Abstract
Introduction
Swabhimaan is a community-based programme to improve adolescent girls’ and women’s nutrition in the rural areas of three Indian states—Bihar, Chhattisgarh and Odisha with high prevalence of undernutrition.
Methods and analysis
Swabhimaan has a nested prospective, non-randomised controlled evaluation. Since 2017, five intervention sites receive community-led interventions through national government’s livelihood mission supported women’s self-help group federations and five control sites will initiate these activities 36 months later, in 2020. Community-led activities aim to improve coverage of 18 interventions including adequacy of food consumed, prevention of micronutrient deficiencies, access to basic health services and special care of nutritionally ‘at risk’ girls and women, improving hygiene and access to water and sanitation services and access to family planning services. The evaluation includes baseline (2016–2017), midline (2018–2019) and endline (2020–2021) surveys covering 6638 adolescent girls, 2992 pregnant women and 8755 mothers of children under 2. The final impact analysis will be by intention to treat, comparing primary and secondary outcomes in five intervention areas and five control areas. The primary outcomes are: (1) a 15% reduction in the proportion of adolescent girls with a body mass index (BMI) <18.5 kg/m2; (2) a 15% reduction in the proportion of mothers of children under two with a BMI <18.5 kg/m2 and (3) and a 0.4 cm improvement in mean mid-upper arm circumference among pregnant women.
Ethics and dissemination
All procedures involving human subjects were approved by the Institutional Ethics Committee of the All India Institute of Medical Sciences, Bihar, Chhattisgarh and Odisha and in compliance with guidelines laid down in the Declaration of Helsinki. Evidence will inform maternal and preconception nutrition policy at national and state level.
Trial registration number
58261b2f46876 and CTRI/2016/11/007482; Pre-results.
Keywords: adolescent girls, nutrition, agriculture, multi-sector, women collectives, India
Strengths and limitations of this study.
The study will provide evidence on effectiveness of a community-led model in delivering a comprehensive package of 18 nutrition services, on improving nutrition status of adolescent girls, pregnant women and mothers of children under two in resource-poor settings.
The model is based on sustainable government resources with only one of the three states receiving additional non-government funding to test the model.
The pace of implementation will vary considerably across three states due to variable governance, availability of resources, maturity of self-help groups and intensity of non-government engagement which is likely to impact the study outcomes.
While the design includes a comparator site, introduction of new government schemes that can have variable influence in intervention and control sites are not ruled out.
The evaluation is led by an independent third party with no role in implementation of the model.
Introduction
There is compelling evidence on the importance of women’s nutrition prior to and during pregnancy, to ensure optimal fetal growth and development and for the health and well-being of the mother.1 Globally, over 800 000 neonatal deaths and 20% of stunting in children less than 5 years of age is attributable to poor nutrition in utero, including protein-energy and micronutrient deficiencies.2 Nearly 4.5 million Indian women become pregnant in adolescence, 58% have anaemia and 23% are thin. It is unsurprising that over 50 million children under 5 (38%) are stunted.3 4 India has both policies and programmes in place to deliver and monitor globally recommended preconception and antenatal nutrition interventions. Most recently, India’s National Nutrition Mission or Poshan Abhiyaan (2018–2022) aims to reduce the proportion of children born with low birth weight from 19% to 11% and under 5 children stunted from 38% to 13%, by 2022. It also aims to reduce anaemia among adolescent girls and pregnant women, which is over 50%, by 3% per annum. This is to be achieved through coordinated efforts across 11 different ministries that together can make all essential nutrition services available to women and children through integration of their ongoing vertical programmes and schemes.5 Despite these policies and programmes, in 2015–2016, the coverage of at least four antenatal care visits was just over 50%, only one-third of pregnant women consumed iron folic acid (IFA) tablets for at least 100 days during the pregnancy, and less than 40% used the maternity benefit scheme.3 Challenge lies in lack of effective operational models to deliver a comprehensive package of essential nutrition interventions for adolescent girls and women, models that can overcome both systemic challenges and those around user service uptake.
Evidence from randomised controlled trials within and outside India suggests that working with women’s groups as a platform for promoting health interventions and increasing service uptake is a feasible approach in low-resource settings.6–10 This is provided the necessary requisites, such as high-quality facilitators for establishing and maintaining the group, high coverage of intervention, sufficient time for implementation of the intervention, concomitant supply strengthening interventions and appropriate safeguards against harm such as conflict with service providers and domestic violence, are met. However, none of these trials investigated nutrition outcomes for adolescent girls or women.
In view of the undisputed role of income poverty in the aetiology of undernutrition, there is a need to integrate women-centric poverty alleviation in nutrition programmes and vice versa. Notable global examples where women’s collectives have been engaged with to deliver services and promote health and nutrition behaviours in underserved communities, along with economic empowerment include a community conditional cash transfer programme in Indonesia, as well as livelihood and food security programmes in Bangladesh (Shouhardo, Jibaon-o-Jibika) and Nepal (Suaahara).11 12 Indian experiences include Kudumbashree (Kerala), the Society for Elimination of Rural Poverty Project (Andhra Pradesh and Telangana), Self Employed Women’s Association (rural areas of several states), Community Health Care Management Initiative (West Bengal), Jamkhed (Maharashtra) and urban health models by the Urban Health Resource Centre and Mahila Abhivrudhi Society, Andhra Pradesh. Women’s groups are trained on promotion of the health and nutrition interventions, the scope and duration of training varying with the type of programme. The promoting agency, which is mostly a non-government organisation or federated structure of community-based groups, provides capacity building and supervisory support. Most programmes strengthen the health services delivery system in addition to intervening with community groups.13 14
Women’s self-help groups (SHGs) and their federations supported by the Deendayal Antyodaya Yojana-National Rural Livelihoods Mission (DAY-NRLM)’s Government of India’s flagship poverty alleviation programme, remain an untapped platform for improving reach and use of essential nutrition interventions, particularly for women residing in income-constrained settings.15 A 2016 scoping study from UNICEF India suggested that DAY-NRLM village organisations (VOs) have the potential to manage grants for improving last mile delivery of essential nutrition services for women, provided they are enabled, supervised and incentivised.16 DAY-NRLM is also one of the nodal agencies for implementation of the Poshan Abhiyaan. Capitalising on this, the Swabhimaan programme is a 4-year initiative launched in 2016 to improve adolescent girls’ and women’s nutrition.
Swabhimaan is a package of community-led interventions delivered by DAY-NRLM-supported federations of women SHGs comprising VOs and the higher order cluster-level federations (CLFs), to improve the nutrition status of adolescent girls and women in three Indian states: Bihar, Chhattisgarh and Odisha. The objectives of the programme are:
To improve the food and nutrient intake of adolescent girls and women.
To prevent micronutrient deficiencies and nutritional anaemia.
To increase access to services during fixed day, Village Health Sanitation and Nutrition Days (VHSNDs) and provide special care to nutritionally ‘at risk’ women, defined as those with mid-upper arm circumference (MUAC) <23 cm or body mass index (BMI) <18.5 kg/m2.
To increase access to education about water, sanitation and hygiene (WASH) and access to WASH commodities.
To prevent early, poorly spaced and repeated pregnancies.
Methods and analysis
This protocol describes the intervention and evaluation methods for the Swabhimaan programme, which aims to improve the nutrition status of adolescent girls and women in three Indian states: Bihar, Chhattisgarh and Odisha.
Target groups
The primary target groups for the programme are adolescent girls, newlywed women and couples, pregnant women and mothers of children under 2 years of age. Swabhimaan also reaches out to husbands, mothers-in-law and farmer producer groups.
Evaluation design
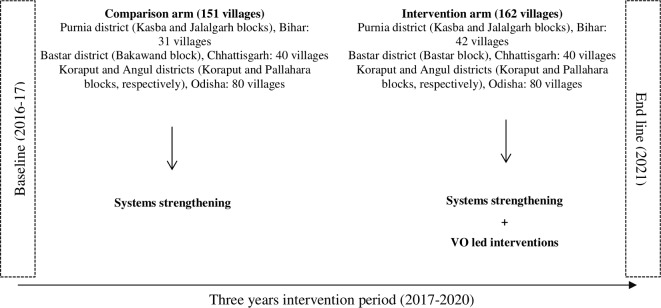
The Swabhimaan evaluation is a prospective, non-randomised controlled study with baseline, midline and endline cross-sectional surveys. Across Bihar, Chhattisgarh and Odisha, five sites covering 162 villages (intervention arm) have been purposively allocated to community-led interventions delivered through VOs and CLFs since 2017, and five sites covering 151 villages (control arm) will initiate these activities 36 months later, in 2020. Both intervention and control sites are located in the poorest areas (also referred to as resource blocks) identified by DAY-NRLM in four districts: Purnia in Bihar, Bastar in Chhattisgarh, and Angul and Koraput in Odisha. In Bihar, within Kasba and Jalalgarh blocks located in Purnia district, we allocated 42 villages to the intervention and 31 villages to control arm. In Chhattisgarh, we allocated 40 villages in Bastar block in Bastar district to intervention and 40 villages in Bakawand block to control. In Odisha, 80 villages within Koraput block in the district of Koraput and Pallahara block in the district of Angul both serve as intervention areas, and 80 more serve as control. The unit of assignment to intervention and control was a cluster of villages in Bihar and Chhattisgarh and a gram panchayat (administrative units of around 5000 population) in Odisha, which was in alignment with NRLM identified administrative boundaries for managing the livelihoods programme in these states (figure 1).
Figure 1.
Evaluation design. VO, village organisation.
Study hypotheses and outcomes
We hypothesise that, over an intervention period of 3 years, Swabhimaan’s community-led interventions will lead to:
A 15% reduction in the proportion of adolescent girls with a BMI <18.5 kg/m2.
A 15% reduction in the proportion of mothers of children under two with a BMI <18.5 kg/m2.
A 0.4 cm improvement in mean MUAC among pregnant women.
These three indicators are considered the evaluation’s primary outcomes. The targets for reduction in proportion of adolescent girls and pregnant women with BMI <18.5 kg/m2 was based on population-based survey data for the selected districts while that for MUAC in pregnancy was based on a rapid assessment undertaken in the intervention sites and the reductions noted in previous research on women’s nutritional status.17 18 We also hypothesise an improvement of between 5% and 20% in the coverage of 18 key nutrition-specific and nutrition-sensitive interventions over 3 years (box 1). These constitute the evaluation’s secondary outcomes.
Box 1. Primary and secondary outcomes for Swabhimaan.
Primary outcomes
Per cent adolescent girls with body mass index <18.5 kg/m2.
Mean mid-upper arm circumference among pregnant women.
Per cent mothers of children under 2 with <18.5 kg/m2.
Secondary outcomes
Adolescent girls (girls aged 10–19)—unmarried, not pregnant and not the mother of a child under 2.
Mean dietary diversity score.
Per cent receiving minimum dietary diversity score (5 of 10 food groups).
Per cent consuming four or more IFA tablets in the month preceding the survey.
Per cent living in a household with iodised salt.
Per cent living in food secure households.
Per cent living in households with a kitchen garden.
Per cent living in households with a toilet or covered pit latrine.
Per cent using safe pads or sanitary pads.
Per cent accessing adolescent health services (Kishori Divas) in 6 months preceding the survey.
Per cent who attended at least three Kishori meetings in 6 months.
Per cent who attended at least three Kishori meetings in in 6 months.
Pregnant women (if she is pregnant, a girl or woman will join this category whether she is an adolescent, newly wed or the mother of any child under 2).
Per cent of pregnant women in the second and third trimester consuming at least 25 IFA tablets in the month preceding the survey.
Mean dietary diversity score.
Per cent receiving minimum dietary diversity (5 out of 10 food groups).
Per cent living in a household with iodised salt.
Per cent living in food secure households.
Per cent living in households with a kitchen garden.
Per cent living in households with a toilet or covered pit latrine.
Per cent receiving Integrated Child Development Services (ICDS) entitlement for supplementary food in month preceding the survey.
Per cent who had one antenatal check-up in the first trimester.
Per cent weighed at least once in first trimester.
Per cent who received one dose of albendazole in second trimester.
Per cent who took two calcium tablets in second trimester.
Per cent below the age of 18.
Per cent who attended at least three Maitri Bethak meetings in 6 months.
Per cent who attended at least three Maitri Bethak meetings in 6 months.
Per cent who attended at least three Village Health Sanitation and Nutrition Days (VHSNDs) in 6 months.
Per cent who attended at least three VHSNDs in 6 months.
Per cent using a modern family planning method (in previous delivery), before the current pregnancy.
Per cent who are members of women’s farmer producer groups and have adopted at least one mix micronutrient-rich cropping methods, against previous practice.
Per cent who are members of women’s farmer producer groups and have adopted at least one pesticide-free agrimethods, against previous practice.
Mothers of children aged under two years
Mean dietary diversity score.
Per cent receiving minimum dietary diversity (5 out of 10 food groups).
Per cent living in a household with iodised salt.
Per cent living in food secure households.
Per cent living in households with a kitchen garden.
Per cent living in households with a toilet or covered pit latrine.
Per cent receiving their minimum Public Distribution System entitlement in month preceding survey.
Per cent receiving ICDS entitlement for supplementary food in month preceding survey.
Per cent who received at least four antenatal care overall in last pregnancy.
Per cent consuming 100 or more IFA tablets during last pregnancy.
Per cent weighed at least four times in last pregnancy.
Per cent using a modern family planning method.
Per cent who accessed at least one of three social protection schemes (JSY, Adarsh Dampati Yojana).
Per cent who delivered in a health facility in last pregnancy.
Per cent who attended at least three Maitri Bethak meetings and three VHSNDs in last year.
Per cent who attended at least three Maitri Bethak meetings and three VHSNDs in last year.
Per cent who are members of women’s farmer producer groups and have adopted at least 1one mix micronutrient-rich cropping methods, against previous practice.
Per cent who are members of women’s farmer producer groups and have adopted at least 1one pesticide-free agrimethods, against previous practice.
Sample size calculation
We conducted state-specific sample size calculations to determine the appropriate number of adolescent girls, pregnant women and mothers of children under 2 to be surveyed to be able to detect achievement of hypothesised targets for primary outcomes (table 1). Sample size accounted for 5% refusal rate and design effect of 1.5. Overall, we estimated that baseline and endline surveys should include a total of 6638 adolescent girls, 10 160 mothers of children under 2 and 2992 pregnant women across the three states.
Table 1.
State-wise estimated total sample in intervention and control areas by target groups
| Bihar | Chhattisgarh | Odisha | Total | |
| Adolescent girls | 1750 | 3294 | 1594 | 6638 |
| Pregnant women | 748 | 1122 | 1122 | 2992 |
| Mothers of children under two | 2846 | 3294 | 4020 | 10 160 |
| Total | 5345 | 7710 | 6736 | 19 790 |
Sample selection
We conducted the baseline survey for the evaluation in 2016–2017. In Bihar, a census was undertaken and full household listing was conducted to identify adolescent girls aged 10–19 years, pregnant women and mothers of children under 2 in all programme areas. Respondents for each of the three target groups were then selected by simple random sampling. In Chhattisgarh, all villages in designated programme site were paired on the basis of population size and whether they had held a monthly VHSND for the last 3 months. Forty such pairs were then randomly selected for data collection, and all eligible respondents in each of the three target groups in these 80 villages were surveyed. In Odisha, all eligible target groups in 26 purposively identified Gram Panchayats—12 intervention and 14 control were surveyed.
Tools
Bilingual questionnaire (Bihar: English and Hindi, Chhattisgarh: English and Hindi and Odisha: English and Odia) for all target groups were developed, field tested and standardised for all states. In baseline, information obtained included but was not limited to sociodemographic and household characteristics, educational attainment, diet diversity, household food security and access to services. Anthropometric measurements (weight, height and MUAC) were conducted using standard techniques.19 Weight to the nearest 0.1 kg was recorded using a SECA electronic weighing scale with minimal clothing. Height was taken barefoot to the nearest 0.1 cm using a stadiometer. MUAC was measured to the nearest 0.1 cm with a non-stretchable measuring tape.
Sample coverage in baseline survey
Sample coverage for both interviews and anthropometric measurements was universal in all states except among mothers of children under two in Bihar where 85% of those sampled could be interviewed and coverage for all anthropometric measurements was 83%.
Intervention
Swabhimaan covers 18 nutrition-specific and nutrition-sensitive interventions (table 2).
Table 2.
Nutrition-specific and nutrition-sensitive interventions package, Swabhimaan
| Relevant target group | |||
| Preconception | Pregnancy | Lactation | |
| Improve food and nutrient intake | |||
| 1. Access to generalised household ration through Public Distribution System, a food subsidy scheme | * | * | * |
| 2. Balanced energy protein supplementation through access to supplementary rations | * | * | * |
| 3. Access to knowledge and choices about how to increase maternal dietary diversity | * | * | * |
| 4. Access to knowledge and support for nutrition-sensitive agriculture at home (kitchen garden) and community-based food insecurity coping strategies. | * | * | * |
| Prevent micronutrient deficiencies and anaemia | |||
| 5. IFA supplementation | * | * | * |
| 6. Universal use of iodised salt | * | * | * |
| 7. Calcium supplementation and deworming | x | * | * |
| 8. Access to information and commodities like insecticide treated bed nets for malaria prevention | * | * | * |
| 9. Access to information on preventing tobacco and alcohol use in pregnancy | x | * | * |
| Increase access to health services and special care to nutritionally ‘at-risk’ women (MUAC <23 cm) | |||
| 10. Early registration in outreach services | * | * | x |
| 11. Recording and monitoring of nutritional status and special community-based at-nutritional risk package | x | * | x |
| 12. Quality reproductive health, antenatal and postnatal care | * | * | * |
| 13. Access to knowledge and entitlements for promotion of institutional deliveries and maternity benefits | x | * | * |
| Increase access to education and commodities for WASH | |||
| 14. Sanitation and hygiene (including menstrual hygiene) education | * | * | * |
| 15. Access to safe drinking water and sanitation commodities | * | * | * |
| Prevent early, poorly spaced or unwanted pregnancies | |||
| 16. Promotion of secondary education and education for delaying the age at marriage to legal age | * | x | x |
| 17. Access to information and family planning commodities for delaying age at first pregnancy and prevention of repeated pregnancies | * | * | * |
| 18. Women’s collective voice and empowerment for decision-making to prevent child marriage, violence against women, child spacing and other gender-related issues | * | * | * |
IFA, iron folic acid; MUAC, mid-upper arm circumference; WASH, water, sanitation and hygiene.
In intervention sites, these interventions are delivered through a combination of community-led and systems-led efforts, while control sites receive only systems strengthening interventions. Community-led interventions are delivered through trained community cadre who are members of VOs, namely Poshan Sakhis (lit. ‘Nutrition sister/friend’) or Community Resource Persons (CRPs) and Krishi Mitras (lit. farmer friends) or Village Resource Persons. The community cadre are part of the DAY-NRLM and State Rural Livelihoods Mission (SRLM) implementation structure. In Bihar, a separate cadre of Kishori Sakhis (lit. ‘Adolescent sister/friend’) for reaching out and serving adolescent girls has been created (table 3).
Table 3.
Geographical scope and service providers for community-led interventions under Swabhimaan
| Bihar | Chhattisgarh | Odisha | Total | |
| Revenue villages | 77 | 111 | 168 | 356 |
| CLF and related (Tier-3) | 5 | 4 | 12 | 21 |
| VOs (Tier 2) | 72 | 80 | 79 | 231 |
| Poshan Sakhis or CRPs of Tier 2 | 72 | 100 | 79 | 251 |
| Kishori Sakhis of Tier 2 | 72 | – | – | 72 |
| SHGs (Tier-1) | 1985 | 1488 | 702 | 4175 |
| VRPs/Krishi mitras | 115 | 80 | 39 | 234 |
CLF, cluster-level federation; CRPs, community resource persons; SHGs, self-help groups; VOs, village organisations; VRPs, village resource persons.
Poshan Sakhis and Kishori Sakhis undergo 3 days of pre-service training on integrated nutrition microplanning, which includes a theoretical orientation and practical on consultative identification and prioritisation of nutrition and related problems among target groups in their village/s, developing an annual plan of activities including a budget to address these problems, the use of MUAC tapes, recording and using MUAC measurements for screening nutritionally ‘at-risk’ adolescent girls and women. As no standard MUAC cut-offs are available for screening adolescent girls at risk of undernutrition and <21 cm as well as <22 cm have been reported in research, a stricter cut-off of <19 cm is being used to identify those, most at risk.20–22 In addition, clinical examination for signs of anaemia is also done followed by a diagnostic test for blood haemoglobin level by a health service provider at VHSND. Post-training, they cofacilitate the development of the integrated nutrition microplan with the block coordinator/supervisor through a 12-day process, which can spread over almost 2 months. The process entails microplanning at VO level, its validation by reaching out to the most vulnerable communities and village clusters, then consolidation of all VO plans at CLF and block levels. Poshan Sakhis and Kishori Sakhis are then trained over 3 days on use of participatory learning and action to facilitate monthly women’s group and adolescent girls’ group meetings. Poshan Sakhis and Kishori Sakhis lead activities in their village/s as per decided activities in the microplan. More cost-intensive and complex grant management activities are led by CLFs (table 4).
Table 4.
Community-led interventions under Swabhimaan
| Responsible agency/service provider | Intervention | Frequency |
| Village organisation (VO) | ||
| Social action committee | Selection of Poshan Sakhi (1 per VO) | One time |
| Poshan sakhi/CRP | Integrated nutrition microplanning (12 days over 2 months) |
Once, followed by annual review |
| Maitri bethak (lit. friendly meeting) of women open to non-group members using Participatory Learning and Action | Monthly | |
| One additional monthly home visit/group meeting of nutritionally ‘at-risk’ women | Monthly | |
| Krishi mitra/VRP | Maitri kishan bethak (lit. friendly farmers meeting) on nutrition-sensitive agriculture Participatory Learning and Action | Monthly |
| Home-based Poshan beds/backyard poultry | Monthly | |
| CLF | ||
| Social action committee | Families with women and children at risk of undernutrition linked to agripoultry linkage and social protection schemes | Monthly |
| Loans for secondary education | Monthly | |
| Creating farmer training school sites | Monthly | |
| Training for Poshan sakhi and Krishi mitras | Quarterly | |
| Newly wed couples meetings | Biannual | |
| Entitlement camps and health checkups for SHG members | Biannual | |
| Review of integrated nutrition plan | Annual |
CLF, cluster-level federation; CRP, community resource person; SHG, self-help group; VRP, Village Resource Person.
The CRPs receive INR450 (US$7) for developing the poshan microplan and thereafter a similar incentive every month for completed activities. CLFs also receive grants including: INR500 (~US$ 7) for meetings with newly wed couples; INR500 for each ‘welcome kit’ given to newlywed couples with essential items like IFA, contraceptives, sanitary napkins; INR1500 (~US$22) for review of each VO’s integrated nutrition microplan; and INR5000 (~US$77) for developing farmer training school sites which are model nutri-farms for training farmer producer group members interested in nutri-sensitive agriculture.
The system strengthening activities include five components:
Strengthening VHSNDs to improve access to antenatal care, family planning and micronutrient supplementation through quarterly trainings of health service providers, monthly review of nutrition indicators, and the identification of women at risk of undernutrition (MUAC <23 cm) for special supplementary food and counselling.
Strengthening adolescent health days to improve access to adolescent health and nutrition services via quarterly trainings of health service providers.
An extended VHSND once every 6 months for newly weds and women, including individual counselling and information about entitlement camps.
Annual training and follow-up meetings with service providers from food security, Integrated Child Development Services (ICDS), water and sanitation departments to help them improve the delivery of entitlements and services.
Ensuring regular review meetings with representation across government departments involved in service delivery.
Thus, in addition to DAY-NRLM, system strengthening activities engage four other government departments: Department of Woman and Child Development for increasing ICDS reach and quality, Department of Health and Family Welfare for VHSND strengthening, Department of Water and Sanitation for improving water quality and achieving open defecation free villages and districts, and finally Department of Civil and Food Supply for increasing coverage of food subsidy schemes.
The theory of change for Swabhimaan is presented in online supplementary file 1.
bmjopen-2019-031632supp001.pdf (834KB, pdf)
Blinding
It is not possible to blind participants to allocation, but data collection teams and analysts are blind to allocation.
Data analysis
In each state, we will assess the comparability of intervention and control areas at baseline by examining area-level and individual-level characteristics, including: the number of SHGs and VOs in each area, the sociodemographic profile of respondents and their households (caste, literacy and assets) and key evaluation outcomes at baseline.
The final impact analysis will be by intention to treat, comparing primary and secondary outcomes in five intervention areas and five control areas. This analysis will be carried out at an individual level, adjusting for clustering at the level of the village and VO, using linear and logistic random effects models in STATA V.14. We will use the difference-in-difference method to compare primary and secondary outcomes between intervention and control areas at endline, adjusting for their baseline values and for other characteristics that differed significantly between the two areas at baseline. We will present analyses both a state level, and conducted a pooled analysis with data from all states.
Patient and public involvement
This research did not have any patients. The public (community) was involved in the design and implementation of the intervention package at the village level but not in the evaluation. Public were not invited to contribute to the writing or editing of this document for readability or accuracy.
Process monitoring and progress review
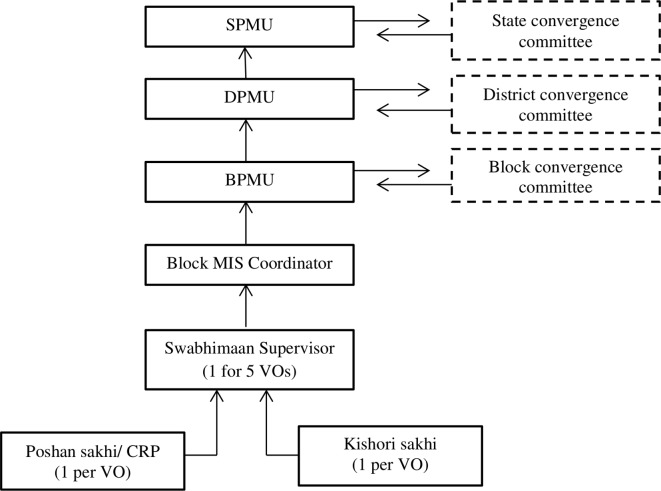
In addition to the impact evaluation described above, we are conducting process monitoring. The process monitoring system is based on the reporting structures within the SRLM (figure 2).
Figure 2.
SRLM organisation structure and its adaptation in Swabhimaan, Bihar. BPMU, Block Project Management Unit; CRP, Community Resource Person; DPMU, District Project Management Unit; MIS, Management Information System; SPMU, State Project Management Unit; SRLM, State Rural Livelihoods Mission; VO, Village Organisation.
SRLMs have a project management units at state, district and block levels (SPMU, DPMU, BPMU). The block management information system coordinator is the reporting link between the CRPs and their supervisors and the BPMU. In Bihar, a supervisor position has been embedded in the organisation structure while in Chhattisgarh and Odisha, supervisory staff is a representative from the SRLM’s organogram.
CRPs/Poshan sakhis collect data and report coverage of community-led interventions on monthly monitoring formats which are available in both web-based and paper formats. Key performance indicators include:
Target women who attended the VHSND (%).
Target women who attended the maitri bethak (%).
At-risk women visited fortnightly in their home visits (%).
At-risk women attended fortnightly food demonstration and counselling session (%).
Target newly wed who attended the couple meeting (reported quarterly).
Target groups who attended the women only camps (reported biannually).
All CRP reports are collated monthly at the block level. A CLF-level review of the progress on performance indicators and the planned activities as per the poshan microplan is planned for every quarter, however, Swabhimaan has mixed experience in achieving this with Chhattisgarh undertaking monthly reviews while other states undertaking annual reviews. DAY-NRLM hosts annual reviews with the respective SRLMs for stock taking and approval for next annual cycle.
Timeline
Baseline was completed in 2017. The first phase of implementation is between 2017 and 2020. Midline and endline for first phase will be completed in 2019 and 2021, respectively.
Ethics and dissemination
Written informed consent was obtained from all subjects. The impact evaluation has been registered with the Registry for International Development Impact Evaluations (RIDIE-STUDY-ID-58261b2f46876)23 and Indian Council of Medical Research National Clinical Trials Registry of India (CTRI/2016/11/007482).
Government of India is committed to reviewing its antenatal care guidelines with focus on nutrition in addition to other components of antenatal care in line with new recommendations of WHO, 2016.24 Evidence from the evaluation will inform maternal nutrition policy as well as incorporation of nutrition interventions for adolescent girls and newly wed women in existing and new policies.
Conclusion and implications
Being a controlled evaluation, Swabhimaan will measure impact of community-led interventions over standard practice of public health and nutrition services for adolescent girls, pregnant women and mothers of children under two. A third party evaluator, International Institute for Population Sciences, India, with no role in implementation, further bolsters the evaluation design. Swabhimaan operates in complete alignment with DAY-NRLM’s mandate under the joint convergent action plan for Poshan Abhiyaan. In coordination with departments of Woman and Child Development and Health, DAY-NRLM shares responsibility for (1) SHG members mobilising communities for using entitled services through Department of Health, (2) SHG members participating in Behaviour Change and Communication activities, promoting recommended health, nutrition and WASH behaviours, (3) common use of infrastructure by the three departments such as use of Panchayat halls for SHG and VO meetings and (4) promoting nutri-based livelihoods for women’s collectives. These activities are integrated in VO’s poshan microplans and system strengthening activities under Swabhimaan.
Swabhimaan operates as three different models in Bihar, Chhattisgarh and Odisha. Bihar is the demonstration and learning site, with financial support for human resources and activities through UNICEF India. In Chhattisgarh and Odisha, the initiative is almost completely led by the respective SRLMs with UNICEF to SRLM cost ratio at 1:5. UNICEF India supports some human resource at state and block levels, but none at the VO level in these two states. By 2020, it is planned to advocate for increased number of positions at SRLMs to support implementation of the convergent action plan and create a system of CRPs graduating to block-level positions in the three states. UNICEF India’s support on human resource will gradually lessen. DAY-NRLM has recognised the Chhattisgarh model of Swabhimaan as a best practice for integrating health, nutrition and WASH on the SHG platform and has planned to take elements from the initiative for horizontal expansion to poorest resource blocks in other states. Findings from the Swabhimaan midline survey will inform scale-up plans in other states.
bmjopen-2019-031632supp002.pdf (704.1KB, pdf)
bmjopen-2019-031632supp003.pdf (1.8MB, pdf)
bmjopen-2019-031632supp004.pdf (763.8KB, pdf)
Supplementary Material
Acknowledgments
Shivani Dar (UNICEF Bihar) and Anoop Jha (Independent consultant) supported stakeholder coordination in Bihar. Anoop Jha was part of implementation team in Bihar. Shibanand Rath (Ekjut) participated in the designing workshop and made significant contribution to the participatory learning action component of the initiative. CM Singh (AIIMS, Patna, Bihar) managed evaluation teams in Bihar. Aparajita Chattopadhyay, Preeti Dhillon, Prakash H. Fulpagare and Konsam Dinachandra Singh (IIPS) supported quality control in baseline survey and are part of the evaluation team. Sarita Anand (Roshni, Lady Irwin College, New Delhi) leads process documentation of the initiative. Rachna Sharma (UNICEF India) and Dhruv Sengupta (DAY-NRLM) offer technical advice on specific components related to communication and government coordination, respectively.
Footnotes
Contributors: VS and ADW provide technical oversight and VS is the national focal point of the initiative. NK is key contact in NRLM and advises on effective utilisation of NRLM platforms. VS, AB, SB, NN, AD, RNP, SonS, AL and NK were involved in designing Swabhimaan initiative at national and state level. RG, VN and NN contributed to the Participatory Learning Action component of the initiative. DS and US contributed to the agriculture component. SB, RNP, SonS, AL, NaA, FS, MP and PM are involved in the implementation of the initiative in Bihar, Chhattisgarh and Odisha. BM, SonS and ApP are government counterparts; BM provides management support in Odisha and SomS and ApP in Bihar. AuP, HS and SU advise on evaluation of the initiative and AuP drafted the registered protocol. NeA, VB, MR, BS, RRS, SP and LKD were part of evaluation team; NeA, VB and MR led baseline evaluation in Bihar, Odisha and Chhattisgarh, respectively. VS, AB and AuP drafted the manuscript. All authors reviewed the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Ethics approval: The baseline survey was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Institutional Ethics Committee of the All India Institute of Medical Sciences (AIIMS), Bihar, Chhattisgarh and AIIMS, Odisha in July 2016 (see online supplementary files 2–4).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013;382:427–51. 10.1016/S0140-6736(13)60937-X [DOI] [PubMed] [Google Scholar]
- 2. Bhutta ZA, Das JK, Rizvi A, et al. Evidence-Based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet 2013;382:452–77. 10.1016/S0140-6736(13)60996-4 [DOI] [PubMed] [Google Scholar]
- 3. International Institute for Population Sciences (IIPS) and Macro International 2015-16. National family health survey (NFHS-4), 2015–16: India Factsheet.
- 4. Ministry of Home Affairs Office of the registrar general and census commissioner, India. population enumeration data 2011.
- 5.https://www.icds-wcd.nic.in/nnm/home.htm#
- 6. Prost A, Colbourn T, Seward N, et al. Women's groups practising participatory learning and action to improve maternal and newborn health in low-resource settings: a systematic review and meta-analysis. Lancet 2013;381:1736–46. 10.1016/S0140-6736(13)60685-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fottrell E, Azad K, Kuddus A, et al. The Effect of Increased Coverage of Participatory Women’s Groups on Neonatal Mortality in Bangladesh. JAMA Pediatr 2013;167:816–25. 10.1001/jamapediatrics.2013.2534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Colbourn T, Nambiar B, Bondo A, et al. Effects of quality improvement in health facilities and community mobilization through women's groups on maternal, neonatal and perinatal mortality in three districts of Malawi: MaiKhanda, a cluster randomized controlled effectiveness trial. Int Health 2013;5:180–95. 10.1093/inthealth/iht011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. More NS, Bapat U, Das S, et al. Community mobilization in Mumbai slums to improve perinatal care and outcomes: a cluster randomized controlled trial. PLoS Med 2012;9:e1001257 10.1371/journal.pmed.1001257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tripathy P, Nair N, Barnett S, et al. Effect of a participatory intervention with women's groups on birth outcomes and maternal depression in Jharkhand and Orissa, India: a cluster-randomised controlled trial. Lancet 2010;375:1182–92. 10.1016/S0140-6736(09)62042-0 [DOI] [PubMed] [Google Scholar]
- 11. The World Bank Indonesia’s PNPM Generasi Programme. Final impact evaluation 2011.
- 12. TANGO International Inc SHOUHARDO a title II programme of USAID. final evaluation report 2009.
- 13. Saha S, Annear P, Pathak S. The effect of self-help groups on access to maternal health services: evidence from rural India. Int J Equity Health 2013;12:36 10.1186/1475-9276-12-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. VOICES A report on success and failure of SHGs in India- impediments and paradigms of success. 2008. Report submitted to planning Commission, government of India.
- 15. National Rural Livelihoods Mission, Ministry of Rural Development, Government of India . Briefing book, 2012. [Google Scholar]
- 16. Sethi V, Bhanot A, Bhalla S, et al. Partnering with women collectives for delivering essential women’s nutrition interventions in tribal areas of eastern India: a scoping study. J Health Popul Nutr 2017;36 10.1186/s41043-017-0099-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Office of the registrar general and census commissioner, India Annual Health Survey. Clinical, Anthropometry and Biochemical Survey, Purnia, Bihar 2012.
- 18. Kumar P, Sareen N, Agrawal S, et al. Screening maternal acute malnutrition using adult mid-upper arm circumference in resource-poor settings. Indian J Community Med 2018;43:132–4. 10.4103/ijcm.IJCM_248_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. World Health Organization (WHO) Physical status: the use and interpretation of anthropometry. Report of a who expert Committee. World health organ technical report series. Geneva: WHO, 1995. [PubMed] [Google Scholar]
- 20. Bulliyya G, Mallick G, Sethy GS, et al. Hemoglobin status of non-school going adolescent girls in three districts of Orissa, India. Int J Adolesc Med Health 2007;19:395–406. 10.1515/IJAMH.2007.19.4.395 [DOI] [PubMed] [Google Scholar]
- 21. Mramba L, Ngari M, Mwangome M, et al. A growth reference for mid upper arm circumference for age among school age children and adolescents, and validation for mortality: growth curve construction and longitudinal cohort study. BMJ 2017;358 10.1136/bmj.j3423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tang AM, Dong K, Deitchler M, et al. Use of cutoffs for Mid-Upper arm circumference (MUAC) as an indicator or predictor of nutritional and health related outcomes in adolescents and adults: a systematic review. Washington, DC: FHI 360/FANTA, 2013. [Google Scholar]
- 23. Integrated multisectoral strategy to improve girls’ and women’s nutrition before conception, during pregnancy and after birth in India (Swabhimaan): prospective, non-randomised controlled evaluation. Principal investigator: Sethi V. Co-Principal investigator: Unisa S. Available: http://ridie.3ieimpact.org/index.php?r=search/detailView&id=485 [DOI] [PMC free article] [PubMed]
- 24. World Health Organization WHO recommendations on antenatal care for a positive pregnancy experience [Internet]. WHO, 2016. Available: http://apps.who.int/iris/bitstream/10665/250796/1/9789241549912-eng.pdf [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-031632supp001.pdf (834KB, pdf)
bmjopen-2019-031632supp002.pdf (704.1KB, pdf)
bmjopen-2019-031632supp003.pdf (1.8MB, pdf)
bmjopen-2019-031632supp004.pdf (763.8KB, pdf)