOV mutant designed to abrogate inhibition of RLR signaling was generated. The mutations introduced included two residues, K319 and R322, that when individually mutated to alanine in transfection studies impair or inhibit, respectively, IFN induction through RLR pathways (Leung et al., 2010b; Prins et al., 2010; Yen et al., 2014). The other mutated residue, F239, plays a critical role in VP35 end capping of dsRNA and inhibition of RIG-I signaling (Edwards et al., 2016; Leung et al., 2010a). We confirmed these prior findings in transfection studies, examining VP35 inhibition of an IFN-b promoter reporter gene. As expected, F239A and R322A each strongly impaired VP35 IFN-antagonist function, while K319A also inhibited activity, but to a lesser degree. Notably, a combination of all three mutations did not change inhibitory activity compared to the single point mutations. Assessing function of these VP35 mutants in a minigenome assay in which a model viral RNA that encodes luciferase is replicated by a viral RNA polymerase complex generated by co-transfection of NP, VP35, VP30, and L, indicated very modest effects of point mutations on activity and, again, no cumulative effect of combining mutations. Based on these data, we reasoned that introducing all three mutations into a recombinant EBOV would provide redundancy in terms of eliminating IFN-antagonist function, thereby reducing the likelihood of reversion. Despite the modest attenuation in minigenome assays and the substantial loss of IFN suppressing the activity of recombinant VP35, the VP35m virus exhibited surprisingly robust replication in cell culture, with only modest effects of the VP35 mutations on replication in wt A549 cells after infection at a relatively high MOI of 1. Strikingly, disruption of the IFN response by KO of MAVS did not increase replication of either wtEBOV or VP35m.
Upon infection of A549 cells, the VP35m virus triggered not only an IFN response, as indicated by upregulation of ISGs, but also expression of cytokines and genes associated with protein ubiquitination, consistent with broad activation of host signaling pathways related to innate immunity. These responses depended on the presence of the host signaling molecule MAVS, implicating RLR signaling as the main target of inhibition by the VP35 IID in EBOV-infected cells. Gene expression data comparing wtEBOV to VP35m in THP-1 cells corroborated this conclusion. It had not previously been demonstrated that the VP35 IID targets RLR signaling in the context of EBOV infection.
Previous in vivo studies indicated that a recombinant mouse-adapted EBOV (MA-EBOV) carrying a VP35 R312A point mutation was attenuated in mice (Hartman et al., 2008). Furthermore, infection of guinea pigs with recombinant guinea pig-adapted EBOV (GP-EBOV) possessing R322A and K319A mutations was avirulent in guinea pigs and protected animals against subsequent challenge wt GP-EBOV (Prins et al., 2010). However, these earlier studies required the use of a MA-EBOV or GPEBOV, which are genetically different from their parent strains (Bray et al., 1998, 2001; Ebihara et al., 2006; Prins et al., 2010). Further, these rodent models are more readily protected from challenge by antiviral or vaccine approaches than NHP models (Dhama et al., 2018; St Claire et al., 2017). Consequently, it is critical that potential determinants of EBOV virulence be assessed in NHPs, which are susceptible to EBOV strains that cause disease in humans (Geisbert et al., 2003a; Geisbert et al., 2003c). The cynomolgus macaque model closely mirrors human disease and serves as the gold standard for evaluating EBOV virulence (Geisbert et al., 2015). Therefore, while prior studies found that mutation of VP35 reduces lethality and decreases replication in guinea pig and mouse models, the present study provides substantial insight into the role of VP35 in EVD (Hartman et al., 2008; Prins et al., 2010). Challenge of cynomolgus macaques with 2 × 104 infectious units resulted in partial protection. The absence of viremia, clinical signs, and increased antibody titers in the two surviving animals correlated with monocyte and lymphocyte activation as well as earlier and larger transcriptional changes characterized by host defense compared to the fatal animal. Infection of cynomolgus macaques with 3.2 × 105 infectious units, as determined by back-titration of the inoculum, a 300-fold higher dose than the 1,000 infectious units typically given as a 100% lethal wtEBOV challenge, demonstrated remarkable attenuation. VP35m caused only very mild disease characterized by sporadic and low-level viremia in a small subset of animals compared to wtEBOV (4–5 log10 fold lower) (Geisbert et al., 2003a; Versteeg et al., 2017). These animals also had mild fever and modest increases in levels of inflammatory CRP at 3–6 DPI consistent with a modest immune response to the mutant virus. Importantly, we did not observe significant changes in liver and kidney enzymes or hematocrit percentages, features of typical EVD. Cumulatively, the in vivo data indicate that VP35 suppression of RLR signaling is a critical determinant of EBOV virulence.
Our transcriptomic data revealed large and stable gene expression changes following infection with a higher dose of VP35. This is in contrast to transcriptional changes following EBOV-Kikwit or EBOV-Makona infection in which limited transcriptional changes are detected at 3–4 DPI followed by widespread changes at 5–6 DPI (Rubins et al., 2007; Versteeg et al., 2017). A majority of genes that were differentially expressed throughout VP35m infection were involved in cellular metabolism and cell cycle, which may reflect the expansion of immune cells to support the development of a defense response.
Expression of genes important for innate immunity and inflammation peaked 3–6 DPI before decreasing 10 DPI, consistent with the slight increase in the frequency of monocytes and myeloid DCs (mDCs) 3–6 DPI. Although transcript levels of IFNB1 were only slightly increased at 6 DPI in two out of five animals, several ISGs increased in expression at 6 DPI before returning to near-baseline levels at 10 DPI. This response is in stark contrast to the response following wtEBOV infection, where, as infection progressed, the number of ISG transcripts and inflammatory DEGs exponentially increased (Rubins et al., 2007; Versteeg et al., 2017). Previous studies demonstrated that wtEBOV potently blocks DC maturation (Bosio et al., 2003; Mahanty et al., 2003). Studies using transfected VP35 or comparing infection of DCs with wtEBOV versus VP35 mutant EBOVs indicate that VP35 is necessary and sufficient to suppress the ability of DCs to induce T cell responses (Lubaki et al., 2013; Yen et al., 2014). This inhibition was abrogated by the introduction of F239A and R322A mutations in transfection studies or R312A in studies with EBOV (Lubaki et al., 2013; Yen et al., 2014). In line with these observations, we demonstrate an increased frequency of classical monocytes and mDCs expressing maturation marker CD86 as early as 3 DPI in addition to increased expression of genes that play a role in antigen presentation 6–10 DPI. We also report significant changes in genes that play a role in cellular metabolism 3–6 DPI. Up- and downregulated DEGs that enriched to cellular metabolic process are involved in signal transduction, protein degradation, and transcriptional regulation. Most noteworthy was an upregulation of genes that are involved in glycogenolysis (PYGB), glycolysis (ISYNA1), fatty acid oxidation (ACADVL), and cellular respiration (NDUFA1), which may support the energy demands of initiating an immune response.
In contrast to the lymphopenia observed post wtEBOV infection (Geisbert et al., 2000, 2003a; Versteeg et al., 2017), challenge with VP35m results in the development of a protective adaptive immune response. Specifically, we observed an increased proliferation of CD4 CM T cells, CD8 EM T cells and memory B cells consistent with the cluster 1 and 2 gene expression signatures that were associated with the cell cycle. Additionally, DEGs that dramatically increased 10 DPI enriched to T cell receptor (TCR) signaling, B cell activation, and the development of plasma B cells. We also detected an increase in the number CD8 EM T cells and memory B cells. Interestingly, genes associated with the development of T follicular helper cells (CXCR5 and CD40LG) significantly increased 3–6 DPI, preceding the peak of B cell activation and differentiation. Indeed, a humoral response was observed in four out of five animals at 14 DPI, and all animals developed EBOV GP-specific IgG and neutralizing antibodies before wtEBOV challenge. The antibody responses likely contributed to protection.
Cumulatively, the analyses above demonstrate that despite limited in vivo replication, an EBOV that lacks VP35 RLR inhibitory activity elicits robust immunity. Consistent with this finding, all VP35m-infected animals were able to survive a subsequent wtEBOV challenge. DEGs detected 10 days after wtEBOV infection were downregulated, indicative of the resolution of host responses to both VP35m and the subsequent back-challenge. Furthermore, this transcriptional response was substantially distinct from that observed in animals challenged with wtEBOV only. By day 28 after back-challenge, the transcriptional profiles of the PBMCs were similar to those detected on the day of wtEBOV challenge with a limited number of DEGs, further suggesting a resolution of transcriptional responses. These findings are consistent with, but substantially advance upon, an earlier study that demonstrated protection of guinea pigs to challenge with a guinea-pig-adapted EBOV by prior infection with a VP35 mutant EBOV (Prins et al., 2010).
In total, our data reveal that RLR signaling pathways are critical targets of VP35 in EBOV-infected cells and that inhibition of these pathways is critical for the development of EVD. Underlying the attenuation of the VP35m virus are large gene expression changes associated with cellular metabolism, cell cycle, and translation. These gene signatures are distinct from those detected in animals infected with wtEBOV, which exhibit exacerbated inflammation and an absence of adaptive immunity. Overall, the data demonstrate that VP35m is immunogenic and yields a strong yet controlled innate immune response that fosters the development of adaptive immunity to protect animals against EBOV challenge. These findings point to VP35 RLR inhibition as a therapeutic target. The efficient in vitro replication and substantial attenuation of the VP35m virus also suggest that it should be possible to develop fully replication-competent mutant EBOVs that can be safely grown outside of the biosafety level 4 (BSL4) containment used for filoviruses. This offers the prospect of developing live attenuated filoviruses as tools to facilitate basic and translation research without the need for constraints imposed by the BSL4 laboratory. The data further suggest it could be possible, despite the obvious regulatory hurdles and the need for multiple attenuating mutations to prevent reversion, to develop a live attenuated filovirus vaccine.
STAR★METHODS
LEAD CONTACT AND MATERIALS AVAILABILITY
Further information and requests for resources and reagents should be directed to and will be fulfilled by the Lead Contact, Christopher Basler (cbasler@gsu.edu). Plasmids generated in this study are available upon request. There are restrictions to the availability of wtEBOV and VP35m because they are classified as Select Agents by the United States Federal Select Agent Program.
EXPERIMENTAL MODEL AND SUBJECT DETAILS
Virus Strains
VP35m, a recombinant EBOV strain Mayinga-76 containing mutations F239A, R322A and K319A in VP35 (VP35m) was previously described (Luthra et al., 2013). Stocks of this virus and parental wt EBOV strain Mayinga-76 were prepared by amplification on Vero E6 cells. Ebola virus Zaire isolate 199510621 (strain Kikwit) originated from a 65-year-old female patient who had died on 5 May 1995. The study challenge material was from the second Vero E6 passage of Zaire isolate 199510621. Briefly, the first passage at the University of Texas Medical Branch at Galveston (UTMB) consisted of inoculating CDC 807223 (passage 1 of Ebola virus isolate 199510621) at a multiplicity of infection (MOI) of 0.001 onto Vero E6 cells. The cell supernatants were subsequently harvested at 10 days post-infection and put in vials in 1 mL aliquots. Deep sequencing indicated the Zaire virus was greater than 98% 7U (consecutive stretch of 7 uridines).
Cell Lines
Vero E6 (VERO C1008 [Vero 76, clone E6, Vero E6] (ATCC® CRL-1586)), HEK293T (ATCC® CRL-3216), and THP-1 (ATCC® TIB-202) cells used for filovirus propagation and plaque assays were obtained from ATCC. wt and MAVS KO A549 cells were provided by Susan Weiss (University of Pennsylvania). All cell lines were maintained in Dulbecco’s Modified Eagle’s Medium, 10% fetal bovine serum, 2mM L-glutamine.
Animal Subjects
Healthy adult (3–8 years of age) cynomolgus macaques (Macaca fascicularis) of Chinese origin (~3–7.5 kg) were used. Animal studies were conducted in compliance with the Animal Welfare Act and other federal statutes and regulations relating to animals and experiments involving animals and adhered to principles stated in the eighth edition of the “Guide for the Care and Use of Laboratory Animals” (National Research Council, 2011). The facility where this research was conducted (UTMB) is fully accredited by the Association for the Assessment and Accreditation of Laboratory Animal Care International and has an approved OLAW Assurance (#A3314–01). Additional information on sex and care through the course of the experiments is provided below under Method Details in the Virus challenge section.
METHOD DETAILS
Virus Challenge
Thirteen healthy cynomolgus macaques were used to conduct three separate studies. In an initial pilot study two males were inoculated intramuscularly (i.m.) with a target dose of 20,000 pfu of VP35m (actual dose of VP35m was determined to be 18,000 pfu). In a second lower dose study three males were inoculated i.m. with a target dose of 20,000 pfu of VP35m (actual dose of VP35m was determined to be 27,750 pfu). At day 28 after the VP35m exposure, these three animals were back-challenged i.m. with a target dose of 1,000 pfu EBOV (Kikwit strain) (actual challenge dose of EBOV was determined to be 1,063 pfu). In the third and final higher dose study five animals (two males and three females) were inoculated i.m. with a target dose of 5×105 pfu of VP35m (actual dose of VP35m was determined to be 3.2×105 pfu) and were also back-challenged i.m. with 1000 pfu EBOV-Kikwit at the same time point. One monkey not inoculated with VP35m served as a control for the back-challenge; this animal also received a target dose of 1000 pfu of EBOV-Kikwit. All thirteen animals were given physical exams and blood was collected at the time of infection and at various times after VP35m or EBOV infection. In addition, all animals were monitored daily and scored for disease progression with an internal filovirus scoring protocol approved by the UTMB Institutional Animal Care and Use Committee. The scoring changes measured from baseline included posture/activity level, attitude/behavior, food and water intake, respiration, and disease manifestations such as visible rash, hemorrhage, and/or ecchymosis. A score of ≥ 9 indicated that an animal met criteria for euthanasia. These studies were not blinded.
Sample Collection and PBMC Isolation
Blood was collected by venipuncture into EDTA and serum tubes according to the study design (Figure 2A). To separate plasma and serum, tubes were spun at 2500 rpm for 10 minutes at 4°C. EDTA plasma and serum were stored at 80°C for future analysis and virus quantification. To isolate PBMC, WB was centrifuged over Histopaque (Sigma-Aldrich, St. Louis, MO) using AccuSpin Tubes (Sigma-Aldrich, St. Louis, MO) at 1400 rpm for 45 minutes, room temperature with no brake. The PBMC buffy coat was extracted and washed in RPMI media. Isolated cells were counted on a TC20 Automated Cell Counter (Bio-Rad, Hercules, CA). 1.0 × 106 PBMC were put into Trizol (Invivogen) buffer for RNA isolation. Remaining PBMC were frozen and stored at −80°C (stable for 6 months) for future analysis.
Viral RNA and Viremia
RNA was isolated from whole blood utilizing the Viral RNA mini-kit (QIAGEN) using 100 μL of blood added to 600 μL of the viral lysis buffer supplied in the kit. Primers or probe targeting the VP30 gene of EBOV were used for real-time quantitative PCR (RT-qPCR) with the probe used here being EBOV, 6-carboxyfluorescein (FAM)-5′ CCG TCA ATC AAG GAG CGC CTC 3′-6 carboxytetramethylrhodamine (TAMRA; Life Technologies). Viral RNA was detected using the CFX96 detection system (Bio-Rad Laboratories, Hercules, CA) in one-step probe RT-qPCR kits (QIAGEN) with the following cycle conditions: 50°C for 10 min, 95°C for 10 s, and 40 cycles of 95°C for 10 s and 57°C for 30 s. Threshold cycle (CT) values representing viral genomes were analyzed with CFX Manager software, and the data are shown as genome equivalents (GEq) per milliliter. To create the GEq standard, RNA from viral stocks was extracted, and the number of strain-specific genomes was calculated using Avogadro’s number and the molecular weight of each viral genome.
Virus titration was performed by plaque assay with Vero E6 cells from all plasma samples, as previously described (Geisbert et al., 2003a). Briefly, increasing tenfold dilutions of the samples were adsorbed to Vero E6 monolayers in duplicate wells (200 μl); the limit of detection was 25 pfu/ml.
Hematology and Clinical Chemistry
Total white blood cell counts, white blood cell differentials, red blood cell counts, platelet counts, hematocrit values, total hemoglobin concentrations, mean cell volumes, mean corpuscular volumes, and mean corpuscular hemoglobin concentrations were analyzed from blood collected in tubes containing EDTA using a laser based hematologic analyzer (Beckman Coulter). A Piccolo point-of-care analyzer and Biochemistry Panel Plus analyzer discs (Abaxis) were used to test for serum concentrations of albumin, amylase, alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), gamma-glutamyltransferase (GGT), glucose, cholesterol, total protein, blood urea nitrogen (BUN), creatinine (CRE), uric acid, and C-reactive protein (CRP).
Histopathology and Immunohistochemistry
Necropsy was performed on all subjects. Tissue samples of all major organs were collected for histopathologic and immunohistochemical examination, immersion-fixed in 10% neutral buffered formalin, and processed for histopathology as previously described (Thi et al., 2015) For immunohistochemistry, specific anti-EBOV immunoreactivity was detected using an anti-EBOV VP40 protein rabbit primary antibody (Integrated BioTherapeutics) at a 1:4000 dilution. In brief, tissue sections were processed for immunohistochemistry using the Dako Autostainer (Dako). Secondary antibody used was biotinylated goat anti-rabbit IgG (Vector Laboratories) at 1:200 followed by Dako LSAB2 streptavidin-HRP (Dako). Slides were developed with Dako DAB chromogen (Dako) and counter-stained with hematoxylin. Non-immune rabbit IgG was used as a negative control.
Enzyme-Linked Immunosorbent Assay
NHP sera collected at times before and after exposure to VP35m were tested for cross-reactive immunoglobulin G (IgG) antibodies against EBOV. Enzyme-linked immunosorbent assay was used to detect cross-reactive IgG as previously described (Jahrling et al., 2007)
Virus Neutralization Assay
Neutralizing antibody titers were determined by performing plaque reduction neutralization titration assays (PRNT50). Briefly, Vero cells were seeded into 6 well plates to generate a confluent monolayer on the day of infection. Serum dilutions were prepared in DMEM and 100 μL were incubated with ~100 pfu of EBOV (Kikwit strain) in a total volume of 200 μL at 37 C for 60 min. Media was removed from cells, the serum-virus mixture was added in duplicate, and samples were incubated for 60 min at 37°C. The mixture was removed from the cells and 2 mL of 0.9% agarose in EMEM with 5% FBS was overlaid onto the wells. Cells were observed 7 days post-incubation and plaques were counted using neutral red stain. The neutralizing antibody titer of a serum sample was considered positive at a dilution showing a ≥ 50% reduction (PRNT50) compared with the virus control without serum.
Flow Cytometry Staining and Analysis
Cryopreserved PBMCs were thawed rapidly in a 37°C water bath and washed in BD staining buffer. To delineate cell subsets in the innate panel, PBMCs were stained with anti-human CD3, CD20, HLA-DR, CD14, CD16, CD11c, CD123, and CD86 fluorochromeconjugated antibodies for ~30 minutes in the dark and fixed with a 4% paraformaldehyde solution. Live CD3-CD20-HLA-DR+ populations that were positive for CD14, CD11c, and CD123, were classified as monocytes, myeloid DCs, and plasmacytoid DCs, respectively. Any additional PBMCs within this population that did not express CD14, CD11c, and CD123 were defined as “other DCs.” Within the CD14+ population, monocytes were further separated into classical (CD16-) and nonclassical (CD16+) subsets. Activated monocytes and DC populations were identified based on increased expression of CD86. For the adaptive panel, PBMCs were stained with antibodies against CD4, CD8b, CD20, CD27, CD28, and CD95 surface markers and fixed/permeabilized with a Tonbo Foxp3/Transcription Factor Staining Buffer Kit according to the manufacturer recommendations. Thereafter, a Ki67-specific intracellular antibody was added to discriminate proliferating subsets. Live cells were gated on CD4 or CD8β for the T cell populations and stained with antibodies against CD28 and CD95 (BioLegend) to distinguish naive (CD28+CD95−), central memory (CD28+CD95+), and effector memory (CD28−CD95+) subsets. For B cells, CD20 and CD27 markers were used to denote naïve (CD20+CD27−) and memory (CD20+CD27+) subsets. For both innate and adaptive panels, live versus dead cells were differentiated with BV510 fixable viability dye. Approximately one million events per sample were collected on a FACS Canto II cytometer (BD Biosciences, San Jose, CA) using BD FACS Diva acquisition software and analyzed using FlowJo version 10. Color compensation was calculated using BD CompBeads.
Cytokine, Chemokine, and Growth Factor Analysis
Circulating cytokines were measured in the serum using Invitrogen eBioscience ProcartaPlex NHP Cytokine/Chemokine/Growth factor 37-plex panel that measures Brain-Derived Neurotrophic Factor (BDNF), CCL2 (MCP-1), CCL3 (MIP-1 alpha), CCL4 (MIP-1 beta), CXCL10 (IP-10), CXCL12 alpha (SDF-1 alpha), CXCL13, CXCL9 (MIG), Eotaxin, FGF basic, G-CSF, GM-CSF, I-TAC/CXCL11, IFN alpha, IFN gamma, IL-1 beta, IL-1 Receptor Antagonist, IL-10, IL-12, IL-13, IL-15, IL-17A, IL-18, IL-2, IL-23, IL-4, IL-5, IL-6, IL-7, IL-8, NGF beta, PDGF-BB, sCD40, Stem Cell Factor (SCF), TNF alpha, VEGF-A, and VEGF-D.
Library Generation and Sequencing
RNA was isolated from PBMC using a Zymo Research Direct-zol RNA mini-prep kit. RNA concentration and integrity was determined using an Agilent 2100 Bioanalyzer. Ribosomal RNA (rRNA) was depleted and libraries were constructed using the TruSeq Stranded Total RNA LT-LS kit. First, rRNA-depleted RNA was fragmented and converted to double stranded cDNA. Adapters were ligated and the ~300 base pair (bp) long fragments were then amplified by PCR and selected by size exclusion. Each library was prepared with a unique indexed primer for multiplexing. In order to ensure proper sizing, quantitation, and quality prior to sequencing, libraries were analyzed on the Agilent 2100 Bioanalyzer. Multiplexed libraries were subjected to single-end 75bp sequencing using the Illumina NextSeq500 platform.
IFN-β Luciferase Assay
HEK293T cells were transfected using lipofectamine 2000 with VP35 or VP35 mutant expression plasmids (at 10 and 100 ng) along with an IFN-b promoter-firefly reporter plasmid (100ng) and a plasmid that constitutively expressed Renilla luciferase (50ng) as a transfection control. The indicated plasmid amounts are per well of 96 well plates. The next day, cells were infected with Sendai virus (SeV, 100 HA units). 20h later, luciferase activity was determined using Dual Glo reagents from Promega and firefly luciferase activity was normalized to Renilla luciferase activity.
Ebola Virus Minigenome Assay
The Ebola virus polymerase complex was tested for function using a minigenome assay (Edwards et al., 2015). Briefly, the viral polymerase complex was reconstituted by transfecting plasmids that express EBOV nucleoprotein (NP) (62.5ng), large protein (L) (125ng), VP30 protein (25ng), VP35 or VP35 mutants (12.5, 31.25, or 62.5ng), T7 RNA polymerase (50ng), and a plasmid that produces a model EBOV “minigenome” RNA that encodes Renilla luciferase (50ng), and a plasmid that constitutively-expresses firefly luciferase (1ng) by using lipofectamine 2000 (Thermo Fisher) in HEK293T cells in 96 well plates. The luciferase activities were determined 48h post transfection using Dual Glo reagents (Promega). Minigenome activity was calculated by normalizing Renilla luciferase to firefly luciferase activities.
Ebola Virus Infection in A549 Cells
A549-wt or MAVS deficient A549 cells were infected with wtEBOV (Mayinga strain) or VP35m virus at MOI of 1. The supernatants were collected at 1, 24, 48 and 72h post infection. The viral titers were determined by plaque assay. The RNA extractions were performed using Direct-zol RNA kit from Zymo research following the manufacturer’s instructions.
QUANTIFICATION AND STATISTICAL ANALYSIS
Viral Load, Clinical Data, Reporter Assays, and ELISA Data
Statistical analysis of viral load, hematology and clinical chemistry data, and antibody titers was conducted using GraphPad Prism software (GraphPad, Software, Inc., La Jolla, CA). Significant values were determined using one-way ANOVA with an alpha value of 0.05 or less.
Flow Cytometry Data
Because we did not have the same number of animals at each time point, statistical analysis of flow cytometry data was carried out using the SAS software, PROC MIXED. A repeated-measures analysis was used to model each of the dependent variables. Intra-animal correlation was modeled using a compound symmetric variance-covariance structure. A nonparametric trend was used where each time point was modeled by its own mean. Missing data were handled by using maximum likelihood algorithms to fit the model. When a linear model was an adequate trend, the p value for the estimated slope was reported. When each time point was modeled by its own mean, the mean response at each non-zero time point was contrasted with the mean response at the zero time point. Holm’s multiple comparison method was used to adjust the p values for each contrast.
RNA-Seq Bioinformatic Analysis
Data analysis was performed with the RNA-seq workflow module of the systemPipeR package available on Bioconductor (Backman and Girke, 2016) and as previously described (Versteeg et al., 2017). RNA-seq reads were demultiplexed, quality filtered, and trimmed using Trim Galore with an average phred score cutoff of 30 and minimum length of 50bp. Quality reports were generated with the FastQC function. For in vitro infection assays, the human genome (Homo_sapiens.GRCh38.dna.primary_assembly.fa) and annotation file (Homo_sapiens.GRCh38.85.gtf) was used as reference. For gene expression studies in Cynomolgus macaques, the Macaca fascicularis reference genome (Macaca_fascicularis.Macaca_fascicularis_5.0.dna.toplevel.fa) and annotation file (Macaca_fascicularis.Macaca_fascicularis_5.0.94.gtf) was used as reference. RNA-seq reads were mapped with the alignment suite Bowtie2/Tophat2 against the reference genome. Raw expression values in the form of gene-level read counts were generated with the summarizeOverlaps function, counting only the reads overlapping exonic regions of genes, and discarding reads mapping to ambiguous regions of exons from overlapping genes. Normalization and statistical analysis of differentially expressed genes (DEGs) was performed using the edgeR package.
Gene clusters following VP35m infection in vivo were identified by Short Time-series Expression Miner (STEM) of median normalized reads focusing on transcripts an average RPKM of 5 or greater. The parameter for “model profiles” and “maximum unit change between time points” was set to default 50 and 2, respectively. Only statistically significant clusters with a p value ≤ 0.05 were included for downstream analysis. Host differentially expressed genes (DEGs) following in vitro infection or in vivo wtEBOV infection were obtained using the RNA-seq workflow module of systemPipeR and defined as those with a fold change ≥ 2 and a false discovery rate (FDR) corrected p value ≤ 0.05 compared to 0 DPI. Only protein coding genes with human homologs and an average of 5 reads per kilobase of transcript per million mapped reads (RPKM) were included for further analysis. Principal component, violin plots, heatmaps, and Venn diagrams were generated using R packages DESeq2, ggplot2 and VennDiagram.
Functional enrichment of these genes was done to identify clusters of genes mapping to specific biological pathways, specifically gene ontology (GO) terms using MetaCore™ (Thomson Reuters, New York, NY).
DATA AND CODE AVAILABILITY
The accession number for the RNA-sequencing data reported in this paper is SRA: PRJNA548965.
Supplementary Material
KEY RESOURCES TABLE
| REAGENT or RESOURCE | SOURCE | IDENTIFIER |
|---|---|---|
| Antibodies | ||
| BV510 Viability Stain (Innate and Adaptive Flow Panels) | BD Biosciences | cat#: 564406 |
| Anti-human CD3 FITC | BD Biosciences | Cat#556611; RRID:AB_396484 |
| Anti-human CD20 FITC | BD Biosciences | Cat#556632; RRID:AB_396501 |
| Anti-human HLA-DR APC-Cy7 | Biolegend | Cat#307618; RRID:AB_493586 |
| Anti-human CD14 APC | Biolegend | Cat#301808; RRID:AB_314190 |
| Anti-human CD16 PE | Biolegend | Cat#302008; RRID:AB_314208 |
| Anti-human CD11c PE-Cy7 | Biolegend | Cat#301608; RRID:AB_389351 |
| Anti-human CD123 PerCP-Cy5.5 | Biolegend | Cat#306016; RRID:AB_2264693 |
| Anti-human CD86 BV421 | Biolegend | Cat#305426; RRID:AB_11204252 |
| Anti-human CD4 PerCP-Cy5.5 | Tonbo Biosciences | Cat#65–0048; RRID:AB_2621878 |
| Anti-human CD8β ECD | Beckman Coulter | Cat#IM2014; RRID:AB_131677 |
| Anti-human CD20 PE-Cy7 | eBioscience | Cat#560735; RRID:AB_1727450 |
| Anti-human CD28 BV421 | Biolegend | Cat#302930; RRID:AB_2561910 |
| Anti-human CD95 APC | Biolegend | Cat#558814; RRID:AB_398659 |
| Anti-human CD27 APC-Cy7 | Biolegend | Cat#302816; RRID:AB_571977 |
| Anti-Ki67 FITC | BD Biosciences | Cat#556026; RRID:AB_396302 |
| Mouse monoclonal anti-β-tubulin antibody | Sigma Aldrich | Cat#T8328; RRID: AB_1844090 |
| Mouse monoclonal anti-FLAG M2 antibody | Sigma Aldrich | Cat#F1804; RRID: AB_262044 |
| Goat anti-NHP IgG HRP | Fitzgerald Industries International | Cat: 43R-IG020HRP; RRID:AB_1287018 |
| Goat anti-NHP IgM HRP | Fitzgerald Industries International | Cat: 43R-IG074hrp; RRID:AB_1287508 |
| Bacterial and Virus Strains | ||
| EBOV-Kitwit | CDC | 807223 (passage 1 of Ebola virus isolate 199510621) |
| VP35 mutant EBOV | (Luthra et al., 2013) | N/A |
| Sendai virus | ATCC | VR907 |
| Critical Commercial Assays | ||
| QIAmp Viral RNA kit | QIAGEN | Cat#: 52904 |
| TruSeq Stranded Total RNA LT-LS kit | Illumina | Cat#: 20020597 |
| NextSeq 500/550 High Output v2 kit | Illumina | FC-404–2005 |
| Zymo Research Direct-zol RNA mini-prep | Zymo Research Corp. | Cat# R2070 |
| InvitrogenT eBioscienceT ProcartaPlex NHP Cytokine/Chemokine/Growth Factor Panel (37 plex) | Invitrogen | Cat# EPX37040045901; RRID:AB_2576125 |
| Dual-Glo® Luciferase Assay System | Promega | Cat#E2940 |
| SuperScript® III First-Strand Synthesis System | Thermo Fisher Scientific | Cat#18080051 |
| Deposited Data | ||
| RNA seq data | This paper | SRA: PRJNA548965 |
| Homo sapiens genome, build 38 GRCh38 | Ensembl | Homo_sapiens.GRCh38.dna.primary_assembly.fa |
| Homo sapiens annotation file build 38 | Ensembl | Homo_sapiens.GRCh38.85.gtf |
| Macaca mulatta genome build 78 | Ensembl | Macaca_mulatta.MMUL_1.dna.toplevel.fa |
| Macaca mulatta annotation file build 78 | Ensembl | Macaca_mulatta.MMUL_1.78.gtf |
| PBMC Transcriptome data from EBOV-Makona infected macaques | (Versteeg et al., 2017) | SRA Accession number PRJNA398558 |
| Experimental Models: Cell Lines | ||
| A549 cells | Susan R. Weiss, University of Pennsylvania (Li et al., 2017) | N/A |
| MAVS knockout A549 cells | Susan R. Weiss, University of Pennsylvania (Li et al., 2017) | N/A |
| Thp1 cells | ATCC | Cat.# TIB-202; RRID:CVCL_0006 |
| HEK293T | ATCC | Cat. # CRL-11268; RRID:CVCL_0063 |
| Experimental Models: Organisms/Strains | ||
| Cynomolgus macaques | PrimGen | N/A |
| Oligonucleotides | ||
| Forward human RIG-I primer: ggcatgttacacagctgacg | (Luthra et al., 2013) | N/A |
| Reverse human RIG-I primer: tgcaatatcctccaccacaa | (Luthra et al., 2013) | N/A |
| Forward human IFNβ primer: GTCAGAGTGGAAATCCTAAG | (Luthra et al., 2013) | N/A |
| Reverse human IFNβ primer: CAGCATCTGCTGGTTGAAG | (Luthra et al., 2013) | N/A |
| Forward human IFIT1 primer: AGTGTGGGAATACACAACCTACT | (Luthra et al., 2013) | N/A |
| Reverse human IFIT1 primer: GGTCACCAGACTCCTCACATTT | (Luthra et al., 2013) | N/A |
| Forward human β-actin primer:ACTGGAACGGTGAAGGTGAC | (Luthra et al., 2013) | N/A |
| Recombinant DNA | ||
| pCAGGS-FLAG VP35-F239A | This paper | N/A |
| pCAGGS-FLAG VP35-R322A | This paper | N/A |
| pCAGGS-FLAG VP35-K319A/R322A | This paper | N/A |
| pCAGGS-FLAG VP35-F239A/K319A/R322A | This paper | N/A |
| pCAGGS-NP | Edwards et al., 2015 | N/A |
| pCAGGS-VP35 | Edwards et al., 2015 | N/A |
| pCAGGS-VP30 | Edwards et al., 2015 | N/A |
| pCAGGS-L | Edwards et al., 2015 | N/A |
| pCAGGS-T7 | Edwards et al., 2015 | N/A |
| pM1-MG | Edwards et al., 2015 | N/A |
| IFNβ-Firefly luciferase | Luthra et al., 2013 | N/A |
| pRL-TK | Luthra et al., 2013 | N/A |
| pCAGGS-Firefly luciferase | Luthra et al., 2017 | N/A |
| Software and Algorithms | ||
| TrimGalore | Babraham Bioinformatics | https://github.com/FelixKrueger/TrimGalore/blob/master/Docs/Trim_Galore_User_Guide.md |
| Short Time-series Expression Miner (STEM) | (Ernst and Bar-Joseph, 2006) | http://www.cs.cmu.edu/~jernst/stem/ |
| DESeq2 | (Love et al., 2014) | https://bioconductor.org/packages/release/bioc/html/DESeq2.html |
| Ggplot2 | Hadley Wickham | https://ggplot2.tidyverse.org/ |
| VennDiagram | Hanbo Chen | https://cran.r-project.org/web/packages/VennDiagram/index.html |
| MetaCore version 6.36 build 69400 | Thomson Rheuters | https://portal.genego.com/ |
| BD FACS Diva | BD Biosciences | http://www.bdbiosciences.com/en-us/instruments/research-instruments/research-software/flow-cytometry-acquisition/facsdiva-software |
| FlowJo Version 10 | Tree Star | https://www.flowjo.com/ |
Highlights.
A VP35 mutant Ebola virus (VP35m) induces MAVS-dependent interferon responses
VP35m is highly attenuated in cynomolgus macaques
VP35m elicits robust adaptive immune responses despite minimal replication in vivo
VP35m protects cynomolgus macaques from challenge with wild-type Ebola virus
ACKNOWLEDGMENTS
This work was supported by the National Institute of Allergy and Infectious Diseases (NIAID) and NIH grant U19A109945 (to C.F.B., I.M., and T.W.G.). Preparation of the Ebola virus seed stock was supported by NIAID/NIH grant U19AI109711 to T.W.G. Operations support of the Galveston National Laboratory was supported by NIAID/NIH grant UC7AI094660. We thank Daniel Deer for assistance in performing the nonhuman primate studies. We also thank the UTMB Animal Resource Center for husbandry of laboratory animals and Natalie Dobias (Department of Microbiology and Immunology, UTMB) for expert assistance with histology and immunohistochemistry assays. We thank Drs. Yize (Henry) Li and Susan R. Weiss (Department of Microbiology, Perelman School of Medicine, University of Pennsylvania) for kindly providing the parental and MAVS KO A549 cells.
Footnotes
SUPPLEMENTAL INFORMATION
Supplemental Information can be found online at https://doi.org/10.1016/j.celrep.2019.08.047.
DECLARATION OF INTERESTS
The authors declare no competing interests.
REFERENCES
- Backman TWH, and Girke T (2016). systemPipeR: NGS workflow and report generation environment. BMC Bioinformatics 17, 388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baize S, Pannetier D, Oestereich L, Rieger T, Koivogui L, Magassouba N, Soropogui B, Sow MS, Keı¨ta S, De Clerck H, et al. (2014). Emergence of Zaire Ebola virus disease in Guinea. N. Engl. J. Med 371, 1418–1425. [DOI] [PubMed] [Google Scholar]
- Bale S, Julien JP, Bornholdt ZA, Krois AS, Wilson IA, and Saphire EO (2013). Ebolavirus VP35 coats the backbone of double-stranded RNA for interferon antagonism. J. Virol 87, 10385–10388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bausch DG (2017). West Africa 2013 Ebola: From Virus Outbreak to Humanitarian Crisis. Curr. Top. Microbiol. Immunol 411, 63–92. [DOI] [PubMed] [Google Scholar]
- Bosio CM, Aman MJ, Grogan C, Hogan R, Ruthel G, Negley D, Mohamadzadeh M, Bavari S, and Schmaljohn A (2003). Ebola and Marburg viruses replicate in monocyte-derived dendritic cells without inducing the production of cytokines and full maturation. J. Infect. Dis 188, 1630–1638. [DOI] [PubMed] [Google Scholar]
- Bray M, Davis K, Geisbert T, Schmaljohn C, and Huggins J (1998). A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J. Infect. Dis 178, 651–661. [DOI] [PubMed] [Google Scholar]
- Bray M, Hatfill S, Hensley L, and Huggins JW (2001). Haematological, biochemical and coagulation changes in mice, guinea-pigs and monkeys infected with a mouse-adapted variant of Ebola Zaire virus. J. Comp. Pathol 125, 243–253. [DOI] [PubMed] [Google Scholar]
- Callendret B, Vellinga J, Wunderlich K, Rodriguez A, Steigerwald R, Dir-meier U, Cheminay C, Volkmann A, Brasel T, Carrion R, et al. (2018). A prophylactic multivalent vaccine against different filovirus species is immunogenic and provides protection from lethal infections with Ebolavirus and Marburgvirus species in non-human primates. PLoS ONE 13, e0192312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cárdenas WB, Loo YM, Gale M Jr., Hartman AL, Kimberlin CR, Martínez-Sobrido L, Saphire EO, and Basler CF (2006). Ebola virus VP35 protein binds double-stranded RNA and inhibits alpha/beta interferon production induced by RIG-I signaling. J. Virol 80, 5168–5178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow KT, Gale M Jr., and Loo YM (2018). RIG-I and other RNA sensors in antiviral immunity. Annu. Rev. Immunol 36, 667–694. [DOI] [PubMed] [Google Scholar]
- Cross RW, Mire CE, Feldmann H, and Geisbert TW (2018). Post-exposure treatments for Ebola and Marburg virus infections. Nat. Rev. Drug Discov 17, 413–434. [DOI] [PubMed] [Google Scholar]
- Dhama K, Karthik K, Khandia R, Chakraborty S, Munjal A, Latheef SK, Kumar D, Ramakrishnan MA, Malik YS, Singh R, et al. (2018). Advances in designing and developing vaccines, drugs, and therapies to counter Ebola virus. Front. Immunol 9, 1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebihara H, Takada A, Kobasa D, Jones S, Neumann G, Theriault S, Bray M, Feldmann H, and Kawaoka Y (2006). Molecular determinants of Ebola virus virulence in mice. PLoS Pathog 2, e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards MR, Pietzsch C, Vausselin T, Shaw ML, Bukreyev A, and Basler CF (2015). High-throughput minigenome system for identifying small-molecule inhibitors of Ebola virus replication. ACS Infect. Dis 1, 380–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards MR, Liu G, Mire CE, Sureshchandra S, Luthra P, Yen B, Shabman RS, Leung DW, Messaoudi I, Geisbert TW, et al. (2016). Differential regulation of interferon responses by Ebola and Marburg virus VP35 proteins. Cell Rep. 14, 1632–1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst J, and Bar-Joseph Z (2006). STEM: a tool for the analysis of short time series gene expression data. BMC Bioinformatics 7, 191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldmann H, Sanchez A, and Geisbert TW (2013). Fields VirologySixth Edition, Volume 1 (Wolters Kluwer; ). [Google Scholar]
- Geisbert TW, Hensley LE, Gibb TR, Steele KE, Jaax NK, and Jahrling PB (2000). Apoptosis induced in vitro and in vivo during infection by Ebola and Marburg viruses. Lab. Invest 80, 171–186. [DOI] [PubMed] [Google Scholar]
- Geisbert TW, Hensley LE, Larsen T, Young HA, Reed DS, Geisbert JB, Scott DP, Kagan E, Jahrling PB, and Davis KJ (2003a). Pathogenesis of Ebola hemorrhagic fever in cynomolgus macaques: evidence that dendritic cells are early and sustained targets of infection. Am. J. Pathol 163, 2347–2370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisbert TW, Young HA, Jahrling PB, Davis KJ, Kagan E, and Hensley LE (2003b). Mechanisms underlying coagulation abnormalities in ebola hemorrhagic fever: overexpression of tissue factor in primate monocytes/macrophages is a key event. J. Infect. Dis 188, 1618–1629. [DOI] [PubMed] [Google Scholar]
- Geisbert TW, Young HA, Jahrling PB, Davis KJ, Larsen T, Kagan E, and Hensley LE (2003c). Pathogenesis of Ebola hemorrhagic fever in primate models: evidence that hemorrhage is not a direct effect of virus-induced cytolysis of endothelial cells. Am. J. Pathol 163, 2371–2382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisbert TW, Strong JE, and Feldmann H (2015). Considerations in the use of nonhuman primate models of ebola virus and marburg virus infection. J. Infect. Dis 212 (Suppl 2), S91–S97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harcourt BH, Sanchez A, and Offermann MK (1998). Ebola virus inhibits induction of genes by double-stranded RNA in endothelial cells. Virology 252, 179–188. [DOI] [PubMed] [Google Scholar]
- Hartman AL, Towner JS, and Nichol ST (2004). A C-terminal basic amino acid motif of Zaire ebolavirus VP35 is essential for type I interferon antagonism and displays high identity with the RNA-binding domain of another interferon antagonist, the NS1 protein of influenza A virus. Virology 328, 177–184. [DOI] [PubMed] [Google Scholar]
- Hartman AL, Dover JE, Towner JS, and Nichol ST (2006). Reverse genetic generation of recombinant Zaire Ebola viruses containing disrupted IRF-3 inhibitory domains results in attenuated virus growth in vitro and higher levels of IRF-3 activation without inhibiting viral transcription or replication. J. Virol 80, 6430–6440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman AL, Bird BH, Towner JS, Antoniadou ZA, Zaki SR, and Nichol ST (2008). Inhibition of IRF-3 activation by VP35 is critical for the high level of virulence of Ebola virus. J. Virol 82, 2699–2704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahrling PB, Geisbert JB, Swearengen JR, Larsen T, and Geisbert TW (2007). Ebola hemorrhagic fever: evaluation of passive immunotherapy in nonhuman primates. J. Infect. Dis 196 (Suppl 2), S400–S403. [DOI] [PubMed] [Google Scholar]
- Kato H, Sato S, Yoneyama M, Yamamoto M, Uematsu S, Matsui K, Tsujimura T, Takeda K, Fujita T, Takeuchi O, and Akira S (2005). Cell type-specific involvement of RIG-I in antiviral response. Immunity 23, 19–28. [DOI] [PubMed] [Google Scholar]
- Kimberlin CR, Bornholdt ZA, Li S, Woods VL Jr., MacRae IJ, and Saphire EO (2010). Ebolavirus VP35 uses a bimodal strategy to bind dsRNA for innate immune suppression. Proc. Natl. Acad. Sci. USA 107, 314–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung DW, Ginder ND, Fulton DB, Nix J, Basler CF, Honzatko RB, and Amarasinghe GK (2009). Structure of the Ebola VP35 interferon inhibitory domain. Proc. Natl. Acad. Sci. USA 106, 411–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung DW, Prins KC, Borek DM, Farahbakhsh M, Tufariello JM, Ramanan P, Nix JC, Helgeson LA, Otwinowski Z, Honzatko RB, et al. (2010a). Structural basis for dsRNA recognition and interferon antagonism by Ebola VP35. Nat. Struct. Mol. Biol 17, 165–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung DW, Shabman RS, Farahbakhsh M, Prins KC, Borek DM, Wang T, Mühlberger E, Basler CF, and Amarasinghe GK (2010b). Structural and functional characterization of Reston Ebola virus VP35 interferon inhibitory domain. J. Mol. Biol 399, 347–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Banerjee S, Wang Y, Goldstein SA, Dong B, Gaughan C, Silverman RH, and Weiss SR (2016). Activation of RNase L is dependent on OAS3 expression during infection with diverse human viruses. Proc. Natl. Acad. Sci. USA 113, 2241–2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Banerjee S, Goldstein SA, Dong B, Gaughan C, Rath S, Donovan J, Korennykh A, Silverman RH, and Weiss SR (2017). Ribonuclease L mediates the cell-lethal phenotype of double-stranded RNA editing enzyme ADAR1 deficiency in a human cell line. eLife 6, e25687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Love MI, Huber W, and Anders S (2014). Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol 15, 550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubaki NM, Ilinykh P, Pietzsch C, Tigabu B, Freiberg AN, Koup RA, and Bukreyev A (2013). The lack of maturation of Ebola virus-infected dendritic cells results from the cooperative effect of at least two viral domains. J. Virol 87, 7471–7485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthra P, Ramanan P, Mire CE, Weisend C, Tsuda Y, Yen B, Liu G, Leung DW, Geisbert TW, Ebihara H, et al. (2013). Mutual antagonism between the Ebola virus VP35 protein and the RIG-I activator PACT determines infection outcome. Cell Host Microbe 14, 74–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthra P, Aguirre S, Yen BC, Pietzsch CA, Sanchez-Aparicio MT, Tigabu B, Morlock LK, García-Sastre A, Leung DW, Williams NS, et al. (2017). Topoisomerase II inhibitors induce DNA damage-dependent interferon responses circumventing Ebola virus immune evasion. MBio 8, 283e00368–1777530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahanty S, Hutchinson K, Agarwal S, McRae M, Rollin PE, and Pulendran B (2003). Cutting edge: impairment of dendritic cells and adaptive immunity by Ebola and Lassa viruses. J. Immunol 170, 2797–2801. [DOI] [PubMed] [Google Scholar]
- Matassov D, Mire CE, Latham T, Geisbert JB, Xu R, Ota-Setlik A, Agans KN, Kobs DJ, Wendling MQS, Burnaugh A, et al. (2018). Single-dose trivalent VesiculoVax vaccine protects macaques from lethal Ebolavirus and Marburgvirus challenge. J. Virol 92, e01190–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menicucci AR, Versteeg K, Woolsey C, Mire CE, Geisbert JB, Cross RW, Agans KN, Jankeel A, Geisbert TW, and Messaoudi I (2017). Transcriptome analysis of circulating immune cell subsets highlight the role of monocytes in Zaire Ebola virus Makona pathogenesis. Front. Immunol 8, 1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messaoudi I, Amarasinghe GK, and Basler CF (2015). Filovirus pathogenesis and immune evasion: insights from Ebola virus and Marburg virus. Nat. Rev. Microbiol 13, 663–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Research Council (2011). Guide for the Care and Use of Laboratory Animals: Eighth Edition (The National Academies Press; ). [Google Scholar]
- Olejnik J, Hume AJ, Leung DW, Amarasinghe GK, Basler CF, and Mühlberger E (2017). Filovirus Strategies to Escape Antiviral Responses. Curr. Top. Microbiol. Immunol 411, 293–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins KC, Cárdenas WB, and Basler CF (2009). Ebola virus protein VP35 impairs the function of interferon regulatory factor-activating kinases IKKepsilon and TBK-1. J. Virol 83, 3069–3077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins KC, Delpeut S, Leung DW, Reynard O, Volchkova VA, Reid SP, Ramanan P, Cárdenas WB, Amarasinghe GK, Volchkov VE, and Basler CF (2010). Mutations abrogating VP35 interaction with double-stranded RNA render Ebola virus avirulent in guinea pigs. J. Virol 84, 3004–3015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reikine S, Nguyen JB, and Modis Y (2014). Pattern recognition and signaling mechanisms of RIG-I and MDA5. Front. Immunol 5, 342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubins KH, Hensley LE, Wahl-Jensen V, Daddario DiCaprio KM, Young HA, Reed DS, Jahrling PB, Brown PO, Relman DA, and Geisbert TW (2007). The temporal program of peripheral blood gene expression in the response of nonhuman primates to Ebola hemorrhagic fever. Genome Biol. 8, R174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satoh T, Kato H, Kumagai Y, Yoneyama M, Sato S, Matsushita K, Tsujimura T, Fujita T, Akira S, and Takeuchi O (2010). LGP2 is a positive regulator of RIG-I- and MDA5-mediated antiviral responses. Proc. Natl. Acad. Sci. USA 107, 1512–1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St Claire MC, Ragland DR, Bollinger L, and Jahrling PB (2017). Animal models of Ebolavirus infection. Comp. Med 67, 253–262. [PMC free article] [PubMed] [Google Scholar]
- Thi EP, Mire CE, Lee AC, Geisbert JB, Zhou JZ, Agans KN, Snead NM, Deer DJ, Barnard TR, Fenton KA, et al. (2015). Lipid nanoparticle siRNA treatment of Ebola-virus-Makona-infected nonhuman primates. Nature 521, 362–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Versteeg K, Menicucci AR, Woolsey C, Mire CE, Geisbert JB, Cross RW, Agans KN, Jeske D, Messaoudi I, and Geisbert TW (2017). Infection with the Makona variant results in a delayed and distinct host immune response compared to previous Ebola virus variants Sci. Rep 7, 9730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (2019). Ebola virus disease. https://www.who.int/health-topics/ebola/#tab=overview.
- Yen B, Mulder LC, Martinez O, and Basler CF (2014). Molecular basis for ebolavirus VP35 suppression of human dendritic cell maturation. J. Virol 88, 12500–12510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoneyama M, Onomoto K, Jogi M, Akaboshi T, and Fujita T (2015). Viral RNA detection by RIG-I-like receptors. Curr. Opin. Immunol 32, 48–53. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The accession number for the RNA-sequencing data reported in this paper is SRA: PRJNA548965.