Abstract
Introduction
Little is known about the applicability of mindfulness-based interventions in Spanish adults with overweight/obesity. The objective of the present study protocol is to describe the methods that will be used in a cluster randomised trial (CRT) that aims to evaluate the effectiveness of a mindfulness eating (ME) programme to reduce emotional eating (EE) in adults with overweight/obesity in primary care (PC) settings.
Methods and analysis
A CRT will be conducted with approximately 76 adults with overweight/obesity from four PC health centres (clusters) in the city of Zaragoza, Spain. Health centres matched to the average per capita income of the assigned population will be randomly allocated into two groups: ‘ME +treatment as usual (TAU)’ and ‘TAU alone’. The ME programme will be composed of seven sessions delivered by a clinical psychologist, and TAU will be offered by general practitioners. The primary outcome will be EE measured by the Dutch Eating Behaviour Questionnaire (DEBQ) at post test as primary endpoint. Other outcomes will be external and restrained eating (DEBQ), binge eating (Bulimic Investigatory Test Edinburgh), eating disorder (Eating Attitude Test), anxiety (General Anxiety Disorder-7), depression (Patient Health Questionnaire-9), mindful eating (Mindful Eating Scale), dispositional mindfulness (Five Facet Mindfulness Questionnaire) and self-compassion (Self-Compassion Scale). Anthropometric measures, vital signs and blood tests will be taken. A primary intention-to-treat analysis on EE will be conducted using linear mixed models. Supplementary analyses will include secondary outcomes and 1-year follow-up measures; adjusted models controlling for sex, weight status and levels of anxiety and depression; the complier average causal effect of treatment; and the clinical significance of improvements.
Ethics and dissemination
Positive results of this study may have a significant impact on one of the most important current health-related problems. Approval was obtained from the Ethics Committee of the Regional Authority. The results will be submitted to peer-reviewed journals, and reports will be sent to participants.
Trial registration number
NCT03927534 (5/2019).
Keywords: CRT, primary care, mindfulness, mindful eating, overweight, obesity
Strengths and limitations of this study.
This study is going to lead the first intervention based on mindful eating applied to overweight and obesity in the Spanish primary care (PC) context.
It will open new perspectives about current recommendations included in the clinical guidelines for the treatment of these conditions in Spanish PC settings.
It will carry out a long-term follow-up using both biological and psychological assessments to analyse changes that the treatment may produce.
The sample size used will be a main limitation, because it has been estimated based on foreign works due to the lack of previous studies in the Spanish context.
Background
According to WHO, overweight and obesity are disorders in which there is abnormal or excessive fat accumulation in adipose tissue that can be harmful to health.1 They are defined operationally as a body mass index (BMI)—weight in kilograms divided by the square height in metres (kg/m²)—from 25 to 29.9 and ≥30 kg/m2, respectively. WHO estimated that, in 2014, 39% of adults worldwide were overweight (approximately 38% of men and 40% of women), and 13% were obese (approximately 11% of men and 15% of women).2 In absolute terms, it is estimated that approximately 1 billion adults are overweight and that at least 300 million are obese throughout the world, with an increasing prevalence in most countries.3 Unhealthy diet and the lack of physical activity are important causes of obesity4 and also the most important non-communicable obesity-related diseases, such as cardiovascular disease, type 2 diabetes and certain types of cancer.5 6 They contribute substantially to global morbidity, mortality and disability burden.7 Obesity has been associated with a higher prevalence of hypertension, dyslipidaemia, sedentary lifestyle, diabetes, subclinical organ injury and cardiovascular disease,8 depression,9 migraine10 and hypertension.11
Even in the Mediterranean region (in which Spain is located), traditionally associated with a healthy lifestyle, the evolution of eating habits has led to a progressive abandonment of the traditional pattern, for example, decrease in the consumption of fruits and vegetables and increase in the consumption of fast food, especially among the youngest age groups.12 These eating style changes have also been complemented by a physical activity decrease pattern and longer sedentary time.13 In fact, Mediterranean countries currently express high obesity prevalence rates.14 15 The investigation of new ways to treat this problem in the primary care (PC) context is developing successfully, although incipiently, throughout virtual platforms that allow for the training and interaction of different professionals.16 The most common users of the PC system are patients between 45 and 75 years, and precisely this age range presents a higher prevalence of overweight and obesity than other age groups in Spain.17 Reducing the prevalence of obesity is not an easy task because a multiplicity of factors may be involved.18 In most cases, an individualised and multidisciplinary treatment is recommended because of the efficiency and resource complexities that such treatment may involve.19 20 Obesity treatment is a challenge to which societies have not yet adequately responded, and the prevalence of obesity has increased, leading to an encrusted problem.21
There are factors on which experts agree: diet and physical activity are fundamental pillars for the treatment of obesity to achieve a ‘negative’ energy balance.22 The fundamental objective in the initial treatment of overweight and obesity is to reduce body fat until it reaches a level that allows for an improvement in health and a reduction, as much as possible, in risk factors.23 To achieve long-term maintenance of weight loss, it is essential to modify and establish habits related to diet, eating patterns and physical activity.19 24 25 However, between 25% and 30% of patients with obesity seeking treatment to reduce their weight suffer from a marked depression condition or other psychological disorders. Thus, physicians or psychologists should routinely inquire about the mood, sleep, appetite, fun activities and eating patterns of patients with obesity. In fact, individuals with obesity with marked depression, anxiety or binge-eating problems may require pharmacological treatment and/or psychotherapy before trying to lose weight.26
Psychological treatments, mostly included in the cognitive–behavioural therapy umbrella, have shown favourable, but not definitive, results for weight loss.27 However, not all the studies reviewed have showed such positive outcomes,28 29 and given the intense debate in this field, there is an evident need for more trials and long-term evaluations. Less encouraging in their long-term results are other psychological treatments employed, such as psychoanalysis or hypnosis.30 31 On the other hand, it has been established that between one and two-thirds of the people who follow restricted diets gain more weight than they lose.32 The degree to which restricted diets are counterproductive has probably been underestimated due to several methodological problems, focusing on the results of successful weight loss instead of the long-term maintenance of weight loss. Moreover, studies do not provide consistent evidence that dietary restriction results in significant health improvements, regardless of possible weight change32; in fact, it is a significant contributor to binge eating.33 Nevertheless, changes in dietary habits do not necessarily have associated restrictions, since healthy changes may be made to food consumption without restriction, such as a healthy choice of food.34–36
At this point, a fundamental debate in the field has been the consideration or not of weight loss as a main outcome.37 Weight is a very simple measure that is not always directly related to the interaction that a person has with food, because there may be other factors to take into account, such as endocrine disorders or drug treatments. However, it has been observed that the consumption of certain problematic foods and eating behaviours, such as binge eating and eating linked to the satisfaction of emotional needs rather than the satisfaction of physical hunger, are related to the presence of obesity.38 In fact, our relationship with food is an important issue. Recently, a line of study interested in promoting the conscious choice of food, developing awareness of the differences between physical hunger and psychological hunger, noticing the satiety signs and eating healthily as a response to all those signals, has been developed.39 40 Within this current stream of the literature, the ‘mindful eating’ (ME) movement emphasises being aware of the present moment when one is eating, paying attention to the effect that food has on the senses and taking into account the physical and emotional sensations in response to the eating process.37 41
The first ME study42 showed that, through a 7-session group programme, it was possible to reduce the number of binge-eating episodes, as well as depressive symptomatology. The meditative practice related to eating was the best predictor regarding the improvement in eating control. Later, although a pilot study found no effects on weight change,43 it was observed that ME produces improvements in depressive symptoms, expectations of results, food-related self-efficacy and cognitive control with respect to eating behaviours in patients suffering from diabetes.39 44 More robust studies have concluded that dispositional mental awareness plays an important role in eating behaviours, supporting the use of ME feeding techniques in diabetes self-management interventions.45 It has recently been stated that ME seems to be an effective approach to weight and glycaemic control in people with diabetes, and thus, promoting mindfulness could be one of several behavioural tools to support key self-care aspects to regulate glycosylated haemoglobin.46 ME has also shown efficacy in binge-eating disorders47 and could contribute to weight loss and a reduction in sweets consumption and fasting glucose levels,36 although only moderate effects have been found when specifically trying to reduce weight in the long term.48
It has been said that ME appears to be effective in addressing emotional eating (EE), binge eating and eating in response to external cues, with the potential of improving problematic eating behaviours and controlling food intake.48 However, evidence of ME training on weight is mixed and additional research to determine comparative and long-term effects is needed.49 In recent years, EE—that is overeating in response to negative emotions50—has been seen as a potential explanatory factor of the complexity of overweight and obesity.51 It has been observed that: (1) EE interacts with loss of control eating, increasing disordered eating attitudes, BMI and adiposity52; (2) EE is implicated in the use of compensatory behaviours to regulate weight50; and that (3) decreases in EE are associated with weight loss success in overweight adults.53 It has been suggested that ME approaches might have a positive influence as adjuvant therapies for weight management and for the development of a more conscious eating style with healthier eating behaviours.54 55 This could be achieved because mindfulness-based programmes which usually incorporates training in dispositional mindfulness and self-compassionate attitudes improve emotion regulation processes,56 which in turn are inversely related to EE,51 suggesting the treatment of overweight and obesity should focus on calorie-restricted diets and on emotion regulation skills. However, to the best of our knowledge, no studies have attempted to improve these eating variables in patients suffering from overweight or obesity using ME interventions in the Spanish PC context.
Objectives
The main aim of this study will be to evaluate an ME psychological intervention plus treatment as usual (‘ME +TAU’) to promote a healthy change in relations with food by reducing EE in patients with overweight or obesity in PC settings, compared with a control group that will receive medical treatment as usual (‘TAU alone’). The secondary aims will be to assess the possible differences between groups in external, restrained, binge and ME as well as eating disorder risk, anxiety, depression, dispositional mindfulness and self-compassion. Finally, we will also explore the possible differences in anthropometric, vital sign and blood test measures to determine the scope of the intervention on these physical parameters.
The principal hypothesis is that ‘ME +TAU’ will be more effective than ‘TAU alone’ in reducing EE in patients with overweight or obesity in PC settings. The secondary hypothesis is that ‘ME +TAU’ will function better than ‘TAU alone’ to improve the levels of external, restrained, binge and ME, eating disorder risk, anxiety, depression, dispositional mindfulness and self-compassion, as well as the anthropometric, vital sign and blood tests physical parameters.
Trial design
This study is a multicentre, two-armed, parallel, cluster randomised trial (CRT) with PC health centres as clusters, with pretreatment, post-treatment and 1-year follow-up measures, and an equal cluster allocation rate between groups as well as equal cluster size. PC centres (ie, clusters) in the city of Zaragoza, Spain, will be randomly assigned to two different conditions, with one psychological intervention group (‘ME +TAU’) or one usual treatment group (‘TAU alone’) managed by their general practitioner (GP), to test the superiority of the ‘ME +TAU’ provision compared with the ‘TAU alone’ provision, considering outcomes at the individual participant level. A CRT design will be used because the intervention will be performed in PC settings and persons within the same PC health centre may respond more similarly to the intervention than persons drawn from different PC health centres—they could have more characteristics in common owing to the fact of sharing the same environment and deliverer of intervention treatment (GP).57 For ethical reasons, those PC health centres allocated to ‘TAU alone’ will also be offered the ME programme after finishing the trial at 1-year follow-up.
Methods
This protocol was designed in accordance with the Standard Protocol Items: Recommendations for Interventional Trials 2013 statement.58 The timeline of the study is presented in table 1.
Table 1.
Schedule of enrolment, interventions and assessments
| Study period | |||||||
| Timepoint | Enrolment | Allocation | Intervention | 12-month follow-up | |||
| April 2019 |
May 2019 |
June 2019 |
July 2019 |
August 2019 | September 2019 | June/August 2020 |
|
| Enrolment | |||||||
| Eligibility form | X | ||||||
| Informed consent | X | ||||||
| Allocation | X | ||||||
| Interventions | |||||||
| ME+TAU C1(1) |

|
||||||
| ME+TAU C1(2) |

|
||||||
| ME+TAU C2(1) |

|
||||||
| ME+TAU C2(2) |

|
||||||
| TAU alone C3 |

|
||||||
| TAU alone C4 |

|
||||||
| Assessments | |||||||
| Sociodemographic | X | ||||||
| DEBQ | X | X | X | X | X | ||
| BITE | X | X | X | X | X | ||
| EAT-26 | X | X | X | X | X | ||
| FFMQ | X | X | X | X | X | ||
| SCS | X | X | X | X | X | ||
| MES | X | X | X | X | X | ||
| GAD-7 | X | X | X | ||||
| PHQ-9 | X | X | X | ||||
| Weight (kg) | X | X | X | ||||
| Waist perimeter (cm) | X | X | X | ||||
| Vital signs (DBP, SBP) | X | X | X | ||||
| Cholesterol (HDL, LDL) | X | X | X | ||||
| Glucose | X | X | X | ||||
| HbA1c | X | X | X | ||||
| ALT | X | X | X | ||||
ALT, alanine aminotransferase; BITE, Bulimic Investigatory Test Edinburgh; C, cluster (subgroup in brackets); DBP, diastolic blood pressure; DEBQ, Dutch Food Behaviour Questionnaire; EAT-26, Eating Attitude Test; FFMQ, Five Facet Mindfulness Questionnaire;GAD-7, General Anxiety Disorder; HbA1c, glycosylated haemoglobin;HDL, high density lipoprotein; LDL, low density lipoprotein; MES, Mindful Eating Scale; ME+TAU, Mindful eating;PHQ-9, Patient Health Questionnaire; SBP, systolic blood pressure; SCS, Self-Compassion Scale; TAU, treatment as usual.
Participants, study setting and eligibility criteria
Participants will be chosen from the four PC health centres of Las Fuentes Norte, Parque Goya, La Almozara and La Jota in the city of Zaragoza (Spain). The city of Zaragoza has a population of 663 023 inhabitants, with approximately an average age of 44 years, a percentage of women of 52%, an average per capita income of €11 800, a percentage of emigrants of 14% and a dependency rate of 53%.59 Each of the four PC health centres has an assigned population of between 10 000 and 24 000 patients whose average age is between 41 and 46 years, a percentage of women between 51% and 53%, an average per capita income between €9000 and €12 000, a percentage of emigrants between 6% and 17% and a dependency rate of between 41% and 58%, and thus can be considered representative of the PC health centres of Zaragoza according to the previously described variables. Patients will be selected by GPs working in the PC centres (with one GP for each PC health centre, which will function as a cluster). When the GPs observe potential participants who meets the eligibility criteria, they will be informed about the general characteristics of the study, providing them with the opportunity to participate. The inclusion and exclusion criteria of the patients are specified in table 2.
Table 2.
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|
|
BMI, body mass index.
Within the general framework of promoting healthy and active lifestyles in the community, participants are required to have two of the following three risk factors in order to be included in the study: (1) sedentary lifestyle, (2) poor diet or (3) binge episodes. GPs will evaluate the suitability of patients for the trial in terms of their age and overweight/obesity condition, ability to understand Spanish and willingness to participate in the study. A psychologist assessor will assess the level of physical activity, using the International Physical Activity Questionnaire—a sedentary lifestyle will be established in case of a low level of physical activity60; a possible poor diet, using the Diet Quality Index-International—a poor diet will be considered when obtaining a score <5061; and the presence of binge episodes, using the Bulimic Investigatory Test Edinburgh (BITE)—with a cut-off point of two binge episodes in a week.47
Exclusion criteria were derived from the typical criteria used to rule out patients in this type of study, including serious mental illness, acute-phase depression, schizophrenia or psychotic disorders, drug abuse or dependence and medical conditions that make it difficult to participate in the intervention.62–64 These exclusion criteria will add proper functioning to the intervention groups and also patient safety, avoiding possible exacerbations of psychosis, mania or suicidal ideation.65–67 Anxiety or personality disorders will not be excluded so as not to bias the selected sample, because they are particularly related to eating disorders.68 69 All in all, an adequate monitoring through the study will be carried out regarding the safety of all patients (described next). If patients are interested in participating, they will be asked to sign a written informed consent form. Patients who do not accept participation will be treated in their PC centres as usual due to ethical reasons.
Patient and public involvement
The research question was based on one of the most principal problems that the PC population suffers from. Patients and GPs require more tools to face the existing high prevalence of overweight and obesity, which leads to more risk and high costs for society.70 71 Taking this into account, we started with an 8-session uncontrolled open-label pilot study offered to the public in general, with the main aim of adjusting an ME programme to the PC population.
We recruited 10 patients from the Arrabal PC health centre in the city of Zaragoza who were willing to participate (8 women and 2 men, with an age range of between 45 and 65 years). After the last session of this early iteration, we inquired specifically about the content of the programme and the results they could have experienced during these 8 weeks, the appropriateness of the length of the intervention and about homework management. We did not quantitatively assess the potential changes of this pilot presentation because we were more interested in how they experienced the programme, as well as possible implementation issues. We specifically asked for the following aspects: ‘How do you feel about the content and results of the programme?’, ‘Has the programme been long enough?’ and ‘Did you follow the weekly home task?’ The most common responses pointed out that the content of the programme was helpful and had changed their level of awareness of unhealthy eating patterns, but also that the programme had too many sessions, and that the home tasks were too difficult to be carried out during the programme. Due to the good participation and feedback obtained, and considering the difficulties reported, we decided to continue working on this research line involving patients and GPs. Following the comments of the pilot participants, we adjusted the original programme length down to seven sessions, and also lightened the homework load.
The individual results of the present study will be shared by email with the corresponding participants who express their desire to know the results. The resulting publications will also be disseminated to participants, and a free lecture of a summarised report, once the study has finished, will be offered. In addition, participants will answer a questionnaire that includes open questions regarding the professionals involved, the programme and their own experience.
Sample size
The sample size estimation has been based on the main comparison, which contemplates the possible differences between the ‘ME +TAU’ and ‘TAU alone’ groups of patients. Based on previous research,72 we assume that ‘ME +TAU’ would be able to present high effects compared with ‘TAU alone’ on EE at post test. To operationalise this, we consider a standardised difference between arms on the referred main outcome of 0.80.72 To detect this difference between the groups, assuming a common SD, a 5% significance level and a statistical power of 80% using a 1:1 ratio, we need 25 subjects in each group. However, these numbers correspond to the sample size needed under individual randomisation, which is the absolute upper bound for cluster size—clusters are randomised and thus we need to allow for the correlation between the EE outcomes of participants from the same cluster.73 To determine the minimum number of clusters needed, we used the formula ‘n * ICC’, where n is the sample size for each arm under individual randomisation and ICC is the intracluster correlation coefficient that quantifies the amount of within-cluster correlation for the outcome of interest, assuming a typical fairly value in CRTs of ICC=0.03,74 with a result of approximately one cluster in each arm. Because the number of clusters in the trial is limited by the number of PC settings available to implement the ME programme, we increased the number of clusters to one more than the minimum, supposing that the cluster size would be at most ‘n/1’. Thus, we fixed the number of clusters per arm to 2 in order to determine the required cluster size.75 In order to maintain the same absolute difference and significance level described above to achieve 80% power with 2 clusters in each arm, we needed a cluster size of 16 participants. In addition, by fixing the cluster size at 16 participants in the same conditions, we obtained the need of 2 clusters per arm, equating to a total sample size of 64 subjects under the condition of equal cluster sizes. Finally, we inflated the numbers to reach a total sample size of 76 patients (38 per arm), considering a drop-out rate of approximately 20% at 1-year follow-up.76 This can be considered an efficient design based on the rule that cluster size should not exceed the number estimated in each arm under individual randomisation.73 This number also enlarges the sample size under individual randomisation in a measure that includes the design effect ‘DEFF=1 + (m – 1) * ICC’—where m is the average number of patients per cluster—with a value of DEFF=1.45, and thus demanding an increase with regard to individual randomisation of around 45%.57
Recruitment
Participants will be identified and recruited in PC settings by involving the GPs of patients who fulfil the study criteria. The GPs will complete referral forms, indicating that the patients meet the criteria and will provide a brochure and an information sheet to present the study. The GPs will send the referrals and the patients’ signed written consent forms by mail to a local researcher. Some patients may prefer to postpone their decision to participate in the study, in which case they will be provided with information about how to contact the research team (by phone, email or leaving their information on the group’s website).
An assessor-researcher, who is not part of the study team, will contact the participants to agree on the established evaluation times and will clarify any points, ensure that the participants have read the information about the study, and ensure they have understood the two experimental conditions. The assessor will then finally determine their inclusion in the study after considering the inclusion and exclusion criteria described above, and before contacting an independent researcher to implement the randomisation sequence to the clusters. Recruitment will be performed consecutively until the final sample size is reached. The assessor will collect the baseline data, including the primary outcome. GPs will adhere to the study protocol before the randomisation of clusters, and they will be blinded to the allocation group of clusters together with the assessor-researcher. Possible migrations of participants out of clusters will be especially taken into account so as not to lose post-treatment and follow-up measures.
Randomisation, allocation and masking of study groups
The identification and inclusion of participants will take place before the randomisation of clusters, ensuring allocation concealment to cluster guardians (who are the corresponding GPs), assessors and patients during recruitment.77 78 Restricted randomisation will be applied to balance clusters, creating comparable arms in terms of the number of clusters but also in the average per capita income of the assigned population to each PC health centre.79 The rationale of this is that this variable has been inversely related to the presence of overweight and obesity,80 81 and also to possible limitations in gaining benefits after mindfulness-based programmes.82 The maximally homogeneous cluster pairs in the average per capita income at the level of PC health centres will be matched and randomly divided between the intervention and control arms, as shown in figure 1. As a result of this matching process, we will obtain a number of strata that is half the total number of clusters to be allocated, which is considered the minimum number of clusters to safely achieve balance.83 This matching procedure is particularly useful when there are few clusters in the study,84 and it provides face validity regarding balance between allocation arms.85 No other cluster or individual-level imbalances for important covariates related to the main outcome are expected between arms.
Figure 1.
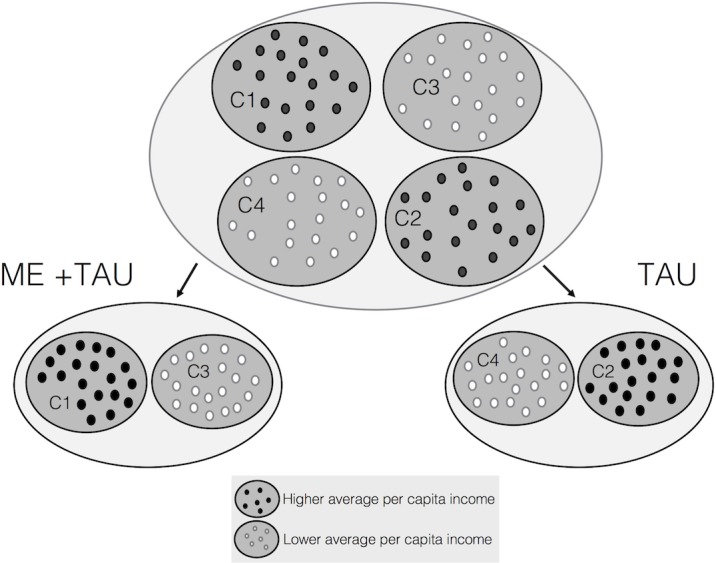
Restricted randomisation applied to primary care (PC) health centres. Figure represents the matching process: the maximally homogeneous PC health centres pairs in terms of the predefined average per capita income of the assigned population (higher average per capita income pair and lower average per capita income pair) will be divided randomly between the ‘mindful eating (ME) + treatment as usual (TAU)’ (intervention) and only ‘TAU’ (control) arms. The number of points reflects the cluster size. C, cluster.
An independent assistant not involved in the study will be in charge of performing the cluster randomisation by using a computer programme to generate an unpredictable random allocation sequence. This assistant will be unaware of the characteristics of the study and will inform the data manager of a code that corresponds to the type of treatment to be added to the baseline data. The meaning of this code will be unknown by the person in charge of randomisation and by the data manager—it will be known only to the data monitoring committee (DMC) and will be kept under a password-protected database system. The DMC will receive the baseline data from the data manager and will be in charge of implementing the random sequence.
Participants will agree to their inclusion before finding out the treatment to which they will be allocated. As we have previously explained, the baseline assessor will be blind to the type of treatment that will be administered to clusters and patients. This assessor will be different from the person responsible for collecting the post-test and follow-up measurements, who will be a blinded external assistant specifically advised not to ask for the study aims and the allocation of clusters/patients. GPs will be blinded to the intervention arm to which each patient is allocated since their intervention should be based only on usual practice, and they will also be advised not to ask for that information. The person responsible for performing the data analysis will be blinded to the type of intervention in the main outcome analysis, receiving the database without any data that permits this identification. Any doubt regarding the data will be resolved in contact with the data manager, and the other researchers will be blinded while analysis and data interpretation processes are taking place. However, due to the characteristics of the intervention, participants will be able to know what kind of intervention they are receiving; thus, this will be a single blind study—although both ‘ME +TAU’ and ‘TAU alone’ groups will be treated one way or another. A verification of successful blinding at all stages referred will be performed by the DMC.
Data management
A researcher psychologist will perform the data handling and monitoring. All study information will be confined in secure drawers with limited access. Electronic data files will be password protected. Participant codes and personal information will be stored in a separate password-protected file. Data will be stored for 5 years after the end of the study. Only the researchers directly involved in the study and led by the principal investigator will have access to the final dataset. Paper-based data entry will be double checked, and possible out-of-range values will be specifically revised. In case data are actually correct, they will be analysed altogether by boxplot graphical representations to see whether the previously described values constitute extreme outliers. If extreme outliers appear, a sensitivity analysis after removing them will be performed to ensure robustness of results. The study results will be presented via peer-review publications and congresses. In addition, the study participants will receive a summarised report on request, and the funders and involved clinicians will also receive an anonymised report.
Interventions
All participants, regardless of the treatment arm in which they have been assigned, will receive the TAU at the PC level. According to the pragmatic nature of the present study, ad hoc adherence optimisation procedures will not be used, as not to interfere with diverse routine practices. In fact, patients will be free to decide whether they will discontinue intervention on request. If participants decide to be part of any other medical or psychological treatment focused on changing their relation with the food or weight reduction, the contact person of the study should be informed to exclude those participants when developing the corresponding data analyses. The rest of the treatments will be allowed.
Treatment as usual
TAU in PC is any kind of treatment administered by the GP to the patient with overweight or obesity. According to nutritional status, overweight or obesity, as well as the presence of comorbidity, different actions can comprise the treatment offered at the PC level. For individuals presenting with overweight (BMI 25–29.9 kg/m2) or obesity (≥30 kg/m2) but with no comorbidities, PC teams organise care plans adjusted to the characteristics of patients to enable them to achieve a normal BMI range (BMI 18.5–24.9 kg/m2). In cases of suicide risk, severe social dysfunction or worsening of symptoms, it is recommended that patients are referred to mental health facilities.86 In Spain, GPs spend a minimum of 4 years completing their medical specialty. The GPs who will be participating in the present study have more than 20 years of clinical experience treating patients with overweight or obesity, and they will have undergone specific training focused on endocrinology and internal medicine for a better understanding of obesity and its implications and comorbidities such as diabetes and hypertension.
Mindful eating
The ME group will be composed of 7 weekly group sessions with a minimum duration of 2 hours, mixing theoretical content with practices. Sessions will always be the same day of the week, except for bank holidays or eventualities, and will be conducted by a clinical psychologist. This psychologist has been specially trained in ME programmes, for example, Mindfulness-Based Eating Awareness87 and Mindful Eating Conscious Living,88 and he is also a board member of The Center for Mindful Eating (TCME).89 The TCME is a non-profit international organisation that provides resources for educating professionals in the field of ME. This clinical psychologist has also run several ME groups over the past 5 years and he is a coauthor of the manual on which the present programme was based.90 Group sizes will range between 8 and 12 participants in four different subgroups of treatment. At the end of each session, participants will receive theoretical content and homework activities to be practised during the week. The programme is summarised in table 3 and described as follows:
Table 3.
Summary of the mindful eating sessions and content
| Session | Content | Practices | Home task |
| Session 1 Mindful eating introduction |
|
|
|
| Session 2 Mindful eating and compassion |
|
|
|
| Session 3 Integrating consciousness |
|
|
|
| Session 4 Satiety and appetite values |
|
|
|
| Session 5 Conscious choice and forgiveness |
|
|
|
| Session 6 New balance consciousness |
|
|
|
| Session 7 Wisdom and pursuing the path |
|
|
– |
Session 1: this session is aimed at motivating home practice and is complemented by an introduction to ME. Observation is an attitude that will be developed during this session, allowing patients to connect with their emotions, thoughts and body sensations, moment by moment, to be aware of possible unhealthy eating patterns. The awareness of automatised patterns can give patients the chance to change behaviour, making decisions more connected with necessities. The ME efficacy mechanisms are explained.
Session 2: the objective of this session is to be aware, at any moment, of one’s hunger level, observing eating patterns and their possible relation with the emotions that are felt at the same time. This session works by identifying EE triggers and knowing how compassion and the inner critical voice are related to the food.
Session 3: the objective is to recognise the differences between real hunger signals and other body sensations generated by the environment that trigger the desire to eat. Training at the body consciousness level helps one find the point of balance that allows for eating and enjoying, paying attention to eating, feelings, body sensations, emotions and thoughts.
Session 4: This session aims to work with the corporal sensations that food produces. When the physical sensations are of discomfort, swelling or heaviness, this indicates that the food intake was excessive. When the sensation is related to satiety, this is a good moment to stop eating. The satiety signal is identified through mindfulness (chocolate practice).
Session 5: it address the fullness sensation as something different from not being hungry and the ‘EE’ concept. It encourages us to accept all we experiment, managing the inner critical voice. The practice of conscious movements to become aware of the body and bring full attention to the present moment is a guide in decision-making.
Session 6: this session emphasises the relationship between the knowledge of feeding and nutrition and conscious and balanced decision-making. It works with emotional triggers through the chain practice and also integrates the potluck practice. Foods that trigger greater EE are shared and discussed in the group.
Session 7: this session is focused on binge episodes and how we can manage EE in the future by substituting the inner critical voice with a compassionate voice. The way we are aware of our thoughts, emotions and decisions is what allows us to break the chain of EE and start a new relationship with food, managing and making decisions about emotions and food in a wiser way.
Outcomes
Patients will be assessed at baseline, after treatment and at 1-year follow-up to test whether the improvements achieved during therapy are maintained in the long term. Several variables will be assessed to compare the ‘ME +TAU’ and ‘TAU alone’ groups to evaluate the effects of the ME programme. EE styles, which will compose the main outcome, have a direct relation with overweight and obesity.51 These eating styles are related to how much you eat and even more to how you eat. The Dutch Eating Behaviour Questionnaire (DEBQ) is a good evaluator of this construct (EE is a subscale of this questionnaire) and has been rated ‘up to the mark’, that is, appropriate, by the Dutch Committee on Test and Testing and by the European Federation of Psychologists Association.91
The secondary outcomes will be other eating patterns that could be modified as a result of the application of the programme, such as external and restrained eating, also measured by the DEBQ (both are also subscales of this questionnaire); binge eating, measured by the BITE92; and eating disorder risk, measured by the Eating Attitude Test (EAT).93 Other secondary outcomes will be emotional states, which affect the way we eat. To evaluate this, the General Anxiety Disorder (GAD-7), which is one of the most frequent screening scales in PC, will be used to assess anxiety.94 The GAD-7 is often used in combination with the Patient Health Questionnaire (PHQ-9) to measure depressive symptoms, which will also be included.95–100 Physiological variables will also be important to evaluate whether changes in eating style and emotional state have consequences for the general health condition in the long term. For this purpose, anthropometric and vital signs will be assessed—including weight, abdominal diameter, diastolic blood pressure (DBP) and systolic blood pressure (SBP)—as well as blood tests, all of which are described next.
To relate the awareness of the present moment and the way in which compassionate and critical attitudes towards the self can be managed as possible emotion regulation strategies,56 101 the evaluation of the dispositional mindfulness and self-compassion levels will be pursued as mechanistic variables of the programme through application of the widely used Five Facet Mindfulness Questionnaire (FFMQ), the Mindful Eating Scale (MES) and the Self-Compassion Scale (SCS). Mindfulness is a way of self-regulating attention to focus it on the present moment experience with an attitude of curiosity, openness and acceptance of bodily sensations, thoughts and emotions.102 Deficits in dispositional mindfulness have been reported in patients suffering from eating disorders and obesity.103 104 It has also been observed that the non-judgemental awareness of physical and emotional sensations, specifically associated with eating, correlates inversely with the severity of eating disorders105 and increases healthy food choices.106 Finally, self-compassion has received much attention in assisting individuals with eating behaviours and weight regulation.107 It is a kind approach towards oneself, with a mindful awareness and understanding of one’s experiences as part of shared reality that all people go through during personally challenging or difficult times.108 It has been observed that receiving a self-compassionate induction to cope after the experience of breaking the diet enables further regulation to occur,109 and that self-compassion could be a determinant for weight regulation and losing weight.110 111 Overall, the combination between mindfulness and self-compassion appears to be complementary, creating better health-related outcomes for both eating behaviours and obesity.55 All the study measurements, together with the sociodemographic data taken at baseline, are summarised in table 4.
Table 4.
Study outcomes
| Variables | Assessment area | Level of measurement | Time to assessment |
| Sociodemographic | Age, sex, nationality, marital status, work activity, study level and PC health centre | Varies depending on the distribution of data | Baseline |
| DEBQ | Eating style: emotional, external and restrained eating | Treated as interval | Baseline, post treatment and 1-year follow-up |
| BITE | Binge eating: symptoms, severity and frequency of bingeing | Treated as interval | Baseline, post treatment and 1-year follow-up |
| EAT | Eating disorder: dieting, bulimia and food preoccupation, and oral control | Treated as interval | Baseline, post treatment and 1-year follow-up |
| GAD-7 | General anxiety symptoms | Treated as interval | Baseline and 1-year follow-up |
| PHQ-9 | Depression symptomatology | Treated as interval | Baseline and 1-year follow-up |
| FFMQ | Mindfulness: observing, describing, acting with awareness, non-judging and non-reactivity | Treated as interval | Baseline, post treatment and 1-year follow-up |
| MES | Mindful eating: acceptance, awareness, non-reactivity, acting with awareness, routine and unstructured eating | Treated as interval | Baseline, post treatment and 1-year follow-up |
| SCS | Self-compassion: self-kindness, self-judgement, common humanity, isolation, mindfulness, and overidentification | Treated as interval | Baseline, post treatment and 1-year follow-up |
| Anthropometrics | Weight, height, waist circumference and abdominal diameter | Treated as ratio | Baseline and 1-year follow-up |
| Blood test | Cholesterol total, LDL, HDL, triglycerides, ALT, glucose and glycated haemoglobin | Treated as ratio | Baseline and 1-year follow-up |
| Vital signs | Systolic and diastolic blood pressure | Treated as ratio | Baseline and 1-year follow-up |
| Attendance | Compliance with the programme | Treated as interval | Post treatment |
ALT, alanine aminotransferase; BITE, Bulimic Investigatory Test Edinburgh;DEBQ, Dutch Eating Behaviour Questionnaire; EAT, Eating Attitude Test; FFMQ, Five Facet Mindfulness Questionnaire; GAD-7, General Anxiety Disorder; MES, Mindful Eating Scale;PC, primary care; PHQ-9, Patient Health Questionnaire; SCS, Self-Compassion Scale.
Sociodemographics
The following sociodemographic information will be collected at baseline: age, sex, nationality, marital status (single, married, separated/divorced or widowed), work activity (student, worker, sick leave, unemployment, housewife, disability or retired), study level (no studies, primary, secondary or university) and the PC health centre of provenance in the city of Zaragoza, Spain (Las Fuentes Norte, Parque Goya, La Almozara or La Jota).
Main outcome
The DEBQ was designed to measure eating styles that may attenuate or contribute to the development of overweight and obesity.112 It comprises three scales that measure emotional, external and restrained eating. The EE pattern corresponds to the tendency towards overeating in response to negative emotions113 and will be considered the main outcome of this study (both external and restrained subscales will be included as secondary outcomes even though they are presented here). Emotional and external eating are correlated with BMI. The restraint factor has shown relationships with other scales, such as the EAT-26 and the Restrain Scale, which measure eating disorders and restrained eating, respectively. The Spanish version112 of the DEBQ114 has 33 items, 13 of which refer to the EE scale (eg, ‘Desire to eat when irritated’) and 10 of which refer to the external (eg, ‘Eating when you feel lonely’) and restrictive (eg, ‘Difficult to resist delicious food’) scales. The items can be rated on a five-point Likert-type scale, with a score of 1 indicating ‘never’ and 5 indicating ‘very often’. In a non-clinical sample of normal weight, overweight, and obese participants, Cronbach’s alpha coefficients presented values between 0.96 and 0.97 for the DEBQ-EE subscale, between 0.79 and 0.84 for the DEBQ-external eating subscale and between 0.92 and 0.94 for the DEBQ-restrained eating subscale.33
Secondary outcomes
We will administer the BITE92 in its Spanish version.115 This questionnaire is used to measure the presence of bulimic symptoms in non-clinical samples and has two subscales measuring symptoms (eg, ‘Desire to eat when irritated’; with 30 items in a ‘yes’/‘no’ dichotomous scale; range=0‒30) and severity (eg, ‘Do you do any of the following to help you lose weight?’; with 6-dimensional items addressing bulimic behaviours; range=0‒39), with a total of 33 items. In addition to normative values for total and subscale scores in clinical and nonclinical samples,116 another measure has been derived to report the frequency of bingeing (item no. 27, ‘If you do binge, how often is this?’; this item will be mainly framed in the last month so as not to overlap pretest and post-test measures, with the following type of response: ‘2–3 times a day’=6; ‘Once a day’=5; ‘2–3 times a week’=4; ‘once a week’=3; ‘once a month’=2; ‘almost never’=1). The BITE has shown an internal consistency value of α=0.96 for the symptoms and of α=0.62 for the severity subscales.117
To assess any other eating disorder, we will use the EAT-26,93 in its Spanish version.118 This questionnaire has the following three subscales: dieting (eg, ‘Am terrified about being overweight’), bulimia and food preoccupation (eg, ‘Find myself preoccupied with food’) and oral control (eg, ‘Avoid eating when I am hungry’). The EAT-26 is an abbreviated version of the original EAT-40, with an excellent correlation between them (r=0.98). In the EAT-26, each item is answered on a 6-point Likert-type scale (‘always’=3, ‘usually’=2, ‘often’=1, ‘sometimes’=0 ‘rarely’=0 and ‘never’=0), and if the score is 20 or higher, the patient should seek professional advice. The EAT-26 has an elevated reliability (α=0.80).
The GAD-7 is one of the most frequently used diagnostic self-report scales for screening, diagnosis and anxiety disorder severity assessment,119 defined as an excessive anxiety and worry (apprehensive expectation) related to a number of events or activities associated with experiencing difficulties to control that worry.120 Items (eg, ‘Not being able to stop or control worrying’) are rated on a 4-point Likert-type scale (between 0 = ‘not at all’ and 3 = ‘nearly every day’). The GAD-7 inquires about events occurring over the last 2 weeks to know how often the patient has been bothered by them, and it has shown a sensitivity of 89% and a specificity of 82% when discriminating patients suffering from generalised anxiety disorder. The Spanish version of the GAD-7 has shown appropriate psychometric characteristics.121
We will use the PHQ-9122 to assess depressive symptomatology. This scale is one of the most widely used questionnaires to assess the intensity of depression in pharmacological and psychological studies.123 124 It is useful to monitor the changes experienced by patients over time and presents a sensitivity value of 88% and a specificity of 88% to detect major depression. Through items such as ‘Little interest or pleasure in doing things’ and using a Likert-type scale between 0 (‘not at all’) and 3 (‘nearly every day’), the PHQ-9 reflects the experience of participants during the last 2 weeks. The Spanish validated version, which has shown adequate psychometrics, will be used.86
Process measures
The FFMQ-short form125 is a 24-item questionnaire that measures 5 aspects of trait mindfulness, and there is a Spanish version based on it with appropriate psychometrics.126 The five facets of the FFMQ are observing (eg, ‘I pay attention to physical experiences, such as the wind in my hair or sun on my face’; four items, α=0.65), describing (eg, ‘I am good at finding words to describe my feelings’; five items, α=0.79), acting with awareness (eg, ‘It seems I am running on automatic without much awareness of what I am doing’—item reversed; five items, α=0.80), non-judging towards inner experience (eg, ‘I make judgements about whether my thoughts are good or bad’—item reversed; five items, α=0.73) and non-reacting of inner experience (eg, ‘When I have distressing thoughts or images, I do not let myself get carried away by them’; five items, α=0.68). The participants indicate, on a 5-point Likert-type scale, the degree to which each item is generally true for them, ranging from 1 (‘never or very rarely true’) to 5 (‘very often or always true’). Higher scores indicate greater levels of mindfulness.
It has been observed that mindful awareness towards eating may minimise automatic and impulsive reactions, thereby fostering self-regulation.127 We will measure ME through the MES questionnaire.128 The MES questionnaire has 28 items, including the following 6 factors: acceptance (α=0.89; assessed through items such as ‘I criticize myself for the way I eat’), awareness (α=0.82; for example, ‘It is easy for me to concentrate on what I am eating’), non-reactivity (α=0.77; for example, ‘I can tolerate being hungry for a while’), acting with awareness (α=0.81; for example, ‘I eat something without really being aware of it’), routine (α=0.75; for example, ‘I have a routine for what I eat’) and unstructured eating (α=0.60; for example, ‘I multi-task while eating’. Items can be rated on a 4-point Likert-type scale, with 1 indicating ‘never’ and 4 indicating ‘very often’. The MES Spanish validated version has shown adequate psychometric features.128
The SCS129 is the most used self-report instrument to measure self-compassion. It is divided into six subscales: self-kindness (eg, ‘I am kind to myself when I am experiencing suffering’); self-judgement (eg, ‘When I see aspects of myself that I do not like, I get down on myself’); common humanity (eg, ‘I try to see my failings as part of the human condition’); isolation (eg, ‘When I fail at something that is important to me, I tend to feel alone in my failure’); mindfulness (eg, ‘When something upsets me, I try to keep my emotions in balance’); and overidentification (eg, ‘When something upsets me, I get carried away with my feelings’). The items can be rated on a five-point Likert-type scale, with 1 indicating ‘almost never’ and 5f indicating ‘almost always’. After reversing the negatively formulated items, a total score can be calculated, which may range from 24 to 120, with higher scores indicating greater self-compassion.129 The SCS total has shown good internal reliability (Cronbach’s α=0.92), as did the six subscales (ranging from α=0.75 to α=0.81.129 The Spanish validated version of the SCS has demonstrated good psychometric properties.130
Physical parameters
Weight and body measurements will be quantified, with weight in kilograms, and height, waist circumference and abdominal perimeter in centimetres (cm); weight without any anthropometric measures is not an accurate assessment of the physical changes associated with a healthy food relation. The evaluations will be made the same day and just before the psychometric assessments, using a measuring tape and the same digital scales. Blood tests will evaluate the levels of total cholesterol (HDL and LDL), triglycerides, alanine aminotransferase, glucose and glycated haemoglobin. The blood test will be performed in the morning (between 08:00 and 09:00, and all participants should have fasted for 8 hours prior to the test. Vital signs such as DBP and SBP will also be assessed. To evaluate vital signs, we will use a vascular screening system (version VaSera VS-1500).
Other measures
In addition, the number of ME programme group sessions attended, as well as the number of visits to the corresponding GP in both groups, will be recorded. Video recordings will not be taken in order not to interfere with the natural way in which exercises are held.
Harms
Thus far, there is no described evidence in the literature regarding any side effect as a result of specific ME practice, although participation in meditation programmes in general might exacerbate negative experiences to the same extent as psychotherapy.131 Any adverse event observed by the GPs or psychologist in charge of the groups or referred from patients during the sessions or along the whole programme will be communicated to the trial manager (the leader of the research group, who is a psychiatrist and will be able to refer the patient directly to mental health services should this be necessary), and also to an independent GP and an independent psychologist with broad experience in the clinical field of mindfulness and eating disorders; they will act together to form the DMC. If the unintended effects are related to the treatment, the DMC will be committed to informing the corresponding PC physician and providing the individualised treatment to each case scenario in PC settings or derived to mental health services by their PC physician or the trial manager if required. Then, the DMC and the corresponding PC physician will decide whether to discontinue or modify the allocated intervention depending on the nature and severity of the side effects. The DMC will audit trial conduct at least three times throughout the study (after baseline, post treatment and follow-up assessments, as well as at the request of any of the members of the research group), in coordination with the psychologist responsible for data handling and the psychologist in charge of the groups—but independently of the other parts. To ensure that the procedures are being correctly implemented and that the trial works adequately, audits will revise aspects such as the level of attendance in group sessions and TAU, adverse events emerged through the study and possible extreme cases that might require specific attention in any of the variables assessed.
Analysis strategy
The reporting of the results will follow the Consolidated Standards of Reporting Trials recommendations.132 133 Sociodemographic and clinical data will be described at baseline by means of frequencies and percentages, for categorical variables, or by means and SDs, for continuous variables. Treatment conditions will be compared at baseline by visual inspection to ensure the success of randomisation, as recommended.134
Main analysis
The effectiveness of ‘ME +TAU’ compared with ‘TAU alone’ will be estimated at post test, based on the EE main outcome, which will be considered a continuous variable at the individual level. Multilevel mixed-effect regression models—including time as an independent variable and subjects and PC health centre (cluster) as random-effect variables—will be developed by means of a repeated-measures (RM) design on an intention-to-treat basis, using the restricted maximum likelihood method. This method is considered robust in the case of small and/or unbalanced sample sizes.135 Non-standardised and unadjusted slopes as well as 95% CI will be calculated. To study the specific trajectories of each group throughout the trial and determine whether the differences between groups are consistent over time, the ‘group × time’ interaction will be calculated as a supportive analysis (ie, the 1-year follow-up time point will be considered as a secondary analysis). Cohen’s d effect sizes (ESs) from raw scores will be estimated at each time point using the combined SD at baseline.136 ESs are considered small when d≤0.2; medium when d=0.5 and large when d≥0.8.137
Secondary analyses
A recent study observed that multiple imputation is not necessary before computing RM mixed effects model analysis irrespective of the type of missing data,138 and other studies have suggested there are no gains in imputing outcomes in randomised trials.139 140 Thus, imputed scores will not be calculated to estimate sensibility analyses regarding any statistics. Nevertheless, supportive analysis of the EE main outcome at 1-year follow-up, as well as models of EE at post test and at follow-up with the interaction of sex, weight status and the baseline levels of anxiety and depression as possible covariates, will be considered. Relationships have been observed between EE and sex (females present higher EE), weight status (the more the EE the higher the weight status) and emotional disorders derived from anxiety and depression (higher levels of anxiety and depression are associated with greater levels of EE),50 141 142 and thus these variables will be included in the adjusted models.143 The effectiveness of the ‘ME +TAU’ compared with the ‘TAU alone’ group with regard to the secondary outcomes, process variables and physical parameters will be calculated following the same analytical strategy used for the main unadjusted analysis. In addition, secondary outcomes will be also analysed using adjusted models controlling for sex, weight status, anxiety and depression. ESs of all the adjusted models will be estimated from adjusted average marginal effects (AMEs), using the actual observed values for the variables whose values are not otherwise fixed.144
Further exploratory analyses of the EE primary outcome will be developed to estimate the complier average causal effect of treatment (CACE) in order to assess the potentially unbiased effect of fully participating.145 Compliers will be only observed among those randomised to receive the ME programme (ie, individuals assigned to the control group will not have access to the ME treatment), and will be defined as those patients who attend at least ≥50% of the ME sessions.146 A new variable will be created to identify whether each patient randomised to the ME group finally complied or not. Both within-cluster and between-cluster baseline covariates of compliers and non-compliers (intervention group) will be compared, and the CACE estimation will be calculated using the robust maximum likelihood expectation-maximisation algorithm for a multilevel mixture model, considering both clustering and non-compliance.147
The clinical significance of improvements between groups will be explored by calculating the absolute risk reduction and the number needed to treat (and their 95% CI). We will use two criteria for improvement: (1) changing to a less severe cluster in the EE main outcome148 compared with the one the patient was allocated to at baseline, and (2) calculating the clinical significance of improvements by establishing both the cut-off point and reliable change index on the EE main outcome using the Jacobson and Truax method.149
Level of significance
An alpha level of 0.05 will be established using a two-tailed test. The probability value relative to the sole primary model, as well as the probability values of secondary analyses proposed, will not be adjusted on the basis of number of tests done, although they will be interpreted with due caution. No interim analyses will be carried out.
Discussion
The present study proposes the evaluation of a leading and novel intervention based on ME in the field of overweight and obesity in the context of Spanish PC settings. The main interest of this study is to evaluate the effectiveness of this treatment in changing the relationship with food in patients suffering from overweight or obesity. The study addresses overweight and obesity from the point of view of the change in intake styles, specifically one of these, the emotional style of eating, which in turn has been linked to overweight and obesity conditions.50 51 53 This study may be able to generate knowledge to expand the content included in the clinical guidelines for the treatment of these conditions in Spanish PC settings and throughout the healthcare system. To date, the implementation of these clinical guidelines has been shown to be improvable.150 There is a lack of knowledge in this particular field due to the novelty of mindfulness and self-compassion interventions in PC settings. One of the most important goals here is to generate processes to facilitate new effective programmes to control the high prevalence of overweight and obesity in PC. Mindfulness-based programmes seem to present certain effectiveness for treating obesity‐related eating behaviours, such as EE, external eating and binge eating, with also possible beneficial effects in weight reduction,151–153 as well as depressive symptoms154 and well-being.155
No particular difficulties are expected regarding the recruitment of PC health centres and patients with overweight/obesity or their participation and monitoring throughout the study.156–158 CRTs involve randomisation of groups of individuals to intervention or control groups, and their use is growing because they fit well with the functioning of healthcare systems when introducing new forms of treatment. However, CRTs are particularly limited owing to the loss of follow-up from individuals and even more importantly from entire clusters when using restricted randomisation methods such as matching, which could suppose a break in the pairs of randomised clusters. To avoid this limitation, possible missing data will be minimised by a careful trial management of the PC professionals involved as cluster guardians and by attempting to follow-up all study participants.77 139 The long follow-up period could turn out to be an added difficulty when trying to evaluate all the participants at 1 year after the intervention—no outcome data will be collected for participants who do not complete follow-up. Nevertheless, with the assistance of the cluster guardians, efforts will be made to maintain low drop-out rates—ideally in the range of 20%—to reduce this possible limitation. We will also be cautious regarding ‘breaking the matching’ when determining the possible impact of baseline covariates on the intervention effect, because it might increase type I error.159
Possible subsequent difficulties might be those derived from the fact that the sample size has been estimated based on foreign studies,72 because there have previously been no similar publications in the Spanish context. Another limitation is that the intervention will be located only in the city of Zaragoza (located in the north-east of Spain), without having the possibility to expand the study area. In this respect, the low number of PC health centres playing the role of clusters is likely to underestimate standard errors, something that might lead to type I error increases, even using analyses that are prepared to account for clustering. Thus, we will have to be aware of whether observed standard errors tend to exaggerate the significance of results.147 Nevertheless, because we will model non-compliance and clustering in the CACE analysis, we will be able to reduce variance inflation due to the interaction between the two.
On the other hand, the measurement of different types of outcomes, using self-report instruments and anthropometric and vital signs measures, as well as blood tests, will be a strength of the present study, thus overcoming possible response biases. Furthermore, the exclusion criteria established, although may favour group functioning and patient safety, might also limit the range of potential affective symptoms and EE, which is likely to have implications for results. Finally, the fact that the instructor-led ME intervention is conducted in a group setting creates a particular context that could potentially introduce significant biases related to attention and support that are not present in the same way in other forms of treatment delivery, such as individual face-to-face treatments or online psychotherapies.
Ethical aspects
Written informed consent will be obtained from the participants before they are aware of the group to which they are allocated. Patients will be informed with a detailed overview of the aims and characteristics of the study and the intervention arms, and also that all participants will be free to withdraw from the study at any time, before they provide their consent. As mentioned above, patients in the TAU arm will be allowed to partake in the psychological intervention programme at the end of the study for ethical reasons—they will be informed of this possibility after the 1-year follow-up measure to avoid the intrusion of possible expectations that might affect the development of the programme, level of participation or outcomes.
The study has been developed according to national and international standards, for example, Declaration of Helsinki, Tokyo Convention and the corresponding later amendments. The data will be treated anonymously and will only be used for purposes related to the study. The limits to fully guarantee confidentiality and privacy of the participants included in the study will rely on Fair Information Practice Principles (FIPPS)160—that is, openness and transparency, purpose specification, collection limitation and data minimisation, use limitation, individual participation and control, data quality and integrity, security safeguards and controls, accountability and oversight—and will be in accordance with the ethical standards laid out in the EU General Data Protection Regulation regime as well as the Spanish Organic Law on Protection of Personal Data and Guarantee of Digital Rights, ensuring that the responsibility for protecting data privacy rests primarily on the data holders. If the necessity of fulfilling the objectives of the CRT creates a scenario that could lead to a break in the total compliance with confidentiality, the FIPPS principles in accordance with the ethical standards referred above will ensure a framework of privacy, autonomy and respect for the participants that will minimise the breach of the confidence and in turn the possibility of error due to low quality of data.161 In cases of adverse events or unintended effects, the DMC will be responsible for ensuring anonymity.
The research team will only have access to the numerical data of the results of the previously established tests derived from blood samples. Blood samples will be handled on a regular basis from the PC consultations and according to the regulation of the Spanish Royal Decree 1277/2003. This study protocol has been approved by the Research Ethics Committee of the regional authority (CEICA Aragon, Spain registry number PI19/086). Any important modification of the protocol will be immediately communicated to this committee by both letter and email. Publication authorship of the final trial report will be based on making substantial contributions according to published scholarly work in medical journals.162
Supplementary Material
Acknowledgments
The authors would like to thank the support received by the Aragon Health Research Institute (IIS), and they are also grateful to the Prevention and Promotion of Health Network in Primary Care (RD16/0007/0005) of the Carlos III Health Institute of the Ministry of Economy and Competitiveness of Spain.
Footnotes
Collaborators: Dharamsala Institute of Mindfulness and Psychotherapy, Zaragoza (Spain).
Contributors: HMS, JG-C, JM-M, and MN-G participated in the design and planning of the intervention evaluated here. HMS, JM-M and JG-C coordinated all the processes. JM-M designed the methods section and statistical analyses protocol. AB-S was in charge of the protocol registration. JM-M and HMS prepared the first draft of the manuscript. PH-M and BP collaborated in the editing of the final manuscript. All authors have read and corrected draft versions and approved the final version of this document.
Funding: The project received funding from the DGA group (B17-17R) and the Network for Prevention and Health Promotion in Primary Care (REDIAPP) grant from the Carlos III Health Institute of the Spanish Ministry of Economy and Competitiveness, cofinanced by European Union ERDF funds (RD16/0007/0005). The funding sources have no influence on the study design; collection, management, analysis and interpretation of the data; writing of the report and the decision to submit the report for publication; and they will have no authority over any of these activities in the trial development.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: Approval was obtained from the Ethics Committee of the corresponding regional authority (CEICA Aragon, Spain registry number PI19/086).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. World Health Organization Obesity : preventing and managing the global epidemic : report of a WHO consultation. World Health Organization, 2000. [PubMed] [Google Scholar]
- 2. Organización Mundial de la Salud Informe sobre La situación mundial de las Enfermedades no transmisibles 2014.
- 3. Rössner S. Obesity: the disease of the twenty-first century. Int J Obes 2002;26:S2–4. 10.1038/sj.ijo.0802209 [DOI] [PubMed] [Google Scholar]
- 4. Rush E, Yan M. Evolution not revolution: nutrition and obesity. Nutrients 2017;9:519 10.3390/nu9050519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pi-Sunyer X. The medical risks of obesity. Postgrad Med 2009;121:21–33. 10.3810/pgm.2009.11.2074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nyberg ST, Batty GD, Pentti J, et al. Obesity and loss of disease-free years owing to major non-communicable diseases: a multicohort study. The Lancet Public Health 2018;3:e490–7. 10.1016/S2468-2667(18)30139-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gómez Candela C. Estrategia mundial sobre régimen alimentario, actividad física Y salud. In: Nutricion Clinica y Dietetica Hospitalaria, 2004: 10–13. [Google Scholar]
- 8. Cinza Sanjurjo S, MÁ PD, Llisterri Caro JL, et al. Prevalencia de obesidad Y comorbilidad cardiovascular asociada en Los pacientes incluidos en El estudio IBERICAN (Identificación de la poBlación Española de RIesgo cardiovascular Y reNal). Med Fam Semer 2018. online. [DOI] [PubMed] [Google Scholar]
- 9. Chauvet-Gelinier J-C, Roussot A, Cottenet J, et al. Depression and obesity, data from a national administrative database study: geographic evidence for an epidemiological overlap. PLoS One 2019;14:e0210507 10.1371/journal.pone.0210507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Huang Q, Liang X, Wang S, et al. Association between body mass index and migraine: a survey of adult population in China. Behav Neurol 2018;2018:1–6. 10.1155/2018/6585734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Arrieta F, Iglesias P, Pedro-Botet J, et al. Diabetes mellitus Y riesgo cardiovascular. Actualización de las recomendaciones del Grupo de Trabajo de diabetes Y Riesgo cardiovascular de la Sociedad Española de diabetes (SED, 2018). Clínica e Investigación en Arteriosclerosis 2018;30:137–53. 10.1016/j.arteri.2018.03.002 [DOI] [PubMed] [Google Scholar]
- 12. Salvatore Benito A, MÁ VZ, Alarza Cano M, et al. Adherencia a la dieta mediterránea: comparación entre pacientes Con cáncer de cabeza Y cuello Y población sana. Endocrinol Diabetes y Nutr 2019. online. [DOI] [PubMed] [Google Scholar]
- 13. Moreno Aznar LA. Situaciones Fisiológicas Y etapas de la vida: Adolescencia. 607 In: Libro Blanco de la Nutrición en España, 2013. [Google Scholar]
- 14. Papandreou C, Mourad TA, Jildeh C, et al. Obesity in Mediterranean region (1997-2007): a systematic review. Obes Rev 2008;9:389–99. 10.1111/j.1467-789X.2007.00466.x [DOI] [PubMed] [Google Scholar]
- 15. Musaiger AO. Overweight and obesity in eastern Mediterranean region: prevalence and possible causes. J Obes 2011;2011:1–17. 10.1155/2011/407237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sanz-Valero J, Guardiola-Wanden-Berghe R, Wanden-Berghe C. Appropriateness and Adequacy of the Keywords Listed in Papers Published in Eating Disorders Journals Indexed Using the MEDLINE Database. In: Advanced Biomedical Engineering. InTech 2011. [Google Scholar]
- 17. Nota Técnica Encuesta Nacional de Salud España 2017 Principales resultados 2017.
- 18. Centro Nacional de Información de Ciencias Médicas. M, Borroto Díaz G. Revista cubana de investigaciones biomédicas. Centro Nacional de Información de Ciencias Médicas, Ministerio de Salud Pública 1982. [Google Scholar]
- 19. Martin E. Diagnóstico de la obesidad. n.d. Rev Salud y bienestar, 2017. Available: https://www.webconsultas.com/obesidad/diagnostico-de-la-obesidad-653
- 20. Elliott EJ. Dietas de bajo índice glucémico O Baja carga glucémica para El sobrepeso Y La obesidad. Bibl Cochrane Plus 2007;4. [Google Scholar]
- 21. Agha M, Agha R. The rising prevalence of obesity: Part A: impact on public health. Int J surgery Oncol 2017;2:e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rubio MA, Salas-Salvadó J, Barbany M, et al. Consenso SEEDO 2007 para La evaluación del sobrepeso Y La obesidad Y El establecimiento de criterios de intervención terapéutica. Rev Española Obes 2007;52. [DOI] [PubMed] [Google Scholar]
- 23. Yumuk V, Tsigos C, Fried M, et al. European guidelines for obesity management in adults. Obes Facts 2015;8:402–24. 10.1159/000442721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Thomas D, Elliott EJ, index Lglycaemic. Or low glycaemic load, diets for diabetes mellitus. Cochrane Database Syst Rev 2009:CD006296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bersh S. La obesidad: aspectos psicológicos Y conductuales. Rev Colomb Psiquiatr 2006;25:537–46. [Google Scholar]
- 26. Brolin RE, Kenler HA, Gorman JH, et al. Long-limb gastric bypass in the superobese. A prospective randomized study. Ann Surg 1992;215:387–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Raman J, Hay P, Tchanturia K, et al. A randomised controlled trial of manualized cognitive remediation therapy in adult obesity. Appetite 2018;123:269–79. 10.1016/j.appet.2017.12.023 [DOI] [PubMed] [Google Scholar]
- 28. Rogers JM, Ferrari M, Mosely K, et al. Mindfulness-based interventions for adults who are overweight or obese: a meta-analysis of physical and psychological health outcomes. Obesity Reviews 2017;18:51–67. 10.1111/obr.12461 [DOI] [PubMed] [Google Scholar]
- 29. Carrière K, Khoury B, Günak MM, et al. Mindfulness-based interventions for weight loss: a systematic review and meta-analysis. Obesity Reviews 2018;19:164–77. 10.1111/obr.12623 [DOI] [PubMed] [Google Scholar]
- 30. Rand C, Stunkard AJ. Obesity and psychoanalysis. Am J Psychiatry 1978;135:547–51. [DOI] [PubMed] [Google Scholar]
- 31. Stradling J, Roberts D, Wilson A, et al. Controlled trial of hypnotherapy for weight loss in patients with obstructive sleep apnoea. Int J Obes 1998;22:278–81. 10.1038/sj.ijo.0800578 [DOI] [PubMed] [Google Scholar]
- 32. Mann T, Tomiyama AJ, Westling E, et al. Medicare's search for effective obesity treatments: diets are not the answer. Am Psychol 2007;62:220–33. 10.1037/0003-066X.62.3.220 [DOI] [PubMed] [Google Scholar]
- 33. Bohrer BK, Forbush KT, Hunt TK. Are common measures of dietary restraint and disinhibited eating reliable and valid in obese persons? Appetite 2015;87:344–51. 10.1016/j.appet.2014.12.226 [DOI] [PubMed] [Google Scholar]
- 34. Hendrickson KL, Rasmussen EB. Mindful eating reduces impulsive food choice in adolescents and adults. Health Psychol 2017;36:226–35. 10.1037/hea0000440 [DOI] [PubMed] [Google Scholar]
- 35. Ogden J, Coop N, Cousins C, et al. Distraction, the desire to eat and food intake. towards an expanded model of mindless eating. Appetite 2013;62:119–26. 10.1016/j.appet.2012.11.023 [DOI] [PubMed] [Google Scholar]
- 36. Mason AE, Epel ES, Kristeller J, et al. Effects of a mindfulness-based intervention on mindful eating, sweets consumption, and fasting glucose levels in obese adults: data from the shine randomized controlled trial. J Behav Med 2016;39:201–13. 10.1007/s10865-015-9692-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kristeller JL, Wolever RQ. Mindfulness-Based Eating Awareness Training for Treating Binge Eating Disorder : The Conceptual Foundation Mindfulness-Based Eating Awareness Training for Treating Binge Eating Disorder : The Conceptual Foundation 2011:37–41. [DOI] [PubMed]
- 38. Warren JM, Smith N, Ashwell M. A structured literature review on the role of mindfulness, mindful eating and intuitive eating in changing eating behaviours: effectiveness and associated potential mechanisms. Nutr Res Rev 2017;30:272–83. 10.1017/S0954422417000154 [DOI] [PubMed] [Google Scholar]
- 39. Miller CK, Kristeller JL, Headings A, et al. Comparison of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes. Health Educ Behav 2014;41:145–54. 10.1177/1090198113493092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Dalen J, Smith BW, Shelley BM, et al. Pilot study: mindful eating and living (meal): weight, eating behavior, and psychological outcomes associated with a mindfulness-based intervention for people with obesity. Complement Ther Med 2010;18:260–4. 10.1016/j.ctim.2010.09.008 [DOI] [PubMed] [Google Scholar]
- 41. Hendrickson KL, Rasmussen EB. Effects of mindful eating training on delay and probability discounting for food and money in obese and healthy-weight individuals. Behav Res Ther 2013;51:399–409. 10.1016/j.brat.2013.04.002 [DOI] [PubMed] [Google Scholar]
- 42. Kristeller JL, Hallett CB. An exploratory study of a Meditation-based intervention for binge eating disorder. J Health Psychol 1999;4:357–63. 10.1177/135910539900400305 [DOI] [PubMed] [Google Scholar]
- 43. Rosenzweig S, Reibel DK, Greeson JM, et al. Mindfulness-based stress reduction is associated with improved glycemic control in type 2 diabetes mellitus: a pilot study. Altern Ther Health Med 2007;13:36–8. [PubMed] [Google Scholar]
- 44. Miller CK, Kristeller JL, Headings A, et al. Comparative effectiveness of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: a pilot study. J Acad Nutr Diet 2012;112:1835–42. 10.1016/j.jand.2012.07.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Fanning J, Osborn CY, Lagotte AE, et al. Relationships between dispositional mindfulness, health behaviors, and hemoglobin A1c among adults with type 2 diabetes. J Behav Med 2018;41:798–805. 10.1007/s10865-018-9938-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Medina W, Wilson D, de Salvo V, et al. Effects of mindfulness on diabetes mellitus: rationale and overview. Curr Diabetes Rev 2017;13:141–7. 10.2174/1573399812666160607074817 [DOI] [PubMed] [Google Scholar]
- 47. Kristeller J, Wolever RQ, Sheets V. Mindfulness-Based eating awareness training (MB-EAT) for binge eating: a randomized clinical trial. Mindfulness 2014;5:282–97. 10.1007/s12671-012-0179-1 [DOI] [Google Scholar]
- 48. Mason AE, Epel ES, Aschbacher K, et al. Reduced reward-driven eating accounts for the impact of a mindfulness-based diet and exercise intervention on weight loss: data from the shine randomized controlled trial. Appetite 2016;100:86–93. 10.1016/j.appet.2016.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Katterman SN, Kleinman BM, Hood MM, et al. Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: a systematic review. Eat Behav 2014;15:197–204. 10.1016/j.eatbeh.2014.01.005 [DOI] [PubMed] [Google Scholar]
- 50. Frayn M, Livshits S, Knäuper B. Emotional eating and weight regulation: a qualitative study of compensatory behaviors and concerns. J Eat Disord 2018;6 10.1186/s40337-018-0210-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. van Strien T. Causes of emotional eating and matched treatment of obesity. Curr Diab Rep 2018;18:35 10.1007/s11892-018-1000-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Stojek MMK, Tanofsky-Kraff M, Shomaker LB, et al. Associations of adolescent emotional and loss of control eating with 1-year changes in disordered eating, weight, and adiposity. Int J Eat Disord 2017;50:551–60. 10.1002/eat.22636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Braden A, Flatt SW, Boutelle KN, et al. Emotional eating is associated with weight loss success among adults enrolled in a weight loss program. J Behav Med 2016;39:727–32. 10.1007/s10865-016-9728-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Godsey J. The role of mindfulness based interventions in the treatment of obesity and eating disorders: an integrative review. Complement Ther Med 2013;21:430–9. 10.1016/j.ctim.2013.06.003 [DOI] [PubMed] [Google Scholar]
- 55. Mantzios M, Wilson JC. Mindfulness, eating behaviours, and obesity: a review and reflection on current findings. Curr Obes Rep 2015;4:141–6. 10.1007/s13679-014-0131-x [DOI] [PubMed] [Google Scholar]
- 56. Guendelman S, Medeiros S, Rampes H. Mindfulness and emotion regulation: insights from neurobiological, psychological, and clinical studies. Front Psychol 2017;8:220 10.3389/fpsyg.2017.00220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Lorenz E, Köpke S, Pfaff H, et al. Cluster-Randomized studies. Dtsch Arztebl Int 2018;115:163–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Chan A-W, Tetzlaff JM, Altman DG, et al. Spirit 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med 2013;158:200 10.7326/0003-4819-158-3-201302050-00583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Ayuntamiento de Zaragoza Datos Demograficos Padron municipal. Zaragoza, 2018. [Google Scholar]
- 60. Hagströmer M, Oja P, Sjöström M. The International physical activity questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr 2006;9:755–62. [DOI] [PubMed] [Google Scholar]
- 61. Tur JA, Romaguera D, Pons A. The diet quality Index-International (DQI-I): is it a useful tool to evaluate the quality of the Mediterranean diet? Br J Nutr 2005;93:369–76. 10.1079/BJN20041363 [DOI] [PubMed] [Google Scholar]
- 62. Gouveia MJ, Canavarro MC, Moreira H. Is Mindful Parenting Associated With Adolescents’ Emotional Eating? The Mediating Role of Adolescents’ Self-Compassion and Body Shame. Front Psychol 2004;2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Salvo V, Kristeller J, Montero Marin J, et al. Mindfulness as a complementary intervention in the treatment of overweight and obesity in primary health care: study protocol for a randomised controlled trial. Trials 2018;19:277 10.1186/s13063-018-2639-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Mason AE, Saslow L, Moran PJ, et al. Examining the effects of mindful eating training on adherence to a Carbohydrate-Restricted diet in patients with type 2 diabetes (the DELISH study): protocol for a randomized controlled trial. JMIR Res Protoc 2019;8:e11002 10.2196/11002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Van Dam NT, van Vugt MK, Vago DR, et al. Reiterated concerns and further challenges for mindfulness and meditation research: a reply to Davidson and Dahl. Perspect Psychol Sci 2018;13:66–9. 10.1177/1745691617727529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. da Luz F, Hay P, Touyz S, et al. Obesity with comorbid eating disorders: associated health risks and treatment approaches. Nutrients 2018;10:829 10.3390/nu10070829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Kuijpers HJH, van der Heijden FMMA, Tuinier S, et al. Meditation-Induced psychosis. Psychopathology 2007;40:461–4. 10.1159/000108125 [DOI] [PubMed] [Google Scholar]
- 68. Swinbourne J, Hunt C, Abbott M, et al. The comorbidity between eating disorders and anxiety disorders: prevalence in an eating disorder sample and anxiety disorder sample. Aust N Z J Psychiatry 2012;46:118–31. 10.1177/0004867411432071 [DOI] [PubMed] [Google Scholar]
- 69. Martinussen M, Friborg O, Schmierer P, et al. The comorbidity of personality disorders in eating disorders: a meta-analysis. Eat Weight Disord 2017;22:201–9. 10.1007/s40519-016-0345-x [DOI] [PubMed] [Google Scholar]
- 70. Cecchini M, Sassi F, Lauer JA, et al. Tackling of unhealthy diets, physical inactivity, and obesity: health effects and cost-effectiveness. The Lancet 2010;376:1775–84. 10.1016/S0140-6736(10)61514-0 [DOI] [PubMed] [Google Scholar]
- 71. Hauner H, Bramlage P, Lösch C, et al. Prevalence of obesity in primary care using different anthropometric measures – results of the German metabolic and cardiovascular risk project (GEMCAS). BMC Public Health 2008;8:282 10.1186/1471-2458-8-282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Alberts HJEM, Thewissen R, Raes L. Dealing with problematic eating behaviour. The effects of a mindfulness-based intervention on eating behaviour, food cravings, dichotomous thinking and body image concern. Appetite 2012;58:847–51. 10.1016/j.appet.2012.01.009 [DOI] [PubMed] [Google Scholar]
- 73. Hemming K, Eldridge S, Forbes G, et al. How to design efficient cluster randomised trials. BMJ 2017;358 10.1136/bmj.j3064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Hemming K, Girling AJ, Sitch AJ, et al. Sample size calculations for cluster randomised controlled trials with a fixed number of clusters. BMC Med Res Methodol 2011;11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Hooper R, Teerenstra S, de Hoop E, et al. Sample size calculation for stepped wedge and other longitudinal cluster randomised trials. Stat Med 2016;35:4718–28. 10.1002/sim.7028 [DOI] [PubMed] [Google Scholar]
- 76. Nam S, Toneatto T. The influence of attrition in evaluating the efficacy and effectiveness of Mindfulness-Based interventions. Int J Ment Health Addict 2016;14:969–81. 10.1007/s11469-016-9667-1 [DOI] [Google Scholar]
- 77. Giraudeau B, Ravaud P. Preventing bias in cluster randomised trials. PLoS Med 2009;6:e1000065 10.1371/journal.pmed.1000065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Puffer S, Torgerson D, Watson J. Evidence for risk of bias in cluster randomised trials: review of recent trials published in three general medical journals. BMJ 2003;327:785–9. 10.1136/bmj.327.7418.785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Campbell MJ, Donner A, Klar N. Developments in cluster randomized trials andStatistics in medicine. Stat Med 2007;26:2–19. 10.1002/sim.2731 [DOI] [PubMed] [Google Scholar]
- 80. Newton S, Braithwaite D, Akinyemiju TF. Socio-Economic status over the life course and obesity: systematic review and meta-analysis. PLoS One 2017;12:e0177151 10.1371/journal.pone.0177151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Heraclides A, Brunner E. Social mobility and social accumulation across the life course in relation to adult overweight and obesity: the Whitehall II study. J Epidemiol Community Heal 2010;64:714–9. 10.1136/jech.2009.087692 [DOI] [PubMed] [Google Scholar]
- 82. Spears CA, Houchins SC, Bamatter WP, et al. Perceptions of mindfulness in a low-income, primarily African American treatment-seeking sample. Mindfulness 2017;8:1532–43. 10.1007/s12671-017-0720-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Therneau TM. How many stratification factors are “too many” to use in a randomization plan? Control Clin Trials 1993;14:98–108. 10.1016/0197-2456(93)90013-4 [DOI] [PubMed] [Google Scholar]
- 84. Martin DC, Diehr P, Perrin EB, et al. The effect of matching on the power of randomized community intervention studies. Stat Med 1993;12:329–38. 10.1002/sim.4780120315 [DOI] [PubMed] [Google Scholar]
- 85. Donner A, Klar N. Pitfalls of and controversies in cluster randomization trials. Am J Public Health 2004;94:416–22. 10.2105/AJPH.94.3.416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Diez-Quevedo C, Rangil T, Sanchez-Planell L, et al. Validation and utility of the patient health questionnaire in diagnosing mental disorders in 1003 General Hospital Spanish inpatients. Psychosom Med 2001;63:679–86. 10.1097/00006842-200107000-00021 [DOI] [PubMed] [Google Scholar]
- 87. Kristeller JL, Wolever RQ. Mindfulness-Based eating awareness training for treating binge eating disorder: the conceptual Foundation. Eat Disord 2010;19:49–61. 10.1080/10640266.2011.533605 [DOI] [PubMed] [Google Scholar]
- 88. Chozen J, Wilkins C. Mindful eating conscious living. n.d. Available: https://me-cl.com/
- 89. The Center for Mindful Eating Home. n.d. Available: https://www.thecenterformindfuleating.org/
- 90. García Campayo J, Morillo H, López Montoyo A, et al. Mindful eating: el sabor de la atención. Siglantana, 2017. [Google Scholar]
- 91. Ducht Committee on test and testing. COTAN. Review Ducht Eating Behavior Questionnaire 2013. www.cotandocumentatie.nl/test_details.php?id=848 [Google Scholar]
- 92. Henderson M, Freeman CPL. A Self-rating Scale for Bulimia the ‘BITE’. Br J Psychiatry 1987;150:18–24. 10.1192/bjp.150.1.18 [DOI] [PubMed] [Google Scholar]
- 93. Garner DM, Olmsted MP, Bohr Y, et al. The eating attitudes test: psychometric features and clinical correlates. Psychol Med 1982;12:871–8. 10.1017/S0033291700049163 [DOI] [PubMed] [Google Scholar]
- 94. Jordan P, Shedden-Mora MC, Löwe B. Psychometric analysis of the generalized anxiety disorder scale (GAD-7) in primary care using modern item response theory. PLoS One 2017;12:e0182162 10.1371/journal.pone.0182162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Herr NR, Williams JW, Benjamin S, et al. Does this patient have generalized anxiety or panic disorder? JAMA 2014;312 10.1001/jama.2014.5950 [DOI] [PubMed] [Google Scholar]
- 96. Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the patient health questionnaire (PHQ-9): a meta-analysis. Can Med Assoc J 2012;184:E191–6. 10.1503/cmaj.110829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Kroenke K, Spitzer RL, Williams JBW, et al. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med 2007;146:317–25. 10.7326/0003-4819-146-5-200703060-00004 [DOI] [PubMed] [Google Scholar]
- 98. Gilbody S, Richards D, Brealey S, et al. Screening for depression in medical settings with the patient health questionnaire (PHQ): a diagnostic meta-analysis. J Gen Intern Med 2007;22:1596–602. 10.1007/s11606-007-0333-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Wittkampf K, van Ravesteijn H, Baas K, et al. The accuracy of patient health Questionnaire-9 in detecting depression and measuring depression severity in high-risk groups in primary care. Gen Hosp Psychiatry 2009;31:451–9. 10.1016/j.genhosppsych.2009.06.001 [DOI] [PubMed] [Google Scholar]
- 100. Kroenke K, Spitzer RL, Williams JBW, et al. The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry 2010;32:345–59. 10.1016/j.genhosppsych.2010.03.006 [DOI] [PubMed] [Google Scholar]
- 101. Strachan SM, Bean C, Jung ME. 'I'm on the train and I can't stop it': Western Canadians' reactions to prediabetes and the role of self-compassion. Health Soc Care Community 2018;26:979–87. 10.1111/hsc.12628 [DOI] [PubMed] [Google Scholar]
- 102. Bishop SR, Lau M, Shapiro S, et al. Mindfulness: a proposed operational definition. Clin Psychol Sci Pract 2006;11:230–41. 10.1093/clipsy.bph077 [DOI] [Google Scholar]
- 103. Elices M, Carmona C, Narváez V, et al. Direct experience while eating: laboratory outcomes among individuals with eating disorders versus healthy controls. Eat Behav 2017;27:23–6. 10.1016/j.eatbeh.2017.10.002 [DOI] [PubMed] [Google Scholar]
- 104. Camilleri GM, Méjean C, Bellisle F, et al. Association between mindfulness and weight status in a general population from the NutriNet-Santé study. PLoS One 2015;10:e0127447 10.1371/journal.pone.0127447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Soler J, Soriano J, Ferraz L, et al. Direct experience and the course of eating disorders in patients on partial hospitalization: a pilot study. Eur. Eat. Disorders Rev. 2013;21:399–404. 10.1002/erv.2224 [DOI] [PubMed] [Google Scholar]
- 106. Allirot X, Miragall M, Perdices I, et al. Effects of a brief mindful eating induction on food choices and energy intake: external eating and mindfulness state as Moderators. Mindfulness 2018;9:750–60. 10.1007/s12671-017-0812-0 [DOI] [Google Scholar]
- 107. Mantzios M, Egan H, Bahia H, et al. How does grazing relate to body mass index, self-compassion, mindfulness and mindful eating in a student population? Health Psychology Open 2018;5 10.1177/2055102918762701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Neff K. Self-Compassion: an alternative conceptualization of a healthy attitude toward Oneself. Self and Identity 2003;2:85–101. 10.1080/15298860309032 [DOI] [Google Scholar]
- 109. Adams CE, Leary MR. Promoting Self–Compassionate attitudes toward eating among restrictive and guilty Eaters. J Soc Clin Psychol 2007;26:1120–44. 10.1521/jscp.2007.26.10.1120 [DOI] [Google Scholar]
- 110. Mantzios M, Wilson JC. Exploring mindfulness and mindfulness with Self-Compassion-Centered interventions to assist weight loss: theoretical considerations and preliminary results of a randomized pilot study. Mindfulness 2015;6:824–35. 10.1007/s12671-014-0325-z [DOI] [Google Scholar]
- 111. Mantzios M, Wilson JC, Linnell M, et al. The role of negative cognition, intolerance of uncertainty, mindfulness, and Self-Compassion in weight regulation among male Army recruits. Mindfulness 2015;6:545–52. 10.1007/s12671-014-0286-2 [DOI] [Google Scholar]
- 112. Cebolla A, Barrada JR, van Strien T, et al. Validation of the Dutch eating behavior questionnaire (DEBQ) in a sample of Spanish women. Appetite 2014;73:58–64. 10.1016/j.appet.2013.10.014 [DOI] [PubMed] [Google Scholar]
- 113. Van Strien T, Schippers GM, Cox WM. On the relationship between emotional and external eating behavior. Addict Behav 1995;20:585–94. 10.1016/0306-4603(95)00018-8 [DOI] [PubMed] [Google Scholar]
- 114. van Strien T, Frijters JER, Bergers GPA, et al. The Dutch eating behavior questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int. J. Eat. Disord. 1986;5:295–315. [DOI] [Google Scholar]
- 115. Moya TR, Bersabé R, Jiménez M. Fiabilidad Y validez del test de Investigación Bulímica de Edimburgo (bite) en Una muestra de adolescentes españoles. = reliability and validity of bulimic Investigatory test, Edinburgh (bite) in a sample of Spanish adolescents. Psicol Conduct Rev Int Psicol Clínica la Salud 2004;12:447–61. [Google Scholar]
- 116. Orlandi E, Mannucci E, Cuzzolaro M, et al. Bulimic Investigatory test, Edinburgh (bite). A validation study of the Italian version. Eat Weight Disord 2005;10:e14–20. 10.1007/BF03354662 [DOI] [PubMed] [Google Scholar]
- 117. Daniel Le Grange JL. ed). Eating Disorders in Children and Adolescents: A Clinical Handbook. New York 2001. [Google Scholar]
- 118. Gandarillas A, Zorrilla B, Munoz P, et al. Validez del eating attitudes test (EAT-26) para cribado de Trastornos del comportamiento alimentario. Gac Sanit 2002;1:40–2. [Google Scholar]
- 119. Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder. Arch Intern Med 2006;166:1092 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 120. American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders. 5th ed, 2013. [Google Scholar]
- 121. García-Campayo J, Zamorano E, Ruiz MA, et al. Cultural adaptation into Spanish of the generalized anxiety disorder-7 (GAD-7) scale as a screening tool. Health Qual Life Outcomes 2010;8:8 10.1186/1477-7525-8-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Arrieta J, Aguerrebere M, Raviola G, et al. Validity and Utility of the Patient Health Questionnaire (PHQ)-2 and PHQ-9 for Screening and Diagnosis of Depression in Rural Chiapas, Mexico: A Cross-Sectional Study. J Clin Psychol 2017;73:1076–90. 10.1002/jclp.22390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Tomitaka S, Kawasaki Y, Ide K, et al. Distributional patterns of item responses and total scores on the PHQ-9 in the general population: data from the National health and nutrition examination survey. BMC Psychiatry 2018;18:108 10.1186/s12888-018-1696-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Bohlmeijer E, ten Klooster PM, Fledderus M, et al. Psychometric properties of the five facet mindfulness questionnaire in depressed adults and development of a short form. Assessment 2011;18:308–20. 10.1177/1073191111408231 [DOI] [PubMed] [Google Scholar]
- 126. Á A-M, Masluk B, Montero-Marin J, et al. Validation of five facets mindfulness questionnaire – short form, in Spanish, general health care services patients sample: prediction of depression through mindfulness scale. PLoS One 2019;14:e0214503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Mantzios M, Mindfulness WJC, Behaviours E. And obesity: a review and reflection on current findings. Curr Obes Rep 2015;4:141–6. [DOI] [PubMed] [Google Scholar]
- 128. Hulbert-Williams L, Nicholls W, Joy J, et al. Initial validation of the mindful eating scale. Mindfulness 2014;5:719–29. 10.1007/s12671-013-0227-5 [DOI] [Google Scholar]
- 129. Neff KD, Tóth-Király I, Yarnell LM, et al. Examining the factor structure of the Self-Compassion scale in 20 diverse samples: support for use of a total score and six subscale scores. Psychol Assess 2019;31:27–45. 10.1037/pas0000629 [DOI] [PubMed] [Google Scholar]
- 130. Garcia-Campayo J, Navarro-Gil M, Andrés E, et al. Validation of the Spanish versions of the long (26 items) and short (12 items) forms of the Self-Compassion scale (scs). Health Qual Life Outcomes 2014;12:4 10.1186/1477-7525-12-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Lindahl JR, Fisher NE, Cooper DJ, et al. The varieties of contemplative experience: a mixed-methods study of meditation-related challenges in Western Buddhists. PLoS One 2017;12:e0176239 10.1371/journal.pone.0176239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Moher D, Hopewell S, Schulz KF, et al. Consort 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c869 10.1136/bmj.c869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Moher D, Schulz KF, Altman DG, et al. The CONSORT statement: revised recommendations for improving the quality of reports of parallel group randomized trials. BMC Med Res Methodol 2001;1:2 10.1186/1471-2288-1-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. de Boer MR, Waterlander WE, Kuijper LDJ, et al. Testing for baseline differences in randomized controlled trials: an unhealthy research behavior that is hard to eradicate. Int J Behav Nutr Phys Act 2015;12 10.1186/s12966-015-0162-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Egbewale BE, Lewis M, Sim J. Bias, precision and statistical power of analysis of covariance in the analysis of randomized trials with baseline imbalance: a simulation study. BMC Med Res Methodol 2014;14:49 10.1186/1471-2288-14-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Morris SB. Estimating effect sizes from Pretest-Posttest-Control group designs. Organ Res Methods 2008;11:364–86. 10.1177/1094428106291059 [DOI] [Google Scholar]
- 137. Cohen J. Statistical power analysis for the behavioral sciences second edition. 2nd ed Lawrence Erlbaum Associates, 1988. [Google Scholar]
- 138. Twisk J, de Boer M, de Vente W, et al. Multiple imputation of missing values was not necessary before performing a longitudinal mixed-model analysis. J Clin Epidemiol 2013;66:1022–8. 10.1016/j.jclinepi.2013.03.017 [DOI] [PubMed] [Google Scholar]
- 139. White IR, Horton NJ, Carpenter J, et al. Strategy for intention to treat analysis in randomised trials with missing outcome data. BMJ 2011;342:d40 10.1136/bmj.d40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. White IR, Thompson SG. Adjusting for partially missing baseline measurements in randomized trials. Stat Med 2005;24:993–1007. 10.1002/sim.1981 [DOI] [PubMed] [Google Scholar]
- 141. Péneau S, Ménard E, Méjean C, et al. Sex and dieting modify the association between emotional eating and weight status. Am J Clin Nutr 2013;97:1307–13. 10.3945/ajcn.112.054916 [DOI] [PubMed] [Google Scholar]
- 142. Braden A, Musher-Eizenman D, Watford T, et al. Eating when depressed, anxious, bored, or happy: are emotional eating types associated with unique psychological and physical health correlates? Appetite 2018;125:410–7. 10.1016/j.appet.2018.02.022 [DOI] [PubMed] [Google Scholar]
- 143. Pourhoseingholi MA, Baghestani AR, Vahedi M. How to control confounding effects by statistical analysis. Gastroenterol Hepatol from bed to bench 2012;5:79–83. [PMC free article] [PubMed] [Google Scholar]
- 144. Williams R. Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata J 2012;12:308–31. 10.1177/1536867X1201200209 [DOI] [Google Scholar]
- 145. Little RJ, Rubin DB. Causal effects in clinical and epidemiological studies via potential outcomes: concepts and analytical approaches. Annu Rev Public Health 2000;21:121–45. 10.1146/annurev.publhealth.21.1.121 [DOI] [PubMed] [Google Scholar]
- 146. Gu J, Strauss C, Bond R, et al. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin Psychol Rev 2015;37:1–12. 10.1016/j.cpr.2015.01.006 [DOI] [PubMed] [Google Scholar]
- 147. Jo B, Asparouhov T, Muthén BO, et al. Cluster randomized trials with treatment noncompliance. Psychol Methods 2008;13:1–18. 10.1037/1082-989X.13.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. van ST. Nederlandse vragenlijst voor eetgedrag (NVE). Handleiding. (Dutch eating behaviour questionnaire. manual. Hogrefe, 2015: 80. [Google Scholar]
- 149. Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol 1991;59:12–19. 10.1037/0022-006X.59.1.12 [DOI] [PubMed] [Google Scholar]
- 150. Forgione N, Deed G, Kilov G, et al. Managing obesity in primary care: breaking down the barriers. Adv Ther 2018;35:191–8. 10.1007/s12325-017-0656-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Olson KL, Emery CF. Mindfulness and weight loss. Psychosom Med 2015;77:59–67. 10.1097/PSY.0000000000000127 [DOI] [PubMed] [Google Scholar]
- 152. Carrière K, Khoury B, Günak MM, et al. Mindfulness-based interventions for weight loss: a systematic review and meta-analysis. Obes Rev 2018;19:164–77. 10.1111/obr.12623 [DOI] [PubMed] [Google Scholar]
- 153. O'Reilly GA, Cook L, Spruijt-Metz D, et al. Mindfulness-based interventions for obesity-related eating behaviours: a literature review. Obes Rev 2014;15:453–61. 10.1111/obr.12156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Winkens LHH, van Strien T, Brouwer IA, et al. Associations of mindful eating domains with depressive symptoms and depression in three European countries. J Affect Disord 2018;228:26–32. 10.1016/j.jad.2017.11.069 10.1016/j.jad.2017.11.069 [DOI] [PubMed] [Google Scholar]
- 155. Khan Z, Zadeh ZF, Eating SM. and It’s Relationship with Mental Well-Being. Procedia - Soc Behav Sci 2014;159:69–73. [Google Scholar]
- 156. Mattar A, Carlston D, Sariol G, et al. The prevalence of obesity documentation in primary care electronic medical records. are we acknowledging the problem? Appl Clin Inform 2017;8:67–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Stecker T, Sparks S. Prevalence of obese patients in a primary care Setting*. Obesity 2006;14:373–6. 10.1038/oby.2006.49 [DOI] [PubMed] [Google Scholar]
- 158. Gutiérrez Angulo ML, Amenabar Azurmendi MD, Cuesta Solé ML, et al. Prevalencia de la obesidad registrada en Atención Primaria. Endocrinología y Nutrición 2014;61:469–73. 10.1016/j.endonu.2014.03.012 [DOI] [PubMed] [Google Scholar]
- 159. Klar N, Donner A. The merits of matching in community intervention trials: a cautionary tale. Stat Med 1997;16:1753–64. [DOI] [PubMed] [Google Scholar]
- 160. MARKLE COMMON FRAMEWORK CONNECTING Consumers Advancing America’s Future.n.d. Available: https://www.markle.org/health/markle-common-framework/connecting-consumers
- 161. McGraw D, Greene SM, Miner CS, et al. Privacy and confidentiality in pragmatic clinical trials. Clin Trials 2015;12:520–9. 10.1177/1740774515597677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. International Committee of medical Journal editors (ICMJE). Available: http://www.icmje.org [Accessed 2 November 2017].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


