Abstract
Objective
The study compared spinal block characteristics of equipotent doses of plain 0.5% levobupivacaine, plain 0.75% ropivacaine and hyperbaric 0.5% bupivacaine for elective caesarean (CS) delivery.
Methods
A total of 100 parturient women undergoing elective CS under spinal anaesthesia were enrolled for the study. The parturients were randomly assigned to receive one of the following in a subarachnoid block: hyperbaric 0.5% bupivacaine 10 mg (group B), plain 0.5% levobupivacaine 10 mg (group L), or plain 0.5% ropivacaine 15 mg (group R).
Results
Motor block duration [groups B, LB, R: 143.78 (30.43) minutes, 139.31 (33.38) minutes, 137.32 (27.39) minutes, respectively; P=0.80], sensory block duration [groups B, LB, R: 122.87 (34.93) minutes, 113.03 (39.24) minutes, 125.58 (24.93) minutes, respectively; p=0.30] and first analgesic request time [groups B, LB, R: 136.87 (28.70) minutes, 133.59 (27.30) minutes, 144.19 (32.09) minutes, respectively; p=0.35] were statistically comparable. The groups were statistically comparable for sensory block onset time [T6 block; groups B, LB, R: 4.62 (2.80) minutes, 4.93 (2.63) minutes, 5.73 (3.00) minutes, respectively; p=0.29] but motor block onset time was statistically prolonged for group R as compared to group B [Bromage 3 block; group B, LB, R: 5.93 (3.41) minutes, 9.00 (4.00) minutes, 10.16 (5.66) minutes, respectively; p=0.001]. No statistically significant differences were seen in sensory and motor block recovery times, haemodynamic parameters or side-effects.
Conclusion
The anaesthesia from a spinal block with 10 mg plain levobupivacaine or 15 mg plain ropivacaine is comparable to the anaesthetic effect of 10 mg hyperbaric bupivacaine in elective caesarean deliveries.
Keywords: Bupivacaine, caesarean delivery, levobupivacaine, ropivacaine, spinal block
Introduction
The clinical application and pharmacology of levobupivacaine and ropivacaine (commercially available as glucose-free plain preparations) support their widespread use in regional anaesthesia practice because they carry a lower risk of cardiotoxicity and neurotoxicity and offer differential block characteristics especially via the epidural route (1, 2). Previous studies on the intrathecal use of glucose-free plain solutions of levobupivacaine and ropivacaine for obstetric anaesthesia have demonstrated faster block recovery and greater haemodynamic stability with a lower incidence of hypotension (3, 4). In spite of these favourable results, hyperbaric bupivacaine is still the more widely used local anaesthetic for spinal anaesthesia in parturients undergoing elective caesarean delivery, due to its rapid onset of action and lower incidence of conversion to general anaesthesia as compared to isobaric bupivacaine (5).
Although spinal block characteristics of three plain local anaesthetics in caesarean deliveries were previously compared in the last decade, the comparative characteristics of these drugs have been re-evaluated since, to elucidate advantages or disadvantages of their use in place of hyperbaric bupivacaine (6, 7). Gunaydin and Tan (8) investigated both plain and hyperbaric preparations of bupivacaine and ropivacaine combined with fentanyl in parturients scheduled for elective caesarean delivery under combined spinal-epidural anaesthesia. They found that plain and hyperbaric ropivacaine with fentanyl provided a shorter motor block with a lower requirement of ephedrine when compared to either plain or hyperbaric bupivacaine. However, the onset time for the sensory block was longer for plain ropivacaine when compared to hyperbaric ropivacaine and bupivacaine with fentanyl. Sundarathiti et al. (9) found that isobaric levobupivacaine (11 mg) with fentanyl provided anaesthesia that was comparable to either isobaric bupivacaine (11 mg) or hyperbaric bupivacaine (10 mg).
The aim of this prospective, double-blind, randomised control trial was to compare the spinal block characteristics of equipotent doses of plain 0.5% levobupivacaine, plain 0.75% ropivacaine and hyperbaric 0.5% bupivacaine in elective caesarean deliveries. The primary outcome of the current study was the difference in the duration of the motor block. Studies have reported a less profound motor block and faster motor block recovery with newer local anaesthetics such as levobupivacaine and ropivacaine (3, 4, 6–8, 10–12). While early recovery from motor block aids in parturient ambulation, an insufficient motor block during surgery can result in inadequate muscle relaxation, parturient discomfort and need for anaesthetic supplementation. The secondary outcomes were sensory and motor block onset and recovery times, sensory block duration, first analgesic request time, maternal haemodynamic parameters, quality of anaesthesia graded by an anaesthesiologist, quality of muscle relaxation graded by a surgeon and side-effects such as hypotension, bradycardia, nausea and vomiting and shivering.
Methods
This study was conducted at a tertiary care teaching hospital, the Employees’ State Insurance Cooperation-Postgraduate Institute of Medical Sciences and Research (ESIC PGIMSR), New Delhi) from February 2015 to February 2016. The Institute’s Ethics Committee approved the study protocol (DMAH-14/19/17/2012-PGIMSR) and the trial was registered at the Central Trial Registry, India (CTRI/2002/18/011711). A total of 100 term parturients with an uncomplicated pregnancy scheduled for elective caesarean delivery were enrolled in this prospective, double-blind, randomised trial after obtaining their written informed consent. The inclusion criteria were ASA status 2 parturients aged 18–40 years with a body weight of 45–85 kg and height of 145–155 cm. Parturients with hypersensitivity to local anaesthetics, contraindications to neuraxial block, twin pregnancy and obstetric complications such as pre-eclampsia, antepartum haemorrhage or foetal compromise were excluded. All parturients were enrolled by a principal investigator after a thorough pre-anaesthetic check. They were then assigned to groups B, LB or R using a computer-generated random numbers list followed by group allotment concealed in sealed envelopes.
After a fasting period of 8 hours for solids and 2 hours for clear liquids, intravenous (i.v.) ranitidine 30 mg and metoclopramide 10 mg were given to the parturients 1 hour prior to surgery. In the operating theatre, the sealed envelope was handed over to the junior resident who attached all the monitors to the parturient (electrocardiogram, pulse oximetry and non-invasive blood pressure) and secured an 18-gauge i.v. access. The parturients’ baseline heart rate (HR), systolic, diastolic and mean blood pressure (SBP, DBP and MBP) and SpO2 (oxygen saturation) were recorded and co-loaded with 10 mL kg−1 of Ringer’s lactate solution within 10 minutes. The drug syringes for the spinal block were prepared by the junior resident as per the group allotted in the sealed envelope, following which the resident was not further involved in the study.
Thereafter, the spinal block and subsequent assessment of the parturient were done by a senior resident who was blinded to the study group. After skin disinfection, spinal block was administered with a 25-gauge Quincke needle in the L3–L4 interspace with the parturient in the left lateral position. Parturients in groups B, LB and R intrathecally received 2 ml of 0.5% hyperbaric bupivacaine, 0.5% isobaric levobupivacaine and 0.75% isobaric ropivacaine (Neon Laboratories Ltd., Mumbai, India), respectively. The parturient was then immediately made supine with a 15-degree left lateral tilt of the table; this stage was noted as time ‘zero’. The haemodynamic parameters were recorded at time ‘zero’, at 2 minutes after the spinal block and thereafter at 5-minute intervals throughout the surgery.
The effectiveness of the sensory block was assessed using pain sensation by pricking with a hypodermic needle and the motor block was assessed using the Bromage scale (B0=no motor loss, B1=inability to flex the hip, B2=inability to flex the knee and B3=inability to flex the ankle) (13). The sensory and motor blocks were evaluated at 2-minute intervals for the initial 14 minutes. The onset times of sensory block to T10, T8, T6 dermatomes and motor block to B1, B2 and B3 were noted. The maximum sensory and motor blocks at 15 minutes were recorded. The senior resident signalled to the surgeons to start the surgery after a sensory block of T6 dermatome and a motor block of B2 were reached.
Thereafter, during surgery and in the postoperative period, the blocks were assessed for regression at 15-minute intervals. The regression times of sensory block to T10 and L1 dermatomes and motor block to B2, B1 and B0 were noted. The durations of motor block (regression time to B1 minus onset time to B2) and sensory block were also calculated for each parturient (regression time to T10 minus onset time to T6). However, if the sensory block of T6 dermatome or motor block of B2 was not achieved at 15 minutes, the parturient was given general anaesthesia. This was recorded as a failure of the block and the parturient was excluded from the study.
During the surgery, Ringer’s lactate solution was infused at 20 mL kg−1 hour−1. After the delivery, oxytocin 10 IU diluted in 100 ml normal saline was infused slowly over 30 minutes. The occurrence of hypotension (decline in MAP<20% from baseline, SBP<90 mm or MAP<50 mmHg) was noted during surgery and was treated with 5 mg intravenous (i.v.) boluses of ephedrine and an additional i.v. fluid bolus (Ringer’s lactate 5 mL kg−1 over 5 minutes). Maternal bradycardia (HR<50 beats min−1) was treated with i.v. atropine 0.6 mg and nausea/vomiting with i.v. ondansetron 4 mg. Parturients who complained of intra-operative pain (visual analogue scale [VAS]>3) were given i.v. fentanyl 2 mcg kg−1 for analgesia. At the end of the surgery, the anaesthesiologist again confirmed if the parturient had felt any pain or discomfort during the surgery and graded the quality of anaesthesia on the following scale: grade 4=Excellent (no parturient pain or discomfort), grade 3=Good (mild pain or discomfort not requiring fentanyl), grade 2=Fair (moderate pain or discomfort requiring fentanyl for analgesia) and grade 1=Poor (intolerable pain and need for supplementation with additional anaesthetic drugs, e.g. ketamine or propofol). The surgeon graded the quality of muscle relaxation as; Excellent (no abdominal strain), Satisfactory (acceptable abdominal strain), or Poor (unacceptable abdominal strain).
On completion of the surgery, parturients was transferred to the recovery room and were followed up every 15 minutes for pain and recovery of sensory and motor blocks. The pain score was recorded on a 10 cm VAS 0=no pain and VAS 10=severe pain). For a VAS score of 3 or more, the parturient was administered paracetamol 1 gm i.v. (Perfalgan 10 mg mL−1, Bristol-Myers Squibb Ltd., India), which was recorded as the first analgesic request time since time ‘zero’. If any parturient had a VAS score of 5 or more or requested additional analgesia after paracetamol infusion, fentanyl 2 mcg kg−1 i.v. was administered. All parturients were also followed on postoperative days 1 and 3 in the ward and asked about any complaints of headache, backache or tingling or numbness in the lower limbs.
Statistical analysis
The null hypothesis of the study was that motor block duration provided by intrathecal plain 10 mg levobupivacaine or plain 15 mg ropivacaine for caesarean delivery was not equivalent to the motor block duration provided by 10 mg hyperbaric bupivacaine. If the null hypothesis was rejected by the statistical test (p<0.05), an alternative hypothesis would be true, which indicated that intrathecal plain 10 mg levobupivacaine or plain 15 mg ropivacaine was able to provide a motor block of the same duration as 10 mg hyperbaric bupivacaine in caesarean deliveries.
Statistical analysis was performed using Statistical Package for the Social Sciences software 17.0 for Windows (SPSS Inc.; Chicago, IL, USA). To detect a difference of 0.8 SD (standard deviation) units between the mean duration of motor block among the study groups, it was calculated that 29 patients per group were required for the study to have a power of 85% and type I error of 0.05, using a confidence interval of 95% (14). We enrolled 100 parturients to compensate for dropouts during the study period.
Continuous variables are presented as mean±SD and categorical variables are presented as absolute numbers and percentages. Data were checked for normality using the Shapiro-Wilk test before statistical analysis. Normally distributed continuous variables (including age, weight, height, onset and regression time, duration of the block and haemodynamic parameters) were compared using one-way analysis of variance (ANOVA). Haemodynamic parameters over time within the groups were analysed using repeated-measure ANOVA. For comparison of categorical variables (adverse events), the Pearson’s chi-square test was used, whereas the Kruskal-Wallis test was used for comparison of quality of anaesthesia and muscle relaxation. For all statistical tests, a p-value of less than 0.05 was considered as a significant difference.
Results
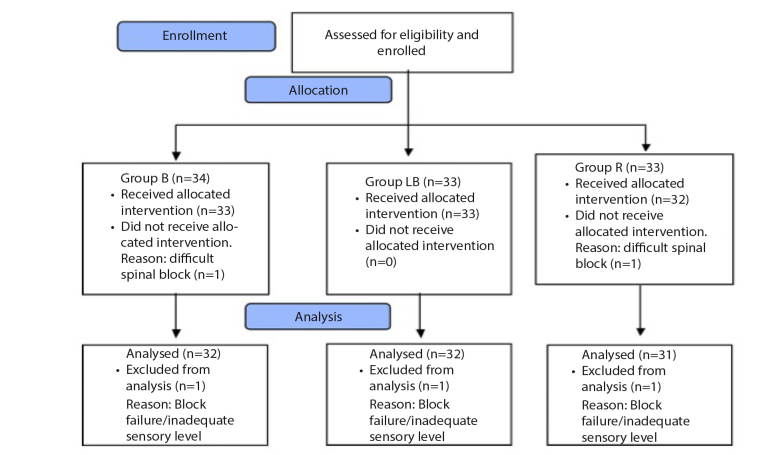
The details of recruitment of the subjects are shown in a CONSORT diagram (Figure 1). Out of 100 parturients enrolled for the study, 5 were excluded during the course of the study, 3 due to failure of the block (1 in each of the groups due to inadequate sensory level) and 2 due to technical difficulty in performing spinal block (1 in Group B and R), who were given general anaesthesia for caesarean delivery. A total of 54 parturients were nulliparous, 28 were para 1 and 13 were para 2 and above. Eighteen parturients had previously undergone 1 caesarean delivery and 4 parturients had previously undergone 2 caesarean deliveries. Table 1 shows the demographic profile, total surgical time and spinal to skin incision time (I) for the three groups, which were these were all statistically comparable. Skin incision to delivery time (D) was under 120 seconds for all cases.
Figure 1.
CONSORT Flow diagram
Table 1.
Demographic profile and surgical data
| Group B (n=32) | Group LB (n=32) | Group R (n=31) | |
|---|---|---|---|
|
| |||
| Age (years) | 25.65 (3.42) | 25.46 (4.16) | 26.77 (3.53) |
| Weight (kg) | 59.53 (5.61) | 57.28 (5.13) | 58.09 (6.06) |
| Height (cm) | 150.34 (4.74) | 150.50 (3.37) | 150.80 (3.64) |
| Total Surgical time (minutes) | 45.34 (7.40) | 47.81 (6.59) | 44.35 (7.04) |
| Spinal to skin incision time (minutes) | 6.55 (1.24) | 6.63 (1.52) | 6.74 (1.36) |
Values are represented as mean (SD).
The motor block duration (primary outcome) was statistically comparable for the 3 groups [group B=143.78 (30.43) minutes, group LB=139.31 (33.38) minutes, group R=137.32 (27.39) minutes, p=0.80]. No statistically significant difference was seen in the sensory block onset times to T10, T8 and T6 dermatomes between the groups. Statistically, a significant difference was observed in the motor block onset times to B2 and B3; a post-hoc analysis showed that the difference was statistically significant between groups B and R (Table 2). The maximum sensory and motor blocks level achieved at 15 minutes were T4 (T2–T6) and B3 respectively in all three groups, respectively. The sensory block regression times to T10 and L1 dermatomes and motor block regression times to B2, B1 and B0 were statistically comparable for the three groups (Table 3). Sensory block duration [group B=122.87 (34.93) minutes, group LB=113.03 (39.24) minutes, group R=125.58 (24.93) minutes, p=0.30] and first analgesic request time [group B=136.87 (28.70) minutes, group LB=133.59 (27.30) minutes, group R=144.19 (32.09) minutes, p=0.35] were also statistically comparable.
Table 2.
Sensory and Motor Block Onset Times
| Onset Times (minutes) | Group B (n=32) | Group LB (n=32) | Group R (n=31) | p |
|---|---|---|---|---|
|
| ||||
| Sensory onset to T10 | 2.34 (1.09) | 2.50 (1.13) | 2.38 (1.08) | 0.84 |
| Sensory onset to T8 | 3.12 (1.89) | 3.12 (1.75) | 3.54 (2.40) | 0.64 |
| Sensory onset to T6 | 4.62 (2.80) | 4.93 (2.63) | 5.73 (3.00) | 0.29 |
| Motor onset to B1 | 1.89 (0.32) | 2.15 (0.67) | 2.20 (0.62) | 0.16 |
| Motor onset to B2 | 2.93 (1.34) | 3.81 (1.17) | 4.45 (2.61) | 0.005* |
| Motor onset to B3 | 5.93 (3.41) | 9.00 (4.00) | 10.16 (5.66) | 0.001† |
Values are represented as mean (SD). Post-hoc analysis showed statistically significant difference between groups B and R (*p=0.005, †p=0.001) with no statistical difference between groups B and LB or groups LB and R.
Table 3.
Sensory and motor block regression times
| Regression Times (mins) | Group B (n=32) | Group LB (n=32) | Group R (n=31) | p |
|---|---|---|---|---|
|
| ||||
| Sensory two Segment Regression | 102.18 (29.12) | 91.40 (33.94) | 95.80 (21.45) | 0.32 |
| Sensory Regression to T10 | 127.50 (33.86) | 117.50 (38.30) | 131.12 (25.38) | 0.27 |
| Sensory Regression to L1 | 151.40 (33.94) | 152.81 (36.43) | 156.77 (25.93) | 0.80 |
| Motor Regression to B2 | 115.31 (25.11) | 106.40 (26.71) | 107.25 (20.92) | 0.50 |
| Motor Regression to B1 | 146.71 (30.89) | 143.12 (33.89) | 141.77 (26.78) | 0.87 |
| Motor Regression to B0 | 179.06 (35.11) | 178.12 (32.48) | 174.19 (29.15) | 0.88 |
Values are represented as mean (SD).
Figure 2 shows the quality of anaesthesia scores that were statistically comparable in all the groups (p=0.98). The quality of muscle relaxation was ‘Excellent’ for parturients of all three groups except for 1 parturient in group B, 3 parturients in group LB and 2 parturients in group R, for whom it was ‘Good’ (p=0.59). Haemodynamic parameters HR, SBP, DBP and MBP were statistically comparable at various points of time between the groups (Figures 3–6). Table 4 shows the occurrence of intraoperative adverse events; these were statistically comparable. Atropine 0.6 mg i.v. was used for treating bradycardia in each of the six parturients and ondansetron 4 mg was used for treating nausea and vomiting in 2 parturients. The median number of bolus injections of ephedrine 5 mg used for treating hypotension in parturients in all the three groups was 1 (1–2). Postoperatively, 14 parturients (group B=4, group LB=5, group R=5) required fentanyl in addition to paracetamol infusion for pain relief. The parturients were followed up on days 1 and 3; there was no incidence of headache, backache or tingling or numbness in the lower limbs in any parturient of any group.
Figure 2.
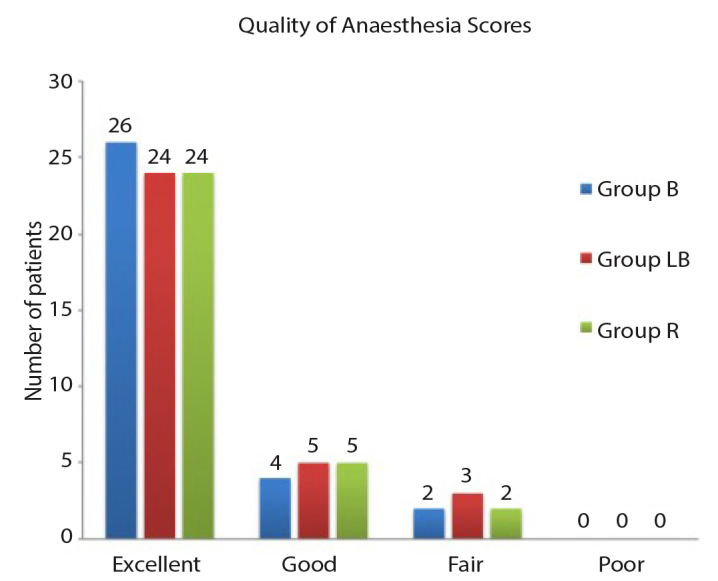
The quality of anaesthesia scores was statistically comparable for the three groups (p-value=0.98)
Figure 3.
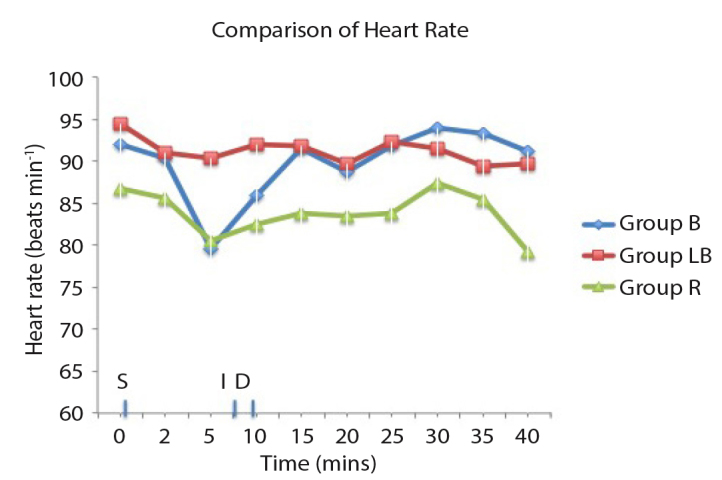
No statistically significant difference was seen in the between-group or within-group comparison of heart rate
S: time of giving spinal block; I: skin incision; D:baby delivery
Figure 4.
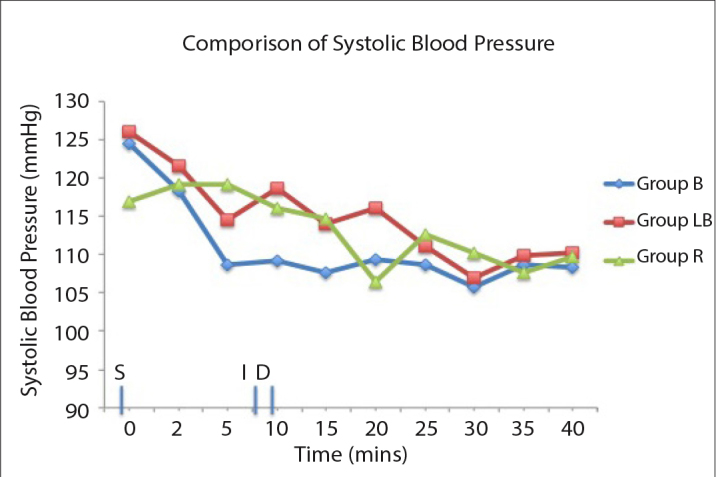
No statistically significant difference was seen in the between-group or within-group comparison of systolic blood pressure
S: time of giving spinal block; I: skin incision; D: baby delivery
Figure 5.
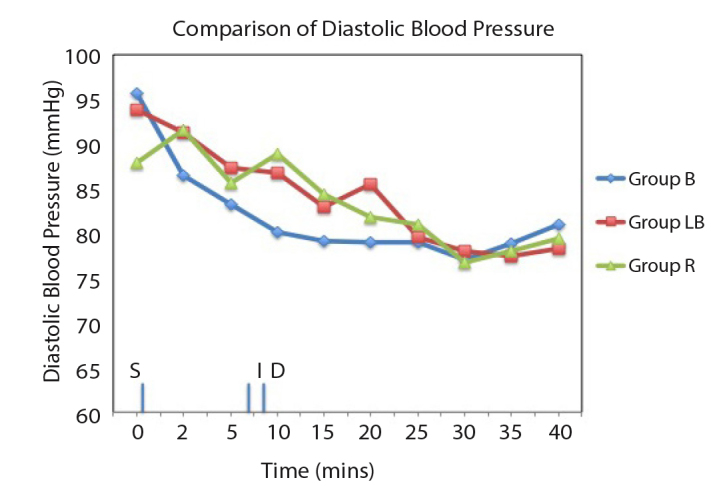
No statistically significant difference was seen in the between-group or within-group comparison of diastolic blood pressure
S: time of giving spinal block; I: skin incision; D: baby delivery
Figure 6.
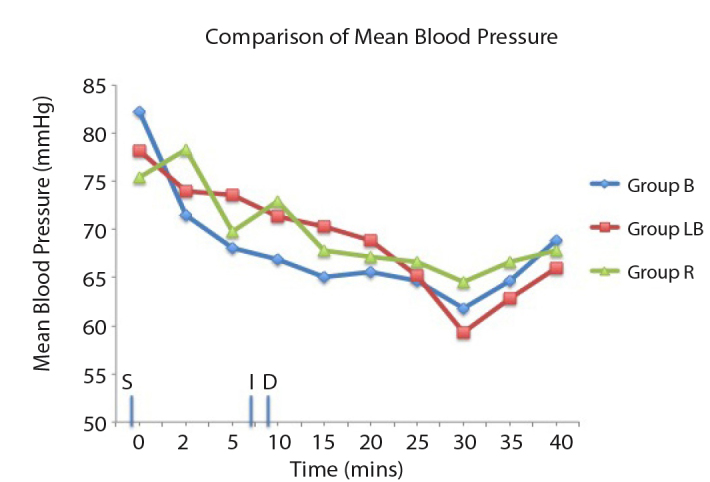
No statistically significant difference was seen in the between-group or within-group comparison of mean blood pressure
S: time of giving spinal block; I: skin incision; D: baby delivery
Table 4.
Adverse events occurring in the subjects
| Group B (n=32) | Group LB (n=32) | Group R (n=31) | p | |
|---|---|---|---|---|
|
| ||||
| Hypotension | 8 (25%) | 9 (28%) | 2 (6.5%) | 0.07 |
| Bradycardia | 2 (6.3%) | 2 (6.3%) | 2 (6.5%) | 0.99 |
| Nausea and Vomiting | - | 2 (6.3%) | - | - |
| Shivering | 3 (9.4%) | 2 (6.3%) | - | 0.24 |
Values are represented as the number of parturients (%).
Discussion
This study compared spinal block characteristics of equipotent doses of hyperbaric 0.5% bupivacaine, plain 0.5% levobupivacaine and plain 0.75% ropivacaine for elective caesarean delivery. The study was adequately powered, as the primary outcome (motor block duration) was statistically comparable for the three groups, the null hypothesis stood rejected, and the alternative hypothesis was validated. The motor block onset time to B2 and B3 was statistically prolonged in group R compared to group B, which is significant in emergency caesarean delivery as it can delay surgical incision. The other spinal block parameters including sensory block onset time, sensory block duration and regression times of sensory and motor blocks were comparable for the groups.
Previous studies have found levobupivacaine and bupivacaine to be almost equipotent and ropivacaine to be 0.4 to 0.7 times less potent than bupivacaine and levobupivacaine for intrathecal anaesthesia. Lee et al. (15) obtained the ED50 values for bupivacaine, levobupivacaine and ropivacaine as 5.50 mg, 5.68 mg and 8.41 mg respectively for intrathecal anaesthesia in lower limb surgeries. The relative anaesthetic potency ratios were 0.97 for levobupivacaine/bupivacaine, 0.65 for ropivacaine/bupivacaine and 0.68 for ropivacaine/levobupivacaine. Parpaglioni et al. (16) determined the ED50 dose of levobupivacaine and ropivacaine as 10.58 mg and 14.22 mg respectively using Dixon and Massey formula, and 10.14 mg and 13.46 mg respectively using logical regression for intrathecal anaesthesia in caesarean delivery. The estimated potency ratio for spinal levobupivacaine/ropivacaine was 1.34. The estimated ED95 doses for levobupivacaine and ropivacaine were 12.56 mg and 15.97 mg respectively, which were lower than the doses previously estimated by Kwaw et al. (13.5 mg and 27 mg for levobupivacaine and ropivacaine, respectively) (17, 18).
Glaser et al. (19) and Fattorini et al. (20) compared intrathecal levobupivacaine and bupivacaine in 1:1 dose ratio for orthopaedic surgeries and found these to have similar anaesthetic effects. Malinovsky et al. (21) and Erturk et al. (22) studied intrathecal ropivacaine and bupivacaine in a dose ratio of 3: 2 for urological and orthopaedic surgeries respectively and found these to provide comparable anaesthesia. Gautier et al. (6) observed that 8 mg bupivacaine, 8 mg levobupivacaine and 12 mg ropivacaine with 2.5 mcg sufentanil provided equivalent sensory and motor anaesthesia in spinal block for caesarean deliveries. For this study, we chose intrathecal doses of bupivacaine, levobupivacaine and ropivacaine based on the pilot cases we had treated at the start of the study and considered an estimated potency ratio of 3:2 between bupivacaine/ropivacaine and levobupivacaine/ropivacaine as described in the above studies.
The drug baricity and parturients’ position while performing the spinal block can influence the intrathecal spread of the local anaesthetic. On measuring the densities, plain 0.5% ropivacaine is slightly hypobaric and plain 0.75% levobupivacaine is isobaric to CSF (cerebrospinal fluid) (23). Also, the density of CSF in pregnant women is slightly lower than the density in men and non-pregnant women (24). Hallworth et al. (25) compared hyperbaric, isobaric and hypobaric bupivacaine for elective caesarean delivery and found that when spinal block was performed in the lateral position, drug baricity did not affect the level of the sensory block. In the sitting position, the sensory block level was one dermatomal level higher with hypobaric solution than with hyperbaric solution. For an isobaric drug like levobupivacaine, positioning had no influence on the sensory block level achieved (26). In all parturients, SAB was given in lateral position, followed by supine positioning with a wedge. Therefore, the difference in the baricities of local anaesthetic drugs used ideally should not have led to any difference in sensory block levels.
This study shows that plain levobupivacaine and ropivacaine are suitable alternatives to hyperbaric bupivacaine for elective caesarean delivery. A few studies have explored the clinical utility of isobaric levobupivacaine and ropivacaine for intrathecal anaesthesia for caesarean delivery, however, their results vary with regard to block characteristics, which could be due to difference in the doses of drugs and adjuvants and variations in the regional anaesthesia technique. Although in most of these studies opioids have been added as adjuvants to intrathecal drugs to improve the quality of spinal block, this was not done in the present study because the objective was to explore the characteristics of spinal block of the newer local anaesthetics when used as sole anaesthetics. Gunusen et al. (27) compared three different doses of intrathecal levobupivacaine (5 mg, 7.5 mg and 10 mg) with fentanyl and concluded that levobupivacaine 7.5 mg with fentanyl 15 mcg was most appropriate for elective caesarean delivery. Wong et al. (28) recommended isobaric 0.75% ropivacaine in doses of 18.75 mg or 22.5 mg, whereas Ateser et al. (29) suggested 15 mg or 20 mg of isobaric 1% ropivacaine for SAB in caesarean delivery. Eryilmaz and Gunaydin (10) studied plain 15 mg ropivacaine and plain 10 mg bupivacaine with 25 mcg fentanyl in spinal block and found a longer sensory block and a shorter motor block in the ropivacaine group.
For elective caesarean delivery, Camorcia et al. (30) reported relative motor block potencies for bupivacaine, levobupivacaine and ropivacaine as high (ED50-3.44 mg), intermediate (ED-4.83 mg) and low (ED-5.79 mg) respectively, when used for intrathecal anaesthesia in caesarean delivery. Also, the concentration of intrathecal drug injected has a significant effect on motor block; this has been seen for both levobupivacaine and ropivacaine where increasing concentration resulted in a more intense motor block and decreasing concentration led to a higher dose being required to achieve the same motor block (31, 32). The use of local anaesthetics along with low dose with opioids has been studied for elective caesarean delivery using the CSE technique; while Coppejans et al. (7) found a less intense motor block, Gautier et al. (6) reported a shorter motor block with levobupivacaine and ropivacaine as compared to bupivacaine. In the above studies, the need for increased epidural supplementation was also seen, which could be due to the use of submaximal drug doses. The present study has shown that a dose of 10 mg plain levobupivacaine or 15 mg plain ropivacaine is as effective as 10 mg hyperbaric bupivacaine, both in terms of the duration and intensity (i.e. Bromage 3) of the motor block.
The incidence of hypotension was much lower in group R (6.5%) as compared to groups LB (28%) and B (25%), though the difference was not proved to be statistically significant. Therefore, further studies are needed to confirm the haemodynamic effects of ropivacaine. One possible explanation for greater haemodynamic stability could be the slower onset of the block with plain ropivacaine. Ogun et al. (3) found a lower requirement for ephedrine during caesarean deliveries with ropivacaine than with bupivacaine. Two previous studies reported better haemodynamics and lesser hypotension with intrathecal ropivacaine as compared to bupivacaine for orthopaedic and lower extremity surgeries (28, 33).
The dose of intrathecal drugs used in this study is similar to the dose used by Gautier et al. (6) but is lower than what has been used by most other researchers. This is because of the shorter average height of women in the Indian subcontinent (5 feet or 150 cm) as compared to western countries (34). Harten et al. (35) studied the height- and weight-adjusted doses of local anaesthetics for spinal anaesthesia in elective caesarean delivery. For a similar average patient height (150 cm) and weight (60 kg) as in this study, Harten et al. (35) used a dose of 1.7 mL of 0.5% hyperbaric bupivacaine with 0.4 mcg morphine. As we did not use an opioid, we chose a higher dose of 2 mL of 0.5% hyperbaric bupivacaine or an equipotent dose of plain 0.5% levobupivacaine and plain 0.75% ropivacaine in this study.
The study has a few limitations. Blood pressure was measured at the initial 2 minutes after the spinal block and thereafter at 5-minute intervals, therefore, it is possible that episodes of mild hypotension were missed. Hypotension episodes are often preceded by complaints such as dizziness or nausea and vomiting, which were seen only in two parturients in this study. Phenylephrine is the preferred drug for the treatment of hypotension in caesarean delivery, however, ephedrine was used due to the non-availability of phenylephrine in the hospital pharmacy store. Although an intrathecal opioid was not used, the parturients’ pain during the surgery and in the postoperative period was adequately managed with i.v. fentanyl. The postoperative analgesic regime comprised multimodal analgesia with paracetamol infusion and i.v. fentanyl, which reduced the pain to a tolerable level (VAS<3) and enabled parturients to successfully breastfeed their infants.
The failure rate of spinal anaesthesia in the study was 5%, which is higher than what is recommended for elective caesarean delivery. The possible cause for this could be that all spinal blocks were performed by resident anaesthesiologists. The omission of an opioid adjuvant along with the intrathecal drug could be another reason. In an audit on failed spinal blocks, a higher failure rate of the block was seen if intrathecal opioid was omitted (36). We excluded all cases of pre-operative failure of the spinal block from the final analysis. However, there were no cases of intraoperative failure of spinal anaesthesia or a need for conversion to general anaesthesia during the surgery.
The results of this study can be applied to parturients with a height of 145–155 cm, which was the inclusion criterion for the study. Also, we can infer that as an alternative to hyperbaric 0.5% bupivacaine, an equipotent dose of plain 0.5% levobupivacaine or plain 0.75% ropivacaine can be used effectively in the spinal block for caesarean delivery. However, in clinical application, it is common practice to add an opioid adjuvant to the intrathecal drug, therefore, we would like to evaluate the use of levobupivacaine and ropivacaine with an opioid in a spinal block for caesarean delivery in the future.
Conclusion
This study shows that for parturients with a height of 145–155 cm, plain 0.5% levobupivacaine (10 mg) or 0.75% ropivacaine (15 mg) can provide anaesthesia comparable to that of hyperbaric 0.5% bupivacaine (10 mg) when used in a spinal block in elective caesarean delivery. The only difference observed between the spinal block characteristics was a prolonged motor block onset time with ropivacaine. The haemodynamic parameters and side-effects were comparable for the three local anaesthetics.
Acknowledgements
I would like to thank Assistant Professor Dr. Unati Asthana, senior residents Dr. Harpriya Shergill and Dr. Sweta Singh and junior residents Dr. Beenu Kumari and Dr. Priyanka Aggarwal from the Department of Anaesthesiology, ESIC PGIMSR, New Delhi for their help in conducting cases and collecting data for the study. I would also like to thank Dr. Ravi Rohilla (Assistant Professor, Department of Community Medicine, Government Medical College and Hospital, Chandigarh, India) for his help in performing the statistical analysis of the study.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Employees’ State Insurance Cooperation Postgraduate Institute of Medical Sciences and Research (DMAH-14/19/17/2012-PGIMSR).
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Conflict of Interest: The author have no conflicts of interest to declare.
Financial Disclosure: This work was entirely supported by the Department of Anaesthesia, ESIC PGIMSR, New Delhi, India.
References
- 1.Stienstra R. Clinical application of ropivacaine in obstetrics. Curr Top Med Chem. 2001;1:215–8. doi: 10.2174/1568026013395218. [DOI] [PubMed] [Google Scholar]
- 2.Foster RH, Markham A. Levobupivacaine: a review of its pharmacology and use as a local anaesthetic. Drugs. 2000;9:551–79. doi: 10.2165/00003495-200059030-00013. [DOI] [PubMed] [Google Scholar]
- 3.Ogun CO, Kirgiz EN, Duman A, Okesli S, Akyurek C. Comparison of intrathecal isobaric bupivacaine-morphine and ropivacaine-morphine for caesarean delivery. Br J Anaesth. 2003;90:659–64. doi: 10.1093/bja/aeg123. [DOI] [PubMed] [Google Scholar]
- 4.Danelli G, Fanelli G, Berti M, Cornini A, Lacava L, Fanelli A. Spinal ropivacaine or bupivacaine for caesarean delivery: a prospective, randomized, double-blind comparison. Reg Anesth Pain Med. 2004;29:221–6. doi: 10.1016/j.rapm.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 5.Sia AT, Tan KH, Sng BL, Lim Y, Chan ES, Siddiqui FJ. Use of hyperbaric versus isobaric bupivacaine for spinal anaesthesia for caesarean section. Cochrane Database Syst Rev. 2013;5:CD005143. doi: 10.1002/14651858.CD005143.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Gautier P, De Kock M, Huberty L, Demir T, Izydorczic M, Vanderick B. Comparison of the effects of intrathecal ropivacaine, levobupivacaine, and bupivacaine for Caesarean section. Br J Anaesth. 2003;91:684–9. doi: 10.1093/bja/aeg251. [DOI] [PubMed] [Google Scholar]
- 7.Coppejans HC, Vercauteren MP. Low-dose combined spinal-epidural anesthesia for caesarean delivery: a comparison of three plain local anesthetics. Acta Anaesthesiol Belg. 2006;57:39–43. [PubMed] [Google Scholar]
- 8.Gunaydin B, Tan ED. Intrathecal hyperbaric or isobaric bupivacaine and ropivacaine with fentanyl for elective caesarean section. J Matern Fetal Neonatal Med. 2010;23:1481–6. doi: 10.3109/14767051003678051. [DOI] [PubMed] [Google Scholar]
- 9.Sundarathiti P, Sangdee N, Sangasilpa I, Prayoonhong W, Papoun S. Comparison of intrathecal bupivacaine, levobupivacaine for caesarean section. J Med Assoc Thai. 2014;97:710–6. [PubMed] [Google Scholar]
- 10.Eryilmaz NC, Gunaydin B. A comparison of the effects of intrathecal ropivacaine and bupivacaine during cesarean section. Turk J Med Sci. 2011;41:219–26. [Google Scholar]
- 11.Misirlioglu K, Sivrikaya G, Hanci A, Yalcinkaya A. Intrathecal low-dose levobupivacaine and bupivacaine combined with fentanyl in a randomised controlled study for caesarean section: blockade characteristics, maternal and neonatal effects. Hippokratia. 2013;17:262–7. [PMC free article] [PubMed] [Google Scholar]
- 12.Malhotra R, Johnstone C, Halpern S, Hunter J, Banerjee A. Duration of motor block with intrathecal ropivacaine versus bupivacaine for caesarean section: a meta-analysis. Int J Obstet Anesth. 2016;27:9–16. doi: 10.1016/j.ijoa.2016.03.004. [DOI] [PubMed] [Google Scholar]
- 13.Graham AC, McClure JH. Quantitative assessment of motor block in labouring women receiving epidural analgesia. Anaesthesia. 2001;56:470–6. doi: 10.1046/j.1365-2044.2001.01524-6.x. [DOI] [PubMed] [Google Scholar]
- 14.Cohen J. The t test for means. In: Cohen J, editor. Statistical Power Analysis for the Behavioural Sciences. 2nd ed. United States of America; Laurence Eribaum Associates; 1988. pp. 19–74. [DOI] [Google Scholar]
- 15.Lee YY, Ngan Kee WD, Fong SY, Liu JT, Gin T. The median effective dose of bupivacaine, levobupivacaine, and ropivacaine after intrathecal injection in lower limb surgery. Anesth Analg. 2009;109:1331–4. doi: 10.1213/ane.0b013e3181b1912b. [DOI] [PubMed] [Google Scholar]
- 16.Parpaglioni R, Frigo MG, Lemma A, Sebastiani M, Barbati G, Celleno D. Minimum local anaesthetic dose (MLAD) of intrathecal levobupivacaine and ropivacaine for Caesarean section. Anaesthesia. 2006;61:110–5. doi: 10.1111/j.1365-2044.2005.04380.x. [DOI] [PubMed] [Google Scholar]
- 17.Khaw KS, Ngan Kee WD, Wong ELY, Liu JYW, Chung R. Spinal ropivacaine for caesarean section. Anesthesiology. 2001;95:1346–50. doi: 10.1097/00000542-200112000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Khaw K, Ngan Kee WD, Ng F, Leung P. Dose-finding comparison of spinal levobupivacaine and bupivacaine for caesarean section. Int J Obstet Anesth. 2004;13:S17. [Google Scholar]
- 19.Glaser C, Marhofer P, Zimpfer G, Heinz MT, Sitzwohl C, Kapral S, et al. Levobupivacaine versus racemic bupivacaine for spinal anesthesia. Anesth Analg. 2002;94:194–8. doi: 10.1097/00000539-200201000-00037. [DOI] [PubMed] [Google Scholar]
- 20.Fattorini F, Ricci Z, Rocco A, Romano R, Pascarella MA, Pinto G. Levobupivacaine versus racemic bupivacaine for spinal anaesthesia in orthopaedic major surgery. Minerva Anestesiol. 2006;72:637–44. [PubMed] [Google Scholar]
- 21.Malinovsky JM, Charles F, Kick O, Lepage JY, Malinge M, Cozian A, et al. Intrathecal anesthesia: ropivacaine versus bupivacaine. Anesth Analg. 2000;91:1457–60. doi: 10.1097/00000539-200012000-00030. [DOI] [PubMed] [Google Scholar]
- 22.Erturk E, Tutuncu C, Eroglu A, Gokben M. Clinical comparison of 12 mg ropivacaine and 8 mg bupivacaine, both with 20 microg fentanyl, in spinal anaesthesia for major orthopaedic surgery in geriatric parturients. Med Princ Pract. 2010;19:142–7. doi: 10.1159/000249581. [DOI] [PubMed] [Google Scholar]
- 23.McLeod GA. Density of spinal anaesthetic solutions of bupivacaine, levobupivacaine, and ropivacaine with and without dextrose. Br J Anaesth. 2004;92:547–51. doi: 10.1093/bja/aeh094. [DOI] [PubMed] [Google Scholar]
- 24.Lui AC, Polis TZ, Cicutti NJ. Densities of cerebrospinal fluid and spinal anaesthetic solutions in surgical parturients at body temperature. Can J Anaesth. 1998;45:297–303. doi: 10.1007/BF03012018. [DOI] [PubMed] [Google Scholar]
- 25.Hallworth SP, Fernando R, Columb MO, Stocks GM. The effect of posture and baricity on the spread of intrathecal bupivacaine for elective caesarean delivery. Anesth Analg. 2005;100:1159–65. doi: 10.1213/01.ANE.0000149548.88029.A2. [DOI] [PubMed] [Google Scholar]
- 26.Gori F, Corradetti F, Cerotto V, Peduto VA. Influence of Positioning on Plain Levobupivacaine Spinal Anesthesia in Caesarean Section. Anesthesiol Res Pract. 2010 doi: 10.1155/2010/212696. 212696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gunusen I, Karaman S, Sargin A, Firat V. A randomized comparison of different doses of intrathecal levobupivacaine combined with fentanyl for elective caesarean section: prospective, double-blinded study. J Anesth. 2011;25:205–12. doi: 10.1007/s00540-011-1097-4. [DOI] [PubMed] [Google Scholar]
- 28.Wong JO, Tan TD, Leung PO, Tseng KF, Cheu NW. Spinal anesthesia with two different dosages of 0.75% glucose-free ropivacaine: a comparison of efficacy and safety in Chinese parturients undergoing caesarean section. Acta Anaesthesiologica Singapore. 2003;41:131–8. [PubMed] [Google Scholar]
- 29.Ateser RY, Kayacan N. Intrathecal ropivacaine in caesarean delivery. Niger J Clin Pract. 2017;20:1322–7. doi: 10.4103/1119-3077.219520. [DOI] [PubMed] [Google Scholar]
- 30.Camorcia M, Capogna G, Berritta C, Columb MO. The relative potencies for motor block after intrathecal ropivacaine, levobupivacaine, and bupivacaine. Anesth Analg. 2007;104:904–7. doi: 10.1213/01.ane.0000256912.54023.79. [DOI] [PubMed] [Google Scholar]
- 31.Camorcia M, Capogna G, Lyons G, Columb MO. The relative motor blocking potencies of intrathecal ropivacaine: Effects of concentration. Anesth Analg. 2004;98:1779–82. doi: 10.1213/01.ANE.0000117147.56528.33. [DOI] [PubMed] [Google Scholar]
- 32.Celleno D, Parpaglioni R, Frigo MG, Barbati G. Intrathecal levobupivacaine and ropivacaine for caesarean section. New perspectives. Minerva Anestesiol. 2005;71:521–5. [PubMed] [Google Scholar]
- 33.Kallio H, Snall EV, Kero MP, Rosenberg PH. A comparison of intrathecal plain solutions containing ropivacaine 20 or 15 mg versus bupivacaine 10 mg. Anesth Analg. 2004;99:713–7. doi: 10.1213/01.ANE.0000129976.26455.32. [DOI] [PubMed] [Google Scholar]
- 34.List of average human height worldwide - Wikipedia. [Accessed June 22, 2018]. Available at: https://en.wikipedia.org/wiki/List_of_average_human_height_worldwide.
- 35.Harten JM, Boyne I, Hannah P, Varveris D, Brown A. Effects of a height and weight adjusted dose of local anaesthetic for spinal anaesthesia for elective Caesarean section. Anaesthesia. 2005;60:348–53. doi: 10.1111/j.1365-2044.2005.04113.x. [DOI] [PubMed] [Google Scholar]
- 36.Kinsella SM. A prospective audit of regional anaesthesia failure in 5080 Caesarean sections. Anaesthesia. 2008;63:822–32. doi: 10.1111/j.1365-2044.2008.05499.x. [DOI] [PubMed] [Google Scholar]